Abstract
Metabolic syndrome (MetS) is a clinical manifestation characterized by a plethora of comorbidities, including hyperglycemia, abdominal obesity, arterial hypertension, and dyslipidemia. All MetS comorbidities participate to induce a low-grade inflammation state and oxidative stress, typical of this syndrome. MetS is related to an increased risk of cardiovascular diseases and early death, with an important impact on health-care costs. For its clinic management a poly-pharmaceutical therapy is often required, but this can cause side effects and reduce the patient’s compliance. For this reason, finding a valid and alternative therapeutic strategy, natural and free of side effects, could represent a useful tool in the fight the MetS. In this context, the use of functional foods, and the assumption of natural bioactive compounds (NBCs), could exert beneficial effects on body weight, blood pressure and glucose metabolism control, on endothelial damage, on the improvement of lipid profile, on the inflammatory state, and on oxidative stress. This review focuses on the possible beneficial role of NBCs in the prevention and in the clinical management of MetS and its comorbidities.
1. Introduction
In the last century, there has been a rampant increase in chronic degenerative non-communicable diseases (CDNCDs) incidence. This, both because of the enhancement in the average life span of the population, and because of the spread of risk factors related to unhealthy lifestyle like smoking, alcohol abuse, sedentary, and incorrect eating habits [1].
Among the most common CDNCDs, an important role for the enormous worldwide spread is played by the metabolic syndrome (MetS). MetS is a clinic syndrome characterized by a cluster of multiple comorbidities, including hyperglycemia, abdominal obesity, arterial hypertension (AH) and dyslipidemia, which together represent an important risk factor for the onset of cardiovascular (CV) diseases and early death [2], as well as having an important impact on health care costs [3]. MetS has been estimated to increase the risk of all-cause mortality by approximately 1.5 times, with respect to the general population [4]. It is easy to understand how the spread of the MetS goes hand in hand with the spread of its comorbidities. It is estimated that around ¼ of the world’s population is affected by MetS, over a billion people, and this incidence is expected to increase [5]. The prevalence of MetS appears to be higher in the USA and Europe than in Eastern countries, although its incidence is slowly increasing in the latter as well, becoming a global epidemic. Its prevalence seems to be related to gender, in fact it is more frequent in male subjects compared to female ones [5,6]. These huge numbers make us reflect on the importance of finding new strategies to counteract this rampant world problem.
In this context, it is important to underline how an improvement in eating habits towards healthier lifestyles can play a fundamental role in the prevention and clinical management of MetS. Mediterranean diet (MD), rich in polyphenols, represents a healthy dietary pattern, characterized by regular consumption of fruit and vegetables and extra virgin olive oil (EVOO) as the main plant-based fat source; numerous studies suggest, in fact, that it is associated with the risk reduction in CDNCDs onset, including the MetS [7,8]. A recent study compared different diets such as plant-based diets, low-carbohydrates, low-fat diet, and MD, underlining that the latter is the most effective nutritional strategy for the prevention and treatment of MetS [9].
Focusing on preventive and therapeutic methods that are based on the use of natural bioactive compounds (NBCs), free from side effects, they could represent a valid adjuvant treatment to reduce hospitalization and health costs, as well as to improve the quality of life of MetS patients.
2. Metabolic Syndrome
MetS is characterized by the concomitant presence of multiple CV risk factors, which represent simultaneously the causes and the effects of MetS [10].
In 1988, MetS was called “syndrome X”, namely a particular condition that included alterations in glucose and lipid metabolism and AH [11]. Subsequently, MetS was defined by various organizations, as reported in Table 1 [5]. According to the World Health Organization (WHO), in the late 1990s, for MetS diagnosis, it was necessary that the patient had hyperglycemia or insulin resistance (IR), with blood glucose (BG) values >110 mg/dl, and postprandial BG >140 mg/dl, accompanied by at least one of the following factors: high-density lipoprotein cholesterol (HDL-C) <35 mg/dl in men or <40 mg/dl in women; triglycerides (TG) >150 mg/dl; central obesity defined by waist to hip ratio (WHR) >0.90 in men or >0.85 in women, or body mass index (BMI) >30 kg/m2; blood pressure (BP) >140/90 mmHg [12]. Furthermore, at first, microalbuminuria was included among the MetS diagnostic criteria, but subsequently has been removed [5]. In 2001 the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) defined MetS as the co-presence of at least three of the following factors: BG >100 mg/dl or pharmacological therapy for hyperglycemia; HDL-C <40 mg/dl in men or <50 mg/dl in women or lipid-lowering therapy; TG >150 mg/dl or lipid-lowering therapy; waist circumference (WC) >102 cm in men or >88 cm in women; BP > 130/85 mmHg or antihypertensive therapy [13]. Afterwards, in 2005, the International Diabetes Foundation (IDF) defined new criteria for MetS diagnosis, including obesity (WC ≥ 94 cm in men and ≥80 cm in women) as a necessary criterion. In addition, at least two of the following factors must be present: BG > 100 mg/dL or diagnosis of type 2 diabetes mellitus (T2DM); HDL-C < 40 mg/dl in men or <50 mg/dl in women or lipid-lowering therapy; TG > 150 mg/dl or lipid-lowering therapy; BP > 130/85 mmHg or antihypertensive therapy [14].

Table 1.
Principal definitions of MetS.
The three definitions focus on different metabolic alterations while describing the same clinical condition. In fact, the definition reported by the WHO focuses mainly on T2DM and CV risk, defining hyperglycemia or IR as a necessary criterion for MetS diagnosis. The NCEP ATP III definition, on the other hand, does not focus on a main pathology but on the co-presence of multiple risk factors. At last, the IDF defines the presence of obesity as necessary, determined by WC, which is however variable in different ethnic groups [15]. In fact, WC ranges were subsequently defined based on the patient’s ethnicity: for Europeans, Canadians, and Americans from the USA, WC ≥ 102 cm in men and ≥88 cm in women; for the Mediterranean, Middle Eastern, and sub-Saharan African populations, WC ≥ 94 cm in men and ≥80 cm in women; for Asian and Central-South American populations, WC ≥ 90 cm in men and ≥80 cm in women [16,17].
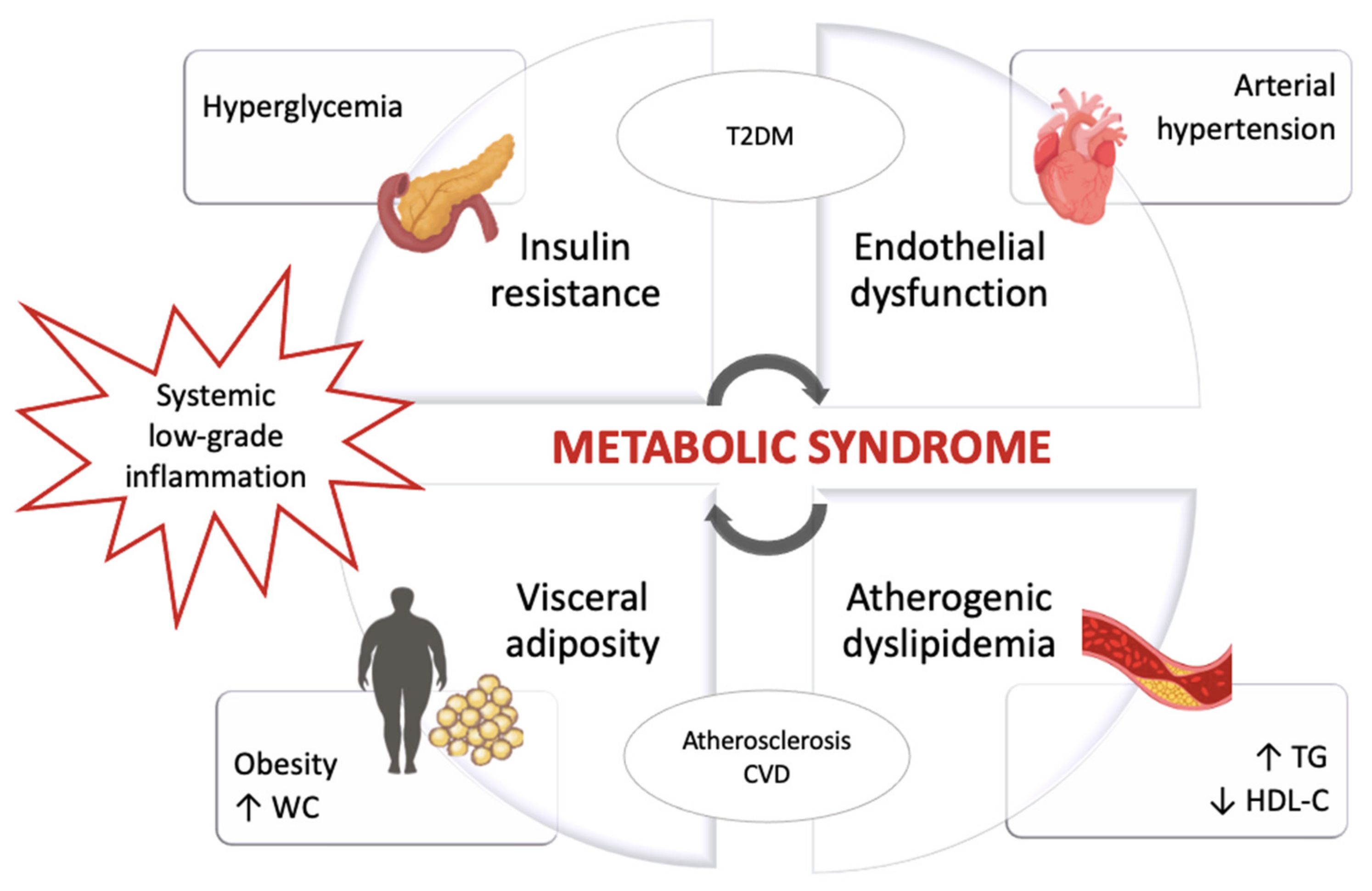
The pathophysiological processes that involve the metabolic alterations typical of MetS are interrelated and characterized by a low-grade chronic inflammatory state [18], as shown in Figure 1.

Figure 1.
Pathophysiology of the metabolic syndrome. Abbreviations: ↑, Increase; ↓, Decrease; CVD, Cardiovascular disease; HDL-C, High-density lipoprotein cholesterol; T2DM, Type 2 diabetes mellitus; TG, Triglycerides; WC, Waist circumference.
A high accumulation of adipose tissue in the abdominal area represents a greater risk factor both for CV disease, for IR and T2DM [19,20]. In fact, the adipose tissue, divided into brown adipose tissue (BAT) and white adipose tissue (WAT), thanks to its endocrine role, regulates numerous metabolic pathways that, if altered, can lead to an impaired carbohydrate and lipid metabolism. BAT regulates adaptive thermogenesis [21] while WAT represents the storage site of lipids, releasing them in the form of energy when needed. Furthermore, WAT secretes leptin and adiponectin (important regulators of metabolic processes), adipsin, fatty acid-binding protein 4 (FABP4), fatty acid esters of hydroxyl fatty acids (FAHFAs) and palmitoleate; these substances act on the pancreas, liver, skeletal muscles, CV system, and brain. The WAT is in turn divided into visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT); only the former is associated with CV morbidity, as it determines a significant release in the blood of fatty acids and pro-inflammatory cytokines, like interleukin (IL)-6, IL-8 and tumor necrosis factor-α (TNF-α) [22,23], but also of plasminogen activator inhibitor-1 (PAI-1) capable to favor a prothrombotic state [24].
Excessive caloric intake causes hypertrophy and hyperplasia of the adipocytes, as occurs in obese subjects, resulting in metabolic alterations and in the onset of a low-grade chronic inflammatory state [25]. In fact, the pro-inflammatory substances that are released from adipose tissue can provoke IR, T2DM, metabolic, and CV diseases [25,26,27]. Some studies have identified in MetS patients, the presence of some inflammatory cytokines, such as IL-1β and IL-18, which play a crucial role in the development of atherosclerotic plaques [28,29,30].Atherogenic dyslipidemia is characterized by an increase in the level of circulating triglycerides, a reduction in HDL-C levels and therefore, an increase in low-density lipoprotein cholesterol (LDL-C). These alterations are closely related to impaired insulin metabolism. Indeed, in case of IR, it is possible to observe an increase in lipolysis and in apolipoprotein B (apoB) and very low-density lipoprotein (VLDL) levels, and a lipase dysfunction that leads to a reduction in the clearance of VLDL. Therefore, there will be a significant amount of TG-rich HDL lipoproteins, obtained from VLDL, which will be rapidly cleared by hepatic lipase, with a reduction in circulating HDL levels [10].
The chronic low-grade inflammatory state, the IR and the alteration of the lipid profile could lead to endothelial dysfunction [31]. Hyperglycemia can cause a glucose increase in endothelial cells, favoring the oxidative degradation of glucose metabolites, with a consequent oxidative stress (OS) [19]. Furthermore, they increase the levels of advanced glycation end products (AGEs) involved in the processes of vascular damage [32,33]. Another factor that induces the endothelial dysfunction in MetS patients is the insulin, which, in physiological conditions, could exert a vasodilator action; in fact, insulin acts on the phosphorylation of endothelial nitric oxide synthase (eNOS) which causes the nitric oxide (NO) increase, able to induce vasodilation. An alteration in the phosphorylation of eNOS, could lead to an enhancement of OS, inflammation, prothrombotic state and BP values [31,34,35].
3. Research Methods
The search of the paper (review or original articles) was conducted on Pubmed and Scopus electronic databases, until December 2020. The keywords used were: “metabolic syndrome” in combination with “natural bioactive compounds” and “body weight” or “body composition” and “metabolic alterations” and “endothelial dysfunction” and “lipid profile” and “inflammation” or “oxidative stress” or “gut microbiota modulation”. In addition, we included only papers in the English language. All the references were manually selected by the authors.
4. Natural Bioactive Compounds
Fruit and vegetables, and all plant-based products, are the key foods of the MD and, thanks to their polyphenols content, contribute to their well-known and well-studied cardioprotective and anticarcinogenic properties. These foods are rich in vitamins and minerals and contribute to achieve the right daily fiber intake. Moreover, they are rich in NBCs that induce numerous beneficial healthy effects [36,37]. NBCs are organic compounds of various derivations that exert important actions at the level of biological tissues. The NBCs of fruit, vegetables, and other plant-based foods are commonly called “phytochemicals” and can be classified into numerous categories based on their chemical structure and biological activity. Although it is hypothesized that many plant-derived bioactive compounds are yet to be discovered, more than 5000 phytochemicals have currently been isolated and studied [38]. These NBCs can be classified into phenolics, carotenoids, alkaloids, phytosterols, nitrogen-containing compounds, and organosulfur compounds [39]. Among these, the most studied are certainly the phenolics one. These are products of the secondary metabolism of plants, responsible for the typical coloring of fruit and vegetables, for the defense of the plant from microorganisms and other parasites, and commonly intervene in the growth, reproduction, and metabolism of the plant [40].
Numerous studies have highlighted their pivotal role in the onset and slowing progression of CDNCDs, such as CV diseases [41], cancer [39], diabetes mellitus [42], Alzheimer’s disease [43], and chronic kidney disease, both in the form of fresh food and as oral food supplements [44,45,46]. In fact, these NBCs seem to exert anti-inflammatory, antioxidant and antimicrobial effects and have cardioprotective, neuroprotective, hepatoprotective, hypoglycemic, and antihypertensive properties [47,48]. Precisely for this reason, the use of NBCs as adjuvant therapy could represent a valid therapeutic and preventive strategy to counteract the onset and the progression of numerous CDNCDs and of their comorbidities, such as the MetS.
5. Possible Effects of Natural Bioactive Compounds in Metabolic Syndrome
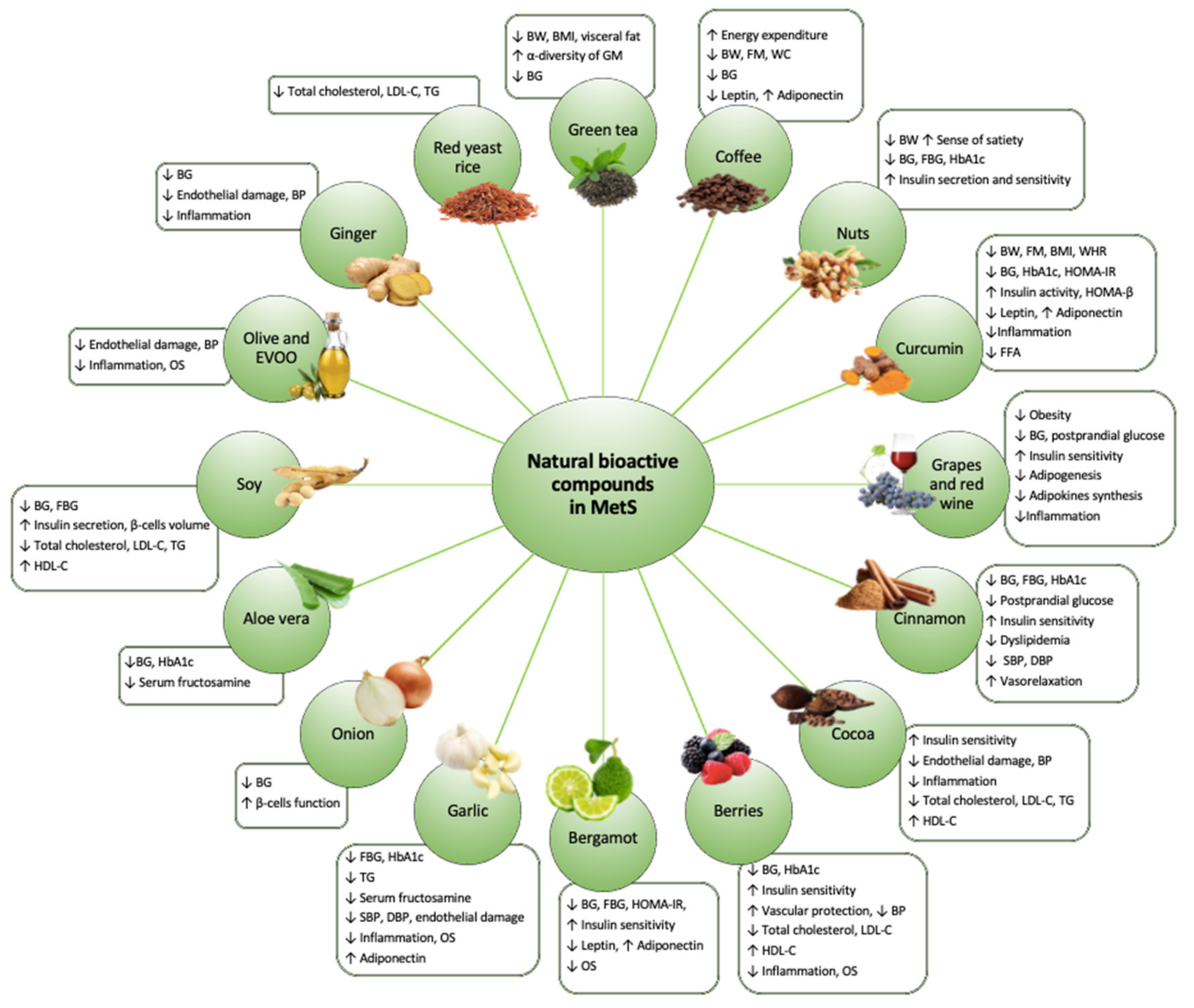
Given the enormous worldwide spread of the MetS and all its clinical implications, it is extremely important to find a valid therapeutic strategy to counteract it. The first therapeutic approach applied in case of MetS is the modification of eating habits and lifestyle. It is in fact known how an improvement in eating habits, with a reduction in caloric intake in the case of overweight and obesity, a reduction in the intake of sodium, saturated fats, cholesterol, and simple sugars, can help in the clinical management of MetS comorbidities [49]. In some cases, it may be necessary to resort to pharmacological therapy. As there is not a single drug targeted against MetS, it is often necessary a poly-pharmaceutical therapy that can have side effects and reduce the patient compliance. For this reason, it is important to find a natural approach, free of side effects, which can help the MetS patients to delay the onset and progression of comorbidities typical of this syndrome [50]. Recently, numerous studies have highlighted how NBCs can play a crucial role in delaying the progression of MetS, exerting beneficial long-term effects (Figure 2).

