Impact of Sarcopenia on Acute Kidney Injury after Infrarenal Abdominal Aortic Aneurysm Surgery: A Propensity Matching Analysis
Abstract
:1. Introduction
2. Methods
2.1. Patients
2.2. Clinical Data
2.3. Definitions
2.3.1. Preoperative Imaging Variables
2.3.2. Postoperative AKI
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Ethical Approval and Consent to Participate
References
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the european working group on sarcopenia in older people. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoon, Y.H.; Ko, Y.; Kim, K.W.; Kang, D.Y.; Ahn, J.M.; Ko, E.; Park, H.; Cho, S.C.; Kim, H.J.; Kim, J.B.; et al. Prognostic value of baseline sarcopenia on 1-year mortality in patients undergoing transcatheter aortic valve implantation. Am. J. Cardiol. 2020. [Google Scholar] [CrossRef]
- Martini, K.; Chassagnon, G.; Fournel, L.; Prieto, M.; Hoang-Thi, T.N.; Halm, N.; Bobbio, A.; Revel, M.P.; Alifano, M. Sarcopenia as independent risk factor of postpneumonectomy respiratory failure, ards and mortality. Lung Cancer 2020, 149, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Berardi, G.; Antonelli, G.; Colasanti, M.; Meniconi, R.; Guglielmo, N.; Laurenzi, A.; Ferretti, S.; Levi Sandri, G.B.; Spagnoli, A.; Moschetta, G.; et al. Association of sarcopenia and body composition with short-term outcomes after liver resection for malignant tumors. JAMA Surg. 2020, e203336. [Google Scholar] [CrossRef]
- Nakano, Y.; Hirata, Y.; Shimogawara, T.; Yamada, T.; Mihara, K.; Nishiyama, R.; Nishiya, S.; Taniguchi, H.; Egawa, T. Frailty is a useful predictive marker of postoperative complications after pancreaticoduodenectomy. World J. Surg. Oncol. 2020, 18, 194. [Google Scholar] [CrossRef] [PubMed]
- Sakalihasan, N.; Limet, R.; Defawe, O.D. Abdominal aortic aneurysm. Lancet 2005, 365, 1577–1589. [Google Scholar] [CrossRef]
- Lindstrom, I.; Khan, N.; Vanttinen, T.; Peltokangas, M.; Sillanpaa, N.; Oksala, N. Psoas muscle area and quality are independent predictors of survival in patients treated for abdominal aortic aneurysms. Ann. Vasc. Surg. 2019, 56, 183–193.e183. [Google Scholar] [CrossRef]
- Lee, J.S.; He, K.; Harbaugh, C.M.; Schaubel, D.E.; Sonnenday, C.J.; Wang, S.C.; Englesbe, M.J.; Eliason, J.L.; Michigan Analytic Morphomics, G. Frailty, core muscle size, and mortality in patients undergoing open abdominal aortic aneurysm repair. J. Vasc. Surg. 2011, 53, 912–917. [Google Scholar] [CrossRef] [Green Version]
