Mediterranean-Style Diet and Birth Outcomes in an Urban, Multiethnic, and Low-Income US Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cohort Design
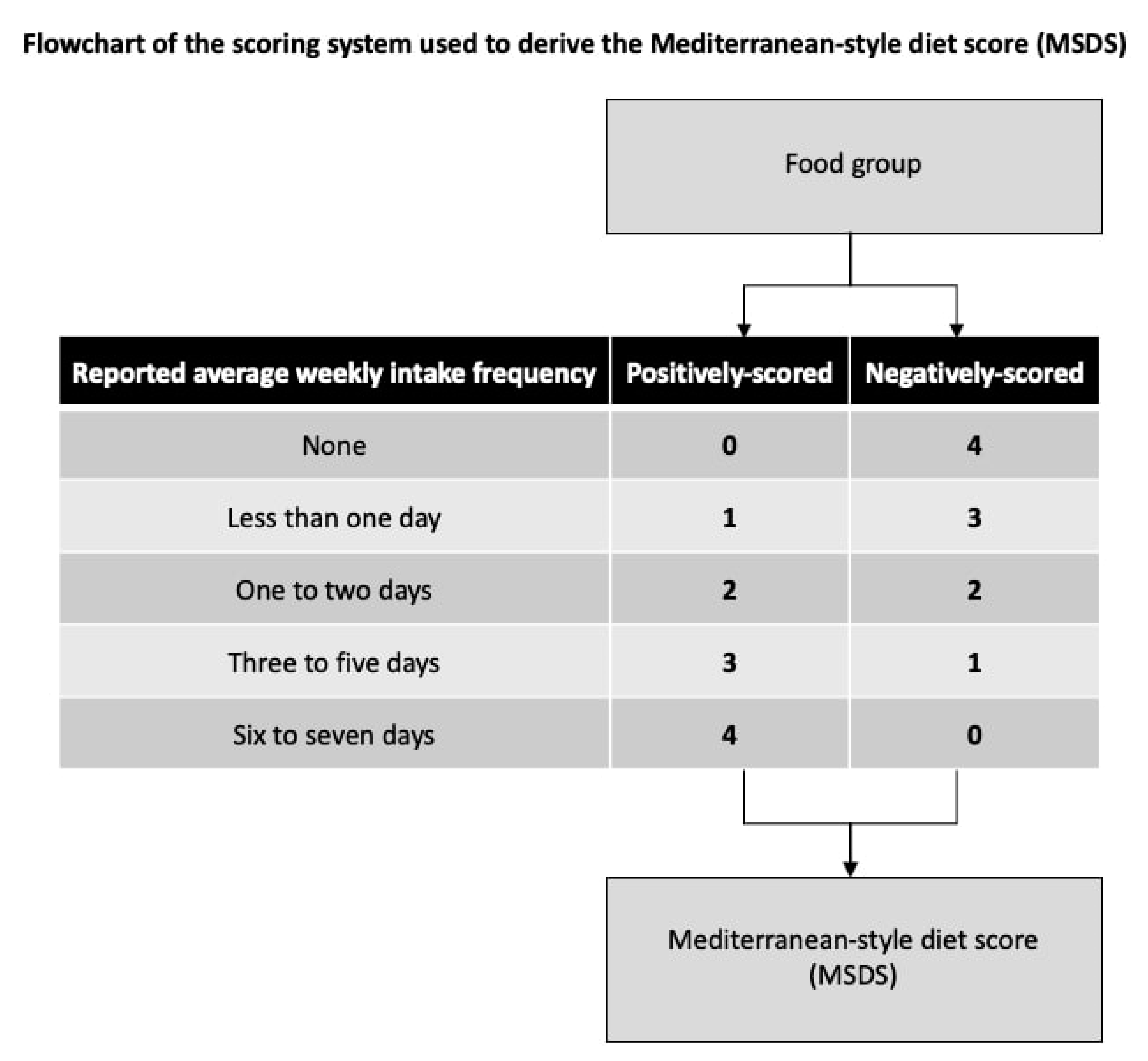
2.2. Dietary Assessment
2.3. Assessment of Covariates
2.4. Assessment of Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Preterm Birth. Available online: https://www.who.int/news-room/fact-sheets/detail/preterm-birth (accessed on 13 June 2020).
