Latent Class Analysis of Multiple Health Risk Behaviors among Australian University Students and Associations with Psychological Distress
Abstract
:1. Introduction
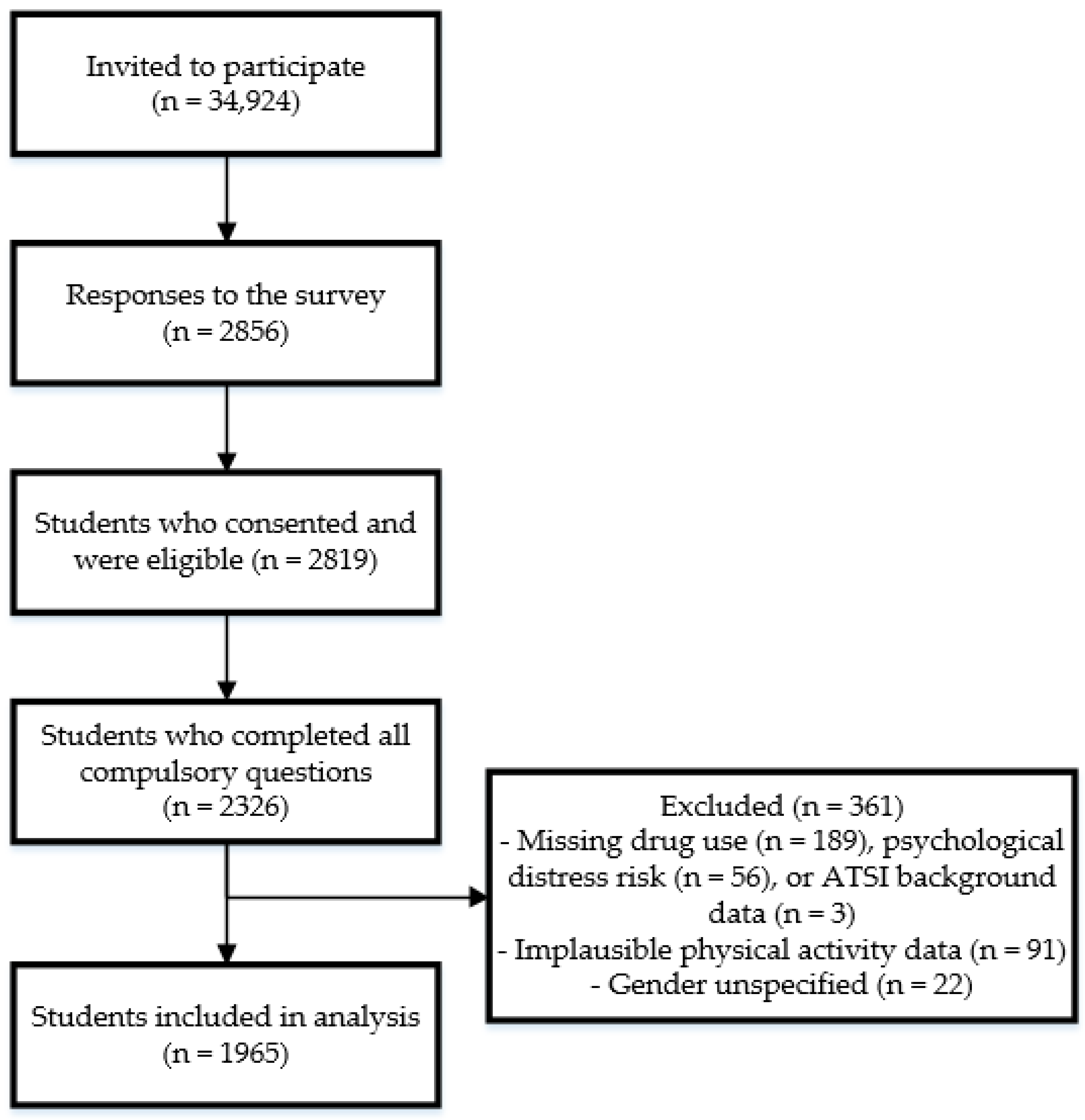
2. Materials and Methods
2.1. Study Design
2.2. Population and Setting
2.3. Measures
2.3.1. Health Behaviors
2.3.2. Psychological Distress
2.3.3. Socio-Demographic Factors
2.4. Statistical Analysis
3. Results
3.1. Summary of Sample Characteristics
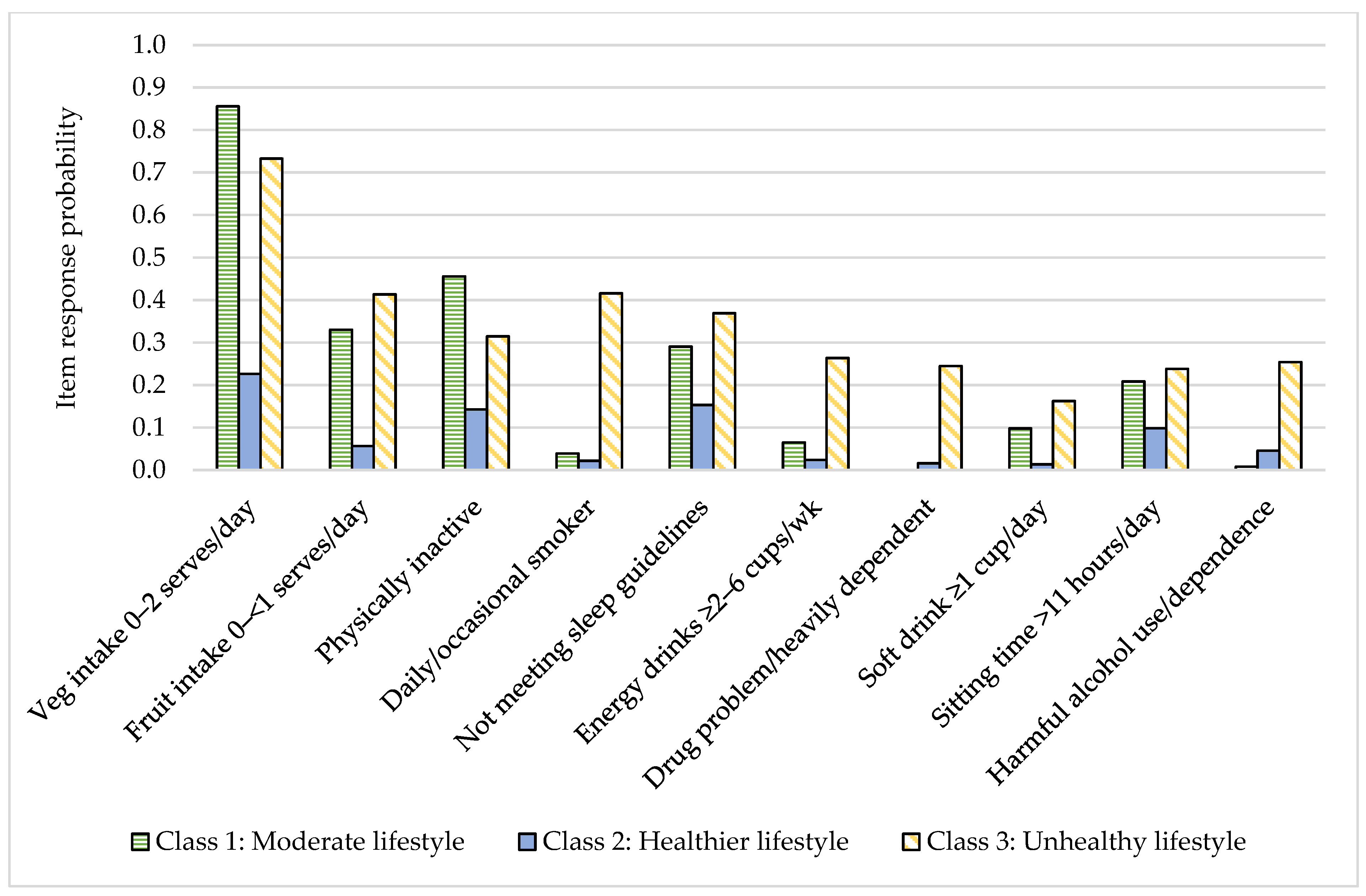
3.2. Patterns of Health Behaviors
3.3. Associations of Psychological Distress Risk and Demographic Characteristics with Health Behavior Classes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Cuijpers, P.; Auerbach, R.P.; Benjet, C.; Bruffaerts, R.; Ebert, D.; Karyotaki, E.; Kessler, R.C. The World Health Organization World Mental Health International College Student initiative: An overview. Int. J. Methods Psychiatr. Res. 2019, 28, e1761. [Google Scholar] [CrossRef]
- Auerbach, R.P.; Mortier, P.; Bruffaerts, R.; Alonso, J.; Benjet, C.; Cuijpers, P.; Demyttenaere, K.; Ebert, D.D.; Green, J.G.; Hasking, P.; et al. WHO world mental health surveys international college student project: Prevalence and distribution of mental disorders. J. Abnorm. Psychol. 2018, 127, 623–638. [Google Scholar] [CrossRef]
- Karyotaki, E.; Cuijpers, P.; Albor, Y.; Alonso, J.; Auerbach, R.P.; Bantjes, J.; Bruffaerts, R.; Ebert, D.D.; Hasking, P.; Kiekens, G.; et al. Sources of Stress and Their Associations With Mental Disorders Among College Students: Results of the World Health Organization World Mental Health Surveys International College Student Initiative. Front. Psychol. 2020, 11, 1759. [Google Scholar] [CrossRef]
