Moderate Consumption of Beer and Its Effects on Cardiovascular and Metabolic Health: An Updated Review of Recent Scientific Evidence
Abstract
:1. Introduction
2. Materials and Methods
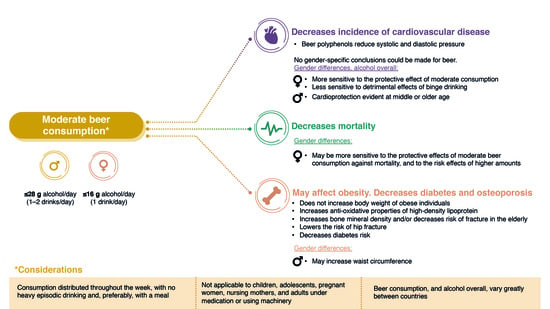
3. Results
Gender Differences
4. Moderate Beer Consumption and Mortality
Gender Differences
5. Moderate Beer Consumption and Obesity, Diabetes, and Osteoporosis
Gender Differences
6. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kalinowski, A.; Humphreys, K. Governmental Standard Drink Definitions and Low-Risk Alcohol Consumption Guidelines in 37 Countries. Addiction 2016, 111, 1293–1298. [Google Scholar] [CrossRef] [Green Version]
- Arbesu, J.A.; Armenteros del Olmo, L.; Casquero, R.; Goncalves, F.; Guardia Serecigni, J.; López Santiago, A.; Pascual Pastor, F.; Represas Carrera, F.J.; Sala Añó, C. Manual de Consenso Sobre Alcohol En Atención Primaria; Socidrogalcohol: Barcelona, Spain, 2016. [Google Scholar]
- Aranceta-Bartrina, J.; Partearroyo, T.; López-Sobaler, A.M.; Ortega, R.M.; Varela-Moreiras, G.; Serra-Majem, L.; Pérez-Rodrigo, C. Updating the Food-Based Dietary Guidelines for the Spanish Population: The Spanish Society of Community Nutrition (Senc) Proposal. Nutrients 2019, 11, 2675. [Google Scholar] [CrossRef] [Green Version]
- Department of Health. UK Chief Medical Officers’ Low Risk Drinking Guidelines; Department of Health: London, UK, 2016.
- U.S. Department of Health and Human Services. 2015–2020 Dietary Guidelines for Americans, 8th ed.; U.S. Department of Health and Human Services: Washington, DC, USA, 2015.
- Canadian Centre on Substance Use and Adiction. Alcohol Drinking Guidelines; Canadian Centre on Substance Use and Adiction: Ottawa, ON, Canada, 2018. [Google Scholar]
- Arranz, S.; Chiva-Blanch, G.; Valderas-Martínez, P.; Medina-Remón, A.; Lamuela-Raventós, R.M.; Estruch, R. Wine, Beer, Alcohol and Polyphenols on Cardiovascular Disease and Cancer. Nutrients 2012, 4, 759–781. [Google Scholar] [CrossRef] [Green Version]
- Chiva-Blanch, G.; Magraner, E.; Condines, X.; Valderas-Martínez, P.; Roth, I.; Arranz, S.; Casas, R.; Navarro, M.; Hervas, A.; Sisó, A.; et al. Effects of Alcohol and Polyphenols from Beer on Atherosclerotic Biomarkers in High Cardiovascular Risk Men: A Randomized Feeding Trial. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 36–45. [Google Scholar] [CrossRef]
- The Brewers of Europe. European Beer Trends-Statistics Report | 2019 Edition; The Brewers of Europe: Brussels, Belgium, 2020. [Google Scholar]
- Shield, K.D.; Rylett, M.; Rehm, J. Public Health Gains and Missed Opportunities. Trends in Alcohol Consumption and Attributable Mortality in the WHO European Region, 1990–2014: A Report to the WHO European Region; Centre for Addiction and Mental Health: Toronto, ON, Canada, 2016; ISBN 9781771143684. [Google Scholar]
- Missbach, B.; Majchrzak, D.; Sulzner, R.; Wansink, B.; Reichel, M.; Koenig, J. Exploring the Flavor Life Cycle of Beers with Varying Alcohol Content. Food Sci. Nutr. 2017, 5, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Sohrabvandi, S.; Mortazavian, A.M.; Rezaei, K. Health-Related Aspects of Beer: A Review. Int. J. Food Prop. 2012, 15, 350–373. [Google Scholar] [CrossRef]
- Romeo, J.; Díaz, L.; González-Gross, M.; Wärnberg, J.; Marcos, A. Contribución a La Ingesta de Macro y Micronutrientes Que Ejerce Un Consumo Moderado de Cerveza. Nutr. Hosp. 2006, 21, 84–91. [Google Scholar] [PubMed]
- Hill, S.T.; Sudarsanam, R.; Henning, J.; Hendrix, D. HopBase: A Unified Resource for Humulus Genomics. Database J. Biol. Databases Curation 2017, 2017, bax009. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carvalho, D.O.; Curto, A.F.; Guido, L.F. Determination of Phenolic Content in Different Barley Varieties and Corresponding Malts by Liquid Chromatography-Diode Array Detection-Electrospray Ionization Tandem Mass Spectrometry. Antioxidants 2015, 4, 563–576. [Google Scholar] [CrossRef] [Green Version]
- Řehová, L.; Škeříkova, V.; Jandera, P. Optimisation of Gradient HPLC Analysis of Phenolic Compounds and Flavonoids in Beer Using a CoulArray Detector. J. Sep. Sci. 2004, 27, 1345–1359. [Google Scholar] [CrossRef]
- Gerhäuser, C. Beer Constituents as Potential Cancer Chemopreventive Agents. Eur. J. Cancer 2005, 41, 1941–1954. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Hansen, P.E.; Wang, G.; Qiu, L.; Dong, J.; Yin, H.; Qian, Z.; Yang, M.; Miao, J. Pharmacological Profile of Xanthohumol, a Prenylated Flavonoid from Hops (Humulus Lupulus). Molecules 2015, 20, 754–779. [Google Scholar] [CrossRef] [PubMed]
- Xin, G.; Wei, Z.; Ji, C.; Zheng, H.; Gu, J.; Ma, L.; Huang, W.; Morris-Natschke, S.L.; Yeh, J.L.; Zhang, R.; et al. Xanthohumol Isolated from Humulus Lupulus Prevents Thrombosis without Increased Bleeding Risk by Inhibiting Platelet Activation and MtDNA Release. Free Radic. Biol. Med. 2017, 108, 247–257. [Google Scholar] [CrossRef]
- Wunderlich, S.; Zürcher, A.; Back, W. Enrichment of Xanthohumol in the Brewing Process. Mol. Nutr. Food Res. 2005, 49, 874–881. [Google Scholar] [CrossRef] [PubMed]
- Humia, B.V.; Santos, K.S.; Barbosa, A.M.; Sawata, M.; Mendonça, M.d.C.; Padilha, F.F. Beer Molecules and Its Sensory and Biological Properties: A Review. Molecules 2019, 24, 1568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sacanella Anglés, I.; Casas Rodriguez, R.; Viñas Esmel, E.; Castro Barquero, S.; Sacanella Meseguer, E. Prevención de La Enfermedad Cardiovascular y Bebidas Alcohólicas Fermentadas. ¿Realidad o Ficción? Nutr. Hosp. 2019, 36, 58–62. [Google Scholar]
- Williamson, G.; Manach, C. Bioavailability and Bioefficacy of Polyphenols in Humans. II. Review of 93 Intervention Studies. Am. J. Clin. Nutr. 2005, 81, 243S–255S. [Google Scholar] [CrossRef] [PubMed]
