Vitamin K and D Supplementation and Bone Health in Chronic Kidney Disease—Apart or Together?
Abstract
1. Introduction
2. Vitamin D and Vitamin K in CKD
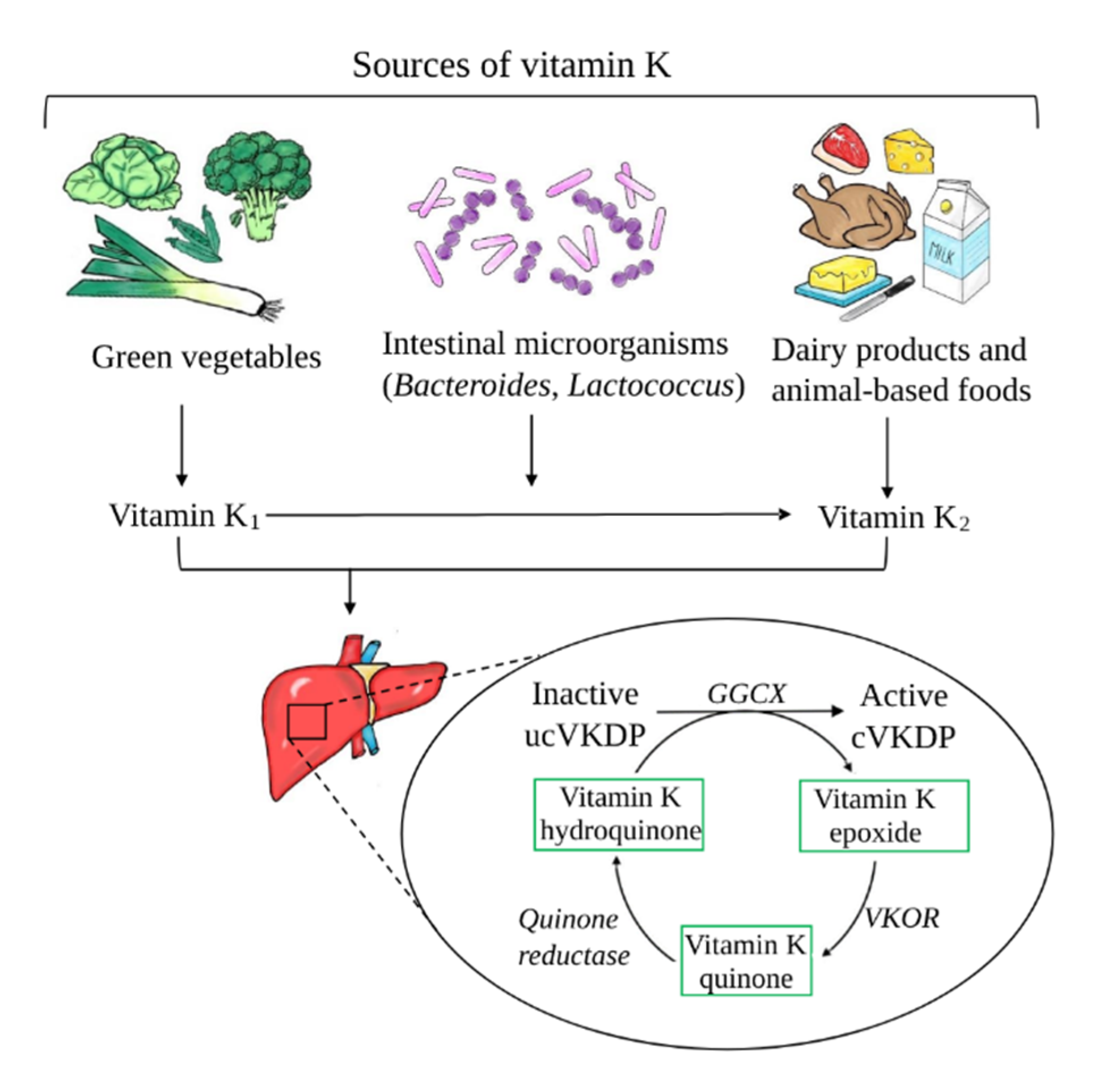
2.1. General Characteristics of Vitamin K—Chemical Structure, Metabolism, and Laboratory Evaluation
2.2. Vitamin K Status in CKD Patients
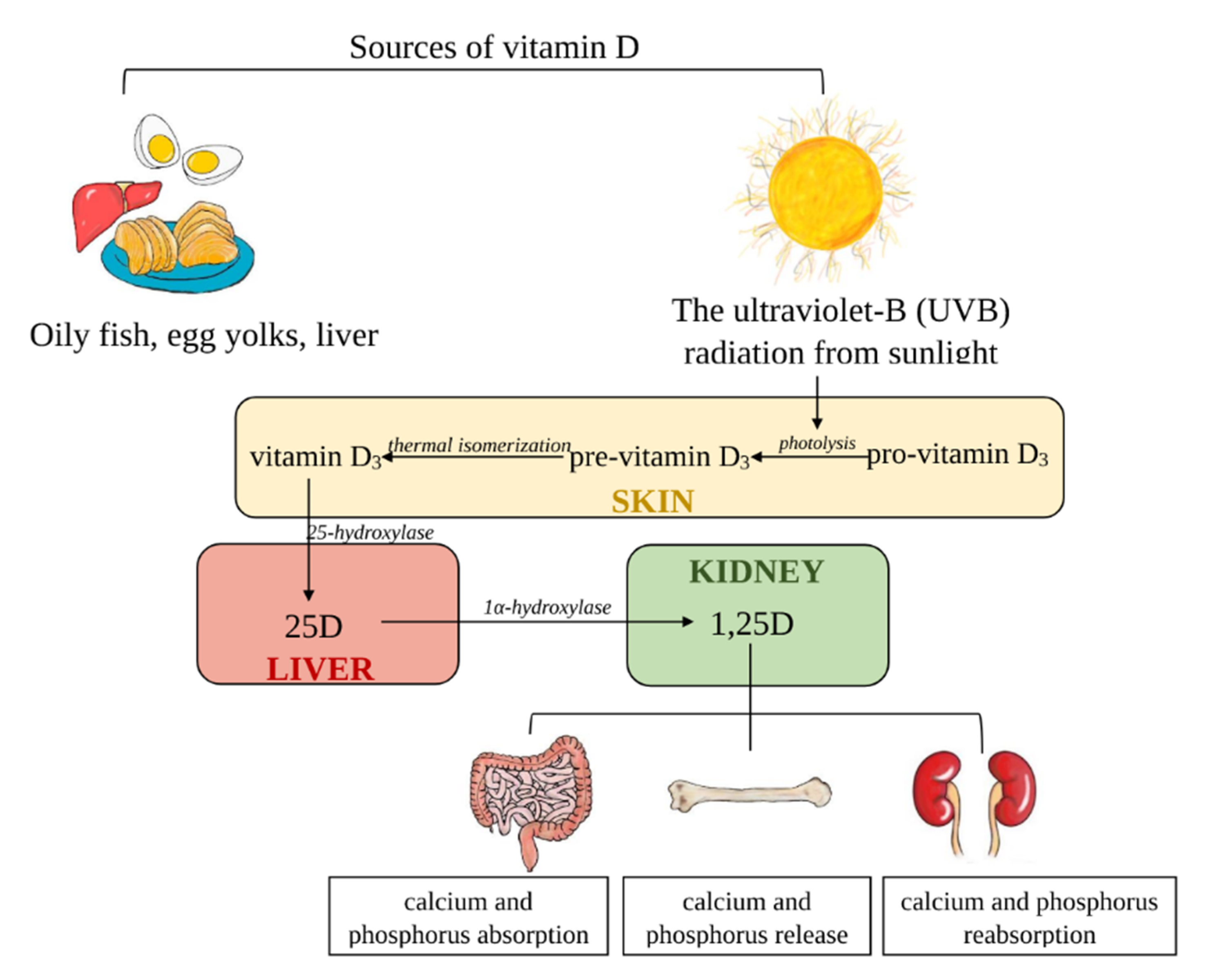
2.3. General Characteristics of Vitamin D
2.4. Vitamin D Deficiency in CKD Patients
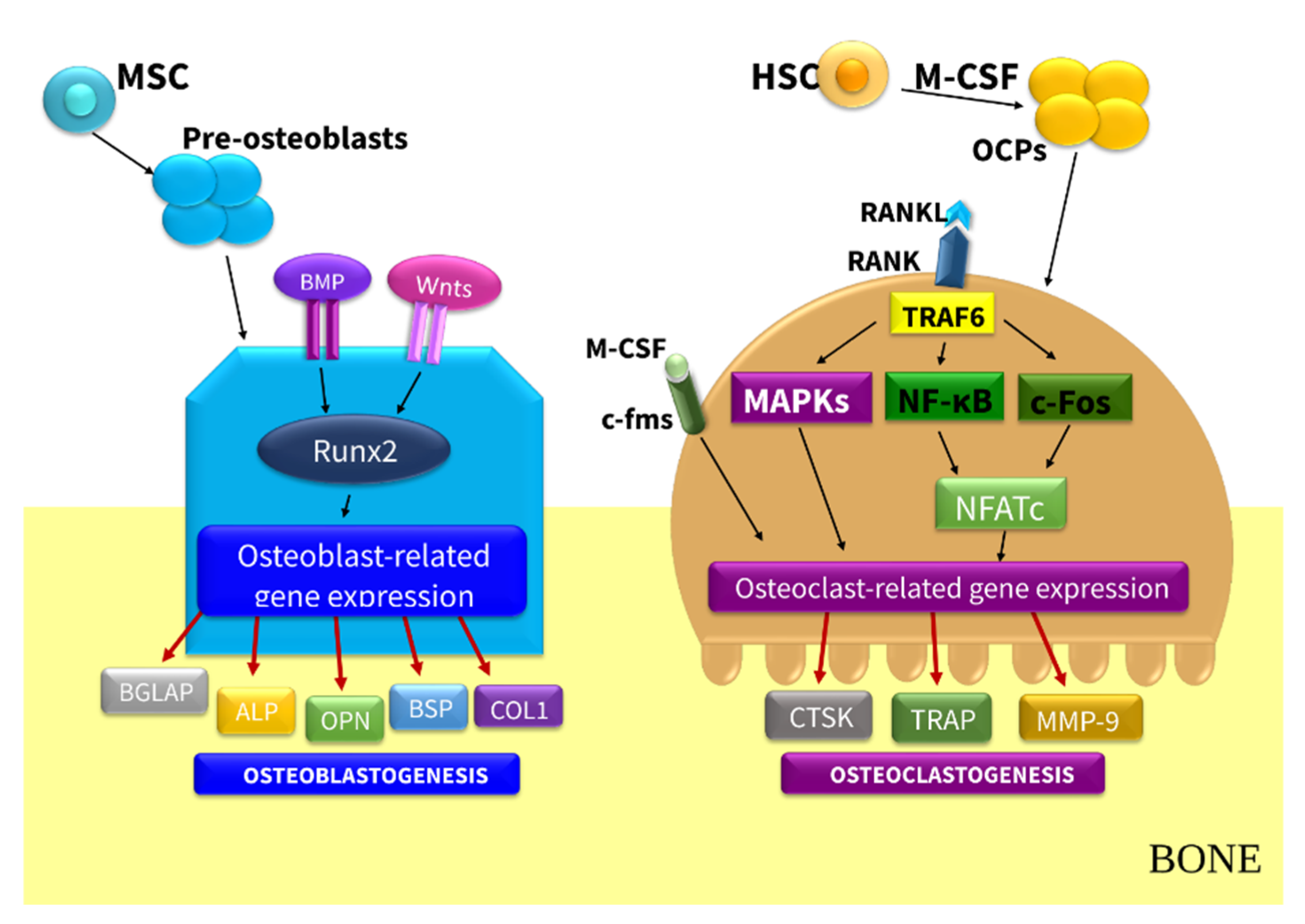
3. Role of Vitamin K and Vitamin D in Bone Remodeling in CKD: Pre-Clinical Evidence
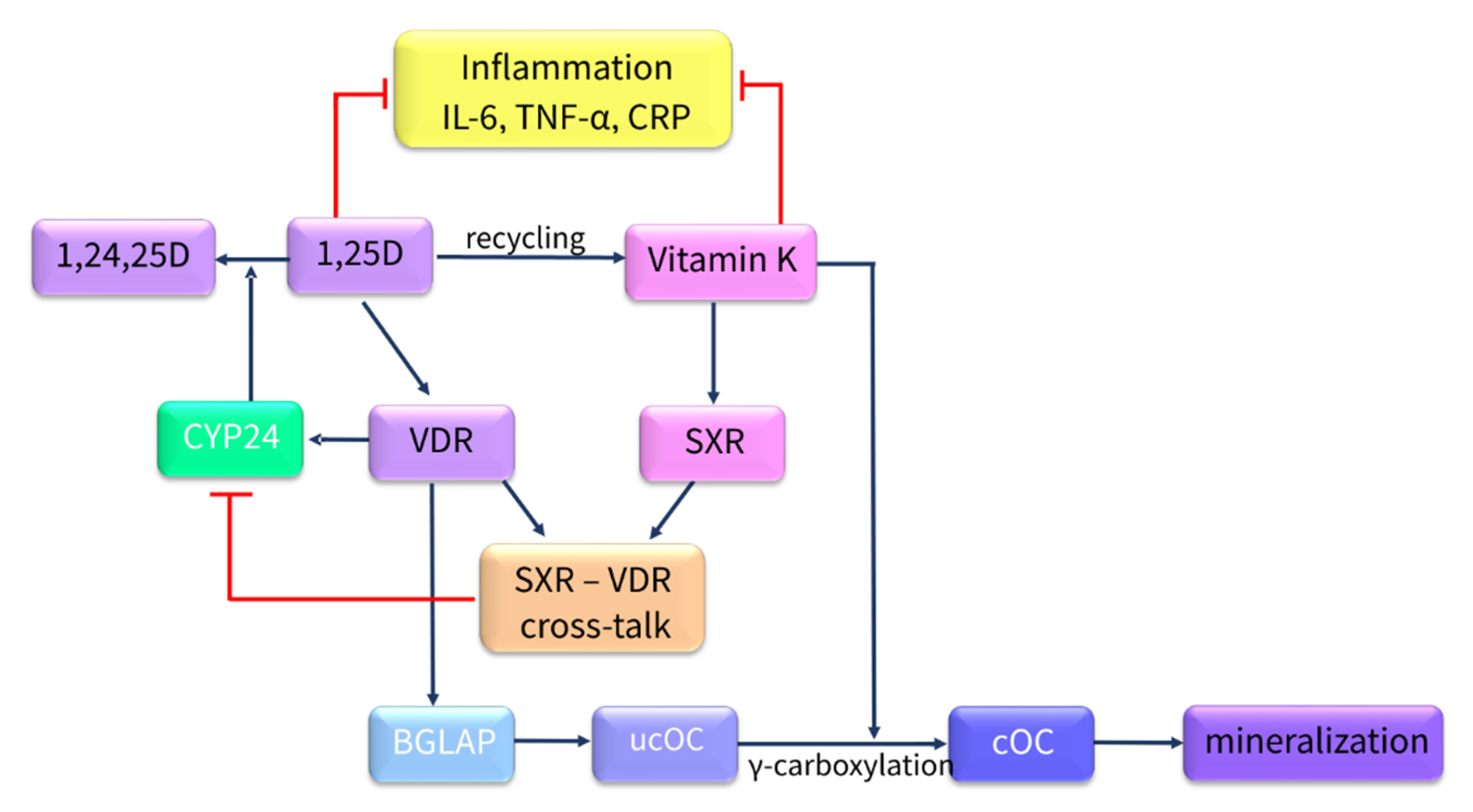
3.1. Vitamin K and Bone Remodeling—In Vitro Studies
3.2. Vitamin D and Bone Remodeling—In Vitro Studies
3.2.1. Impact of 1,25D on Osteoblast Function
3.2.2. Effect of 1,25D on hOBs and hMSCs
3.2.3. Effect of 1,25D on hOCs and Human Peripheral Blood Mononuclear Cells (hPBMCs)
4. Vitamin K and Vitamin D in Bone Remodeling—In Vivo Studies
4.1. Vitamin K and Bone Remodeling—In Vivo Animal Models
4.2. Vitamin D and Bone Remodeling—In Vivo CKD Animal Models
5. Vitamin K, Vitamin D, and Bone Health in Patients with CKD—Clinical Evidence
5.1. The Impact of Vitamin K on Bone Health in Patients with CKD
5.2. Impact of Vitamin D on Bone Health in Patients with CKD
6. Impact of Combined Vitamin K and Vitamin D Supplementation on Bone Health in Patients with CKD
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 1,25D | 1,25-dihydroxyvitamin D |
| 25D | 25-hydroxyvitamin D |
| ALP | alkaline phosphatase |
| ApoE4 | apolipoprotein E4 |
| BGLAP | bone-Gla-protein; osteocalcin |
| BMD | bone mineral density |
| BMP-2 | bone morphogenetic protein-2 |
| BMP-7 | bone morphogenic protein-7 |
| BW | body weight |
| CKD | chronic kidney disease |
| CKD-MBD | chronic kidney disease–mineral bone disorders |
| CLIA | chemiluminescent immunoassay |
| cOC | carboxylated osteocalcin |
| COL1A1 | collagen type I |
| CYP2R1 | 25-hydroxylase; cytochrome P450 family 2 subfamily R member 1 |
| CYP24A1 | cytochrome P450 family 24 subfamily A member 1 |
| CYP27B1 | 1α-hydroxylase; cytochrome P450 family 27 subfamily B member 1 |
| DCKD | diabetes chronic kidney disease |
| DECALYOS II | Vitamin D, Calcium, Lyon Study II |
| DKK1 | Dickkopf-related protein 1 |
| dp-ucMGP | desphospho-uncarboxylated matrix Gla protein |
| DXA | dual X-ray absorptiometry |
| ECM | extracellular matrix |
| ELISA | enzyme-linked immunosorbent assay |
| ESRD | end-stage renal disease |
| FGF-23 | fibroblast growth factor 23 |
| Gas6 | growth arrest specific protein 6 |
| GGCX | γ-glutamyl carboxylase |
| Gla | gamma carboxyglutamic acid |
| Glu | glutamic acid |
| GRP | Gla-rich protein |
| HD | hemodialysis |
| hMSCs | human bone marrow stromal cells |
| hOBs | human OBs |
| hOCs | human OCs |
| hPBMCs | human peripheral blood mononuclear cells |
| HPLC | high-performance liquid chromatography |
| IBSP | integrin-binding sialoprotein |
| IGFBPs | insulin-like growth factor-binding proteins |
| IL1α | interleukin 1α |
| KDIGO | Kidney Disease Improvement Global Outcomes |
| KDOQI | Kidney Disease Outcomes Quality Initiative |
| LC-MS/MS | liquid chromatography-tandem mass spectrometry |
| LRP5 | low-density lipoprotein receptor-related protein 5 |
| m-CSF | colony-stimulating factor |
| MKs | menaquinones |
| NFATC1 | nuclear factor of activated T cells-c1 |
| NF-κB | nuclear factor kappa-light-chain-enhancer of activated B cells |
| NR1I2 | nuclear receptor subfamily 1 group I member 2 |
| NTx | N-terminal telopeptide |
| OBs | osteoblasts |
| OCs | osteoclasts |
| OPG | osteoprotegerin |
| OSX | osterix |
| OVX | ovariectomized |
| PD | peritoneal dialysis |
| PGE2 | prostaglandin E2 |
| PIVKA-II | protein induced by VK absence/antagonism II |
| PTH | parathyroid hormone |
| PXR | pregnane X receptor |
| RANKL | Receptor Activator for Nuclear Factor κ B Ligand |
| RIA | radioimmunoassay |
| RUNX2 | Runt-related transcription factor 2 |
| SMAD | small mother against decapentaplegic |
| SPP1 | osteopontin |
| SXR | steroid and xenobiotic receptor |
| TM7SF4 | transmembrane 7 superfamily member 4 |
| TNFα | tumor necrosis factor α |
| TRAP | tartrate-resistant acid phosphatase |
| TRPV6 | Transient Receptor Potential Cation Channel Subfamily V Member 6 |
| UBIAD1 | UbiA prenyltransferase domain-containing protein |
| ucOC | uncarboxylated osteocalcin |
| UV | ultraviolet |
| VC | vascular calcification |
| VD | vitamin D |
| VDBP | VD binding protein |
| VDR | VD receptor |
| VEGF | Vascular endothelial growth factor |
| VK | vitamin K |
| VK1 | vitamin K1 |
| VK2 | vitamin K2 |
| VKDPs | VK-dependent proteins |
| VKOR | VK epoxide reductase |
| Wnt | Wingless-type |
| Wnt-10b | Wnt ligand 10b |
References
- Banerjee, D.; Jha, V. Vitamin D and cardiovascular complications of CKD: What’s next? Clin. J. Am. Soc. Nephrol. 2019, 14, 932–934. [Google Scholar] [CrossRef] [PubMed]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int. Suppl. 2017, 7, 1–59. [Google Scholar] [CrossRef] [PubMed]
- Holden, R.M.; Morton, A.R.; Garland, J.S.; Pavlov, A.; Day, A.G.; Booth, S.L. Vitamins K and D Status in Stages 3–5 Chronic Kidney Disease. Clin. J. Am. Soc. Nephrol. 2010, 5, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Garland, J.S.; Holden, R.M.; Groome, P.A.; Lam, M.; Nolan, R.L.; Morton, A.R.; Pickett, W. Prevalence and Associations of Coronary Artery Calcification in Patients With Stages 3 to 5 CKD Without Cardiovascular Disease. Am. J. Kidney Dis. 2008, 52, 849–858. [Google Scholar] [CrossRef] [PubMed]
- Florencio-Silva, R.; Sasso, G.R.d.S.; Sasso-Cerri, E.; Simões, M.J.; Cerri, P.S. Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. BioMed Res. Int. 2015, 2015, 421746. [Google Scholar] [CrossRef] [PubMed]
- Katsimbri, P. The biology of normal bone remodelling. Eur. J. Cancer Care 2017, 26, e12740. [Google Scholar] [CrossRef] [PubMed]
- Jadoul, M.; Albert, J.; Akiba, T.; Akizawa, T.; Arab, L.; Bragggresham, J.L.; A Mason, N.; Prutz, K.-G.; Young, E.W.; Pisoni, R.L. Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2006, 70, 1358–1366. [Google Scholar] [CrossRef] [PubMed]
- Pimentel, A.; Ureña-Torres, P.; Zillikens, M.C.; Bover, J.; Cohen-Solal, M. Fractures in patients with CKD—diagnosis, treatment, and prevention: A review by members of the European Calcified Tissue Society and the European Renal Association of Nephrology Dialysis and Transplantation. Kidney Int. 2017, 92, 1343–1355. [Google Scholar] [CrossRef]
- Ureña, P.; Bernard-Poenaru, O.; Ostertag, A.; Baudoin, C.; Cohen-Solal, M.; Cantor, T.; De Vernejoul, M.C. Bone mineral density, biochemical markers and skeletal fractures in haemodialysis patients. Nephrol. Dial. Transplant. 2003, 18, 2325–2331. [Google Scholar] [CrossRef]
- Elliott, M.J.; Booth, S.L.; Hopman, W.M.; Holden, R.M. Assessment of Potential Biomarkers of Subclinical Vitamin K Deficiency in Patients with End-Stage Kidney Disease. Can. J. Kidney Health Dis. 2014, 1, 13. [Google Scholar] [CrossRef]
- Holden, R.M.; Iliescu, E.; Morton, A.R.; Booth, S.L. Vitamin K Status of Canadian Peritoneal Dialysis Patients. Perit. Dial. Int. 2008, 28, 415–418. [Google Scholar] [CrossRef] [PubMed]
