An Assessment of Risk Factors for Insufficient Levels of Vitamin D during Early Infancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.3. Data Analysis
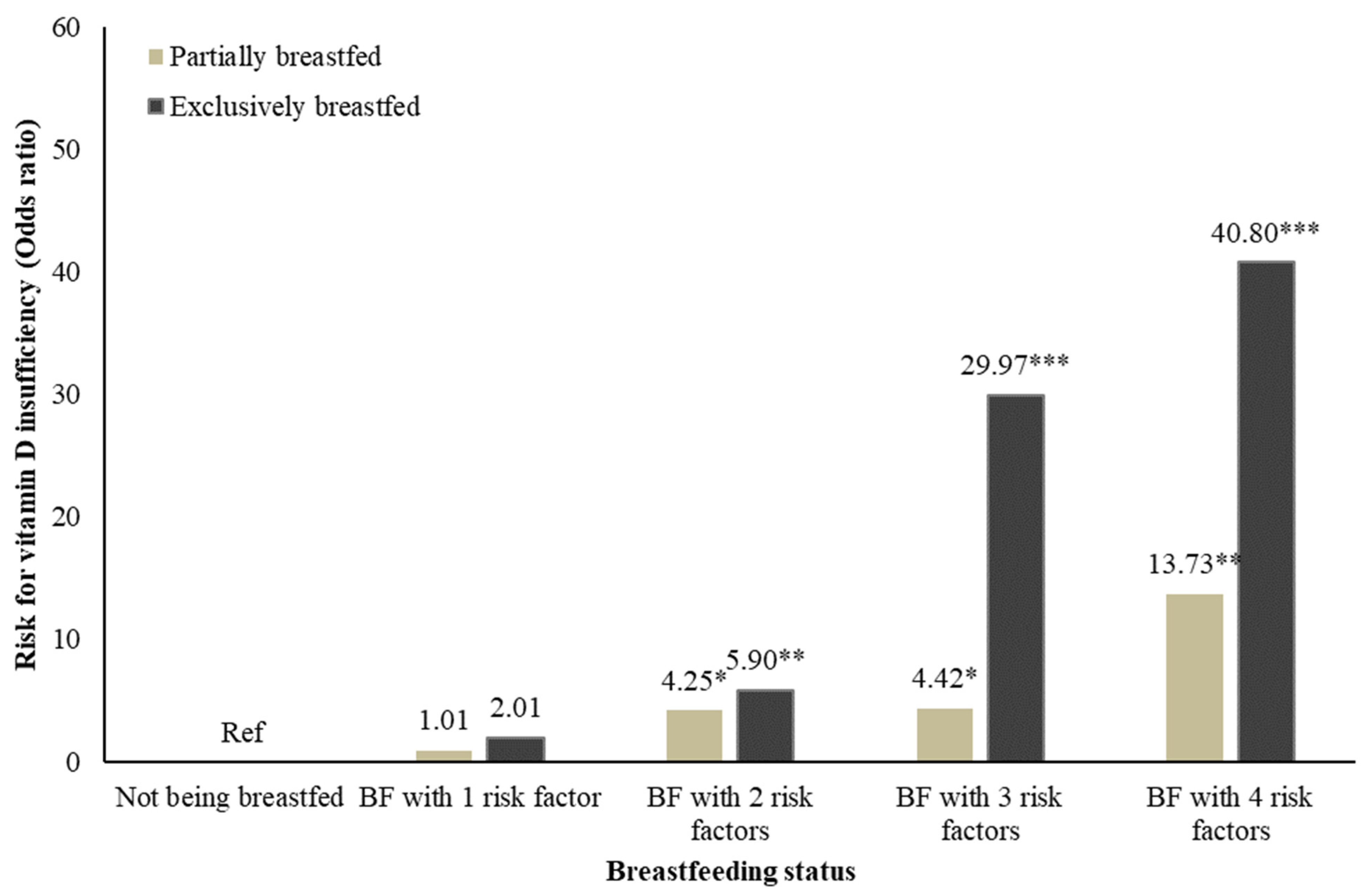
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hong Kong Department of Health. Breastfeeding Survey 2019; Department of Health, Family Health Service: Hong Kong, China, 2019.