- Romeo, J.; González-Gross, M.; Wärnberg, J.; Díaz, L.E.; Marcos, A. Effects of Moderate Beer Consumption on Blood Lipid Profile in Healthy Spanish Adults. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 365–372. [Google Scholar] [CrossRef] [Green Version]
- Nishiwaki, M.; Kora, N.; Matsumoto, N. Ingesting a Small Amount of Beer Reduces Arterial Stiffness in Healthy Humans. Physiol. Rep. 2017, 5, 1–9. [Google Scholar] [CrossRef]
- Rimm, E.B.; Williams, P.; Fosher, K.; Criqui, M.; Stampfer, M.J. Moderate Alcohol Intake and Lower Risk of Coronary Heart Disease: Meta-Analysis of Effects on Lipids and Haemostatic Factors. Br. Med. J. 1999, 319, 1523–1528. [Google Scholar] [CrossRef] [Green Version]
- Di Castelnuovo, A.; Costanzo, S.; di Giuseppe, R.; de Gaetano, G.; Iacoviello, L. Alcohol Consumption and Cardiovascular Risk: Mechanisms of Action and Epidemiologic Perspectives. Future Cardiol. 2009, 5, 467–477. [Google Scholar] [CrossRef]
- Piano, M.R. Alcohol’s Effects on the Cardiovascular System. Alcohol Res. Curr. Rev. 2017, 38, 219–241. [Google Scholar]
- Hätönen, K.A.; Virtamo, J.; Eriksson, J.G.; Perälä, M.M.; Sinkko, H.K.; Leiviskä, J.; Valsta, L.M. Modifying Effects of Alcohol on the Postprandial Glucose and Insulin Responses in Healthy Subjects. Am. J. Clin. Nutr. 2012, 96, 44–49. [Google Scholar] [CrossRef] [Green Version]
- Traversy, G.; Chaput, J.P. Alcohol Consumption and Obesity: An Update. Curr. Obes. Rep. 2015, 4, 122–130. [Google Scholar] [CrossRef] [Green Version]
- Block, G. Foods Contributing to Energy Intake in the US: Data from NHANES III and NHANES 1999–2000. J. Food Compos. Anal. 2004, 17, 439–447. [Google Scholar] [CrossRef]
- Roe, M.; Pinchen, H.; Church, S.; Finglas, P. McCance and Widdowson’s The Composition of Foods Seventh Summary Edition and Updated Composition of Foods Integrated Dataset. Nutr. Bull. 2015, 40, 36–39. [Google Scholar] [CrossRef]
- Tujague, J.; Kerr, W.C. Energy Intake Estimates of Respondent-Measured Alcoholic Beverages. Alcohol Alcohol. 2009, 44, 34–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Gaetano, G.; Costanzo, S.; di Castelnuovo, A.; Badimon, L.; Bejko, D.; Alkerwi, A.; Chiva-Blanch, G.; Estruch, R.; la Vecchia, C.; Panico, S.; et al. Effects of Moderate Beer Consumption on Health and Disease: A Consensus Document. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 443–467. [Google Scholar] [CrossRef] [Green Version]
- Kawano, Y. Physio-Pathological Effects of Alcohol on the Cardiovascular System: Its Role in Hypertension and Cardiovascular Disease. Hypertens. Res. 2010, 33, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Gardner, J.D.; Mouton, A.J. Alcohol Effects on Cardiac Function. Compr. Physiol. 2015, 5, 791–802. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Shu, X.O.; Li, H.; Cai, H.; Liu, Q.; Zheng, W.; Xiang, Y.B.; Villegas, R. Physical Activity, Smoking, and Alcohol Consumption in Association with Incidence of Type 2 Diabetes among Middle-Aged and Elderly Chinese Men. PLoS ONE 2013, 8, e7791. [Google Scholar] [CrossRef] [Green Version]
- Sato, K.K.; Hayashi, T.; Harita, N.; Koh, H.; Maeda, I.; Endo, G.; Nakamura, Y.; Kambe, H.; Kiyotaki, C. Relationship between Drinking Patterns and the Risk of Type 2 Diabetes: The Kansai Healthcare Study. J. Epidemiol. Community Health 2012, 66, 507–511. [Google Scholar] [CrossRef]
- Marques-Vidal, P.; Vollenweider, P.; Waeber, G. Alcohol Consumption and Incidence of Type 2 Diabetes. Results from the CoLaus Study. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 75–84. [Google Scholar] [CrossRef]
- Wei, M.; Gibbons, L.W.; Mitchell, T.L.; Kampert, J.B.; Blair, S.N. Alcohol Intake and Incidence of Type 2. Diabetes Care 2000, 23, 18–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wannamethee, S.G.; Shaper, A.G.; Perry, I.J.; Alberti, K.G.M.M. Alcohol Consumption and the Incidence of Type II Diabetes. J. Epidemiol. Community Health 2002, 56, 542–548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Athyros, V.G.; Liberopoulos, E.N.; Mikhailidis, D.P.; Papageorgiou, A.A.; Ganotakis, E.S.; Tziomalos, K.; Kakafika, A.I.; Karagiannis, A.; Lambropoulos, S.; Elisaf, M. Association of Drinking Pattern and Alcohol Beverage Type with the Prevalence of Metabolic Syndrome, Diabetes, Coronary Heart Disease, Stroke, and Peripheral Arterial Disease in a Mediterranean Cohort. Angiology 2008, 58, 689–697. [Google Scholar] [CrossRef] [PubMed]
- Cullmann, M.; Hilding, A.; Östenson, C.G. Alcohol Consumption and Risk of Pre-Diabetes and Type 2 Diabetes Development in a Swedish Population. Diabet. Med. 2012, 29, 441–452. [Google Scholar] [CrossRef]
- Osorio-Paz, I.; Brunauer, R.; Alavez, S. Beer and Its Non-Alcoholic Compounds in Health and Disease. Crit. Rev. Food Sci. Nutr. 2019, 60, 1–14. [Google Scholar] [CrossRef]
- Redondo, N.; Nova, E.; Díaz-Prieto, L.E.; Marcos, A. Effects of Moderate Beer Consumption on Health. Nutr. Hosp. 2018, 35, 41–44. [Google Scholar] [CrossRef]
- Padro, T.; Muñoz-García, N.; Vilahur, G.; Chagas, P.; Deyà, A.; Antonijoan, R.M.; Badimon, L. Moderate Beer Intake and Cardiovascular Health in Overweight Individuals. Nutrients 2018, 10, 1237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wood, A.M.; Kaptoge, S.; Butterworth, A.; Nietert, P.J.; Warnakula, S.; Bolton, T.; Paige, E.; Paul, D.S.; Sweeting, M.; Burgess, S.; et al. Risk Thresholds for Alcohol Consumption: Combined Analysis of Individual-Participant Data for 599 912 Current Drinkers in 83 Prospective Studies. Lancet 2018, 391, 1513–1523. [Google Scholar] [CrossRef] [Green Version]