- Jean, G.; Souberbielle, J.C.; Chazot, C. Vitamin D in Chronic Kidney Disease and Dialysis Patients. Nutrients 2017, 9, 328. [Google Scholar] [CrossRef]
- Gois, P.H.F.; Wolley, M.; Ranganathan, D.; Seguro, A.C. Vitamin D Deficiency in Chronic Kidney Disease: Recent Evidence and Controversies. Int. J. Environ. Res. Public Health 2018, 15, 1773. [Google Scholar] [CrossRef]
- Caravaca-Fontán, F.; Gonzales-Candia, B.; Luna, E.; Caravaca, F. Relative importance of the determinants of serum levels of 25-hydroxy vitamin D in patients with chronic kidney disease. Nefrología 2016, 36, 510–516. [Google Scholar] [CrossRef]
- Melamed, M.L.; Thadhani, R.I. Vitamin D Therapy in Chronic Kidney Disease and End Stage Renal Disease. Clin. J. Am. Soc. Nephrol. 2011, 7, 358–365. [Google Scholar] [CrossRef]
- Thrailkill, K.M.; Jo, C.-H.; Cockrell, G.E.; Moreau, C.S.; Fowlkes, J.L. Enhanced Excretion of Vitamin D Binding Protein in Type 1 Diabetes: A Role in Vitamin D Deficiency? J. Clin. Endocrinol. Metab. 2011, 96, 142–149. [Google Scholar] [CrossRef]
- Tian, X.-Q.; Zhao, L.-M.; Ge, J.-P.; Zhang, Y.; Xu, Y.-C. Elevated urinary level of vitamin D-binding protein as a novel biomarker for diabetic nephropathy. Exp. Ther. Med. 2013, 7, 411–416. [Google Scholar] [CrossRef]
- Shah, N.; Bernardini, J.; Piraino, B. Prevalence and Correction of 25(OH) Vitamin D Deficiency in Peritoneal Dialysis Patients. Perit. Dial. Int. 2005, 25, 362–366. [Google Scholar] [CrossRef] [PubMed]
- McCabe, K.M.; Booth, S.L.; Fu, X.; Ward, E.; Adams, M.A.; Holden, R.M. Vitamin K Metabolism in a Rat Model of Chronic Kidney Disease. Am. J. Nephrol. 2017, 45, 4–13. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, R.B.; Stinghen, A.E.M.; Massy, Z.A. Vitamin K role in mineral and bone disorder of chronic kidney disease. Clin. Chim. Acta 2020, 502, 66–72. [Google Scholar] [CrossRef]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef]
- Ennis, J.L.; Worcester, E.M.; Coe, F.L.; Sprague, S.M. Current recommended 25-hydroxyvitamin D targets for chronic kidney disease management may be too low. J. Nephrol. 2015, 29, 63–70. [Google Scholar] [CrossRef]
- Cranenburg, E.C.M.; Schurgers, L.J.; Uiterwijk, H.H.; Beulens, J.W.; Dalmeijer, G.W.; Westerhuis, R.; Magdeleyns, E.J.; Herfs, M.; Vermeer, C.; Laverman, G.D. Vitamin K intake and status are low in hemodialysis patients. Kidney Int. 2012, 82, 605–610. [Google Scholar] [CrossRef]
- Booth, S.L. Vitamin K: Food composition and dietary intakes. Food Nutr. Res. 2012, 56, 5505. [Google Scholar] [CrossRef]
- Thijssen, H.H.W.; Drittij-Reijnders, M.J. Vitamin K distribution in rat tissues: Dietary phylloquinone is a source of tissue menaquinone-4. Br. J. Nutr. 1994, 72, 415–425. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, K.; Hirota, Y.; Sawada, N.; Yuge, N.; Watanabe, M.; Uchino, Y.; Okuda, N.; Shimomura, Y.; Suhara, Y.; Okano, T. Identification of UBIAD1 as a novel human menaquinone-4 biosynthetic enzyme. Nat. Cell Biol. 2010, 468, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Silaghi, C.N.; Ilyés, T.; Filip, V.P.; Farcaș, M.; Van Ballegooijen, A.J.; Crăciun, A.M. Vitamin K Dependent Proteins in Kidney Disease. Int. J. Mol. Sci. 2019, 20, 1571. [Google Scholar] [CrossRef]
- Tabb, M.M.; Sun, A.; Zhou, C.; Grün, F.; Errandi, J.; Romero, K.; Pham, H.; Inoue, S.; Mallick, S.; Lin, M.; et al. Vitamin K2 Regulation of Bone Homeostasis Is Mediated by the Steroid and Xenobiotic Receptor SXR. J. Biol. Chem. 2003, 278, 43919–43927. [Google Scholar] [CrossRef]
- Ichikawa, T.; Horie-Inoue, K.; Ikeda, K.; Blumberg, B.; Inoue, S. Steroid and Xenobiotic Receptor SXR Mediates Vitamin K2-activated Transcription of Extracellular Matrix-related Genes and Collagen Accumulation in Osteoblastic Cells. J. Biol. Chem. 2006, 281, 16927–16934. [Google Scholar] [CrossRef]
- Booth, S.L.; Pennington, J.A.; Sadowski, J.A. Food sources and dietary intakes of vitamin K-1 (phylloquinone) in the American diet: Data from the FDA Total Diet Study. J. Am. Diet. Assoc. 1996, 96, 149–154. [Google Scholar] [CrossRef]
- Schurgers, L.J.; Vermeer, C. Determination of phylloquinone and menaquinones in food. Effect of food matrix on circulating vitamin K concentrations. Haemostasis 2000, 30, 298–307. [Google Scholar]
- Schurgers, L.J.; Vermeer, C. Differential lipoprotein transport pathways of K-vitamins in healthy subjects. Biochim. Biophys. Acta BBA Gen. Subj. 2002, 1570, 27–32. [Google Scholar] [CrossRef]
- Akbari, S.; Rasouli-Ghahroudi, A.A. Vitamin K and Bone Metabolism: A Review of the Latest Evidence in Preclinical Studies. BioMed Res. Int. 2018, 2018, 1–8. [Google Scholar] [CrossRef]
- Tie, J.-K.; Stafford, D.W. Structural and functional insights into enzymes of the vitamin K cycle. J. Thromb. Haemost. 2016, 14, 236–247. [Google Scholar] [CrossRef]
- Paroni, R.; Faioni, E.M.; Razzari, C.; Fontana, G.; Cattaneo, M. Determination of vitamin K1 in plasma by solid phase extraction and HPLC with fluorescence detection. J. Chromatogr. B 2009, 877, 351–354. [Google Scholar] [CrossRef] [PubMed]
- Caluwé, R.; Verbeke, F.; De Vriese, A.S. Evaluation of vitamin K status and rationale for vitamin K supplementation in dialysis patients. Nephrol. Dial. Transplant. 2018, 35, 23–33. [Google Scholar] [CrossRef]
- Voong, K.; Harrington, D.; Goldsmith, D. Vitamin K status in chronic kidney disease: A report of a study and a mini-review. Int. Urol. Nephrol. 2013, 45, 1339–1344. [Google Scholar] [CrossRef] [PubMed]
- Iwamoto, J.; Matsumoto, H.; Takeda, T.; Sato, Y.; Yeh, J.K. Effects of Vitamin K2 on Cortical and Cancellous Bone Mass, Cortical Osteocyte and Lacunar System, and Porosity in Sciatic Neurectomized Rats. Calcif. Tissue Int. 2010, 87, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Nagata, Y.; Inaba, M.; Imanishi, Y.; Okazaki, H.; Yamada, S.; Mori, K.; Shoji, S.; Koyama, H.; Okuno, S. Increased undercar-boxylated osteocalcin/intact osteocalcin ratio in patients undergoing hemodialysis. Osteoporos. Int. 2015, 26, 1053–1061. [Google Scholar] [CrossRef] [PubMed]
- Fusaro, M.; Noale, M.; Viola, V.; Galli, F.; Tripepi, G.; Vajente, N.; Plebani, M.; Zaninotto, M.; Guglielmi, G.; Miotto, D.; et al. Vitamin K, vertebral fractures, vascular calcifications, and mortality: VItamin K Italian (VIKI) dialysis study. J. Bone Miner. Res. 2012, 27, 2271–2278. [Google Scholar] [CrossRef] [PubMed]
- Westenfeld, R.; Krueger, T.; Schlieper, G.; Cranenburg, E.C.; Magdeleyns, E.J.; Heidenreich, S. Effect of vitamin K2 supple-mentation on functional vitamin K deficiency in hemodialysis patients: A randomized trial. Am. J. Kidney Dis. 2012, 59, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Cozzolino, M.; Cianciolo, G.; Podestà, M.A.; Ciceri, P.; Galassi, A.; Gasperoni, L.; La Manna, G. Current Therapy in CKD Patients Can Affect Vitamin K Status. Nutrients 2020, 12, 1609. [Google Scholar] [CrossRef] [PubMed]
- Cozzolino, M.; Mangano, M.; Galassi, A.; Ciceri, P.; Messa, P.; Nigwekar, S. Vitamin K in Chronic Kidney Disease. Nutrients 2019, 11, 168. [Google Scholar] [CrossRef]
- Stankowiak-Kulpa, H.; Krzyżanowska, P.; Kozioł, L.; Grzymisławski, M.; Wanic-Kossowska, M.; Moczko, J.; Walkowiak, J. Vitamin K status in peritoneally dialyzed patients with chronic kidney disease. Acta Biochim. Pol. 2011, 58, 617–620. [Google Scholar] [CrossRef]