- Dawodu, A.; Tsang, R.C. Maternal vitamin D status: Effect on milk vitamin D content and vitamin D status of breastfeeding infants. Adv. Nutr. 2012, 3, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Dawodu, A.; Zalla, L.; Woo, J.G.; Herbers, P.M.; Davidson, B.S.; Heubi, J.E.; Morrow, A.L. Heightened attention to supplementation is needed to improve the vitamin D status of breastfeeding mothers and infants when sunshine exposure is restricted. Matern. Child Nutr. 2014, 10, 383–397. [Google Scholar] [CrossRef]
- Hilger, J.; Friedel, A.; Herr, R.; Rausch, T.; Roos, F.; Wahl, D.A.; Pierroz, D.D.; Weber, P.; Hoffmann, K. A systematic review of vitamin D status in populations worldwide. Br. J. Nutr. 2014, 111, 23–45. [Google Scholar] [CrossRef] [PubMed]
- Atas, E.; Karademır, F.; Ersen, A.; Meral, C.; Aydınoz, S.; Suleymanoglu, S.; Gultepe, M.; Gocmen, İ. Comparison between daily supplementation doses of 200 versus 400 IU of vitamin D in infants. Eur. J. Pediatrics 2013, 172, 1039–1042. [Google Scholar] [CrossRef] [PubMed]
- Gallo, S.; Comeau, K.; Vanstone, C.; Agellon, S.; Sharma, A.; Jones, G.; L’Abbé, M.; Khamessan, A.; Rodd, C.; Weiler, H. Effect of different dosages of oral vitamin D supplementation on vitamin D status in healthy, breastfed infants: A randomized trial. JAMA 2013, 309, 1785–1792. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Protecting, Promoting and Supporting Breastfeeding in Facilities Providing Maternity and Newborn Services; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Gallo, S.; Jean-Philippe, S.; Rodd, C.; Weiler, H.A. Vitamin D supplementation of Canadian infants: Practices of Montreal mothers. Appl. Physiol. Nutr. Metab. 2010, 35, 303–309. [Google Scholar] [CrossRef]
- Chan, K.C.C.; Tam, W.H.; Chan, M.H.M.; Chan, R.S.M.; Li, A.M. Vitamin D deficiency among healthy infants in Hong Kong: A pilot study. Hong Kong Med. J. 2018, 24 (Suppl. 3), 32–35. [Google Scholar]
- Mithal, A.; Wahl, D.A.; Bonjour, J.-P.; Burckhardt, P.; Dawson-Hughes, B.; Eisman, J.A.; Fuleihan, G.E.-H.; Josse, R.G.; Lips, P.; Morales-Torres, J. Global vitamin D status and determinants of hypovitaminosis D. Osteoporos. Int. 2009, 20, 1807–1820. [Google Scholar] [CrossRef]
- Basit, S. Vitamin D in health and disease: A literature review. Br. J. Biomed. Sci. 2013, 70, 161–172. [Google Scholar] [CrossRef]
- Wagner, C.L.; Greer, F.R. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics 2008, 122, 1142–1152. [Google Scholar] [CrossRef]
- Hyppönen, E.; Läärä, E.; Reunanen, A.; Järvelin, M.-R.; Virtanen, S.M. Intake of vitamin D and risk of type 1 diabetes: A birth-cohort study. Lancent 2001, 358, 1500–1503. [Google Scholar] [CrossRef]
- Ascherio, A.; Munger, K.L.; Simon, K.C. Vitamin D and multiple sclerosis. Lancet Neurol. 2010, 9, 599–612. [Google Scholar] [CrossRef]
- Kilkkinen, A.; Knekt, P.; Aro, A.; Rissanen, H.; Marniemi, J.; Heliövaara, M.; Impivaara, O.; Reunanen, A. Vitamin D status and the risk of cardiovascular disease death. Am. J. Epidemiol. 2009, 170, 1032–1039. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am. J. Clin. Nutr. 2004, 80, 1678S–1688S. [Google Scholar] [CrossRef] [PubMed]
