Vitamin D and Temporomandibular Disorders: What Do We Know So Far?
Abstract
:1. Introduction
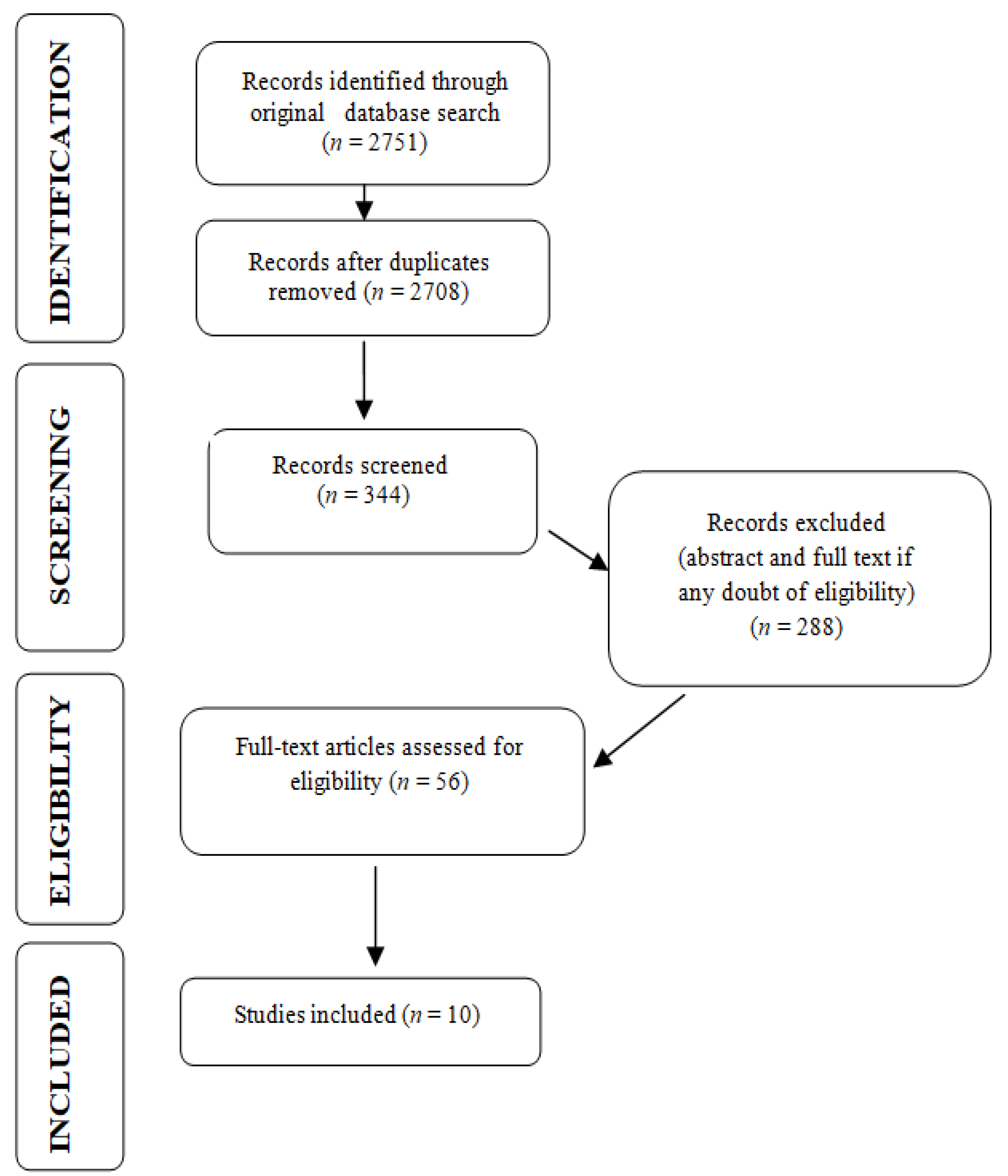
2. Method for Literature Search
3. Current Status of Knowledge
3.1. Definitions
3.1.1. Temporomandibular Disorders
3.1.2. Physiology and Actions of Vitamin D
3.1.3. Vitamin D and Genetic Variances
3.2. Vitamin D and Temporomandibular Disorders
4. Vitamin D and Pain Management
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Straube, S.; Derry, S.; Straube, C.; Moore, R.A. Vitamin D for the treatment of chronic painful conditions in adults. Cochrane Database Syst. Rev. 2015, 5, CD007771. [Google Scholar] [CrossRef]
- Holick, M.F. Vitamin D deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef]
- Gauer, R.L.; Semidey, M.J. Diagnosis and treatment of temporomandibular disorders. Am. Fam. Physician 2015, 91, 378–386. [Google Scholar]
- De Rossi, S.S.; Greenberg, M.S.; Liu, F.; Steinkeler, A. Temporomandibular disorders: Evaluation and management. Med. Clin. N. Am. 2014, 98, 1353–1384. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. International RDC/TMD Consortium Network, International association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6–27. [Google Scholar]
- Ryan, J.; Akhter, R.; Hassan, N.; Hilton, G.; Wickham, J.; Ibaragi, S. Epidemiology of Temporomandibular Disorder in the General Population: A Systematic Review. Adv. Dent. Oral Health 2019, 10, 555787. [Google Scholar]
- Paduano, S.; Bucci, R.; Rongo, R.; Silva, R.; Michelotti, A. Prevalence of temporomandibular disorders and oral parafunctions in adolescents from public schools in Southern Italy. Cranio 2020, 38, 370–375. [Google Scholar] [CrossRef]
- Lövgren, A.; Häggman-Henrikson, B.; Visscher, C.M.; Lobbezoo, F.; Marklund, S.; Wänman, A. Temporomandibular pain and jaw dysfunction at different ages covering the lifespan—A population based study. Eur. J. Pain 2016, 20, 532–540. [Google Scholar] [CrossRef] [Green Version]
- Al-Khotani, A.; Naimi-Akbar, A.; Albadawi, E.; Ernberg, M.; Hedenberg-Magnusson, B.; Christidis, N. Prevalence of diagnosed temporomandibular disorders among Saudi Arabian children and adolescents. J. Headache Pain 2016, 17, 41. [Google Scholar] [CrossRef] [Green Version]
- Graue, A.M.; Jokstad, A.; Assmus, J.; Skeie, M.S. Prevalence among adolescents in Bergen, Western Norway, of temporomandibular disorders according to the DC/TMD criteria and examination protocol. Acta Odontol. Scand. 2016, 74, 449–455. [Google Scholar] [CrossRef]
- Zemb, P.; Bergman, P.; Camargo, C.A., Jr.; Cavalier, E.; Cormier, C.; Courbebaisse, M.; Hollis, B.; Joulia, F.; Minisola, S.; Pilz, S.; et al. Vitamin D deficiency and the COVID-19 pandemic. J. Glob. Antimicrob. Resist. 2020, 22, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Ali, N. Role of vitamin D in preventing of COVID-19 infection, progression and severity. J. Infect. Public Health 2020, 13, 1373–1380. [Google Scholar] [CrossRef]