- Stallman, H.M. Psychological distress in university students: A comparison with general population data. Aust. Psychol. 2010, 45, 249–257. [Google Scholar] [CrossRef]
- American College Health Association. National College Health Assessment—Spring 2020 Reference Group Executive Summary; American College Health Association: Silver Spring, MD, USA, 2020. [Google Scholar]
- El Ansari, W.; Ssewanyana, D.; Stock, C. Behavioral Health Risk Profiles of Undergraduate University Students in England, Wales, and Northern Ireland: A Cluster Analysis. Front. Public Health 2018, 6, 120. [Google Scholar] [CrossRef] [Green Version]
- Bennasar-Veny, M.; Yañez, A.M.; Pericas, J.; Ballester, L.; Fernandez-Dominguez, J.C.; Tauler, P.; Aguilo, A. Cluster Analysis of Health-Related Lifestyles in University Students. Int. J. Environ. Res. Public Health 2020, 17, 1776. [Google Scholar] [CrossRef] [Green Version]
- Laska, M.N.; Pasch, K.E.; Lust, K.; Story, M.; Ehlinger, E. Latent class analysis of lifestyle characteristics and health risk behaviors among college youth. Prev. Sci. 2009, 10, 376–386. [Google Scholar] [CrossRef] [Green Version]
- Kang, J.; Ciecierski, C.C.; Malin, E.L.; Carroll, A.J.; Gidea, M.; Craft, L.L.; Spring, B.; Hitsman, B. A latent class analysis of cancer risk behaviors among U.S. college students. Prev. Med. 2014, 64, 121–125. [Google Scholar] [CrossRef] [Green Version]
- Duffy, A.; Keown-Stoneman, C.; Goodday, S.; Horrocks, J.; Lowe, M.; King, N.; Pickett, W.; McNevin, S.H.; Cunningham, S.; Rivera, D.; et al. Predictors of mental health and academic outcomes in first-year university students: Identifying prevention and early-intervention targets. BJPsych Open 2020, 6, e46. [Google Scholar] [CrossRef]
