Nutritional Supplements and Neuroprotective Diets and Their Potential Clinical Significance in Post-Stroke Rehabilitation
Abstract
:1. Introduction
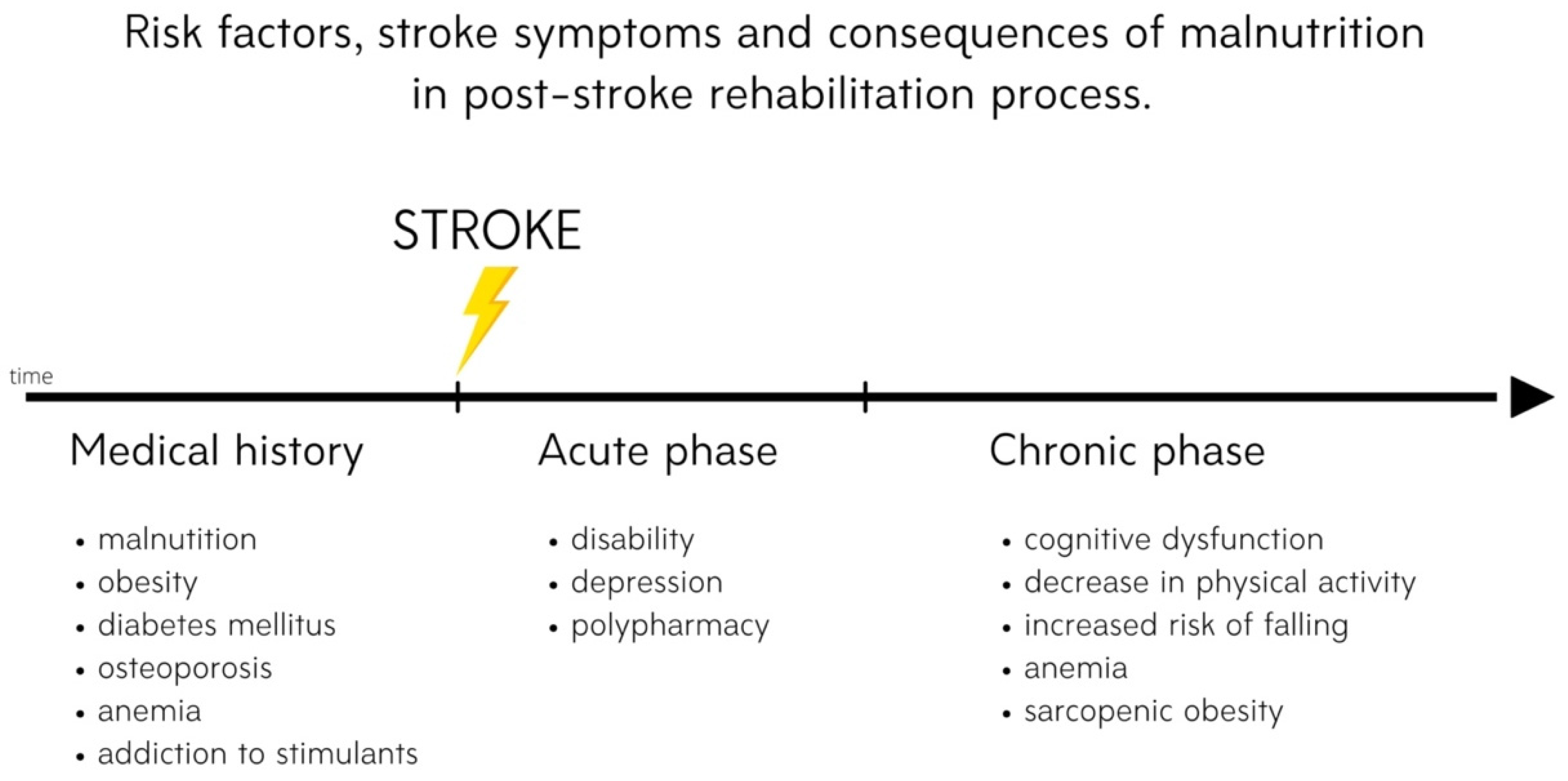
2. Risk of Malnutrition after Stroke
3. Nutrition-Related Chronic Diseases in Post-Stroke Patients
3.1. Osteoporosis
3.2. Anemia
3.3. Sarcopenia
3.4. Diabetes Mellitus
4. Preventive Strategies
Neuroprotective Diets
5. The Role of Nutritional Status in Post-Stroke Rehabilitation
6. Impact of Nutritional Supplementation on Post-Stroke Rehabilitation
6.1. Amino Acid Supplementation
6.2. Vitamin D Supplementation
7. Agents from Marine Sources—A New Approach to Post-Stroke Neuroplasticity
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hardie, K.; Hankey, G.J.; Jamrozik, K.; Broadhurst, R.J.; Anderson, C. Ten-year risk of first recurrent stroke and disability after first-ever stroke in the Perth Community Stroke Study. Stroke 2004, 35, 731–735. [Google Scholar] [CrossRef]
- Han, J.; Mao, W.; Ni, J.; Wu, Y.; Liu, J.; Bai, L.; Shi, M.; Tu, J.; Ning, X.; Wang, J. Rate and Determinants of Recurrence at 1 Year and 5 Years After Stroke in a Low-Income Population in Rural China. Front. Neurol. 2020, 11, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ballester, B.R.; Maier, M.; Duff, A.; Cameirão, M.; Bermúdez, S.; Duarte, E.; Cuxart, A.; Rodríguez, S.; San Segundo Mozo, R.M.; Verschure, P.F.M.J. A critical time window for recovery extends beyond one-year post-stroke. J. Neurophysiol. 2019, 122, 350–357. [Google Scholar] [CrossRef] [Green Version]
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. Guidelines for Adult Stroke Rehabilitation and Recovery: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef] [PubMed]
- Foley, N.C.; Salter, K.L.; Robertson, J.; Teasell, R.W.; Woodbury, M.G. Which reported estimate of the prevalence of malnutrition after stroke is valid? Stroke 2009, 40, e66–e74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, H.C.; Chen, H.F.; Peng, L.N.; Lin, M.H.; Chen, L.K.; Liang, C.K.; Lo, Y.K.; Hwang, S.J. Impact of nutritional status on long-term functional outcomes of post-acute stroke patients in Taiwan. Arch. Gerontol. Geriatr. 2011, 53, e149–e152. [Google Scholar] [CrossRef] [PubMed]
- Sabbouh, T.; Torbey, M.T. Malnutrition in Stroke Patients: Risk Factors, Assessment, and Management. Neurocrit. Care 2018, 29, 374–384. [Google Scholar] [CrossRef]
- Chauwa, L.; Appiah, C.A.; Nsiah, K.; Sarfo, F.S. Nutritional risk markers among stroke out-patients at the neurology clinic of a teaching hospital in Ghana. Pan Afr. Med. J. 2020, 37, 258. [Google Scholar] [CrossRef]
- Mullins, N. Nutrition and hydration management among stroke patients in inpatient rehabilitation: A best practice implementation project. JBI Evid. Implement. 2021, 19, 56–67. [Google Scholar] [CrossRef]
- Sato, Y.; Yoshimura, Y.; Abe, T. Nutrition in the First Week after Stroke Is Associated with Discharge to Home. Nutrients 2021, 13, 943. [Google Scholar] [CrossRef]
- Chen, N.; Li, Y.; Fang, J.; Lu, Q.; He, L. Risk factors for malnutrition in stroke patients: A meta-analysis. Clin. Nutr. 2019, 38, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Dennis, M.S.; Lewis, S.C.; Warlow, C.; Collaboration, F.T. Routine oral nutritional supplementation for stroke patients in hospital (FOOD): A multicentre randomised controlled trial. Lancet 2005, 365, 755–763. [Google Scholar] [CrossRef]
- Bramanti, E.; Arcuri, C.; Cecchetti, F.; Cervino, G.; Nucera, R.; Cicciù, M. Dental management in dysphagia syndrome patients with previously acquired brain damages. Dent. Res. J. 2012, 9, 361–367. [Google Scholar]
- Clavé, P.; Shaker, R. Dysphagia: Current reality and scope of the problem. Nat. Rev. Gastroenterol. Hepatol. 2015, 12, 259–270. [Google Scholar] [CrossRef]
- Roden, D.F.; Altman, K.W. Causes of dysphagia among different age groups: A systematic review of the literature. Otolaryngol. Clin. N. Am. 2013, 46, 965–987. [Google Scholar] [CrossRef]