- Toma, A.; Paré, G.; Leong, D.P. Alcohol and Cardiovascular Disease: How Much Is Too Much? Curr. Atheroscler. Rep. 2017, 19, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bell, S.; Daskalopoulou, M.; Rapsomaniki, E.; George, J.; Britton, A.; Bobak, M.; Casas, J.P.; Dale, C.E.; Denaxas, S.; Shah, A.D.; et al. Association between Clinically Recorded Alcohol Consumption and Initial Presentation of 12 Cardiovascular Diseases: Population Based Cohort Study Using Linked Health Records. BMJ 2017, 356, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polsky, S.; Akturk, H.K. Alcohol Consumption, Diabetes Risk, and Cardiovascular Disease Within Diabetes. Curr. Diabetes Rep. 2017, 17, 136. [Google Scholar] [CrossRef] [PubMed]
- Xi, B.; Veeranki, S.P.; Zhao, M.; Ma, C.; Yan, Y.; Mi, J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-Related Mortality in U.S. Adults. J. Am. Coll. Cardiol. 2017, 70, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Fresán, U.; Gea, A.; Bes-Rastrollo, M.; Ruiz-Canela, M.; Martínez-Gonzalez, M.A. Substitution Models of Water for Other Beverages, and the Incidence of Obesity and Weight Gain in the SUN Cohort. Nutrients 2016, 8, 688. [Google Scholar] [CrossRef] [Green Version]
- Stockwell, T.; Zhao, J.; Panwar, S.; Roemer, A.; Naimi, T.; Chikritzhs, T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J. Stud. Alcohol Drugs 2016, 77, 185–198. [Google Scholar] [CrossRef] [Green Version]
- Roerecke, M.; Rehm, J. Alcohol Consumption, Drinking Patterns, and Ischemic Heart Disease: A Narrative Review of Meta-Analyses and a Systematic Review and Meta-Analysis of the Impact of Heavy Drinking Occasions on Risk for Moderate Drinkers. BMC Med. 2014, 12, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Bendsen, N.T.; Christensen, R.; Bartels, E.M.; Kok, F.J.; Sierksma, A.; Raben, A.; Astrup, A. Is Beer Consumption Related to Measures of Abdominal and General Obesity? A Systematic Review and Meta-Analysis. Nutr. Rev. 2013, 71, 67–87. [Google Scholar] [CrossRef]
- Roerecke, M.; Rehm, J. The Cardioprotective Association of Average Alcohol Consumption and Ischaemic Heart Disease: A Systematic Review and Meta-Analysis. Addiction 2012, 107, 1246–1260. [Google Scholar] [CrossRef] [PubMed]
- Costanzo, S.; di Castelnuovo, A.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Wine, Beer or Spirit Drinking in Relation to Fatal and Non-Fatal Cardiovascular Events: A Meta-Analysis. Eur. J. Epidemiol. 2011, 26, 833–850. [Google Scholar] [CrossRef]
- Yin, J.; Winzenberg, T.; Quinn, S.; Giles, G.; Jones, G. Beverage-Specific Alcohol Intake and Bone Loss in Older Men and Women: A Longitudinal Study. Eur. J. Clin. Nutr. 2011, 65, 526–532. [Google Scholar] [CrossRef]
- Schütze, M.; Schulz, M.; Steffen, A.; Bergmann, M.M.; Kroke, A.; Lissner, L.; Boeing, H. Beer Consumption and the “Beer Belly”: Scientific Basis or Common Belief? Eur. J. Clin. Nutr. 2009, 63, 1143–1149. [Google Scholar] [CrossRef] [Green Version]
- Snow, W.M.; Murray, R.; Ekuma, O.; Tyas, S.L.; Barnes, G.E. Alcohol Use and Cardiovascular Health Outcomes: A Comparison across Age and Gender in the Winnipeg Health and Drinking Survey Cohort. Age Ageing 2009, 38, 206–212. [Google Scholar] [CrossRef] [Green Version]
- Suadicani, P.; Hein, H.O.; Gyntelberg, F. Wine Intake, ABO Phenotype, and Risk of Ischemic Heart Disease and All-Cause Mortality: The Copenhagen Male Study-a 16-Year Follow-Up. Alcohol 2008, 42, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Mukamal, K.J.; Robbins, J.A.; Cauley, J.A.; Kern, L.M.; Siscovick, D.S. Alcohol Consumption, Bone Density, and Hip Fracture among Older Adults: The Cardiovascular Health Study. Osteoporos. Int. 2007, 18, 593–602. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.J.; Chin, S.L.; Rangarajan, S.; Xavier, D.; Liu, L.; Zhang, H.; Rao-Melacini, P.; Zhang, X.; Pais, P.; Agapay, S.; et al. Global and Regional Effects of Potentially Modifiable Risk Factors Associated with Acute Stroke in 32 Countries (INTERSTROKE): A Case-Control Study. Lancet 2016, 388, 761–775. [Google Scholar] [CrossRef]
- Smyth, A.; Teo, K.K.; Rangarajan, S.; O’Donnell, M.; Zhang, X.; Rana, P.; Leong, D.P.; Dagenais, G.; Seron, P.; Rosengren, A.; et al. Alcohol Consumption and Cardiovascular Disease, Cancer, Injury, Admission to Hospital, and Mortality: A Prospective Cohort Study. Lancet 2015, 386, 1945–1954. [Google Scholar] [CrossRef]
- Di Castelnuovo, A.; Costanzo, S.; Bagnardi, V.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Alcohol Dosing and Total Mortality in Men and Women: An Updated Meta-Analysis of 34 Prospective Studies. Arch. Intern. Med. 2006, 166, 2437–2445. [Google Scholar] [CrossRef]
- Renaud, S.C.; Guéguen, R.; Siest, G.; Salamon, R. Wine, Beer, and Mortality in Middle-Aged Men from Eastern France. Arch. Intern. Med. 1999, 159, 1865–1870. [Google Scholar] [CrossRef] [Green Version]
- Wannamethee, S.G.; Shaper, A.G. Type of Alcoholic Drink and Risk of Major Coronary Heart Disease Events and All-Cause Mortality. Am. J. Public Health 1999, 89, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, N.R.; Schnohr, P.; Jensen, G.; Grønbæk, M. Is the Relationship between Type of Alcohol and Mortality Influenced by Socio-Economic Status? J. Intern. Med. 2004, 255, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, P.; Licaj, I.; Muller, D.C.; Andersen, P.K.; Johansson, M.; Boeing, H.; Weiderpass, E.; Dossus, L.; Dartois, L.; Fagherazzi, G.; et al. Lifetime Alcohol Use and Overall and Cause-Specific Mortality in the European Prospective Investigation into Cancer and Nutrition (EPIC) Study. BMJ Open 2014, 4, e005245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, J.; Wang, X.; Zhang, Y. Specific Types of Alcoholic Beverage Consumption and Risk of Type 2 Diabetes: A Systematic Review and Meta-Analysis. J. Diabetes Investig. 2017, 8, 56–68. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.Y.; Lee, D.Y.; Lee, Y.J.; Park, K.J.; Kim, K.H.; Kim, J.W.; Kim, W.-H. Chronic Alcohol Consumption Potentiates the Development of Diabetes through Pancreatic β-Cell Dysfunction. World J. Biol. Chem. 2015, 6, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Kim, D.J. Alcoholism and Diabetes Mellitus. Diabetes Metab. J. 2012, 36, 108–115. [Google Scholar] [CrossRef]