- Tallgren, M.; Niemi, T.; Poyhia, R.; Raininko, E.; Railo, M.; Salmenpera, M.; Lepantalo, M.; Hynninen, M. Acute renal injury and dysfunction following elective abdominal aortic surgery. Eur. J. Vasc. Endovasc. Surg. 2007, 33, 550–555. [Google Scholar] [CrossRef] [Green Version]
- Demirjian, S.; Schold, J.D.; Navia, J.; Mastracci, T.M.; Paganini, E.P.; Yared, J.P.; Bashour, C.A. Predictive models for acute kidney injury following cardiac surgery. Am. J. Kidney Dis. 2012, 59, 382–389. [Google Scholar] [CrossRef]
- Meroni, R.; Simonini, M.; Lanzani, C.; Bignami, E. Predictive models for acute kidney injury after cardiac surgery. Eur. J. Anaesthesiol. 2018, 35, 63–65. [Google Scholar] [CrossRef]
- Nonaka, T.; Kimura, N.; Hori, D.; Sasabuchi, Y.; Nakano, M.; Yuri, K.; Sanui, M.; Matsumoto, H.; Yamaguchi, A. Predictors of acute kidney injury following elective open and endovascular aortic repair for abdominal aortic aneurysm. Ann. Vasc. Dis. 2018, 11, 298–305. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saratzis, A.; Melas, N.; Mahmood, A.; Sarafidis, P. Incidence of acute kidney injury (aki) after endovascular abdominal aortic aneurysm repair (evar) and impact on outcome. Eur. J. Vasc. Endovasc. Surg. 2015, 49, 534–540. [Google Scholar] [CrossRef] [Green Version]
- Tang, Y.; Chen, J.; Huang, K.; Luo, D.; Liang, P.; Feng, M.; Chai, W.; Fung, E.; Lan, H.Y.; Xu, A. The incidence, risk factors and in-hospital mortality of acute kidney injury in patients after abdominal aortic aneurysm repair surgery. BMC Nephrol. 2017, 18, 184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kopolovic, I.; Simmonds, K.; Duggan, S.; Ewanchuk, M.; Stollery, D.E.; Bagshaw, S.M. Risk factors and outcomes associated with acute kidney injury following ruptured abdominal aortic aneurysm. BMC Nephrol. 2013, 14, 99. [Google Scholar] [CrossRef] [Green Version]
- Bang, J.Y.; Lee, J.B.; Yoon, Y.; Seo, H.S.; Song, J.G.; Hwang, G.S. Acute kidney injury after infrarenal abdominal aortic aneurysm surgery: A comparison of akin and rifle criteria for risk prediction. Br. J. Anaesth. 2014, 113, 993–1000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molinari, L.; Sakhuja, A.; Kellum, J.A. Perioperative renoprotection: General mechanisms and treatment approaches. Anesth. Analg. 2020, 131, 1679–1692. [Google Scholar] [CrossRef]
- Walrand, S.; Guillet, C.; Salles, J.; Cano, N.; Boirie, Y. Physiopathological mechanism of sarcopenia. Clin. Geriatr. Med. 2011, 27, 365–385. [Google Scholar] [CrossRef]
- Park, H.J.; Shin, Y.; Park, J.; Kim, H.; Lee, I.S.; Seo, D.W.; Huh, J.; Lee, T.Y.; Park, T.; Lee, J.; et al. Development and validation of a deep learning system for segmentation of abdominal muscle and fat on computed tomography. Korean J. Radiol. 2020, 21, 88–100. [Google Scholar] [CrossRef]
