Association of Hemoglobin and Hematocrit Levels during Pregnancy and Maternal Dietary Iron Intake with Allergic Diseases in Children: The Japan Environment and Children’s Study (JECS)
Abstract
:1. Introduction
2. Methods
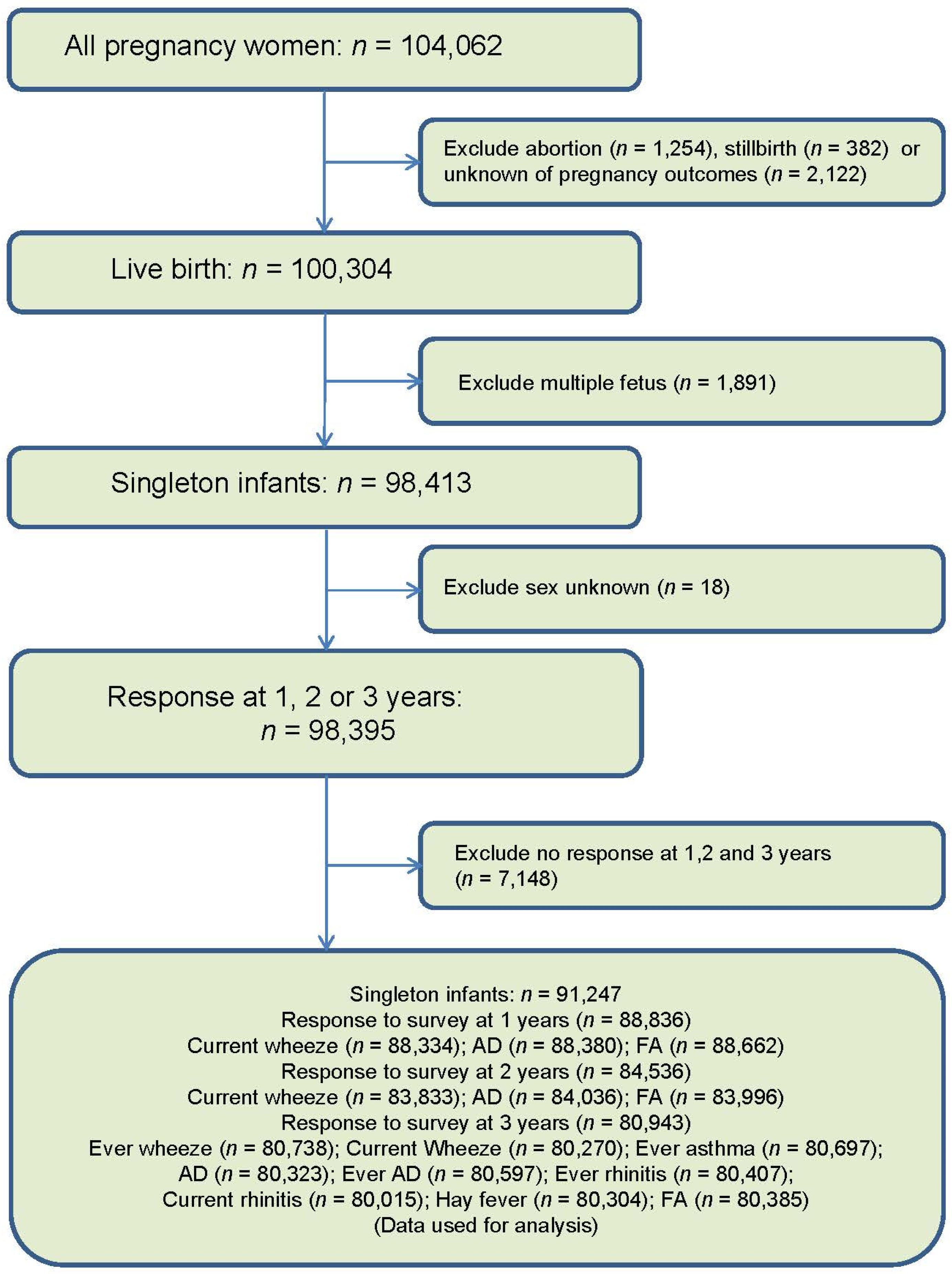
2.1. Study Design
2.2. Data Collection
2.3. Allergies in Children
- Current wheeze: Caregiver’s report of wheeze in the past 12 months.