- Warnecke, T.; Labeit, B.; Schroeder, J.; Reckels, A.; Ahring, S.; Lapa, S.; Claus, I.; Muhle, P.; Suntrup-Krueger, S.; Dziewas, R. Neurogenic Dysphagia: Systematic Review and Proposal of a Classification System. Neurology 2021, 96, e876–e889. [Google Scholar] [CrossRef]
- Lapa, S.; Foerch, C.; Singer, O.C.; Hattingen, E.; Luger, S. Ischemic Lesion Location Based on the ASPECT Score for Risk Assessment of Neurogenic Dysphagia. Dysphagia 2020. [Google Scholar] [CrossRef]
- Singh, A.; Khatri, G.; Handa, K.K. Unusual cause of dysphagia and dysphonia. BMJ Case Rep. 2021, 14, e243060. [Google Scholar] [CrossRef]
- Schumann-Werner, B.; Dogan, I.; Mirzazade, S.; Mall, B.; Overbeck, R.; Honrath, P.; Schulz, J.B.; Reetz, K.; Werner, C.J. Clinical predictors and neural correlates for compromised swallowing safety in Huntington’s Disease. Eur. J. Neurol. 2021. [Google Scholar] [CrossRef]
- Zeng, L.; Song, Y.; Dong, Y.; Wu, Q.; Zhang, L.; Yu, L.; Gao, L.; Shi, Y. Risk Score for Predicting Dysphagia in Patients After Neurosurgery: A Prospective Observational Trial. Front. Neurol. 2021, 12, 605687. [Google Scholar] [CrossRef]
- Kazachkov, M.; Palma, J.A.; Norcliffe-Kaufmann, L.; Bar-Aluma, B.E.; Spalink, C.L.; Barnes, E.P.; Amoroso, N.E.; Balou, S.M.; Bess, S.; Chopra, A.; et al. Respiratory care in familial dysautonomia: Systematic review and expert consensus recommendations. Respir. Med. 2018, 141, 37–46. [Google Scholar] [CrossRef]
- Alty, J.; Robson, J.; Duggan-Carter, P.; Jamieson, S. What to do when people with Parkinson’s disease cannot take their usual oral medications. Pract. Neurol. 2016, 16, 122–128. [Google Scholar] [CrossRef]
- Dziewas, R.; Allescher, H.D.; Aroyo, I.; Bartolome, G.; Beilenhoff, U.; Bohlender, J.; Breitbach-Snowdon, H.; Fheodoroff, K.; Glahn, J.; Heppner, H.J.; et al. Diagnosis and treatment of neurogenic dysphagia—S1 guideline of the German Society of Neurology. Neurol. Res. Pract. 2021, 3, 23. [Google Scholar] [CrossRef]
- Yang, F.Z.; Jehu, D.A.M.; Ouyang, H.; Lam, F.M.H.; Pang, M.Y.C. The impact of stroke on bone properties and muscle-bone relationship: A systematic review and meta-analysis. Osteoporos. Int. 2020, 31, 211–224. [Google Scholar] [CrossRef]
- Carda, S.; Cisari, C.; Invernizzi, M.; Bevilacqua, M. Osteoporosis after stroke: A review of the causes and potential treatments. Cerebrovasc. Dis. 2009, 28, 191–200. [Google Scholar] [CrossRef]
- Siotto, M.; Germanotta, M.; Santoro, M.; Di Blasi, C.; Loreti, C.; Mastropaolo, S.; Aprile, I. Total Serum Calcium and Recovery after Rehabilitation in Patients with Stroke. Appl. Sci. 2020, 10, 7893. [Google Scholar] [CrossRef]
- Lee, H.Y.; Park, J.H.; Lee, H.; Kim, T.W.; Yoo, S.D. Does Hip Bone Density Differ between Paretic and Non-Paretic Sides in Hemiplegic Stroke Patients? and Its Relationship with Physical Impairment. J. Bone Metab. 2020, 27, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.Y.; Sung, S.F.; Huang, H.K. Drug treatment strategies for osteoporosis in stroke patients. Expert Opin. Pharm. 2020, 21, 811–821. [Google Scholar] [CrossRef]
- Kaiafa, G.; Savopoulos, C.; Kanellos, I.; Mylonas, K.S.; Tsikalakis, G.; Tegos, T.; Kakaletsis, N.; Hatzitolios, A.I. Anemia and stroke: Where do we stand? Acta Neurol. Scand. 2017, 135, 596–602. [Google Scholar] [CrossRef]
- Li, Z.; Zhou, T.; Li, Y.; Chen, P.; Chen, L. Anemia increases the mortality risk in patients with stroke: A meta-analysis of cohort studies. Sci. Rep. 2016, 6, 26636. [Google Scholar] [CrossRef]
- Milionis, H.; Papavasileiou, V.; Eskandari, A.; D’Ambrogio-Remillard, S.; Ntaios, G.; Michel, P. Anemia on admission predicts short- and long-term outcomes in patients with acute ischemic stroke. Int. J. Stroke 2015, 10, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Bhavi, S.B.; Jaju, P.B. Intravenous iron sucrose v/s oral ferrous fumarate for treatment of anemia in pregnancy. A randomized controlled trial. BMC Pregnancy Childbirth 2017, 17, 137. [Google Scholar] [CrossRef] [Green Version]