- Park, J.; Gil, J.R.; Shin, Y.; Won, S.E.; Huh, J.; You, M.W.; Park, H.J.; Sung, Y.S.; Kim, K.W. Reliable and robust method for abdominal muscle mass quantification using ct/mri: An explorative study in healthy subjects. PLoS ONE 2019, 14, e0222042. [Google Scholar] [CrossRef]
- Lee, K.; Shin, Y.; Huh, J.; Sung, Y.S.; Lee, I.S.; Yoon, K.H.; Kim, K.W. Recent issues on body composition imaging for sarcopenia evaluation. Korean J. Radiol. 2019, 20, 205–217. [Google Scholar] [CrossRef]
- Santilli, V.; Bernetti, A.; Mangone, M.; Paoloni, M. Clinical definition of sarcopenia. Clin. Cases Miner. Bone Metab. 2014, 11, 177–180. [Google Scholar] [CrossRef] [PubMed]
- Cheng, B.T.; Soult, M.C.; Helenowski, I.B.; Rodriguez, H.E.; Eskandari, M.K.; Hoel, A.W. Sarcopenia predicts mortality and adverse outcomes after endovascular aneurysm repair and can be used to risk stratify patients. J. Vasc. Surg. 2019, 70, 1576–1584. [Google Scholar] [CrossRef]
- Hale, A.L.; Twomey, K.; Ewing, J.A.; Langan, E.M., 3rd; Cull, D.L.; Gray, B.H. Impact of sarcopenia on long-term mortality following endovascular aneurysm repair. Vasc. Med. 2016, 21, 217–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Indrakusuma, R.; Zijlmans, J.L.; Jalalzadeh, H.; Planken, R.N.; Balm, R.; Koelemay, M.J.W. Psoas muscle area as a prognostic factor for survival in patients with an asymptomatic infrarenal abdominal aortic aneurysm: A retrospective cohort study. Eur. J. Vasc. Endovasc. Surg. 2018, 55, 83–91. [Google Scholar] [CrossRef] [Green Version]
- Antoniou, G.A.; Rojoa, D.; Antoniou, S.A.; Alfahad, A.; Torella, F.; Juszczak, M.T. Effect of low skeletal muscle mass on post-operative survival of patients with abdominal aortic aneurysm: A prognostic factor review and meta-analysis of time-to-event data. Eur. J. Vasc. Endovasc. Surg. 2019, 58, 190–198. [Google Scholar] [CrossRef]
- Waduud, M.A.; Wood, B.; Keleabetswe, P.; Manning, J.; Linton, E.; Drozd, M.; Hammond, C.J.; Bailey, M.A.; Scott, D.J.A. Influence of psoas muscle area on mortality following elective abdominal aortic aneurysm repair. Br. J. Surg. 2019, 106, 367–374. [Google Scholar] [CrossRef]
- Drudi, L.M.; Phung, K.; Ades, M.; Zuckerman, J.; Mullie, L.; Steinmetz, O.K.; Obrand, D.I.; Afilalo, J. Psoas muscle area predicts all-cause mortality after endovascular and open aortic aneurysm repair. Eur. J. Vasc. Endovasc. Surg. 2016, 52, 764–769. [Google Scholar] [CrossRef] [PubMed]