- Preterm Birth|Maternal and Infant Health|Reproductive Health|CDC. Available online: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm (accessed on 13 June 2020).
- Premature Births Cost Health Plans $6 Billion Annually: New Study in Pediatrics Provides Estimate of High Costs of Premature Infants Especially Those with Major Birth Defects. ScienceDaily. Available online: https://www.sciencedaily.com/releases/2017/09/170921090256.htm (accessed on 13 June 2020).
- Schieve, L.A.; Tian, L.H.; Rankin, K.; Kogan, M.D.; Yeargin-Allsopp, M.; Visser, S.; Rosenberg, D. Population impact of preterm birth and low birth weight on developmental disabilities in US children. Ann. Epidemiol. 2016, 26, 267–274. [Google Scholar] [CrossRef] [Green Version]
- Moss, T.J. Respiratory Consequences of Preterm Birth. Clin. Exp. Pharmacol. Physiol. 2006, 33, 280–284. [Google Scholar] [CrossRef] [PubMed]
- Ream, M.A.; Lehwald, L. Neurologic Consequences of Preterm Birth. Curr. Neurol. Neurosci. Rep. 2018, 18, 48. [Google Scholar] [CrossRef] [PubMed]
- Henderson, J.; Carson, C.; Redshaw, M. Impact of preterm birth on maternal well-being and women’s perceptions of their baby: A population-based survey. BMJ Open 2016, 6, e012676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jonn-Seed, M.S.; Weiss, S. Maternal Expressed Emotion as a Predictor of Emotional and Behavioral Problems in Low Birth Weight Children. Issues Ment. Health Nurs. 2002, 23, 649–672. [Google Scholar] [CrossRef]
- Stylianou-Riga, P.; Kouis, P.; Kinni, P.; Rigas, A.; Papadouri, T.; Yiallouros, P.K.; Theodorou, M. Maternal socioeconomic factors and the risk of premature birth and low birth weight in Cyprus: A case-control study. Reprod. Health 2018, 15, 157. [Google Scholar] [CrossRef]
- Shapiro-Mendoza, C.K.; Lackritz, E.M. Epidemiology of late and moderate preterm birth. Semin. Fetal Neonatal Med. 2012, 17, 120–125. [Google Scholar] [CrossRef] [Green Version]
- Kosa, J.L.; Guendelman, S.; Pearl, M.; Graham, S.; Abrams, B.; Kharrazi, M. The Association Between Pre-pregnancy BMI and Preterm Delivery in a Diverse Southern California Population of Working Women. Matern. Child Health J. 2010, 15, 772–781. [Google Scholar] [CrossRef] [Green Version]
- Shah, P.S. Parity and low birth weight and preterm birth: A systematic review and meta-analyses. Acta Obstet. Gynecol. Scand. 2010, 89, 862–875. [Google Scholar] [CrossRef]
- De Bernabé, J.V.; Soriano, T.; Albaladejo, R.; Juarranz, M.; Calle, M.E.; Martínez, D.; Domínguez-Rojas, V. Risk factors for low birth weight: A review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2004, 116, 3–15. [Google Scholar] [CrossRef]
- Di Renzo, G.C.; Rosati, A.; Sarti, R.D.; Cruciani, L.; Cutuli, A.M. Does fetal sex affect pregnancy outcome? Gend. Med. 2007, 4, 19–30. [Google Scholar] [CrossRef]