- Jansz, T.T.; Neradova, A.; Van Ballegooijen, A.J.; Verhaar, M.C.; Vervloet, M.G.; Schurgers, L.J.; Van Jaarsveld, B.C. The role of kidney transplantation and phosphate binder use in vitamin K status. PLoS ONE 2018, 13, e0203157. [Google Scholar] [CrossRef]
- Hauschka, P.V.; Lian, J.B.; Cole, D.E.; Gundberg, C.M. Osteocalcin and matrix Gla protein: Vitamin K-dependent proteins in bone. Physiol. Rev. 1989, 69, 990–1047. [Google Scholar] [CrossRef]
- Carvallo, L.; Henriquez, B.; Paredes, R.; Olate, J.; Onate, S.; Van Wijnen, A.J.; Lian, J.B.; Stein, G.S.; Stein, J.L.; Montecino, M. 1α,25-dihydroxy vitamin D3-enhanced expression of the osteocalcin gene involves increased promoter occupancy of basal transcription regulators and gradual recruitment of the 1α,25-dihydroxy vitamin D3 receptor-SRC-1 coactivator complex. J. Cell. Physiol. 2007, 214, 740–749. [Google Scholar] [CrossRef]
- Bouleftour, W.; Bouët, G.; Granito, R.N.; Thomas, M.; Linossier, M.-T.; Vanden-Bossche, A.; Aubin, J.E.; Lafage-Proust, M.-H.; Vico, L.; Malaval, L. Blocking the Expression of Both Bone Sialoprotein (BSP) and Osteopontin (OPN) Impairs the Anabolic Action of PTH in Mouse Calvaria Bone. J. Cell. Physiol. 2014, 230, 568–577. [Google Scholar] [CrossRef]
- Turner, M.E.; Adams, M.A.; Holden, R.M. The Vitamin K Metabolome in Chronic Kidney Disease. Nutrients 2018, 10, 1076. [Google Scholar] [CrossRef]
- Pilkey, R.M.; Morton, A.R.; Boffa, M.B.; Noordhof, C.; Day, A.G.; Su, Y.; Miller, L.M.; Koschinsky, M.L.; Booth, S.L. Subclinical Vitamin K Deficiency in Hemodialysis Patients. Am. J. Kidney Dis. 2007, 49, 432–439. [Google Scholar] [CrossRef]
- Verstuyf, A.; Carmeliet, G.; Bouillon, R.; Mathieu, C. Vitamin D: A pleiotropic hormone. Kidney Int. 2010, 78, 140–145. [Google Scholar] [CrossRef]
- Levin, A.; Li, Y.C. Vitamin D and its analogues: Do they protect against cardiovascular disease in patients with kidney disease? Kidney Int. 2005, 68, 1973–1981. [Google Scholar] [CrossRef]
- DeLuca, H.F. History of the discovery of vitamin D and its active metabolites. BoneKEy Rep. 2014, 3, 479. [Google Scholar] [CrossRef]
- Holick, M.; Frommer, J.; McNeill, S.; Richtand, N.; Henley, J.; Potts, J. Photometabolism of 7-dehydrocholesterol to previtamin D3 in skin. Biochem. Biophys. Res. Commun. 1977, 76, 107–114. [Google Scholar] [CrossRef]
- Dusso, A.S.; Brown, A.J.; Slatopolsky, E. Vitamin D. Am. J. Physiol. Ren. Physiol. 2005, 289, F8–F28. [Google Scholar] [CrossRef] [PubMed]
- Fraser, D.R.; Kodicek, E. Unique Biosynthesis by Kidney of a Biologically Active Vitamin D Metabolite. Nat. Cell Biol. 1970, 228, 764–766. [Google Scholar] [CrossRef] [PubMed]
- Drechsler, C.; Pilz, S.; Obermayer-Pietsch, B.; Verduijn, M.; Tomaschitz, A.; Krane, V.; Espe, K.; Dekker, F.; Brandenburg, V.M.; März, W.; et al. Vitamin D deficiency is associated with sudden cardiac death, combined cardiovascular events, and mortality in haemodialysis patients. Eur. Heart J. 2010, 31, 2253–2261. [Google Scholar] [CrossRef] [PubMed]
- Peterlik, M.; Cross, H.S. Vitamin D and calcium deficits predispose for multiple chronic diseases. Eur. J. Clin. Investig. 2005, 35, 290–304. [Google Scholar] [CrossRef] [PubMed]
- Ramasamy, I. Vitamin D Metabolism and Guidelines for Vitamin D Supplementation. Clin. Biochem. Rev. 2020, 41, 103–126. [Google Scholar] [CrossRef]
- Christakos, S.; Dhawan, P.; Verstuyf, A.; Verlinden, L.; Carmeliet, G. Vitamin D: Metabolism, Molecular Mechanism of Action, and Pleiotropic Effects. Physiol. Rev. 2016, 96, 365–408. [Google Scholar] [CrossRef]
- Khundmiri, S.J.; Murray, R.D.; Lederer, E. PTH and Vitamin D. Compr. Physiol. 2016, 6, 561–601. [Google Scholar] [PubMed]
- Goltzman, D.; Mannstadt, M.; Marcocci, C. Physiology of the Calcium-Parathyroid Hormone-Vitamin D Axis. Front. Horm. Res. 2018, 50, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, G.; Ziemann, E.; Banfi, G.; Corbetta, S. Physical activity-dependent regulation of parathyroid hormone and calci-um-phosphorous metabolism. Int. J. Mol. Sci. 2020, 21, 5388. [Google Scholar] [CrossRef] [PubMed]
- Jacquillet, G.; Unwin, R.J. Physiological regulation of phosphate by vitamin D, parathyroid hormone (PTH) and phosphate (Pi). Pflügers Archiv Eur. J. Physiol. 2019, 471, 83–98. [Google Scholar] [CrossRef]
- Cardoso, M.P.; Pereira, L.A.L. Native vitamin D in pre-dialysis chronic kidney disease. Nefrologia 2019, 39, 18–28. [Google Scholar] [CrossRef]
- A Schmidt, J. Measurement of 25-Hydroxyvitamin D Revisited. Clin. Chem. 2006, 52, 2304–2305. [Google Scholar] [CrossRef][Green Version]
- Terry, A.H.; Sandrock, T.; Meikle, A.W. Measurement of 25-Hydroxyvitamin D by the Nichols ADVANTAGE, DiaSorin LIAISON, DiaSorin RIA, and Liquid Chromatography–Tandem Mass Spectrometry. Clin. Chem. 2005, 51, 1565–1566. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sirajudeen, S.; Shah, I.; Al Menhali, A. A Narrative Role of Vitamin D and Its Receptor: With Current Evidence on the Gastric Tissues. Int. J. Mol. Sci. 2019, 20, 3832. [Google Scholar] [CrossRef]
- Shah, I.; James, B.; Barker, J.; Petroczi, A.; Naughton, D.P. Misleading measures in Vitamin D analysis: A novel LC-MS/MS assay to account for epimers and isobars. Nutr. J. 2011, 10, 46. [Google Scholar] [CrossRef]
- Holick, M.F. Vitamin D Deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef]
- Mehrotra, R.; Kermah, D.; Budoff, M.; Salusky, I.B.; Mao, S.S.; Gao, Y.L.; Takasu, J.; Adler, S.; Norris, K. Hypovitaminosis D in Chronic Kidney Disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1144–1151. [Google Scholar] [CrossRef]
- Huang, Y.; Yu, H.; Lu, J.; Guo, K.; Zhang, L.; Bao, Y.; Chen, H.; Jia, W. Oral Supplementation with Cholecalciferol 800 IU Ameliorates Albuminuria in Chinese Type 2 Diabetic Patients with Nephropathy. PLoS ONE 2012, 7, e50510. [Google Scholar] [CrossRef]
- Capelli, I.; Cianciolo, G.; Gasperoni, L.; Galassi, A.; Ciceri, P.; Cozzolino, M. Nutritional vitamin D in CKD: Should we measure? Should we treat? Clin. Chim. Acta 2020, 501, 186–197. [Google Scholar] [CrossRef] [PubMed]
- Çankaya, E.; Bilen, Y.; Keleş, M.; Uyanık, A.; Akbaş, M.; Güngör, A.; Arslan, Ş.; Aydınlı, B. Comparison of Serum Vitamin D Levels Among Patients With Chronic Kidney Disease, Patients in Dialysis, and Renal Transplant Patients. Transplant. Proc. 2015, 47, 1405–1407. [Google Scholar] [CrossRef] [PubMed]
- Ravani, P.; Malberti, F.; Tripepi, G.; Pecchini, P.; Cutrupi, S.; Pizzini, P.; Mallamaci, F.; Zoccali, C. Vitamin D levels and patient outcome in chronic kidney disease. Kidney Int. 2009, 75, 88–95. [Google Scholar] [CrossRef]
- Mehrotra, R.; Kermah, D.A.; Salusky, I.B.; Wolf, M.S.; Thadhani, R.I.; Chiu, Y.-W.; Martins, D.; Adler, S.G.; Norris, K.C. Chronic kidney disease, hypovitaminosis D, and mortality in the United States. Kidney Int. 2009, 76, 977–983. [Google Scholar] [CrossRef]
- KDOQI US Commentary on the 2017 KDIGO Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease—Mineral and Bone Disorder (CKD-MBD). Available online: https://www.ajkd.org/action/showPdf?pii=S0272-6386%2817%2930898-3 (accessed on 19 August 2018).