- Newton, D.H.; Kim, C.; Lee, N.; Wolfe, L.; Pfeifer, J.; Amendola, M. Sarcopenia predicts poor long-term survival in patients undergoing endovascular aortic aneurysm repair. J. Vasc. Surg. 2018, 67, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Thurston, B.; Pena, G.N.; Howell, S.; Cowled, P.; Fitridge, R. Low total psoas area as scored in the clinic setting independently predicts midterm mortality after endovascular aneurysm repair in male patients. J. Vasc. Surg. 2018, 67, 460–467. [Google Scholar] [CrossRef]
- Prado, C.M.; Lieffers, J.R.; McCargar, L.J.; Reiman, T.; Sawyer, M.B.; Martin, L.; Baracos, V.E. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: A population-based study. Lancet Oncol. 2008, 9, 629–635. [Google Scholar] [CrossRef]
- Yang, R.; Zhang, Y.; Shen, X.; Yan, S. Sarcopenia associated with renal function in the patients with type 2 diabetes. Diabetes Res. Clin. Pract. 2016, 118, 121–129. [Google Scholar] [CrossRef]
- Foley, R.N.; Wang, C.; Ishani, A.; Collins, A.J.; Murray, A.M. Kidney function and sarcopenia in the united states general population: Nhanes iii. Am. J. Nephrol. 2007, 27, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Jo, E.; Lee, S.R.; Park, B.S.; Kim, J.S. Potential mechanisms underlying the role of chronic inflammation in age-related muscle wasting. Aging Clin. Exp. Res. 2012, 24, 412–422. [Google Scholar] [CrossRef]
- Van Ancum, J.M.; Scheerman, K.; Jonkman, N.H.; Smeenk, H.E.; Kruizinga, R.C.; Meskers, C.G.M.; Maier, A.B. Change in muscle strength and muscle mass in older hospitalized patients: A systematic review and meta-analysis. Exp. Gerontol. 2017, 92, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Souza, V.A.; Oliveira, D.; Barbosa, S.R.; Correa, J.; Colugnati, F.A.B.; Mansur, H.N.; Fernandes, N.; Bastos, M.G. Sarcopenia in patients with chronic kidney disease not yet on dialysis: Analysis of the prevalence and associated factors. PLoS ONE 2017, 12, e0176230. [Google Scholar] [CrossRef] [Green Version]
- Avin, K.G.; Chen, N.X.; Organ, J.M.; Zarse, C.; O’Neill, K.; Conway, R.G.; Konrad, R.J.; Bacallao, R.L.; Allen, M.R.; Moe, S.M. Skeletal muscle regeneration and oxidative stress are altered in chronic kidney disease. PLoS ONE 2016, 11, e0159411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Enoki, Y.; Watanabe, H.; Arake, R.; Sugimoto, R.; Imafuku, T.; Tominaga, Y.; Ishima, Y.; Kotani, S.; Nakajima, M.; Tanaka, M.; et al. Indoxyl sulfate potentiates skeletal muscle atrophy by inducing the oxidative stress-mediated expression of myostatin and atrogin-1. Sci. Rep. 2016, 6, 32084. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Nathan, J.A.; Goldberg, A.L. Muscle wasting in disease: Molecular mechanisms and promising therapies. Nat. Rev. Drug Discov. 2015, 14, 58–74. [Google Scholar] [CrossRef]