- Stevenson, D.K.; Verter, J.; Fanaroff, A.A.; Oh, W.; Ehrenkranz, R.A.; Shankaran, S.; Donovan, E.F.; Wright, L.L.; Lemons, J.A.; Tyson, J.E.; et al. Sex differences in outcomes of very low birthweight infants: The newborn male disadvantage. Arch. Dis. Child. Fetal Neonatal Ed. 2000, 83, 182–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varner, M.W.; Esplin, M.S. Current understanding of genetic factors in preterm birth. BJOG Int. J. Obstet. Gynaecol. 2005, 112, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Yaghootkar, H.; Freathy, R.M. Genetic origins of low birth weight. Curr. Opin. Clin. Nutr. Metab. Care 2012, 15, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Srivastava, A.; Bacelis, J.; Juodakis, J.; Jacobsson, B.; Muglia, L.J. Genetic studies of gestational duration and preterm birth. Best Pr. Res. Clin. Obstet. Gynaecol. 2018, 52, 33–47. [Google Scholar] [CrossRef]
- Spiegler, J.; Network, G.T.G.N.; Stichtenoth, G.; Weichert, J.; König, I.R.; Schlaud, M.; Wense, A.V.; Olbertz, D.; Gurth, H.; Schiffmann, J.-H.; et al. Pregnancy risk factors for very premature delivery: What role do hypertension, obesity and diabetes play? Arch. Gynecol. Obstet. 2013, 288, 57–64. [Google Scholar] [CrossRef]
- Persson, M.; Shah, P.S.; Rusconi, F.; Reichman, B.; Modi, N.; Kusuda, S.; Lehtonen, L.; Håkansson, S.; Yang, J.; Isayama, T.; et al. Association of Maternal Diabetes with Neonatal Outcomes of Very Preterm and Very Low-Birth-Weight Infants: An International Cohort Study. JAMA Pediatr. 2018, 172, 867–875. [Google Scholar] [CrossRef]
- Ratnasiri, A.W.G.; Parry, S.S.; Arief, V.N.; DeLacy, I.H.; Halliday, L.A.; Dilibero, R.J.; Basford, K.E. Recent trends, risk factors, and disparities in low birth weight in California, 2005–2014: A retrospective study. Matern. Health Neonatol. Perinatol. 2018, 4, 1–13. [Google Scholar] [CrossRef] [Green Version]
- Collins, J.W.; David, R.J.; Simon, D.M.; Prachand, N.G. Preterm birth among African American and white women with a lifelong residence in high-income Chicago neighborhoods: An exploratory study. Ethn. Dis. 2007, 17, 113–117. [Google Scholar]
- Kramer, M.R.; Hogue, C.R. What Causes Racial Disparities in Very Preterm Birth? A Biosocial Perspective. Epidemiol. Rev. 2009, 31, 84–98. [Google Scholar] [CrossRef]
- Gete, D.G.; Waller, M.; Mishra, G.D. Effects of maternal diets on preterm birth and low birth weight: A systematic review. Br. J. Nutr. 2019, 123, 446–461. [Google Scholar] [CrossRef]
- Kibret, K.T.; Chojenta, C.; Gresham, E.; Tegegne, T.K.; Loxton, D. Maternal dietary patterns and risk of adverse pregnancy (hypertensive disorders of pregnancy and gestational diabetes mellitus) and birth (preterm birth and low birth weight) outcomes: A systematic review and meta-analysis. Public Health Nutr. 2018, 22, 506–520. [Google Scholar] [CrossRef]
- Davis, C.R.; Bryan, J.; Hodgson, J.M.; Murphy, K.J. Definition of the Mediterranean Diet; A Literature Review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Sofi, F.; Dinu, M.; Pagliai, G.; Marcucci, R.; Casini, A. Validation of a literature-based adherence score to Mediterranean diet: The MEDI-LITE score. Int. J. Food Sci. Nutr. 2017, 68, 757–762. [Google Scholar] [CrossRef]