- Misra, M.; Pacaud, D.; Petryk, A.; Collett-Solberg, P.F.; Kappy, M. Vitamin D deficiency in children and its management: Review of current knowledge and recommendations. Pediatrics 2008, 122, 398–417. [Google Scholar] [CrossRef]
- Andıran, N.; Yordam, N.; Özön, A. Risk factors for vitamin d deficiency in breast-fed newborns and their mothers. Nutrition 2002, 18, 47–50. [Google Scholar] [CrossRef]
- Hooper, S.R.; Burchinal, M.R.; Roberts, J.E.; Zeisel, S.; Neebe, E.C. Social and family risk factors for infant development at one year: An application of the cumulative risk model. J. Appl. Dev. Psychol. 1998, 19, 85–96. [Google Scholar] [CrossRef]
- Koinis-Mitchell, D.; McQuaid, E.L.; Seifer, R.; Kopel, S.J.; Esteban, C.; Canino, G.; Garcia-Coll, C.; Klein, R.; Fritz, G.K. Multiple urban and asthma-related risks and their association with asthma morbidity in children. J. Pediatric Psychol. 2007, 32, 582–595. [Google Scholar] [CrossRef] [PubMed]
- Vitamin D Roundtable on the NHANES Monitoring of Serum 25D: Assay Challenges Options for Resolving Them, NHANES Monitoring of Serum 25-Hydroxyvitamin D: A Roundtable Summary. J. Nutr. 2010, 140, 2030S–2045S. [CrossRef] [PubMed]
- Carter, G.D.; Berry, J.; Durazo-Arvizu, R.; Gunter, E.; Jones, G.; Jones, J.; Makin, H.L.J.; Pattni, P.; Phinney, K.W.; Sempos, C.T.; et al. Quality assessment of vitamin D metabolite assays used by clinical and research laboratories. J. Steroid Biochem. Mol. Biol. 2017, 173, 100–104. [Google Scholar] [CrossRef]
- Amrein, K.; Scherkl, M.; Hoffmann, M.; Neuwersch-Sommeregger, S.; Köstenberger, M.; Tmava Berisha, A.; Martucci, G.; Pilz, S.; Malle, O. Vitamin D deficiency 2.0: An update on the current status worldwide. Eur. J. Clin. Nutr. 2020, 74, 1498–1513. [Google Scholar] [CrossRef] [PubMed]
- Noel-Weiss, J.; Taljaard, M.; Kujawa-Myles, S. Breastfeeding and lactation research: Exploring a tool to measure infant feeding patterns. Int. Breastfeed. J. 2014, 9, 5. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Diet and Nutrition Survey of Infants and Young Children; Department of Health: London, UK, 2011.
- Leung, Y.K.; Cheng, Y.Y.; Ginn, E.W.L. Technical Note (Local) No. 80—Solar Ultraviolet Index in Hong Kong, 1999–2003; Hong Kong Observatory: Hong Kong, China, 2004.
- Vanicek, K.; Frei, T.; Litynska, Z.; Schmalwieser, A. UV-Index for the Public; COST-713 Action; European Union: Brussels, Belgium, 2000. [Google Scholar]
- Ziegler, E.E.; Hollis, B.W.; Nelson, S.E.; Jeter, J.M. Vitamin D deficiency in breastfed infants in Iowa. Pediatrics 2006, 118, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Mulligan, M.L.; Felton, S.K.; Riek, A.E.; Bernal-Mizrachi, C. Implications of vitamin D deficiency in pregnancy and lactation. Am. J. Obstet. Gynecol. 2010, 202, 429.e1–429.e9. [Google Scholar] [CrossRef]
- Mohamed, H.J.J.; Rowan, A.; Fong, B.; Loy, S.-L. Maternal serum and breast milk vitamin D levels: Findings from the Universiti Sains Malaysia Pregnancy Cohort Study. PLoS ONE 2014, 9, e100705. [Google Scholar] [CrossRef]