- Koshihara, Y.; Hoshi, K.; Okawara, R.; Ishibashi, H.; Yamamoto, S. Vitamin K stimulates osteoblastogenesis and inhibits osteoclastogenesis in human bone marrow cell culture. J. Endocrinol. 2003, 176, 339–348. [Google Scholar] [CrossRef]
- Li, W.; Zhang, S.; Liu, J.; Liu, Y.; Liang, Q. Vitamin K2 stimulates Mc3T3‑E1 osteoblast differentiation and mineralization through autophagy induction. Mol. Med. Rep. 2019, 19, 3676–3684. [Google Scholar] [CrossRef] [PubMed]
- Urayama, S.; Kawakami, A.; Nakashima, T.; Tsuboi, M.; Yamasaki, S.; Hida, A.; Ichinose, Y.; Nakamura, H.; Ejima, E.; Aoyagi, T.; et al. Effect of vitamin K2 on osteoblast apoptosis: Vitamin K2 inhibits apoptotic cell death of human osteoblasts induced by Fas, proteasome inhibitor, etoposide, and staurosporine. J. Lab. Clin. Med. 2000, 136, 181–193. [Google Scholar] [CrossRef] [PubMed]
- Katsuyama, H.; Saijoh, K.; Otsuki, T.; Tomita, M.; Fukunaga, M.; Sunami, S. Menaquinone-7 regulates gene expression in osteoblastic MC3T3E1 cells. Int. J. Mol. Med. 2007, 19, 279–284. [Google Scholar] [CrossRef][Green Version]
- Yamaguchi, M.; Weitzmann, M.N. Vitamin K2 stimulates osteoblastogenesis and suppresses osteoclastogenesis by suppressing NF-κB activation. Int. J. Mol. Med. 2011, 27, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Poon, C.C.; Li, R.W.; Seto, S.W.; Kong, S.K.; Ho, H.P.; Hoi, M.P.; Lee, S.M.; Ngai, S.M.; Chan, S.W.; Leung, G.P.; et al. In vitro vitamin K2 and 1α,25-dihydroxyvitamin D3 combination enhances osteoblasts anabolism of diabetic mice. Eur. J. Pharmacol. 2015, 767, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Kameda, T.; Miyazawa, K.; Mori, Y.; Yuasa, T.; Shiokawa, M.; Nakamaru, Y.; Mano, H.; Hakeda, Y.; Kameda, A.; Kumegawa, M. Vitamin K2Inhibits Osteoclastic Bone Resorption by Inducing Osteoclast Apoptosis. Biochem. Biophys. Res. Commun. 1996, 220, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Yamaguchi, M.; Uchiyama, S.; Tsukamoto, Y. Inhibitory effect of menaquinone-7 (vitamin K2) on the bone-resorbing fac-tors-induced bone resorption in elderly female rat femoral tissues in vitro. Mol. Cell. Biochem. 2003, 245, 115–120. [Google Scholar] [CrossRef]
- Pereira, R.C.; Salusky, I.B.; Bowen, R.E.; Freymiller, E.G.; Wesseling-Perry, K. Vitamin D sterols increase FGF23 expression by stimulating osteoblast and osteocyte maturation in CKD bone. Bone 2019, 127, 626–634. [Google Scholar] [CrossRef]
- Zhou, S.; Glowacki, J.; Kim, S.W.; Hahne, J.; Geng, S.; Mueller, S.M.; Shen, L.; Bleiberg, I.; LeBoff, M.S. Clinical characteristics influence in vitro action of 1,25-dihydroxyvitamin D3 in human marrow stromal cells. J. Bone Miner. Res. 2012, 27, 1992–2000. [Google Scholar] [CrossRef] [PubMed]
- Al Saedi, A.; Myers, D.E.; Stupka, N.; Duque, G. 1,25(OH)2D3 ameliorates palmitate-induced lipotoxicity in human primary osteoblasts leading to improved viability and function. Bone 2020, 141, 115672. [Google Scholar] [CrossRef] [PubMed]
- Allard, L.; Demoncheaux, N.; Machuca-Gayet, I.; Georgess, D.; Coury-Lucas, F.; Jurdic, P.; Bacchetta, J. Biphasic Effects of Vitamin D and FGF23 on Human Osteoclast Biology. Calcif. Tissue Int. 2015, 97, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Ji, L.; Gao, J.; Kong, R.; Gao, Y.; Ji, X.; Zhao, D. Autophagy exerts pivotal roles in regulatory effects of 1α,25-(OH)2D3 on the osteoclastogenesis. Biochem. Biophys. Res. Commun. 2019, 511, 869–874. [Google Scholar] [CrossRef]
- Zhou, S.; Leboff, M.S.; Waikar, S.S.; Glowacki, J. Vitamin D metabolism and action in human marrow stromal cells: Effects of chronic kidney disease. J. Steroid. Biochem. Mol. Biol. 2013, 136, 342–344. [Google Scholar] [CrossRef][Green Version]
- Pereira, R.C.; Salusky, I.B.; Roschger, P.; Klaushofer, K.; Yadin, O.; Freymiller, E.G.; Bowen, R.; Delany, A.M.; Fratzl-Zelman, N.; Wesseling-Perry, K. Impaired osteocyte maturation in the pathogenesis of renal osteodystrophy. Kidney Int. 2018, 94, 1002–1012. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Bertucci, C.; Gao, Y.; Li, J.; Luu, S.; LeBoff, M.S.; Glowacki, J.; Zhou, S. Fibroblast growth factor 23 counters vitamin D metabolism and action in human mesenchymal stem cells. J. Steroid Biochem. Mol. Biol. 2020, 199, 105587. [Google Scholar] [CrossRef]
- Suda, T.; Ueno, Y.; Fujii, K.; Shinki, T. Vitamin D and bone. J. Cell. Biochem. 2002, 88, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Van Leeuwen, J.P.; Van Driel, M.; Bemd, G.J.V.D.; Pols, H.A. Vitamin D control of osteoblast function and bone extracellular matrix mineralization. Crit. Rev. Eukaryot. Gene Expr. 2001, 11, 199–226. [Google Scholar] [CrossRef]
- Zarei, A.; Morovat, A.; Javaid, K.; Brown, C.P. Vitamin D receptor expression in human bone tissue and dose-dependent activation in resorbing osteoclasts. Bone Res. 2016, 4, 16030. [Google Scholar] [CrossRef]
- Ženata, O.; Marcalíková, A.; Vrzal, R. The effect of caffeine on calcitriol-inducible vitamin D receptor-controlled gene expres-sion in intestinal and osteoblastic cells. Calcif. Tissue Int. 2019, 105, 651–659. [Google Scholar] [CrossRef] [PubMed]
- Turner, A.G.; Hanrath, M.A.; Morris, H.A.; Atkins, G.J.; Anderson, P.H. The local production of 1,25(OH)2D3 promotes osteoblast and osteocyte maturation. J. Steroid Biochem. Mol. Biol. 2014, 144, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Van de Peppel, J.; van Leeuwen, J.P. Vitamin D and gene networks in human osteoblasts. Front. Physiol. 2014, 5, 137. [Google Scholar] [CrossRef]
- Meyer, M.B.; Benkusky, N.A.; Lee, C.-H.; Pike, J.W. Genomic Determinants of Gene Regulation by 1,25-Dihydroxyvitamin D3 during Osteoblast-lineage Cell Differentiation. J. Biol. Chem. 2014, 289, 19539–19554. [Google Scholar] [CrossRef]
- Geng, S.; Zhou, S.; Bi, Z.; Glowacki, J. Vitamin D metabolism in human bone marrow stromal (mesenchymal stem) cells. Metabolism 2013, 62, 768–777. [Google Scholar] [CrossRef]
- Van Driel, M.; Koedam, M.; Buurman, C.; Hewison, M.; Chiba, H.; Uitterlinden, A.; Pols, H.; Van Leeuwen, J. Evidence for auto/paracrine actions of vitamin D in bone: 1a-hydroxylase expression and activity in human bone cells. FASEB J. 2006, 20, 2417–2419. [Google Scholar] [CrossRef]
- Duque, G.; El Abdaimi, K.; E Henderson, J.; Lomri, A.; Kremer, R. Vitamin D inhibits Fas ligand-induced apoptosis in human osteoblasts by regulating components of both the mitochondrial and Fas-related pathways. Bone 2004, 35, 57–64. [Google Scholar] [CrossRef]
- Zhang, X.; Zanello, L.P. Vitamin D Receptor-Dependent 1α,25(OH)2 Vitamin D3-Induced Anti-Apoptotic PI3K/AKT Signaling in Osteoblasts. J. Bone Miner. Res. 2008, 23, 1238–1248. [Google Scholar] [CrossRef]
- Weinstein, R.S.; Manolagas, S.C. Apoptosis and osteoporosis. Am. J. Med. 2000, 108, 153–164. [Google Scholar] [CrossRef]
- Prince, M.; Banerjee, C.; Javed, A.; Green, J.; Lian, J.B.; Stein, G.S.; Bodine, P.V.; Komm, B.S. Expression and regulation of Runx2/Cbfa1 and osteoblast phenotypic markers during the growth and differentiation of human osteoblasts. J. Cell. Biochem. 2001, 80, 424–440. [Google Scholar] [CrossRef]
- Maehata, Y.; Takamizawa, S.; Ozawa, S.; Kato, Y.; Sato, S.; Kubota, E.; Hata, R.-I. Both direct and collagen-mediated signals are required for active vitamin D3-elicited differentiation of human osteoblastic cells: Roles of osterix, an osteoblast-related transcription factor. Matrix Biol. 2006, 25, 47–58. [Google Scholar] [CrossRef] [PubMed]
- Piek, E.; Sleumer, L.S.; van Someren, E.P.; Heuver, L.; de Haan, J.R.; de Grijs, I.; Gilissen, C.; Hendriks, J.M.; van Ravestein-van Os, R.I.; Bauerschmidt, S.; et al. Osteo-transcriptomics of human mesenchymal stem cells: Accelerated gene expression and osteoblast differentiation induced by vitamin D reveals c-MYC as an enhancer of BMP2-induced osteo-genesis. Bone 2010, 46, 613–627. [Google Scholar] [CrossRef] [PubMed]
- Kveiborg, M.; Flyvbjerg, A.; Eriksen, E.F.; Kassem, M. 1,25-Dihydroxyvitamin D3 stimulates the production of insulin-like growth factor-binding proteins-2, -3 and -4 in human bone marrow stromal cells. Eur. J. Endocrinol. 2001, 144, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Li, H. Tricin enhances osteoblastogenesis through the regulation of Wnt/β-catenin signaling in human mesenchymal stem cells. Mech. Dev. 2018, 152, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Zhang, Y.; Xin, N.; Yuan, Y.; Zhang, Q.; Gong, P.; Wu, Y. 1α,25-Dihydroxyvitamin D3 promotes osteogenesis by promoting Wnt signaling pathway. J. Steroid Biochem. Mol. Biol. 2017, 174, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Jo, S.; Yoon, S.; Lee, S.Y.; Kim, S.Y.; Park, H.; Han, J.; Choi, S.H.; Han, J.-S.; Yang, J.-H.; Kim, T.-H. DKK1 Induced by 1,25D3 Is Required for the Mineralization of Osteoblasts. Cells 2020, 9, 236. [Google Scholar] [CrossRef] [PubMed]
- Hocking, L.J.; Whitehouse, C.; Helfrich, M.H. Autophagy: A new player in skeletal maintenance? J. Bone Miner. Res. 2012, 27, 1439–1447. [Google Scholar] [CrossRef] [PubMed]
- Nollet, M.; Santucci-Darmanin, S.; Breuil, V.; Al-Sahlanee, R.; Cros, C.; Topi, M.; Momier, D.; Samson, M.; Pagnotta, S.; Cailleteau, L.; et al. Autophagy in osteoblasts is involved in mineralization and bone homeostasis. Autophagy 2014, 10, 1965–1977. [Google Scholar] [CrossRef] [PubMed]
- Mayer, H.; Bertram, H.; Lindenmaier, W.; Korff, T.; Weber, H.; Weich, H. Vascular endothelial growth factor (VEGF-A) ex-pression in human mesenchymal stem cells: Autocrine and paracrine role on osteoblastic and endothelial differentiation. J. Cell. Biochem. 2005, 95, 827–839. [Google Scholar] [CrossRef]
- Wang, D.S.; Yamazaki, K.; Nohtomi, K.; Shizume, K.; Ohsumi, K.; Shibuya, M.; Demura, H.; Sato, K. Increase of vascular endothelial growth factor mRNA expression by 1,25-dihydroxyvitamin D3 in human osteoblast-like cells. J. Bone Miner. Res. 2009, 11, 472–479. [Google Scholar] [CrossRef]
