Magnitude, Temporal Trends, and Inequalities in the DALYs and YLDs of Nutritional Deficiency among Older Adults in the Western Pacific Region: Findings from the Global Burden of Disease Study 1990–2019
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Statistical Analysis
3. Results
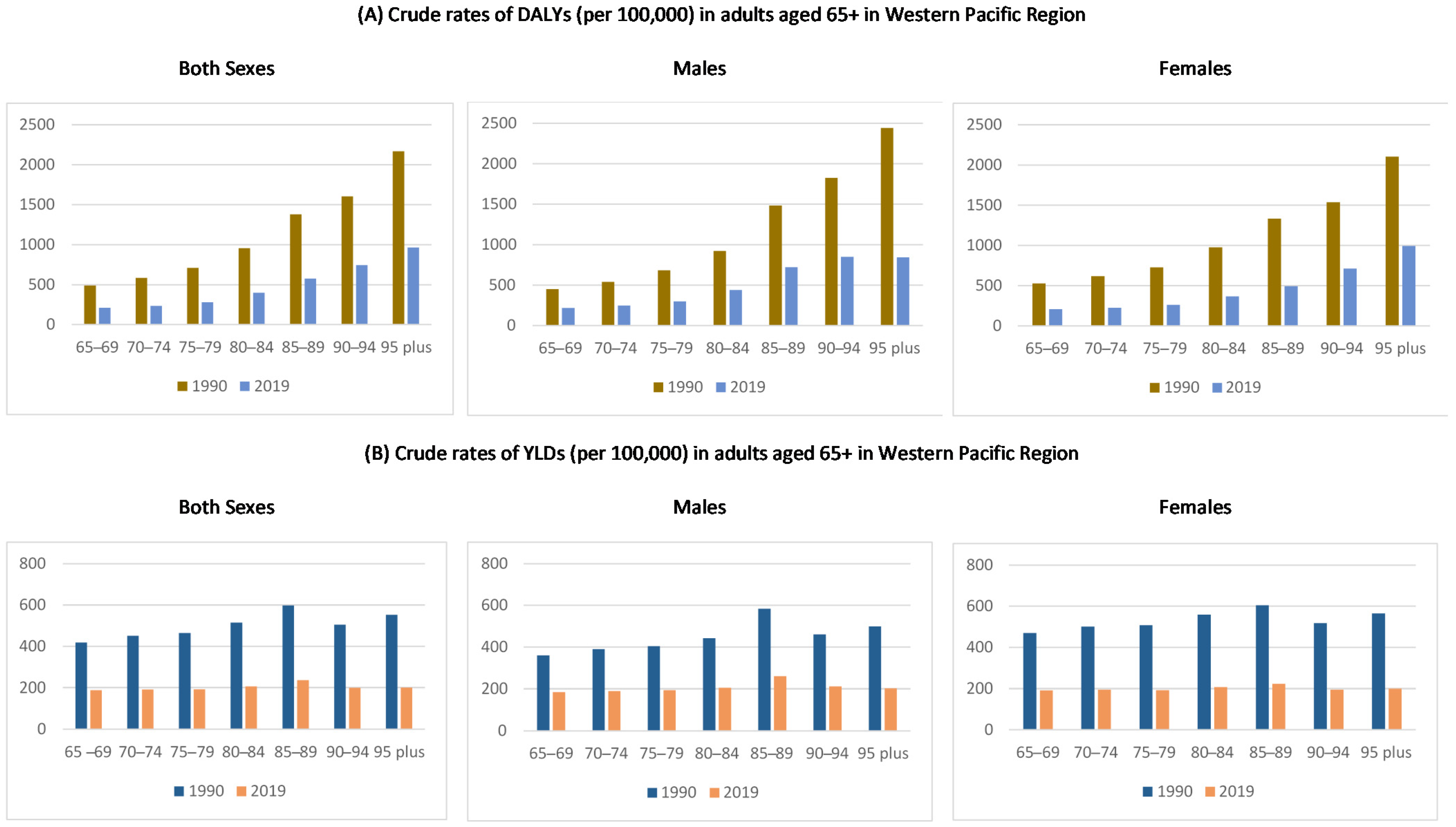
3.1. Age-Specific Crude Rates of DALYs and YLDs Attributed to Nutritional Deficiency in the Western Pacific Region
3.2. Temporal Trends in DALYs and YLD Attributed to Nutritional Deficiency in the Western Pacific Region
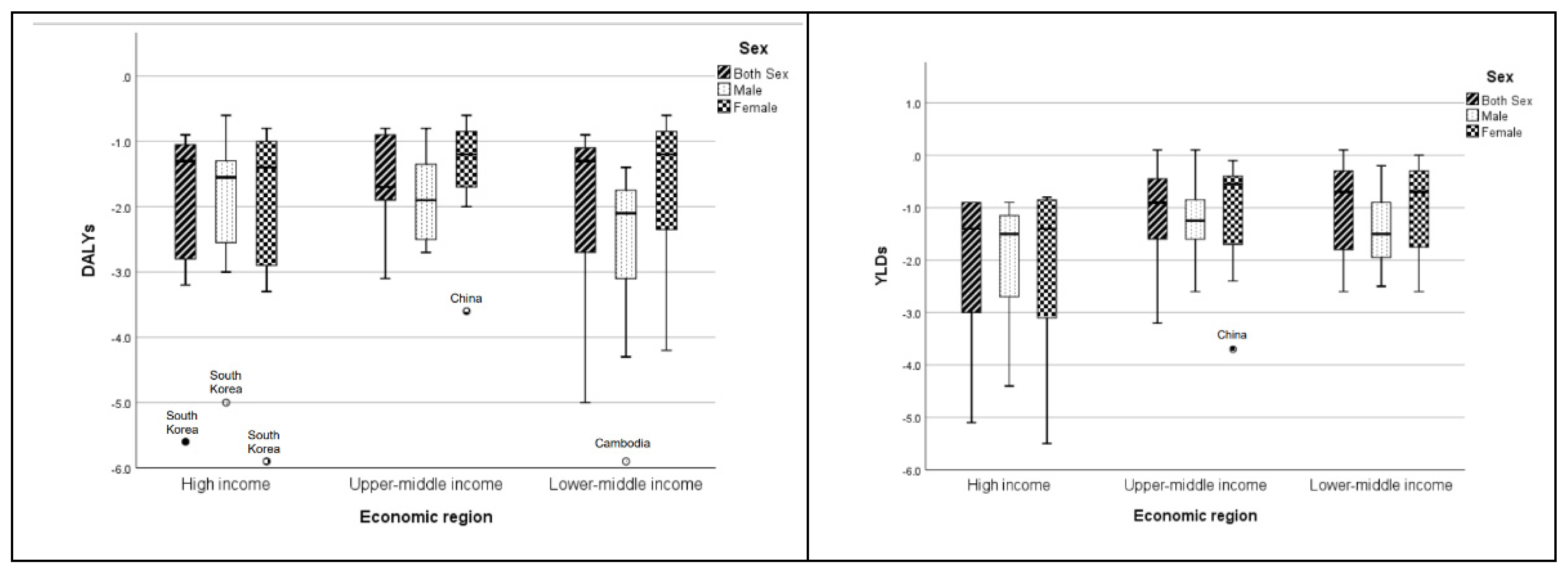
3.3. Relationship of the Age-Standardized Rates in DALYs and YLDs with Sex, SDI, and Time
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Regional Action Plan on Healthy Ageing in the Western Pacific. Available online: https://www.who.int/publications/i/item/9789290619352 (accessed on 2 September 2021).
- United Nations Department of Economic and Social Affairs. World Population Prospects: The 2019 Revision; United Nations Department of Economic and Social Affairs, Population Division: New York, NY, USA, 2019; Available online: https://population.un.org/wpp/ (accessed on 17 September 2021).