Figure 2.
The effects of natural bioactive compounds on Metabolic syndrome management. Abbreviations: ↑, Increase; ↓, Decrease; BG, Blood glucose; BMI, Body mass index; BP, Blood pressure; BW, Body weight; DBP, Diastolic blood pressure; FBG, Fasting blood glucose; FFA, Fatty free acids; FM, Fat mass; GM, Gut microbiota; HbA1c, Hemoglobin A1c; HDL-C, High-density lipoprotein cholesterol; HOMA-IR, Homeostatic model assessment for insulin resistance; HOMA-β, Homeostatic model assessment for β -cell function; LDL-C, Low-density lipoprotein cholesterol; OS, oxidative stress; SBP, Systolic blood pressure; TG, Triglycerides; WC, Waist circumference, WHR, Waist to hip ratio.
5.1. Body Weight and Body Composition
The effect on body weight control and the reduction in visceral obesity exerted by NBCs has been demonstrated in numerous clinical studies (Table 2). Among the most studied NBCs for their potential anti-obesity action are catechins and their derivatives. In fact, these bioactive molecules seem to be able to reduce body weight through two main mechanisms: (I) increase in energy expenditure through stimulation of the sympathetic nervous system which, in turn, induces an enhancement in lipid oxidation, especially at the adipose tissue level [51]; and (II) reduction in intestinal absorption of lipids, contributing to the decrease in caloric intake [52]. Catechins are polyphenols belonging to the class of flavonoids, much studied for their antioxidant properties. Through their esterification, they can give rise to numerous molecules with bioactive properties, particularly detectable in green tea and cocoa.

Table 2.
NBCs in body weight and body composition management.
Green tea is rich in epigallocatechin gallate (EGCG). Several clinical trials have shown that EGCG assumption is associated with a statistically significant reduction in body weight, BMI and visceral fat [53,54,55,56,69]. These effects have often been studied in association with the consumption of caffeine, which seems to act in synergy with EGCG in reducing body weight [70]. EGCG seems to be able to increase the activity of AMP-activated protein kinase (AMPK) which is involved in the reduction in fat biosynthesis and in the increase in fat catabolism, as well as in the improvement of insulin sensitivity, thus leading to a reduction in body weight [57,71]. Finally, EGCG would also appear to have a beneficial effect in the gut microbiota, increasing bacterial species such as Bacteroides and Bifidobacterium, improving the energy metabolism [72,73,74]. Pharmacokinetic studies have shown that the EGCG bioavailability, after oral administration, is dose-dependent. In fact, the pre-systemic elimination of tea polyphenols is saturable, consequently increasing their intake likely growths their bioavailability [58]. According to a recent study, the maximum plasma concentration of EGCG is obtained with the administration of EGCG extract after 8 h of overnight fasting, while the intake of EGCG as an oral food supplement reduces its intestinal absorption but improves the stability of the molecule in the body. Currently, in literature, there is no uniqueness about the EGCG dose needed to achieve the maximum beneficial effect [75].
Coffee is rich in NBCs, among these, the most studied are caffeine, belonging to the alkaloids, and chlorogenic acid, of the polyphenols class. In recent decades, the effect on the increase in energy expenditure, through the activation of thermogenesis, induced by caffeine, and its possible role in controlling body weight, has been much discussed. According to some studies, in fact, the habitual consumption of caffeine seems to be associated with the reduction in body weight, fat mass (FM) and WC [59,76,77,78]. The consumption of coffee is also able to prevent the accumulation of visceral fat and excessive body weight, thanks to the high content of chlorogenic acid, which seems to act thought the modulation of the peroxisome proliferator-activated receptor (PPAR) γ responsible of lipid metabolism [60,61].
Another food that acts on body weight control are nuts. Despite their high caloric density, the habitual consumption of nuts would seem to have an important effect on body weight control, especially if used as a snack instead of other foods rich in fats. Because these properties, the nuts are commonly used in diet-therapy for the body weight reduction [62]. Nuts are, in fact, functional foods rich in monounsaturated fatty acids (MUFAs), polyunsaturated fatty acids (PUFAs) as well as fiber, folate, calcium, magnesium, and potassium. Their action on body weight control would seem to be exerted by an increase in the sense of satiety [63,64,79,80]. Furthermore, the consumption of nuts has beneficial effects in the control of glucose and lipid metabolism, making them an excellent food for the MetS management [81].
Further studies focused on the role of curcumin, a natural phenol of Curcuma longa, in the modulation of obesity pathways. The consumption of curcumin, in association with a low-caloric diet, increases the loss of body weight, reducing FM%, BMI, and body circumferences [65,82,83]. In a recent in vitro study, Wu et al. highlighted that curcumin is able to inhibit the differentiation of adipocytes, and at the same time induces apoptosis of preadipocytes [66]. Curcumin also acts as an anti-inflammatory pathway, inducing the expression of adiponectin, a powerful anti-inflammatory agent produced by adipose tissue [67]. This results in an improvement in the chronic low-grade inflammatory status that occurs in obese subjects with MetS. Pharmacokinetic studies reveal that the bioavailability of curcumin after oral administration is very low, due both to poor intestinal absorption and to an important hepatic metabolism [84]. These obstacles can be overcome thanks to the use of specific inhibitors of the curcumin metabolism or the use of solid or liquid formulations that improve its absorption and slow down its elimination [85]. Furthermore, the effective safety of administering curcumin extracts has been demonstrated, in fact no toxic effects were observed up to the chronic daily intake of 180 mg of curcumin [86].
Quercetin, a flavonoid abundant in apples, grapes and red wine, seems to modulate in mitochondria the lipolysis pathways, inducing the body weight reduction [87,88]. Specifically, quercetin is able to decrease adipogenesis through the activation of AMPK [89] and the modulation of PPARγ [68]. Furthermore, quercetin seems to be able to reduce the synthesis of adipokines in adipose tissue, improving systemic low-grade inflammation. Therefore, quercetin would seem to act as a tissue-specific anti-inflammatory, contributing to the reduction in the expansion of adipose tissue induced by the inflammatory state [90]. It has been shown that the bioavailability of quercetin depends by the molecule carbohydrate fraction, in fact, its absorption is higher when it is assumed as glycoside rather than as free quercetin [91]. The food matrix in which quercetin is assumed, as a food or as oral food supplement, does not seem to influence the bioavailability of the flavonoid [92]. In addition, interindividual variability in the quercetin bioavailability was observed, possibly due to genetic polymorphisms, gut microbiota composition, BMI, and health status [93].
5.2. Metabolic Alterations
IR and T2DM play a crucial role in the pathogenesis of MetS. Therefore, numerous NBCs and their action on these pathological conditions have been analyzed over the years (Table 3) [50,94].

Table 3.
NBCs in metabolic alterations management.
Among the NBCs, curcuma or turmeric appears to have an important modulatory function on T2DM and IR, indeed it has been studied for its anti-inflammatory, antioxidant and antidiabetic properties [95,143]. Some animal studies have highlighted the hypoglycemic role of curcumin and an improvement in insulin sensitivity following its assumption. Curcumin seems to play its hypoglycemic action through the inhibition of hepatic gluconeogenesis by an independent-insulin pathway. Furthermore, its antihyperglycemic role has been attributed both to its anti-inflammatory action thanks to the reduction in TNF-α and anti-lipolytic action with decrease in circulating levels of fatty free acids (FFAs) [96,97,98]. In particular, a study conducted on hamsters showed a significant reduction in homeostatic model assessment for insulin resistance (HOMA-IR) and in leptin levels, in animals treated for 10 days with curcumin compared to the control group [96]. Studies conducted on humans showed how turmeric appears to be able to reduce plasma glucose levels and improve insulin activity [99,100,101]. A study conducted on 240 prediabetic patients divided into a study group and in a control group, showed that none of the patients treated with curcumin (250 g/day for 9 months) developed T2DM, showing also a significantly higher homeostatic model assessment for β -cell function (HOMA-β) score [99]. Another research group treated overweight or obese diabetic patients with 300 mg/day of curcuminoids for 3 months; comparing the results obtained with the control group treated with placebo for the same period, the authors found a significant reduction in BG, hemoglobin A1c (HbA1c) and HOMA-IR in the study group [100]. Instead, Panahi et al. [101] used curcumin in association with piperine, an alkaloid contained in black pepper, on population of 100 T2DM patients divided equally into treated group and control group. The results obtained showed a significant reduction in circulating levels of glucose and HbA1c in patients treated with curcumin and piperine. The use of curcumin showed a reduction also in the leptin–adiponectin ratio, resulting from a decrease in the leptin levels and an increase in adiponectin levels. In fact, curcumin appears to be able to reduce the activity of the nuclear factor-κB (NF-kB) factor that is directly involved in inflammatory processes and in the synthesis of pro-inflammatory cytokines [144]. The reduction in inflammation results in an increase in adiponectin production and an inhibition of leptin synthesis [67,102]. The mechanism of curcumin action on these metabolic alterations typical of MetS, would seem to be related to its ability to reduce FFAs with a consequent decrease in BG. In fact, high circulating levels of FFAs are capable of causing IR as they are both associated with visceral fat deposits [97]. Furthermore, its strong anti-inflammatory activity prevents damage to pancreatic β cells, acting on NF-κB [95,145,146]. Indeed, a study conducted by Adibian M. et al. highlighted how the consumption of turmeric can counteract the complications of T2DM by reducing both TG and inflammatory biomarkers levels [95].
Cinnamon is a genus of the Lauraceae family from which is obtained the spice cinnamon, widely used since ancient times both in food and medicine [147]. Cinnamon can perform an action similar to insulin activating numerous mechanisms that lead to a reduction in BG [148]. The first human study about the beneficial effects of cinnamon on IR and T2DM was conducted by Khan A. et al., who showed a reduction in BG with three different doses of cinnamon per day (1, 3, and 6 g) in T2DM patients [103]. Numerous studies over the years investigated the compounds present in cinnamon and their beneficial effects on IR and T2DM. These healthy effects have often been associated with hydro-soluble polyphenols, more precisely with the flavonoids catechin and epicatechin [104]. A study conducted on MetS patients taking cinnamon hydro-soluble extract-based supplement for 12 weeks found a reduction in fasting blood glucose (FBG) [105]. The main action of hydro-soluble polyphenolic extracts seems to be a promotion of insulin signaling, resulting in increased IR-β insulin receptor and improved cellular glucose absorption. In fact, cinnamon promotes the increase in glucose transporter type 4 (GLUT4) acting as an insulin receptor that allows the entry of glucose into the cells [106]. Additionally, Jarvill-Taylor K.J. et al. [107] have highlighted how the hydroxychalcone present in cinnamon, induces a greater biosynthesis of glycogen, activating the glycogen synthase and inhibiting the glycogen synthase kinase3 β (GSK3 β). A clinical study conducted on healthy subjects evaluated the effect of a specific hydroalcoholic extract of Ceylon cinnamon on the reduction in post-prandial BG, showing a significant reduction in this parameter in the area under the curve (AUC) 0-60 min [108]. Furthermore, cinnamon seems to be a possible source of NBCs for the prevention and treatment of IR and T2DM, activating PPARγ and PPARα [109,149], that induce an improvement in dyslipidemia and increases the insulin sensitivity [150,151]. These actions of NBCs seem to improve, in combination with hypoglycemic therapy, the glucose metabolism of patients with IR and T2DM [110,149,152]. In fact, a study conducted by Crawford P. [110] found a reduction in HbA1c in T2DM patients treated with 1 g of cinnamon per day for 90 days in association with traditional hypoglycemic therapy, compared to the control group treated with hypoglycemic therapy alone. The study conducted by Sonal Gupta J. et al. [111] evaluated the effect of 3 g of cinnamon per day for 16 weeks on 116 MetS patients, comparing the results with a control group that took a placebo for the same period. At the end of the 16 weeks, numerous improvements were obtained in the treated group, regarding the lipid profile, body composition, FBG and HbA1c. Therefore, these results lead us to suppose that supplementation with cinnamon may lead to a reduction in the MetS risk factors and a decrease in its prevalence [111]. The cinnamon polyphenols bioavailability depends on several factors including the food matrix of assumption, the total polyphenols content and the gastrointestinal tract healthy state [153]. A study evaluated the effective bioavailability of polyphenols in a cinnamon-based drink, concluding that it is equal to 80% of the total content. The addition of sweeteners seems to increase this value. Furthermore, it has been observed that the polyphenols bioavailability is reduced when they assumed concomitantly with milk and its derivatives, as the polyphenols have a high affinity with the milk caseins [154].
Among the food rich in polyphenols, which exert a positive action on IR and T2DM, there are cocoa, coffee, and tea. Cocoa and its derivatives are natural products rich in catechins and flavonoids with numerous biological activities. Cocoa and dark chocolate contain a particular flavanols called flavan-3-ols, which appear to have a beneficial effect on CV disease, protecting against endothelial damage and improving insulin sensitivity [94,112,155]. Specifically, the study conducted by Grassi D. et al. [113] highlighted how the consumption of flavanol-rich dark chocolate (100 g per day for 15 days) was able to reduce IR and increase insulin sensitivity by improving pancreatic β cells functionality. The potential hypoglycemic role of cocoa depends also on its fiber content. In fact, the study conducted by Sarria B. et al. [156] detected a reduction in BG after daily consumption of soluble cocoa product rich in dietary fiber (10.17 g of total-dietary-fiber, 43.8 mg of flavanols and 168.6 mg methylxanthines per day) compared to the daily consumption of a product rich only in polyphenols (falavanols and methylxanthines with low fiber intake). Methylxanthines are a class of polyphenols with numerous health benefits. Among the methylxanthines, the cocoa theobromine seems to play a crucial role on glucose metabolism by regulating the intracellular levels of cyclic adenosine monophosphate (cAMP) which induces a greater release of insulin by the pancreas and glucose by the liver [157,158]. In addition, several studies have associated coffee methylxanthines with a reduced risk of developing T2DM [159,160]. Furthermore, caffeine has been associated with a dose-dependent reduction in glucose absorption [114,161,162]. Similar mechanisms have been highlighted in studies that evaluated the potential beneficial effects of tea on reduced risk of onset T2DM [163]. A study conducted on borderline MetS patients showed that the treatment based on green tea catechin extract reduced the risk factors of MetS in 68% of patients [115]. The hypoglycemic effect of tea was mainly associated with its catechin content, especially EGCG [117,118,164,165]. A study evaluated the effective bioavailability of caffeine and theobromine after methylxanthines assumption in the form of caffeine capsules, cola drinks, and chocolate. The authors observed that compared to the capsules, the absorption of caffeine was delayed when assumed in the form of food, while the absorption of theobromine from chocolate was faster [166]. Furthermore, it has been observed that the tissue distribution, the metabolism and the elimination of methylxanthines, such as caffeine and theobromine, can be altered by numerous factors such as obesity, smoking and alcohol abuse, sedentary lifestyle, and pharmacological therapy [167]. MetS is characterized by an increase in leptin levels and a decrease in adiponectin levels [168]. Several studies have demonstrated that coffee and tea had a modulatory action on these hormones, as well. Indeed, a recent meta-analysis has evaluated the effects of coffee consumption on circulating leptin and adiponectin levels, highlighting an inversely correlation between coffee consumption and leptin levels and a direct correlation with adiponectin [116]. Furthermore, a study evaluated the consumption of green coffee bean extract (400 mg per day) in association with a low-calorie diet, demonstrated a reduction in leptin and a significant increase in adiponectin in the treated group compared to the control group (placebo) [119]. A meta-analysis that instead examined the effect of green tea on leptin levels revealed that this hormone increased only in case of treatments lasting more than 12 weeks. Therefore, the anti-inflammatory effect of green tea, which involves a reduction in the synthesis of leptin, exercised only in case of prolonged treatment [120,169].
Berries (such as strawberries, blackberries, red fruits, blueberries, and raspberries) are functional foods rich in NBCs, including anthocyanins and flavonoids, with numerous biological properties [170]. Several studies have evaluated the hypoglycemic action of berries. Stull A.J. et al. [121] studied the effect of a smoothie, obtained from 22.5 g of blueberries rich in NBCs, consumed twice daily for 6 weeks by a group of obese patients with IR. At the end of the study, the treated patients showed an improvement in insulin sensitivity compared to the control group (placebo). Another study evaluated the metabolic effects of purified anthocyanins on 80 prediabetic and diabetic patients. The enrolled patients took 300 mg per day of purified anthocyanins obtained from bilberry and blackcurrant for 12 weeks. Treated patients showed a reduction in HbA1c compared to the control group (placebo), confirming a positive action of anthocyanins on glycemic control [122]. The anthocyanins in cranberry would seem to carry out their hypoglycemic activity as a consequence of the reduction in lipotoxicity. In fact, they act by activating the AMPK which leads an increase in GLUT4 transporters and glucose uptake, and the suppression of gluconeogenesis. In addition, AMPK acts on hepatic lipid metabolism, upregulating the gene expression of PPARα, acyl-coenzyme A (acyl-CoA) oxidase and carnitine palmitoyltransferase-1A [123,171]. Furthermore, anthocyanins seem to induce the secretion of incretin glucagon-like peptide-1 (GLP-1) that in turn, causes insulin secretion [171,172]. Among the berries, elderberry seems to exert important antioxidant, lipid-lowering and hypoglycemic roles in the treatment of T2DM and MetS patients. The patients treated with elderberry showed an improvement in HbA1c compared to no-treated subjects (control group) [124]. Elderflower extracts are able to activate PPARγ, stimulating the absorption of glucose [173]. Finally, the various berries seem to have different effects, based on their polyphenolic content and in the way of their consumption (for example fresh or frozen fruits) [174]. Pharmacokinetic studies suggest that berries anthocyanins are rapidly absorbed and eliminated, but their effective intestinal absorption rate has not yet been estimated [175]. In addition, anthocyanins appear to undergo important first-pass intestinal metabolic processes and circulate into the bloodstream as metabolites, which are the real effectors of the beneficial effects observed after berries assumption. Part of the anthocyanins assumed orally reach the colon at the level of which they may exert important effects on the gut microbiota [176].
Bergamot is a citrus fruit that has numerous health benefits. Bergamot essential oil contains bergapten and bergamottin with antioxidant, lipid-lowering and hypoglycemic action. Mainly, its hypoglycemic action was detected as a consequence of improvement of lipid metabolism. In fact, it has been shown that bergamot polyphenols are able to modulate lipid metabolism by inhibiting of hepatic 3-Hydroxy-3-Methylglutaryl-Coenzyme A (HMG-CoA) reductase and acyl-CoA cholesterol acyltransferase (ACAT) activities [8,125,177]. However, the bergamot polyphenols have also a direct hypoglycemic action by increasing the AMPK activity and stimulating glucose uptake in muscle and liver [126]. Furthermore, the polyphenols of bergamot act on the leptin–adiponectin ratio, increasing the levels of adiponectin and reducing those of leptin [127]. A study conducted to evaluate the action of bergamot extract (650, 1300 mg, and placebo) on MetS risk factors, showed an improvement in the lipid profile, a reduction in FBG, HOMA-IR, and insulin. In addition, the authors observed a reduction in leptin and ghrelin concentrations, and an increase in adiponectin. Therefore, supplements based on bergamot extract could be an effective in the treatment of the metabolic alterations typical of MetS [128].
Garlic is a spice of the Alliaceae family widely used since ancient times for its countless benefits. Some studies report its positive effects on the lipid profile and its hypoglycemic action [8]. A meta-analysis showed how garlic appears to reduce FBG and HbA1c levels in diabetic patients and those with CV diseases [178]. Its mechanism of action is linked to its ability to inhibit HMG-CoA reductase [129,130] and cholesteryl ester transfer protein (CETP) [131]. An improvement in the lipid profile leads to a decrease in BG and IR. A study, evaluating the effects of prolonged-release garlic powder tablets in T2DM patients, highlighted a reduction in the metabolic impairments. After 4 weeks, the patients treated with the tablets showed a better metabolic assessment, in particular the authors observed the reduction in TG, FBG, and serum fructosamine [132].