- Neve, A.; Cantatore, F.P.; Corrado, A.; Gaudio, A.; Ruggieri, S.; Ribatti, D. In vitro and in vivo angiogenic activity of osteo-arthritic and osteoporotic osteoblasts is modulated by VEGF and vitamin D3 treatment. Regul. Pept. 2013, 184, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Atkins, G.J.; Kostakis, P.; Pan, B.; Farrugia, A.; Gronthos, S.; Evdokiou, A.; Harrison, K.; Findlay, D.M.; Zannettino, A.C.W. RANKL Expression Is Related to the Differentiation State of Human Osteoblasts. J. Bone Miner. Res. 2003, 18, 1088–1098. [Google Scholar] [CrossRef] [PubMed]
- Woeckel, V.; Alves, R.; Swagemakers, S.; Eijken, M.; Chiba, H.; Van Der Eerden, B.; Van Leeuwen, J. 1α,25-(OH)2D3 acts in the early phase of osteoblast differentiation to enhance mineralization via accelerated production of mature matrix vesicles. J. Cell. Physiol. 2010, 225, 593–600. [Google Scholar] [CrossRef]
- Woeckel, V.; Van Der Eerden, B.; Schreuders-Koedam, M.; Eijken, M.; Van Leeuwen, J. 1α,25-dihydroxyvitamin D3 stimulates activin A production to fine-tune osteoblast-induced mineralization. J. Cell. Physiol. 2013, 228, 2167–2174. [Google Scholar] [CrossRef]
- Atkins, G.J.; Anderson, P.H.; Findlay, D.M.; Welldon, K.J.; Vincent, C.; Zannettino, A.C.; O’Loughlin, P.D.; Morris, H.A. Metabolism of vitamin D3 in human osteoblasts: Evidence for autocrine and paracrine activities of 1 alpha,25-dihydroxyvitamin D3. Bone 2007, 40, 1517–1528. [Google Scholar] [CrossRef]
- Li, J.J.; Sodek, J. Cloning and characterization of the rat bone sialoprotein gene promoter. Biochem. J. 1993, 289, 625–629. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ormsby, R.T.; Findlay, D.M.; Kogawa, M.; Anderson, P.H.; Morris, H.A.; Atkins, G.J. Analysis of vitamin D metabolism gene expression in human bone: Evidence for autocrine control of bone remodelling. J. Steroid Biochem. Mol. Biol. 2014, 144, 110–113. [Google Scholar] [CrossRef]
- Giner, M.; Rios, M.J.; Montoya, M.J.; Vázquez, M.A.; Naji, L.; Pérez-Cano, R. RANKL/OPG in primary cultures of osteoblasts from post-menopausal women. Differences between osteoporotic hip fractures and osteoarthritis. J. Steroid Biochem. Mol. Biol. 2009, 113, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Yasuda, H.; Shima, N.; Nakagawa, N.; Yamaguchi, K.; Kinosaki, M.; Mochizuki, S.-I.; Tomoyasu, A.; Yano, K.; Goto, M.; Murakami, A.; et al. Osteoclast differentiation factor is a ligand for osteoprotegerin/osteoclastogenesis-inhibitory factor and is identical to TRANCE/RANKL. Proc. Natl. Acad. Sci. USA 1998, 95, 3597–3602. [Google Scholar] [CrossRef] [PubMed]
- Bikle, D.D. Vitamin D and bone. Curr. Osteoporos. Rep. 2012, 10, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, N.; Udagawa, N.; Suda, T. Vitamin D endocrine system and osteoclasts. Bonekey Rep. 2014, 3, 495. [Google Scholar] [CrossRef] [PubMed]
- Suda, T.; Takahashi, N.; Abe, E. Role of vitamin D in bone resorption. J. Cell. Biochem. 1992, 49, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Kogawa, M.; Findlay, D.M.; Anderson, P.H.; Ormsby, R.; Vincent, C.; Morris, H.A.; Atkins, G.J. Osteoclastic Metabolism of 25(OH)-Vitamin D3: A Potential Mechanism for Optimization of Bone Resorption. Endocrinology 2010, 151, 4613–4625. [Google Scholar] [CrossRef]
- Sakai, S.; Takaishi, H.; Matsuzaki, K.; Kaneko, H.; Furukawa, M.; Miyauchi, Y.; Shiraishi, A.; Saito, K.; Tanaka, A.; Taniguchi, T.; et al. 1-Alpha, 25-dihydroxy vitamin D3 inhibits osteoclastogenesis through IFN-beta-dependent NFATc1 suppression. J. Bone Miner. Metab. 2009, 27, 643–652. [Google Scholar] [CrossRef]
- Kudo, O.; Sabokbar, A.; Pocock, A.; Itonaga, I.; Athanasou, N. Isolation of Human Osteoclasts Formed In Vitro: Hormonal Effects on the Bone-Resorbing Activity of Human Osteoclasts. Calcif. Tissue Int. 2002, 71, 539–546. [Google Scholar] [CrossRef]
- Kim, T.-H.; Lee, B.; Kwon, E.; Choi, C.H.; Sung, I.-H.; Kim, Y.; Sohn, J.; Ji, J.D. 1,25-dihydroxyvitamin D3 inhibits directly human osteoclastogenesis by down-regulation of the c-Fms and RANK expression. Jt. Bone Spine 2013, 80, 307–314. [Google Scholar] [CrossRef]
- Kim, H.; Baek, S.; Hong, S.M.; Lee, J.; Jung, S.M.; Lee, J.; Cho, M.; Kwok, S.K.; Park, S.H. 1,25-dihydroxy vitamin D3 and interleukin-6 blockade synergistically regulate rheumatoid arthritis by suppressing interleukin-17 production and osteoclas-togenesis. J. Korean Med. Sci. 2020, 35, e40. [Google Scholar] [CrossRef]
- Bennett, C.N.; Ouyang, H.; Ma, Y.L.; Zeng, Q.; Gerin, I.; Sousa, K.M.; Lane, T.F.; Krishnan, V.; Hankenson, K.D.; MacDougald, O.A. Wnt10b Increases Postnatal Bone Formation by Enhancing Osteoblast Differentiation. J. Bone Miner. Res. 2007, 22, 1924–1932. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.-L.; Shyu, J.-F.; Wu, C.-C.; Hung, C.-F.; Liao, M.-T.; Liu, W.-C.; Zheng, C.-M.; Hou, Y.-C.; Lin, Y.-F.; Lu, K.-C. Association of Anabolic Effect of Calcitriol with Osteoclast-Derived Wnt 10b Secretion. Nutrients 2018, 10, 1164. [Google Scholar] [CrossRef] [PubMed]
- DeSelm, C.J.; Miller, B.C.; Zou, W.; Beatty, W.L.; van Meel, E.; Takahata, Y.; Klumperman, J.; Tooze, S.A.; Teitelbaum, S.L.; Virgin, H.W. Autophagy Proteins Regulate the Secretory Component of Osteoclastic Bone Resorption. Dev. Cell 2011, 21, 966–974. [Google Scholar] [CrossRef] [PubMed]
- Sul, O.J.; Park, H.J.; Son, H.J.; Choi, H.S. Lipopolysaccharide (LPS)-induced autophagy is responsible for enhanced osteo-clastogenesis. Mol. Cells 2017, 40, 880–887. [Google Scholar]
- Iwamoto, J.; Seki, A.; Sato, Y.; Matsumoto, H. Vitamin K2 Improves Renal Function and Increases Femoral Bone Strength in Rats with Renal Insufficiency. Calcif. Tissue Int. 2011, 90, 50–59. [Google Scholar] [CrossRef]
- Akiyama, Y.; Hara, K.; Kobayashi, M.; Tomiuga, T.; Nakamura, T. Inhibitory effect of vitamin K2 (menatetrenone) on bone resorption in ovariectomized rats: A histomorphometric and dual energy X-ray absorptiometric study. Jpn. J. Pharmacol. 1999, 80, 67–74. [Google Scholar] [CrossRef][Green Version]
- Nagura, N.; Komatsu, J.; Iwase, H.; Hosoda, H.; Ohbayashi, O.; Nagaoka, I.; Kaneko, K. Effects of the combination of vitamin K and teriparatide on the bone metabolism in ovariectomized rats. Biomed. Rep. 2015, 3, 295–300. [Google Scholar] [CrossRef][Green Version]
- Iwasaki, Y.; Yamato, H.; Murayama, H.; Sato, M.; Takahashi, T.; Ezawa, I.; Kurokawa, K.; Fukagawa, M. Maintenance of trabecular structure and bone volume by vitamin K 2 in mature rats with long-term tail suspension. J. Bone Miner. Metab. 2002, 20, 216–222. [Google Scholar] [CrossRef]
- Kim, M.; Na, W.; Sohn, C. Vitamin K1 (phylloquinone) and K2 (menaquinone-4) supplementation improves bone formation in a high-fat diet-induced obese mice. J. Clin. Biochem. Nutrients 2013, 53, 108–113. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Iwasaki, Y.; Yamato, H.; Murayama, H.; Sato, M.; Takahashi, T.; Ezawa, I.; Kurokawa, K.; Fukagawa, M. Combination use of vitamin K 2 further increases bone volume and ameliorates extremely low turnover bone induced by bisphosphonate therapy in tail-suspension rats. J. Bone Miner. Metab. 2003, 21, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Matsunaga, S.; Ito, H.; Sakou, T. The effect of vitamin K and D supplementation on ovariectomy-induced bone loss. Calcif. Tissue Int. 1999, 65, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Otomo, H.; Sakai, A.; Ikeda, S.; Tanaka, S.; Ito, M.; Phipps, R.J.; Nakamura, T. Regulation of mineral-to-matrix ratio of lumbar trabecular bone in ovariectomized rats treated with risedronate in combination with or without vitamin K2. J. Bone Miner. Metab. 2004, 22, 404–414. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, Y.; Mikuni-Takagaki, Y.; Kozai, Y.; Miyagawa, K.; Naruse, K.; Wakao, H.; Kawamata, R.; Kashima, I.; Sakurai, T. Prior treatment with vitamin K2 significantly improves the efficacy of risedronate. Osteoporos. Int. 2009, 20, 1863–1872. [Google Scholar] [CrossRef][Green Version]
- Jokihaara, J.; Pörsti, I.; Pajamäki, I.; Vuohelainen, T.; Jolma, P.; Kööbi, P.; Kalliovalkama, J.; Niemela, O.; Kannus, P.; Sievanen, H.; et al. Paricalcitol [19-Nor-1,25-(OH)2D2] in the Treatment of Experimental Renal Bone Disease. J. Bone Miner. Res. 2006, 21, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Díaz, M.N.; Rodríguez, A.R.; Fernandez-Martin, J.L.; Arias, M.S.; Rodríguez, P.M.; Cannata-Andía, J.B. Effects of estradiol, calcitriol and both treatments combined on bone histomorphometry in rats with chronic kidney disease and ovariectomy. Bone 2007, 41, 614–619. [Google Scholar] [CrossRef]
- Sanchez, C.P.; He, Y.Z. Bone growth during daily or intermittent calcitriol treatment during renal failure with advanced secondary hyperparathyroidism. Kidney Int. 2007, 72, 582–591. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, W.E.; Bordier, P.; Marie, P.; Hruska, K.; Harter, H.; Greenwalt, A.; Blondin, J.; Haddad, J.; Bricker, N.; Slatopolsky, E. Phosphate Control and 25-Hydroxycholecalciferol Administration in Preventing Experimental Renal Osteodystrophy in the Dog. J. Clin. Investig. 1977, 60, 332–341. [Google Scholar] [CrossRef] [PubMed]
- Jablonski, G.; Mortensen, B.M.; Klem, K.H.; Mosekilde, L.; Danielsen, C.C.; Gordeladze, J.O. Vitamin D3 analogs and salmon calcitonin partially reverse the development of renal osteodystrophy in rats. Calcif. Tissue Int. 1995, 57, 385–391. [Google Scholar] [CrossRef]
- Newman, C.L.; Tian, N.; Hammond, M.A.; Wallace, J.M.; Brown, D.M.; Chen, N.X.; Moe, S.M.; Allen, M.R. Calcitriol sup-pression of parathyroid hormone fails to improve skeletal properties in an animal model of chronic kidney disease. Am. J. Nephrol. 2016, 43, 20–31. [Google Scholar] [CrossRef]
- De Schutter, T.M.; Behets, G.J.; Jung, S.; Neven, E.; D’Haese, P.C.; Querfeld, U. Restoration of Bone Mineralization by Cinacalcet is Associated with a Significant Reduction in Calcitriol-Induced Vascular Calcification in Uremic Rats. Calcif. Tissue Int. 2012, 91, 307–315. [Google Scholar] [CrossRef]
- Bisson, S.-K.; Ung, R.-V.; Picard, S.; Valade, D.; Agharazii, M.; Larivière, R.; Mac-Way, F. High calcium, phosphate and calcitriol supplementation leads to an osteocyte-like phenotype in calcified vessels and bone mineralisation defect in uremic rats. J. Bone Miner. Metab. 2018, 37, 212–223. [Google Scholar] [CrossRef]