- Jain, V.; Gupta, N.; Kalaivani, M.; Jain, A.; Sinha, A.; Agarwal, R. Vitamin D deficiency in healthy breastfed term infants at 3 months & their mothers in India: Seasonal variation & determinants. Indian J. Med Res. 2011, 133, 267. [Google Scholar]
- Dawodu, A.; Wagner, C.L. Mother-child vitamin D deficiency: An international perspective. Arch. Dis. Child. 2007, 92, 737–740. [Google Scholar] [CrossRef]
- Hatun, S.; Ozkan, B.; Orbak, Z.; Doneray, H.; Cizmecioglu, F.; Toprak, D.; Calikoglu, A.S.H. Vitamin D deficiency in early infancy. J. Nutr. 2005, 135, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Specker, B.L.; Valanis, B.; Hertzberg, V.; Edwards, N.; Tsang, R.C. Sunshine exposure and serum 25-hydroxyvitamin D concentrations in exclusively breast-fed infants. J. Pediatrics 1985, 107, 372–376. [Google Scholar] [CrossRef]
- Dawodu, A.; Akinbi, H. Vitamin D nutrition in pregnancy: Current opinion. Int. J. Women’s Health 2013, 5, 333. [Google Scholar] [CrossRef] [PubMed]
- Cole, C.R.; Grant, F.K.; Tangpricha, V.; Swaby-Ellis, E.D.; Smith, J.L.; Jacques, A.; Chen, H.; Schleicher, R.L.; Ziegler, T.R. 25-hydroxyvitamin D status of healthy, low-income, minority children in Atlanta, Georgia. J. Am. Acad. Pediatrics 2010, 125, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Li, X.; Zhao, A.; Zheng, W.; Guo, M.; Xue, Y.; Wang, P.; Zhang, Y. High Prevalence of Insufficient Vitamin D Intake and Serum 25-Hydroxyvitamin D in Chinese School-Age Children: A Cross-Sectional Study. Nutrients 2018, 10, 822. [Google Scholar] [CrossRef]
- Ruan, Y.; Zhang, Q.; Li, J.; Wan, R.; Bai, J.; Wang, W.; Zhou, Y.; Wan, Q.; Zhao, J.; Yu, S. Factors associated with exclusive breast-feeding: A cross-sectional survey in Kaiyuan, Yunnan, Southwest China. PLoS ONE 2019, 14, e0223251. [Google Scholar] [CrossRef] [PubMed]
- Lange, N.E.; Sparrow, D.; Vokonas, P.; Litonjua, A.A. Vitamin D deficiency, smoking, and lung function in the Normative Aging Study. Am. J. Respir. Crit. Care Med. 2012, 186, 616–621. [Google Scholar] [CrossRef] [PubMed]
- Banihosseini, S.Z.; Baheiraei, A.; Shirzad, N.; Heshmat, R.; Mohsenifar, A. The effect of cigarette smoke exposure on vitamin D level and biochemical parameters of mothers and neonates. J. Diabetes Metab. Disord. 2013, 12, 19. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Choi, Y.J.; Kim, M.K.; Jeong, S.J. Vitamin D deficiency in infants aged 1 to 6 months. Korean J. Pediatrics 2013, 56, 205. [Google Scholar] [CrossRef] [PubMed]
- Krementsov, D.N.; Asarian, L.; Fang, Q.; McGill, M.M.; Teuscher, C. Sex-Specific Gene-by-Vitamin D Interactions Regulate Susceptibility to Central Nervous System Autoimmunity. Front. Immunol. 2018, 9, 1622. [Google Scholar] [CrossRef] [PubMed]
- Fink, C.; Peters, R.L.; Koplin, J.J.; Brown, J.; Allen, K.J. Factors Affecting Vitamin D Status in Infants. Children 2019, 6, 7. [Google Scholar] [CrossRef]
- Urrutia-Pereira, M.; Solé, D. Vitamin D deficiency in pregnancy and its impact on the fetus, the newborn and in childhood. Rev. Paul. De Pediatr. 2015, 33, 104–113. [Google Scholar] [CrossRef]