- D’Alessandro, A.; De Pergola, G. The Mediterranean Diet: Its definition and evaluation of a priori dietary indexes in primary cardiovascular prevention. Int. J. Food Sci. Nutr. 2018, 69, 647–659. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Tomaino, L.; Dernini, S.; Berry, E.M.; Lairon, D.; De La Cruz, J.N.; Bach-Faig, A.; Donini, L.M.; Medina, F.-X.; Belahsen, R.; et al. Updating the Mediterranean Diet Pyramid towards Sustainability: Focus on Environmental Concerns. Int. J. Environ. Res. Public Health 2020, 17, 8758. [Google Scholar] [CrossRef] [PubMed]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mikkelsen, T.B.; Østerdal, M.L.; Knudsen, V.K.; Haugen, M.; Meltzer, H.M.; Bakketeig, L.; Olsen, S.F. Association between a Mediterranean-type diet and risk of preterm birth among Danish women: A prospective cohort study. Acta Obstet. Gynecol. Scand. 2008, 87, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Chatzi, L.; Méndez, M.A.; García, A.T.; Roumeliotaki, T.; Ibarluzea, J.; Tardón, A.; Amiano, P.; Lertxundi, A.; Iñiguez, C.; Vioque, J.; et al. Mediterranean diet adherence during pregnancy and fetal growth: INMA (Spain) and RHEA (Greece) mother–child cohort studies. Br. J. Nutr. 2011, 107, 135–145. [Google Scholar] [CrossRef]
- Parlapani, E.; Agakidis, C.; Karagiozoglou-Lampoudi, T.; Sarafidis, K.; Agakidou, E.; Athanasiadis, A.; Diamanti, E. The Mediterranean diet adherence by pregnant women delivering prematurely: Association with size at birth and complications of prematurity. J. Matern. Neonatal Med. 2017, 32, 1084–1091. [Google Scholar] [CrossRef]
- Martínez-Galiano, J.M.; Olmedo-Requena, R.; Barrios-Rodríguez, R.; Amezcua-Prieto, C.; Bueno-Cavanillas, A.; Salcedo-Bellido, I.; Jimenez-Moleon, J.J.; Delgado-Rodríguez, M. Effect of Adherence to a Mediterranean Diet and Olive Oil Intake during Pregnancy on Risk of Small for Gestational Age Infants. Nutrients 2018, 10, 1234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amati, F.; Hassounah, S.; Swaka, A. The Impact of Mediterranean Dietary Patterns During Pregnancy on Maternal and Offspring Health. Nutrients 2019, 11, 1098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raghavan, R.; Dreibelbis, C.; Kingshipp, B.L.; Wong, Y.P.; Abrams, B.; Gernand, A.D.; Rasmussen, K.M.; Siega-Riz, A.M.; Stang, J.; Casavale, K.O.; et al. Dietary patterns before and during pregnancy and birth outcomes: A systematic review. Am. J. Clin. Nutr. 2019, 109, 729S–756S. [Google Scholar] [CrossRef] [PubMed]
- Azuine, R.E.; Ji, Y.; Chang, H.-Y.; Kim, Y.; Ji, H.; DiBari, J.; Hong, X.; Wang, G.; Singh, G.K.; Pearson, C.; et al. Prenatal Risk Factors and Perinatal and Postnatal Outcomes Associated with Maternal Opioid Exposure in an Urban, Low-Income, Multiethnic US Population. JAMA Netw. Open 2019, 2, e196405. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Zuckerman, B.; Pearson, C.; Kaufman, G.; Chen, C.; Wang, G.; Niu, T.; Wise, P.H.; Bauchner, H.; Xu, X. Maternal Cigarette Smoking, Metabolic Gene Polymorphism, and Infant Birth Weight. JAMA 2002, 287, 195–202. [Google Scholar] [CrossRef] [Green Version]