- Chan, T.; Ganasekaran, G. The Effect of Anemia on the Functional Outcomes of the Stroke Patients and the Efficiency of their Stroke Rehabilitation. J. Stroke Cereb. Dis. 2015, 24, 1438–1442. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, Y.; Wakabayashi, H.; Shiraishi, A.; Nagano, F.; Bise, T.; Shimazu, S. Hemoglobin Improvement is Positively Associated with Functional Outcomes in Stroke Patients with Anemia. J. Stroke Cereb. Dis. 2021, 30, 105453. [Google Scholar] [CrossRef]
- Mas, M.F.; González, J.; Frontera, W.R. Stroke and sarcopenia. Curr. Phys. Med. Rehabil. Rep. 2020, 8, 452–460. [Google Scholar] [CrossRef]
- Su, Y.; Yuki, M.; Otsuki, M. Prevalence of stroke-related sarcopenia: A systematic review and meta-analysis. J. Stroke Cereb. Dis. 2020, 29, 105092. [Google Scholar] [CrossRef] [PubMed]
- Nagano, F.; Yoshimura, Y.; Bise, T.; Shimazu, S.; Shiraishi, A. Muscle mass gain is positively associated with functional recovery in patients with sarcopenia after stroke. J. Stroke Cereb. Dis. 2020, 29, 105017. [Google Scholar] [CrossRef]
- Yoshimura, Y.; Bise, T.; Shimazu, S.; Tanoue, M.; Tomioka, Y.; Araki, M.; Nishino, T.; Kuzuhara, A.; Takatsuki, F. Effects of a leucine-enriched amino acid supplement on muscle mass, muscle strength, and physical function in post-stroke patients with sarcopenia: A randomized controlled trial. Nutrition 2019, 58, 1–6. [Google Scholar] [CrossRef]
- Lathuilière, A.; Mareschal, J.; Graf, C.E. How to Prevent Loss of Muscle Mass and Strength among Older People in Neuro-Rehabilitation? Nutrients 2019, 11, 881. [Google Scholar] [CrossRef] [Green Version]
- Hill, M.D. Stroke and diabetes mellitus. Handb. Clin. Neurol. 2014, 126, 167–174. [Google Scholar] [CrossRef]
- Chen, R.; Ovbiagele, B.; Feng, W. Diabetes and Stroke: Epidemiology, Pathophysiology, Pharmaceuticals and Outcomes. Am. J. Med. Sci. 2016, 351, 380–386. [Google Scholar] [CrossRef] [Green Version]
- Lau, L.H.; Lew, J.; Borschmann, K.; Thijs, V.; Ekinci, E.I. Prevalence of diabetes and its effects on stroke outcomes: A meta-analysis and literature review. J. Diabetes Investig. 2019, 10, 780–792. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; He, J.R.; Liang, H.B.; Lu, W.J.; Yang, G.Y.; Liu, J.R.; Zeng, L.L. Diabetes mellitus is associated with late-onset post-stroke depression. J. Affect. Disord. 2017, 221, 222–226. [Google Scholar] [CrossRef]
- Gaillard, T.; Miller, E. Guidelines for Stroke Survivors with Diabetes Mellitus. Stroke 2018, 49, e215–e217. [Google Scholar] [CrossRef]
- Papadaki, A.; Nolen-Doerr, E.; Mantzoros, C.S. The Effect of the Mediterranean Diet on Metabolic Health: A Systematic Review and Meta-Analysis of Controlled Trials in Adults. Nutrients 2020, 12, 3342. [Google Scholar] [CrossRef]
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Das, A.; Hartley, L.; Stranges, S. Mediterranean-Style Diet for the Primary and Secondary Prevention of Cardiovascular Disease: A Cochrane Review. Glob. Heart 2020, 15, 56. [Google Scholar] [CrossRef]
- Grosso, G.; Marventano, S.; Yang, J.; Micek, A.; Pajak, A.; Scalfi, L.; Galvano, F.; Kales, S.N. A comprehensive meta-analysis on evidence of Mediterranean diet and cardiovascular disease: Are individual components equal? Crit. Rev. Food Sci. Nutr. 2017, 57, 3218–3232. [Google Scholar] [CrossRef]
- Coltell, O.; Ortega-Azorín, C.; Sorlí, J.V.; Portolés, O.; Asensio, E.M.; Saiz, C.; Barragán, R.; Estruch, R.; Corella, D. Circulating Adiponectin and Its Association with Metabolic Traits and Type 2 Diabetes: Gene-Diet Interactions Focusing on Selected Gene Variants and at the Genome-Wide Level in High-Cardiovascular Risk Mediterranean Subjects. Nutrients 2021, 13, 541. [Google Scholar] [CrossRef]
- Barnard, N.D.; Alwarith, J.; Rembert, E.; Brandon, L.; Nguyen, M.; Goergen, A.; Horne, T.; do Nascimento, G.F.; Lakkadi, K.; Tura, A.; et al. A Mediterranean Diet and Low-Fat Vegan Diet to Improve Body Weight and Cardiometabolic Risk Factors: A Randomized, Cross-over Trial. J. Am. Coll. Nutr. 2021, 62, 100060. [Google Scholar] [CrossRef]
- Yubero-Serrano, E.M.; Fernandez-Gandara, C.; Garcia-Rios, A.; Rangel-Zuñiga, O.A.; Gutierrez-Mariscal, F.M.; Torres-Peña, J.D.; Marin, C.; Lopez-Moreno, J.; Castaño, J.P.; Delgado-Lista, J.; et al. Mediterranean diet and endothelial function in patients with coronary heart disease: An analysis of the CORDIOPREV randomized controlled trial. PLoS Med. 2020, 17, e1003282. [Google Scholar] [CrossRef]