- Kroencke, L.; Harari, G.M.; Katana, M.; Gosling, S.D. Personality trait predictors and mental well-being correlates of exercise frequency across the academic semester. Soc. Sci. Med. 2019, 236, 112400. [Google Scholar] [CrossRef]
- Uddin, R.; Burton, N.W.; Khan, A. Combined Effects of Physical Inactivity and Sedentary Behaviour on Psychological Distress among University-Based Young Adults: A One-Year Prospective Study. Psychiatr. Q. 2020, 91, 191–202. [Google Scholar] [CrossRef] [PubMed]
- Kwan, M.Y.; Arbour-Nicitopoulos, K.P.; Duku, E.; Faulkner, G. Patterns of multiple health risk-behaviours in university students and their association with mental health: Application of latent class analysis. Health Promot. Chronic Dis. Prev. Can. 2016, 36, 163–170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ye, Y.L.; Wang, P.G.; Qu, G.C.; Yuan, S.; Phongsavan, P.; He, Q.Q. Associations between multiple health risk behaviors and mental health among Chinese college students. Psychol. Health Med. 2016, 21, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Jao, N.C.; Robinson, L.D.; Kelly, P.J.; Ciecierski, C.C.; Hitsman, B. Unhealthy behavior clustering and mental health status in United States college students. J. Am. Coll. Health 2019, 67, 790–800. [Google Scholar] [CrossRef] [PubMed]
- Whatnall, M.C.; Patterson, A.J.; Brookman, S.; Convery, P.; Swan, C.; Pease, S.; Hutchesson, M.J. Lifestyle behaviors and related health risk factors in a sample of Australian university students. J. Am. Coll. Health 2019. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gotzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Epidemiology 2007, 18, 805–835. [Google Scholar] [CrossRef] [Green Version]
- Centre for Epidemiology and Evidence. NSW Population Health Survey; NSW Health: Canberra, Australia, 2014.