- Mohamed, M.J.; Ochola, S.; Owino, V.O. Comparison of knowledge, attitudes and practices on exclusive breastfeeding between primiparous and multiparous mothers attending Wajir District hospital, Wajir County, Kenya: A cross-sectional analytical study. Int. Breastfeed. J. 2018, 13, 11. [Google Scholar] [CrossRef] [PubMed]
- Hackman, N.M.; Schaefer, E.W.; Beiler, J.S.; Rose, C.M.; Paul, I.M. Breastfeeding outcome comparison by parity. Breastfeed. Med. 2015, 10, 156–162. [Google Scholar] [CrossRef]
- Lanier, P.; Jonson-Reid, M. Comparing Primiparous and Multiparous Mothers in a Nurse Home Visiting Prevention Program. Birth 2014, 41, 344–352. [Google Scholar] [CrossRef] [PubMed]
- Lagerberg, D.; Magnusson, M. Utilization of child health services, stress, social support and child characteristics in primiparous and multiparous mothers of 18-month-old children. Scand. J. Public Health 2013, 41, 374–383. [Google Scholar] [CrossRef]
- Bentley, M.E.; Johnson, S.L.; Wasser, H.; Creed-Kanashiro, H.; Shroff, M.; Fernandez-Rao, S.; Cunningham, M. Formative research methods for designing culturally appropriate, integrated child nutrition and development interventions: An overview. Ann. N. Y. Acad. Sci. 2014, 1308, 54. [Google Scholar] [CrossRef] [PubMed]
- Prado, E.L.; Dewey, K.G. Nutrition and brain development in early life. Nutr. Rev. 2014, 72, 267–284. [Google Scholar] [CrossRef]
- Cashman, K.D. Vitamin D in childhood and adolescence. Postgrad. Med. J. 2007, 83, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Rothman, M.; Faber, M.; Covic, N.; Matsungo, T.M.; Cockeran, M.; Kvalsvig, J.D.; Smuts, C.M.J.N. Infant development at the age of 6 months in relation to feeding practices, Iron status, and growth in a peri-urban community of South Africa. Nutrients 2018, 10, 73. [Google Scholar] [CrossRef] [PubMed]
| Total | Sufficient Vitamin D (25(OH)D > 50 nmol/L) | Insufficient Vitamin D (25(OH)D ≤ 50 nmol/L) | p-Value | |
|---|---|---|---|---|
| (N = 208) | (N = 131) | (N = 77) | ||
| Age, month, mean (SD) | 4.36 (1.6) | 4.69 (1.4) | 3.79 (1.6) | <0.001 |
| Sex, N (%) | 0.084 | |||
| Boys | 112 (53.8%) | 77 (58.8%) | 35 (45.5%) | |
| Girls | 96 (46.2%) | 54 (41.2%) | 42 (54.5%) | |
| Mother’s occupation, N (%) | 0.462 | |||
| Housewife/ Home maker | 91 (43.8%) | 60 (45.8%) | 31 (40.3%) | |
| Full-time employed | 100 (48.1%) | 58 (44.3%) | 42 (54.5%) | |
| Part-time employed | 6 (2.9%) | 5 (3.8%) | 1 (1.3%) | |
| Mother’s educational level, N (%) | 0.117 | |||
| Lower secondary education or below | 19 (9.1%) | 12 (9.2%) | 7 (9.1%) | |
| Upper secondary education | 57 (27.4%) | 39 (29.8%) | 18 (23.4%) | |
| Tertiary education or above | 129 (62.0%) | 78 (59.5%) | 51 (66.2%) | |
| 1 Family income, N (%) | 0.937 | |||
| Low income | 68 (32.7%) | 44 (33.6%) | 24 (31.2%) | |
| Median income | 36 (17.3%) | 22 (16.8%) | 14 (18.2%) | |
| High income | 93 (44.7%) | 59 (45.0%) | 34 (44.2%) | |
| Infants’ vitamin D supplementation intake, N (%) | 0.211 | |||
| Yes | 18 (8.7%) | 14 (10.7%) | 4 (5.2%) | |
| No | 189 (90.9%) | 117 (89.3%) | 72 (93.5%) | |