- Chrysohoou, C.; Panagiotakos, D.B.; Pitsavos, C.; Das, U.N.; Stefanadis, C. Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: The ATTICA Study. J. Am. Coll. Cardiol. 2004, 44, 152–158. [Google Scholar] [CrossRef] [Green Version]
- Dai, J.; Jones, D.P.; Goldberg, J.; Ziegler, T.R.; Bostick, R.M.; Wilson, P.W.; Manatunga, A.K.; Shallenberger, L.; Jones, L.; Vaccarino, V. Association between adherence to the Mediterranean diet and oxidative stress. Am. J. Clin. Nutr. 2008, 88, 1364–1370. [Google Scholar] [CrossRef]
- Estruch, R. Anti-inflammatory effects of the Mediterranean diet: The experience of the PREDIMED study. Proc. Nutr. Soc. 2010, 69, 333–340. [Google Scholar] [CrossRef] [Green Version]
- Morris, M.C.; Tangney, C.C.; Wang, Y.; Sacks, F.M.; Barnes, L.L.; Bennett, D.A.; Aggarwal, N.T. MIND diet slows cognitive decline with aging. Alzheimers Dement. 2015, 11, 1015–1022. [Google Scholar] [CrossRef] [Green Version]
- Berendsen, A.M.; Kang, J.H.; Feskens, E.J.M.; de Groot, C.P.G.M.; Grodstein, F.; van de Rest, O. Association of Long-Term Adherence to the MIND Diet with Cognitive Function and Cognitive Decline in American Women. J. Nutr. Health Aging 2018, 22, 222–229. [Google Scholar] [CrossRef]
- Morris, M.C.; Tangney, C.C.; Wang, Y.; Sacks, F.M.; Bennett, D.A.; Aggarwal, N.T. MIND diet associated with reduced incidence of Alzheimer’s disease. Alzheimers Dement. 2015, 11, 1007–1014. [Google Scholar] [CrossRef] [Green Version]
- Cherian, L.; Wang, Y.; Fakuda, K.; Leurgans, S.; Aggarwal, N.; Morris, M. Mediterranean-Dash Intervention for Neurodegenerative Delay (MIND) Diet Slows Cognitive Decline After Stroke. J. Prev. Alzheimers Dis. 2019, 6, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Samieri, C.; Féart, C.; Proust-Lima, C.; Peuchant, E.; Tzourio, C.; Stapf, C.; Berr, C.; Barberger-Gateau, P. Olive oil consumption, plasma oleic acid, and stroke incidence: The Three-City Study. Neurology 2011, 77, 418–425. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Hoffmann, G. Monounsaturated fatty acids, olive oil and health status: A systematic review and meta-analysis of cohort studies. Lipids Health Dis. 2014, 13, 154. [Google Scholar] [CrossRef] [Green Version]
- Martínez-González, M.A.; Dominguez, L.J.; Delgado-Rodríguez, M. Olive oil consumption and risk of CHD and/or stroke: A meta-analysis of case-control, cohort and intervention studies. Br. J. Nutr. 2014, 112, 248–259. [Google Scholar] [CrossRef] [Green Version]
- Mohagheghi, F.; Bigdeli, M.R.; Rasoulian, B.; Hashemi, P.; Pour, M.R. The neuroprotective effect of olive leaf extract is related to improved blood-brain barrier permeability and brain edema in rat with experimental focal cerebral ischemia. Phytomedicine 2011, 18, 170–175. [Google Scholar] [CrossRef]
- Rabiei, Z.; Bigdeli, M.R.; Rasoulian, B.; Ghassempour, A.; Mirzajani, F. The neuroprotection effect of pretreatment with olive leaf extract on brain lipidomics in rat stroke model. Phytomedicine 2012, 19, 940–946. [Google Scholar] [CrossRef]
- Zamani, M.; Hassanshahi, J.; Soleimani, M.; Zamani, F. Neuroprotective effect of olive oil in the hippocampus CA1 neurons following ischemia: Reperfusion in mice. J. Neurosci. Rural Pract. 2013, 4, 164–170. [Google Scholar] [CrossRef]
- Vargas-Molina, S.; Petro, J.L.; Romance, R.; Kreider, R.B.; Schoenfeld, B.J.; Bonilla, D.A.; Benítez-Porres, J. Effects of a ketogenic diet on body composition and strength in trained women. J. Int. Soc. Sports Nutr. 2020, 17, 19. [Google Scholar] [CrossRef] [Green Version]
- Takeuchi, F.; Nishikata, N.; Nishimura, M.; Nagao, K.; Kawamura, M. Leucine-Enriched Essential Amino Acids Enhance the Antiseizure Effects of the Ketogenic Diet in Rats. Front. Neurosci. 2021, 15, 225. [Google Scholar] [CrossRef]
- Arora, N.; Mehta, T.R. Role of the ketogenic diet in acute neurological diseases. Clin. Neurol. Neurosurg. 2020, 192, 105727. [Google Scholar] [CrossRef]