- Potì, F.; Santi, D.; Spaggiari, G.; Zimetti, F.; Zanotti, I. Polyphenol Health Effects on Cardiovascular and Neurodegenerative Disorders: A Review and Meta-Analysis. Int. J. Mol. Sci. 2019, 20, 351. [Google Scholar] [CrossRef] [Green Version]
- Chiva-Blanch, G.; Condines, X.; Magraner, E.; Roth, I.; Valderas-Martínez, P.; Arranz, S.; Casas, R.; Martínez-Huélamo, M.; Vallverdú-Queralt, A.; Quifer-Rada, P.; et al. The Non-Alcoholic Fraction of Beer Increases Stromal Cell Derived Factor 1 and the Number of Circulating Endothelial Progenitor Cells in High Cardiovascular Risk Subjects: A Randomized Clinical Trial. Atherosclerosis 2014, 233, 518–524. [Google Scholar] [CrossRef]
- Hodge, A.M.; English, D.R.; O’Dea, K.; Giles, G.G. Alcohol Intake, Consumption Pattern and Beverage Type, and the Risk of Type 2 Diabetes. Diabet. Med. 2006, 23, 690–697. [Google Scholar] [CrossRef]
- Rasouli, B.; Ahlbom, A.; Andersson, T.; Grill, V.; Midthjell, K.; Olsson, L.; Carlsson, S. Alcohol Consumption Is Associated with Reduced Risk of Type2 Diabetes and Autoimmune Diabetes in Adults: Results from the Nord-Trøndelag Health Study. Diabet. Med. 2013, 30, 56–64. [Google Scholar] [CrossRef]
- Bagnardi, V.; Rota, M.; Botteri, E.; Tramacere, I.; Islami, F.; Fedirko, V.; Scotti, L.; Jenab, M.; Turati, F.; Pasquali, E.; et al. Alcohol Consumption and Site-Specific Cancer Risk: A Comprehensive Dose-Response Meta-Analysis. Br. J. Cancer 2015, 112, 580–593. [Google Scholar] [CrossRef]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean Diet Pyramid: A Cultural Model for Healthy Eating. Am. J. Clin. Nutr. 1995, 6, 1402S–1406S. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism Governments Confront Drunken Violence. Bull. World Health Organ. 2010, 88, 644–645. [CrossRef] [PubMed]
- National Institute on Alcohol Abuse and Alcoholism. NIAAA Council Approves Definition of Binge Drinking. NIAAA Newsl. 2004, 3, 3. [Google Scholar]
- Ruidavets, J.B.; Ducimetière, P.; Evans, A.; Montaye, M.; Haas, B.; Bingham, A.; Yarnell, J.; Amouyel, P.; Arveiler, D.; Kee, F.; et al. Patterns of Alcohol Consumption and Ischaemic Heart Disease in Culturally Divergent Countries: The Prospective Epidemiological Study of Myocardial Infarction (PRIME). BMJ 2010, 341, 1146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Horvat, P.; Stefler, D.; Murphy, M.; King, L.; McKee, M.; Bobak, M. Alcohol, Pattern of Drinking and All-Cause Mortality in Russia, Belarus and Hungary: A Retrospective Indirect Cohort Study Based on Mortality of Relatives. Addiction 2018, 113, 1252–1263. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Aranceta, J. Carta al Editor. Réplica: “La Recomendación Del Consumo de Alcohol En Las ‘Guías Alimentarias Para La Población Española’. Un Mensaje Demasiado Ambiguo”. Nutr. Hosp. 2017, 34, 1006–1008. [Google Scholar] [CrossRef]
- Li, Y.; Pan, A.; Wang, D.D.; Liu, X.; Dhana, K.; Franco, O.H.; Kaptoge, S.; di Angelantonio, E.; Stampfer, M.; Willett, W.C.; et al. Impact of Healthy Lifestyle Factors on Life Expectancies in the Us Population. Circulation 2018, 138, 345–355. [Google Scholar] [CrossRef] [PubMed]
| Country. Year Guidelines | 1 SDU = g Pure Alcohol | Term | Daily a,b (g Alcohol) | Weekly a,b (g Alcohol) |
|---|---|---|---|---|
| Spain. 2016 Socidrogalcohol consensus on alcohol in Primary Care [2] | 1 SDU = 10 g Wine: 1 glass Beer: 1 beer (≈200 mL) Spirits: 25 g | Risky consumption (starting at) | Women: 20 g Men: 40–60 g | Women: 140 g Men: 280 g |
| Spain. 2019 Update Dietary Guidelines for the Spanish population [3] | 1 SDU = 10 g | Moderate consumption (upper limit) | Women: <20 g Men: <40 g | - - |
| UK. 2016 UK Chief Medical Officers’ Low Risk Drinking Guidelines [4] | 1 SDU = 8 g Wine: 1 glass (125 mL) (11% ABV) | Low-risk drinking (upper limit) | - - | Women: 112 g Men: 112 g |
| USA. 2015 Dietary guidelines [5] | 1 SDU = 14 g Wine: 5 fl oz or 147.9 mL (12% ABV) Beer: 12 fl oz or 354.9 mL (5% ABV) Spirits: 1.5 fl oz or 44.4 mL (40% ABV) | Moderate drinking (upper limit) | Women: 14 g Men: 28 g | - - |
| Canada. 2018 Canada low-risk alcohol drinking guidelines [6] | 1 SDU c ≈ 13 g Wine: 142 mL (12% ABV) Beer: 341 mL (5% ABV) Spirits: 43 mL (40% ABV) | Recommended limit | - - | Women: 130 g Men: 210 g |
| 37 countries. 2016 [1] | 1 SDU = 8–20 g | Low-risk drinking (upper limits range) | Women: 10–42 g Men: 10–56 g | Women: 98–140 g Men: 150–280 g |
| Data Base | Search Syntax | No. Articles |
|---|---|---|
| PubMed | ((Beer[MeSH Major Topic]) and (“2007”[Date—Publication]: “2020/04/01”[Date—Publication])) and (health or mortality or cardiovascular or diabetes or obesity or women or men or gender or young or adolescent or age or alcoholism) | 82 |
| Filtered by: | ||
| Clinical study | ||
| Comparative study | ||
| Multicenter study | ||
| Observational study | ||
| Randomized controlled trial | ||
| Systematic reviews | ||
| EMBASE | ‘beer’/de and ‘beer’:ab,ti and ((‘health’/de or ‘mortality’/de or ‘cardiovascular’/de or ‘diabetes’/de or ‘obesity’/de or ‘female’/de or ‘male’/de or ‘sex’/de) and difference or ‘adolescent’/de or ‘young adult’/de or ‘alcoholism’/de) and ((article)/lim or (review)/lim) and ((adolescent)/lim or (young adult)/lim or (adult)/lim or (middle aged)/lim or (aged)/lim or (very elderly)/lim) and (humans)/lim and (clinical study)/lim and (2007–2017)/py | 210 |
| Alcohol/Beer Paper | Study Type | Related Subject |
|---|---|---|
| Osorio-Paz et al. 2019 [44] | Review | CV |
| Sacanella et al. Nutr Hosp. 2019 [22] | Review | CV |
| Humia et al. Molecules 2019 [21] | Review | CV |
| Redondo et al. Nutr Hosp 2018 [45] | Review | CV and osteoporosis |