Onion is made up of numerous NBCs, including flavonoids, phenolic acids, quercetin, and others [8]. Among its many benefits, onion plays a positive role in reducing BG, allowing the physiological functions of pancreatic β cells through a mechanism involving in enhancement of skeletal muscle mitochondrial number and function [133,179].
Resveratrol, an abundant polyphenol in grapes and wine, exerts a positive effect in T2DM patients. The action of resveratrol in this patient’s population, is linked to the activation of AMPK and consequently of sirtuin1 (SIRT1) [134,135,180,181]. The latter activation induces an improvement of insulin sensitivity and glycemic homeostasis [182,183]. The flavonoic glycoside rutin, instead, present in various plant sources such as wine, peppermint, and citrus fruits, reduces the absorption of glucose in the small intestine. Indeed, it appears to be able to inhibit α-glucosidase, reducing the digestion of carbohydrates and thus decreasing postprandial BG [184]. In addition, rutin seems to stimulate insulin secretion, activate the translocation of GLUT4 and increase glucose uptake into tissues [136,185,186]. The bioavailability and metabolism of resveratrol are strongly dependent by the food matrix of assumption. A study compared the resveratrol bioavailability after assumption of grape juice, red wine, and oral food supplement based on resveratrol, highlighting how the bioavailability would appear to be greater after resveratrol assumption in natural and fresh products than an oral food supplement [187]. However, another study observed that the resveratrol absorption is strongly delayed after assumption of grape extracts allowing the molecule to be more metabolized in the intestine, increasing the concentrations of its active metabolites in the systemic circulation [188].
Aloe vera seems to have anti-diabetic properties. Some studies have investigated about aloe vera showing that it is able to reduce BG and fructosamine levels [94,137]. The meta-analysis conducted by Dick W.R. et al. demonstrated significant reductions in FBG and HbA1c [189]. The aloe vera assumption appears to be able to inhibit the glucose intestinal absorption, as well as stimulate the glucose catabolism and inhibit its synthesis [138]. Moreover, aloe vera has been shown to be able to increase the AMPK activity through the same metformin mechanism [139]. Therefore, the treatment with aloe vera of T2DM and MetS patients would seem to be an adjuvant tool to traditional pharmacological therapy [137,189].
Soy is known as a valuable source of proteins with high biological value, PUFAs and dietary fiber. In fact, soy is rich in phytochemical compounds, in particular isoflavones and phytosterols, which act with different, often synergistic, mechanisms that exert beneficial effects on human health [190]. Some studies report the antidiabetic effects of soy. A study conducted by Li et al., showed that black-soybean-leaf extract can exert hypoglycemic effects through the activation of hepatic AMPK and the PPARs pathways modulation [191]. Moreover, the estrogens contained in it seem to act on IR, improving insulin secretion and increasing the volume of pancreatic β cells [94,192]. Supplementation with soy isoflavones showed significant improvements in FBG and BG, leading to the hypothesis of their possible use as adjuvant treatment in T2DM and MetS patients [140,193]. The soy isoflavones bioavailability was investigated in pharmacokinetic studies. A high concentration of isoflavones, such as genistein and daidzein, was observed for several hours after ingestion of soy powder, suggesting that these compounds exhibit good bioavailability after its assumption [194]. Furthermore, soy isoflavones are more bioavailable when assumed in the glucoside form, more present in unfermented soybeans, compared to the aglycone form, whose concentration increases as result of the fermentation processes necessary to produce soy fermented derivatives [195].
Certain nuts categories have been shown to reduce the incidence of some CDNCDs, including T2DM. Hazelnuts are mainly composed of MUFAs and PUFAs, that exerts a cardioprotective role and they are rich in numerous NBCs [80,196,197]. Their consumption in T2DM and MetS patients seems to reduce BG and HbA1c, and improve insulin secretion and sensitivity thanks to their antioxidant, anti-inflammatory and lipid-lowering effects [8,198,199]. Walnuts and their tree components are also able to act positively on glycemic control [94]. Nuts α-Linolenic acid seems to modulate the circulating microRNAs involved in the control of insulin sensitivity [141]. Furthermore, the nuts complex set of MUFAs, PUFAs, and polyphenols can improve insulin sensitivity through the regulation of the phosphoinositide 3-kinase/protein kinase B (PI3K/AKT) signaling pathway [200]. A study evaluated the effect of the extract obtained from the leaves of the walnut plant (Juglans regia L.) in T2DM patients. The study population took two capsules (100 mg Juglans regia leaf per dose) for 3 months without interrupting their usual pharmacological therapy. At the end of 3 months, a significant reduction in FBG and HbA1c was highlighted, as well as an improvement in the lipid profile compared to the control group who took a placebo for the same time-period [142]. Therefore, the use of these products could support the usual hypoglycemic pharmacological treatments, improving the risk factors of MetS and delaying its onset.
5.3. Endothelial Dysfunction
Endothelial dysfunction is one of the complications of the MetS. The main causes of endothelial dysfunction are related to the metabolic alterations of T2DM, to dyslipidemia and to chronic low-grade inflammatory state [31]. Several NBCs seem to counteract and improve endothelial damage (Table 4) [201].

Table 4.
NBCs in endothelial dysfunction management.
The NCBs present in garlic have been extensively studied for their hypotensive function. Indeed, garlic consumption would appear to induce a reduction in both systolic and diastolic BP [212,213,214]. One study evaluated the effects of garlic consumption on a population of MetS patients. They took 100 mg per kg body weight of raw crushed garlic, twice a day for 4 weeks, showing significant improvements not only in carbohydrates metabolism and in lipid profile, but also in BP. This study highlighted how an intake of garlic can prevent and improve MetS condition [215]. Garlic seems to be able to increase eNOS activity and to reduce the expression of vascular cell adhesion molecule 1 (VCAM-1), leading to a decrease in inflammation and OS, with a consequent protection by endothelial damage, as well as an improvement of BP values [202,216].
Cinnamon NBCs seem to modulate positively the MetS risk factors and exert an important antihypertensive action [148]. Various studies have evaluated this effect especially in prediabetic or T2DM patients, highlighting a reduction in BP and vasorelaxation [217]. Its mechanism of action seems to be related to the activation of chemosensory cation channel (TRPA1) capable to stimulate vasodilatory and vasorelaxant actions [203]. A study conducted on MetS patients, showed a significant reduction in BP after cinnamon assumption with consequent decrease in MetS prevalence compared to the control group [111]. A recent meta-analysis evaluating the effects of oral cinnamon supplementation on BP, confirmed its hypotensive effect on both systolic and diastolic BP [218].
Olive is rich in polyphenolic compounds, such as oleuropein, hydroxytyrosol and tyrosol with several beneficial actions. Olive tree leaf through the reduction in inflammation and OS, decrease endothelial damage [219]. EVOO, one of the basic foods of the MD, is associated with numerous health benefits. Several authors have associated consumption of EVOO with a reduction in BP [204,205,220,221,222,223]. The NBCs present in the EVOO seem to act by increasing of the eNOS expression and the NO synthesis [206,222]. Furthermore, it appears to be able to regulate the NF-κB and activator protein-1 (AP-1) activities [223,224]. Regular consumption of EVOO can lead to significant improvements in MetS patients, both in terms of BP control and in ameliorating other risk factors [7,225].
Ginger, from the Zingiberaceae family, has been shown to have hypoglycemic and hypotensive properties [226]. A recent meta-analysis highlighted that an intake of ginger (≥3 g per day for more than 8 weeks) was related to a significant reduction in AH [207]. Its beneficial action seems to be related to its ability to act on PPARs, AMPK, and NF-κB signaling pathways. Therefore, it allows a reduction in the inflammatory state and in the adipogenesis, increasing glucose uptake. These mechanisms prevent the onset of AH and endothelial damage [227]. It has been shown that the ginger phenols have a high stability in the gastric fluids. However, pharmacokinetic studies have demonstrated an important first-pass metabolism, which reduces the systemic concentration of active phenols [228]. In addition, the ginger phenols shown to have a wide distribution in various tissues, including the stomach, intestines, liver, lungs, and kidneys, which probably represent the main target organs [229].
Other foods rich in NBCs can play a protective role on endothelial damage. Among these, there is cocoa. In fact, it appears to be responsible for the increase in eNOS and NO, reducing endothelial damage and BP values [113,208,230]. Cocoa flavanol, thanks to its anti-inflammatory capacity, has a positive action on organ damage related to AH, improving endothelial function, allowing vasodilation, and inhibiting the platelets activation [230,231].
Foods containing resveratrol perform a protective vascular action [232]. Several studies report positive results of resveratrol on reducing BP by activating the cyclic guanosine monophosphate (cGMP)-dependent protein kinase 1α (PKG1 α) activity which exerts a vasodilatory-NO dependent action [209,210,211]. Therefore, its mechanism of vascular protection would seem to be related to its high antioxidant capacity, acting on all the risk factors of MetS [233].
5.4. Lipid Profile
Dyslipidemia is one of the main conditions that characterize the MetS. In fact, low HDL-C levels and increased blood TG levels are often observed in MetS patients. To improve the lipid profile of these patients, it is possible to resort to NBCs, capable of modulate the lipid metabolism (Table 5).

Table 5.
NBCs in lipid profile management.
Resveratrol is able to act on lipid metabolism through numerous mechanisms, promoting the reduction in adipogenesis and the increase in lipolysis [241]. Specifically, the main mechanism of the SIRT1 pathway, a nicotinamide dinucleotide (NAD+)-dependent deacetylase, involved in energy and mitochondrial metabolism. Imamura et al. have shown that resveratrol is able to increase the expression of SIRT1, preventing the accumulation of TG in differentiated 3T3-L1 preadipocytes. The authors conclude that resveratrol regulates the expression of PPARγ, responsible of the lipid metabolism [234]. Analyzing the most recent clinical trials, resveratrol appears to reduce plasma concentrations of total cholesterol and TG [235] but it does not affect HDL-C and LDL-C concentrations [242].
Several clinical studies have shown an important action on the control of the lipid metabolism by cocoa and dark chocolate. Their assumption, from 2 to 12 weeks, would seem to be able to reduce plasma levels of total cholesterol and LDL-C [243]. Mursu et al. showed that daily consumption of 45 g of dark chocolate for 3 weeks seems to increase the serum HDL-C concentration in a group of healthy subjects [244]. In another study, Hamed et al. observed an improvement in the lipid profile, in particular a reduction in LDL-C and an increase in HDL-C, in healthy subjects taking 700 mg/day of flavonoids in the form of dark chocolate for one week [236]. More recently, a randomized and placebo-controlled study conducted by Leyva-Soto et al., revealed that total cholesterol, LDL-C and TG decreased after a daily intake of 2 g of dark chocolate (70%) for 6 months [237]. The cocoa polyphenols regulate the main pathways involved in both fat synthesis and catabolism. In particular, the main targets of cocoa polyphenols are NF-κB, AP-1, PPARs, and AMPK pathways [245]. All this evidence suggest that flavonoids are able to improve the lipid profile, if consumed daily. The bioavailability and metabolism of cocoa polyphenols has been extensively studied. Pharmacokinetic studies have highlighted their moderate bioavailability in a dose-dependent manner after intestinal absorption [246]. A study has shown that the absorption of cocoa polyphenols can be significantly increased with a concomitant intake of carbohydrates [247]. However, another study highlighted how the phase II metabolism of cocoa polyphenols appears to be increased by the presence of sucrose and milk in chocolate, suggesting a greater bioavailability of polyphenols in dark chocolate [248].
Red yeast rice is a food of Chinese origin, obtained from the fermentation of rice by Monascus purpureus. This treatment allows to red yeast rice to be rich in substances called monacolins. Among these, there is monacolin K, with well-known lipid-lowering properties, able to reduce total cholesterol and LDL-C [249]. Red yeast rice, in fact, seems to act in a similar way to statins, inhibiting HMG-CoA reductase, a key enzyme in cholesterol synthesis [238,250]. Thanks to this mechanism of action, it is called “natural statin”. Red yeast rice is also rich in pigments, organic acids, flavonoids, and natural phytosterols that contribute to the lipid-lowering action [251,252], namely reducing total cholesterol, LDL-C and TG. These results suggest that red yeast rice is an excellent oral food supplement without side effects, useful for the treatment of dyslipidemia, in particular in subjects intolerant to statins [253]. Pharmacokinetic studies propose that red yeast rice monacolin K exhibits poor bioavailability after oral administration, less than 5%. This is mainly due to an important intestinal and hepatic metabolism [251]. However, the monacolin K bioavailability would appear to be higher if assumed through the food matrix than as oral food supplement. This phenomenon is due to a higher dissolution rate which increases intestinal absorption [254].
Recent studies have shown that berries are able to improve the concentrations of total cholesterol, LDL-C and HDL-C, reducing CV risk in T2DM and MetS patients [170]. In particular, berries anthocyanins interact with the pathways of lipid metabolism, reducing the gene transcription responsible of fatty acids the synthesis stimulating their catabolism [170]. Furthermore, the berries anthocyanins would seem capable of inhibiting the CETP activity [239], improving lipid profile. The berry anthocyanins also have important antioxidant and anti-inflammatory effects, as well as lipid-lowering action, which help to protect against the main comorbidities of CV and metabolic diseases [255].
Soy is rich in isoflavones and phytosterols that had a beneficial role on lipid profile [190]. Specifically, numerous clinical studies demonstrated that soy isoflavones are able to decrease serum levels of total cholesterol, LDL-C and TG and showed slight effects on the increase in HDL-C, only after treatments longer than 12 weeks [240,256]. The authors also observed a reduction in LDL-C–HDL-C ratio [257]. In particular, soy isoflavones appear to be capable to modulate estrogen gene transcription. Specifically, soy isoflavones act through the activation of the PPARγ pathway, modulating positively the levels of circulating cholesterol [258].
5.5. Inflammation and Oxidative Stress
The presence of a low-grade chronic inflammatory state and an imbalance between pro- and antioxidant species that induce OS condition, are the basis of all the comorbidities of MetS. These conditions can be counteracted by taking NBCs, tested in in vitro studies and in numerous clinical trials (Table 6).

Table 6.
NBCs in inflammation and oxidative stress management.
In recent years, EVOO has attracted particular scientific interest for its antioxidant and anti-inflammatory properties. EVOO has beneficial properties that counteract the onset and progression of CDNCDs [259,260,261,272,273]. These properties seem to be exerted by the antioxidant and anti-inflammatory action of the polyphenols that it contains, in particular hydroxytyrosol and oleocanthal. Hydroxytyrosol is a phenolic alcohol with important antioxidant actions. In fact, hydroxytyrosol seems to act as a free radical scavenger, donating hydrogen atoms to the peroxyl radicals [274]. At the same time, hydroxytyrosol would seem to implement the body’s endogenous defenses through various mechanisms, including the activation of the nuclear factor E2-related factor 2 (Nrf2), involved in the expression of phase II detoxification enzymes [262]. Furthermore, hydroxytyrosol appears to exert an anti-inflammatory action. Several in vitro and in vivo studies suggest that hydroxytyrosol is able to inhibit the synthesis of pro-inflammatory cytokines (like TNF-α) and the activity of cyclooxygenases (COX)-2 [263,264]. Pharmacokinetic studies have highlighted how the dose-dependent bioavailability of hydroxytyrosol is greater when assumed by EVOO compared to other food matrices such as margarine, wine, and pineapple juice. These results demonstrated how the oily nature of EVOO was important for the absorption of hydroxytyrosol [275]. The hydroxytyrosol bioavailability, like other phenols, is strongly influenced by factors such as age, gender, and hormonal order. In addition, hydroxytyrosol and its metabolites have an excellent distribution in all body tissues at the level of which it exerts its beneficial effects [276].
Oleocanthal is a secoiridoid responsible for the pungent taste of EVOO, which pharmacological mechanisms seem to counteract the inflammatory state. In fact, oleocanthal has an important anti-inflammatory action similar to that of ibuprofen (non-steroidal anti-inflammatory drug), as it is capable of inhibit COX-1 and COX-2 enzymes, and consequently the synthesis of inflammatory prostaglandins, in a dose-dependent manner [277]. Moreover, oleocanthal would seems to inhibit the synthesis of pro-inflammatory cytokines, such as TNF-α, IL-6, and IL-1β [265]. In a recent study conducted by Carpi et al., it was observed that oleocanthal is able to modulate the gene expression of genes related to inflammation in preadipocytes. In fact, the authors suggest that oleocanthal seems to attenuate the activation of NF-κB, a transcription factor that responds to inflammatory stimuli and which in turn regulates the production of cytokines and adipokines. This data proposes that oleocanthal plays a key role in the modulation of inflammatory processes at the level of adipose tissue and could therefore improve the chronic low-grade inflammatory state, typical of obesity-related diseases and MetS [266]. However, in vivo pharmacokinetic studies conducted in rats demonstrated a low intestinal absorption of oleocanthal [278]. Human studies investigating the oleocanthal bioavailability after EVOO assumption are limited. Only one study found good oleocanthal concentrations in human urine after 2–6 h from EVOO consumption [279]. Probably the oleocanthal bioavailability in humans is higher than in rats.
Quercetin has proven anti-inflammatory and antioxidant properties [280,281]. An in vivo study conducted on 60 subjects showed a statistically significant reduction in IL-6 and C-reactive protein (CRP), after a supplementation of 500 mg/day of quercetin for 8 weeks [267]. Furthermore, quercetin seems to be able to reduce COX-2 [268] and inducible nitric oxide synthase (iNOS) gene expression [269,282]. Quercetin can improve the body’s antioxidant defenses by stimulating the synthesis of glutathione (GSH) and modulating the expression of catalase, GSH peroxidase and superoxide dismutase (SOD) [281].
Supplementation with resveratrol could be a valid strategy for the improvement of the inflammatory state of MetS. Several studies suggest that resveratrol is able to reduce the production of pro-inflammatory cytokines, decreasing the chronic low-grade inflammatory state. Resveratrol also exerts an antioxidant action, neutralizing reacting oxygen species (ROS) and reactive nitrogen species (RNS) [270,283].
Other NBCs useful for counteract the chronic low-grade inflammation, are allicin and its derivatives contained in garlic. Garlic compounds seems to inhibit the gene transcription of numerous pro-inflammatory cytokines, including IL-6, TNF-α, and IL-1β [284]. Furthermore, garlic shown an improvement of adiponectin in plasma levels in MetS patients [271]. A study evaluated the allicin bioavailability after assumption of several food matrices, observing a good allicin bioavailability (about 80%) after garlic powder capsules assumption and a very similar bioavailability after raw garlic assumption. The allicin bioavailability from garlic-based food assumption is equally good, ranging from 16 to 66%. This bioavailability was reduced when allicin was assumed after a protein-rich meal [285].
5.6. Effects of Natural Bioactive Compounds on Gut Microbiota Metabolites
The gut microbiota is considered an “ecological community” of bacteria localized in the intestinal tract, capable of maintaining the homeostasis in human body. The main activities, exerted by gut microbiota, are represented by extraction, synthesis, and absorption of nutrients and metabolites like vitamins, short-chain fatty acids (SCFA), etc. [286]. Regarding its composition, gut microbiota is constituted up to 90% by two phyla, namely by Firmicutes and Bacteroidetes [287]. The first one is characteristic of high-fiber and high-carbohydrate diets, while the second one is characteristic of a high-fiber and animal proteins foods diet [288]. Gut microbiota changes in the lifespan and multiple factors are able to interfere with its composition as dietary habits, aging, physical exercise, stress, drugs, etc. [289,290]. Moreover, numerous studies have shown that in presence of metabolic alterations like MetS, the gut microbiota composition results altered [291,292].