- National Health and Medical Research Council. Eat for Health Educator Guide; National Health and Medical Research Council: Canberra, Australia, 2013.
- Australian Institute of Health and Welfare. The Active Australia Survey; Australian Institute of Health and Welfare: Canberra, Australia, 2003.
- Australian Government Department of Health. Australia’s Physical Activity and Sedentary Behaviour Guidelines; Australian Government Department of Health: Canberra, Australia, 2014.
- Van der Ploeg, H.P.; Chey, T.; Korda, R.J.; Banks, E.; Bauman, A. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch. Intern. Med. 2012, 172, 494–500. [Google Scholar] [CrossRef] [Green Version]
- Babor, T.; Higgins-Biddle, J.; Saunders, J.; Monteiro, M. The Alcohol Use Disorders Identification Test Department of Mental Health and Substance Dependence; WHO, Ed.; WHO: Geneva, Switzerland, 2001. [Google Scholar]
- Berman, A.H.; Bergman, H.; Palmstierna, T.; Schlyter, F. Evaluation of the Drug Use Disorders Identification Test (DUDIT) in criminal justice and detoxification settings and in a Swedish population sample. Eur. Addict. Res. 2005, 11, 22–31. [Google Scholar] [CrossRef]
- National Center for Chronic Disease Prevention and Health Promotion. Data and Statistics-Sleep and Sleep Disorders. Available online: https://www.cdc.gov/sleep/surveillance.html (accessed on 28 May 2020).
- Sleep Health Foundation. Sleep Needs across the Lifespan; Sleep Health Foundation: Blacktown, Australia, 2015. [Google Scholar]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Hillard, P.J.A.; Katz, E.S.; et al. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- El Ansari, W.; Berg-Beckhoff, G. Country and Gender-Specific Achievement of Healthy Nutrition and Physical Activity Guidelines: Latent Class Analysis of 6266 University Students in Egypt, Libya, and Palestine. Nutrients 2017, 9, 738. [Google Scholar] [CrossRef] [PubMed]
- Oftedal, S.; Vandelanotte, C.; Duncan, M.J. Patterns of Diet, Physical Activity, Sitting and Sleep Are Associated with Socio-Demographic, Behavioural, and Health-Risk Indicators in Adults. Int. J. Environ. Res. Public Health 2019, 16, 2375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ma, C.M.; Lai, C.C. Mental health profile and health-related behavior among Hong Kong Chinese university students. Health Psychol. Open 2018, 5. [Google Scholar] [CrossRef] [PubMed]
- Molendijk, M.; Molero, P.; Ortuno Sanchez-Pedreno, F.; Van der Does, W.; Martinez-Gonzalez, M.A. Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 2018, 226, 346–354. [Google Scholar] [CrossRef] [Green Version]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Silva, E.S.; Hallgren, M.; De Leon, A.P.; Dunn, A.L.; Deslandes, A.C.; et al. Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129 (Suppl. 2), 19–31. [Google Scholar] [CrossRef] [Green Version]
- Australian Institute of Health and Welfare. Rural & Remote Health; Australian Institute of Health and Welfare: Canberra, Australia, 2019.