- Maalouf, M.; Sullivan, P.G.; Davis, L.; Kim, D.Y.; Rho, J.M. Ketones inhibit mitochondrial production of reactive oxygen species production following glutamate excitotoxicity by increasing NADH oxidation. Neuroscience 2007, 145, 256–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, B.; Yang, X.; An, L.; Gao, B.; Liu, X.; Liu, S. Ketogenic diet protects dopaminergic neurons against 6-OHDA neurotoxicity via up-regulating glutathione in a rat model of Parkinson’s disease. Brain Res. 2009, 1286, 25–31. [Google Scholar] [CrossRef]
- Julio-Amilpas, A.; Montiel, T.; Soto-Tinoco, E.; Gerónimo-Olvera, C.; Massieu, L. Protection of hypoglycemia-induced neuronal death by β-hydroxybutyrate involves the preservation of energy levels and decreased production of reactive oxygen species. J. Cereb. Blood Flow Metab. 2015, 35, 851–860. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, M.; Sato, K.; Dohi, S.; Sato, T.; Matsuura, A.; Hiraide, A. Effect of beta-hydroxybutyrate, a cerebral function improving agent, on cerebral hypoxia, anoxia and ischemia in mice and rats. Jpn. J. Pharm. 2001, 87, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, M.; Kitamura, Y.; Mori, S.; Sato, K.; Dohi, S.; Sato, T.; Matsuura, A.; Hiraide, A. Beta-hydroxybutyrate, a cerebral function improving agent, protects rat brain against ischemic damage caused by permanent and transient focal cerebral ischemia. Jpn. J. Pharm. 2002, 89, 36–43. [Google Scholar] [CrossRef] [Green Version]
- Yang, Q.; Guo, M.; Wang, X.; Zhao, Y.; Zhao, Q.; Ding, H.; Dong, Q.; Cui, M. Ischemic preconditioning with a ketogenic diet improves brain ischemic tolerance through increased extracellular adenosine levels and hypoxia-inducible factors. Brain Res. 2017, 1667, 11–18. [Google Scholar] [CrossRef]
- Shaafi, S.; Sharifi-Bonab, M.; Ghaemian, N.; Mokhtarkhani, M.; Akbari, H. Early Motor-Behavioral Outcome of Ischemic Stroke with Ketogenic Diet Preconditioning: Interventional Animal Study. J. Stroke Cereb. Dis. 2019, 28, 1032–1039. [Google Scholar] [CrossRef] [PubMed]
- Han, P.; Zhang, W.; Kang, L.; Ma, Y.; Fu, L.; Jia, L.; Yu, H.; Chen, X.; Hou, L.; Wang, L.; et al. Clinical Evidence of Exercise Benefits for Stroke. Adv. Exp. Med. Biol. 2017, 1000, 131–151. [Google Scholar] [CrossRef]
- Diekmann, R.; Wojzischke, J. The role of nutrition in geriatric rehabilitation. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 14–18. [Google Scholar] [CrossRef] [PubMed]
- Kokura, Y.; Maeda, K.; Wakabayashi, H.; Nishioka, S.; Higashi, S. High Nutritional-Related Risk on Admission Predicts Less Improvement of Functional Independence Measure in Geriatric Stroke Patients: A Retrospective Cohort Study. J. Stroke Cereb. Dis. 2016, 25, 1335–1341. [Google Scholar] [CrossRef]
- Nishioka, S.; Wakabayashi, H.; Nishioka, E.; Yoshida, T.; Mori, N.; Watanabe, R. Nutritional Improvement Correlates with Recovery of Activities of Daily Living among Malnourished Elderly Stroke Patients in the Convalescent Stage: A Cross-Sectional Study. J. Acad. Nutr. Diet. 2016, 116, 837–843. [Google Scholar] [CrossRef] [PubMed]
- Shimazu, S.; Yoshimura, Y.; Kudo, M.; Nagano, F.; Bise, T.; Shiraishi, A.; Sunahara, T. Frequent and personalized nutritional support leads to improved nutritional status, activities of daily living, and dysphagia after stroke. Nutrition 2021, 83, 111091. [Google Scholar] [CrossRef]
- Nishioka, S.; Wakabayashi, H.; Yoshida, T.; Mori, N.; Watanabe, R.; Nishioka, E. Obese Japanese Patients with Stroke Have Higher Functional Recovery in Convalescent Rehabilitation Wards: A Retrospective Cohort Study. J. Stroke Cereb. Dis. 2016, 25, 26–33. [Google Scholar] [CrossRef]
- Burke, D.T.; Al-Adawi, S.; Bell, R.B.; Easley, K.; Chen, S.; Burke, D.P. Effect of body mass index on stroke rehabilitation. Arch. Phys. Med. Rehabil. 2014, 95, 1055–1059. [Google Scholar] [CrossRef]
- Rabadi, M.H.; Coar, P.L.; Lukin, M.; Lesser, M.; Blass, J.P. Intensive nutritional supplements can improve outcomes in stroke rehabilitation. Neurology 2008, 71, 1856–1861. [Google Scholar] [CrossRef] [PubMed]