The main compounds of natural origin that “interact” with gut microbiota are represented by polyphenols [293,294,295,296]. Polyphenols, once introduced into the human body, are metabolized as xenobiotics, in fact their bioavailability is lower compared to micro- and macro-nutrients [297]. Several studies speculate that phenolic compounds, as well as their aromatic metabolites, are able to modulate the gut microbiota composition, exerting prebiotic effects and antimicrobial actions to counteract pathogens [298,299]. In particular, polyphenols thanks to the colonic microflora are transformed into bioactive compounds and studies both in vitro and in vivo have demonstrated that they exert a modulatory action in the composition of the gut microflora, inhibiting and promoting the release of compounds that modulate its composition [300]. For example, in vitro study conducted by Monagas et al. [301] on lipopolysaccharide-induced peripheral blood mononuclear cells of healthy subjects, revealed that dihydroxylated phenolic acids, a proanthocyanidins metabolite, induced an important anti-inflammatory action through the inhibition of pro-inflammatory cytokines like TNF- α, IL-1β, and IL-6. In a following study conducted by Rastmanesh [302], the author demonstrated that, in obese subjects, drinks like green tea, vinegar and foods like fruit, favor body weight reduction thanks to their polyphenols content, that modulates the gut microbiota both for the greater glycans-degradation of Bacteroidetes, and for the metabolites-derived production from polyphenols. Another study conducted by Zanzer at el. [303] demonstrated that polyphenols contained in spices are able to inhibit glucose uptake in the gut microflora. In particular, the authors highlighted that cinnamon and turmeric lowered plasma glucose up to 45 min, compared to controls. Moreover, turmeric, thanks to release-induction of peptide YY (PYY) diminished hunger, compared to the control group. The authors concluded that modulating glucose response and appetite, some spices should play an “adjuvant” role in the prevention of metabolic diseases.
A further action is due to the SCFAs release. The latter are particularly important because they act as modulators of colonic functions and of inflammatory and metabolic processes [304]. A recent in vitro study by Vamanu et al. [305], demonstrated that Curcuma longa extract, particularly rich in curcumin, changes the gut microflora composition of hypertensive patients through the increased release of SCFAs thus, in turn, enhances the Enterobacteriaceae and decreases Bacteroidetes-Prevotella-Porphyromonas genera. Several studies speculate that the modulation of metabolic pattern producing SCFAs may represent an innovative approach to counteract pathological conditions, such as MetS, chronic kidney disease, and AH, characterized by a low-grade inflammatory status [44,45,49,74,261,306]. In this perspective, the most SCFA studied is represented by butyric acid. Some activities ascribable to this compound are represented by the control of the inflammatory proliferation and of intestinal bacterial species growth (favorable to the body homeostasis) and by the reduction in OS [307].
The role exerted by NBCs, such as polyphenols, is attracting increasingly attention. In fact, the conscious use of NBCs on specific metabolic patterns could help the clinical management of CDNCDs, such as the MetS.
6. Conclusions
In conclusion, there is a clear evidence on the NBCs positive role in the clinical management of MetS and its comorbidities. In fact, their assumption, especially in the long term, presents numerous beneficial effects such as body weight control, glucose and lipid metabolisms improvements, BP control, endothelial protection, and finally reduction in chronic low-grade inflammatory state and OS. Therefore, this evidence suggests that the habitual assumption of functional foods rich in NBCs could represent a valid preventive strategy for MetS and it could be an adjuvant therapy in its treatment. However, even if the possible beneficial effects of a large number of NBCs have already been widely studied, further clinical trials on larger samples are needed, in order to understand their specific mechanisms of action useful in control of metabolic pathways. As future perspective, it is necessary to define international guidelines for determine the NBCs minimum effective dose and their duration of assumption for obtain the beneficial effects described in the literature.
Author Contributions
Conceptualization, A.N., N.D.D.; writing—original draft preparation, M.D.L., F.D.D., A.P.Z., G.M., P.B.; writing—review and editing, A.N., N.D.D.; visualization, M.D.L., A.P.Z.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| Acyl- CoA | acyl- coenzyme A |
| ACAT | Acyl-CoA cholesterol acyltransferase |
| AGEs | Advanced glycation end products |
| AH | Arterial hypertension |
| AMPK ApoB | AMP-actived protein kinase Apolipoprotein B |
| AP-1 | Activator protein-1 |
| ATP III | Adult Treatment Panel III |
| AUC | Area under the curve |
| BAT | Brown adipose tissue |
| BMI | Body mass index |
| BG | Blood glucose |
| BP cAMP | Blood pressure Cyclic adenosine monophosphate |
| CDNCDs | Chronic degenerative non-communicable diseases |
| CETP cGMP | Cholesteryl ester transfer protein Cyclic guanosine monophosphate |
| COX | Cyclooxygenases |
| CRP | C-reactive protein |
| CV | Cardiovascular |
| EGCG | Epigallocatechin gallate |
| eNOS | Endothelial nitric oxide synthase |
| EVOO | Extra virgin olive oil |
| FABP4 | Fatty acid-binding protein 4 |
| FAHFAs | Fatty acid esters of hydroxy fatty acids |
| FBG | Fasting blood glucose |
| FFAs | Free fatty acids |
| FM | Fat mass |
| GLP-1 | Glucagon-like peptide-1 |
| GLUT4 | Glucose transporter type 4 |
| GSH | Glutathione |
| GSK3 β | Glycogen synthase kinase 3 β |
| HbA1c | Hemoglobin A1c |
| HDL-C | High-density lipoprotein cholesterol |
| HMG-CoA | 3-hydroxy-3-methylglutaryl- coenzyme A |
| HOMA-IR | Homeostatic model assessment for insulin resistance |
| HOMA-β | Homeostatic model assessment for β -cell function |
| IDF | International Diabetes Foundation |
| IL | Interleukin |
| iNOS | Inducible nitric oxide synthase |
| IR | Insulin resistance |
| LDL-C | Low-density lipoprotein cholesterol |
| MD | Mediterranean diet |
| MetS | Metabolic syndrome |
| MUFA | Monounsaturated fatty acid |
| NAD+ | Nicotinamide dinucleotide |
| NBCs | Natural bioactive compounds |
| NCEP | National Cholesterol Education Program |
| NF-κB | Nuclear factor-κB |
| NO | Nitric oxide |
| Nrf2 | Nuclear factor E2-related factor 2 |
| OS | Oxidative stress |
| PAI-1 | Plasminogen activator inhibitor-1 |
| PI3K/AKT | Phosphoinositide 3-kinase/ protein kinase B |
| PPAR | Peroxisome proliferator-activated receptor |
| PUFA | Polyunsaturated fatty acid |
| PYY | Peptide YY |
| RNS ROS | Reactive nitrogen species Reacting oxygen species |
| SAT | Subcutaneous adipose tissue |
| SCFAs | Short-chain fatty acids |
| SIRT1 | Sirtuin1 |
| SOD | Superoxide dismutase |
| T2DM | Type 2 diabetes mellitus |
| TG | Triglycerides |
| TNF-α | Tumor necrosis factor -α |
| TRPA1 | Chemosensory cation channel |
| VAT | Visceral adipose tissue |
| VCAM-1 | Vascular cell adhesion molecule 1 |
| VLDL | Very low-density lipoprotein |
| WAT | White adipose tissue |
| WC | Waist circumference |
| WHO | World Health Organization |
| WHR | Waist to hip ratio |
References
- Peters, R.; Ee, N.; Peters, J.; Beckett, N.; Booth, A.; Rockwood, K.; Anstey, K.J. Common risk factors for major noncommunicable disease, a systematic overview of reviews and commentary: The implied potential for targeted risk reduction. Ther. Adv. Chronic Dis. 2019, 10. [Google Scholar] [CrossRef]
- Tune, J.D.; Goodwill, A.G.; Sassoon, D.J.; Mather, K.J. Cardiovascular consequences of metabolic syndrome. Transl. Res. 2017, 183, 57–70. [Google Scholar] [CrossRef]
- Boudreau, D.M.; Malone, D.C.; Raebel, M.A.; Fishman, P.A.; Nichols, G.A.; Feldstein, A.C.; Boscoe, A.N.; Ben-Joseph, R.H.; Magid, D.J.; Okamoto, L.J. Health Care Utilization and Costs by Metabolic Syndrome Risk Factors. Metab. Syndr. Relat. Disord. 2009, 7, 305–314. [Google Scholar] [CrossRef]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gallù, M.; Marrone, G.; Legramante, J.M.; De Lorenzo, A.; Di Daniele, N.; Noce, A. Female Sex as a Thromboembolic Risk Factor in the Era of Nonvitamin K Antagonist Oral Anticoagulants. Cardiovasc. Ther. 2020, 2020, 1743927. [Google Scholar] [CrossRef]
- Di Daniele, N.; Noce, A.; Vidiri, M.F.; Moriconi, E.; Marrone, G.; Annicchiarico-Petruzzelli, M.; D’Urso, G.; Tesauro, M.; Rovella, V.; De Lorenzo, A. Impact of Mediterranean diet on metabolic syndrome, cancer and longevity. Oncotarget 2017, 8, 8947–8979. [Google Scholar] [CrossRef] [PubMed]
- Bagetta, D.; Maruca, A.; Lupia, A.; Mesiti, F.; Catalano, R.; Romeo, I.; Moraca, F.; Ambrosio, F.A.; Costa, G.; Artese, A.; et al. Mediterranean products as promising source of multi-target agents in the treatment of metabolic syndrome. Eur. J. Med. Chem. 2020, 186, 111903. [Google Scholar] [CrossRef] [PubMed]
- Castro-Barquero, S.; Ruiz-León, A.M.; Sierra-Pérez, M.; Estruch, R.; Casas, R. Dietary Strategies for Metabolic Syndrome: A Comprehensive Review. Nutrients 2020, 12, 2983. [Google Scholar] [CrossRef]
- Huang, P.L. A comprehensive definition for metabolic syndrome. Dis. Model. Mech. 2009, 2, 231–237. [Google Scholar] [CrossRef]
- Reaven, G.M. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 1988, 37, 1595–1607. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- Lorenzo, C.; Williams, K.; Hunt, K.J.; Haffner, S.M. The National Cholesterol Education Program-Adult Treatment Panel III, International Diabetes Federation, and World Health Organization Definitions of the Metabolic Syndrome as Predictors of Incident Cardiovascular Disease and Diabetes. Diabetes Care 2007, 30, 8–13. [Google Scholar] [CrossRef]
- Zimmet, P.; Magliano, D.; Matsuzawa, Y.; Alberti, G.; Shaw, J. The Metabolic Syndrome: A Global Public Health Problem and A New Definition. J. Atheroscler. Thromb. 2005, 12, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Reaven, G.M. The metabolic syndrome: Is this diagnosis necessary? Am. J. Clin. Nutr. 2006, 83, 1237–1247. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Lear, S.A.; Gasevic, D. Ethnicity and Metabolic Syndrome: Implications for Assessment, Management and Prevention. Nutrients 2019, 12, 15. [Google Scholar] [CrossRef]
- Monteiro, R.; Azevedo, I. Chronic Inflammation in Obesity and the Metabolic Syndrome. Mediat. Inflamm. 2010, 2010, 289645. [Google Scholar] [CrossRef] [PubMed]
- Blüher, M. Adipose tissue inflammation: A cause or consequence of obesity-related insulin resistance? Clin. Sci. (Lond.) 2016, 130, 1603–1614. [Google Scholar] [CrossRef]
- Mohamed, E.I.; Maiolo, C.; Iacopino, L.; Pepe, M.; Di Daniele, N.; De Lorenzo, A. The Impact of Body-Weight Components on Forced Spirometry in Healthy Italians. Lung 2002, 180, 149–159. [Google Scholar] [CrossRef]
- Scheja, L.; Heeren, J. The endocrine function of adipose tissues in health and cardiometabolic disease. Nat. Rev. Endocrinol. 2019, 15, 507–524. [Google Scholar] [CrossRef]
- Klein, S.; Allison, D.B.; Heymsfield, S.B.; Kelley, D.E.; Leibel, R.L.; Nonas, C.; Kahn, R. Waist circumference and cardiometabolic risk: A consensus statement from Shaping America’s Health: Association for Weight Management and Obesity Prevention; NAASO, The Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Am. J. Clin. Nutr. 2007, 85, 1197–1202. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, N.; Katritsis, D.; Raggi, P. Visceral adipose tissue as a source of inflammation and promoter of atherosclerosis. Atherosclerosis 2014, 233, 104–112. [Google Scholar] [CrossRef]
- Barnard, S.A.; Pieters, M.; De Lange, Z. The contribution of different adipose tissue depots to plasma plasminogen activator inhibitor-1 (PAI-1) levels. Blood Rev. 2016, 30, 421–429. [Google Scholar] [CrossRef] [PubMed]
- Saltiel, A.R.; Olefsky, J.M. Inflammatory mechanisms linking obesity and metabolic disease. J. Clin. Investig. 2017, 127, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Varghese, J.F.; Patel, R.; Yadav, U.C.S. Novel Insights in the Metabolic Syndrome-induced Oxidative Stress and Inflammation-mediated Atherosclerosis. Curr. Cardiol. Rev. 2018, 14, 4–14. [Google Scholar] [CrossRef]
- Noce, A.; Fabrini, R.; Dessì, M.; Bocedi, A.; Santini, S.; Rovella, V.; Pastore, A.; Tesauro, M.; Bernardini, S.; Di Daniele, N.; et al. Erythrocyte glutathione transferase activity: A possible early biomarker for blood toxicity in uremic diabetic patients. Acta Diabetol. 2014, 51, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Gombault, A.; Baron, L.; Couillin, I. ATP release and purinergic signaling in NLRP3 inflammasome activation. Front. Immunol. 2013, 3, 414. [Google Scholar] [CrossRef]
- Wang, J.; Sun, C.; Gerdes, N.; Liu, C.; Liao, M.; Liu, J.; Shi, M.A.; He, A.; Zhou, Y.; Sukhova, G.K.; et al. Interleukin 18 function in atherosclerosis is mediated by the interleukin 18 receptor and the Na-Cl co-transporter. Nat. Med. 2015, 21, 820–826. [Google Scholar] [CrossRef]
- Noce, A.; Canale, M.P.; Capria, A.; Rovella, V.; Tesauro, M.; Splendiani, G.; Annicchiarico-Petruzzelli, M.; Manzuoli, M.; Simonetti, G.; Di Daniele, N. Coronary artery calcifications predict long term cardiovascular events in non diabetic Caucasian hemodialysis patients. Aging (Albany NY) 2015, 7, 269–279. [Google Scholar] [CrossRef] [PubMed]
- Grandl, G.; Wolfrum, C. Hemostasis, endothelial stress, inflammation, and the metabolic syndrome. Semin. Immunopathol. 2018, 40, 215–224. [Google Scholar] [CrossRef]
- Yamagishi, S.-I. Role of advanced glycation end products (AGEs) and receptor for AGEs (RAGE) in vascular damage in diabetes. Exp. Gerontol. 2011, 46, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Moldogazieva, N.T.; Mokhosoev, I.M.; Mel’Nikova, T.I.; Porozov, Y.B.; Terentiev, A.A. Oxidative Stress and Advanced Lipoxidation and Glycation End Products (ALEs and AGEs) in Aging and Age-Related Diseases. Oxidative Med. Cell. Longev. 2019, 2019, 3085756. [Google Scholar] [CrossRef]
- Tejero, J.; Shiva, S.; Gladwin, M.T. Sources of Vascular Nitric Oxide and Reactive Oxygen Species and Their Regulation. Physiol. Rev. 2019, 99, 311–379. [Google Scholar] [CrossRef] [PubMed]
- Schinzari, F.; Iantorno, M.; Campia, U.; Mores, N.; Rovella, V.; Tesauro, M.; Di Daniele, N.; Cardillo, C. Vasodilator responses and endothelin-dependent vasoconstriction in metabolically healthy obesity and the metabolic syndrome. Am. J. Physiol. Endocrinol. Metab. 2015, 309, E787–E792. [Google Scholar] [CrossRef]
- Couto, E.; Boffetta, P.; Lagiou, P.; Ferrari, P.; Buckland, G.; Overvad, K.; Dahm, C.C.; Tjonneland, A.; Olsen, A.O.; Clavelchapelon, F.; et al. Mediterranean dietary pattern and cancer risk in the EPIC cohort. Br. J. Cancer 2011, 104, 1493–1499. [Google Scholar] [CrossRef] [PubMed]
- Bendinelli, B.; Masala, G.; Saieva, C.; Salvini, S.; Calonico, C.; Sacerdote, C.; Agnoli, C.; Grioni, S.; Frasca, G.; Mattiello, A.; et al. Fruit, vegetables, and olive oil and risk of coronary heart disease in Italian women: The EPICOR Study. Am. J. Clin. Nutr. 2010, 93, 275–283. [Google Scholar] [CrossRef]
- Liu, R.H. Dietary Bioactive Compounds and Their Health Implications. J. Food Sci. 2013, 78 (Suppl. S1), A18–A25. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.H. Potential Synergy of Phytochemicals in Cancer Prevention: Mechanism of Action. J. Nutr. 2004, 134, 3479S–3485S. [Google Scholar] [CrossRef]
- Liu, R.H. Health-Promoting Components of Fruits and Vegetables in the Diet. Adv. Nutr. 2013, 4, 384S–392S. [Google Scholar] [CrossRef]
- Arauna, D.; Furrianca, M.; Espinosa-Parrilla, Y.; Fuentes, E.; Alarcón, M.; Palomo, I. Natural Bioactive Compounds As Protectors Of Mitochondrial Dysfunction In Cardiovascular Diseases And Aging. Molecules 2019, 24, 4259. [Google Scholar] [CrossRef]
- Li, R.; Zhang, Y.; Rasool, S.; Geetha, T.; Babu, J.R. Effects and Underlying Mechanisms of Bioactive Compounds on Type 2 Diabetes Mellitus and Alzheimer’s Disease. Oxidative Med. Cell. Longev. 2019, 2019, 8165707. [Google Scholar] [CrossRef]
- Andrade, S.; Ramalho, M.J.; Loureiro, J.A.; Pereira, M.D.C. Natural Compounds for Alzheimer’s Disease Therapy: A Systematic Review of Preclinical and Clinical Studies. Int. J. Mol. Sci. 2019, 20, 2313. [Google Scholar] [CrossRef]