| Padro et al. Nutrients 2018 [46] | Prospective randomized cross-over | Obesity (metabolic syndrome) |
| Wood et al. Lancet. 2018 [47] | System. Review/Meta | CV and Mortality |
| Toma et al. Curr Atheroscler Rep. 2017 [48] | Review | CV |
| Bell et al. BMJ 2017 [49] | Prospective cohort | CV |
| Polsky et al. Curr Diab Rep. 2017 [50] | System. Review | Diabetes |
| Xi et al. J Am Coll Cardiol. 2017 [51] | Prospective population-based cohort | Mortality |
| de Gaetano et al. Nutr Metab Cardiovasc Dis. 2016 [34] | Review | CV and Mortality |
| Fresán et al. Nutrients. 2016 [52] | Prospective cohort | Obesity |
| Stockwell et al. J. Stud. Alcohol Drugs. 2016 [53] | System. Review/Meta | Mortality |
| Roerecke et al. BMC Med. 2014 [54] | System. Review/Meta | CV |
| Bendsen et al. Nutr Rev. 2013 [55] | System. Review/Meta | Obesity |
| Cullmann et al. Diabetic Medicine. 2012 [43] | Prospective cohort | Diabetes |
| Roerecke et al. Addiction. 2012 [56] | System. Review/Meta | CV |
| Costanzo S, et al. Eur J Epidemiol. 2011 [57] | System. Review/Meta | CV |
| Yin et al. Eur J Clin Nutr. 2011 [58] | Prospective cohort | Osteoporosis |
| Schütze et al. Eur J Clin Nutr 2009 [59] | Prospective cohort | Obesity |
| Snow et al. Age and Ageing. 2009 [60] | Prospective cohort | CV and Mortality |
| Suadicani et al. Alcohol. 2008 [61] | Prospective cohort | Mortality |
| Mukamal et al. Osteoporos Int. 2007 [62] | Prospective population-based cohort | Osteoporosis |
| Study Funding/COI a | Design (Mean/Median Years of Follow-Up) | n | Categories of Consumption/Type of Drink | Variables | Reference Group (HR = 1) | Outcomes/Conclusions b |
|---|---|---|---|---|---|---|
| Costanzo et al., 2011 [57] Cervisia Consulenze and Istituto Nazionale per la Comunicazione. | Systematic review-meta-analysis | 12 prospective studies (n ranged from 1373 to 87,536) and 6 case-control studies (n ranged from 616 to 1746) | Wine, beer, and spirits | Fatal non-fatal CHD, CHD, CVD, AMI, stroke, CHD mortality, IHD mortality, CVD mortality AND/OR total mortality. | 13 studies: J-shaped relationship for beer and CV risk. 16 studies: J-shaped relationship between wine intake and CV risk. 12 studies reporting separate data on wine or beer consumption: two closely overlapping dose-response curves. | |
| Roerecke et al., 2012 [56] Global Burden of Disease Study and by the grant “Drinking Patterns & Ethnicity: Impact on Mortality Risks”, NIAAA | Systematic review-meta-analysis | 44 observational studies including 957,684 participants | Lifetime abstainer. Occasional: 2.5–11.99 g/week; 12–23.99 g/week; 24–35.99 g/week / Alcohol in general | IHD | Lifetime abstainers | Cardioprotection was observed in all strata, and substantial heterogeneity was noted across studies. Wide confidence intervals observed particularly for average consumption of 1–2 drinks per day. |
| Roerecke et al., 2014 [54] The European Community’s Seventh Framework Programme—Addictions and Lifestyle in Contemporary Europe—Reframing Addictions Project. | Systematic review and meta-analysis | 7 studies for the meta-analysis | For the meta-analysis: Current drinkers with an average alcohol consumption <30 g/day of pure alcohol with or without HED / Alcohol in general | IHD | Lifetime abstainers | Beneficial effect of low alcohol consumption without HED episodes as compared to life-time abstainers |
| Wood et al., 2018 [47] Various government, private, and pharmaceutical sources. / None declared. | Systematic review and meta-analysis | 83 prospective studies including 599,912 participants | Current drinkers / Alcohol in general, also separate analyses for wine, beer, and spirits | Mortality, stroke, CHD, AMI, heart failure, fatal hypertensive disease, fatal aortic aneurysm | Lowest baseline alcohol consumption category (0–25 g/week) | Threshold for lowest risk of all-cause mortality was ~100 g/week. Association between alcohol consumption and total CVD risk showed higher HR for beer and spirits than for wine. |
| de Gaetano et al., 2016 [34] Assobirra, the Italian Association of the Beer and Malt Industries/Some authors were consultants for the Web Newsletter of Assobirra, or were on the board/received lecture fees from FIVIN, the Beer and Health Foundation, ERAB, or Cerveceros de España. | Systematic review | 7 prospective studies (n ranged from 1373 to 87,526) and 4 case-control studies (n ranged from 937 to 1514) | Wine, beer, and spirits | Fatal non-fatal CHD, AMI, CHD, CHD mortality, AND/OR CVD mortality. | Some benefit of beer against CVD | |
| Toma et al., 2017 [48]/ None declared | Review | 1 case-control study (INTERSTROKE [63]; n = 26,919) and 1 prospective study (PURE; [64] n = 114,970) | INTERSTROKE: low-moderate alcohol use: ≤14 drinks/w in women and ≤21 drinks/w in men. / Alcohol in general | INTERSTROKE: any stroke, ischemic stroke, and hemorrhagic stroke PURE: mortality, CVD, myocardial infarction, stroke, and a composite of all outcomes, which also included alcohol-related cancers and injury. | INTERSTROKE: Non-drinkers or former drinkers. PURE: Non-drinkers | INTERSTROKE: Low-moderate alcohol use was associated with stroke (OR: 1.14; 95%CI 1.01–1.28), ischemic stroke (OR: 1.07; 0.93–1.23) and hemorrhagic stroke (OR: 1.43; 1.17–1.74). PURE: Current drinking was associated with reduced myocardial infarction (HR: 0.76; 95% CI 0.63–0.93). In addition, it was associated with a reduced composite outcome in high-income and upper-middle-income countries (HR 0.84 (0.77–0.92)), but not in lower-middle-income and low-income countries (HR 1.07 (0.95–1.21); p-interaction < 0.0001). |