- Imamura, F.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Shi, P.; Powles, J.; Mozaffarian, D. Dietary quality among men and women in 187 countries in 1990 and 2010: A systematic assessment. Lancet Glob. Health 2015, 3, e132–e142. [Google Scholar] [CrossRef] [Green Version]
- Whatnall, M.C.; Patterson, A.J.; Chiu, S.; Oldmeadow, C.; Hutchesson, M.J. Determinants of eating behaviours in Australian university students: A cross-sectional analysis. Nutr. Diet. 2020, 77, 331–343. [Google Scholar] [CrossRef]
- Munt, A.E.; Partridge, S.R.; Allman-Farinelli, M. The barriers and enablers of healthy eating among young adults: A missing piece of the obesity puzzle: A scoping review. Obes. Rev. 2017, 18, 1–17. [Google Scholar] [CrossRef]
- Ashton, L.M.; Hutchesson, M.J.; Rollo, M.E.; Morgan, P.J.; Collins, C.E. A scoping review of risk behaviour interventions in young men. BMC Public Health 2014, 14, 1–23. [Google Scholar] [CrossRef] [Green Version]
- Batten, R.; Liddiard, K.; Raynor, A.J.; Brown, C.A.; Stanley, M. Cross-Sectional Survey of Sleep Practices of Australian University Students. Nat. Sci. Sleep 2020, 12, 39–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallè, F.; Sabella, E.A.; Da Molin, G.; Liguori, G.; Montagna, M.T.; Orsi, G.B.; Valerio, G.; Napoli, C. A cross-sectional study investigating lifestyle and weight perception of undergraduate students in southern Italy. BMC Public Health 2019, 19, 1316. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Hegde, S.; Son, C.; Keller, B.; Smith, A.; Sasangohar, F. Investigating Mental Health of US College Students during the COVID-19 Pandemic: Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e22817. [Google Scholar] [CrossRef] [PubMed]
- Australian Government Department of Education. Selected Higher Education Statistics—2019 Student Data. Available online: https://www.education.gov.au/selected-higher-education-statistics-2019-student-data (accessed on 14 September 2020).
- Gallo, L.A.; Gallo, T.F.; Young, S.L.; Moritz, K.M.; Akison, L.K. The Impact of Isolation Measures Due to COVID-19 on Energy Intake and Physical Activity Levels in Australian University Students. Nutrients 2020, 12, 1865. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef]
- James, E.; Freund, M.; Booth, A.; Duncan, M.J.; Johnson, N.; Short, C.E.; Wolfenden, L.; Stacey, F.G.; Kay-Lambkin, F.; Vandelanotte, C. Comparative efficacy of simultaneous versus sequential multiple health behavior change interventions among adults: A systematic review of randomised trials. Prev. Med. 2016, 89, 211–223. [Google Scholar] [CrossRef]
- Okanagan Charter: An International Charter for Health Promoting Universities and Colleges; University of British Columbia: Kelowna, BC, Canada, 2015.

| Variable | N | % |
|---|---|---|
| Gender | ||
| Male | 575 | 29.3 |
| Female | 1390 | 70.7 |
| Age (years) (Mean ± SD) | 25.8 | 8.6 |
| 17–24 | 1191 | 60.6 |
| 25–35 | 543 | 27.6 |
| >35 | 231 | 11.8 |
| Country of birth | ||
| Australia | 1625 | 82.7 |
| Other | 340 | 17.3 |
| Aboriginal or Torres Strait Islander background | ||
| Yes | 70 | 3.6 |
| No | 1895 | 96.4 |
| Marital status | ||
| Never married | 1398 | 71.2 |
| Married | 284 | 14.5 |
| De facto | 213 | 10.8 |
