Testing and Prescribing Vitamin B12 in Swiss General Practice: A Survey among Physicians
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design, Setting, and Participants
2.2. Instruments and Procedures
2.3. Statistics
3. Results
3.1. Sampling and Sample Characteristics
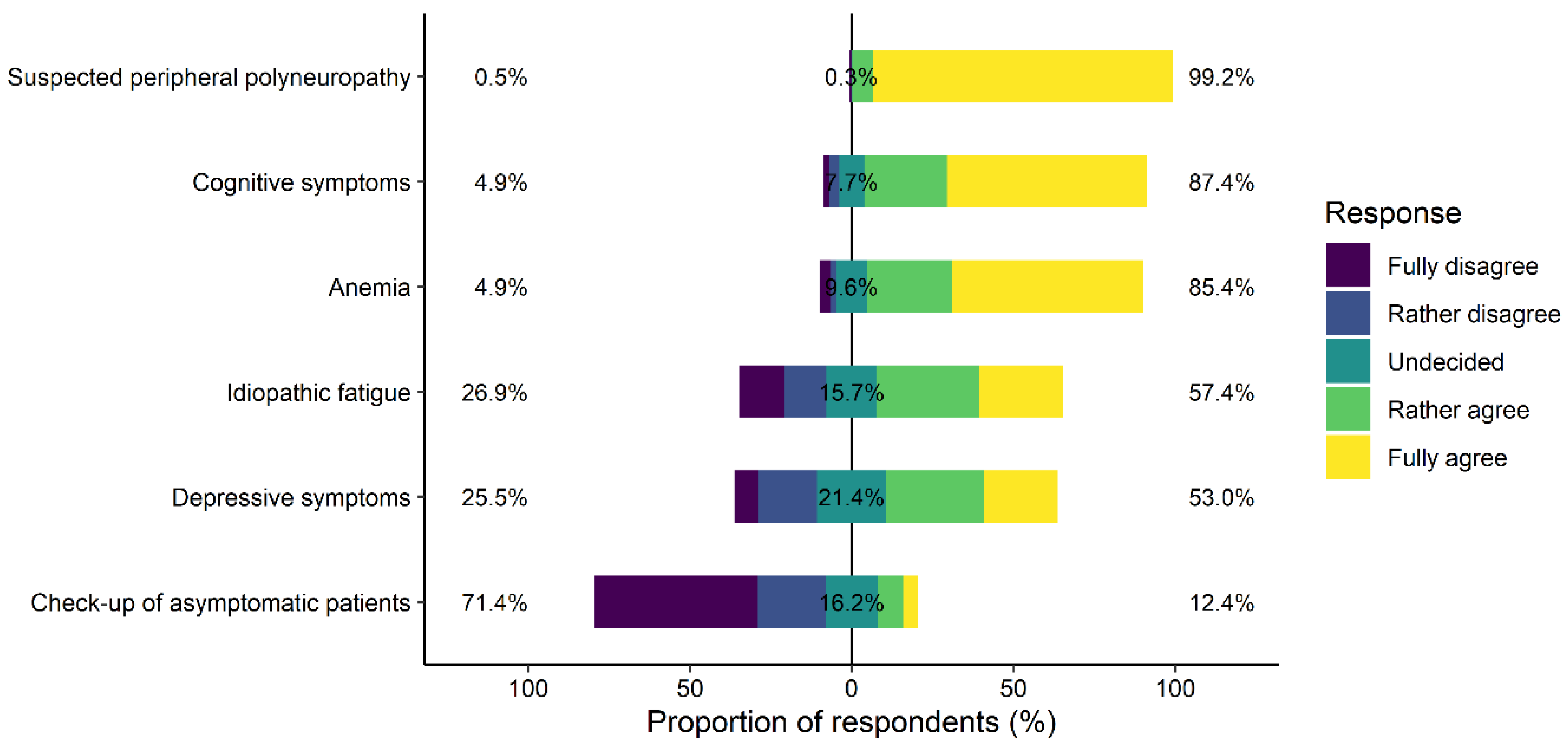
3.2. GPs’ Mindsets Regarding the Role of Vitamin B12 Testing and Treatment in Specific Clinical Situations
3.3. Testing Strategy, Route of Application, Patient Involvement, and Confidence in Effectiveness
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Green, R.; Allen, L.H.; Bjørke-Monsen, A.L.; Brito, A.; Guéant, J.L.; Miller, J.W.; Molloy, A.M.; Nexo, E.; Stabler, S.; Toh, B.H.; et al. Vitamin B(12) deficiency. Nat. Rev. Dis. Primers 2017, 3, 17040. [Google Scholar] [CrossRef] [PubMed]
- Briani, C.; Dalla Torre, C.; Citton, V.; Manara, R.; Pompanin, S.; Binotto, G.; Adami, F. Cobalamin deficiency: Clinical picture and radiological findings. Nutrients 2013, 5, 4521–4539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carmel, R. Subclinical cobalamin deficiency. Curr. Opin. Gastroenterol. 2012, 28, 151–158. [Google Scholar] [CrossRef]
- Nielsen, M.J.; Rasmussen, M.R.; Andersen, C.B.; Nexø, E.; Moestrup, S.K. Vitamin B12 transport from food to the body’s cells--a sophisticated, multistep pathway. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Aparicio-Ugarriza, R.; Palacios, G.; Alder, M.; González-Gross, M. A review of the cut-off points for the diagnosis of vitamin B12 deficiency in the general population. Clin. Chem. Lab. Med. 2015, 53, 1149–1159. [Google Scholar] [CrossRef]
- Carmel, R. Biomarkers of cobalamin (vitamin B-12) status in the epidemiologic setting: A critical overview of context, applications, and performance characteristics of cobalamin, methylmalonic acid, and holotranscobalamin II. Am. J. Clin. Nutr. 2011, 94, 348S–358S. [Google Scholar] [CrossRef] [Green Version]
- Lewerin, C.; Ljungman, S.; Nilsson-Ehle, H. Glomerular filtration rate as measured by serum cystatin C is an important determinant of plasma homocysteine and serum methylmalonic acid in the elderly. J. Intern. Med. 2007, 261, 65–73. [Google Scholar] [CrossRef]