| Bell et al., 2017 [49] National Institute for Health Research, Welcome Trust, the Medical Research Council prognosis research strategy Partnership and other government health-related agencies. / None declared | Prospective cohort (6 y) | 1,937,360 (51% women) | Non-drinkers. Former drinkers. Occasional drinkers: drinks rarely or occasionally. Moderate: Men: 21 SDU/week or 3 SDU/day. Women: 14 SDU/w or 2 SDU/da. Heavy drinkers / Alcohol in general | 12 common symptomatic manifestations of CVD. Aggregated CVD (all CV endpoints other than stable angina). | Moderate drinkers | Non-drinking: unstable angina (HR 1.33, 95% CI 1.21 to 1.45), myocardial infarction (1.32, 1.24 to1.41), unheralded coronary death (1.56, 1.38 to 1.76), heart failure (1.24, 1.11 to 1.38), ischemic stroke (1.12, 1.01 to 1.24), peripheral arterial disease (1.22, 1.13 to 1.32), and abdominal aortic aneurysm (1.32, 1.17 to 1.49). Heavy drinking: unheralded coronary death (HR 1.21, 95%CI 1.08 to 1.35), heart failure (1.22, 1.08 to 1.37), cardiac arrest/sudden coronary death (1.50, 1.26 to 1.77), transient ischemic attack (1.11, 1.02 to 1.21), ischemic stroke (1.33, 1.09 to 1.63), intra-cerebral hemorrhage (1.37, 1.16 to 1.62), peripheral arterial disease (1.35, 1.23 to 1.48); myocardial infarction (0.88, 0.79 to 1.00) and stable angina (0.93, 0.86 to 1.00). |
| Snow et al., 2009 [60] None declared | Prospective cohort (10 y) | 1154 (574 women) | 1 SDU: 13 g ethanol. Men: Light: 0.65–5.77 g/day; Moderate: 5.78–18.1 g/day; Heavy: >18.1 g/day. HED: ≥8 drinks/episode in past year Women: Light: 0.65–2.92 g/day; Moderate: 2.93–9.15 g/day; Heavy: >9.15 g/day. HED: frequency of ≥8 drinks/episode / Alcohol in general | CHD events; hypertension; Other CVD | Lifetime abstainers and occasional drinkers who consumed <0.05 drinks (<0.65 g) per day. | Men for CHD events: Heavy: HR: 0.28 (0.08–0.93) p = 0.037 in old men; HED: 4.13 (1.46−11.62) p = 0.0073 in middle-aged men. Men for hypertension: HED: HR 1.62 (0.99–2.63), p = 0.054 in old men. Men for other CVD: Light: HR 0.54 (0.28−1.04), p = 0.066 in old men; Heavy: HR 0.40 (0.19−0.85, p = 0.017 in old men. Women for hypertension: Light: HR 0.26 (0.07–1.01), p = 0.052 in young women. Women for other CVD: Light: HR 0.23 (0.08−0.65), p = 0.0057 and Moderate: HR 0.14 (0.05−0.45), p = 0.0009 in young women. |
| Study Funding/COI a | Design (Mean/Median Years of Follow-Up) | n (Women) | Categories of Alcohol Consumption/Type of Drink | Variable/s | Reference Group (HR = 1) | Outcomes/Conclusions b |
|---|---|---|---|---|---|---|
| de Gaetano et al., 2016 [34] Assobirra, the Italian Association of the Beer and Malt Industries/ Some authors were consultants for the Web Newsletter of Assobirra, or were on the board/received lecture fees from Fundación Cerveza y Salud, FIVIN, the Beer and Health Foundation, ERAB, or Cerveceros de España. | Systematic review | Wine, beer, and spirits | All-cause mortality | Evidence suggests a J-shaped relationship between alcohol consumption and total mortality, with lower risk for moderate alcohol consumers than for abstainers or heavy drinkers. Specific data on beer are not conclusive, although some results indicate a positive role of drinking beer in moderation (1 drink/day, about 12 g of ethanol) against mortality for any cause | ||
| 1 meta-analysis of 34 prospective studies [65] | Over 1 million adults | Low to moderate Women: 1 drink/day. Men: 2 drinks/day / Wine, beer, and spirits | All-cause mortality | Low to moderate consumption of alcohol significantly reduces total mortality, while higher doses increase it | ||
| 1 Prospective cohort [66] (12–18 y) | 36,250 men | Wine and beer | CV death All-cause mortality | Non-drinkers | Moderate wine or beer drinking reduced the risk of CV death. Only moderate wine drinking was associated with lower all-cause mortality: RR: 0.67 (0.58 to 0.77; p < 0.001) | |
| 1 Prospective cohort [67] (16.8 y) | 7735 British men 40–59 y old | 1 SDU: Half pint beer (8–10 g alcohol). Frequency: Non-drinkers; Occasional (1–2 SDU/month); Weekend drinkers; Daily or on most days. Quantity: 1–2, 3–6, >6 / Wine, beer, and spirits | All-cause mortality | Occasional drinkers | Regular beer drinking [HR: 0.84 (0.71 to 1.01)] showed no significant difference vs. occasional drinking | |
| 1 Prospective cohort [68] Copenhagen City Heart Study (25 y) | 14,223 adults | 1 SDU: 1 bottle beer (12 g alcohol). Never, Hardly ever, Monthly, Weekly Daily: 1–2 SDUs Daily: >2 SDUs / Wine, beer, and spirits | All-cause mortality | Never beer drinkers | In men, monthly beer intake (RR: 0.86 (0.77 to 0.97)) was associated with lower mortality, and daily intake >2 beers (RR: 1.14 (1.02 to 1.27)) to increased risk. In women the associations were not statistically significant: Monthly beer intake (RR: 0.98 (0.88 to 1.08)), and daily intake >2 beers (RR: 1.31 (0.92 to 1.88)) At a medium education level, monthly beer intake was associated with lower risk (RR: 0.87 (0.77 to 0.97)), and at low [RR:1.20 (1.07 to 1.34) and medium education level (RR:1.18 (1.02 to 1.37)), >2 beers daily was associated with increased risk. | |
| 1 Prospective cohort [69] (12.6 y) | 380,395 adults (247,795 women) | For beer: Never. Light: 0.1–2.9 g/day, 3–9.9 g/day, 10–19.9 g/day, 20–39.9 g/day (only for men). ≥20 g/day (extreme for women) ≥40 g/day (extreme for men) / Wine and beer | All-cause mortality | Light consumers (0.1–2.9 g/day) | In women: Compared to low-level consumers, lifetime non-drinkers (HR: 1.06; 1.02 to 1.12), and consumers of beer at amounts ≥3 g/day displayed significantly higher overall mortality risk. In men: Lifetime non-drinkers (HR: 1.07; 0.98 to 1.16) and consumers of 3–9.9 g/day (HR: 1.04; 0.98 to 1.10) showed no significant differences compared to light consumers. Consumers of beer amounts ≥10 g/day displayed a significantly higher overall mortality risk. | |