- Noce, A.; Bocedi, A.; Campo, M.; Marrone, G.; Di Lauro, M.; Cattani, G.; Di Daniele, N.; Romani, A. A Pilot Study of a Natural Food Supplement as New Possible Therapeutic Approach in Chronic Kidney Disease Patients. Pharmaceuticals (Basel) 2020, 13, 148. [Google Scholar] [CrossRef]
- Noce, A.; Marrone, G.; Di Lauro, M.; Urciuoli, S.; Pietroboni Zaitseva, A.; Wilson Jones, G.; Di Daniele, N.; Romani, A. Cardiovascular Protection of Nephropathic Male Patients by Oral Food Supplements. Cardiovasc. Ther. 2020, 2020, 1807941. [Google Scholar] [CrossRef]
- Noce, A.; Marrone, G.; Ottaviani, E.; Guerriero, C.; Di Daniele, F.; Pietroboni Zaitseva, A.; Di Daniele, N. Uremic Sarcopenia and Its Possible Nutritional Approach. Nutrients 2021, 13, 147. [Google Scholar] [CrossRef]
- Karasawa, M.M.G.; Mohan, C. Fruits as Prospective Reserves of bioactive Compounds: A Review. Nat. Prod. Bioprospecting 2018, 8, 335–346. [Google Scholar] [CrossRef]
- Noce, A.; Di Daniele, F.; Campo, M.; Di Lauro, M.; Zaitseva, A.P.; Di Daniele, N.; Marrone, G.; Romani, A. Effect of Hydrolysable Tannins and Anthocyanins on Recurrent Urinary Tract Infections in Nephropathic Patients: Preliminary Data. Nutrients 2021, 13, 591. [Google Scholar] [CrossRef]
- Di Daniele, N.; Marrone, G.; Di Lauro, M.; Di Daniele, F.; Palazzetti, D.; Guerriero, C.; Noce, A. Effects of Caloric Restriction Diet on Arterial Hypertension and Endothelial Dysfunction. Nutrients 2021, 13, 274. [Google Scholar] [CrossRef] [PubMed]
- Rochlani, Y.; Pothineni, N.V.; Kovelamudi, S.; Mehta, J.L. Metabolic syndrome: Pathophysiology, management, and modulation by natural compounds. Ther. Adv. Cardiovasc. Dis. 2017, 11, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Rains, T.M.; Agarwal, S.; Maki, K.C. Antiobesity effects of green tea catechins: A mechanistic review. J. Nutr. Biochem. 2011, 22, 1–7. [Google Scholar] [CrossRef]
- Huang, J.; Wang, Y.; Xie, Z.; Zhou, Y.; Zhang, Y.; Wan, X. The anti-obesity effects of green tea in human intervention and basic molecular studies. Eur. J. Clin. Nutr. 2014, 68, 1075–1087. [Google Scholar] [CrossRef]
- Hibi, M.; Takase, H.; Iwasaki, M.; Osaki, N.; Katsuragi, Y. Efficacy of tea catechin-rich beverages to reduce abdominal adiposity and metabolic syndrome risks in obese and overweight subjects: A pooled analysis of 6 human trials. Nutr. Res. 2018, 55, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.-H.; Liu, C.-Y.; Wang, L.-Y.; Huang, C.-J.; Hsu, C.-H. Effects of green tea extract on overweight and obese women with high levels of low density-lipoprotein-cholesterol (LDL-C): A randomised, double-blind, and cross-over placebo-controlled clinical trial. BMC Complement. Altern. Med. 2018, 18, 294. [Google Scholar] [CrossRef] [PubMed]
- Mielgo-Ayuso, J.; Barrenechea, L.; Alcorta, P.; Larrarte, E.; Margareto, J.; Labayen, I. Effects of dietary supplementation with epigallocatechin-3-gallate on weight loss, energy homeostasis, cardiometabolic risk factors and liver function in obese women: Randomised, double-blind, placebo-controlled clinical trial. Br. J. Nutr. 2014, 111, 1263–1271. [Google Scholar] [CrossRef]
- Chen, I.-J.; Liu, C.-Y.; Chiu, J.-P.; Hsu, C.-H. Therapeutic effect of high-dose green tea extract on weight reduction: A randomized, double-blind, placebo-controlled clinical trial. Clin. Nutr. 2016, 35, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Gao, C.; Yan, P.; Zhang, M.; Wang, Y.; Hu, Y.; Wu, X.; Wang, X.; Sheng, J. EGCG Reduces Obesity and White Adipose Tissue Gain Partly Through AMPK Activation in Mice. Front. Pharmacol. 2018, 9, 1366. [Google Scholar] [CrossRef]
- Chow, H.H.; Cai, Y.; Alberts, D.S.; Hakim, I.; Dorr, R.; Shahi, F.; Crowell, J.A.; Yang, C.S.; Hara, Y. Phase I pharmacokinetic study of tea polyphenols following single-dose administration of epigallocatechin gallate and polyphenon E. Cancer Epidemiol. Biomarkers Prev. 2001, 10, 53–58. [Google Scholar]
- Clark, K.S.; Coleman, C.; Shelton, R.; Heemstra, L.A.; Novak, C.M. Caffeine enhances activity thermogenesis and energy expenditure in rats. Clin. Exp. Pharmacol. Physiol. 2019, 46, 475–482. [Google Scholar] [CrossRef]
- Watanabe, T.; Kobayashi, S.; Yamaguchi, T.; Hibi, M.; Fukuhara, I.; Osaki, N. Coffee Abundant in Chlorogenic Acids Reduces Abdominal Fat in Overweight Adults: A Randomized, Double-Blind, Controlled Trial. Nutrients 2019, 11, 1617. [Google Scholar] [CrossRef]
- Zhong, Y.; Ding, Y.; Li, L.; Ge, M.; Ban, G.; Yang, H.; Dai, J.; Zhang, L. Effects and Mechanism of Chlorogenic Acid on Weight Loss. Curr. Pharm. Biotechnol. 2020, 21, 1099–1106. [Google Scholar] [CrossRef]
- Rock, C.L.; Flatt, S.W.; Barkai, H.-S.; Pakiz, B.; Heath, D.D. Walnut consumption in a weight reduction intervention: Effects on body weight, biological measures, blood pressure and satiety. Nutr. J. 2017, 16, 76. [Google Scholar] [CrossRef] [PubMed]
- Cassady, B.A.; Hollis, J.H.; Fulford, A.D.; Considine, R.V.; Mattes, R.D. Mastication of almonds: Effects of lipid bioaccessibility, appetite, and hormone response. Am. J. Clin. Nutr. 2009, 89, 794–800. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.; Mattes, R.D. Appetitive, dietary and health effects of almonds consumed with meals or as snacks: A randomized, controlled trial. Eur. J. Clin. Nutr. 2013, 67, 1205–1214. [Google Scholar] [CrossRef]
- Di Pierro, F.; Bressan, A.; Ranaldi, D.; Rapacioli, G.; Giacomelli, L.; Bertuccioli, A. Potential role of bioavailable curcumin in weight loss and omental adipose tissue decrease: Preliminary data of a randomized, controlled trial in overweight people with metabolic syndrome. Preliminary study. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 4195–4202. [Google Scholar] [PubMed]
- Wu, L.-Y.; Chen, C.-W.; Chen, L.-K.; Chou, H.-Y.; Chang, C.-L.; Juan, C.-C. Curcumin Attenuates Adipogenesis by Inducing Preadipocyte Apoptosis and Inhibiting Adipocyte Differentiation. Nutrients 2019, 11, 2307. [Google Scholar] [CrossRef]
- Panahi, Y.; Hosseini, M.S.; Khalili, N.; Naimi, E.; Soflaei, S.S.; Majeed, M.; Sahebkar, A. Effects of supplementation with curcumin on serum adipokine concentrations: A randomized controlled trial. Nutritions 2016, 32, 1116–1122. [Google Scholar] [CrossRef]
- Jia, Q.; Cao, H.; Shen, D.; Li, S.; Yan, L.; Chen, C.; Xing, S.; Dou, F. Quercetin protects against atherosclerosis by regulating the expression of PCSK9, CD36, PPARγ, LXRα and ABCA1. Int. J. Mol. Med. 2019, 44, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Vazquez Cisneros, L.C.; López-Uriarte, P.; López-Espinoza, A.; Navarro Meza, M.; Espinoza-Gallardo, A.C.; Guzman Aburto, M.B. EEffects of green tea and its epigallocatechin (EGCG) content on body weight and fat mass in humans: A systematic review. Nutr. Hosp. 2017, 34, 731–737. [Google Scholar] [CrossRef]
- Hursel, R.; Viechtbauer, W.; Dulloo, A.G.; Tremblay, A.; Tappy, L.; Rumpler, W.; Westerterp-Plantenga, M.S. The effects of catechin rich teas and caffeine on energy expenditure and fat oxidation: A meta-analysis. Obes. Rev. 2011, 12, e573–e581. [Google Scholar] [CrossRef]
- Yang, C.S.; Zhang, J.; Zhang, L.; Huang, J.; Wang, Y. Mechanisms of body weight reduction and metabolic syndrome alleviation by tea. Mol. Nutr. Food Res. 2016, 60, 160–174. [Google Scholar] [CrossRef] [PubMed]
- Unno, T.; Sakuma, M.; Mitsuhashi, S. Effect of Dietary Supplementation of (−)-Epigallocatechin Gallate on Gut Microbiota and Biomarkers of Colonic Fermentation in Rats. J. Nutr. Sci. Vitaminol. (Tokyo) 2014, 60, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Pervin, M.; Goto, S.; Isemura, M.; Nakamura, Y. Beneficial Effects of Tea and the Green Tea Catechin Epigallocatechin-3-gallate on Obesity. Molecules 2016, 21, 1305. [Google Scholar] [CrossRef]
- Noce, A.; Marrone, G.; Di Daniele, F.; Ottaviani, E.; Wilson Jones, G.; Bernini, R.; Romani, A.; Rovella, V. Impact of Gut Microbiota Composition on Onset and Progression of Chronic Non-Communicable Diseases. Nutrients 2019, 11, 1073. [Google Scholar] [CrossRef] [PubMed]
- Andreu-Fernandez, V.; Almeida Toledano, L.; Pizarro, N.; Navarro-Tapia, E.; Gomez-Roig, M.D.; de la Torre, R.; Garcia-Algar, O. Bioavailability of Epigallocatechin Gallate Administered with Different Nutritional Strategies in Healthy Volunteers. Antioxidants (Basel) 2020, 9, 440. [Google Scholar] [CrossRef]
- Tabrizi, R.; Saneei, P.; Lankarani, K.B.; Akbari, M.; Kolahdooz, F.; Esmaillzadeh, A.; Nadi-Ravandi, S.; Mazoochi, M.; Asemi, Z. The effects of caffeine intake on weight loss: A systematic review and dos-response meta-analysis of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 2019, 59, 2688–2696. [Google Scholar] [CrossRef] [PubMed]
- Harpaz, E.; Tamir, S.; Weinstein, A.; Weinstein, Y. The effect of caffeine on energy balance. J. Basic Clin. Physiol. Pharmacol. 2017, 28, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Lim, W.; Kim, S.; Khil, H.; Cheon, E.; An, S.; Hong, S.; Lee, D.H.; Kang, S.-S.; Oh, H.; et al. Coffee Intake and Obesity: A Meta-Analysis. Nutrients 2019, 11, 1274. [Google Scholar] [CrossRef]
- Noce, A.; Marrone, G.; Di Daniele, F.; Di Lauro, M.; Pietroboni Zaitseva, A.; Wilson Jones, G.; De Lorenzo, A.; Di Daniele, N. Potential Cardiovascular and Metabolic Beneficial Effects of ω-3 PUFA in Male Obesity Secondary Hypogonadism Syndrome. Nutrients 2020, 12, 2519. [Google Scholar] [CrossRef] [PubMed]
- Dessì, M.; Noce, A.; Bertucci, P.; Noce, G.; Rizza, S.; De Stefano, A.; Manca Di Villahermosa, S.; Bernardini, S.; De Lorenzo, A.; Di Daniele, N. Plasma and erythrocyte membrane phospholipids and fatty acids in Italian general population and hemodialysis patients. Lipids Health Dis. 2014, 13, 54. [Google Scholar] [CrossRef]
- Konstantinidi, M.; Koutelidakis, A.E. Functional Foods and Bioactive Compounds: A Review of Its Possible Role on Weight Management and Obesity’s Metabolic Consequences. Medicines (Basel) 2019, 6, 94. [Google Scholar] [CrossRef]
- Mousavi, S.M.; Milajerdi, A.; Varkaneh, H.K.; Gorjipour, M.M.; Esmaillzadeh, A. The effects of curcumin supplementation on body weight, body mass index and waist circumference: A systematic review and dose-response meta-analysis of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 2020, 60, 171–180. [Google Scholar] [CrossRef]
- Akbari, M.; Lankarani, K.B.; Tabrizi, R.; Ghayour-Mobarhan, M.; Peymani, P.; Ferns, G.; Ghaderi, A.; Asemi, Z. The Effects of Curcumin on Weight Loss Among Patients With Metabolic Syndrome and Related Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Pharmacol. 2019, 10, 649. [Google Scholar] [CrossRef]
- Sharma, R.A.; Steward, W.P.; Gescher, A.J. Pharmacokinetics and pharmacodynamics of curcumin. Adv. Exp. Med. Biol. 2007, 595, 453–470. [Google Scholar]
- Dei Cas, M.; Ghidoni, R. Dietary Curcumin: Correlation between Bioavailability and Health Potential. Nutrients 2019, 11, 2147. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.A.; McLelland, H.R.; Hill, K.A.; Ireson, C.R.; Euden, S.A.; Manson, M.M.; Pirmohamed, M.; Marnett, L.J.; Gescher, A.J.; Steward, W.P. Pharmacodynamic and pharmacokinetic study of oral Curcuma extract in patients with colorectal cancer. Clin. Cancer Res. 2001, 7, 1894–1900. [Google Scholar] [PubMed]
- Leiherer, A.; Stoemmer, K.; Muendlein, A.; Saely, C.H.; Kinz, E.; Brandtner, E.M.; Fraunberger, P.; Drexel, H. Quercetin Impacts Expression of Metabolism- and Obesity-Associated Genes in SGBS Adipocytes. Nutrients 2016, 8, 282. [Google Scholar] [CrossRef] [PubMed]
- Romani, A.; Campo, M.; Urciuoli, S.; Marrone, G.; Noce, A.; Bernini, R. An Industrial and Sustainable Platform for the Production of Bioactive Micronized Powders and Extracts Enriched in Polyphenols From Olea europaea L. and Vitis vinifera L. Wastes. Front. Nutr. 2020, 7, 120. [Google Scholar] [CrossRef]
- Ahn, J.; Lee, H.; Kim, S.; Park, J.; Ha, T. The anti-obesity effect of quercetin is mediated by the AMPK and MAPK signaling pathways. Biochem. Biophys. Res. Commun. 2008, 373, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Forney, L.A.; Lenard, N.R.; Stewart, L.K.; Henagan, T.M. Dietary Quercetin Attenuates Adipose Tissue Expansion and Inflammation and Alters Adipocyte Morphology in a Tissue-Specific Manner. Int. J. Mol. Sci. 2018, 19, 895. [Google Scholar] [CrossRef]
- Graefe, E.U.; Wittig, J.; Mueller, S.; Riethling, A.-K.; Uehleke, B.; Drewelow, B.; Pforte, H.; Jacobasch, G.; Derendorf, H.; Veit, M. Pharmacokinetics and Bioavailability of Quercetin Glycosides in Humans. J. Clin. Pharmacol. 2001, 41, 492–499. [Google Scholar] [CrossRef]
- Petersen, B.; Egert, S.; Bosy-Westphal, A.; Müller, M.J.; Wolffram, S.; Hubbermann, E.M.; Rimbach, G.; Schwarz, K. Bioavailability of quercetin in humans and the influence of food matrix comparing quercetin capsules and different apple sources. Food Res. Int. 2016, 88, 159–165. [Google Scholar] [CrossRef]
- Almeida, A.F.; Borge, G.I.A.; Piskula, M.; Tudose, A.; Tudoreanu, L.; Valentová, K.; Williamson, G.; Santos, C.N. Bioavailability of Quercetin in Humans with a Focus on Interindividual Variation. Compr. Rev. Food Sci. Food Saf. 2018, 17, 714–731. [Google Scholar] [CrossRef] [PubMed]
- Ríos, J.L.; Francini, F.; Schinella, G.R. Natural Products for the Treatment of Type 2 Diabetes Mellitus. Planta Medica 2015, 81, 975–994. [Google Scholar] [CrossRef] [PubMed]
- Adibian, M.; Hodaei, H.; Nikpayam, O.; Sohrab, G.; Hekmatdoost, A.; Hedayati, M. The effects of curcumin supplementation on high-sensitivity C-reactive protein, serum adiponectin, and lipid profile in patients with type 2 diabetes: A randomized, double-blind, placebo-controlled trial. Phytother. Res. 2019, 33, 1374–1383. [Google Scholar] [CrossRef] [PubMed]
- Gutierres, V.O.; Pinheiro, C.M.; Assis, R.P.; Vendramini, R.C.; Pepato, M.T.; Brunetti, I.L. Curcumin-supplemented yoghurt improves physiological and biochemical markers of experimental diabetes. Br. J. Nutr. 2011, 108, 440–448. [Google Scholar] [CrossRef] [PubMed]
- El-Moselhy, M.A.; Taye, A.; Sharkawi, S.S.; El-Sisi, S.F.; Ahmed, A.F. The antihyperglycemic effect of curcumin in high fat diet fed rats. Role of TNF-α and free fatty acids. Food Chem. Toxicol. 2011, 49, 1129–1140. [Google Scholar] [CrossRef]
- Na, L.-X.; Zhang, Y.-L.; Li, Y.; Liu, L.-Y.; Li, R.; Kong, T.; Sun, C.-H. Curcumin improves insulin resistance in skeletal muscle of rats. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 526–533. [Google Scholar] [CrossRef] [PubMed]
- Chuengsamarn, S.; Rattanamongkolgul, S.; Luechapudiporn, R.; Phisalaphong, C.; Jirawatnotai, S. Curcumin Extract for Prevention of Type 2 Diabetes. Diabetes Care 2012, 35, 2121–2127. [Google Scholar] [CrossRef] [PubMed]
- Na, L.-X.; Li, Y.; Pan, H.-Z.; Zhou, X.-L.; Sun, D.-J.; Meng, M.; Li, X.-X.; Sun, C.-H. Curcuminoids exert glucose-lowering effect in type 2 diabetes by decreasing serum free fatty acids: A double-blind, placebo-controlled trial. Mol. Nutr. Food Res. 2012, 57, 1569–1577. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Khalili, N.; Sahebi, E.; Namazi, S.; Simental-Mendía, L.E.; Majeed, M.; Sahebkar, A. Effects of Curcuminoids Plus Piperine on Glycemic, Hepatic and Inflammatory Biomarkers in Patients with Type 2 Diabetes Mellitus: A Randomized Double-Blind Placebo-Controlled Trial. Drug Res. (Stuttg.) 2018, 68, 403–409. [Google Scholar] [CrossRef]
- Panahi, Y.; Khalili, N.; Sahebi, E.; Namazi, S.; Atkin, S.L.; Majeed, M.; Sahebkar, A. Curcuminoids Plus Piperine Modulate Adipokines in Type 2 Diabetes Mellitus. Curr. Clin. Pharmacol. 2018, 12, 253–258. [Google Scholar] [CrossRef]
- Khan, A.; Safdar, M.; Ali Khan, M.M.; Khattak, K.N.; Anderson, R.A. Cinnamon improves glucose and lipids of people with type 2 diabetes. Diabetes Care 2003, 26, 3215–3218. [Google Scholar] [CrossRef]
- Anderson, R.A.; Broadhurst, C.L.; Polansky, M.M.; Schmidt, W.F.; Khan, A.; Flanagan, V.P.; Schoene, N.W.; Graves, D.J. Isolation and characterization of polyphenol type-A polymers from cinnamon with insulin-like biological activity. J. Agric. Food Chem. 2004, 52, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Ziegenfuss, T.N.; Hofheins, J.E.; Mendel, R.W.; Landis, J.; Anderson, R.A. Effects of a water-soluble cinnamon extract on body composition and features of the metabolic syndrome in pre-diabetic men and women. J. Int. Soc. Sports Nutr. 2006, 3, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Polansky, M.M.; Anderson, R.A. Cinnamon extract and polyphenols affect the expression of tristetraprolin, insulin receptor, and glucose transporter 4 in mouse 3T3-L1 adipocytes. Arch. Biochem. Biophys. 2007, 459, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Jarvill-Taylor, K.J.; Anderson, R.A.; Graves, D.J. A hydroxychalcone derived from cinnamon functions as a mimetic for insulin in 3T3-L1 adipocytes. J. Am. Coll. Nutr. 2001, 20, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Beejmohun, V.; Peytavy-Izard, M.; Mignon, C.; Muscente-Paque, D.; Deplanque, X.; Ripoll, C.; Chapal, N. Acute effect of Ceylon cinnamon extract on postprandial glycemia: Alpha-amylase inhibition, starch tolerance test in rats, and randomized crossover clinical trial in healthy volunteers. BMC Complement. Altern. Med. 2014, 14, 351. [Google Scholar] [CrossRef]