- Ramasamy, D.K.; Dutta, T.; Kannan, V.; Chandramouleeswaran, V. Amino acids in post-stroke rehabilitation. Nutr. Neurosci. 2021, 24, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Aquilani, R.; Boselli, M.; D’Antona, G.; Baiardi, P.; Boschi, F.; Viglio, S.; Iadarola, P.; Pasini, E.; Barbieri, A.; Dossena, M.; et al. Unaffected arm muscle hypercatabolism in dysphagic subacute stroke patients: The effects of essential amino acid supplementation. BioMed Res. Int. 2014, 2014, 964365. [Google Scholar] [CrossRef]
- Ikeda, T.; Morotomi, N.; Kamono, A.; Ishimoto, S.; Miyazawa, R.; Kometani, S.; Sako, R.; Kaneko, N.; Iida, M.; Kawate, N. The Effects of Timing of a Leucine-Enriched Amino Acid Supplement on Body Composition and Physical Function in Stroke Patients: A Randomized Controlled Trial. Nutrients 2020, 12, 1928. [Google Scholar] [CrossRef] [PubMed]
- Sari, A.; Durmus, B.; Karaman, C.A.; Ogut, E.; Aktas, I. A randomized, double-blind study to assess if vitamin D treatment affects the outcomes of rehabilitation and balance in hemiplegic patients. J. Phys. Ther. Sci. 2018, 30, 874–878. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.; Prabhakar, S.; Modi, M.; Bhadada, S.K.; Kalaivani, M.; Lal, V.; Khurana, D. Effect of Vitamin D and calcium supplementation on ischaemic stroke outcome: A randomised controlled open-label trial. Int. J. Clin. Pract. 2016, 70, 764–770. [Google Scholar] [CrossRef]
- Siotto, M.; Santoro, M.; Aprile, I. Vitamin D and Rehabilitation after Stroke: Status of Art. Appl. Sci. 2020, 10, 1973. [Google Scholar] [CrossRef] [Green Version]
- Utkan Karasu, A.; KarataŞ, G.K. Effect of Vitamin D Supplementation on Lower Extremity Motor Function and Ambulation in Stroke Patients. Turk. J. Med. Sci. 2021, 51, 1413–1419. [Google Scholar] [CrossRef]
- Momosaki, R.; Abo, M.; Urashima, M. Vitamin D Supplementation and Post-Stroke Rehabilitation: A Randomized, Double-Blind, Placebo-Controlled Trial. Nutrients 2019, 11, 1295. [Google Scholar] [CrossRef] [Green Version]
- Hannan, M.A.; Dash, R.; Haque, M.N.; Mohibbullah, M.; Sohag, A.A.M.; Rahman, M.A.; Uddin, M.J.; Alam, M.; Moon, I.S. Neuroprotective Potentials of Marine Algae and Their Bioactive Metabolites: Pharmacological Insights and Therapeutic Advances. Mar. Drugs 2020, 18, 347. [Google Scholar] [CrossRef]
- Hu, L.; Chen, W.; Tian, F.; Yuan, C.; Wang, H.; Yue, H. Neuroprotective role of fucoxanthin against cerebral ischemic/reperfusion injury through activation of Nrf2/HO-1 signaling. Biomed. Pharm. 2018, 106, 1484–1489. [Google Scholar] [CrossRef] [PubMed]
- Pangestuti, R.; Vo, T.S.; Ngo, D.H.; Kim, S.K. Fucoxanthin ameliorates inflammation and oxidative reponses in microglia. J. Agric. Food Chem. 2013, 61, 3876–3883. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Zhang, J.; Wang, C.; Sun, Q. Tanshinone inhibits neuronal cell apoptosis and inflammatory response in cerebral infarction rat model. Int. J. Immunopathol. Pharm. 2017, 30, 123–129. [Google Scholar] [CrossRef] [Green Version]
- Lin, J.; Huang, L.; Yu, J.; Xiang, S.; Wang, J.; Zhang, J.; Yan, X.; Cui, W.; He, S.; Wang, Q. Fucoxanthin, a Marine Carotenoid, Reverses Scopolamine-Induced Cognitive Impairments in Mice and Inhibits Acetylcholinesterase in Vitro. Mar. Drugs 2016, 14, 67. [Google Scholar] [CrossRef] [Green Version]
- Wu, S.; Yue, Y.; Tian, H.; Tao, L.; Wang, Y.; Xiang, J.; Wang, S.; Ding, H. Tramiprosate protects neurons against ischemic stroke by disrupting the interaction between PSD95 and nNOS. Neuropharmacology 2014, 83, 107–117. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, N.S.; Jeong, Y.G.; Lee, J.H.; Kim, E.J.; Han, S.Y. Protective efficacy of an Ecklonia cava extract used to treat transient focal ischemia of the rat brain. Anat. Cell Biol. 2012, 45, 103–113. [Google Scholar] [CrossRef] [Green Version]
- Cui, Y.; Amarsanaa, K.; Lee, J.H.; Rhim, J.K.; Kwon, J.M.; Kim, S.H.; Park, J.M.; Jung, S.C.; Eun, S.Y. Neuroprotective mechanisms of dieckol against glutamate toxicity through reactive oxygen species scavenging and nuclear factor-like 2/heme oxygenase-1 pathway. Korean J. Physiol Pharm. 2019, 23, 121–130. [Google Scholar] [CrossRef] [Green Version]