- World Report on Ageing and Health 2015. Available online: http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=9E053CD8C6E80CC827437CA7B9BADC8F?sequence=1 (accessed on 3 September 2021).
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.C.; et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin. Nutr. 2019, 38, 10–47. [Google Scholar] [CrossRef] [Green Version]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Norman, K.; Haβ, U.; Pirlich, M. Malnutrition in older adults–recent advances and remaining challenges. Nutrients 2021, 13, 2764. [Google Scholar] [CrossRef]
- Baugreet, S.; Hamill, R.M.; Kerry, J.P.; McCarthy, S.N. Mitigating nutrition and health deficiencies in older adults: A role for food innovation? J. Food Sci. 2017, 82, 848–855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yannakoulia, M.; Mamalaki, E.; Anastasiou, C.A.; Mourtzi, N.; Lambrinoudaki, I.; Scarmeas, N. Eating habits and behaviors of older people: Where are we now and where should we go? Maturitas 2018, 114, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Leij-Halfwerk, S.; Verwijs, M.H.; van Houdt, S.; Borkent, J.W.; Guaitoli, P.R.; Pelgrim, T.; Heymans, M.W.; Power, L.; Visser, M.; Corish, C.A.; et al. Prevalence of protein-energy malnutrition risk in European older adults in community, residential and hospital settings, according to 22 malnutrition screening tools validated for use in adults >/=65 years: A systematic review and meta-analysis. Maturitas 2019, 126, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Crichton, M.; Craven, D.; Mackay, H.; Marx, W.; de van der Schueren, M.; Marshall, S. A systematic review, meta-analysis and meta-regression of the prevalence of protein-energy malnutrition: Associations with geographical region and sex. Age Ageing 2019, 48, 38–48. [Google Scholar] [CrossRef]
- Gentile, S.; Lacroix, O.; Durand, A.C.; Cretel, E.; Alazia, M.; Sambuc, R.; Bonin-Guillaume, S. Malnutrition: A highly predictive risk factor of short-term mortality in elderly presenting to the emergency department. J. Nutr. Health Aging 2013, 17, 290–294. [Google Scholar] [CrossRef]
- Komici, K.; Vitale, D.F.; Mancini, A.; Bencivenga, L.; Conte, M.; Provenzano, S.; Grieco, F.V.; Visaggi, L.; Ronga, I.; Cittadini, A.; et al. Impact of malnutrition on long-term mortality in elderly patients with acute myocardial infarction. Nutrients 2019, 11, 224. [Google Scholar] [CrossRef] [Green Version]
- Söderström, L.; Rosenblad, A.; Thors Adolfsson, E.; Bergkvist, L. Malnutrition is associated with increased mortality in older adults regardless of the cause of death. Br. J. Nutr. 2017, 117, 532–540. [Google Scholar] [CrossRef] [Green Version]
- Khalatbari-Soltani, S.; Marques-Vidal, P. The economic cost of hospital malnutrition in Europe; a narrative review. Clin. Nutr. ESPEN 2015, 10, e89–e94. [Google Scholar] [CrossRef] [Green Version]
- Yeung, S.S.Y.; Chan, R.S.M.; Kwok, T.; Lee, J.S.W.; Woo, J. Malnutrition according to GLIM criteria and adverse outcomes in community-dwelling Chinese older adults: A prospective analysis. J. Am. Med. Dir. Assoc. 2021, 22, 1953–1959. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Sánchez, B.; Sulo, S.; Carnicero, J.A.; Rueda, R.; Rodriguez-Mañas, L. Malnutrition prevalence and burden on healthcare resource use among Spanish community-living older adults: Results of a longitudinal analysis. Clin. Outcomes Res. 2020, 12, 355–367. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Peng, W.; Berry, E.M. Global nutrition 1990–1995: A shrinking hungry, and expanding fat world. PLoS ONE 2019, 13, e0194821. [Google Scholar] [CrossRef] [Green Version]
- Ong, S.; Woo, J.; Parikh, P.; Chan, R.; Jianqin, S.; Mun, C.Y.; Wee, S.L.; Thu, N.N.; Thang, P.; Setiati, S.; et al. Addressing nutritional requirements of ageing consumers in Asia—Recommendations from an expert workshop. Asia Pac. J. Clin. Nutr. 2019, 28, 204–213. [Google Scholar] [CrossRef]
- World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519 (accessed on 2 September 2021).