- Ever wheeze: Caregiver’s report of wheeze ever.
- Ever asthma: A positive answer to the question “Has your children ever had asthma?”
- Ever rhinitis: Caregiver’s report of sneezing or runny or congested nose ever when the child did not have cold or flu.
- Current rhinitis: Sneezing or a runny or congested nose accompanied by itchy when the child did not have cold or flu in the past 12 months.
- Ever atopic dermatitis: Caregiver’s report of AD ever.
- Current atopic dermatitis: Caregiver’s report of an itchy rash at any time in the past 12 months that occurred at the folds of the elbows, behind the knees, in front of the ankles, under the buttocks, or around the neck, ears, or eyes.
- Hay fever: Caregiver’s report of hay fever ever.
- Food allergy: Caregiver’s report of any allergic symptoms (urticaria, swelling, sneezing, runny nose, itchiness of the mouth, wheezing, cough, vomiting, abdominal pains, fainting, or becoming unconscious within 3 h of food intake).
2.4. Hemoglobin, Hematocrit Concentration and Dietary Iron Intake during Pregnancy
2.5. Covariates in the Models
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
3.2. Effect of Low Hemoglobin and Hematocrit in Pregnancy on Allergy in Offspring
3.3. Role of Maternal Dietary Iron Intake on Allergy in Offspring
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- A Stevens, G.; Finucane, M.M.; De-Regil, L.M.; Paciorek, C.J.; Flaxman, S.R.; Branca, F.; Peña-Rosas, J.P.; A Bhutta, Z.; Ezzati, M. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: A systematic analysis of population-representative data. Lancet Glob. Heal. 2013, 1, e16–e25. [Google Scholar] [CrossRef] [Green Version]
- International Nutritional Anemia Consultative Group (INACG) WHOW, United Nations Childrens Fund (UNICEF). Guidelines for the Use of Iron Supplements to Prevent and Treat Iron Defciency Anemia; ILSI Press: Washington, DC, USA, 1998. [Google Scholar]
- Milman, N.; Byg, K.-E.; Agger, A.O. Hemoglobin and erythrocyte indices during normal pregnancy and postpartum in 206 women with and without iron supplementation. Acta Obstet. et Gynecol. Scand. 2000, 79, 89–98. [Google Scholar] [CrossRef]
- Morikawa, E.; Sasaki, M.; Yoshida, K.; Adachi, Y.; Odajima, H.; Akasawa, A. Nationwide survey of the prevalence of wheeze, rhino-conjunctivitis, and eczema among Japanese children in 2015. Allergol. Int. 2020, 69, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Bousquet, J.; Khaltaev, N. Global Surveillance, Prevention and Control of Chronic Respiratory Diseases: A Comprehensive Approach. 2007. World Health Organization. Available online: http://www.whoint/gard/publications/GARD Book 2007.pdf (accessed on 20 January 2021).