- Zhao, D.; Kwon, S.H.; Chun, Y.S.; Gu, M.Y.; Yang, H.O. Anti-Neuroinflammatory Effects of Fucoxanthin via Inhibition of Akt/NF-κB and MAPKs/AP-1 Pathways and Activation of PKA/CREB Pathway in Lipopolysaccharide-Activated BV-2 Microglial Cells. Neurochem. Res. 2017, 42, 667–677. [Google Scholar] [CrossRef]

| Study, Year, Reference | Study Design | Group 1 | Group 2 | Group 3 | Outcome Measures | Main Findings |
|---|---|---|---|---|---|---|
| Kokura et al., 2016 [76] | Retrospective cohort study; n = 540 | High GNRI < 92; n = 480 | Low GNRI ≥ 92; n = 60 | - | FIM |
|
| Nishioka et al., 2016 [77] | cross-sectional study n = 178 | MNA-SF NI | MNA-SF LI | MNA-SF GI | FIM |
|
| Shimazu et al., 2021 [78] | single-left prospective cohort study; n = 454 | low- frequency dietary prescription | high- frequency dietary prescription | - | FIM | Patients in the high-frequency group had lower FIM-motor scores at discharge but greater FIM-motor gains than low-frequency group. |
| Rabadi et al., 2008 [81] | Clinical trial, n = 116 | intensive nutritional supplementation | standard nutritional supplementation | - | FIM, 2-minute and 6-minute timed walk tests | Intensive nutritional supplementation group improved more than standard nutritional supplementation group in motor function. |
| Study, Year, Reference | Study Design | Group 1 | Group 2 | Outcome Measures | Main Findings |
|---|---|---|---|---|---|
| Yoshimura et al., 2019 [38] | RCT; n = 44 | Supplement composition: 3 g of leucine 40% enriched essential amino acids and 9.7 g of carbohydrate | No supplementation | FIM, SMI, handgrip strength | ↑ FIM score, significantly greater improvement in the IG than in the CG (p < 0.045). ↑ handgrip strength, significantly greater improvement in the IG (p < 0.01). ↑ SMI in the IG but not in the CG over time, significantly greater improvement in the intervention group. |
| Ikeda T, et al., 2020 [84] | RCT; n = 69 | 3.5 g of amino acids, 6.5 g of protein and 40 IU of vitamin D per 125 mL at breakfast | 3.5 g of amino acids, 6.5 g of protein and 40 IU of vitamin D per 125 mL post-exercise | skeletal muscle mass, lower limb isometric strength, grip strength, TUGT, BBS, FIM |
|
| Utkan Karasu 2021 et al., [88] | n = 76 | 50,000 IU of vitamin D weekly for 4–12 weeks | No supplementation | FAC, BRS lower extremity | ↑ changes in FAC and BRS scores in group 1 (p = 0.005 and p = 0.018). ↑ changes in FAC and BRS scores in patients who were undergoing rehabilitation for the first time and/or in the first 3 months after stroke in group 1 than group 2 (p < 0.05). In patients > 3 months after stroke, vitamin D treatment did not affect FAC and BRS scores. |
| Gupta et al., 2016 [86] | RCT; n = 73 | Vitamin D (600,000 IU single intramuscular injection and 60,000 IU once a month) + calcium (one gram per day) for 6 months | No supplementation, only usual care | Modified Rankin scale | Patients supplemented with vitamin D and calcium had better results in modified Rankin scale than control group receiving only usual care. |
| Sari et al., 2018 [85] | RCT; n = 132 | 300,000 IU vitamin D injection | saline intramuscular injection | BRS, FAS, MBI, BBS | The BBS results and MBI scores significantly differed between the two groups (higher scores in vitamin D group), but BRS and FAS test results did not significantly differ. |
| Momosaki et al., 2019 [89] | RCT; n = 100 | Vitamin D (2000 IU per day) 8 weeks | placebo | Barthel index | The mean gain in the Barthel index score: 19.0 ± 14.8 in group 1 and 19.5 ± 13.1 in group 2 (p = 0.88). The Barthel index efficiency was 0.32 ± 0.31 in group 1 and 0.28 ± 0.21 in group 2 (p = 0.38). There was no significantly higher improvement in rehabilitation outcomes in the supplemented group. |
| Study, Year, Reference | Study Design | Supplementation | Outcome Measures | Main Findings | |
|---|---|---|---|---|---|
| Fucoxanthin (Fx) | Hu et al., 2018 [91] | MCAO rat | Intragastrically administrated; 30, 60 and 90 mg/kg Fx; 1 h before MCAO induction | Infarct area; neurological function; brain water content of rats | Effect in dose-dependent manner Improvement of the neurologic deficit Decrease in the infarct volume Reduction in the level of apoptosis-associated proteins in brain tissues |