- Carmel, R. Chemiluminescence-based cobalamin assay errors: Background and perspectives. Clin. Chem. Lab. Med. 2013, 51, e253–e256. [Google Scholar] [CrossRef]
- Cullen, W.; Kearney, Y.; Bury, G. Prevalence of fatigue in general practice. Ir. J. Med Sci. 2002, 171, 10–12. [Google Scholar] [CrossRef]
- King, M.; Nazareth, I.; Levy, G.; Walker, C.; Morris, R.; Weich, S.; Bellon-Saameno, J.A.; Moreno, B.; Svab, I.; Rotar, D.; et al. Prevalence of common mental disorders in general practice attendees across Europe. Br. J. Psychiatry J. Ment. Sci. 2008, 192, 362–367. [Google Scholar] [CrossRef]
- Luck, T.; Riedel-Heller, S.G.; Kaduszkiewicz, H.; Bickel, H.; Jessen, F.; Pentzek, M.; Wiese, B.; Koelsch, H.; van den Bussche, H.; Abholz, H.H.; et al. Mild cognitive impairment in general practice: Age-specific prevalence and correlate results from the German study on ageing, cognition and dementia in primary care patients (AgeCoDe). Dement. Geriatr. Cogn. Disord. 2007, 24, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, L.D.; Jager, L.; Meier, R.; Rachamin, Y.; Senn, O.; Rosemann, T.; Markun, S. Trends and Between-Physician Variation in Laboratory Testing: A Retrospective Longitudinal Study in General Practice. J. Clin. Med. 2020, 9, 1787. [Google Scholar] [CrossRef]
- Huber, C.A.; Nagler, M.; Rosemann, T.; Blozik, E.; Napflin, M.; Markun, S. Trends in Micronutrient Laboratory Testing in Switzerland: A 7-Year Retrospective Analysis of Healthcare Claims Data. Int. J. Gen. Med. 2020, 13, 1341–1348. [Google Scholar] [CrossRef]
- Chmiel, C.; Bhend, H.; Senn, O.; Zoller, M.; Rosemann, T.; FIRE Study-Group. The FIRE project: A milestone for research in primary care in Switzerland. Swiss Med. Wkly. 2011, 140, w13142. [Google Scholar] [CrossRef] [Green Version]
- Swiss Confederation. 810.30 Federal Act of 30 September 2011 on Research involving Human Beings (Human Research Act, HRA). Available online: https://www.fedlex.admin.ch/eli/cc/2013/617/en (accessed on 16 November 2020).