- Bilezikian, J.P.; Bikle, D.; Hewison, M.; Lazaretti-Castro, M.; Formenti, A.M.; Gupta, A.; Madhavan, M.V.; Nair, N.; Babalyan, V.; Hutchings, N.; et al. Mechanisms in Endocrinology: Vitamin D and COVID-19. Eur. J. Endocrinol. 2020, 183, R133–R147. [Google Scholar] [CrossRef] [PubMed]
- Grant, W.B.; Lahore, H.; McDonnell, S.L.; Baggerly, C.A.; French, C.B.; Aliano, J.L.; Bhattoa, H.P. Evidence that Vitamin D Supplementation Could Reduce Risk of Influenza and COVID-19 Infections and Deaths. Nutrients 2020, 12, 988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machon, V.; Hirjak, D.; Lukas, J. Therapy of the osteoarthritis of the temporomandibular joint. J. Cranio-maxillofac. Surg. 2011, 39, 127–130. [Google Scholar] [CrossRef]
- Poveda Roda, R.; Bagan, J.V.; Díaz Fernández, J.M.; Hernández Bazán, S.; Jiménez Soriano, Y. Review of temporomandibular joint pathology. Part I: Classification, epidemiology and risk factors. Med. Oral Patol. Oral Cir. Bucal 2007, 12, E292–E298. [Google Scholar]
- Poveda Roda, R.; Díaz Fernández, J.M.; Hernández Bazán, S.; Jiménez Soriano, Y.; Margaix, M.; Sarrión, G. A review of temporomandibular joint disease (TMJD). Part II: Clinical and radiological semiology. Morbidity processes. Med. Oral Patol. Oral Cir. Bucal 2008, 13, E102–E109. [Google Scholar]
- Okeson, J.P.; de Leeuw, R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dent. Clin. N. Am. 2011, 55, 105–120. [Google Scholar] [CrossRef]
- Tanaka, E.; Detamore, M.S.; Mercuri, L.G. Degenerative disorders of the temporomandibular joint: Etiology, diagnosis, and treatment. J. Dent. Res. 2008, 87, 296–307. [Google Scholar] [CrossRef]
- Hoffmann, R.G.; Kotchen, J.M.; Kotchen, T.A.; Cowley, T.; Dasgupta, M.; Cowley, A.W., Jr. Temporomandibular disorders and associated clinical comorbidities. Clin. J. Pain 2011, 27, 268–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batacchi, Z.; Robinson-Cohen, C.; Hoofnagle, A.N.; Isakova, T.; Kestenbaum, B.; Martin, K.J.; Wolf, M.S.; de Boer, I.H. Effects of Vitamin D2 Supplementation on Vitamin D3 Metabolism in Health and CKD. Clin. J. Am. Soc. Nephrol. 2017, 12, 1498–1506. [Google Scholar] [CrossRef] [Green Version]
- Chau, Y.Y.; Kumar, J. Vitamin D in chronic kidney disease. Indian J. Pediatr. 2012, 79, 1062–1068. [Google Scholar] [CrossRef] [Green Version]
- Helde-Frankling, M.; Björkhem-Bergman, L. Vitamin D in Pain Management. Int. J. Mol. Sci. 2017, 18, 2170. [Google Scholar] [CrossRef] [Green Version]
- Ross, A.C.; Manson, J.E.; Abrams, S.A.; Aloia, J.F.; Brannon, P.M.; Clinton, S.K.; Durazo-Arvizu, R.A.; Gallagher, J.C.; Gallo, R.L.; Jones, G.; et al. The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: What clinicians need to know. J. Clin. Endocrinol. Metab. 2011, 96, 53–58. [Google Scholar] [CrossRef]