- Bønnelykke, K.; Ober, C. Leveraging gene-environment interactions and endotypes for asthma gene discovery. J. Allergy Clin. Immunol. 2016, 137, 667–679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pawankar, R. Allergic diseases and asthma: A global public health concern and a call to action. World Allergy Organ. J. 2014, 7, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Briana, D.D.; Malamitsi-Puchner, A. Small for gestational age birth weight: Impact on lung structure and function. Paediatr. Respir. Rev. 2013, 14, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Duijts, L. Fetal and infant origins of asthma. Eur. J. Epidemiology 2012, 27, 5–14. [Google Scholar] [CrossRef] [Green Version]
- Yip, R. Significance of an abnormally low or high hemoglobin concentration during pregnancy: Special consideration of iron nutrition. Am. J. Clin. Nutr. 2000, 72, 272S–279S. [Google Scholar] [CrossRef] [PubMed]
- Welten, M.; Gaillard, R.; Hofman, A.; De Jonge, L.; Jaddoe, V. Maternal haemoglobin levels and cardio-metabolic risk factors in childhood: The Generation R Study. BJOG Int. J. Obstet. Gynaecol. 2014, 122, 805–815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steer, P.; Alam, M.A.; Wadsworth, J.; Welch, A. Relation between maternal haemoglobin concentration and birth weight in different ethnic groups. BMJ 1995, 310, 489–491. [Google Scholar] [CrossRef] [Green Version]
- Stangret, A.; Wnuk, A.; Szewczyk, G.; Pyzlak, M.; Szukiewicz, D. Maternal hemoglobin concentration and hematocrit values may affect fetus development by influencing placental angiogenesis. J. Matern. Neonatal Med. 2016, 30, 199–204. [Google Scholar] [CrossRef]
- Duijts, L.; Reiss, I.K.; Brusselle, G.; De Jongste, J.C. Early origins of chronic obstructive lung diseases across the life course. Eur. J. Epidemiology 2014, 29, 871–885. [Google Scholar] [CrossRef]
- Maritz, G.S.; Morley, C.J.; Harding, R. Early developmental origins of impaired lung structure and function. Early Hum. Dev. 2005, 81, 763–771. [Google Scholar] [CrossRef]
- Dekker, H.T.D.; der Voort, A.M.S.-V.; de Jongste, J.C.; Anessi-Maesano, I.; Arshad, S.H.; Barros, H.; Beardsmore, C.S.; Bisgaard, H.; Phar, S.C.; Craig, L.; et al. Early growth characteristics and the risk of reduced lung function and asthma: A meta-analysis of 25,000 children. J. Allergy Clin. Immunol. 2016, 137, 1026–1035. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harding, R.; Maritz, G. Maternal and fetal origins of lung disease in adulthood. Semin. Fetal Neonatal Med. 2012, 17, 67–72. [Google Scholar] [CrossRef]
- De Jesus, S.M.C.B.P.; Dekker, H.T.D.; De Jongste, J.C.; Reiss, I.K.; Steegers, E.A.; Jaddoe, V.W.V.; Duijts, L. Maternal hemoglobin and hematocrit levels during pregnancy and childhood lung function and asthma. The Generation R Study. Pediatr. Pulmonol. 2018, 53, 130–137. [Google Scholar] [CrossRef] [Green Version]