- Global Burden of Disease (GBD). Available online: http://www.healthdata.org/gbd/2019 (accessed on 2 September 2021).
- GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: A comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1160–1203. [Google Scholar] [CrossRef]
- GBD 2019 Risk Factor Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- Kim, H.J.; Fay, M.P.; Feuer, E.J.; Midthune, D.N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- Brownie, S.; Muggleston, H.; Oliver, C. The 2013 Australian dietary guidelines and recommendations for older Australians. Aust. Fam. Physician 2015, 44, 311–315. [Google Scholar]
- Singapore Standards Council. Guidelines on Nutrition and Food Service for Older Adults, 1st ed.; Enterprise Singapore: Singapore, 2015. [Google Scholar]
- Ministry of Health. Food and Nutrition Guidelines for Healthy Older People: A Background Paper, 1st ed.; Ministry of Health: Wellington, New Zealand, 2013. [Google Scholar]
- Robinson, S.M. Improving nutrition to support healthy ageing: What are the opportunities for intervention? Proc. Nutr. Soc. 2018, 77, 257–264. [Google Scholar] [CrossRef]
- Shlisky, J.; Bloom, D.E.; Beaudreault, A.R.; Tucker, K.L.; Keller, H.H.; Freund-Levi, Y.; Fielding, R.A.; Cheng, F.W.; Jensen, G.L.; Wu, D.; et al. Nutritional considerations for healthy aging and reduction in age-related chronic disease. Adv. Nutr. 2017, 8, 17–26. [Google Scholar] [CrossRef] [Green Version]
- Saffel-Shrier, S.; Johnson, M.A.; Francis, S.L. Position of the Academy of Nutrition and Dietetics and the Society for Nutrition Education and Behavior: Food and nutrition programs for community-residing older adults. J. Nutr. Educ. Behav. 2019, 51, 781–797. [Google Scholar] [CrossRef]
- Dorner, B.; Friedrich, E.K. Position of the Academy of Nutrition and Dietetics: Individualized nutrition approaches for older adults: Long-term care, post-acute care, and other settings. J. Acad. Nutr. Diet. 2018, 118, 724–735. [Google Scholar] [CrossRef] [Green Version]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cereda, E.; Cruz-Jentoft, A.; Goisser, S.; de Groot, L.; Groβhauser, F.; Kiesswetter, E.; Norman, K.; et al. Management of malnutrition in older patients—Current approaches, evidence and open questions. J. Clin. Med. 2019, 8, 974. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhu, Y.; Minović, I.; Dekker, L.H.; Eggersdorfer, M.L.; van Zon, S.K.R.; Reijneveld, S.A.; Kootstra-Ros, J.E.; Kema, I.P.; Bakker, S.J.L.; Navis, G.J.; et al. Vitamin status and diet in elderly with low and high socioeconomic status: The Lifelines-MINUTHE Study. Nutrients 2020, 12, 2659. [Google Scholar] [CrossRef]
- Nutrition in the Western Pacific. Available online: https://www.who.int/westernpacific/health-topics/nutrition (accessed on 2 September 2021).