| Separated/Divorced/Widowed | 70 | 3.6 |
| Living situation | ||
| Own home | 278 | 14.2 |
| Parents’ home | 700 | 35.6 |
| On campus | 154 | 7.8 |
| Renting | 775 | 39.4 |
| Boarding/Homestay | 36 | 1.8 |
| Irregular | 22 | 1.1 |
| Income (per week) | ||
| $1500 or more | 147 | 7.5 |
| $1000–$1499 | 106 | 5.4 |
| $500–$999 | 423 | 21.5 |
| $1–$499 | 930 | 47.3 |
| Nil income | 221 | 11.2 |
| Unsure/Don’t want to answer | 138 | 7.0 |
| Ability to manage on income | ||
| Impossible | 56 | 2.9 |
| Difficult all the time | 411 | 20.9 |
| Difficult sometimes | 698 | 35.5 |
| Not too bad | 587 | 29.9 |
| Easy | 213 | 10.8 |
| Receiving financial support | ||
| Yes | 1167 | 59.4 |
| No | 798 | 40.6 |
| Hours of paid work/week (mean ± SD) | 13.6 | 12.9 |
| Type of degree | ||
| Undergraduate | 1487 | 75.7 |
| Postgraduate | 344 | 17.5 |
| Other a | 134 | 6.8 |
| Domestic/international student | ||
| Domestic | 1772 | 90.2 |
| International | 193 | 9.8 |
| Psychological distress risk | ||
| Low risk | 507 | 25.8 |
| Moderate risk | 567 | 28.9 |
| High risk | 534 | 27.2 |
| Very high risk | 357 | 18.2 |
| Fruit intake | ||
| 0–<1 serve/day | 406 | 20.7 |
| 1 serve/day | 639 | 32.5 |
| 2 or more serves/day | 920 | 46.8 |
| Vegetable intake | ||
| 0–2 serves/day | 1054 | 53.6 |
| 3–<5 serves/day | 691 | 35.2 |
| 5 or more serves/day | 220 | 11.2 |
| Soft drink intake | ||
| 1 cup or less/week | 1460 | 74.3 |
| 2–6 cups/week | 379 | 19.3 |
| 1 cup or more/day | 126 | 6.4 |
| Energy drink intake | ||
| 1 cup or less/week | 1833 | 93.3 |
| 2–6 cups/week | 97 | 4.9 |
| 1 cup or more/day | 35 | 1.8 |
| Physical activity | ||
| Inactive (<150 min/week) | 566 | 28.8 |
| Active (150–300 min/week) | 366 | 18.6 |
| Highly active (>300 min/week) | 1033 | 52.6 |
| Smoking status | ||
| Daily/occasional smoker | 143 | 7.3 |
| Past smoker | 168 | 8.6 |
| Non-smoker | 1654 | 84.2 |
| Meeting sleep duration recommendations | ||
| No | 457 | 23.3 |
| Yes | 1508 | 76.7 |
| Sitting time | ||
| <8 h/day | 1264 | 64.3 |
| 8–11 h/day | 390 | 19.9 |
| >11 h/day | 311 | 15.8 |
| AUDIT classification | ||
| Abstinence/low risk | 1460 | 74.3 |
| Moderate risk | 399 | 20.3 |
| Harmful/hazardous use | 52 | 2.7 |
| Dependence | 54 | 2.8 |
| DUDIT classification | ||
| No drug-related problems | 1896 | 96.5 |
| Drug-related problems | 56 | 2.9 |
| Heavily dependent on drugs | 13 | 0.7 |
| Health Behavior | Health Behavior Class | |||
|---|---|---|---|---|
| Moderate Lifestyle | Healthier Lifestyle | Unhealthy Lifestyle | ||
| Latent Class Membership (%) | 40.2 | 48.6 | 11.2 | |
| Vegetable intake | 0–2 serves/day | 0.86 | 0.23 | 0.73 |
| 3–<5 serves/day | 0.14 | 0.56 | 0.21 | |
| 5 or more serves/day | 0.00 | 0.22 | 0.06 | |
| Fruit intake | 0–<1 serve/day | 0.33 | 0.06 | 0.41 |
| 1 serve/day | 0.40 | 0.26 | 0.36 | |
| 2 or more serves/day | 0.27 | 0.69 | 0.22 | |
| Soft drink intake | 1 cup or less/week | 0.65 | 0.88 | 0.51 |
| 2–6 cups/week | 0.26 | 0.11 | 0.33 | |
| 1 cup or more/day | 0.10 | 0.01 | 0.16 | |
| Energy drink intake | 1 cup or less/week | 0.94 | 0.98 | 0.74 |
| 2–6 cups/week to 1 cup or more/day | 0.06 | 0.02 | 0.26 | |
| Physical activity level | Inactive (<150 min/week) | 0.46 | 0.14 | 0.31 |
| Active (150–300 min/week) | 0.22 | 0.16 | 0.17 | |