- Kindlund, K.; Thomsen, S.F.; Stensballe, L.G.; Skytthe, A.; Kyvik, K.O.; Backer, V.; Bisgaard, H. Birth weight and risk of asthma in 3-9-year-old twins: Exploring the fetal origins hypothesis. Thorax 2010, 65, 146–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Der Voort, A.M.S.-V.; Arends, L.R.; de Jongste, J.C.; Annesi-Maesano, I.; Arshad, S.H.; Barros, H.; Basterrechea, M.; Bisgaard, H.; Chatzi, L.; Corpeleijn, E.; et al. Preterm birth, infant weight gain, and childhood asthma risk: A meta-analysis of 147,000 European children. J. Allergy Clin. Immunol. 2014, 133, 1317–1329. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sottile, R.; Federico, G.; Garofalo, C.; Tallerico, R.; Faniello, M.C.; Quaresima, B.; Cristiani, C.M.; Di Sanzo, M.; Cuda, G.; Ventura, V.; et al. Iron and Ferritin Modulate MHC Class I Expression and NK Cell Recognition. Front. Immunol. 2019, 10, 224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaheen, S.; Newson, R.; Henderson, A.; Emmett, P.; Sherriff, A.; Cooke, M.; ALSPAC Study Team. Umbilical cord trace elements and minerals and risk of early childhood wheezing and eczema. Eur. Respir. J. 2004, 24, 292–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nwaru, B.I.; Hayes, H.; Gambling, L.; Craig, L.C.A.; Allan, K.; Prabhu, N.; Turner, S.W.; McNeill, G.; Erkkola, M.; Seaton, A.; et al. An exploratory study of the associations between maternal iron status in pregnancy and childhood wheeze and atopy. Br. J. Nutr. 2014, 112, 2018–2027. [Google Scholar] [CrossRef] [Green Version]
- Tromp, I.I.; Gaillard, R.; Jong, J.C.K.-D.; Steegers, E.A.; Jaddoe, V.W.; Duijts, L.; Hofman, A.; De Jongste, J.C.; Moll, H.A. Maternal hemoglobin levels during pregnancy and asthma in childhood: The Generation R Study. Ann. Allergy Asthma Immunol. 2014, 112, 263–265. [Google Scholar] [CrossRef]
- Kawamoto, T.; Nitta, H.; Murata, K.; Toda, E.; Tsukamoto, N.; Hasegawa, M.; Yamagata, Z.; Kayama, F.; Kishi, R.; Ohya, Y.; et al. Rationale and study design of the Japan environment and children’s study (JECS). BMC Public Health 2014, 14, 25. [Google Scholar] [CrossRef] [Green Version]
- Saito, M.; Yamamoto-Hanada, K.; Pak, K.; Ayabe, T.; Mezawa, H.; Ishitsuka, K.; Konishi, M.; Yang, L.; Matsumoto, K.; Saito, H.; et al. Having small-for-gestational-age infants was associated with maternal allergic features in the JECS birth cohort. Allergy 2018, 73, 1908–1911. [Google Scholar] [CrossRef]
- Yamamoto-Hanada, K.; Ishitsuka, K.; Pak, K.; Saito, M.; Ayabe, T.; Mezawa, H.; Konishi, M.; Yang, L.; Matsumoto, K.; Saito, H.; et al. Allergy and mental health among pregnant women in the Japan Environment and Children’s Study. J. Allergy Clin. Immunol. Pract. 2018, 6, 1421–1424. [Google Scholar] [CrossRef] [PubMed]
- Japan Environment and Children’s Study (JECS) Study Protocol. Available online: https://www.env.go.jp/chemi/ceh/en/about/advanced/material/jecs-study_protocol_14_en.pdf (accessed on 20 January 2021).