- Idelevich, A.; Kerschnitzki, M.; Shahar, R.; Monsonego-Ornan, E. 1,25(OH)2D3 Alters Growth Plate Maturation and Bone Architecture in Young Rats with Normal Renal Function. PLoS ONE 2011, 6, e20772. [Google Scholar] [CrossRef]
- Wronski, T.; Halloran, B.P.; Bikle, D.D.; Globus, R.K.; Morey-Holton, E.R. Chronic administration of 1,25-dihydroxyvitamin D3: Increased bone but impaired mineralization. Endocrinology 1986, 119, 2580–2585. [Google Scholar] [CrossRef]
- Lieben, L.; Masuyama, R.; Torrekens, S.; Van Looveren, R.; Schrooten, J.; Baatsen, P.; Lafage-Proust, M.-H.; Dresselaers, T.; Feng, J.Q.; Bonewald, L.F.; et al. Normocalcemia is maintained in mice under conditions of calcium malabsorption by vitamin D–induced inhibition of bone mineralization. J. Clin. Investig. 2012, 122, 1803–1815. [Google Scholar] [CrossRef]
- Xue, Y.; Karaplis, A.C.; Hendy, G.N.; Goltzman, D.; Miao, D. Exogenous 1,25-Dihydroxyvitamin D3 Exerts a Skeletal Anabolic Effect and Improves Mineral Ion Homeostasis in Mice that Are Homozygous for Both the 1α-Hydroxylase and Parathyroid Hormone Null Alleles. Endocrinology 2006, 147, 4801–4810. [Google Scholar] [CrossRef] [PubMed]
- Panda, D.K.; Miao, D.; Bolivar, I.; Li, J.; Huo, R.; Hendy, G.N.; Goltzman, D. Inactivation of the 25-Hydroxyvitamin D 1α-Hydroxylase and Vitamin D Receptor Demonstrates Independent and Interdependent Effects of Calcium and Vitamin D on Skeletal and Mineral Homeostasis. J. Biol. Chem. 2004, 279, 16754–16766. [Google Scholar] [CrossRef] [PubMed]
- Kohlmeier, M.; Saupe, J.; Shearer, M.J.; Schaefer, K.; Asmus, G. Bone health of adult hemodialysis patients is related to vitamin K status. Kidney Int. 1997, 51, 1218–1221. [Google Scholar] [CrossRef] [PubMed]
- Fusaro, M.; Tripepi, G.; Noale, M.; Plebani, M.; Zaninotto, M.; Piccoli, A.; Naso, A.; Miozzo, D.; Giannini, S.; Avolio, M.; et al. Prevalence of Vertebral Fractures, Vascular Calcifications, and Mortality in Warfarin Treated Hemodialysis Patients. Curr. Vasc. Pharmacol. 2015, 13, 248–258. [Google Scholar] [CrossRef] [PubMed]
- Evenepoel, P.; Claes, K.; Meijers, B.; Laurent, M.; Bammens, B.; Naesens, M.; Sprangers, B.; Pottel, H.; Cavalier, E.; Kuypers, D. Poor Vitamin K Status Is Associated With Low Bone Mineral Density and Increased Fracture Risk in End-Stage Renal Disease. J. Bone Miner. Res. 2019, 34, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, N.; Kusano, E.; Takahashi, H.; Ando, Y.; Yano, K.; Tsuda, E.; Asano, Y. Vitamin K2 inhibits glucocorticoid-induced bone loss partly by preventing the reduction of osteoprotegerin (OPG). J. Bone Miner. Metab. 2005, 23, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Coen, G.; Mantella, D.; Manni, M.; Balducci, A.; Nofroni, I.; Sardella, D.; Ballanti, P.; Bonucci, E. 25-hydroxyvitamin D levels and bone histomorphometry in hemodialysis renal osteodystrophy. Kidney Int. 2005, 68, 1840–1848. [Google Scholar] [CrossRef] [PubMed]
- Ambrus, C.; Almasi, C.; Berta, K.; Deák, G.; Marton, A.; Molnár, M.Z.; Németh, Z.; Horváth, C.; Lakatos, P.; Szathmári, M.; et al. Vitamin D insufficiency and bone fractures in patients on maintenance hemodialysis. Int. Urol. Nephrol. 2010, 43, 475–482. [Google Scholar] [CrossRef]
- Bosworth, C.; De Boer, I.H.; Targher, G.; Kendrick, J.; Smits, G.; Chonchol, M. The effect of combined calcium and cholecalciferol supplementation on bone mineral density in elderly women with moderate chronic kidney disease. Clin. Nephrol. 2012, 77, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Mager, D.R.; Jackson, S.T.; Hoffmann, M.R.; Jindal, K.; Senior, P.A. Vitamin D 3 supplementation, bone health and quality of life in adults with diabetes and chronic kidney disease: Results of an open label randomized clinical trial. Clin. Nutr. 2017, 36, 686–696. [Google Scholar] [CrossRef]
- Moe, S.M.; Saifullah, A.; LaClair, R.E.; Usman, S.A.; Yu, Z. A Randomized Trial of Cholecalciferol versus Doxercalciferol for Lowering Parathyroid Hormone in Chronic Kidney Disease. Clin. J. Am. Soc. Nephrol. 2010, 5, 299–306. [Google Scholar] [CrossRef]
- Caluwe, R.; Vandecasteele, S.; Van Vlem, B.; Vermeer, C.; De Vriese, A.S. Vitamin K2 supplementation in haemodialysis patients: A randomized dose-finding study. Nephrol. Dial. Transplant. 2014, 29, 1385–1390. [Google Scholar] [CrossRef]
- Aoun, M.; Makki, M.; Azar, H.; Matta, H.; Chelala, D.N. High Dephosphorylated-Uncarboxylated MGP in Hemodialysis patients: Risk factors and response to vitamin K2, A pre-post intervention clinical trial. BMC Nephrol. 2017, 18, 191. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/record/NCT02976246 (accessed on 29 November 2016).
- Krueger, T.; Schlieper, G.; Schurgers, L.; Cornelis, T.; Cozzolino, M.; Jacobi, J.; Jadoul, M.; Ketteler, M.; Rump, L.C.; Stenvinkel, P.; et al. Vitamin K1 to slow vascular calcification in haemodialysis patients (VitaVasK trial): A rationale and study protocol. Nephrol. Dial. Transplant. 2014, 29, 1633–1638. [Google Scholar] [CrossRef]
- Haroon, S.W.; Tai, B.C.; Ling, L.H.; Teo, L.; Davenport, A.; Schurgers, L.; Teo, B.W.; Khatri, P.; Ong, C.C.; Low, S.; et al. Treatment to reduce vascular calcification in he-modialysis patients using vitamin K (Trevasc-HDK): A study protocol for a randomized controlled trial. Medicine 2020, 99, e21906. [Google Scholar] [CrossRef]
- Oikonomaki, T.; Papasotiriou, M.; Ntrinias, T.; Kalogeropoulou, C.; Zabakis, P.; Kalavrizioti, D.; Papadakis, I.; Goumenos, D.S.; Papachristou, E. The effect of vitamin K2 supplementation on vascular calcification in haemodialysis patients: A 1-year follow-up randomized trial. Int. Urol Nephrol. 2019, 51, 2037–2044. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT02324686 (accessed on 24 December 2014).
- ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT02278692 (accessed on 30 October 2014).
- ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT04477811 (accessed on 20 July 2020).
- Levin, A.; Bakris, G.; Molitch, M.; Smulders, M.; Tian, J.; Williams, L.; Andress, D. Prevalence of abnormal serum vitamin D, PTH, calcium, and phosphorus in patients with chronic kidney disease: Results of the study to evaluate early kidney disease. Kidney Int. 2007, 71, 31–38. [Google Scholar] [CrossRef]
- Taal, M.W.; Thurston, V.; McIntyre, N.J.; Fluck, R.J.; McIntyre, C.W. The impact of vitamin D status on the relative increase in fibroblast growth factor 23 and parathyroid hormone in chronic kidney disease. Kidney Int. 2014, 86, 407–413. [Google Scholar] [CrossRef]
- Westerberg, P.-A.; Linde, T.; Wikström, B.; Ljunggren, Ö.; Stridsberg, M.; Larsson, T.E. Regulation of fibroblast growth factor-23 in chronic kidney disease. Nephrol. Dial. Transplant. 2007, 22, 3202–3207. [Google Scholar] [CrossRef] [PubMed]
- Shardlow, A.; McIntyre, N.J.; Fluck, R.J.; McIntyre, C.W.; Taal, M.W. Associations of fibroblast growth factor 23, vitamin D and parathyroid hormone with 5-year outcomes in a prospective primary care cohort of people with chronic kidney disease stage 3. BMJ Open 2017, 7, e016528. [Google Scholar] [CrossRef] [PubMed]
- Metzger, M.; Houillier, P.; Gauci, C.; Haymann, J.P.; Flamant, M.; Thervet, E.; Boffa, J.-J.; Vrtovsnik, F.; Froissart, M.; Stengel, B.; et al. Relation Between Circulating Levels of 25(OH) Vitamin D and Parathyroid Hormone in Chronic Kidney Disease: Quest for a Threshold. J. Clin. Endocrinol. Metab. 2013, 98, 2922–2928. [Google Scholar] [CrossRef] [PubMed]
- González, E.A.; Sachdeva, A.; Oliver, D.A.; Martin, K.J. Vitamin D Insufficiency and Deficiency in Chronic Kidney Disease. Am. J. Nephrol. 2004, 24, 503–510. [Google Scholar] [CrossRef]
- Ishimura, E.; Tsuchida, T. Vitamin D deficiency/insufficiency in patients with chronic kidney disease stage 3 and 4—Current concept and its therapeutic strategy. Clin. Calcium 2004, 14, 764–769. [Google Scholar]
- LaClair, R.E.; Hellman, R.N.; Karp, S.L.; Kraus, M.; Ofner, S.; Li, Q.; Graves, K.L.; Moe, S.M. Prevalence of Calcidiol Deficiency in CKD: A Cross-Sectional Study Across Latitudes in the United States. Am. J. Kidney Dis. 2005, 45, 1026–1033. [Google Scholar] [CrossRef]
- Memon, S.; Alam, A.; Iftikhar, S. Frequency of vitamin D deficiency in chronic kidney disease and its relation with baseline mineral bone markers. J. Pak. Med. Assoc. 2020, 70, 432–436. [Google Scholar] [CrossRef]
- Mucsi, I.; Almási, C.; Deák, G.; Marton, A.; Ambrus, C.; Berta, K.; Lakatos, P.; Szabó, A.; Horváth, C. Serum 25(OH)-vitamin D levels and bone metabolism in patients on maintenance hemodialysis. Clin. Nephrol. 2005, 64, 288–294. [Google Scholar] [CrossRef]
- Ghazali, A.; Fardellone, P.; Pruna, A.; Atik, A.; Achard, J.M.; Oprisiu, R.; Brazier, M.; Remond, A.; Morinière, P.; Garabedian, M.; et al. Is low plasma 25-(OH)vitamin D a major risk factor for hyperparathyroidism and Looser’s zones independent of calcitriol? Kidney Int. 1999, 55, 2169–2177. [Google Scholar] [CrossRef][Green Version]
- Elder, G.J.; Mackun, K. 25-Hydroxyvitamin D Deficiency and Diabetes Predict Reduced BMD in Patients with Chronic Kidney Disease. J. Bone Miner. Res. 2006, 21, 1778–1784. [Google Scholar] [CrossRef]
- Lee, Y.H.; Kim, J.E.; Roh, Y.H.; Choi, H.R.; Rhee, Y.; Kang, D.R.; Lim, S.K. The combination of vitamin D deficiency and mild to moderate chronic kidney disease is associated with low bone mineral density and deteriorated femoral microarchitecture: Results from the KNHANES 2008–2011. J. Clin. Endocrinol. Metab. 2014, 99, 3879–3888. [Google Scholar] [CrossRef] [PubMed]
- Brunerová, L.; Ronová, P.; Verešová, J.; Beranová, P.; Potoèková, J.; Kasalický, P.; Rychlík, I. Osteoporosis and impaired trabecular bone score in hemodialysis patients. Kidney Blood Press. Res. 2016, 41, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.M.; Johnson, D. Vitamin D Therapy (Supplementation) in Early Chronic Kidney Disease. The CARI Guidelines. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.363.4591&rep=rep1&type=pdf (accessed on 17 July 2018).