- Sheng, X.; Zhang, Y.; Gong, Z.; Huang, C.; Zang, Y.Q. Improved Insulin Resistance and Lipid Metabolism by Cinnamon Extract through Activation of Peroxisome Proliferator-Activated Receptors. PPAR Res. 2008, 2008, 581348. [Google Scholar] [CrossRef]
- Crawford, P. Effectiveness of cinnamon for lowering hemoglobin A1C in patients with type 2 diabetes: a randomized, controlled trial. J. Am. Board Fam. Med. 2009, 22, 507–512. [Google Scholar] [CrossRef]
- Gupta Jain, S.; Puri, S.; Misra, A.; Gulati, S.; Mani, K. Effect of oral cinnamon intervention on metabolic profile and body composition of Asian Indians with metabolic syndrome: A randomized double -blind control trial. Lipids Health Dis. 2017, 16, 1–11. [Google Scholar] [CrossRef]
- Hooper, L.; Kay, C.; Abdelhamid, A.; Kroon, P.A.; Cohn, J.S.; Rimm, E.B.; Cassidy, A. Effects of chocolate, cocoa, and flavan-3-ols on cardiovascular health: A systematic review and meta-analysis of randomized trials. Am. J. Clin. Nutr. 2012, 95, 740–751. [Google Scholar] [CrossRef]
- Grassi, D.; Desideri, G.; Necozione, S.; Lippi, C.; Casale, R.; Properzi, G.; Blumberg, J.B.; Ferri, C. Blood pressure is reduced and insulin sensitivity increased in glucose-intolerant, hypertensive subjects after 15 days of consuming high-polyphenol dark chocolate. J. Nutr. 2008, 138, 1671–1676. [Google Scholar] [CrossRef]
- Greer, F.; Hudson, R.; Ross, R.; Graham, T. Caffeine ingestion decreases glucose disposal during a hyperinsulinemic-euglycemic clamp in sedentary humans. Diabetes 2001, 50, 2349–2354. [Google Scholar] [CrossRef] [PubMed]
- Belcaro, G.; Ledda, A.; Hu, S.; Cesarone, M.R.; Feragalli, B.; Dugall, M. Greenselect phytosome for borderline metabolic syndrome. Evid. Based Complement. Altern. Med. 2013, 2013, 869061. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, D.-Z. Associations of coffee consumption with circulating level of adiponectin and leptin. A meta-analysis of observational studies. Int. J. Food Sci. Nutr. 2018, 69, 1003–1012. [Google Scholar] [CrossRef]
- Wu, L.-Y.; Juan, C.-C.; Hwang, L.S.; Hsu, Y.-P.; Ho, P.-H.; Ho, L.-T. Green tea supplementation ameliorates insulin resistance and increases glucose transporter IV content in a fructose-fed rat model. Eur. J. Nutr. 2004, 43, 116–124. [Google Scholar] [CrossRef]
- Nagao, T.; Meguro, S.; Hase, T.; Otsuka, K.; Komikado, M.; Tokimitsu, I.; Yamamoto, T.; Yamamoto, K. A catechin-rich beverage improves obesity and blood glucose control in patients with type 2 diabetes. Obesity (Silver Spring) 2009, 17, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Haidari, F.; Samadi, M.; Mohammadshahi, M.; Jalali, M.T.; Engali, K.A. Energy restriction combined with green coffee bean extract affects serum adipocytokines and the body composition in obese women. Asia Pac. J. Clin. Nutr. 2017, 26, 1048–1054. [Google Scholar]
- Di Lorenzo, C.; Dell’Agli, M.; Sangiovanni, E.; Dos Santos, A.; Uberti, F.; Moro, E.; Bosisio, E.; Restani, P. Correlation between catechin content and NF-κB inhibition by infusions of green and black tea. Plant Foods Hum. Nutr. 2013, 68, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Stull, A.J.; Cash, K.C.; Johnson, W.D.; Champagne, C.M.; Cefalu, W.T. Bioactives in blueberries improve insulin sensitivity in obese, insulin-resistant men and women. J. Nutr. 2010, 140, 1764–1768. [Google Scholar] [CrossRef]
- Yang, L.; Ling, W.; Yang, Y.; Chen, Y.; Tian, Z.; Du, Z.; Chen, J.; Xie, Y.; Liu, Z.; Yang, L. Role of Purified Anthocyanins in Improving Cardiometabolic Risk Factors in Chinese Men and Women with Prediabetes or Early Untreated Diabetes—A Randomized Controlled Trial. Nutrients 2017, 9, 1104. [Google Scholar] [CrossRef] [PubMed]
- Takikawa, M.; Inoue, S.; Horio, F.; Tsuda, T. Dietary anthocyanin-rich bilberry extract ameliorates hyperglycemia and insulin sensitivity via activation of AMP-activated protein kinase in diabetic mice. J. Nutr. 2010, 140, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Ciocoiu, M.; Miron, A.; Mares, L.; Tutunaru, D.; Pohaci, C.; Groza, M.; Badescu, M. The effects of Sambucus nigra polyphenols on oxidative stress and metabolic disorders in experimental diabetes mellitus. J. Physiol. Biochem. 2009, 65, 297–304. [Google Scholar] [CrossRef]
- Mollace, V.; Sacco, I.; Janda, E.; Malara, C.; Ventrice, D.; Colica, C.; Visalli, V.; Muscoli, S.; Ragusa, S.; Muscoli, C.; et al. Hypolipemic and hypoglycaemic activity of bergamot polyphenols: From animal models to human studies. Fitoterapia 2011, 82, 309–316. [Google Scholar] [CrossRef]
- Hwang, J.-T.; Kwon, D.Y.; Yoon, S.H. AMP-activated protein kinase: A potential target for the diseases prevention by natural occurring polyphenols. New Biotechnol. 2009, 26, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Cicero, A.F.G.; Fogacci, F.; Bove, M.; Giovannini, M.; Borghi, C. Three-arm, placebo-controlled, randomized clinical trial evaluating the metabolic effect of a combined nutraceutical containing a bergamot standardized flavonoid extract in dyslipidemic overweight subjects. Phytotherapy Res. 2019, 33, 2094–2101. [Google Scholar] [CrossRef]
- Capomolla, A.S.; Janda, E.; Paone, S.; Parafati, M.; Sawicki, T.; Mollace, R.; Ragusa, S.; Mollace, V. Atherogenic Index Reduction and Weight Loss in Metabolic Syndrome Patients Treated with A Novel Pectin-Enriched Formulation of Bergamot Polyphenols. Nutrients 2019, 11, 1271. [Google Scholar] [CrossRef]
- Liu, L.; Yeh, Y.-Y. S-alk(en)yl cysteines of garlic inhibit cholesterol synthesis by deactivating HMG-CoA reductase in cultured rat hepatocytes. J. Nutr. 2002, 132, 1129–1134. [Google Scholar] [CrossRef]
- Rai, S.K.; Sharma, M.; Tiwari, M. Inhibitory effect of novel diallyldisulfide analogs on HMG-CoA reductase expression in hypercholesterolemic rats: CREB as a potential upstream target. Life Sci. 2009, 85, 211–219. [Google Scholar] [CrossRef]
- Kwon, M.-J.; Song, Y.-S.; Choi, M.-S.; Park, S.-J.; Jeong, K.-S.; Song, Y.-O. Cholesteryl ester transfer protein activity and atherogenic parameters in rabbits supplemented with cholesterol and garlic powder. Life Sci. 2003, 72, 2953–2964. [Google Scholar] [CrossRef]
- Sobenin, I.A.; Nedosugova, L.V.; Filatova, L.V.; Balabolkin, M.I.; Gorchakova, T.V.; Orekhov, A.N. Metabolic effects of time-released garlic powder tablets in type 2 diabetes mellitus: The results of double-blinded placebo-controlled study. Acta Diabetol. 2007, 45, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Taj Eldin, I.M.; Ahmed, E.M.; Elwahab, H.M.A. Preliminary Study of the Clinical Hypoglycemic Effects of Allium cepa (Red Onion) in Type 1 and Type 2 Diabetic patients. Environ. Health Insights 2010, 4, 71–77. [Google Scholar] [CrossRef]
- Um, J.-H.; Park, S.-J.; Kang, H.; Yang, S.; Foretz, M.; McBurney, M.W.; Kim, M.K.; Viollet, B.; Chung, J.H. AMP-activated protein kinase-deficient mice are resistant to the metabolic effects of resveratrol. Diabetes 2009, 59, 554–563. [Google Scholar] [CrossRef]
- Price, N.L.; Gomes, A.P.; Ling, A.J.; Duarte, F.V.; Martin-Montalvo, A.; North, B.J.; Agarwal, B.; Ye, L.; Ramadori, G.; Teodoro, J.S.; et al. SIRT1 is required for AMPK activation and the beneficial effects of resveratrol on mitochondrial function. Cell Metab. 2012, 15, 675–690. [Google Scholar] [CrossRef] [PubMed]
- Kappel, V.D.; Cazarolli, L.H.; Pereira, D.F.; Postal, B.G.; Zamoner, A.; Reginatto, F.H.; Silva, F.R. Involvement of GLUT-4 in the stimulatory effect of rutin on glucose uptake in rat soleus muscle. J. Pharm. Pharmacol. 2013, 65, 1179–1186. [Google Scholar] [CrossRef] [PubMed]
- Devaraj, S.; Yimam, M.; Brownell, L.A.; Jialal, I.; Singh, S.; Jia, Q. Effects ofAloe veraSupplementation in Subjects with Prediabetes/Metabolic Syndrome. Metab. Syndr. Relat. Disord. 2013, 11, 35–40. [Google Scholar] [CrossRef]
- Up, A.; Nna, V.; Ofem, O.; Ab, A.; Osim, E. Suppression of Gut Glucose Absorption and Enhancement of Gut Fluid Absorption in Alloxan—Induced Diabetic Rats Treated with Crude Aloe vera Gel. Res. J. Pharm. Biol. Chem. Sci. 2014, 5, 647–655. [Google Scholar]
- Shin, E.; Shin, S.; Kong, H.; Lee, S.; Do, S.-G.; Jo, T.H.; Park, Y.-I.; Lee, C.-K.; Hwang, I.-K.; Kim, K. Dietary Aloe Reduces Adipogenesis via the Activation of AMPK and Suppresses Obesity-related Inflammation in Obese Mice. Immune Netw. 2011, 11, 107–113. [Google Scholar] [CrossRef]
- Sedaghat, A.; Shahbazian, H.; Rezazadeh, A.; Haidari, F.; Jahanshahi, A.; Mahmoud Latifi, S.; Shirbeigi, E. The effect of soy nut on serum total antioxidant, endothelial function and cardiovascular risk factors in patients with type 2 diabetes. Diabetes Metab. Syndr. 2019, 13, 1387–1391. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Alonso, P.; Giardina, S.; Salas-Salvadó, J.; Arcelin, P.; Bulló, M. Chronic pistachio intake modulates circulating microRNAs related to glucose metabolism and insulin resistance in prediabetic subjects. Eur. J. Nutr. 2017, 56, 2181–2191. [Google Scholar] [CrossRef] [PubMed]
- Hosseini, S.; Jamshidi, L.; Mehrzadi, S.; Mohammad, K.; Najmizadeh, A.R.; Alimoradi, H.; Huseini, H.F. Effects of Juglans regia L. leaf extract on hyperglycemia and lipid profiles in type two diabetic patients: A randomized double-blind, placebo-controlled clinical trial. J. Ethnopharmacol. 2014, 152, 451–456. [Google Scholar] [CrossRef]
- Pivari, F.; Mingione, A.; Brasacchio, C.; Soldati, L. Curcumin and Type 2 Diabetes Mellitus: Prevention and Treatment. Nutrients 2019, 11, 1837. [Google Scholar] [CrossRef]
- Weisberg, S.P.; Leibel, R.; Tortoriello, D.V. Dietary Curcumin Significantly Improves Obesity-Associated Inflammation and Diabetes in Mouse Models of Diabesity. Endocrinology 2008, 149, 3549–3558. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.; Zhang, L.; Joo, D.; Sun, S.-C. NF-κB signaling in inflammation. Signal Transduct. Target. Ther. 2017, 2, 17023. [Google Scholar] [CrossRef]
- Donath, M.Y.; Shoelson, S.E. Type 2 diabetes as an inflammatory disease. Nat. Rev. Immunol. 2011, 11, 98–107. [Google Scholar] [CrossRef]
- Medagama, A.B. The glycaemic outcomes of Cinnamon, a review of the experimental evidence and clinical trials. Nutr. J. 2015, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Mollazadeh, H.; Hosseinzadeh, H. Cinnamon effects on metabolic syndrome: A review based on its mechanisms. Iran. J. Basic Med. Sci. 2016, 19, 1258–1270. [Google Scholar] [CrossRef]
- Rafehi, H.; Ververis, K.; Karagiannis, T.C. Controversies surrounding the clinical potential of cinnamon for the management of diabetes. Diabetes, Obes. Metab. 2012, 14, 493–499. [Google Scholar] [CrossRef]
- Olefsky, J.M. Treatment of insulin resistance with peroxisome proliferator–activated receptor γ agonists. J. Clin. Investig. 2000, 106, 467–472. [Google Scholar] [CrossRef]
- Botta, M.; Audano, M.; Sahebkar, A.; Sirtori, C.R.; Mitro, N.; Ruscica, M. PPAR Agonists and Metabolic Syndrome: An Established Role? Int. J. Mol. Sci. 2018, 19, 1197. [Google Scholar] [CrossRef] [PubMed]
- Costello, R.B.; Dwyer, J.T.; Saldanha, L.; Bailey, R.L.; Merkel, J.; Wambogo, E. Do Cinnamon Supplements Have a Role in Glycemic Control in Type 2 Diabetes? A Narrative Review. J. Acad. Nutr. Diet. 2016, 116, 1794–1802. [Google Scholar] [CrossRef] [PubMed]
- Muhammad, D.R.A.; Dewettinck, K. Cinnamon and its derivatives as potential ingredient in functional food—A review. Int. J. Food Prop. 2017, 20, 2237–2263. [Google Scholar] [CrossRef]
- Helal, A.; Tagliazucchi, D.; Verzelloni, E.; Conte, A. Bioaccessibility of polyphenols and cinnamaldehyde in cinnamon beverages subjected to in vitro gastro-pancreatic digestion. J. Funct. Foods 2014, 7, 506–516. [Google Scholar] [CrossRef]
- Raman, G.; Avendano, E.E.; Chen, S.; Wang, J.; Matson, J.; Gayer, B.; Novotny, J.A.; Cassidy, A. Dietary intakes of flavan-3-ols and cardiometabolic health: Systematic review and meta-analysis of randomized trials and prospective cohort studies. Am. J. Clin. Nutrients 2019, 110, 1067–1078. [Google Scholar] [CrossRef]
- Sarriá, B.; Martínez-López, S.; Sierra-Cinos, J.L.; García-Diz, L.; Goya, L.; Mateos, R.; Bravo, L. Effects of bioactive constituents in functional cocoa products on cardiovascular health in humans. Food Chem. 2015, 174, 214–218. [Google Scholar] [CrossRef]
- Monteiro, J.P.; Alves, M.G.; Oliveira, P.F.; Silva, B.M. Structure-Bioactivity Relationships of Methylxanthines: Trying to Make Sense of All the Promises and the Drawbacks. Molecules 2016, 21, 974. [Google Scholar] [CrossRef] [PubMed]
- Sarriá, B.; Gomez-Juaristi, M.; Martinez López, S.; Garcia Cordero, J.; Bravo, L.; Mateos Briz, M.R. Cocoa colonic phenolic metabolites are related to HDL-cholesterol raising effects and methylxanthine metabolites and insoluble dietary fibre to anti-inflammatory and hypoglycemic effects in humans. PeerJ 2020, 8, e9953. [Google Scholar] [CrossRef] [PubMed]
- Bhupathiraju, S.N.; Pan, A.; Malik, V.S.; Manson, J.E.; Willett, W.C.; Van Dam, R.M.; Hu, F.B. Caffeinated and caffeine-free beverages and risk of type 2 diabetes. Am. J. Clin. Nutr. 2013, 97, 155–166. [Google Scholar] [CrossRef]
- Monteiro, J.; Alves, M.G.; Oliveira, P.F.; Silva, B.M. Pharmacological potential of methylxanthines: Retrospective analysis and future expectations. Crit. Rev. Food Sci. Nutr. 2018, 59, 2597–2625. [Google Scholar] [CrossRef]
- Muley, A.; Muley, P.; Shah, M. Coffee to Reduce Risk of Type 2 Diabetes? A Systematic Review. Curr. Diabetes Rev. 2012, 8, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Ding, M.; Bhupathiraju, S.N.; Satija, A.; Van Dam, R.M.; Hu, F.B. Long-term coffee consumption and risk of cardiovascular disease: A systematic review and a dose-response meta-analysis of prospective cohort studies. Circulation 2014, 129, 643–659. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.-S.; Wang, W.-Y.; Fan, W.-Y.; Deng, Q.; Wang, X. Tea consumption and risk of type 2 diabetes: A dose–response meta-analysis of cohort studies. Br. J. Nutr. 2014, 111, 1329–1339. [Google Scholar] [CrossRef]
- Liu, K.; Zhou, R.; Wang, B.; Chen, K.; Shi, L.-Y.; Zhu, J.-D.; Mi, M.-T. Effect of green tea on glucose control and insulin sensitivity: A meta-analysis of 17 randomized controlled trials. Am. J. Clin. Nutr. 2013, 98, 340–348. [Google Scholar] [CrossRef]
- Xu, R.; Bai, Y.; Yang, K.; Chen, G. Effects of green tea consumption on glycemic control: A systematic review and meta-analysis of randomized controlled trials. Nutr. Metab. (Lond.) 2020, 17, 56. [Google Scholar] [CrossRef] [PubMed]
- Mumford, G.K.; Benowitz, N.L.; Evans, S.M.; Kaminski, B.J.; Preston, K.L.; Sannerud, C.A.; Silverman, K.; Griffiths, R.R. Absorption rate of methylxanthines following capsules, cola and chocolate. Eur. J. Clin. Pharmacol. 1996, 51, 319–325. [Google Scholar] [CrossRef]
- Arnaud, M.J. Pharmacokinetics and Metabolism of Natural Methylxanthines in Animal and Man. Handb. Exp. Pharmacol. 2011, 33–91. [Google Scholar] [CrossRef]
- Frühbeck, G.; Catalán, V.; Rodríguez, A.; Gómez-Ambrosi, J. Adiponectin-leptin ratio: A promising index to estimate adipose tissue dysfunction. Relation with obesity-associated cardiometabolic risk. Adipocyte 2018, 7, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Haghighatdoost, F.; Nobakht, M.G.B.F.; Hariri, M. Effect of green tea on plasma leptin and ghrelin levels: A systematic review and meta-analysis of randomized controlled clinical trials. Nutrition 2018, 45, 17–23. [Google Scholar] [CrossRef]
- Basu, A. Role of Berry Bioactive Compounds on Lipids and Lipoproteins in Diabetes and Metabolic Syndrome. Nutrients 2019, 11, 1983. [Google Scholar] [CrossRef] [PubMed]
- Tsuda, T. Recent Progress in Anti-Obesity and Anti-Diabetes Effect of Berries. Antioxidants (Basel) 2016, 5, 13. [Google Scholar] [CrossRef]
- Tsuda, T. Possible abilities of dietary factors to prevent and treat diabetes via the stimulation of glucagon-like peptide-1 secretion. Mol. Nutr. Food Res. 2015, 59, 1264–1273. [Google Scholar] [CrossRef]