- Park, H.K. Nutrition policy in South Korea. Asia Pac. J. Clin. Nutr. 2008, 17, 343–345. [Google Scholar] [PubMed]
- Nakamura, T. Nutritional policies and dietary guidelines in Japan. Asia Pac. J. Clin. Nutr. 2011, 20, 452–454. [Google Scholar] [PubMed]
- Lee, B.L. Dietary guidelines in Singapore. Asia Pac. J. Clin. Nutr. 2011, 20, 472–476. [Google Scholar]
- Ministry of Health Malaysia. National Plan of Action for Nutrition of Malaysia III 2016–2025, 1st ed.; National Coordinating Committee on Food and Nutrition: Putrajaya, Malaysia, 2016. [Google Scholar]
- Policy—National Nutrition Strategy for 2011–2020, with a Vision toward 2030. Available online: https://extranet.who.int/nutrition/gina/en/node/11519#:~:text=By%20the%20year%202020%2C%20the,and%20obesity%2Foverweight%20will%20be (accessed on 2 September 2021).
- Policy—Fiji Plan of Action for Nutrition (FPAN). Available online: https://extranet.who.int/nutrition/gina/en/node/8151 (accessed on 2 September 2021).
- Vanuatu National Plan of Action on Food and Nutrition Security. Available online: http://extwprlegs1.fao.org/docs/pdf/van158165.pdf (accessed on 2 September 2021).
- Oksuzyan, A.; Singh, P.K.; Christensen, K.; Jasilionis, D. A cross-national study of the gender gap in health among older adults in India and China: Similarities and disparities. Gerontologist 2018, 58, 1156–1165. [Google Scholar] [CrossRef]
- McCracken, K.; Phillips, D.R. Global Health: An Introduction to Current and Future Trends, 2nd ed.; Routledge: London, UK, 2007. [Google Scholar]
- World Health Organization Western Pacific Region. Advancing Health Through Attention to Gender, Equity and Human Rights: Stories from the Western Pacific Region, 1st ed.; World Health Organization: Manila, Philippines, 2017.
- Legato, M.J.; Johnson, A.J.; Manson, J.E. Consideration of sex difference in medicine to improve health care and patient outcomes. JAMA 2016, 316, 1865–1866. [Google Scholar] [CrossRef] [PubMed]
- Doblhanmmer, G.; Gumà, J. A Demographic Perspective on Gender, Family and Health in Europe, 1st ed.; Springer International Publishing: Cham, Switzerland, 2018. [Google Scholar]
- Graham, A.; D’Andrea, A. Gender and Human Rights in Coastal Fisheries and Aquaculture: A Comparative Analysis of Legislation in Fiji, Kiribati, Samoa, Solomon Islands, Tonga and Vanuatu, 1st ed.; SPC: Noumea, New Caledonia, 2021. [Google Scholar]
- World Health Organization Western Pacific Region. Celebrating Women’s Voices in the Western Pacific Region: Leadership, Diversity and Health, 1st ed.; World Health Organization: Geneva, Switzerland, 2021.