- Holick, M.F. The vitamin D deficiency pandemic: Approaches for diagnosis, treatment and prevention. Rev. Endocrmetabdisord. 2017, 18, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.J. Vitamin D analogs for secondary hyperparathyroidism: What does the future hold? J. Steroid Biochem. Mol. Biol. 2007, 103, 578–583. [Google Scholar] [CrossRef]
- Cranney, A.; Horsley, T.; O’Donnell, S.; Weiler, H.; Puil, L.; Ooi, D.; Atkinson, S.; Ward, L.; Moher, D.; Hanley, D.; et al. Effectiveness and safety of vitamin D in relation to bone health. Evid Rep. Technol. Assess. (Full Rep.) 2007, 158, 1–235. [Google Scholar]
- Bouillon, R.; Carmeliet, G.; Verlinden, L.; van Etten, E.; Verstuyf, A.; Luderer, H.F.; Lieben, L.; Mathieu, C.; Demay, M. Vitamin D and human health: Lessons from vitamin D receptor null mice. Endocr. Rev. 2008, 29, 726–776. [Google Scholar] [CrossRef] [PubMed]
- Norman, A.W. From vitamin D to hormone D: Fundamentals of the vitamin D endocrine system essential for good health. Am. J. Clin. Nutr. 2008, 88, 491S–499S. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andress, D.L. Vitamin D in chronic kidney disease: A systemic role for selective vitamin D receptor activation. Kidney Int. 2006, 69, 33–43. [Google Scholar] [CrossRef] [Green Version]
- Bonato, L.L.; Quinelato, V.; Borojevic, R.; Vieira, A.R.; Modesto, A.; Granjeiro, J.M.; Tesch, R.; Casado, P.L. Haplotypes of the RANK and OPG genes are associated with chronic arthralgia in individuals with and without temporomandibular disorders. Int. J. Oral Maxillofac. Surg. 2017, 46, 1121–1129. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, A.D.; Yazicioglu, D.; TüzünerÖncül, A.M.; Yilmaz, E.; Ereş, G. Vitamin D receptor gene polymorphisms (Apa1 and Taq1) in temporomandibular joint internal derangement/osteoarthritis in a group of Turkish patients. Mol. Biol. Rep. 2018, 45, 1839–1848. [Google Scholar] [CrossRef]
- Zilahi, E.; Chen, J.Q.; Papp, G.; Szántó, A.; Zeher, M. Lack of association of vitamin D receptor gene polymorphisms/haplotypes in Sjögren’s syndrome. Clin. Rheumatol. 2015, 34, 247–253. [Google Scholar] [CrossRef] [Green Version]
- Monticielo, O.A.; de Mattos Teixeira, T.; Chies, J.A.B.; Brenol, J.C.T.; Xavier, R.M. Vitamin D and polymorphisms of VDR gene in patients with systemic lupus erythematosus. Clin. Rheumatol. 2012, 31, 1411–1421. [Google Scholar] [CrossRef] [PubMed]
- Bid, H.K.; Mishra, D.K.; Mittal, R.D. Vitamin-D receptor (VDR) gene (Fok-I, Taq-I and Apa-I) polymorphisms in healthy individuals from north Indian population. Asian Pac. J. Cancer Prev. 2005, 6, 147–152. [Google Scholar]
- Uitterlinden, A.G.; Fang, Y.; Van Meurs, J.B.; Pols, H.A.; Van Leeuwen, J.P. Genetics and biology of vitamin D receptor polymorphisms. Gene 2004, 338, 143–156. [Google Scholar] [CrossRef] [Green Version]
- Yildiz, S.; Tumer, M.K.; Yigit, S.; Nursal, A.F.; Rustemoglu, A.; Balel, Y. Relationship of Vitamin D and Bsml variant with Temporomandibular Diseases in Turkish population. Br. J. Oral Maxillofacsurg. 2020. [Google Scholar] [CrossRef]