- Ferré, C.; Callaghan, W.; Olson, C.; Sharma, A.; Barfield, W. Effects of Maternal Age and Age-Specific Preterm Birth Rates on Overall Preterm Birth Rates—United States, 2007 and 2014. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 1181–1184. [Google Scholar] [CrossRef] [Green Version]
- Womack, L.S. Singleton Low Birthweight Rates, by Race and Hispanic Origin: United States, 2006–2016. NCHS Data Brief 2018, 306, 1–8, pmid:29616897. [Google Scholar]
- Shim, J.-S.; Oh, K.; Kim, H.C. Dietary assessment methods in epidemiologic studies. Epidemiol. Health 2014, 36, e2014009. [Google Scholar] [CrossRef]
- Peng, L.; Lei, L. A Review of Missing Data Treatment Methods. Intell. Inf. Manag. Syst. Technol. 2005, 1, 412–419. [Google Scholar]
- Wang, L.; Wang, X.; Laird, N.; Zuckerman, B.; Stubblefield, P.; Xu, X. Polymorphism in Maternal LRP8 Gene Is Associated with Fetal Growth. Am. J. Hum. Genet. 2006, 78, 770–777. [Google Scholar] [CrossRef] [Green Version]
- Wang, H.; Mueller, N.; Wang, G.; Hong, X.; Chen, T.; Ji, Y.; Pearson, C.; Appel, L.J.; Wang, X. The Joint Association of Small for Gestational Age and Nighttime Sleep with Blood Pressure in Childhood. Sci. Rep. 2018, 8, 9632. [Google Scholar] [CrossRef]
- Gresham, E.; Byles, J.E.; Bisquera, A.; Hure, A.J. Effects of dietary interventions on neonatal and infant outcomes: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2014, 100, 1298–1321. [Google Scholar] [CrossRef] [Green Version]
- Chango, A.; Pogribny, I.P. Considering Maternal Dietary Modulators for Epigenetic Regulation and Programming of the Fetal Epigenome. Nutrients 2015, 7, 2748–2770. [Google Scholar] [CrossRef] [Green Version]
- Meltzer, H.M.; Brantsæter, A.L.; Nilsen, R.M.; Magnus, P.; Alexander, J.; Haugen, M. Effect of dietary factors in pregnancy on risk of pregnancy complications: Results from the Norwegian Mother and Child Cohort Study. Am. J. Clin. Nutr. 2011, 94, 1970S–1974S. [Google Scholar] [CrossRef] [Green Version]
- Hajianfar, H.; Esmaillzadeh, A.; Feizi, A.; Shahshahan, Z.; Azadbakht, L. Major Maternal Dietary Patterns during Early Pregnancy and Their Association with Neonatal Anthropometric Measurement. BioMed Res. Int. 2018, 2018, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emond, J.A.; Karagas, M.R.; Baker, E.R.; Gilbert-Diamond, D. Better Diet Quality during Pregnancy Is Associated with a Reduced Likelihood of an Infant Born Small for Gestational Age: An Analysis of the Prospective New Hampshire Birth Cohort Study. J. Nutr. 2018, 148, 22–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saunders, L.; Guldner, L.; Costet, N.; Kadhel, P.; Rouget, F.; Monfort, C.; Thomé, J.-P.; Multigner, L.; Cordier, S. Effect of a Mediterranean Diet during Pregnancy on Fetal Growth and Preterm Delivery: Results from a French Caribbean Mother-Child Cohort Study (TIMOUN). Paediatr. Périnat. Epidemiol. 2014, 28, 235–244. [Google Scholar] [CrossRef] [Green Version]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014, 17, 2769–2782. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panagiotakos, D.B.; Pitsavos, C.; Arvaniti, F.; Stefanadis, C. Adherence to the Mediterranean food pattern predicts the prevalence of hypertension, hypercholesterolemia, diabetes and obesity, among healthy adults; the accuracy of the MedDietScore. Prev. Med. 2007, 44, 335–340. [Google Scholar] [CrossRef] [PubMed]