- Christensen, K.B.; Petersen, R.K.; Kristiansen, K.; Christensen, L.P. Identification of bioactive compounds from flowers of black elder (Sambucus nigra L.) that activate the human peroxisome proliferator-activated receptor (PPAR) γ. Phytotherapy Res. 2010, 24 (Suppl. S2), S129–S132. [Google Scholar] [CrossRef] [PubMed]
- Calvano, A.; Izuora, K.; Oh, E.C.; Ebersole, J.L.; Lyons, T.J.; Basu, A. Dietary berries, insulin resistance and type 2 diabetes: An overview of human feeding trials. Food Funct. 2019, 10, 6227–6243. [Google Scholar] [CrossRef]
- Kay, C.D. Aspects of anthocyanin absorption, metabolism and pharmacokinetics in humans. Nutr. Res. Rev. 2006, 19, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Fang, J. Bioavailability of anthocyanins. Drug Metab. Rev. 2014, 46, 508–520. [Google Scholar] [CrossRef] [PubMed]
- Mollace, V.; Scicchitano, M.; Paone, S.; Casale, F.; Calandruccio, C.; Gliozzi, M.; Musolino, V.; Carresi, C.; Maiuolo, J.; Nucera, S.; et al. Hypoglycemic and Hypolipemic Effects of a New Lecithin Formulation of Bergamot Polyphenolic Fraction: A Double Blind, Randomized, Placebo- Controlled Study. Endocrine, Metab. Immune Disord. Drug Targets 2019, 19, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Shabani, E.; Sayemiri, K.; Mohammadpour, M. The effect of garlic on lipid profile and glucose parameters in diabetic patients: A systematic review and meta-analysis. Prim. Care Diabetes 2019, 13, 28–42. [Google Scholar] [CrossRef]
- Marrelli, M.; Amodeo, V.; Statti, G.; Conforti, F. Biological Properties and Bioactive Components of Allium cepa L.: Focus on Potential Benefits in the Treatment of Obesity and Related Comorbidities. Molecules 2018, 24, 119. [Google Scholar] [CrossRef]
- Oyenihi, O.R.; Oyenihi, A.B.; Adeyanju, A.A.; Oguntibeju, O.O. Antidiabetic Effects of Resveratrol: The Way Forward in Its Clinical Utility. J. Diabetes Res. 2016, 2016, 9737483. [Google Scholar] [CrossRef] [PubMed]
- Bai, X.; Yao, L.; Ma, X.; Xu, X. Small Molecules as SIRT Modulators. Mini-Reviews Med. Chem. 2018, 18, 1151–1157. [Google Scholar] [CrossRef]
- Milne, J.C.; Lambert, P.D.; Schenk, S.; Carney, D.P.; Smith, J.J.; Gagne, D.J.; Jin, L.; Boss, O.; Perni, R.B.; Vu, C.B.; et al. Small molecule activators of SIRT1 as therapeutics for the treatment of type 2 diabetes. Nat. Cell Biol. 2007, 450, 712–716. [Google Scholar] [CrossRef]
- Öztürk, E.; Arslan, A.K.K.; Yerer, M.B.; Bishayee, A. Resveratrol and diabetes: A critical review of clinical studies. Biomed. Pharmacother. 2017, 95, 230–234. [Google Scholar] [CrossRef]
- Li, Y.Q.; Zhou, F.C.; Gao, F.; Bian, J.S.; Shan, F. Comparative Evaluation of Quercetin, Isoquercetin and Rutin as Inhibitors of α-Glucosidase. J. Agric. Food Chem. 2009, 57, 11463–11468. [Google Scholar] [CrossRef]
- Kappel, V.D.; Zanatta, L.; Postal, B.G.; Silva, F.R. Rutin potentiates calcium uptake via voltage-dependent calcium channel associated with stimulation of glucose uptake in skeletal muscle. Arch. Biochem. Biophys. 2013, 532, 55–60. [Google Scholar] [CrossRef]
- Ghorbani, A. Mechanisms of antidiabetic effects of flavonoid rutin. Biomed. Pharmacother. 2017, 96, 305–312. [Google Scholar] [CrossRef]
- Ortuño, J.; Covas, M.-I.; Farre, M.; Pujadas, M.; Fito, M.; Khymenets, O.; Andres-Lacueva, C.; Roset, P.; Joglar, J.; Lamuela-Raventós, R.M.; et al. Matrix effects on the bioavailability of resveratrol in humans. Food Chem. 2010, 120, 1123–1130. [Google Scholar] [CrossRef]
- Rotches-Ribalta, M.; Andres-Lacueva, C.; Estruch, R.; Escribano, E.; Urpi-Sarda, M. Pharmacokinetics of resveratrol metabolic profile in healthy humans after moderate consumption of red wine and grape extract tablets. Pharmacol. Res. 2012, 66, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Dick, W.R.; Fletcher, E.A.; Shah, S.A. Reduction of Fasting Blood Glucose and Hemoglobin A1c Using Oral Aloe Vera: A Meta-Analysis. J. Altern. Complement. Med. 2016, 22, 450–457. [Google Scholar] [CrossRef]
- Ramdath, D.D.; Padhi, E.M.T.; Sarfaraz, S.; Renwick, S.; Duncan, A.M. Beyond the Cholesterol-Lowering Effect of Soy Protein: A Review of the Effects of Dietary Soy and Its Constituents on Risk Factors for Cardiovascular Disease. Nutrients 2017, 9, 324. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Kim, U.-H.; Yoon, J.-H.; Ji, H.-S.; Park, H.-M.; Park, H.-Y.; Jeong, T.-S. Suppression of Hyperglycemia and Hepatic Steatosis by Black-Soybean-Leaf Extract via Enhanced Adiponectin-Receptor Signaling and AMPK Activation. J. Agric. Food Chem. 2018, 67, 90–101. [Google Scholar] [CrossRef]
- Godsland, I.F. Oestrogens and insulin secretion. Diabetologia 2005, 48, 2213–2220. [Google Scholar] [CrossRef]
- Zhang, Y.-B.; Chen, W.-H.; Guo, J.-J.; Fu, Z.-H.; Yi, C.; Zhang, M.; Na, X.-L. Soy isoflavone supplementation could reduce body weight and improve glucose metabolism in non-Asian postmenopausal women—A meta-analysis. Nutrition 2013, 29, 8–14. [Google Scholar] [CrossRef]
- Watanabe, S.; Yamaguchi, M.; Sobue, T.; Takahashi, T.; Miura, T.; Arai, Y.; Mazur, W.; Wahala, K.; Adlercreutz, H. Pharmacokinetics of soybean isoflavones in plasma, urine and feces of men after ingestion of 60 g baked soybean powder (kinako). J. Nutr. 1998, 128, 1710–1715. [Google Scholar] [CrossRef]
- Rüfer, C.E.; Bub, A.; Möseneder, J.; Winterhalter, P.; Stürtz, M.; Kulling, S.E. Pharmacokinetics of the soybean isoflavone daidzein in its aglycone and glucoside form: A randomized, double-blind, crossover study. Am. J. Clin. Nutr. 2008, 87, 1314–1323. [Google Scholar] [CrossRef]
- Alasalvar, C.; Shahidi, F.; Liyanapathirana, C.M.; Ohshima, T. Turkish Tombul Hazelnut (Corylus avellana L.). 1. Compositional Characteristics. J. Agric. Food Chem. 2003, 51, 3790–3796. [Google Scholar] [CrossRef] [PubMed]
- Rusu, M.E.; Gheldiu, A.-M.; Mocan, A.; Vlase, L.; Popa, D.-S. Anti-aging potential of tree nuts with a focus on the phytochemical composition, molecular mechanisms and thermal stability of major bioactive compounds. Food Funct. 2018, 9, 2554–2575. [Google Scholar] [CrossRef] [PubMed]
- Alkhatib, A.; Tsang, C.; Tiss, A.; Bahorun, T.; Arefanian, H.; Barake, R.; Khadir, A.; Tuomilehto, J. Functional Foods and Lifestyle Approaches for Diabetes Prevention and Management. Nutrients 2017, 9, 1310. [Google Scholar] [CrossRef]
- Hernández-Alonso, P.; Camacho-Barcia, L.; Bulló, M.; Salas-Salvadó, J. Nuts and Dried Fruits: An Update of Their Beneficial Effects on Type 2 Diabetes. Nutrients 2017, 9, 673. [Google Scholar] [CrossRef]
- Ribeiro, P.V.M.; Silva, A.; Almeida, A.P.; Hermsdorff, H.H.; Alfenas, R.C. Effect of chronic consumption of pistachios (Pistacia vera L.) on glucose metabolism in pre-diabetics and type 2 diabetics: A systematic review. Crit. Rev. Food Sci. Nutr. 2017, 59, 1115–1123. [Google Scholar] [CrossRef]
- Shayo, S.C.; Kawade, S.; Ogiso, K.; Yoshihiko, N. Strategies to ameliorate endothelial dysfunction associated with metabolic syndrome, where are we? Diabetes Metab. Syndr. 2019, 13, 2164–2169. [Google Scholar] [CrossRef] [PubMed]
- Vazquez-Prieto, M.A.; Rodriguez Lanzi, C.; Lembo, C.; Galmarini, C.R.; Miatello, R.M. Garlic and onion attenuates vascular inflammation and oxidative stress in fructose-fed rats. J. Nutr. Metab. 2011, 2011, 475216. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Collazo, J.; Alonso-Carbajo, L.; López-Medina, A.I.; Alpizar, Y.A.; Tajada, S.; Nilius, B.; Voets, T.; López-López, J.R.; Talavera, K.; Pérez-García, M.T.; et al. Cinnamaldehyde inhibits L-type calcium channels in mouse ventricular cardiomyocytes and vascular smooth muscle cells. Pflügers Arch. 2014, 466, 2089–2099. [Google Scholar] [CrossRef]
- Toledo, E.; Hu, F.B.; Estruch, R.; Buil-Cosiales, P.; Corella, D.; Salas-Salvadó, J.; Covas, M.I.; Arós, F.; Gómez-Gracia, E.; Fiol, M.; et al. Effect of the Mediterranean diet on blood pressure in the PREDIMED trial: Results from a randomized controlled trial. BMC Med. 2013, 11, 207. [Google Scholar] [CrossRef]
- Rozati, M.; Barnett, J.B.; Wu, D.; Handelman, G.J.; Saltzman, E.; Wilson, T.A.; Li, L.; Wang, J.; Marcos, A.; Ordovás, J.M.; et al. Cardio-metabolic and immunological impacts of extra virgin olive oil consumption in overweight and obese older adults: A randomized controlled trial. Nutr. Metab. 2015, 12, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Storniolo, C.E.; Casillas, R.; Bullo, M.; Castaner, O.; Ros, E.; Saez, G.T.; Toledo, E.; Estruch, R.; Ruiz-Gutiérrez, V.; Fito, M.; et al. A Mediterranean diet supplemented with extra virgin olive oil or nuts improves endothelial markers involved in blood pressure control in hypertensive women. Eur. J. Nutr. 2015, 56, 89–97. [Google Scholar] [CrossRef]
- Hasani, H.; Arab, A.; Hadi, A.; Pourmasoumi, M.; Ghavami, A.; Miraghajani, M. Does ginger supplementation lower blood pressure? A systematic review and meta-analysis of clinical trials. Phytotherapy Res. 2019, 33, 1639–1647. [Google Scholar] [CrossRef] [PubMed]
- Ludovici, V.; Barthelmes, J.; Nägele, M.P.; Enseleit, F.; Ferri, C.; Flammer, A.J.; Ruschitzka, F.; Sudano, I. Cocoa, Blood Pressure, and Vascular Function. Front. Nutr. 2017, 4, 36. [Google Scholar] [CrossRef]
- Huang, H.; Chen, G.; Liao, D.; Zhu, Y.; Pu, R.; Xue, X. The effects of resveratrol intervention on risk markers of cardiovascular health in overweight and obese subjects: A pooled analysis of randomized controlled trials. Obes. Rev. 2016, 17, 1329–1340. [Google Scholar] [CrossRef]
- Fogacci, F.; Tocci, G.; Presta, V.; Fratter, A.; Borghi, C.; Cicero, A.F.G. Effect of resveratrol on blood pressure: A systematic review and meta-analysis of randomized, controlled, clinical trials. Crit. Rev. Food Sci. Nutr. 2019, 59, 1605–1618. [Google Scholar] [CrossRef] [PubMed]
- Prysyazhna, O.; Wolhuter, K.; Switzer, C.; Santos, C.; Yang, X.; Lynham, S.; Shah, A.M.; Eaton, P.; Burgoyne, J.R. Blood Pressure–Lowering by the Antioxidant Resveratrol Is Counterintuitively Mediated by Oxidation of cGMP-Dependent Protein Kinase. Circulation 2019, 140, 126–137. [Google Scholar] [CrossRef]
- Stabler, S.N.; Tejani, A.M.; Huynh, F.; Fowkes, C. Garlic for the prevention of cardiovascular morbidity and mortality in hypertensive patients. Cochrane Database Syst. Rev. 2012, 2012, CD007653. [Google Scholar] [CrossRef]
- Xiong, X.J.; Wang, P.Q.; Li, S.J.; Li, X.K.; Zhang, Y.Q.; Wang, J. Garlic for hypertension: A systematic review and meta-analysis of randomized controlled trials. Phytomedicine 2015, 22, 352–361. [Google Scholar] [CrossRef] [PubMed]
- Matsutomo, T. Potential benefits of garlic and other dietary supplements for the management of hypertension. Exp. Ther. Med. 2020, 19, 1479–1484. [Google Scholar] [CrossRef]
- Choudhary, P.R.; Jani, R.D.; Sharma, M.S. Effect of Raw Crushed Garlic (Allium sativum L.) on Components of Metabolic Syndrome. J. Diet. Suppl. 2018, 15, 499–506. [Google Scholar] [CrossRef]
- Al Disi, S.S.; Anwar, M.A.; Eid, A.H. Anti-hypertensive Herbs and their Mechanisms of Action: Part I. Front. Pharmacol. 2016, 6, 323. [Google Scholar] [CrossRef]
- Akilen, R.; Pimlott, Z.; Tsiami, A.; Robinson, N. Effect of short-term administration of cinnamon on blood pressure in patients with prediabetes and type 2 diabetes. Nutrition 2013, 29, 1192–1196. [Google Scholar] [CrossRef]
- Mousavi, S.M.; Karimi, E.; Hajishafiee, M.; Milajerdi, A.; Amini, M.R.; Esmaillzadeh, A. Anti-hypertensive effects of cinnamon supplementation in adults: A systematic review and dose-response Meta-analysis of randomized controlled trials. Crit. Rev. Food Sci. Nutr. 2020, 60, 3144–3154. [Google Scholar] [CrossRef]
- Efentakis, P.; Iliodromitis, E.K.; Mikros, E.; Papachristodoulou, A.; Dagres, N.; Skaltsounis, A.-L.; Andreadou, I. Effects of the olive tree leaf constituents on myocardial oxidative damage and atherosclerosis. Planta Medica 2015, 81, 648–654. [Google Scholar] [CrossRef]
- López, S.; Bermudez, B.; Montserrat de la Paz, S.; Jaramillo, S.; Abia, R.; Muriana, F.J. Virgin Olive Oil and Hypertension. Curr. Vasc. Pharmacol. 2016, 14, 1. [Google Scholar] [CrossRef]
- De Pergola, G.; D’Alessandro, A. Influence of Mediterranean Diet on Blood Pressure. Nutrients 2018, 10, 1700. [Google Scholar] [CrossRef]
- Summerhill, V.; Karagodin, V.; Grechko, A.; Myasoedova, V.; Orekhov, A. Vasculoprotective Role of Olive Oil Compounds via Modulation of Oxidative Stress in Atherosclerosis. Front. Cardiovasc. Med. 2018, 5, 188. [Google Scholar] [CrossRef]
- Massaro, M.; Scoditti, E.; Carluccio, M.A.; Calabriso, N.; Santarpino, G.; Verri, T.; De Caterina, R. Effects of Olive Oil on Blood Pressure: Epidemiological, Clinical, and Mechanistic Evidence. Nutrients 2020, 12, 1548. [Google Scholar] [CrossRef]
- Massaro, M.; Scoditti, E.; Carluccio, M.A.; De Caterina, R. Nutraceuticals and Prevention of Atherosclerosis: Focus on ω-3 Polyunsaturated Fatty Acids and Mediterranean Diet Polyphenols. Cardiovasc. Ther. 2010, 28, e13–e19. [Google Scholar] [CrossRef]
- Saibandith, B.; Spencer, J.P.E.; Rowland, I.R.; Commane, D.M. Olive Polyphenols and the Metabolic Syndrome. Molecules 2017, 22, 1082. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Chen, H.; Song, Z.; Wang, X.; Sun, Z. Effects of Ginger (Zingiber officinale Roscoe) on Type 2 Diabetes Mellitus and Components of the Metabolic Syndrome: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evidence-Based Complement. Altern. Med. 2018, 2018, 5692962. [Google Scholar] [CrossRef]
- Wang, J.; Ke, W.; Bao, R.; Hu, X.; Chen, F. Beneficial effects of gingerZingiber officinale Roscoeon obesity and metabolic syndrome: A review. Ann. N. Y. Acad. Sci. 2017, 1398, 83–98. [Google Scholar] [CrossRef]
- Mukkavilli, R.; Yang, C.; Singh Tanwar, R.; Ghareeb, A.; Luthra, L.; Aneja, R. Absorption, Metabolic Stability, and Pharmacokinetics of Ginger Phytochemicals. Molecules 2017, 22, 553. [Google Scholar] [CrossRef]
- Li, L.-L.; Cui, Y.; Guo, X.-H.; Ma, K.; Tian, P.; Feng, J.; Wang, J.-M. Pharmacokinetics and Tissue Distribution of Gingerols and Shogaols from Ginger (Zingiber officinale Rosc.) in Rats by UPLC(-)Q-Exactive(-)HRMS. Molecules 2019, 24, 512. [Google Scholar] [CrossRef]
- Ried, K.; Fakler, P.; Stocks, N.P. Effect of cocoa on blood pressure. Cochrane Database Syst. Rev. 2017, 4, CD008893. [Google Scholar] [CrossRef]
- Jumar, A.; Schmieder, R.E. Cocoa Flavanol Cardiovascular Effects Beyond Blood Pressure Reduction. J. Clin. Hypertens. (Greenwich) 2015, 18, 352–358. [Google Scholar] [CrossRef]
- Breuss, J.M.; Atanasov, A.G.; Uhrin, P. Resveratrol and Its Effects on the Vascular System. Int. J. Mol. Sci. 2019, 20, 1523. [Google Scholar] [CrossRef]
- Wiciński, M.; Socha, M.; Walczak, M.; Wódkiewicz, E.; Malinowski, B.; Rewerski, S.; Górski, K.; Pawlak-Osińska, K. Beneficial Effects of Resveratrol Administration—Focus on Potential Biochemical Mechanisms in Cardiovascular Conditions. Nutrients 2018, 10, 1813. [Google Scholar] [CrossRef] [PubMed]
- Imamura, H.; Nagayama, D.; Ishihara, N.; Tanaka, S.; Watanabe, R.; Watanabe, Y.; Sato, Y.; Yamaguchi, T.; Ban, N.; Kawana, H.; et al. Resveratrol attenuates triglyceride accumulation associated with upregulation of Sirt1 and lipoprotein lipase in 3T3-L1 adipocytes. Mol. Genet. Metab. Rep. 2017, 12, 44–50. [Google Scholar] [CrossRef]
- Simental-Mendía, L.E.; Guerrero-Romero, F. Effect of resveratrol supplementation on lipid profile in subjects with dyslipidemia: A randomized double-blind, placebo-controlled trial. Nutrition 2019, 58, 7–10. [Google Scholar] [CrossRef]
- Hamed, M.S.; Gambert, S.; Bliden, K.P.; Bailon, O.; Singla, A.; Antonino, M.J.; Hamed, F.; Tantry, U.S.; Gurbel, P.A. Dark Chocolate Effect on Platelet Activity, C-Reactive Protein and Lipid Profile: A Pilot Study. South. Med. J. 2008, 101, 1203–1208. [Google Scholar] [CrossRef] [PubMed]
- Leyva-Soto, A.; Chavez-Santoscoy, R.A.; Lara-Jacobo, L.R.; Chavez-Santoscoy, A.V.; Gonzalez-Cobian, L.N. Daily Consumption of Chocolate Rich in Flavonoids Decreases Cellular Genotoxicity and Improves Biochemical Parameters of Lipid and Glucose Metabolism. Molecules 2018, 23, 2220. [Google Scholar] [CrossRef]
- Becker, D.J.; Gordon, R.Y.; Halbert, S.C.; French, B.; Morris, P.B.; Rader, D.J. Red yeast rice for dyslipidemia in statin-intolerant patients: a randomized trial. Ann. Intern. Med. 2009, 150, 830–839, W147-839. [Google Scholar] [CrossRef]
- Qin, Y.; Xia, M.; Ma, J.; Hao, Y.; Liu, J.; Mou, H.; Cao, L.; Ling, W. Anthocyanin supplementation improves serum LDL- and HDL-cholesterol concentrations associated with the inhibition of cholesteryl ester transfer protein in dyslipidemic subjects. Am. J. Clin. Nutr. 2009, 90, 485–492. [Google Scholar] [CrossRef]