- Zittermann, A. The Biphasic Effect of Vitamin D on the Musculoskeletal and Cardiovascular System. Int. J. Endocrinol. 2017, 2017, 3206240. [Google Scholar] [CrossRef] [Green Version]
- Koundourakis, N.E.; Avgoustinaki, P.D.; Malliaraki, N.; Margioris, A.N. Muscular effects of vitamin D in young athletes and non-athletes and in the elderly. Hormones 2016, 15, 471–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garfinkel, R.J.; Dilisio, M.F.; Agrawal, D.K. Vitamin D and Its Effects on Articular Cartilage and Osteoarthritis. Orthop. J. Sports Med. 2017, 5, 2325967117711376. [Google Scholar] [CrossRef] [PubMed]
- Madani, A.; Shamsian, S.A.; Layegh, P.; Abrisham, S.M.; Ravaghi, A.; TayaraniNajjaran, N. Are certain factors involved in calcium metabolism associated with temporomandibular disorders? Cranio 2019, 31, 1–7. [Google Scholar] [CrossRef]
- Yılmaz, F.; GünenYılmaz, S.; Sözel, H.; Bora, F.; Yılmaz, A.B. The prevalence of temporomandibular disorders in chronic hemodialysis patients: A cross-sectional study. Cranio 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Zand, L.; Kumar, R. The Use of Vitamin D Metabolites and Analogues in the Treatment of Chronic Kidney Disease. Endocrinol. Metab. Clin. N. Am. 2017, 46, 983–1007. [Google Scholar] [CrossRef]
- Khanna, S.; Parulekar, N.R.; Dhaimade, P.A. The Influence of Vitamin D on the Temporomandibular Joint and the Activities of Daily Living. J. Clin. Diagn. Res. 2017, 11, ZC31–ZC34. [Google Scholar] [CrossRef]
- Shen, M.; Luo, Y.; Niu, Y.; Chen, L.; Yuan, X.; Goltzman, D.; Chen, N.; Miao, D. 1,25(OH)2D deficiency induces temporomandibular joint osteoarthritis via secretion of senescence-associated inflammatory cytokines. Bone 2013, 55, 400–409. [Google Scholar] [CrossRef] [PubMed]
- Jagur, O.; Kull, M.; Leibur, E.; Kallikorm, R.; Loorits, D.; Lember, M.; Voog-Oras, U. Relationship between radiographic changes in the temporomandibular joint and bone mineral density: A population based study. Stomatologija 2011, 13, 42–48. [Google Scholar]
- Demir, C.Y.; Ersoz, M.E. Biochemical changes associated with temporomandibular disorders. J. Int. Med. Res. 2019, 47, 765–771. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Staniszewski, K.; Lygre, H.; Berge, T.; Rosén, A. Serum Analysis in Patients with Temporomandibular Disorders: A Controlled Cross-Sectional Study in Norway. Pain Res. Manag. 2019, 2019, 1360725. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.S. Biochemical Changes Related with Temporomandibular Joint Disorders and Inflammatory Arthritis. Biomed. Pharmacol. J. 2017, 10, 2085–2090. [Google Scholar] [CrossRef]
- Beddis, H.; Pemberton, M.; Davies, S. Sleep bruxism: An overview for clinicians. Br. Dent. J. 2018, 225, 497–501. [Google Scholar] [CrossRef]