| N (%) | ||||||
|---|---|---|---|---|---|---|
| Baseline Characteristics | Total | Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 |
| No. | 8507 | 2173 (25.5) | 1481 (17.4) | 1832 (21.5) | 1536 (18.1) | 1485 (17.5) |
| Maternal age (years) # | ||||||
| <21 | 1270 (14.9) | 440 (20.3) | 227 (15.3) | 293 (16.0) | 168 (10.9) | 142 (9.6) |
| 21–30 | 3940 (46.3) | 1042 (48.0) | 703 (47.5) | 845 (46.1) | 710 (46.2) | 640 (43.1) |
| >30 | 3297 (38.8) | 691 (31.8) | 551 (37.2) | 694 (37.9) | 658 (42.8) | 703 (47.3) |
| Race or ethnicity # | ||||||
| African American * | 4030 (47.4) | 1021 (47.0) | 719 (48.6) | 848 (46.3) | 750 (48.8) | 692 (46.6) |
| Non-Hispanic White | 1005 (11.8) | 395 (18.2) | 176 (11.9) | 194 (10.6) | 135 (8.8) | 105 (7.1) |
| Hispanic | 2423 (28.5) | 535 (24.6) | 423 (28.6) | 575 (31.4) | 460 (30.0) | 430 (29.0) |
| Other † | 1049 (12.3) | 222 (10.2) | 163 (11.0) | 215 (11.7) | 191 (12.4) | 258 (17.4) |
| Education level # | ||||||
| Less than HS | 2688 (31.6) | 774 (35.6) | 456 (30.8) | 612 (33.4) | 457 (29.8) | 389 (26.2) |
| HS or equivalent | 2879 (33.8) | 744 (34.2) | 513 (34.6) | 595 (32.5) | 520 (33.9) | 507 (34.1) |
| Greater than HS | 2940 (34.6) | 655 (30.1) | 512 (34.6) | 625 (34.1) | 559 (36.4) | 589 (39.7) |
| Child’s sex | ||||||
| Female | 4272 (50.2) | 1114 (51.3) | 750 (50.6) | 898 (49.0) | 761 (49.5) | 749 (50.4) |
| Male | 4235 (49.8) | 1059 (48.7) | 731 (49.4) | 934 (51.0) | 775 (50.5) | 736 (49.6) |
| Ever smoked during pregnancy # | ||||||
| No | 6869 (80.8) | 1509 (69.4) | 1215 (82.0) | 1505 (82.2) | 1325 (86.3) | 1315 (88.6) |
| Yes | 1638 (19.3) | 664 (30.6) | 266 (18.0) | 327 (17.9) | 211 (13.7) | 170 (11.5) |
| Parity || | ||||||
| 0 | 3661 (43.0) | 986 (45.4) | 621 (41.9) | 806 (44.0) | 624 (40.6) | 624 (42.0) |
| >0 | 4846 (57.0) | 1187 (54.6) | 860 (58.1) | 1026 (56.0) | 912 (59.4) | 861 (58.0) |
| Pre-pregnancy BMI (kg/m2) # | ||||||
| <18.5 | 370 (4.4) | 111 (5.1) | 74 (5.0) | 68 (3.7) | 69 (4.5) | 48 (3.2) |
| 18.5–24.9 | 3902 (45.9) | 963 (44.3) | 661 (44.6) | 870 (47.5) | 699 (45.5) | 709 (47.7) |
| 25–29.9 | 2629 (30.9) | 625 (28.8) | 462 (31.2) | 555 (30.3) | 503 (32.8) | 484 (32.6) |
| ≥30 | 1606 (18.9) | 474 (21.8) | 284 (19.2) | 339 (18.5) | 265 (17.3) | 244 (16.4) |
| Diabetes || | ||||||
| None | 7624 (89.6) | 1903 (87.6) | 1338 (90.3) | 1650 (90.1) | 1398 (91.0) | 1335 (89.9) |
| GDM | 576 (6.8) | 169 (7.8) | 93 (6.3) | 112 (6.1) | 99 (6.5) | 103 (6.9) |
| DM | 307 (3.6) | 101 (4.7) | 50 (3.4) | 70 (3.8) | 39 (2.5) | 47 (3.2) |
| Chronic hypertension prior to pregnancy || | ||||||
| No | 8065 (94.8) | 2055 (94.6) | 1386 (93.6) | 1757 (95.9) | 1453 (94.6) | 1414 (95.2) |
| Yes | 442 (5.2) | 118 (5.4) | 95 (6.4) | 75 (4.1) | 83 (5.4) | 71 (4.8) |