- Japan Environment and Children’s Study (JECS) Sub-Cohort Study Protocol. Available online: https://www.env.go.jp/chemi/ceh/en/about/advanced/material/jecs-sub-cohort_study_protocol_101-en.pdf (accessed on 20 January 2021).
- Asher, M.I.; Keil, U.; Anderson, H.R.; Beasley, R.; Crane, J.; Martinez, F.; Mitchell, E.A.; Pearce, N.; Sibbald, B.; Stewart, A.W.; et al. International study of asthma and allergies in childhood (ISAAC): Rationale and methods. Eur. Respir. J. 1995, 8, 483–491. [Google Scholar] [CrossRef] [PubMed]
- Weiland, S.; Björkstén, B.; Brunekreef, B.; Cookson, W.; Von Mutius, E.; Strachan, D. Phase II of the International Study of Asthma and Allergies in Childhood (ISAAC II): Rationale and methods. Eur. Respir. J. 2004, 24, 406–412. [Google Scholar] [CrossRef]
- Ellwood, P.; Asher, M.I.; Beasley, R.; Clayton, T.O.; Stewart, A.W.; ISAAC Steering Committee. The international study of asthma and allergies in childhood (ISAAC): Phase three rationale and methods. Int. J. Tuberc. Lung Dis. 2005, 9, 10–16. [Google Scholar] [PubMed]
- Yokoyama, Y.; Takachi, R.; Ishihara, J.; Ishii, Y.; Sasazuki, S.; Sawada, N.; Shinozawa, Y.; Tanaka, J.; Kato, E.; Kitamura, K.; et al. Validity of Short and Long Self-Administered Food Frequency Questionnaires in Ranking Dietary Intake in Middle-Aged and Elderly Japanese in the Japan Public Health Center-Based Prospective Study for the Next Generation (JPHC-NEXT) Protocol Area. J. Epidemiology 2016, 26, 420–432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Willett, W.C. Implications of total energy intake for epidemiologic studies of breast and large-bowel cancer. Am. J. Clin. Nutr. 1987, 45, 354–360. [Google Scholar] [CrossRef]
- Buuren, S.V.; Groothuis-Oudshoorn, K. MICE: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef] [Green Version]
- Rothman, K.J. No adjustments are needed for multiple comparisons. Epidemiology 1990, 1, 43–46. [Google Scholar] [CrossRef] [Green Version]
- Triche, E.W.; Lundsberg, L.S.; Wickner, P.G.; Belanger, K.; Leaderer, B.P.; Bracken, M.B. Association of maternal anemia with increased wheeze and asthma in children. Ann. Allergy Asthma Immunol. 2011, 106, 131–139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harju, M.; Pekkanen, J.; Heinonen, S.; Keski-Nisula, L. Maternal anemia during pregnancy and slightly higher risk of asthma in male offspring. J. Obstet. Gynaecol. Res. 2018, 44, 614–622. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, M.; Abernathy, J.; Juul, S.; Short, V.; Derman, R. Prevalence of iron deficiency in first trimester, nonanemic pregnant women. J. Matern. Neonatal Med. 2021, 34, 1002–1005. [Google Scholar] [CrossRef] [PubMed]
- Milman, N. Serum ferritin in Danes: Studies of iron status from infancy to old age, during blood donation and pregnancy. Int. J. Hematol. 1996, 63, 103–135. [Google Scholar] [CrossRef]