- Hayton, J.C.; Allen, D.G.; Scarpello, V. Factor Retention Decisions in Exploratory Factor Analysis: A Tutorial on Parallel Analysis. Organ. Res. Methods 2004, 7, 191–205. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistics notes: Cronbach’s alpha. BMJ (Clin. Res. Ed.) 1997, 314, 572. [Google Scholar] [CrossRef] [Green Version]
- Tavakol, M.; Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2011, 2, 53–55. [Google Scholar] [CrossRef] [PubMed]
- Bryer, J.; Speerschneider, K. Likert: Analysis and Visualization Likert Items, 1.3.5 ed.; 2016. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Wickham, H. Ggplot2: Elegant Graphics for Data Analysis, 1st ed.; Springer: New York, NY, USA, 2009. [Google Scholar]
- Falissard, B. Psy: Various Procedures Used in Psychometry, 1.1 ed.; 2012. [Google Scholar]
- Allaire, J.J.; Gandrud, C.; Russell, K.; Yetman, C. Networkd3: D3 JavaScript Network Graphs for R; R Package Version 0.4; 2017. [Google Scholar]
- Lubec, D.; Müllbacher, W.; Finsterer, J.; Mamoli, B. Diagnostic work-up in peripheral neuropathy: An analysis of 171 cases. Postgrad. Med. J. 1999, 75, 723–727. [Google Scholar] [CrossRef]
- Weytingh, M.; Bossuyt, P.; Van Crevel, H. Reversible dementia: More than 10% or less than 1%? J. Neurol. 1995, 242, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Wirth, J.P.; Woodruff, B.A.; Engle-Stone, R.; Namaste, S.M.; Temple, V.J.; Petry, N.; Macdonald, B.; Suchdev, P.S.; Rohner, F.; Aaron, G.J. Predictors of anemia in women of reproductive age: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am. J. Clin. Nutr. 2017, 106, 416s–427s. [Google Scholar] [CrossRef] [PubMed]
- Devalia, V.; Hamilton, M.S.; Molloy, A.M.; British Committee for Standards in Haematology. Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Br. J. Haematol. 2014, 166, 496–513. [Google Scholar] [CrossRef]
- Huber, F. Müdigkeit. Available online: https://www.medix.ch/media/medix_guideline_muedigkeit_2016.pdf (accessed on 3 May 2021).
- Fosnocht, M.K.; Ende, J. Approach to the Adult Patient with Fatigue. Available online: https://www.uptodate.com/contents/approach-to-the-adult-patient-with-fatigue (accessed on 28 April 2021).
- National Collaborating Centre for Primary Care. National Institute for Health and Clinical Excellence: Guidance. In Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (or Encephalopathy): Diagnosis and Management of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (or Encephalopathy) in Adults and Children; Copyright © 2021, Royal College of General Practitioners; Royal College of General Practitioners (UK): London, UK, 2007. [Google Scholar]
- Carmel, R. Diagnosis and management of clinical and subclinical cobalamin deficiencies: Why controversies persist in the age of sensitive metabolic testing. Biochimie 2013, 95, 1047–1055. [Google Scholar] [CrossRef]
- Lindenbaum, J.; Healton, E.B.; Savage, D.G.; Brust, J.C.; Garrett, T.J.; Podell, E.R.; Marcell, P.D.; Stabler, S.P.; Allen, R.H. Neuropsychiatric disorders caused by cobalamin deficiency in the absence of anemia or macrocytosis. N. Engl. J. Med. 1988, 318, 1720–1728. [Google Scholar] [CrossRef]
- Kim, J.M.; Stewart, R.; Kim, S.W.; Yang, S.J.; Shin, I.S.; Yoon, J.S. Predictive value of folate, vitamin B12 and homocysteine levels in late-life depression. Br. J. Psychiatry J. Ment. Sci. 2008, 192, 268–274. [Google Scholar] [CrossRef] [Green Version]
- Beydoun, M.A.; Shroff, M.R.; Beydoun, H.A.; Zonderman, A.B. Serum folate, vitamin B-12, and homocysteine and their association with depressive symptoms among U.S. adults. Psychosom. Med. 2010, 72, 862–873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petridou, E.T.; Kousoulis, A.A.; Michelakos, T.; Papathoma, P.; Dessypris, N.; Papadopoulos, F.C.; Stefanadis, C. Folate and B12 serum levels in association with depression in the aged: A systematic review and meta-analysis. Aging Ment. Health 2016, 20, 965–973. [Google Scholar] [CrossRef] [PubMed]
- Markun, S.; Gravestock, I.; Jager, L.; Rosemann, T.; Pichierri, G.; Burgstaller, J.M. Effects of Vitamin B12 Supplementation on Cognitive Function, Depressive Symptoms, and Fatigue: A Systematic Review, Meta-Analysis, and Meta-Regression. Nutrients 2021, 13, 923. [Google Scholar] [CrossRef]