| Preeclampsia || | ||||||
| None | 7675 (90.2) | 1939 (89.2) | 1334 (90.1) | 1676 (91.5) | 1384 (90.1) | 1342 (90.4) |
| Mild | 317 (3.7) | 74 (3.4) | 59 (4.0) | 71 (3.9) | 68 (4.4) | 45 (3.0) |
| Severe | 515 (6.1) | 160 (7.4) | 88 (5.9) | 85 (4.6) | 84 (5.5) | 98 (6.6) |
| Eclampsia | ||||||
| No | 8489 (99.8) | 2168 (99.8) | 1478 (99.8) | 1828 (99.8) | 1535 (99.9) | 1480 (99.7) |
| Yes | 18 (0.2) | 5 (0.2) | 3 (0.2) | 4 (0.2) | 1 (0.1) | 5 (0.3) |
| HELLP syndrome | ||||||
| No | 8442 (99.2) | 2155 (99.2) | 1477 (99.7) | 1819 (99.3) | 1521 (99.0) | 1470 (99.0) |
| Yes | 65 (0.8) | 18 (0.8) | 4 (0.3) | 13 (0.7) | 15 (1.0) | 15 (1.0) |
| Outcome | Effect Size (95% CI) | ||||
|---|---|---|---|---|---|
| N (%) | Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | |
| Overall sample | 8507 | N/A | N/A | N/A | N/A |
| Gestational age | |||||
| Continuous (weeks) * | N/A | −0.34 (−0.55–−0.13) # | −0.13 (−0.35–0.10) | −0.01 (−0.22–0.20) | −0.07 (−0.29–0.15) |
| <37 weeks † | 2316 (27.2) | 1.18 (1.06–1.31) ¶ | 1.05 (0.94–1.18) | 0.96 (0.86–1.08) | 1.05 (0.93–1.18) |
| Spontaneous | 1528 (18.0) | 1.28 (1.11–1.49) ¶ | 1.12 (0.95–1.31) | 1.05 (0.90–1.23) | 1.14 (0.97–1.33) |
| Medically-induced | 788 (9.3) | 1.01 (0.85–1.21) | 0.95 (0.77–1.15) | 0.82 (0.67–1.00) | 0.90 (0.74–1.10) |
| Preterm subgroups † | |||||
| ≥37 weeks | 6191 (72.8) | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| 34–36 weeks | 1504 (17.7) | 1.21 (1.05–1.39) ¶ | 1.05 (0.90–1.23) | 0.93 (0.80–1.09) | 1.06 (0.91–1.24) |
| <34 weeks | 812 (9.5) | 1.20 (0.99–1.46) | 1.03 (0.83–1.28) | 0.98 (0.80–1.21) | 1.01 (0.81–1.25) |
| Birth weight | |||||
| Continuous (g) * | N/A | −43.54 (−74.51–−12.57) ¶ | −41.07 (−74.16–−7.98) || | −13.71 (−45.15–17.72) | −9.95 (−42.60–22.69) |
| Low birth weight † | 2221 (26.1) | 1.11 (1.01–1.22) || | 1.16 (1.05–1.28) ¶ | 1.07 (0.97–1.18) | 1.03 (0.93–1.14) |
| Fetal growth † | |||||
| 10–89th %iles | 6649 (78.2) | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| <10th %ile | 777 (9.1) | 1.16 (0.96–1.39) | 1.20 (0.99–1.46) | 1.06 (0.88–1.29) | 1.11 (0.91–1.35) |
| ≥90th %ile | 1080 (12.7) | 0.86 (0.70–1.05) | 0.97 (0.70–1.05) | 0.87 (0.71–1.07) | 0.89 (0.72–1.10) |
| African American sample † | 4030 | N/A | N/A | N/A | N/A |
| Gestational age | |||||
| Continuous (weeks) * | N/A | −0.31 (−0.63–0.01) | −0.18 (−0.53–0.16) | 0.07 (−0.26–0.41) | 0.06 (−0.28–0.40) |
| <37 weeks † | 1160 (28.8) | 1.20 (1.03–1.39) || | 1.13 (0.96–1.33) | 0.98 (0.83–1.15) | 1.04 (0.89–1.23) |
| Spontaneous | 742 (18.4) | 1.39 (1.12–1.71) ¶ | 1.26 (1.00–1.58) | 1.18 (0.94–1.49) | 1.16 (0.92–1.47) |
| Medically-induced | 418 (10.4) | 0.94 (0.74–1.18) | 0.95 (0.73–1.22) | 0.69 (0.52–0.91) ¶ | 0.86 (0.67–1.12) |
| Preterm subgroups † | |||||
| ≥37 weeks | 2870 (71.2) | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| 34–36 weeks | 692 (17.2) | 1.25 (1.01–1.54) || | 1.18 (0.94–1.48) | 0.98 (0.77–1.23) | 1.10 (0.88–1.39) |
| <34 weeks | 468 (11.6) | 1.18 (0.92–1.51) | 1.06 (0.81–1.39) | 0.93 (0.71–1.22) | 0.92 (0.69–1.21) |
| Birth weight | |||||