- Allen, L.H. Anemia and iron deficiency: Effects on pregnancy outcome. Am. J. Clin. Nutr. 2000, 71, 1280S–1284S. [Google Scholar] [CrossRef]
- Jaime-Perez, J.C.; Herrera-Garza, J.L.; Gomez-Almaguer, D. Sub-Optimal Fetal Iron Acquisition under a Maternal Environment. Arch. Med. Res. 2005, 36, 598–602. [Google Scholar] [CrossRef]
- Alwan, N.A.; Cade, J.E.; Greenwood, D.C.; Deanfield, J.; Lawlor, D.A. Associations of Maternal Iron Intake and Hemoglobin in Pregnancy with Offspring Vascular Phenotypes and Adiposity at Age 10: Findings from the Avon Longitudinal Study of Parents and Children. PLoS ONE 2014, 9, e84684. [Google Scholar] [CrossRef] [Green Version]
| Allergic Outcomes | Model 1 † | Model 2 ‡ | Model 1 †,$ | Model 2 ‡,$ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ORs | 95% CI | ORs | 95% CI | ORs | 95% CI | ORs | 95% CI | ||||||
| Lower | Upper | Lower | Upper | Lower | Upper | Lower | Upper | ||||||
| Hemoglobin (g/dL) | |||||||||||||
| <11 vs. ≥11 | Ever wheeze | 0.98 | 0.94 | 1.03 | 0.97 | 0.93 | 1.02 | 1.03 | 0.97 | 1.10 | 1.04 | 0.97 | 1.12 |
| Current wheeze | 1.00 | 0.94 | 1.05 | 1.01 | 0.95 | 1.07 | 1.02 | 0.94 | 1.10 | 1.04 | 0.96 | 1.13 | |
| Ever asthma | 0.95 | 0.89 | 1.02 | 0.95 | 0.89 | 1.03 | 1.00 | 0.90 | 1.11 | 1.01 | 0.91 | 1.13 | |
| AD | 0.99 | 0.93 | 1.05 | 0.99 | 0.93 | 1.06 | 0.95 | 0.87 | 1.04 | 0.98 | 0.89 | 1.07 | |
| Ever AD | 1.01 | 0.95 | 1.08 | 1.02 | 0.95 | 1.10 | 1.03 | 0.94 | 1.13 | 1.07 | 0.97 | 1.18 | |
| Ever rhinitis | 1.03 | 0.99 | 1.08 | 1.05 | 1.00 | 1.10 | 1.09 | 1.02 | 1.16 | 1.10 | 1.03 | 1.18 | |
| Current rhinitis | 1.03 | 0.98 | 1.08 | 1.05 | 1.00 | 1.10 | 1.10 | 1.03 | 1.18 | 1.12 | 1.04 | 1.20 | |
| Hay fever | 1.05 | 0.94 | 1.17 | 1.07 | 0.96 | 1.20 | 1.05 | 0.90 | 1.23 | 1.06 | 0.90 | 1.24 | |
| FA | 1.01 | 0.93 | 1.09 | 1.02 | 0.94 | 1.11 | 1.01 | 0.90 | 1.13 | 1.03 | 0.92 | 1.16 | |
| Hematocrit (%) | |||||||||||||
| <33 vs. ≥33 | Ever wheeze | 0.96 | 0.92 | 1.01 | 0.96 | 0.91 | 1.01 | 1.01 | 0.94 | 1.08 | 1.02 | 0.95 | 1.10 |
| Current wheeze | 0.98 | 0.92 | 1.04 | 1.00 | 0.94 | 1.06 | 1.01 | 0.92 | 1.10 | 1.03 | 0.95 | 1.13 | |
| Ever asthma | 0.94 | 0.87 | 1.01 | 0.95 | 0.88 | 1.03 | 0.96 | 0.86 | 1.07 | 0.99 | 0.88 | 1.11 | |
| AD | 0.99 | 0.92 | 1.06 | 0.99 | 0.92 | 1.06 | 0.98 | 0.89 | 1.07 | 1.01 | 0.92 | 1.12 | |
| Ever AD | 1.01 | 0.94 | 1.08 | 1.03 | 0.96 | 1.10 | 1.04 | 0.94 | 1.15 | 1.08 | 0.98 | 1.20 | |
| Ever rhinitis | 1.04 | 0.99 | 1.09 | 1.06 | 1.01 | 1.11 | 1.12 | 1.05 | 1.20 | 1.13 | 1.05 | 1.21 | |
| Current rhinitis | 1.03 | 0.98 | 1.08 | 1.05 | 1.00 | 1.10 | 1.11 | 1.04 | 1.19 | 1.12 | 1.04 | 1.20 | |
| Hay fever | 1.07 | 0.95 | 1.19 | 1.09 | 0.97 | 1.22 | 1.17 | 1.00 | 1.38 | 1.19 | 1.01 | 1.40 | |
| FA | 1.02 | 0.93 | 1.11 | 1.02 | 0.94 | 1.12 | 1.01 | 0.90 | 1.13 | 1.02 | 0.90 | 1.15 | |
| Allergic Outcomes | Model 1 † | Model 2 ‡ | ||||
|---|---|---|---|---|---|---|