| In vitro study OGD/R model (rat cortical neuron) | 5, 10 and 20 μM Fx | Oxidative stress level; apoptosis level | Inhibition of increased caspase 3 expression Decrease in Bcl-2/Bax ratio Increase in SOD activity Decrease in MDA level Inhibition of OGD/R-induced apoptosis Decrease in ROS accumulation | ||
| Pangestuti et al., 2013 [92] | In vitro study (amyloid-β42-induced BV2 microglia cells) | 5, 10 and 50 μM Fx | Level of oxidative stress and inflammation | Inhibition of phosphorylation of MAPK pathway Inhibition of free radical-induced DNA oxidation Decrease in intracellular ROS production Increase in antioxidative enzymes activity | |
| Zhou et al., 2017 [93] | In vitro study (BV-2 cells) | 5, 10 and 20 μM Fx | Anti-inflammatory, antioxidant and neuroprotective effect | Effect in dose-dependent manner Inhibition of proinflammatory mediators, both protein and mRNA expression: TNF-α, IL-6, PGE2, ROS, NO and COX, iNOS Inhibition of Akt/NFκB and MAPK/AP-1 pathways Promotion of BDNF production | |
| Lin et al., 2016 [94] | Institute of Cancer Research (ICR) mice | Six groups:
| Impact on scopolamine-induced cognitive impairments; impact on AChE activity; further examined if fucoxanthin could directly inhibit AChE in vitro | Improved cognitive impairments Decrease in AChE activity Decrease in choline acetyltransferase activity and BDNF expression Inhibition of AChE with an IC50 value of 81.2 μM | |
| Tramiprosate | Wu et al., 2014 [95] | MCAO rats | 50 mg/kg | Neuroprotective effect and impact on functional recovery | Effect in dose-dependent manner Reduction in the infarct volume Therapeutic window—6 h Improvement of neurological status Neuroprotective effect expressed by NMDAR Decrease in nNOS/PSD95 association Suppression of nNOS translocation to membrane |
| Phlorotannin | Kim et al., 2012 [96] | MCAO rats | Ecklonia cava polyphenols at 10 mg/kg and 50 mg/kg intraperitoneally administrated | Neuroprotective effect | Effect in dose-dependent manner Decrease in the extent of brain edema and infarct volume Inhibition of apoptosis Improvement of decreased neurological motor function |
| In vitro study (differentiated neuroblastoma cell line SH-SY5Y) | Improvement of cell viability Decrease in H2O2-induced oxidative stress Inhibition of increased cytosolic calcium Reduction in calcium-induced neurotoxicity | ||||
| Cui et al., 2019 [97] | In vitro study (primary cortical neurons HT22 neurons) | 100 µM, 24 h; 5 mM, 12 h | Neuroprotective effect | Effect in dose-dependent manner Enhancement of cell viability Recovery of neurons’ morphological deterioration Suppression of intracellular ROS level, disruption of mitochondrial membrane potential, overload of ROS and Ca2+ in mitochondria and ATP depletion Inhibition of oxidative stress Activation of Nrf2/HO-1 pathway |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zielińska-Nowak, E.; Cichon, N.; Saluk-Bijak, J.; Bijak, M.; Miller, E. Nutritional Supplements and Neuroprotective Diets and Their Potential Clinical Significance in Post-Stroke Rehabilitation. Nutrients 2021, 13, 2704. https://doi.org/10.3390/nu13082704
Zielińska-Nowak E, Cichon N, Saluk-Bijak J, Bijak M, Miller E. Nutritional Supplements and Neuroprotective Diets and Their Potential Clinical Significance in Post-Stroke Rehabilitation. Nutrients. 2021; 13(8):2704. https://doi.org/10.3390/nu13082704
Chicago/Turabian StyleZielińska-Nowak, Ewa, Natalia Cichon, Joanna Saluk-Bijak, Michał Bijak, and Elzbieta Miller. 2021. "Nutritional Supplements and Neuroprotective Diets and Their Potential Clinical Significance in Post-Stroke Rehabilitation" Nutrients 13, no. 8: 2704. https://doi.org/10.3390/nu13082704
APA StyleZielińska-Nowak, E., Cichon, N., Saluk-Bijak, J., Bijak, M., & Miller, E. (2021). Nutritional Supplements and Neuroprotective Diets and Their Potential Clinical Significance in Post-Stroke Rehabilitation. Nutrients, 13(8), 2704. https://doi.org/10.3390/nu13082704