| Stockwell et al., 2016 [53] None declared | Systematic review/meta-analysis of 87 studies (13.4 y) | 3998,626 adults | Abstainer. Former drinker. Occasional: <1.30 g/day. Low: 1.30 to <25 g /day. Medium: 25 to <45 g/day High: 45 to <65 g/day. Higher: ≥65 g/day / Alcohol in general | All-cause mortality | Abstainer OR occasional drinker | Standard adjustment: Significant protective effect for low-volume (RR: 0.86 (0.83 to 0.90); p < 0.0001) and occasional drinkers (RR: 0.84 (0.79 to 0.89); p < 0.0001) as compared with abstainers. Abstainers were at significantly higher risk (RR: 1.19 (1.12 to 1.27); p < 0.0001) as compared to occasional drinkers. Full adjustment: No significant protection was estimated for occasional (RR: 0.95 (0.85 to 1.05)), low-volume (RR: 0.97 (0.88 to 1.07)), or medium-volume drinkers (RR: 1.07 (0.97 to 1.18)) as compared with abstainers. |
| Xi et al., 2017 [51] None declared | Population survey data linked to mortality data (8.2 y) | 333,247 adults | 1 SDU: 14 g alcohol. Lifetime abstainers. Lifetime infrequent drinkers. Former drinkers. Current light drinkers. Moderate: >3 to ≤14 drinks/w for men or >3 to ≤7 drinks/w for women. Heavy drinkers. Binge drinking / Alcohol in general | All-cause, cancer, or CVD mortality. | Lifetime abstainers | All cause-mortality: Decreased for Light (HR 0.79 (0.76 to 0.82)) and Moderate (HR 0.78 (0.74 to 0.82)) drinkers. Increased in Heavy: HR: 1.11 (1.04 to 1.19) and binge (HR: 1.13 (1.04 to 1.23)) drinkers. CVD-specific mortality: Light: HR 0.74 (0.69 to 0.80); Moderate: HR 0.71 (0.64 to 0.78) |
| Bell et al., 2017 [49] National Institute for Health Research, Welcome Trust, the Medical Research Council prognosis research strategy Partnership and other government health-related agencies. | Prospective cohort (6 y) | 1937,360 (51% women) | 1 SDU c: 8 g Non-drinkers. Former drinkers Occasional drinkers: drinks rarely or occasionally. Moderate: Men: 21 SDU/w or 3 SDU/day. Women: 14 SDU/w or 2 SDU/day Heavy drinkers / Alcohol in general | CV death and all-cause mortality | Moderate drinkers | Non-drinkers (former and occasional drinkers removed) had an increased risk of CV death (HR: 1.32 (1.27 to 1.38)) and all-cause mortality (HR: 1.24 (1.20 to 1.28)). |
| Suadicani, 2008 [61] The King Christian X’s Foundation, The Danish Medical Research Council, The Danish Heart Foundation, and The Else & Mogens Wedell Wedellsborg Foundation. | Prospective cohort (16 y) | 3022 Caucasian males 53–74 y old | 1 SDU: 10–12 g ethanol / Wine, beer, and spirits | All-cause and IHD-related death within the different blood phenotypes | Alcohol abstainers (comparison only for wine drinkers) | For beer, the median (P20, P80) number of drinks/week among those with the non-O phenotype was significantly higher in those who died (overall mortality): 10.5 (0, 15.5) vs 7.5 (0, 10.5); p ≤ 0.001. The effect of wine intake on all-cause mortality among middle-aged and elderly men may depend on ABO phenotypes. Among non-O phenotype, drinking 1–8 drinks/w: HR: 0.8 (0.7 to 1.8) and drinking >8 drinks/w: HR: 0.7 (0.6 to 0.98) |
| Study Funding/COI a | Design (Mean/Median Years of Follow-Up) | n (Women) | Categories of Alcohol Consumption/Type of Drink | Variable/s | Reference Group (HR = 1) | Outcomes/Conclusions b |
|---|---|---|---|---|---|---|
| Fresan et al., 2016 [52] The Spanish Ministry of Health, the Navarra Regional Government, and the University of Navarra. | Prospective cohort (4 y) | 15,765 adults | Beverages groups: Water, low/non-caloric beverages (diet soda beverages, coffee without sugar), milk, juice, and sugared coffee (dairy products, juices, coffee with sugar). Occasional consumption (SSSBs and spirits). Wine, beer | Change in BW and new-onset obesity | No substitution | Substitution of one beer with one serving of water per day at baseline was related to a lower incidence of obesity (OR 0.81, 95%CI 0.69 to 0.94 and OR 0.84, 95%CI 0.71 to 0.98, when further adjusted for the consumption of other beverage groups) and to higher weight loss (−328 g, 95%CI −566 to −89). |
| Bendsen et al., 2013 [55] The Dutch Beer Institute (funded by the Dutch Brewers)/ Three of the authors are employed by or are board members of the Dutch Beer Institute. | Systematic review of 35 observational studies and 12 experimental studies Meta-analyses: 14 observational studies (11 cross-sectional and 3 prospective) included in dose-response graphs. 10 intervention studies (6 beer vs non-alcoholic beer and 4 beer vs control) included in quantitative synthesis | 1 SDU beer = 330 mL, 4.6% alcohol = 12 g/drink. / Beer | BW increase, BMI, and abdominal obesity (WC and WHR) | Control: Non-drinkers or in the absence of non-drinkers, the group with the lowest beer intake Low or non-alcoholic beer | Dose-response graphs: High beer intake (>4 L/w) was associated with a higher degree of abdominal obesity in men. Quantitative synthesis: High beer consumption (about 1000 mL/day; 5% alcohol) did not result in increased BW compared with control groups but did result in increased BW compared with low- or non-alcoholic beer groups (mean difference 0.73 kg, 95% CI: 0.53 to 0.92; z = 7.39, p < 0.0001, I2 = 0%) | |
| Schütze et al., 2009 [59] The German Cancer Aid, the German Federal Ministry of Education and Research and the European Union. | Prospective cohort (8.5 y) | 20,625 (12,749 women) | WOMEN: No beer. Very light: >0 to <125 mL/day. Light: ≥125 to <250 mL/day. Moderate: ≥250 mL/d MEN: No beer. Very light: >0 to <250 mL/day. Light: ≥250 to <500 mL/day. Moderate: ≥500 to <1000 mL/day Heavy: ≥1000 mL/day / Beer | WC change BW change | Very light | MEN: Moderate beer consumption showed significant lower relative odds for WC loss (OR 0.44, 95%CI 0.24 to 0.80) WOMEN: Although beer-abstaining women showed significantly lower relative odds (OR.0.88; CI 0.81, 0.96) for WC gain compared with their very-low-level-drinking counterparts, significance was lost once the model was adjusted by HC change; however, the new OR was on the border of significance (OR.0.91; CI 0.83, 1.00) |