| ORs | 95% CI | ORs | 95% CI | |||
| Lower | Upper | Lower | Upper | |||
| Hemoglobin (<11 g/dL vs. ≥11 g/dL) | ||||||
| Current wheeze | 1.00 | 0.97 | 1.04 | 0.99 | 0.95 | 1.03 |
| AD | 1.01 | 0.97 | 1.06 | 1.02 | 0.97 | 1.07 |
| FA | 0.96 | 0.91 | 1.01 | 0.97 | 0.92 | 1.02 |
| Hematocrit (<33% vs. ≥33%) | ||||||
| Current wheeze | 0.98 | 0.94 | 1.02 | 0.98 | 0.94 | 1.02 |
| AD | 1.02 | 0.97 | 1.07 | 1.02 | 0.97 | 1.07 |
| FA | 0.97 | 0.92 | 1.03 | 0.97 | 0.92 | 1.03 |
| Allergic Outcomes | Energy Adjusted Maternal Dietary Iron Intake | Model 1 † | Model 2 ‡ | ||||
|---|---|---|---|---|---|---|---|
| ORs | 95% CI | ORs | 95% CI | ||||
| Lower | Upper | Lower | Upper | ||||
| Ever wheeze | Q1 | 1.00 | 0.95 | 1.05 | 0.99 | 0.95 | 1.04 |
| Q2 | 0.99 | 0.95 | 1.04 | 0.99 | 0.94 | 1.04 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 1.01 | 0.96 | 1.06 | 1.01 | 0.96 | 1.06 | |
| Q5 | 1.00 | 0.95 | 1.05 | 1.02 | 0.97 | 1.07 | |
| Current wheeze | Q1 | 0.99 | 0.94 | 1.05 | 0.99 | 0.94 | 1.05 |
| Q2 | 0.98 | 0.92 | 1.04 | 0.98 | 0.92 | 1.04 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 1.01 | 0.95 | 1.07 | 1.01 | 0.95 | 1.07 | |
| Q5 | 1.01 | 0.95 | 1.07 | 1.02 | 0.96 | 1.08 | |
| Ever asthma | Q1 | 0.96 | 0.89 | 1.04 | 0.95 | 0.88 | 1.03 |
| Q2 | 0.96 | 0.89 | 1.03 | 0.95 | 0.88 | 1.03 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 0.99 | 0.92 | 1.07 | 1.00 | 0.93 | 1.08 | |
| Q5 | 1.04 | 0.97 | 1.12 | 1.06 | 0.99 | 1.14 | |
| AD | Q1 | 0.90 | 0.85 | 0.97 | 0.92 | 0.86 | 0.98 |
| Q2 | 0.97 | 0.91 | 1.03 | 0.97 | 0.91 | 1.04 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 0.97 | 0.91 | 1.04 | 0.97 | 0.90 | 1.03 | |
| Q5 | 0.97 | 0.91 | 1.04 | 0.97 | 0.91 | 1.04 | |
| Ever AD | Q1 | 1.03 | 0.96 | 1.10 | 1.03 | 0.96 | 1.11 |
| Q2 | 1.03 | 0.96 | 1.10 | 1.03 | 0.96 | 1.10 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 0.95 | 0.89 | 1.02 | 0.96 | 0.89 | 1.02 | |
| Q5 | 1.00 | 0.93 | 1.07 | 1.01 | 0.94 | 1.08 | |
| Ever rhinitis | Q1 | 1.02 | 0.97 | 1.07 | 0.99 | 0.95 | 1.04 |
| Q2 | 1.02 | 0.98 | 1.07 | 1.01 | 0.97 | 1.06 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 1.01 | 0.96 | 1.06 | 1.02 | 0.97 | 1.06 | |
| Q5 | 1.02 | 0.97 | 1.07 | 1.03 | 0.99 | 1.08 | |
| Current rhinitis | Q1 | 1.00 | 0.96 | 1.05 | 0.98 | 0.93 | 1.03 |
| Q2 | 1.01 | 0.96 | 1.06 | 1.00 | 0.95 | 1.05 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 1.00 | 0.95 | 1.05 | 1.00 | 0.96 | 1.05 | |
| Q5 | 1.00 | 0.95 | 1.05 | 1.01 | 0.96 | 1.06 | |
| Hay fever | Q1 | 1.00 | 0.89 | 1.13 | 0.99 | 0.88 | 1.11 |
| Q2 | 0.96 | 0.85 | 1.08 | 0.95 | 0.85 | 1.07 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 1.04 | 0.93 | 1.17 | 1.04 | 0.93 | 1.17 | |
| Q5 | 1.07 | 0.95 | 1.19 | 1.08 | 0.96 | 1.21 | |
| FA | Q1 | 0.99 | 0.90 | 1.07 | 1.00 | 0.92 | 1.09 |
| Q2 | 0.98 | 0.90 | 1.07 | 0.98 | 0.90 | 1.07 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 1.01 | 0.93 | 1.10 | 1.00 | 0.92 | 1.09 | |