| Continuous (g) * | N/A | −59.66 (−103.83–−15.50) ¶ | −49.57 (−96.68–−2.46) || | −0.04 (−45.43–45.34) | −20.15 (−66.70–26.40) |
| Low birth weight † | 1147 (28.5) | 1.14 (1.01–1.29) || | 1.17 (1.03–1.33) || | 1.01 (0.88–1.16) | 1.11 (0.97–1.27) |
| Fetal growth † | |||||
| 10–89th %iles | 3161 (78.4) | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| <10th %ile | 360 (8.9) | 1.22 (0.93–1.58) | 1.18 (0.89–1.56) | 0.96 (0.72–1.28) | 1.19 (0.89–1.57) |
| ≥90th %ile | 509 (12.6) | 0.84 (0.63–1.13) | 0.89 (0.65–1.23) | 0.91 (0.68–1.23) | 0.93 (0.69–1.26) |
| Non-African American sample | 4477 (52.6) | N/A | N/A | N/A | N/A |
| Gestational age | |||||
| Continuous (weeks) * | N/A | −0.35 (−0.62–−0.09) ¶ | −0.04 (−0.33–0.25) | −0.07 (−0.34–0.20) | −0.18 (−0.46–0.11) |
| <37 weeks † | 1156 (25.8) | 1.17 (1.01–1.36) || | 0.97 (0.82–1.15) | 0.95 (0.80–1.11) | 1.05 (0.89–1.24) |
| Spontaneous | 786 (17.6) | 1.20 (0.98–1.47) | 0.99 (0.79–1.24) | 0.95 (0.76–1.18) | 1.11 (0.89–1.38) |
| Medically-induced | 370 (8.3) | 1.12 (0.85–1.47) | 0.92 (0.67–1.25) | 0.95 (0.71–1.27) | 0.92 (0.68–1.24) |
| Preterm subgroups † | |||||
| ≥37 weeks | 3321 (74.2) | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| 34–36 weeks | 812 (18.1) | 1.18 (0.98–1.43) | 0.95 (0.77–1.18) | 0.90 (0.74–1.11) | 1.03 (0.84–1.27) |
| <34 weeks | 344 (7.7) | 1.22 (0.89–1.68) | 0.98 (0.68–1.40) | 1.04 (0.75–1.45) | 1.15 (0.81–1.62) |
| Birth weight | |||||
| Continuous (g) * | N/A | −17.06 (−60.25–26.13) | −23.65 (−70.08–22.79) | −17.13 (−60.73–26.48) | 6.11 (−39.70–51.93) |
| Low birth weight † | 1074 (24.0) | 1.05 (0.91–1.21) | 1.12 (0.96–1.31) | 1.10 (0.95–1.27) | 0.93 (0.79–1.09) |
| Fetal growth † | |||||
| 10–89th %iles | 3489 (77.9) | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] | 1.00 [Reference] |
| <10th %ile | 417 (9.3) | 1.07 (0.84–1.38) | 1.19 (0.92–1.55) | 1.13 (0.88–1.46) | 1.03 (0.78–1.36) |
| ≥90th %ile | 571 (12.8) | 0.91 (0.69–1.19) | 1.06 (0.80–1.41) | 0.85 (0.64–1.13) | 0.87 (0.64–1.17) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rhee, D.K.; Ji, Y.; Hong, X.; Pearson, C.; Wang, X.; Caulfield, L.E. Mediterranean-Style Diet and Birth Outcomes in an Urban, Multiethnic, and Low-Income US Population. Nutrients 2021, 13, 1188. https://doi.org/10.3390/nu13041188
Rhee DK, Ji Y, Hong X, Pearson C, Wang X, Caulfield LE. Mediterranean-Style Diet and Birth Outcomes in an Urban, Multiethnic, and Low-Income US Population. Nutrients. 2021; 13(4):1188. https://doi.org/10.3390/nu13041188
Chicago/Turabian StyleRhee, Dong Keun, Yuelong Ji, Xiumei Hong, Colleen Pearson, Xiaobin Wang, and Laura E Caulfield. 2021. "Mediterranean-Style Diet and Birth Outcomes in an Urban, Multiethnic, and Low-Income US Population" Nutrients 13, no. 4: 1188. https://doi.org/10.3390/nu13041188
APA StyleRhee, D. K., Ji, Y., Hong, X., Pearson, C., Wang, X., & Caulfield, L. E. (2021). Mediterranean-Style Diet and Birth Outcomes in an Urban, Multiethnic, and Low-Income US Population. Nutrients, 13(4), 1188. https://doi.org/10.3390/nu13041188