- Isakova, T.; Nickolas, T.L.; Denburg, M.; Yarlagadda, S.; Weiner, D.E.; Gutiérrez, O.M.; Bansal, V.; Rosas, S.E.; Nigwekar, S.; Yee, J.; et al. KDOQI US Commentary on the 2017 KDIGO Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD). Am. J. Kidney Dis. 2017, 70, 737–751. [Google Scholar] [CrossRef]
- Cozzolino, M.; Ciceri, P.; Galassi, A.; Mangano, M.; Carugo, S.; Capelli, I.; Cianciolo, G. The Key Role of Phosphate on Vascular Calcification. Toxins 2019, 11, 213. [Google Scholar] [CrossRef]
- Mizobuchi, M.; Ogata, H.; Koiwa, F.; Kinugasa, E.; Akizawa, T. Vitamin D and vascular calcification in chronic kidney disease. Bone 2009, 45, S26–S29. [Google Scholar] [CrossRef] [PubMed]
- Vervloet, M.; Cozzolino, M. Vascular calcification in chronic kidney disease: Different bricks in the wall? Kidney Int. 2017, 91, 808–817. [Google Scholar] [CrossRef] [PubMed]
- Barreto, D.V.; Barreto, F.C.; Liabeuf, S.; Temmar, M.; Boitte, F.; Choukroun, G.; Fournier, A.; Massy, Z.A. Vitamin D Affects Survival Independently of Vascular Calcification in Chronic Kidney Disease. Clin. J. Am. Soc. Nephrol. 2009, 4, 1128–1135. [Google Scholar] [CrossRef]
- Oksa, A.; Spustová, V.; Krivosíková, Z.; Gazdíková, K.; Fedelesová, V.; Lajdová, I.; Stefíková, K.; Bernasovská, G.; Zilinská, Z.; Dzúrik, R. Effects of long-term cholecalciferol supplementation on mineral metabolism and calciotropic hormones in chronic kidney disease. Kidney Blood Press. Res. 2008, 31, 322–329. [Google Scholar] [PubMed]
- Marckmann, P.; Agerskov, H.; Thineshkumar, S.; Bladbjerg, E.-M.; Sidelmann, J.J.; Jespersen, J.; Nybo, M.; Rasmussen, L.M.; Hansen, D.; Scholze, A. Randomized controlled trial of cholecalciferol supplementation in chronic kidney disease patients with hypovitaminosis D. Nephrol. Dial. Transplant. 2012, 27, 3523–3531. [Google Scholar] [CrossRef] [PubMed]
- A Alvarez, J.; Law, J.; E Coakley, K.; Zughaier, S.M.; Hao, L.; Salles, K.S.; Wasse, H.; Gutiérrez, O.M.; Ziegler, T.R.; Tangpricha, V. High-dose cholecalciferol reduces parathyroid hormone in patients with early chronic kidney disease: A pilot, randomized, double-blind, placebo-controlled trial. Am. J. Clin. Nutr. 2012, 96, 672–679. [Google Scholar] [CrossRef]
- Yadav, A.K.; Kumar, V.; Kumar, V.; Banerjee, D.; Gupta, K.L.; Jha, V. The Effect of Vitamin D Supplementation on Bone Metabolic Markers in Chronic Kidney Disease. J. Bone Miner. Res. 2017, 33, 404–409. [Google Scholar] [CrossRef]
- Chandra, P.; Binongo, J.N.G.; Ziegler, T.R.; Schlanger, L.E.; Wang, W.; Someren, J.T.; Tangpricha, V. Cholecalciferol (Vitamin D3) Therapy and Vitamin D Insufficiency in Patients with Chronic Kidney Disease: A Randomized Controlled Pilot Study. Endocr. Pr. 2008, 14, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Rucker, D.; Tonelli, M.; Coles, M.G.; Yoo, S.; Young, K.; McMahon, A.W. Vitamin D insufficiency and treatment with oral vitamin D3 in northern-dwelling patients with chronic kidney disease. J. Nephrol. 2009, 22, 75–82. [Google Scholar]
- Zelnick, L.R.; de Boer, I.H.; Kestenbaum, B.R.; Chonchol, M.; Kendrick, J. Comparative effects of cholecalciferol and calcitriol on circulating markers of CKD mineral bone disorder: A randomized clinical trial. Clin. J. Am. Soc. Nephrol. 2018, 13, 927–928. [Google Scholar] [CrossRef]
- Zisman, A.L.; Hristova, M.; Ho, L.T.; Sprague, S.M. Impact of Ergocalciferol Treatment of Vitamin D Deficiency on Serum Parathyroid Hormone Concentrations in Chronic Kidney Disease. Am. J. Nephrol. 2007, 27, 36–43. [Google Scholar] [CrossRef]
- Porter, A.; Gilmartin, C.; Srisakul, U.; Arruda, J.; Akkina, S. Prevalence of 25-OH Vitamin D Deficiency in a Population of Hemodialysis Patients and Efficacy of an Oral Ergocalciferol Supplementation Regimen. Am. J. Nephrol. 2013, 37, 568–574. [Google Scholar] [CrossRef]
- Deville, J.; Thorp, M.L.; Tobin, L.; Gray, E.; Johnson, E.S.; Smith, D.H. Effect of ergocalciferol supplementation on serum parathyroid hormone and serum 25-hydroxyvitamin D in chronic kidney disease. Nephrology 2006, 11, 555–559. [Google Scholar] [CrossRef]
- Al-Aly, Z.; Qazi, R.A.; González, E.A.; Zeringue, A.; Martin, K.J. Changes in Serum 25-Hydroxyvitamin D and Plasma Intact PTH Levels Following Treatment With Ergocalciferol in Patients With CKD. Am. J. Kidney Dis. 2007, 50, 59–68. [Google Scholar] [CrossRef]
- Gravesen, E.; Hofman-Bang, J.; Lewin, E.; Olgaard, K. Ergocalciferol treatment and aspects of mineral homeostasis in patients with chronic kidney disease stage 4–5. Scand. J. Clin. Lab. Investig. 2013, 73, 107–116. [Google Scholar] [CrossRef]
- Del Valle, E.; Negri, A.L.; Fradinger, E.; Canalis, M.; Bevione, P.; Curcelegui, M.; Bravo, M.; Puddu, M.; Marini, A.; Ryba, J.; et al. Weekly high-dose ergocalciferol to correct vitamin D deficiency/insufficiency in hemodialysis patients: A pilot trial. Hemodial. Int. 2014, 19, 60–65. [Google Scholar] [CrossRef]
- Wetmore, J.B.; Kimber, C.; Mahnken, J.D.; Stubbs, J.R. Cholecalciferol v. ergocalciferol for 25-hydroxyvitamin D (25(OH)D) repletion in chronic kidney disease: A randomised clinical trial. Br. J. Nutr. 2016, 116, 2074–2081. [Google Scholar] [CrossRef] [PubMed]
- Mangoo-Karim, R.; Abreu, J.D.S.; Yanev, G.P.; Perez, N.N.; Stubbs, J.R.; Wetmore, J.B. Ergocalciferol versus Cholecalciferol for Nutritional Vitamin D Replacement in CKD. Nephron 2015, 130, 99–104. [Google Scholar] [CrossRef]
- Glendenning, P.; Chew, G.T.; Inderjeeth, C.A.; Taranto, M.; Fraser, W.D. Calculated free and bioavailable vitamin D metabolite concentrations in vitamin D-deficient hip fracture patients after supplementation with cholecalciferol and ergocalciferol. Bone 2013, 56, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Iwamoto, J.; Takeda, T.; Ichimura, S. Effect of combined administration of vitamin D3 and vitamin K2 on bone mineral density of the lumbar spine in postmenopausal women with osteoporosis. J. Orthop. Sci. 2000, 5, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Torbergsen, A.C.; Watne, L.O.; Wyller, T.B.; Frihagen, F.; Strømsøe, K.; Bøhmer, T.; Mowe, M. Vitamin PK and 25(OH)D are independently and synergistically associated with a risk for hip fracture in an elderly population: A case control study. Clin. Nutr. 2015, 34, 101–106. [Google Scholar] [CrossRef]
- Je, S.H.; Joo, N.-S.; Choi, B.-H.; Kim, K.-M.; Kim, B.-T.; Park, S.-B.; Cho, D.-Y.; Kim, K.-N.; Lee, D.-J. Vitamin K Supplement Along with Vitamin D and Calcium Reduced Serum Concentration of Undercarboxylated Osteocalcin While Increasing Bone Mineral Density in Korean Postmenopausal Women over Sixty-Years-Old. J. Korean Med Sci. 2011, 26, 1093–1098. [Google Scholar] [CrossRef]
- Ushiroyama, T.; Ikeda, A.; Ueki, M. Effect of continuous combined therapy with vitamin K2 and vitamin D3 on bone mineral density and coagulofibrinolysis function in postmenopausal women. Maturitas 2002, 41, 211–221. [Google Scholar] [CrossRef]
- Szulc, P.; Chapuy, M.-C.; Meunier, P.; Delmas, P. Serum undercarboxylated osteocalcin is a marker of the risk of hip fracture: A three year follow-up study. Bone 1996, 18, 487–488. [Google Scholar] [CrossRef]
- Lian, J.; Stewart, C.; Puchacz, E.; Mackowiak, S.; Shalhoub, V.; Collart, D.; Zambetti, G.; Stein, G. Structure of the rat osteocalcin gene and regulation of vitamin D-dependent expression. Proc. Natl. Acad. Sci. USA 1989, 86, 1143–1147. [Google Scholar] [CrossRef] [PubMed]
- Miyake, N.; Hoshi, K.; Sano, Y.; Kikuchi, K.; Tadano, K.; Koshihara, Y. 1,25-Dihydroxyvitamin D 3 Promotes Vitamin K 2 Metabolism in Human Osteoblasts. Osteoporos. Int. 2001, 12, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Furie, B.C.; Bouchard, B.A. Vitamin K-dependent biosynthesis of gamma-carboxyglutamic acid. Blood 1999, 93, 1798–1808. [Google Scholar] [CrossRef] [PubMed]
- Price, P.A.; Baukol, S.A. 1,25-Dihydroxyvitamin D3 increases serum levels of the vitamin K-dependent bone protein. Biochem. Biophys. Res. Commun. 1981, 99, 928–935. [Google Scholar] [CrossRef]
- Szulc, P.; Delmasm, P.D. Influence of vitamin D and retinoids on the gammacarboxylation of osteocalcin in human osteosar-coma MG63 cells. Bone 1996, 19, 615–620. [Google Scholar] [CrossRef]
- Goltzman, D. Functions of vitamin D in bone. Histochem. Cell Biol. 2018, 149, 305–312. [Google Scholar] [CrossRef]
- Koshihara, Y.; Hoshi, K.; Ishibashi, H.; Shiraki, M. Vitamin K2 promotes 1α,25(OH)2 vitamin D3-induced mineralization in human periosteal osteoblasts. Calcif. Tissue Int. 1996, 59, 466–473. [Google Scholar] [CrossRef]
- Buranasinsup, S.; Bunyaratavej, N. The Intriguing Correlation between Undercarboxylated Osteocalcin and Vitamin D. J. Med Assoc. Thail. 2015, 98, 16–20. [Google Scholar]
- Van Ballegooijen, A.J.; Beulens, J.W.J.; Schurgers, L.J.; De Koning, E.J.; Lips, P.; Van Schoor, N.M.; Vervloet, M.G. Effect of 6-Month Vitamin D Supplementation on Plasma Matrix Gla Protein in Older Adults. Nutrients 2019, 11, 231. [Google Scholar] [CrossRef]
- Clowes, J.A.; Riggs, B.L.; Khosla, S. The role of the immune system in the pathophysiology of osteoporosis. Immunol. Rev. 2005, 208, 207–227. [Google Scholar] [CrossRef]
- Reddi, K.; Henderson, B.; Meghji, S.; Wilson, M.; Poole, S.; Hopper, C.; Harris, M.; Hodges, S.J. Interleukin 6 production by lipopolysaccharide-stimulated human fibroblasts is potently inhibited by naphthoquinone (vitamin K) compounds. Interleukin 6 production by lipopolysaccharide-stimulated human fibroblasts is potently inhibited by naphthoquinone (vitamin K) com-pounds. Cytokine 1995, 7, 287–290. [Google Scholar] [PubMed]
- Koshihara, Y.; Hoshi, K.; Shiraki, M. Vitamin K2 (menatetrenone) inhibits prostaglandin synthesis in cultured human osteoblast-like periosteal cells by inhibiting prostaglandin H synthase activity. Biochem. Pharmacol. 1993, 46, 1355–1362. [Google Scholar] [CrossRef]
- Ohsaki, Y.; Shirakawa, H.; Hiwatashi, K.; Furukawa, Y.; Mizutani, T.; Komai, M. Vitamin K suppresses lipopolysaccha-ride-induced inflammation in the rat. Biosci. Biotechnol. Biochem. 2006, 70, 926–932. [Google Scholar] [CrossRef]
- Shea, M.K.; Booth, S.L.; Massaro, J.M.; Jacques, P.F.; D’Agostino, R.B., Sr.; Dawson-Hughes, B.; Ordovas, J.M.; O’Donnell, C.J.; Kathiresan, S.; Keaney, J.F., Jr.; et al. Vitamin K and vitamin D status: Associations with inflammatory markers in the Framingham Offspring Study. Am. J. Epidemiol. 2008, 167, 313–320. [Google Scholar] [CrossRef]
- van Etten, E.; Mathieu, C. Immunoregulation by 1,25-dihydroxyvitamin D3: Basic concepts. J. Steroid. Biochem. Mol. Biol. 2005, 97, 93–101. [Google Scholar] [CrossRef]
- Inanir, A.; Özoran, K.; Tutkak, H.; Mermerci, B. The Effects of Calcitriol Therapy on Serum Interleukin-1, Interleukin-6 and Tumour Necrosis Factor-α Concentrations in Post-menopausal Patients with Osteoporosis. J. Int. Med Res. 2004, 32, 570–582. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Assem, M.; Tay, J.C.; Watkins, P.B.; Blumberg, B.; Schuetz, E.G.; Thummel, K.E. Steroid and xenobiotic receptor and vitamin D receptor crosstalk mediates CYP24 expression and drug-induced osteomalacia. J. Clin. Investig. 2006, 116, 1703–1712. [Google Scholar] [CrossRef]
- Hosseinpour, F.; Ellfolk, M.; Norlin, M.; Wikvall, K. Phenobarbital suppresses vitamin D3 25-hydroxylase expression: A po-tential new mechanism for drug-induced osteomalacia. Biochem. Biophys. Res. Commun. 2007, 357, 603–607. [Google Scholar] [CrossRef]