| Q5 | 0.99 | 0.91 | 1.08 | 0.98 | 0.90 | 1.07 | |
| Allergic Outcomes | Energy Adjusted Maternal Dietary Iron Intake | Model 1 † | Model 2 ‡ | ||||
|---|---|---|---|---|---|---|---|
| ORs | 95% CI | ORs | 95% CI | ||||
| Lower | Upper | Lower | Upper | ||||
| Current wheeze | |||||||
| Q1 | 0.99 | 0.95 | 1.03 | 0.99 | 0.95 | 1.03 | |
| Q2 | 0.98 | 0.94 | 1.01 | 0.97 | 0.94 | 1.01 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 1.02 | 0.98 | 1.06 | 1.03 | 0.99 | 1.07 | |
| Q5 | 1.01 | 0.97 | 1.05 | 1.03 | 0.99 | 1.07 | |
| AD | 1.00 | - | - | 1.00 | - | - | |
| Q1 | 0.94 | 0.90 | 0.99 | 0.95 | 0.91 | 1.00 | |
| Q2 | 0.98 | 0.93 | 1.03 | 0.98 | 0.94 | 1.03 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 0.98 | 0.93 | 1.03 | 0.98 | 0.93 | 1.02 | |
| Q5 | 1.00 | 0.95 | 1.05 | 0.99 | 0.95 | 1.04 | |
| FA | 1.00 | - | - | 1.00 | - | - | |
| Q1 | 0.99 | 0.94 | 1.05 | 1.01 | 0.96 | 1.07 | |
| Q2 | 1.01 | 0.96 | 1.07 | 1.01 | 0.96 | 1.07 | |
| Q3 | 1.00 | - | - | 1.00 | - | - | |
| Q4 | 0.98 | 0.93 | 1.03 | 0.97 | 0.92 | 1.02 | |
| Q5 | 0.96 | 0.91 | 1.02 | 0.95 | 0.90 | 1.01 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, L.; Sato, M.; Saito-Abe, M.; Irahara, M.; Nishizato, M.; Sasaki, H.; Konishi, M.; Ishitsuka, K.; Mezawa, H.; Yamamoto-Hanada, K.; et al. Association of Hemoglobin and Hematocrit Levels during Pregnancy and Maternal Dietary Iron Intake with Allergic Diseases in Children: The Japan Environment and Children’s Study (JECS). Nutrients 2021, 13, 810. https://doi.org/10.3390/nu13030810
Yang L, Sato M, Saito-Abe M, Irahara M, Nishizato M, Sasaki H, Konishi M, Ishitsuka K, Mezawa H, Yamamoto-Hanada K, et al. Association of Hemoglobin and Hematocrit Levels during Pregnancy and Maternal Dietary Iron Intake with Allergic Diseases in Children: The Japan Environment and Children’s Study (JECS). Nutrients. 2021; 13(3):810. https://doi.org/10.3390/nu13030810
Chicago/Turabian StyleYang, Limin, Miori Sato, Mayako Saito-Abe, Makoto Irahara, Minaho Nishizato, Hatoko Sasaki, Mizuho Konishi, Kazue Ishitsuka, Hidetoshi Mezawa, Kiwako Yamamoto-Hanada, and et al. 2021. "Association of Hemoglobin and Hematocrit Levels during Pregnancy and Maternal Dietary Iron Intake with Allergic Diseases in Children: The Japan Environment and Children’s Study (JECS)" Nutrients 13, no. 3: 810. https://doi.org/10.3390/nu13030810
APA StyleYang, L., Sato, M., Saito-Abe, M., Irahara, M., Nishizato, M., Sasaki, H., Konishi, M., Ishitsuka, K., Mezawa, H., Yamamoto-Hanada, K., Matsumoto, K., Ohya, Y., & on behalf of the Japan Environment and Children’s Study (JECS) Group. (2021). Association of Hemoglobin and Hematocrit Levels during Pregnancy and Maternal Dietary Iron Intake with Allergic Diseases in Children: The Japan Environment and Children’s Study (JECS). Nutrients, 13(3), 810. https://doi.org/10.3390/nu13030810