- Alkhatatbeh, M.J.; Hmoud, Z.L.; Razzak, K.K.A.; Alem, E.M. Self-reported sleep bruxism is associated with vitamin D deficiency and low dietary calcium intake: A case-control study. BMC Oral Health 2021, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- International Association for the Study of Pain. IASP Taxonomy. 1994. Available online: http://www.iasp-pain.org/Taxonomy#Pain (accessed on 27 January 2021).
- Arnold, M. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders. Cephalalgia 2018, 38, 1–211. [Google Scholar]
- Nowaczewska, M.; Wiciński, M.; Osiński, S.; Kaźmierczak, H. The Role of Vitamin D in Primary Headache–from Potential Mechanism to Treatment. Nutrients 2020, 12, 243. [Google Scholar] [CrossRef] [Green Version]
- Sohn, J.H.; Chu, M.K.; Park, K.Y.; Ahn, H.Y.; Cho, S.J. Vitamin D deficiency in patients with cluster headache: A preliminary study. J. Headache Pain 2018, 19, 54. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; Malihi, Z.; Stewart, A.W.; Lawes, C.M.; Scragg, R. The association between vitamin D concentration and pain: A systematic review and meta-analysis. Public Health Nutr. 2018, 21, 2022–2037. [Google Scholar] [CrossRef]
- Manoy, P.; Yuktanandana, P.; Tanavalee, A.; Anomasiri, W.; Ngarmukos, S.; Tanpowpong, T.; Honsawek, S. Vitamin D Supplementation Improves Quality of Life and Physical Performance in Osteoarthritis Patients. Nutrients 2017, 9, 799. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, C.Y. Vitamin D in the Prevention and Treatment of Osteoarthritis: From Clinical Interventions to Cellular Evidence. Nutrients 2019, 11, 243. [Google Scholar] [CrossRef] [Green Version]
- Jin, X.; Antony, B.; Wang, X.; Persson, M.S.; McAlindon, T.; Arden, N.K.; Srivastava, S.; Srivastava, R.; Van Middelkoop, M.; Bierma-Zeinstra, S.M.; et al. Effect of vitamin D supplementation on pain and physical function in patients with knee osteoarthritis (OA): An OA Trial Bank protocol for a systematic review and individual patient data (IPD) meta-analysis. BMJ Open 2020, 10, e035302. [Google Scholar] [CrossRef] [Green Version]

| INTRA-ARTICULAR DISORDERS | 1. Joint Pain | Arthralgia/Arthritis/Osteoarthritis | ||
| 2. Joint disorders | Disk disorders/disk displacement | with reduction with intermittent locking without reduction, with limited locking without reduction, without limited locking | ||
| Other hypomobility disorders | Adhesions Adherence Ankylosis (fibrous/osseous) | |||
| Hypermobility disorders | Dislocations (subluxation/luxation) | |||
| 3. Joint diseases | Systemic arthritis/condylysis/osteonecrosis | |||
| Degenerative joint disease/osteochondritis dissecans/ synovial chondromatosis/neoplasm | ||||
| 4. Congenital disorders | Aplasia/hypoplasia/hyperplasia | |||
| EXTRA-ARTICULAR DISORDERS | 1. Muscle pain | Myalgia/ tendonitis/ myositis/spasm | Local myalgia/myofascial pain/ myofascial pain with referral | |
| 2. Contracture | ||||
| 3. Hypertrophy | ||||
| 4. Neoplasm | ||||
| 5. Movement disorders | Orofacial dyskinesia/oromandibular dystonia | |||
| 6. Masticatory muscle pain due to systemic pain disorder | Fibromyalgia Widespread pain | |||