| Highly active (>300 min/week) | 0.32 | 0.70 | 0.52 | |
| Smoking status | Daily/occasional smoker | 0.04 | 0.02 | 0.42 |
| Past smoker | 0.06 | 0.08 | 0.19 | |
| Non-smoker | 0.90 | 0.89 | 0.39 | |
| Meeting sleep recommendations | No | 0.29 | 0.15 | 0.37 |
| Yes | 0.71 | 0.85 | 0.63 | |
| Sitting time | <8 h/day | 0.54 | 0.74 | 0.56 |
| 8–11 h/day | 0.25 | 0.16 | 0.20 | |
| >11 h/day | 0.21 | 0.10 | 0.24 | |
| Alcohol use risk | Abstinence/low risk | 0.87 | 0.74 | 0.31 |
| Moderate risk | 0.12 | 0.22 | 0.44 | |
| Harmful/hazardous use or dependence | 0.01 | 0.05 | 0.25 | |
| Drug use risk | No drug-related problems | 1.00 | 0.98 | 0.76 |
| Drug-related problems or heavily dependent on drugs | 0.00 | 0.02 | 0.24 | |
| Odds Ratio (95% CI) | |||
|---|---|---|---|
| Healthier Lifestyle | Moderate Lifestyle | Unhealthy Lifestyle | |
| Psychological distress risk: Moderate a | Ref | 1.43 (0.96–2.12) | 2.37 (1.04–5.43) |
| Psychological distress risk: High/very high a | Ref | 2.71 (1.84–4.00) | 11.69 (5.47–24.97) |
| Age: 25–35 years b | Ref | 0.65 (0.36–1.17) | 2.06 (0.73–5.85) |
| Age: 17–24 years b | Ref | 0.53 (0.28–0.99) | 1.44 (0.47–4.45) |
| Gender: Male c | Ref | 1.15 (0.79–1.68) | 5.81 (3.52–9.60) |
| Aboriginal or Torres Strait Islander background: Yes d | Ref | 2.42 (1.13–5.18) | 1.63 (0.55–4.84) |
| Living situation: Own home e | Ref | 0.53 (0.30–0.92) | 0.72 (0.29–1.77) |
| Living situation: Other e, f | Ref | 0.44 (0.31–0.63) | 1.21 (0.72–2.01) |
| Type of student: International g | Ref | 13.06 (6.74–25.30) | 1.92 (0.57–6.40) |
| Type of degree: Postgraduate h | Ref | 0.65 (0.40–1.05) | 0.74 (0.36–1.54) |
| Type of degree: Other h, i | Ref | 1.55 (0.79–3.04) | 5.33 (2.60–10.90) |
| Managing on income: Some difficulty j | Ref | 1.24 (0.89–1.74) | 2.26 (1.29–3.97) |
| Managing on income: Difficulty j | Ref | 1.39 (0.89–2.16) | 5.70 (3.19–10.22) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hutchesson, M.J.; Duncan, M.J.; Oftedal, S.; Ashton, L.M.; Oldmeadow, C.; Kay-Lambkin, F.; Whatnall, M.C. Latent Class Analysis of Multiple Health Risk Behaviors among Australian University Students and Associations with Psychological Distress. Nutrients 2021, 13, 425. https://doi.org/10.3390/nu13020425
Hutchesson MJ, Duncan MJ, Oftedal S, Ashton LM, Oldmeadow C, Kay-Lambkin F, Whatnall MC. Latent Class Analysis of Multiple Health Risk Behaviors among Australian University Students and Associations with Psychological Distress. Nutrients. 2021; 13(2):425. https://doi.org/10.3390/nu13020425
Chicago/Turabian StyleHutchesson, Melinda J., Mitch J. Duncan, Stina Oftedal, Lee M. Ashton, Christopher Oldmeadow, Frances Kay-Lambkin, and Megan C. Whatnall. 2021. "Latent Class Analysis of Multiple Health Risk Behaviors among Australian University Students and Associations with Psychological Distress" Nutrients 13, no. 2: 425. https://doi.org/10.3390/nu13020425
APA StyleHutchesson, M. J., Duncan, M. J., Oftedal, S., Ashton, L. M., Oldmeadow, C., Kay-Lambkin, F., & Whatnall, M. C. (2021). Latent Class Analysis of Multiple Health Risk Behaviors among Australian University Students and Associations with Psychological Distress. Nutrients, 13(2), 425. https://doi.org/10.3390/nu13020425