| Burden | Sex | 1990 | 2019 | AAPC |
|---|---|---|---|---|
| DALYs | Both sexes | 697.95 (696.03, 699.87) | 290.95 (290.25, 291.65) | −3.0 (−3.8, −2.2) |
| Males | 676.66 (673.38, 679.94) | 314.45 (313.31, 315.59) | −2.6 (−2.8, −2.5) | |
| Females | 721.59 (719.09, 724.09) | 274.61 (273.71, 275.51) | −3.3 (−3.6, −3.0) | |
| YLDs | Both sexes | 459.03 (457.55, 460.51) | 195.65 (195.09, 196.21) | −2.9 (−3.1, −2.8) |
| Males | 401.88 (399.64, 404.12) | 195.56 (194.70, 196.42) | −2.5 (−2.6, −2.3) | |
| Females | 504.43 (502.41, 506.45) | 196.49 (195.93, 197.05) | −3.2 (−3.3, −3.1) |
| Burden | Economic Region | Country (in Descending Order of SDI in 2019) | Both Sexes | Male | Female |
|---|---|---|---|---|---|
| DALYs | High income | South Korea | −5.6 * (−5.8, −5.3) | −5.0 * (−5.5, −4.5) | −5.9 * (−6.0, −5.8) |
| Japan | −1.2 * (−1.3, −1.2) | −0.6 * (−0.7, −0.4) | −1.4 * (−1.5, −1.4) | ||
| Singapore | −3.2 * (−3.2, −3.2) | −3.0 * (−3.1, −2.9) | −3.3 * (−3.3, −3.3) | ||
| New Zealand | −1.4 * (−1.7, −1.2) | −1.5 * (−1.8, −1.2) | −1.4 * (−1.8, −1.1) | ||
| Australia | −1.0 * (−1.1, −0.9) | −1.3 * (−1.4, −1.1) | −0.8 (−0.9, −0.8) | ||
| Brunei | −2.4 * (−2.8, −2.1) | −2.1 * (−2.4, −1.7) | −2.5 * (−2.7, −2.2) | ||
| Cook Islands | −1.1 * (−1.2, −0.9) | −1.6 * (−1.7, −1.5) | −1.1 * (−1.2, −1.0) | ||
| Palau | −0.9 * (−1.0, −0.9) | −1.3 * (−1.5, −1.2) | −0.9 * (−1.0, −0.9) | ||
| Upper-middle income | Malaysia | −1.9 * (−2.2, −1.6) | −1.7 * (−2.0, −1.4) | −2.0 * (−2.3, −1.7) | |
| Niue | −1.6 * (−1.7, −1.5) | −2.1 * (−2.3, −1.9) | −1.4 (−1.5, −1.3) | ||
| China | −3.1 * (−4.3, −1.9) | −2.3 * (−2.5, −2.1) | −3.6 * (−3.9, −3.4) | ||
| Fiji | −0.9 * (−1.0, −0.8) | −0.8 * (−1.0, −0.7) | −0.9 * (−1.2, −0.7) | ||
| Samoa | −0.9 * (−1.0, −0.8) | −1.5 * (−1.7, −1.4) | −0.6 * (−0.7, −0.5) | ||
| Tonga | −0.8 * (−0.9, −0.7) | −1.2 * (−1.6, −0.1) | −0.8 * (−1.0, −0.6) | ||
| Tuvalu | −1.8 * (−1.9, −1.8) | −2.7 * (−2.8, −2.6) | −1.3 * (−1.4, −1.2) | ||
| Marshall Islands | −1.9 * (−2.1, −1.7) | −2.7 * (−3.0, −2.4) | −1.1 * (−1.2, −1.1) | ||
| Lower-middle income | Philippines | −2.0 * (−2.3, −1.7) | −2.1 * (−2.5, −1.8) | −2.0 * (−2.4, −1.7) | |
| Nauru | −0.9 * (−1.1, −0.8) | −1.4 * (−1.5, −1.3) | −0.9 * (−1.0, −0.8) | ||
| Vietnam | −3.4 * (−3.5, −3.3) | −4.0 * (−4.2, −3.9) | −2.7 * (−2.8, −2.7) | ||
| Mongolia | −1.7 * (−1.8, −1.6) | −1.8 * (−2.0, −1.7) | −1.6 * (−1.7, −1.5) | ||
| Federated States of Micronesia | −1.3 * (−1.4, −1.3) | −2.2 * (−2.3, −1.1) | −1.2 * (−1.2, −1.1) | ||
| Kiribati | −1.1 * (−1.1, −1.0) | −1.7 * (−1.8, −1.6) | −1.0 * (−1.0, −0.9) | ||