| Having a multiparous mother | 0.001 | |||
| Yes | 94 (45.2%) | 48 (36.6%) | 46 (59.7%) | |
| No | 112 (53.8%) | 82 (62.6%) | 30 (39.0%) | |
| Breastfeeding, N (%) | <0.001 | |||
| Yes | 142 (68.3%) | 72 (55.0%) | 70 (90.9%) | |
| Partially | 76 (36.5%) | 53 (40.5%) | 23 (29.9%) | |
| Exclusively | 66 (31.7%) | 19 (14.5%) | 47 (61.0%) | |
| No | 66 (31.7%) | 59 (45.0%) | 7 (9.1%) | |
| Use of sun cream, N (%) | 0.128 | |||
| Yes | 42 (20.2%) | 22 (16.8%) | 20 (26.0%) | |
| No | 151 (72.6%) | 96 (73.3%) | 55 (71.4%) | |
| Mothers with smoking history, N (%) | 0.541 | |||
| Yes | 12 (5.8%) | 9 (6.9%) | 3 (3.9%) | |
| No | 192 (92.3%) | 120 (91.6%) | 72 (93.5%) |
| Risk of Vitamin D Insufficiency (25(OH)D <50nmol/L) | ||||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | aOR (95% CI) + | p | aOR (95% CI) $ | p | |
| Being breastfed | 9.10 (3.69, 22.48) | <0.001 | 9.80 (3.81, 25.21) | <0.001 | 12.81 (4.47, 36.71) | <0.001 |
| Partially breastfed | 4.12 (1.56, 10.91) | 0.004 | 4.35 (1.57, 12.03) | 0.005 | 5.62 (1.82, 17.33) | 0.003 |
| Exclusively breastfed | 23.00 (8.49, 62.31) | <0.001 | 27.76 (9.47, 81.34) | <0.001 | 36.14 (10.84, 120.54) | <0.001 |
| Other risk factors | ||||||
| As a girl | 1.71 (0.97, 3.02) | 0.064 | 1.87 (1.02, 3.41) | 0.041 | 4.30 (1.87, 9.91) | 0.001 |
| From a low-income family | 0.92 (0.50, 1.70) | 0.791 | 0.87 (0.45, 1.65) | 0.662 | 1.13 (0.46, 2.79) | 0.789 |
| Having a multiparous mother | 2.62 (1.46, 4.69) | 0.001 | 3.32 (1.76, 6.29) | <0.001 | 3.74 (1.69, 8.25) | 0.001 |
| No vitamin supplementation intake | 2.15 (0.68, 6.80) | 0.191 | 2.12 (0.65, 6.93) | 0.216 | 3.93 (0.92, 16.80) | 0.065 |
| Applied sun cream by parents | 1.59 (0.80, 3.16) | 0.190 | 1.96 (0.92, 4.17) | 0.080 | 4.08 (1.29, 12.92) | 0.017 |
| Mothers with a smoking history | 0.56 (0.15, 2.12) | 0.390 | 0.35 (0.09, 1.46) | 0.151 | 0.55 (0.09, 3.21) | 0.504 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tung, K.T.S.; Wong, R.S.; Tsang, H.W.; Chan, B.N.K.; Wong, S.Y.; So, H.-K.; Tung, J.Y.L.; Ho, M.H.K.; Wong, W.H.S.; Ip, P. An Assessment of Risk Factors for Insufficient Levels of Vitamin D during Early Infancy. Nutrients 2021, 13, 1068. https://doi.org/10.3390/nu13041068
Tung KTS, Wong RS, Tsang HW, Chan BNK, Wong SY, So H-K, Tung JYL, Ho MHK, Wong WHS, Ip P. An Assessment of Risk Factors for Insufficient Levels of Vitamin D during Early Infancy. Nutrients. 2021; 13(4):1068. https://doi.org/10.3390/nu13041068
Chicago/Turabian StyleTung, Keith T. S., Rosa S. Wong, Hing Wai Tsang, Bianca N. K. Chan, Siew Yan Wong, Hung-Kwan So, Joanna Y. L. Tung, Marco H. K. Ho, Wilfred H. S. Wong, and Patrick Ip. 2021. "An Assessment of Risk Factors for Insufficient Levels of Vitamin D during Early Infancy" Nutrients 13, no. 4: 1068. https://doi.org/10.3390/nu13041068
APA StyleTung, K. T. S., Wong, R. S., Tsang, H. W., Chan, B. N. K., Wong, S. Y., So, H.-K., Tung, J. Y. L., Ho, M. H. K., Wong, W. H. S., & Ip, P. (2021). An Assessment of Risk Factors for Insufficient Levels of Vitamin D during Early Infancy. Nutrients, 13(4), 1068. https://doi.org/10.3390/nu13041068