| Padro et al., 2018 [46] Fundacion Cerveza y Salud, Madrid, Spain; The European Foundation for Alcohol Research; Spanish Ministry of Economy and Competitiveness of Science; Institute of Health Carlos III. | Open-label, prospective randomized, two-arm, longitudinal cross-over | 36 (15 women) | WOMEN: 330 mL/day normal or non-alcoholic beer (15 g/day or 0 g/day alcohol) MEN: 660 mL/day normal or non-alcoholic beer (30 g/day or 0 g/day alcohol) / Beer | BMI T2D Lipid Profile | Moderate beer consumption (traditional or alcohol-free) does not increase body weight in obese healthy individuals or have negative effects on the vascular system. Moderate consumption was associated with reduced risk of dyslipidemia, increased anti-oxidative properties of high-density lipoprotein, and increased efflux of cholesterol. | |
| Polsky et al., 2017 [50] None declared | Systematic Review of 96 studies | 18 studies included more than 10,000 subjects each. | Alcohol in general | Moderate alcohol consumption generally reduces diabetes risk. | ||
| Cullman et al. 2012 [43] The Swedish Research Council; the Swedish Diabetes Association; the Swedish Council of Working Life and Social research; and Novo Nordisk Scandinavia. | Prospective cohort (8–10 y) | 5128 adults (3058 women) with normal glucose tolerance and 111 (41 women) with pre-diabetes. 35–56 y old | Abstainers Total alcohol Occasional: 0.01–1.49 g/day in women, 0.01–6.79 g/day in men. Low: 1.50–4.71 g/day in women, 6.80–13.01 g/day in men. Medium: 4.72–8.75 g/day in women, 13.02–22.13 g/day in men. High: ≥8.76 g/day in women, ≥22.14 g/day in men Wine Occasional: ≤0.32 g/day in women, ≤0.99 g/day in men. Medium: 0.33–1.65 g/day in women, 1–4.99 g/day in men. High: ≥1.66 g/day in women, ≥5 g/day in men Beer (only in men) Occasional: ≤0.99 g/day. Medium: 1–4.99 g/day. High: ≥5 g/day / Wine, beer and spirits | PreD T2D PreD + T2D | Occasional drinkers | Normal glucose tolerance at baseline MEN: High alcohol: Higher risk of preD + T2D (OR 1.42, 95% CI 1.00–2.03). High beer: Higher risk of preD + T2D (OR 1.63, 95% CI 1.07–2.48) and higher risk of preD (OR 1.84, 95% CI 1.13–3.01) Abstainers vs occasional wine or beer drinkers: Higher risk of preD + T2D (OR 2.01, 95%CI 1.01–3.98 and OR 2.13, 95%CI 1.03–4.39, respectively). WOMEN: High wine: lower risk of preD (OR 0.66, 95% CI 0.43–0.99) Normal glucose tolerance or preD at baseline WOMEN: Low alcohol: Lower risk of T2D (OR 0.41, 95% 0.22–0.79). Medium wine: Lower risk of T2D (OR 0.46, 95%CI 0.24–0.88) |
| Yin et al., 2011 [58] National Health and Medical Research Council of Australia, Tasmanian Government and Royal Hobart Hospital Acute Care Programme. | Prospective cohort (2 y) | 862 (49% women) Mean age 63 y, range 51–81 | 1SDU: 10 g alcohol Frequency: Never, <once a month, 1–3 days/month, 1/2/3/4/5/6 days /wk, every day. Amount 30mL spirits: 1 glass. 1 can beer: 2 glasses. 1 bottle wine (750 mL): 6 glasses. 1 bottle sherry (750 mL): 12 glasses. g/day / Wine, beer, and spirits | BMD change | Total alcohol intake in men positively predicted change in BMD at the lumbar spine and hip (beta = 0.008% and 0.006% per year per gram of alcohol intake, p < 0.05). The frequency of drinking red wine was positively associated with percentage change in BMD at the lumbar spine in men (beta= 0.08% per year per class, p= 0.048). At baseline, lumbar spine BMD was positively associated with frequency of low-alcohol beer drinking in women (beta = 0.034 g/cm(2) per category, p = 0.002). | |
| Mukamal et al., 2007 [62] The National Heart, Lung, and Blood Institute. The National Institute on Ageing. | Prospective population-based cohort study (12 y If no hip fracture 7.5 y If hip fracture) | 5865 ≥60 y | 1 SDU: 12-ounce can or bottle of beer, 6-ounce glass of wine, and 1 shot of liquor. 1 SDUc = 14 g Categories Long-term abstainers, former drinkers, <1 drink/w, 1–6 drinks/w, 7–13 drinks/w, ≥14 drinks/w / Wine, beer, and spirits | Hip fracture BMD | Long-term abstainers | Strong, graded, positive relationship between greater alcohol consumption and greater BMD up to 13 drinks/week. U-shaped relationship between alcohol intake and risk for hip fracture (quadratic trend: p = 0.02), with lower HRs in intermediate drinking categories. Drinking <1 beer/w showed a significantly lower risk of hip fracture (HR 0.66, 95%CI 0.44–0.99). |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcos, A.; Serra-Majem, L.; Pérez-Jiménez, F.; Pascual, V.; Tinahones, F.J.; Estruch, R. Moderate Consumption of Beer and Its Effects on Cardiovascular and Metabolic Health: An Updated Review of Recent Scientific Evidence. Nutrients 2021, 13, 879. https://doi.org/10.3390/nu13030879
Marcos A, Serra-Majem L, Pérez-Jiménez F, Pascual V, Tinahones FJ, Estruch R. Moderate Consumption of Beer and Its Effects on Cardiovascular and Metabolic Health: An Updated Review of Recent Scientific Evidence. Nutrients. 2021; 13(3):879. https://doi.org/10.3390/nu13030879
Chicago/Turabian StyleMarcos, Ascensión, Lluís Serra-Majem, Francisco Pérez-Jiménez, Vicente Pascual, Francisco José Tinahones, and Ramón Estruch. 2021. "Moderate Consumption of Beer and Its Effects on Cardiovascular and Metabolic Health: An Updated Review of Recent Scientific Evidence" Nutrients 13, no. 3: 879. https://doi.org/10.3390/nu13030879
APA StyleMarcos, A., Serra-Majem, L., Pérez-Jiménez, F., Pascual, V., Tinahones, F. J., & Estruch, R. (2021). Moderate Consumption of Beer and Its Effects on Cardiovascular and Metabolic Health: An Updated Review of Recent Scientific Evidence. Nutrients, 13(3), 879. https://doi.org/10.3390/nu13030879