- Taku, K.; Umegaki, K.; Sato, Y.; Taki, Y.; Endoh, K.; Watanabe, S. Soy isoflavones lower serum total and LDL cholesterol in humans: A meta-analysis of 11 randomized controlled trials. Am. J. Clin. Nutr. 2007, 85, 1148–1156. [Google Scholar] [CrossRef]
- Zhao, Y.; Chen, B.; Shen, J.; Wan, L.; Zhu, Y.; Yi, T.; Xiao, Z. The Beneficial Effects of Quercetin, Curcumin, and Resveratrol in Obesity. Oxidative Med. Cell. Longev. 2017, 2017, 1459497. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.; Tamtaji, O.R.; Lankarani, K.B.; Tabrizi, R.; Dadgostar, E.; Haghighat, N.; Kolahdooz, F.; Ghaderi, A.; Mansournia, M.A.; Asemi, Z. The effects of resveratrol on lipid profiles and liver enzymes in patients with metabolic syndrome and related disorders: A systematic review and meta-analysis of randomized controlled trials. Lipids Health Dis. 2020, 19, 1–12. [Google Scholar] [CrossRef]
- Tokede, O.A.; Gaziano, J.M.; Djoussé, L. Effects of cocoa products/dark chocolate on serum lipids: A meta-analysis. Eur. J. Clin. Nutr. 2011, 65, 879–886. [Google Scholar] [CrossRef] [PubMed]
- Mursu, J.; Voutilainen, S.; Nurmi, T.; Rissanen, T.H.; Virtanen, J.K.; Kaikkonen, J.; Nyyssönen, K.; Salonen, J.T. Dark chocolate consumption increases HDL cholesterol concentration and chocolate fatty acids may inhibit lipid peroxidation in healthy humans. Free. Radic. Biol. Med. 2004, 37, 1351–1359. [Google Scholar] [CrossRef]
- Ali, F.; Ismail, A.; Kersten, S. Molecular mechanisms underlying the potential antiobesity-related diseases effect of cocoa polyphenols. Mol. Nutr. Food Res. 2014, 58, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Juaristi, M.; Sarria, B.; Martínez-López, S.; Bravo Clemente, L.; Mateos, R. Flavanol Bioavailability in Two Cocoa Products with Different Phenolic Content. A Comparative Study in Humans. Nutrients 2019, 11, 1441. [Google Scholar] [CrossRef] [PubMed]
- Schramm, D.D.; Karim, M.; Schrader, H.R.; Holt, R.R.; Kirkpatrick, N.J.; Polagruto, J.A.; Ensunsa, J.L.; Schmitz, H.H.; Keen, C.L. Food effects on the absorption and pharmacokinetics of cocoa flavanols. Life Sci. 2003, 73, 857–869. [Google Scholar] [CrossRef]
- Neilson, A.P.; Sapper, T.N.; Janle, E.M.; Rudolph, R.; Matusheski, N.V.; Ferruzzi, M.G. Chocolate matrix factors modulate the pharmacokinetic behavior of cocoa flavan-3-ol phase II metabolites following oral consumption by Sprague-Dawley rats. J. Agric. Food Chem. 2010, 58, 6685–6691. [Google Scholar] [CrossRef] [PubMed]
- Patel, S. Functional food red yeast rice (RYR) for metabolic syndrome amelioration: A review on pros and cons. World J. Microbiol. Biotechnol. 2016, 32, 87. [Google Scholar] [CrossRef]
- Cicero, A.F.G.; Fogacci, F.; Banach, M. Red Yeast Rice for Hypercholesterolemia. Methodist Debakey Cardiovasc. J. 2019, 15, 192–199. [Google Scholar]
- Zhu, B.; Qi, F.; Wu, J.; Yin, G.; Hua, J.; Zhang, Q.; Qin, L. Red Yeast Rice: A Systematic Review of the Traditional Uses, Chemistry, Pharmacology, and Quality Control of an Important Chinese Folk Medicine. Front. Pharmacol. 2019, 10, 1449. [Google Scholar] [CrossRef]
- Li, Y.; Jiang, L.; Jia, Z.; Xin, W.; Yang, S.; Yang, Q.; Wang, L. A meta-analysis of red yeast rice: an effective and relatively safe alternative approach for dyslipidemia. PLoS ONE 2014, 9, e98611. [Google Scholar] [CrossRef]
- Shamim, S.; Al Badarin, F.J.; DiNicolantonio, J.J.; Lavie, C.J.; O’Keefe, J.H. Red yeast rice for dysipidemia. Mo. Med. 2013, 110, 349–354. [Google Scholar]
- Chen, C.H.; Yang, J.C.; Uang, Y.S.; Lin, C.J. Improved dissolution rate and oral bioavailability of lovastatin in red yeast rice products. Int. J. Pharm. 2013, 444, 18–24. [Google Scholar] [CrossRef]
- Chan, S.W.; Tomlinson, B. Effects of Bilberry Supplementation on Metabolic and Cardiovascular Disease Risk. Molecules 2020, 25, 1653. [Google Scholar] [CrossRef] [PubMed]
- Zhan, S.; Ho, S.C. Meta-analysis of the effects of soy protein containing isoflavones on the lipid profile. Am. J. Clin. Nutr. 2005, 81, 397–408. [Google Scholar] [CrossRef] [PubMed]
- Hermansen, K.; Dinesen, B.; Hoie, L.H.; Morgenstern, E.; Gruenwald, J. Effects of soy and other natural products on LDL:HDL ratio and other lipid parameters: A literature review. Adv. Ther. 2003, 20, 50–78. [Google Scholar] [CrossRef] [PubMed]
- Ricketts, M.L.; Moore, D.D.; Banz, W.J.; Mezei, O.; Shay, N.F. Molecular mechanisms of action of the soy isoflavones includes activation of promiscuous nuclear receptors. A review. J. Nutr. Biochem. 2005, 16, 321–330. [Google Scholar] [CrossRef]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, e34. [Google Scholar] [CrossRef] [PubMed]
- Riboli, E.; Hunt, K.J.; Slimani, N.; Ferrari, P.; Norat, T.; Fahey, M.; Charrondiere, U.R.; Hemon, B.; Casagrande, C.; Vignat, J.; et al. European Prospective Investigation into Cancer and Nutrition (EPIC): Study populations and data collection. Public Health Nutr. 2002, 5, 1113–1124. [Google Scholar] [CrossRef] [PubMed]
- Romani, A.; Bernini, R.; Noce, A.; Urciuoli, S.; Di Lauro, M.; Pietroboni Zaitseva, A.; Marrone, G.; Di Daniele, N. Potential Beneficial Effects of Extra Virgin Olive Oils Characterized by High Content in Minor Polar Compounds in Nephropathic Patients: A Pilot Study. Molecules 2020, 25, 4757. [Google Scholar] [CrossRef]
- Bayram, B.; Ozcelik, B.; Grimm, S.; Roeder, T.; Schrader, C.; Ernst, I.M.; Wagner, A.E.; Grune, T.; Frank, J.; Rimbach, G. AA diet rich in olive oil phenolics reduces oxidative stress in the heart of SAMP8 mice by induction of Nrf2-dependent gene expression. Rejuvenation Res. 2012, 15, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Fuccelli, R.; Fabiani, R.; Rosignoli, P. Hydroxytyrosol Exerts Anti-Inflammatory and Anti-Oxidant Activities in a Mouse Model of Systemic Inflammation. Molecules 2018, 23, 3212. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Cao, J.; Zhong, L. Hydroxytyrosol inhibits pro-inflammatory cytokines, iNOS, and COX-2 expression in human monocytic cells. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2009, 379, 581–586. [Google Scholar] [CrossRef]
- Scotece, M.; Gómez, R.; Conde, J.; Lopez, V.; Gomez-Reino, J.J.; Lago, F.; Smith, A.B., 3rd; Gualillo, O. Further evidence for the anti-inflammatory activity of oleocanthal: Inhibition of MIP-1α and IL-6 in J774 macrophages and in ATDC5 chondrocytes. Life Sci. 2012, 91, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Carpi, S.; Scoditti, E.; Massaro, M.; Polini, B.; Manera, C.; Digiacomo, M.; Esposito Salsano, J.; Poli, G.; Tuccinardi, T.; Doccini, S.; et al. The Extra-Virgin Olive Oil Polyphenols Oleocanthal and Oleacein Counteract Inflammation-Related Gene and miRNA Expression in Adipocytes by Attenuating NF-κB Activation. Nutrients 2019, 11, 2855. [Google Scholar] [CrossRef]
- Askari, G.; Ghiasvand, R.; Feizi, A.; Ghanadian, S.M.; Karimian, J. The effect of quercetin supplementation on selected markers of inflammation and oxidative stress. J. Res. Med. Sci. 2012, 17, 637–641. [Google Scholar] [PubMed]
- Carlsen, I.; Frøkiær, J.; Nørregaard, R. Quercetin attenuates cyclooxygenase-2 expression in response to acute ureteral obstruction. Am. J. Physiol. Renal. Physiol. 2015, 308, F1297–F1305. [Google Scholar] [CrossRef]
- Rivera, L.; Morón, R.; Sánchez, M.; Zarzuelo, A.; Galisteo, M. Quercetin Ameliorates Metabolic Syndrome and Improves the Inflammatory Status in Obese Zucker Rats. Obes. 2008, 16, 2081–2087. [Google Scholar] [CrossRef]
- Tomé-Carneiro, J.; Larrosa, M.; Yáñez-Gascón, M.J.; Dávalos, A.; Gil-Zamorano, J.; Gonzálvez, M.; García-Almagro, F.J.; Ros, J.A.R.; Tomás-Barberán, F.A.; Espín, J.C.; et al. One-year supplementation with a grape extract containing resveratrol modulates inflammatory-related microRNAs and cytokines expression in peripheral blood mononuclear cells of type 2 diabetes and hypertensive patients with coronary artery disease. Pharmacol. Res. 2013, 72, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Arbeláez, D.; Lahera, V.; Oubiña, P.; Valero-Muñoz, M.; Heras, N.D.L.; Rodríguez, Y.; García, R.G.; Camacho, P.A.; López-Jaramillo, P. Aged garlic extract improves adiponectin levels in subjects with metabolic syndrome: A double-blind, placebo-controlled, randomized, crossover study. Mediat. Inflamm. 2013, 2013, 285795. [Google Scholar] [CrossRef]
- Parkinson, L.; Cicerale, S. The Health Benefiting Mechanisms of Virgin Olive Oil Phenolic Compounds. Molecules 2016, 21, 1734. [Google Scholar] [CrossRef]
- Noce, A.; Marrone, G.; Urciuoli, S.; Di Daniele, F.; Di Lauro, M.; Pietroboni Zaitseva, A.; Di Daniele, N.; Romani, A. Usefulness of Extra Virgin Olive Oil Minor Polar Compounds in the Management of Chronic Kidney Disease Patients. Nutrients 2021, 13, 581. [Google Scholar] [CrossRef]
- Karkovic Markovic, A.; Toric, J.; Barbaric, M.; Jakobusic Brala, C. Hydroxytyrosol, Tyrosol and Derivatives and Their Potential Effects on Human Health. Molecules 2019, 24, 2001. [Google Scholar] [CrossRef]
- Alemán-Jiménez, C.; Domínguez-Perles, R.; Medina, S.; Prgomet, I.; López-González, I.; Simonelli-Muñoz, A.; Campillo-Cano, M.; Auñón, D.; Ferreres, F.; Gil-Izquierdo, A. Pharmacokinetics and bioavailability of hydroxytyrosol are dependent on the food matrix in humans. Eur. J. Nutr. 2020, 1–11. [Google Scholar] [CrossRef]
- Robles-Almazan, M.; Pulido-Moran, M.; Moreno-Fernandez, J.; Ramirez-Tortosa, C.; Rodriguez-Garcia, C.; Quiles, J.L.; Ramirez-Tortosa, M. Hydroxytyrosol: Bioavailability, toxicity, and clinical applications. Food Res. Int. 2018, 105, 654–667. [Google Scholar] [CrossRef] [PubMed]
- Romani, A.; Ieri, F.; Urciuoli, S.; Noce, A.; Marrone, G.; Nediani, C.; Bernini, R. Health Effects of Phenolic Compounds Found in Extra-Virgin Olive Oil, By-Products, and Leaf of Olea europaea L. Nutrients 2019, 11, 1776. [Google Scholar] [CrossRef]
- López-Yerena, A.; Vallverdú-Queralt, A.; Mols, R.; Augustijns, P.; Lamuela-Raventós, R.M.; Escribano-Ferrer, E. Absorption and Intestinal Metabolic Profile of Oleocanthal in Rats. Pharm. 2020, 12, 134. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Villalba, R.; Carrasco-Pancorbo, A.; Nevedomskaya, E.; Mayboroda, O.A.; Deelder, A.M.; Segura-Carretero, A.; Fernández-Gutiérrez, A. Exploratory analysis of human urine by LC–ESI-TOF MS after high intake of olive oil: Understanding the metabolism of polyphenols. Anal. Bioanal. Chem. 2010, 398, 463–475. [Google Scholar] [CrossRef]
- Li, Y.; Yao, J.; Han, C.; Yang, J.; Chaudhry, M.T.; Wang, S.; Liu, H.; Yin, Y. Quercetin, Inflammation and Immunity. Nutrients 2016, 8, 167. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Hu, M.-J.; Wang, Y.-Q.; Cui, Y.-L. Antioxidant Activities of Quercetin and Its Complexes for Medicinal Application. Molecules 2019, 24, 1123. [Google Scholar] [CrossRef]
- Sato, S.; Mukai, Y. Modulation of Chronic Inflammation by Quercetin: The Beneficial Effects on Obesity. J. Inflamm. Res. 2020, 13, 421–431. [Google Scholar] [CrossRef] [PubMed]
- Chaplin, A.; Carpéné, C.; Mercader, J. Resveratrol, Metabolic Syndrome, and Gut Microbiota. Nutrients 2018, 10, 1651. [Google Scholar] [CrossRef]
- Arreola, R.; Quintero-Fabián, S.; López-Roa, R.I.; Flores-Gutiérrez, E.O.; Reyes-Grajeda, J.P.; Carrera-Quintanar, L.; Ortuño-Sahagún, D. Immunomodulation and Anti-Inflammatory Effects of Garlic Compounds. J. Immunol. Res. 2015, 2015, 401630. [Google Scholar] [CrossRef] [PubMed]
- Lawson, L.D.; Hunsaker, S.M. Allicin Bioavailability and Bioequivalence from Garlic Supplements and Garlic Foods. Nutrients 2018, 10, 812. [Google Scholar] [CrossRef]
- Rinninella, E.; Raoul, P.; Cintoni, M.; Franceschi, F.; Miggiano, G.A.D.; Gasbarrini, A.; Mele, M.C. What is the Healthy Gut Microbiota Composition? A Changing Ecosystem across Age, Environment, Diet, and Diseases. Microorganisms 2019, 7, 14. [Google Scholar] [CrossRef]
- Arumugam, M.; Raes, J.; Pelletier, E.; Le Paslier, D.; Yamada, T.; Mende, D.R.; Fernandes, G.R.; Tap, J.; Bruls, T.; Batto, J.M.; et al. Enterotypes of the human gut microbiome. Nature 2011, 473, 174–180. [Google Scholar] [CrossRef]
- De Filippo, C.; Cavalieri, D.; Di Paola, M.; Ramazzotti, M.; Poullet, J.B.; Massart, S.; Collini, S.; Pieraccini, G.; Lionetti, P. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. USA 2010, 107, 14691–14696. [Google Scholar] [CrossRef]
- Conlon, M.A.; Bird, A.R. The impact of diet and lifestyle on gut microbiota and human health. Nutrients 2015, 7, 17–44. [Google Scholar] [CrossRef]
- Krishnan, S.; Alden, N.; Lee, K. Pathways and functions of gut microbiota metabolism impacting host physiology. Curr. Opin. Biotechnol. 2015, 36, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.X.; Deng, X.R.; Zhang, C.H.; Yuan, H.J. Gut microbiota and metabolic syndrome. Chin. Med. J. (Engl.) 2020, 133, 808–816. [Google Scholar] [CrossRef]
- Annalisa, N.; Alessio, T.; Claudette, T.D.; Erald, V.; de Antonino, L.; Nicola, D.D. Gut Microbioma Population: An Indicator Really Sensible to Any Change in Age, Diet, Metabolic Syndrome, and Life-Style. Mediat. Inflamm. 2014, 2014, 901308. [Google Scholar] [CrossRef] [PubMed]
- Kinger, M.; Kumar, S.; Kumar, V. Some Important Dietary Polyphenolic Compounds: An Anti-inflammatory and Immunoregulatory Perspective. Mini-Reviews Med. Chem. 2018, 18, 1270–1282. [Google Scholar] [CrossRef]
- Sharma, U.K.; Sharma, A.K.; Pandey, A.K. Medicinal attributes of major phenylpropanoids present in cinnamon. BMC Complement. Altern. Med. 2016, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Landete, J.M. Updated Knowledge about Polyphenols: Functions, Bioavailability, Metabolism, and Health. Crit. Rev. Food Sci. Nutr. 2012, 52, 936–948. [Google Scholar] [CrossRef]
- Han, X.; Shen, T.; Lou, H. Dietary Polyphenols and Their Biological Significance. Int. J. Mol. Sci. 2007, 8, 950–988. [Google Scholar] [CrossRef]
- Appeldoorn, M.M.; Vincken, J.-P.; Gruppen, H.; Hollman, P.C. Procyanidin dimers A1, A2, and B2 are absorbed without conjugation or methylation from the small intestine of rats. J. Nutr. 2009, 139, 1469–1473. [Google Scholar] [CrossRef] [PubMed]
- Kawabata, K.; Yoshioka, Y.; Terao, J. Role of Intestinal Microbiota in the Bioavailability and Physiological Functions of Dietary Polyphenols. Molecules 2019, 24, 370. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.; Jenner, A.M.; Low, C.S.; Lee, Y.K. Effect of tea phenolics and their aromatic fecal bacterial metabolites on intestinal microbiota. Res. Microbiol. 2006, 157, 876–884. [Google Scholar] [CrossRef]
- Kumar Singh, A.; Cabral, C.; Kumar, R.; Ganguly, R.; Kumar Rana, H.; Gupta, A.; Lauro, M.R.; Carbone, C.; Reis, F.; Pandey, A.K. Beneficial Effects of Dietary Polyphenols on Gut Microbiota and Strategies to Improve Delivery Efficiency. Nutrients 2019, 11, 2216. [Google Scholar] [CrossRef] [PubMed]
- Monagas, M.; Khan, N.; Andres-Lacueva, C.; Urpi-Sarda, M.; Vázquez-Agell, M.; Lamuela-Raventos, R.M.; Estruch, R. Dihydroxylated phenolic acids derived from microbial metabolism reduce lipopolysaccharide-stimulated cytokine secretion by human peripheral blood mononuclear cells. Br. J. Nutr. 2009, 102, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Rastmanesh, R. High polyphenol, low probiotic diet for weight loss because of intestinal microbiota interaction. Chem. Biol. Interactions 2011, 189, 1–8. [Google Scholar] [CrossRef]
- Zanzer, Y.C.; Plaza, M.; Dougkas, A.; Turner, C.; Björck, I.; Östman, E. Polyphenol-rich spice-based beverages modulated postprandial early glycaemia, appetite and PYY after breakfast challenge in healthy subjects: A randomized, single blind, crossover study. J. Funct. Foods 2017, 35, 574–583. [Google Scholar] [CrossRef]
- Gill, P.A.; Van Zelm, M.C.; Muir, J.G.; Gibson, P.R. Review article: Short chain fatty acids as potential therapeutic agents in human gastrointestinal and inflammatory disorders. Aliment. Pharmacol. Ther. 2018, 48, 15–34. [Google Scholar] [CrossRef] [PubMed]
- Vamanu, E.; Gatea, F.; Sârbu, I.; Pelinescu, D. An In Vitro Study of the Influence of Curcuma longa Extracts on the Microbiota Modulation Process, In Patients with Hypertension. Pharm. 2019, 11, 191. [Google Scholar] [CrossRef] [PubMed]
- Smirnov, A.; Panatta, E.; Lena, A.; Castiglia, D.; Di Daniele, N.; Melino, G.; Candi, E. FOXM1 regulates proliferation, senescence and oxidative stress in keratinocytes and cancer cells. Aging (Albany NY) 2016, 8, 1384–1397. [Google Scholar] [CrossRef] [PubMed]
- Sinagra, E.; Tomasello, G.; Raimondo, D.; Rossi, F.; Facella, T.; Cappello, F.; Damiani, P.; Abruzzo, A.; Bruno, A.; Palumbo, V.; et al. Nutrition, malnutrition and dietary interventions in inflammatory bowel disease. Progr. Nutr. 2014, 16, 79–89. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).