- Hara, K.; Akiyama, Y.; Tomiuga, T.; Kobayashi, M.; Nakamura, T.; Tajima, T. Influence of vitamin D3 on inhibitory effect of vitamin K2 on bone loss in ovariectomized rats. Folia Pharmacol. Jpn. 1994, 104, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, A.; Higashi, S.; Masaki, T.; Saito, M.; Ito, M.; Ikeda, S.; Nakamura, T. A Comparison of Alfacalcidol and Menatetrenone for the Treatment of Bone Loss in an Ovariectomized Rat Model of Osteoporosis. Calcif. Tissue Int. 2002, 71, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Omelka, R.; Martiniakova, M.; Svik, K.; Slovak, L.; Payer, J.; Oppenbergerova, I.; Kovacova, V.; Babikova, M.; Soltesova-Prnova, M. The effects of eggshell calcium (Biomin H®) and its combinations with alfacalcidol (1α-hydroxyvitamin D3) and menaquinone-7 (vitamin K2) on ovariectomy-induced bone loss in a rat model of osteoporosis. J. Anim. Physiol. Anim. Nutr. 2020. [Google Scholar] [CrossRef] [PubMed]
- Iwamoto, J.; Yeh, J.K.; Takeda, T.; Ichimura, S.; Sato, Y. Comparative effects of vitamin K and vitamin D supplementation on prevention of osteopenia in calcium-deficient young rats. Bone 2003, 33, 557–566. [Google Scholar] [CrossRef]
- Kuang, X.; Liu, C.; Guo, X.-F.; Li, K.; Deng, Q.; Li, D. The combination effect of vitamin K and vitamin D on human bone quality: A meta-analysis of randomized controlled trials. Food Funct. 2020, 11, 3280–3297. [Google Scholar] [CrossRef]

| Reference | Model | Dose | Results |
|---|---|---|---|
| Vitamin K | |||
| [79] | MC3T3‑E1 osteoblasts cell line | VK2 (10−8–10−3 M) for 1–5 days VK2 (10−5, 10−6 and 10−7 M) for 24 h on days 1, 3, 5 and 7 | VK2 promoted osteoblast differentiation and mineralization, induced autophagy in osteoblasts |
| [28] | The human cell lines HOS, MG-63, Saos-2, LS180, and HeLa | VK2 | VK2 activates SXR and induces expression of the SXR target gene; VK2 treatment of osteosarcoma cells increased mRNA levels of OB: ALP, OPG, OPN, and MGP |
| [85] | Bone marrow cells were isolated from male Wistar rats (3 weeks old) | MK-7 (10−8–10−5 M) | MK-7 can inhibit osteoclastic bone resorption; MK-7 has an inhibitory effect on the bone-resorbing factors-induced decrease in bone calcium content |
| Vitamin D | |||
| [78] | Bone marrow cells from the femur from elderly patients with type II osteoporosis | 10 nM 1,25D and 0.5, 1.0, 2.5, 10 µM MK-4 or VK1 | MK-4 and VK1 inhibited 1,25D-induced osteoclast formation and promoted the differentiation of bone marrow cells; MK-4 and VK1 decreased the RANKL and enhanced OPG |
| [86] | iliac crest bone biopsy samples from 11 paediatric dialysis patients | 8 months of doxercalciferol therapy (an average of 19.3 ± 3.8 mcg of doxercalciferol per week) | 1,25D increases the maturation of OBs lineage cells, stimulates osteocyte apoptosis and increases RANKL/OPG expression, increases the number of osteocytes |
| [87] | hMSCs from 53 subjects scheduled for hip arthroplasty | 10 nM 1,25D | 1,25D stimulated the differentiation of hMSCs to OBs; greater stimulation of in vitro osteoblast differentiation by 1,25D in hMSCs from younger subjects, and who had serum 25D ≤ 20 ng/mL |
| [88] | Primary OB cells, with a pre-osteoblastic phenotype from healthy male donors | 1,25D (10−8 M) | 1,25D increased differentiation, mineralization and survival of osteoblasts |
| [89] | Monocytes from blood of healthy adult volunteer donors | VD (25D-100 nM and 1,25D-5 nM) | 1,25D inhibits osteoclastogenesis |
| [90] | The tibia from 4-week-old littermate C57BL/6J mice | 1,25D can directly (in absence of RANKL) suppress OC precursor autophagy, which negatively regulates the proliferation of these cells; 1,25D can indirectly upregulate the autophagy response of OC precursors, thereby enhancing OC formation in the presence of RANKL | |
| Vitamin D and Vitamin K | |||
| [83] | Primary osteoblasts harvested from the iliac crests of C57BL/KsJ lean (+/+) and obese/diabetic (db/db) mice | VK2 (10 nM) and 1,25D (10 nM) alone and in combination | The combined use of VK2 and 1,25D enhanced calcium deposits formation in OBs and increased the levels of bone anabolic markers and bone formation transcription factors |
| Reference | Model | Dose | Results |
|---|---|---|---|
| Vitamin K | |||
| [138] | n = 30, male Sprague–Dawley rats; assigned to three groups: sham operation (control), 5/6 nephrectomy and 5/6 nephrectomy + oral VK2 | VK2 (menaquinone-4, menatetrenone): 30 mg/kg, 5 days/week | The administration of VK2 increased cortical bone strength without changing bone mineral density (BMD) and improved renal function. |
| [140] | n = 25, OVX female Sprague–Dawley rats assigned to five groups: the sham, ovariectomy (OVX), VK, TPTD and VK + TPTD | VK (menaquinone-4): 30 mg/kg/day TPTD: 30 µg/kg, 3 times/week | The coadministration of VK2 and TPTD improved OB function and the OB surface, and increased Gla-OC serum levels, improved the BMD and bone strength of the femur. |
| [142] | n = 42, male C57BL/6J mice divided into six groups: normal diet, normal diet + VK1, normal diet + VK2, 45% high-fat diet, 45% high-fat diet + VK1, a 45% high-fat diet + VK2 | VK1 and VK2: 200 mg/1000 g | VK administration in high-fat diet mice resulted in an increase in bone formation and a reduction in bone resorption. |
| [143] | n = 30, male Sprague–Dawley rats assigned to five groups: nonsuspended group, tail-suspended group with vehicle alone, tail-suspended group with VK2, tail suspended group with bisphosphonate, tail-suspended group with combination of bisphosphonate and VK2 | Bisphosphonate (incadronate): 0.1 mgP/kg body weight VK2: 24 mg/kg body weight/day | The effect of combined use of VK2 and bisphosphonate showed increased bone volume without supressing bone turnover. |
| [146] | n = 59, female ICR mice after sham-operated or ovariectomized; OVX divided into six groups: treated with risedronate (R), MK-4 (K), R+K, either the treatment was withdrawn or switched to K or R in the case of R and K | Risedronate: 0.25 mg/kg/day VK2: 100 μg MK-4/kg/day | Prior 8-week treatment with MK-4 followed by the 8-week risedronate significantly increased femur strength. |
| Vitamin D | |||
| [147] | n = 45, rats assigned to sham-operation or 5/6 nephrectomy surgery (NTX): divided into two groups: the untreated NTX and NTX + paricalcitol. | 1500 IU/kg VD; for the 12-week: paricalcitol:100 ng/rat, 3 times per week | Paricalcitol efficiently ameliorates advanced renal insufficiency induced loss of mineral and mechanical competence of rat bones, prevented the renal impairment associated decrease in vBMD at the femoral neck and cBMD at the femoral midshaft, and restored bone strength at the femoral neck |
| [148] | n = 49, female Sprague–Dawley rats after 7/8 nephrectomy and CKD + OVX group; CKD + OVX were divided into 6 groups: placebo, E2 (10 μg/kg/day), E2 (30 μg/kg/day), calcitriol (10 ng/kg/day), E2 (10 μg/kg/day) + calcitriol, E2 (30 μg/kg/day) + calcitriol | Calcitriol:10 ng/kg BW, 5 times per week for 8 weeks | Calcitriol reduces bone loss but also improves trabecular connectivity; combined treatment with E2-30 + calcitriol was capable of achieving normal trabecular bone volume, trabecular remodeling, and connectivity |
| [149] | n = 36, 5/6 nephrectomized male Wistar rats divided into groups: control, Nx-Int D, Nx-Daily D, Ns-Phos | Calcium: 1.2%, phosphate: 1.2%, VD: 0.5 µg/kg 3 times per week | Calcitriol enhanced chondrocyte maturation and restoration of the growth plate architecture; calcitriol increased PTH/PTHrP receptor and d markers of chondrocyte differentiation; daily and intermittent calcitriol had similar effects on endochondral bone growth in phosphorus-loaded rats with renal failure |
| Vitamin K and Vitamin D | |||
| [144] | n = 60, female Sprague–Dawley rats after OVX or sham operation; OVX rats were classified into three groups: a VK alone, a VD alone, and combination of VK and VD | VK (menaquinone): 48 mg/100 g diet VD: 0.16 mg/ 100 g diet | VK and VD may have a synergistic effect on reducing bone loss |
| Reference | Population | Outcome Measure | Main Findings |
|---|---|---|---|
| Vitamin K | |||
| [162] | n = 468, Adult patients with ESRD referred for single kidney transplant | VK, BMD, parameters of mineral metabolism | Poor vitamin K status is highly prevalent among patients with ESRD and associates with inflammation and low aBMD |
| [163] | n = 20, patients with chronic glomerulonephritis | VK, markers of bone metabolism | MK-4 supplementation suppressed bone loss |
| [37] | n = 141, patients with CKD stages 1–4 | PIVKA-II | Subclinical VK deficiency is detectable at just the point in terms of loss of renal function with VC |
| [160] | n = 68, HD patients | VK1, OC, ucOC, iPTH | Suboptimal VK nutriture in HD patients is associated both with increased bone fracture risk and with a high prevalence of hyperparathyroidism |
| Vitamin D | |||
| [164] | n = 104, HD patients | VD, transiliac bone biopsy, ALP, iPTH | PTH serum levels are equally elevated in low and high 25D patients; calcitriol levels are constantly low; 25D deficiency resulted in mineralization and bone formation defect; the optimal level of 25D appears to be in the order of 20 to 40 ng/mL |
| [165] | n = 144, HD patients | VD, iPTH, bone densitometry | Increased bone fragility in HD patients is associated with VD deficiency and relative hypoparathyroidism in addition to reduced BMD at the radius |
| [166] | n = 610, elderly women | VD, BMD | Combined calcium and vitamin D3 supplementation was effective in reducing the rate of BMD loss in women with moderate CKD |
| [167] | n = 120, patients with stages 1–4 CKD | VD, BMD, OC, NTx, FGF-23 | Daily (2000 IU/d) and monthly (40,000 IU/month) VD supplementation for six months in adults with DM and CKD was safe, and it resulted in equivalent adherence and improvements in overall VD status, but only modest changes in markers of bone health |
| [168] | n = 47, CKD patients in stage 3 and 4 | PTH, calcium, creatinine, VD | No statistically significant difference between the two treatments: cholecalciferol (4000 IU/d × 1 month, then 2000 IU/d) to doxercalciferol (1 μg/d) in lowering PTH |
| Vitamin K and Vitamin D | |||
| [3] | n = 172, patients with stage 3 to 5 CKD | VK, VD, ucOC | Proteinuria was associated with both a suboptimal VD status as well as worse peripheral VK status; high serum ucOC levels were positively associated with phosphate and PTH, and inversely with 25D levels |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziemińska, M.; Sieklucka, B.; Pawlak, K. Vitamin K and D Supplementation and Bone Health in Chronic Kidney Disease—Apart or Together? Nutrients 2021, 13, 809. https://doi.org/10.3390/nu13030809
Ziemińska M, Sieklucka B, Pawlak K. Vitamin K and D Supplementation and Bone Health in Chronic Kidney Disease—Apart or Together? Nutrients. 2021; 13(3):809. https://doi.org/10.3390/nu13030809
Chicago/Turabian StyleZiemińska, Marta, Beata Sieklucka, and Krystyna Pawlak. 2021. "Vitamin K and D Supplementation and Bone Health in Chronic Kidney Disease—Apart or Together?" Nutrients 13, no. 3: 809. https://doi.org/10.3390/nu13030809
APA StyleZiemińska, M., Sieklucka, B., & Pawlak, K. (2021). Vitamin K and D Supplementation and Bone Health in Chronic Kidney Disease—Apart or Together? Nutrients, 13(3), 809. https://doi.org/10.3390/nu13030809