| Serum Vitamin D Levels | <5 ng/mL | 5–15 ng/mL | 16–30 ng/mL |
|---|---|---|---|
| Definition | Severe vitamin D deficiency | Mild vitamin D deficiency | Vitamin D insufficiency |
| Dose of cholecalciferol | 8000 IU/day orally or enterally for 4 weeks, followed by 4000 IU/day | 4000 IU/day orally or enterally for 12 weeks | 2000 IU/day |
| First Author and Year | Type of Study | Sample Size | Results |
|---|---|---|---|
| Yilmaz, A. D., 2018 [32] | Clinical Trial | 119 subjects | No association between the VDR TaqI and ApaI gene polymorphisms and intra-articular TMDs. |
| Yildiz, S., 2020 [37] | Case–control Study | 206 subjects | Bsml variant of VDR gene, as well as low levels of vitamin D, plays a role in the etiology and pathogenesis of intra-articular TMDs (disk displacement with reduction). |
| Madani, A., 2019 [41] | Case–control study | 80 subjects | No significant association between vitamin D serum concentration levels and TMDs. |
| Yilmaz, F., 2020 [42] | Case–control study | 146 subjects | High prevalence of TMDs among chronic hemodialysis patients. |
| Khanna, S., 2017 [44] | Case–control study | 100 subjects | Vitamin D serum level had a significant impact on the TMJ pain and discomfort. |
| Jagur, O., 2011 [46] | Case–control study | 95 subjects | TMJ radiographic changes and teeth loss seem to be related to the low level of bone mineral density and vitamin D serum levels. |
| Demir, C. Y., 2019 [47] | Clinical trial | 100 subjects | Vitamin D status was similar between patients with TMDs and control group; increased parathyroid hormone levels in response to vitamin D deficiency were significantly higher in patients with TMDs. |
| Staniszewski, K., [48] | Controlled Cross-Sectional Study | 120 subjects | Serum analyses should not be used as a biomarker of TMDs. |
| Ahmed, H. S. [49] | Clinical trial | 45 subjects | Vitamin D levels were significantly lower in TMD patients with RA. |
| Alkhatatbeh, M. J., [51] | Case–control study | 100 subjects | Vitamin D levels were significantly lower in subjects with sleep bruxism. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kui, A.; Buduru, S.; Labunet, A.; Balhuc, S.; Negucioiu, M. Vitamin D and Temporomandibular Disorders: What Do We Know So Far? Nutrients 2021, 13, 1286. https://doi.org/10.3390/nu13041286
Kui A, Buduru S, Labunet A, Balhuc S, Negucioiu M. Vitamin D and Temporomandibular Disorders: What Do We Know So Far? Nutrients. 2021; 13(4):1286. https://doi.org/10.3390/nu13041286
Chicago/Turabian StyleKui, Andreea, Smaranda Buduru, Anca Labunet, Silvia Balhuc, and Marius Negucioiu. 2021. "Vitamin D and Temporomandibular Disorders: What Do We Know So Far?" Nutrients 13, no. 4: 1286. https://doi.org/10.3390/nu13041286
APA StyleKui, A., Buduru, S., Labunet, A., Balhuc, S., & Negucioiu, M. (2021). Vitamin D and Temporomandibular Disorders: What Do We Know So Far? Nutrients, 13(4), 1286. https://doi.org/10.3390/nu13041286