- Wang, X.H.; Mitch, W.E. Mechanisms of muscle wasting in chronic kidney disease. Nat. Rev. Nephrol. 2014, 10, 504–516. [Google Scholar] [CrossRef] [Green Version]
- Gumucio, J.P.; Mendias, C.L. Atrogin-1, murf-1, and sarcopenia. Endocrine 2013, 43, 12–21. [Google Scholar] [CrossRef] [PubMed]
| Before Propensity Score Matching | After Propensity Score Matching | ||||||
|---|---|---|---|---|---|---|---|
| Total (n = 379) | No Sarcopenia (n = 275) | Sarcopenia (n = 104) | p Value | No sarcopenia (n = 104) | Sarcopenia (n = 104) | p Value | |
| Patients’ demographics | |||||||
| Age (yr) | 69.0 (64.0–74.0) | 67.0 (63.0–73.0) | 74.0 (69.0–78.0) | <0.001 | 74 (68–76) | 74 (69–78) | 0.293 |
| Sex, male | 339 (89.4) | 250 (90.9) | 89 (85.6) | 0.187 | 91 (87.5) | 89 (85.6) | 0.839 |
| Body mass index (kg/m2) | 23.8 ± 3.4 | 24.7 ± 3.1 | 21.5 ± 3.1 | <0.001 | - | - | - |
| Diabetes | 62 (16.4) | 46 (16.7) | 16 (15.4) | 0.873 | 15 (14.4) | 16 (15.4) | 1.000 |
| Hypertension | 272 (71.8) | 188 (68.4) | 84 (80.8) | 0.023 | 83 (79.8) | 84 (80.8) | 1.000 |
| Coronary arterial disease | 118 (31.1) | 87 (31.6) | 31 (29.8) | 0.827 | 34 (32.7) | 31 (29.8) | 0.765 |
| CVD | 40 (10.6) | 27 (9.8) | 13 (12.5) | 0.568 | - | ||
| COPD | 107 (28.2) | 71 (25.8) | 36 (34.6) | 0.116 | - | - | - |
| CKD | 31 (8.2) | 20 (7.3) | 11 (10.6) | 0.402 | 8 (7.7) | 11 (10.6) | 0.630 |
| Beta blocker | 119 (31.4) | 83 (30.2) | 36 (34.6) | 0.480 | - | - | - |
| Statin | 134 (35.4) | 102 (37.1) | 32 (30.8) | 0.304 | - | - | - |
| Haemoglobin (g/dL) | 13.3 (12.1–14.2) | 13.5 (12.4–14.4) | 12.4 (10.9–13.8) | <0.001 | 12.6 (11.4–13.8) | 12.4 (10.9–13.8) | 0.481 |
| Albumin (g/dL) | 3.8 (3.4–4.0) | 3.8 (3.5–4.0) | 3.6 (3.2–3.9) | 0.002 | 3.7 (3.4–4.0) | 3.6 (3.2–3.9) | 0.326 |
| Creatinine (mg/dL) | 0.8 ± 0.2 | 0.8 ± 0.2 | 0.8 ± 0.2 | 0.119 | - | - | - |
| eGFR (ml/min/1.73 m2) | 69.0 (60.0–85.9) | 71.0 (60.0–86.0) | 66.0 (60.0–80.8) | 0.126 | 70.0 (60–82.2) | 66.0 (60.0–80.8) | 0.605 |
| Intraoperative variables | |||||||
| Treatment | 0.535 | 1.0 | |||||
| Open surgery | 212 (55.9) | 157 (57.1) | 55 (52.9) | 54 (51.9) | 55 (52.9)- | ||
| EVAR | 167 (44.1) | 118 (42.9) | 49 (47.1) | 50 (48.1) | 49 (47.1) | ||
| Maximal diameter | 5.7 (5.0–6.5) | 5.7 (5.0–6.5) | 5.8 (5.0–6.5) | 0.212 | 6.0 (5.0–6.8) | 5.8 (5.0–6.5) | 0.975 |
| Anaesthesia type | 0.574 | 0.379 | |||||
| General | 314 (82.8) | 230 (83.6) | 84 (80.8) | 84 (80.8) | 84 (80.8) | ||