- Kaminski, M.; Skonieczna-Zydecka, K.; Nowak, J.K.; Stachowska, E. Global and local diet popularity rankings, their secular trends, and seasonal variation in Google Trends data. Nutrition 2020, 79, 110759. [Google Scholar] [CrossRef] [PubMed]
- Devi, A.; Rush, E.; Harper, M.; Venn, B. Vitamin B12 Status of Various Ethnic Groups Living in New Zealand: An Analysis of the Adult Nutrition Survey 2008/2009. Nutrients 2018, 10, 181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brouwer-Brolsma, E.M.; Dhonukshe-Rutten, R.A.; van Wijngaarden, J.P.; Zwaluw, N.L.; Velde, N.; de Groot, L.C. Dietary Sources of Vitamin B-12 and Their Association with Vitamin B-12 Status Markers in Healthy Older Adults in the B-PROOF Study. Nutrients 2015, 7, 7781–7797. [Google Scholar] [CrossRef]
- Linde, K.; Atmann, O.; Meissner, K.; Schneider, A.; Meister, R.; Kriston, L.; Werner, C. How often do general practitioners use placebos and non-specific interventions? Systematic review and meta-analysis of surveys. PLoS ONE 2018, 13, e0202211. [Google Scholar] [CrossRef]
- Sanz-Cuesta, T.; Escortell-Mayor, E.; Cura-Gonzalez, I.; Martin-Fernandez, J.; Riesgo-Fuertes, R.; Garrido-Elustondo, S.; Mariño-Suárez, J.E.; Álvarez-Villalba, M.; Gómez-Gascón, T.; González-García, I.; et al. Oral versus intramuscular administration of vitamin B12 for vitamin B12 deficiency in primary care: A pragmatic, randomised, non-inferiority clinical trial (OB12). BMJ Open 2020, 10, e033687. [Google Scholar] [CrossRef] [PubMed]
- Cham, G.; Davis, N.; Strivens, E.; Traves, A.; Manypeney, G.; Gunnarsson, R. Factors correlating to the propensity of general practitioners to substitute borderline vitamin B12 deficiency. Scand. J. Prim. Health Care 2018, 36, 242–248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hofstede, H.; van der Burg, H.A.M.; Mulder, B.C.; Bohnen, A.M.; Bindels, P.J.E.; de Wit, N.J.; de Schepper, E.I.T.; van Vugt, S.F. Reducing unnecessary vitamin testing in general practice: Barriers and facilitators according to general practitioners and patients. BMJ Open 2019, 9, e029760. [Google Scholar] [CrossRef] [Green Version]
- Silverstein, W.K.; Lin, Y.; Dharma, C.; Croxford, R.; Earle, C.C.; Cheung, M.C. Prevalence of Inappropriateness of Parenteral Vitamin B12 Administration in Ontario, Canada. JAMA Intern. Med. 2019, 179, 1434–1436. [Google Scholar] [CrossRef]

| Characteristic | Value |
|---|---|
| Number of respondents | 376 |
| Years of experience as a GP, median (IQR) | 23.0 (16.0–30.0) |
| Participants that identify as female, n (%) | 153 (40.7) |
| Practice type, n (%) | |
| Single | 56 (14.9) |
| Group | 306 (81.4) |
| Other types | 2 (0.5) |
| Missing | 12 (3.2) |
| Board certification in general internal medicine, n (%) | 345 (91.8) |
| Predominantly working as GP, n (%) | 341 (90.7) |
| Additional qualifications, n (%) | |
| Practices psychosomatic medicine | 17 (4.5) |
| Practices CAM | 16 (4.3) |
| Clinical Situation | Testing, % of Participants | Prescribing, % of Participants |
|---|---|---|
| Suspected peripheral polyneuropathy | 77.1 | 75.5 |
| Known risk for malnutrition/malabsorption | 60.1 | 65.7 |
| Anemia | 49.7 | 47.1 |
| Cognitive symptoms | 34.8 | 35.4 |
| Idiopathic fatigue | 30.9 | 27.9 |
| Depressive symptoms | 11.7 | 10.9 |
| Hair loss/oral aphthae | 10.6 | 7.2 |
| Asymptomatic patients | 9.0 | 11.7 |
| Other | 5.3 | 7.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bardheci, K.; Jäger, L.; Risch, L.; Rosemann, T.; Burgstaller, J.M.; Markun, S. Testing and Prescribing Vitamin B12 in Swiss General Practice: A Survey among Physicians. Nutrients 2021, 13, 2610. https://doi.org/10.3390/nu13082610
Bardheci K, Jäger L, Risch L, Rosemann T, Burgstaller JM, Markun S. Testing and Prescribing Vitamin B12 in Swiss General Practice: A Survey among Physicians. Nutrients. 2021; 13(8):2610. https://doi.org/10.3390/nu13082610
Chicago/Turabian StyleBardheci, Katarina, Levy Jäger, Lorenz Risch, Thomas Rosemann, Jakob M. Burgstaller, and Stefan Markun. 2021. "Testing and Prescribing Vitamin B12 in Swiss General Practice: A Survey among Physicians" Nutrients 13, no. 8: 2610. https://doi.org/10.3390/nu13082610
APA StyleBardheci, K., Jäger, L., Risch, L., Rosemann, T., Burgstaller, J. M., & Markun, S. (2021). Testing and Prescribing Vitamin B12 in Swiss General Practice: A Survey among Physicians. Nutrients, 13(8), 2610. https://doi.org/10.3390/nu13082610