| Laos | −3.6 * (−3.7, −3.5) | −4.3 * (−4.5, −4.1) | −3.1 * (−3.2, −3.0) | ||
| Vanuatu | −0.9 * (−1.0, −0.8) | −1.5 * (−1.6, −1.4) | −0.7 * (−0.8, −0.6) | ||
| Cambodia | −5.0 * (−5.1, −4.9) | −5.9 * (−5.9, −5.8) | −4.2 * (−4.3, −4.1) | ||
| Solomon Islands | −1.1 (−1.3, −1.0) | −2.1 * (−2.2, −2.0) | −0.8 * (−0.9, −0.8) | ||
| Papua New Guinea | −1.1 * (−1.3, −0.9) | −1.9 * (−2.3, −1.6) | −0.6 * (−0.7, −0.5) | ||
| YLDs | High income | South Korea | −5.1 * (−5.3, −5.0) | −4.4 * (−4.6, −4.2) | −5.5 * (−5.7, −5.4) |
| Japan | −3.0 * (−3.0, −3.0 | −2.7 * (−2.8, −2.7) | −3.1 * (−3.1, −3.1) | ||
| Singapore | −3.0 * (−3.0, −3.0) | −2.7 * (−2.8, −2.7) | −3.1 * (−3.1, −3.1) | ||
| New Zealand | −1.2 * (−1.3, −1.0) | −0.9 * (−1.2, −0.6) | −1.2 * (−1.3, −1.0) | ||
| Australia | −0.9 * (−1.0, −0.8) | −1.0 * (−1.3, −0.6) | −0.8 * (−0.9, −0.7) | ||
| Brunei | −1.6 * (−1.6, −1.6) | −1.6 * (−1.7, −1.6) | −1.6 * (−1.7, −1.5) | ||
| Cook Islands | −0.9 * (−1.0, −0.8) | −1.4 * (−1.5, −1.3) | −0.9 * (−1.0, −0.8 | ||
| Palau | −0.9 * (−1.0, −0.8 | −1.3 * (−1.5, −1.1) | −0.8 * (−0.9, −0.7) | ||
| Upper-middle income | Malaysia | −2.1 * (−2.2, −1.9) | −1.7 * (−1.9, −1.5) | −2.4 * (−2.5, −2.3) | |
| Niue | −1.1 * (−1.3, −1.0) | −1.5 * (−1.9, −1.1) | −1.0 * (−1.2, −0.8) | ||
| China | −3.2 * (−3.3, −3.1) | −2.6 * (−2.8, −2.4) | −3.7 * (−3.8, −3.6) | ||
| Fiji | 0.1 * (0.0, 0.2) | 0.1 (−0.1, 0.2) | −0.1 * (−0.2, −0.1) | ||
| Samoa | −0.5 * (−0.7, −0.4) | −0.8 * (−1.0, −0.6) | −0.4 * (−0.6, −0.3) | ||
| Tonga | −0.4 * (−0.4, −0.3) | −1.0 * (−1.3, −0.7) | −0.4 * (−0.5, −0.3) | ||
| Tuvalu | −1.0 * (−1.1, −1.0) | −1.5 * (−1.6, −1.4) | −0.7 * (−0.8, −0.7) | ||
| Marshall Islands | −0.8 * (−0.9, −0.7) | −0.9 * (−1.0, −0.8) | −0.4 * (−0.4, −0.3) | ||
| Lower-middle income | Philippines | −1.8 * (−1.8, −1.7) | −2.0 * (−2.1, −1.9) | −1.7 * (−1.8, −1.7) | |
| Nauru | −0.4 * (−0.5, −0.2) | −1.1 * (−1.3, −0.9) | −0.5 * (−0.5, −0.4) | ||
| Vietnam | −2.6 * (−2.7, −2.5) | −2.5 * (−2.6, −2.3) | −2.6 * (−2.6, −2.6) | ||
| Mongolia | −1.6 * (−1.7, −1.5) | −1.7 * (−1.7, −1.6) | −1.6 * (−1.7, −1.5) | ||
| Federated States of Micronesia | −0.7 * (−1.0, −0.4) | −1.5 * (−1.7, −1.3) | −0.7 * (−0.7, −0.6) | ||
| Kiribati | −0.3 * (−0.3, −0.2) | −0.9 * (−1.0, −0.8) | −0.2 * (−0.3, −0.2) | ||
| Laos | −1.8 * (−1.9, −1.8) | −1.9 * (−1.9, −1.8) | −1.8 * (−1.9, −1.7) | ||
| Vanuatu | 0.1 * (0.0, 0.2) | −0.2 * (−0.4, −0.0) | 0.0 (−0.0, 0.1) | ||
| Cambodia | −2.0 * (−2.1, −1.9) | −2.1 * (−2.3, −1.9) | −2.0 * (−2.1, −1.9) | ||