| Regional | 36 (9.5) | 27 (9.8) | 9 (8.7) | 14 (13.5) | 9 (8.7) | ||
| Local | 29 (7.7) | 18 (6.5) | 11 (10.6) | 6 (5.8) | 11 (10.6) | ||
| Crystalloid (mL) | 3100 (1700–4300) | 3050 (1700–4300) | 3100 (1900–4200) | 0.982 | - | - | - |
| Colloid (mL) | 600 (100–1000) | 600 (125–1000) | 625 (100–1000) | 0.853 | 600 (150–1000) | 625 (100–1000) | 0.767 |
| Red blood cell transfusion (Units) | 2 (0–4) | 2 (0–4) | 2 (0–4) | 0.090 | 2 (0–4) | 2 (0–4) | 0.828 |
| Fresh frozen plasma transfusion (Units) | 0 (0–0) | 0 (0–0) | 0 (0–0) | 0.391 | - | - | - |
| Total urine output (mL) | 680 (400–1070) | 700 (430–1082) | 635 (340–1030) | 0.179 | - | - | - |
| Anaesthesia time (min) | 273 (209.5–340) | 273 (208–336.5) | 276.5 (219.5–357) | 0.503 | 261.5 (207–352) | 276.5 (219.5–357) | 0.706 |
| Aortic clamp time (min) | 55 (0–94.5) | 55 (0–93.5) | 48 (0–95) | 0.631 | 41.5 (0–95) | 48.0 (0–95) | 0.989 |
| Lowest mean arterial pressure (mmHg) | 65.3 (61–72) | 65.7 (61.3–71.8) | 65.0 (59.7–73) | 0.513 | 67 (62–72) | 65 (60–73) | 0.327 |
| Univariate | Multivariable | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Sarcopenia | 2.94 | 1.74–4.95 | <0.001 | 2.19 | 1.20–3.98 | 0.010 |
| Age | 1.06 | 1.02–1.10 | 0.003 | 1.03 | 0.99–1.07 | 0.134 |
| Sex, male | 0.80 | 031–1.79 | 0.611 | |||
| Diabetes | 1.03 | 0.51–1.96 | 0.934 | |||
| Preoperative CKD | 4.92 | 2.30–10.58 | <0.001 | 3.39 | 1.40–8.07 | 0.006 |
| Maximal diameter | 1.19 | 1.00–1.41 | 0.051 | |||
| EVAR | 0.70 | 0.42–1.16 | 0.171 | |||
| Preoperative haemoglobin | 0.72 | 0.62–0.83 | <0.001 | |||
| Preoperative albumin | 0.36 | 0.21–0.59 | <0.001 | 0.58 | 0.33–1.02 | 0.057 |
| Infused colloid | 1.00 | 1.00–1.00 | 0.165 | |||
| Diuretics | 1.18 | 0.92–1.50 | 0.178 | |||
| Intraoperative RBC transfusion | 1.21 | 1.11–1.34 | <0.001 | 1.17 | 1.06–1.30 | 0.002 |
| Aortic clamping time | 1.00 | 1.00–1.00 | 0.725 | |||
| Lowest intraoperative MBP | 1.00 | 1.00–1.01 | 0.919 | |||
| Anaesthetic time | 1.00 | 1.00–1.01 | 0.221 | |||
| Univariate | Multivariable | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Sarcopenia | 2.72 | 1.55–4.77 | 0.005 | 1.92 | 1.01–3.67 | 0.048 |
| Age | 1.11 | 1.06–1.16 | <0.001 | 1.09 | 1.04–1.14 | 0.008 |
| Sex, male | 1.67 | 0.78–3.56 | 0.187 | |||
| DM | 1.81 | 0.92–3.56 | 0.865 | 2.25 | 1.12–4.51 | 0.022 |
| Hypertension | 1.379 | 0.72–2.65 | 0.334 | |||
| Preoperative CKD | 3.52 | 1.75–7.09 | 0.004 | 2.72 | 1.13–6.57 | 0.026 |
| Maximal diameter | 1.08 | 0.89–1.30 | 0.437 | |||
| EVAR | 1.66 | 0.92–3.02 | 0.947 | 1.60 | 0.86–2.97 | 0.136 |