| Solomon Islands | −0.2 * (−0.3, −0.1) | −0.9 * (−1.0, −0.8) | −0.4 * (−0.4, −0.3) | ||
| Papua New Guinea | −0.3 * (−0.4, −0.2) | −0.7 * (−0.8, −0.6) | −0.1 * (−0.2, −0.1) |
| Burden | Sex | Mean (95% CI) | Spearman Correlation with SDI (95% CI) |
|---|---|---|---|
| DALYs | Both sexes | 1038.25 (981.45, 1095.05) | −0.899 ** (−0.911, −0.883) |
| Male | 767.31 (721.45, 823.29) | −0.904 ** (−0.913, −0.893) | |
| Female | 1273.75 (120.8.08, 1345.67) | −0.847 ** (−0.867, −0.824) | |
| YLDs | Both sexes | 503.27 (487.02, 519.52) | −0.855 ** (−0.875, −0.830) |
| Male | 298.16 (287.41, 310.15) | −0.682 ** (−0.729, −0.631) | |
| Female | 685.92 (661.83, 709.61) | −0.844 ** (−0.864, −0.820) |
| Factor | DALYs | YLDs |
|---|---|---|
| Sex (Reference = female) | −1273.13 (−1417.43, −1128.83) | −1095.58 (−1144.96, −1046.19) |
| SDI | −6228.80 (−7144.95, −5312.64) | −2303.50 (−2551.79, −2055.20) |
| Sex × SDI | 1317.44 (1077.74, 1557.14) | 1216.17 (1134.13, 1298.20) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leung, D.Y.P.; Cheng, H.-L.; Tyrovolas, S.; Tang, A.S.K.; Liu, J.Y.W.; Tse, M.M.Y.; Lai, C.K.Y.; Molassiotis, A. Magnitude, Temporal Trends, and Inequalities in the DALYs and YLDs of Nutritional Deficiency among Older Adults in the Western Pacific Region: Findings from the Global Burden of Disease Study 1990–2019. Nutrients 2021, 13, 4421. https://doi.org/10.3390/nu13124421
Leung DYP, Cheng H-L, Tyrovolas S, Tang ASK, Liu JYW, Tse MMY, Lai CKY, Molassiotis A. Magnitude, Temporal Trends, and Inequalities in the DALYs and YLDs of Nutritional Deficiency among Older Adults in the Western Pacific Region: Findings from the Global Burden of Disease Study 1990–2019. Nutrients. 2021; 13(12):4421. https://doi.org/10.3390/nu13124421
Chicago/Turabian StyleLeung, Doris Y. P., Hui-Lin Cheng, Stefanos Tyrovolas, Angel S. K. Tang, Justina Y. W. Liu, Mimi M. Y. Tse, Claudia K. Y. Lai, and Alex Molassiotis. 2021. "Magnitude, Temporal Trends, and Inequalities in the DALYs and YLDs of Nutritional Deficiency among Older Adults in the Western Pacific Region: Findings from the Global Burden of Disease Study 1990–2019" Nutrients 13, no. 12: 4421. https://doi.org/10.3390/nu13124421
APA StyleLeung, D. Y. P., Cheng, H.-L., Tyrovolas, S., Tang, A. S. K., Liu, J. Y. W., Tse, M. M. Y., Lai, C. K. Y., & Molassiotis, A. (2021). Magnitude, Temporal Trends, and Inequalities in the DALYs and YLDs of Nutritional Deficiency among Older Adults in the Western Pacific Region: Findings from the Global Burden of Disease Study 1990–2019. Nutrients, 13(12), 4421. https://doi.org/10.3390/nu13124421