| Preoperative haemoglobin | 0.81 | 0.69–0.94 | 0.007 | 1.18 | 0.96–1.45 | 0.119 |
| Preoperative albumin | 0.32 | 0.20–0.51 | <0.001 | 0.31 | 0.18–0.54 | <0.001 |
| Diuretics | 0.93 | 0.70–1.23 | 0.608 | |||
| Intraoperative RBC transfusion | 1.08 | 0.99–1.17 | 0.084 | |||
| Aortic clamping time | 1.00 | 0.99–1.00 | 0.500 | |||
| Lowest intraoperative MBP | 1.01 | 0.98–1.04 | 0.603 | |||
| Anaesthetic time | 1.00 | 1.00–1.00 | 0.670 | |||
| Multivariate | PS Matching | ||||||
| Event/N (%) | OR (95% CI) | p Value | Event/N (%) | OR (95% CI) | p Value | ||
| AKI | No sarcopenia | 42/275 (15.3) | 1 | 16/104 (15.4) | 1 | ||
| Sarcopenia | 36/104 (34.6) | 2.19 (1.20–3.98) | 0.010 | 36/104 (34.6) | 2.36 (1.19 –4.83) | 0.016 | |
| Event/N (%) | HR (95% CI) | p Value | Event/N (%) | HR (95% CI) | p Value | ||
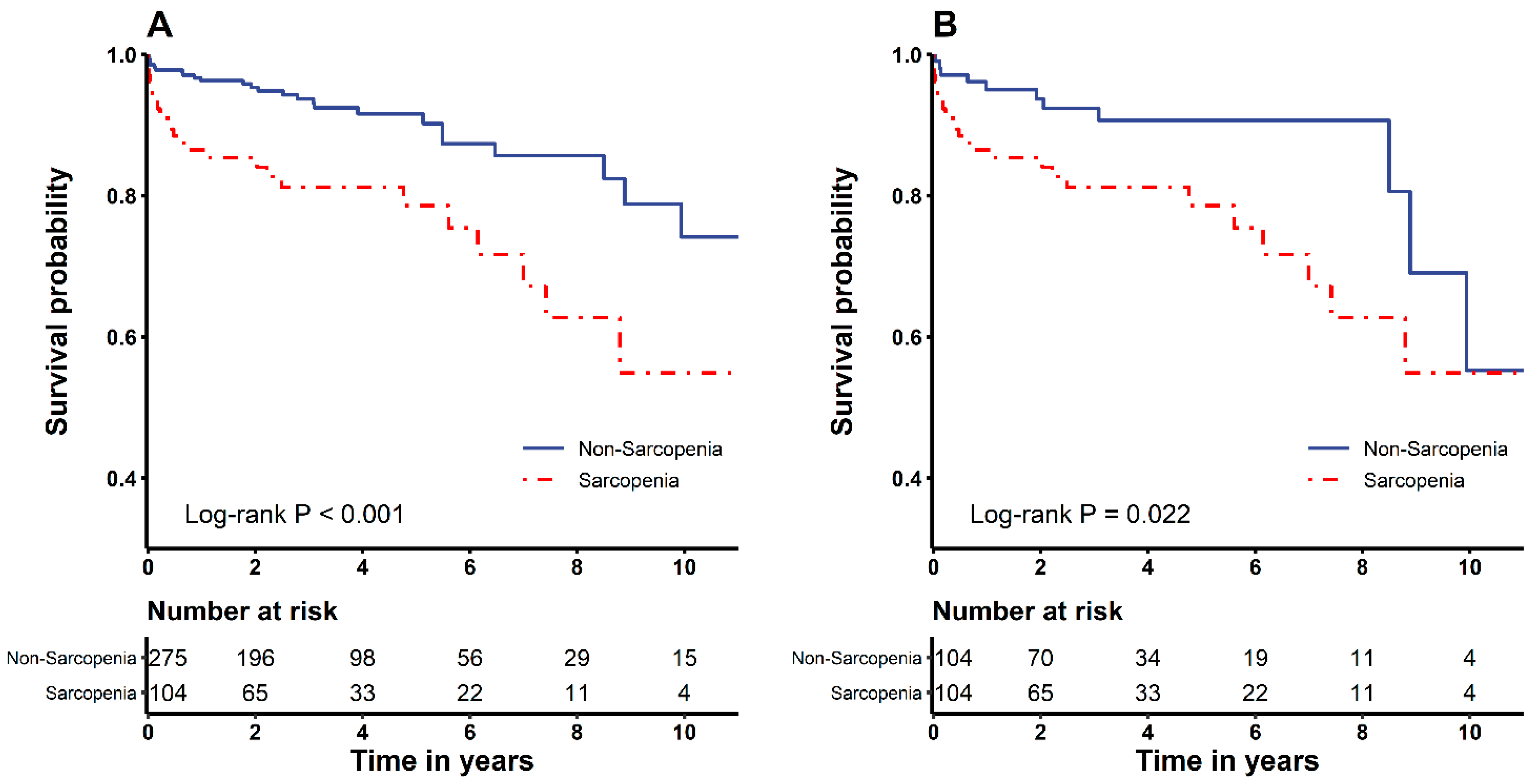
| Overall mortality | No sarcopenia | 25/275 (9.1) | 1 | 11/104 (10.6) | 1 | ||
| Sarcopenia | 24/104 (23.1) | 1.92 (1.01–3.67) | 0.048 | 24/104 (23.1) | 2.28 (1.08–4.84) | 0.032 | |
| Before PS Matching | After PS Matching | ||||||
| Median (IQR) | p Value | Median (IQR) | p Value | ||||
| Hospital stay | No sarcopenia | 8 (6–10) | 0.001 | 8 (5.5–9) | 0.003 | ||
| Sarcopenia | 9 (6.5–15) | 9 (6.5–15) | |||||
| ICU stay | No sarcopenia | 2 (2–3) | 0.017 | 2 (2–3) | 0.026 | ||
| Sarcopenia | 2 (2–3.5) | 2 (2–3.5) | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bang, J.-Y.; Jun, I.-G.; Lee, J.-B.; Ko, Y.-S.; Kim, K.-W.; Jeong, J.-H.; Kim, S.-H.; Song, J.-G. Impact of Sarcopenia on Acute Kidney Injury after Infrarenal Abdominal Aortic Aneurysm Surgery: A Propensity Matching Analysis. Nutrients 2021, 13, 2212. https://doi.org/10.3390/nu13072212
Bang J-Y, Jun I-G, Lee J-B, Ko Y-S, Kim K-W, Jeong J-H, Kim S-H, Song J-G. Impact of Sarcopenia on Acute Kidney Injury after Infrarenal Abdominal Aortic Aneurysm Surgery: A Propensity Matching Analysis. Nutrients. 2021; 13(7):2212. https://doi.org/10.3390/nu13072212
Chicago/Turabian StyleBang, Ji-Yeon, In-Gu Jun, Jeong-Bok Lee, You-Sun Ko, Kyung-Won Kim, Jun-Hyeop Jeong, Sung-Hoon Kim, and Jun-Gol Song. 2021. "Impact of Sarcopenia on Acute Kidney Injury after Infrarenal Abdominal Aortic Aneurysm Surgery: A Propensity Matching Analysis" Nutrients 13, no. 7: 2212. https://doi.org/10.3390/nu13072212
APA StyleBang, J.-Y., Jun, I.-G., Lee, J.-B., Ko, Y.-S., Kim, K.-W., Jeong, J.-H., Kim, S.-H., & Song, J.-G. (2021). Impact of Sarcopenia on Acute Kidney Injury after Infrarenal Abdominal Aortic Aneurysm Surgery: A Propensity Matching Analysis. Nutrients, 13(7), 2212. https://doi.org/10.3390/nu13072212






