Association of Diet, Physical Activity Guidelines and Cardiometabolic Risk Markers in Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Physical Activity
2.2. Dietary Habits
2.3. Body Composition
2.4. Blood Cardiometabolic Risk Markers
2.5. Statistical Analysis
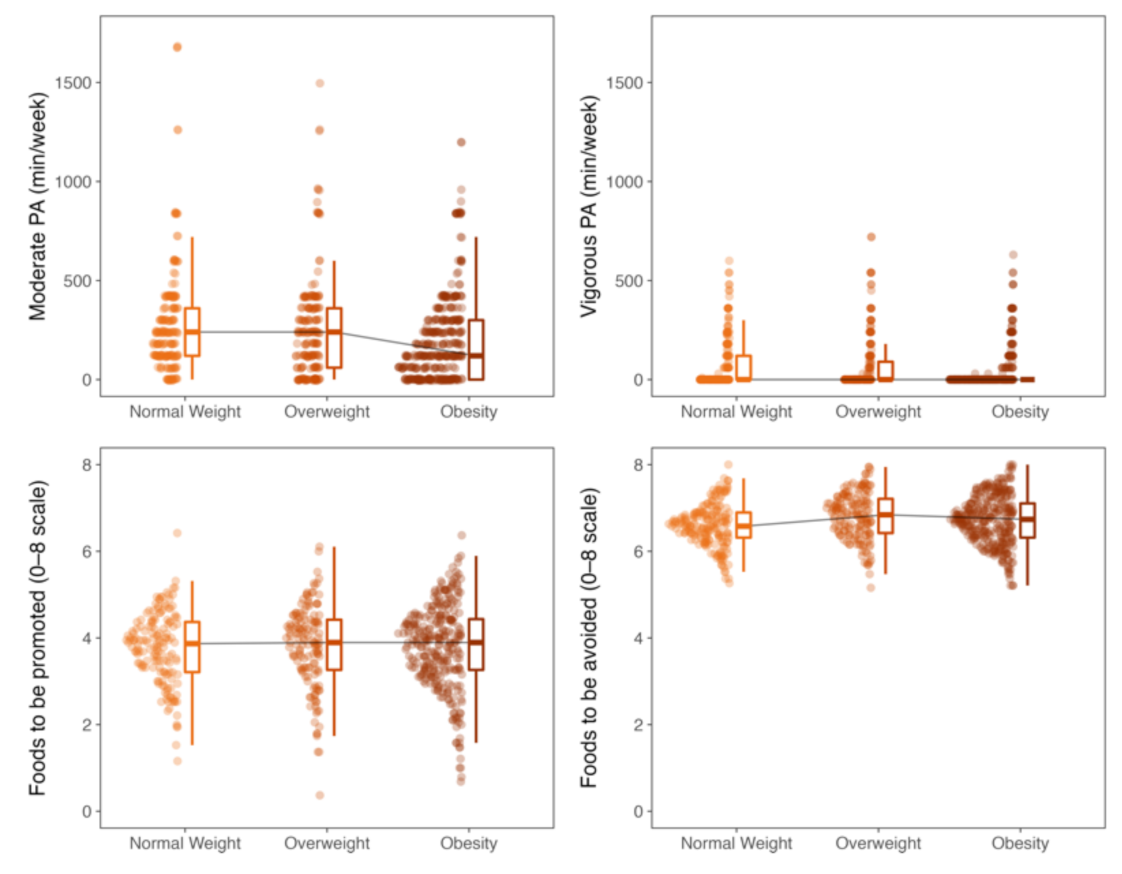
3. Results
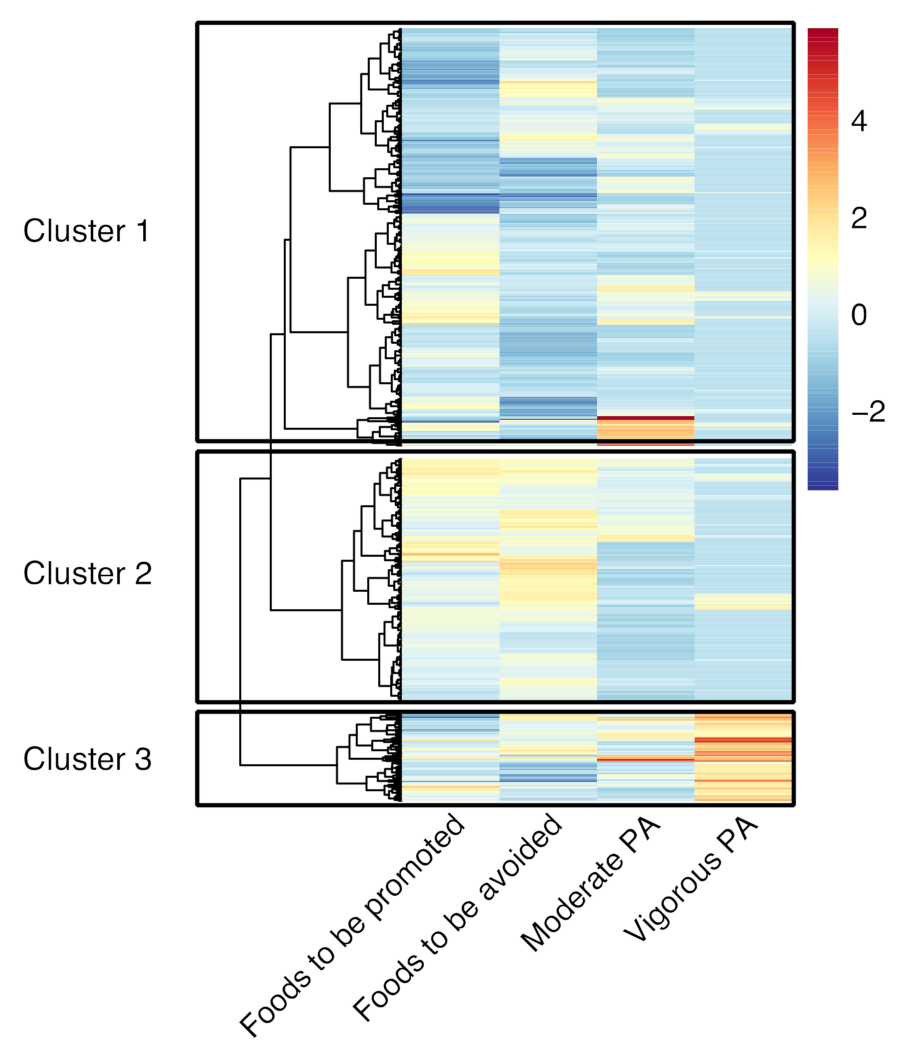
Clusters of Adherence to Dietary and Physical Activity Recommendations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- Anguita-Ruiz, A.; Mendez-Gutierrez, A.; Ruperez, A.I.; Leis, R.; Bueno, G.; Gil-Campos, M.; Tofe, I.; Gomez-Llorente, C.; Moreno, L.A.; Gil, Á.; et al. The protein S100A4 as a novel marker of insulin resistance in prepubertal and pubertal children with obesity. Metabolism 2020, 105, 154187. [Google Scholar] [CrossRef]
- Olza, J.; Ruperez, A.I.; Gil-Campos, M.; Leis, R.; Fernandez-Orth, D.; Tojo, R.; Cañete, R.; Gil, A.; Aguilera, C.M. Influence of FTO variants on obesity, inflammation and cardiovascular disease risk biomarkers in Spanish children: A case–control multicentre study. BMC Med. Genet. 2013, 14, 123. [Google Scholar] [CrossRef] [Green Version]
- Olza, J.; Aguilera, C.M.; Gil-Campos, M.; Leis, R.; Bueno, G.; Valle, M.; Cañete, R.; Tojo, R.; Moreno, L.A.; Gil, Á. A Continuous Metabolic Syndrome Score Is Associated with Specific Bi-omarkers of Inflammation and CVD Risk in Prepubertal Children. Ann. Nutr. Metab. 2015, 66, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Han, J.C.; Lawlor, D.A.; Kimm, S.Y. Childhood obesity. Lancet 2010, 375, 1737–1748. [Google Scholar] [CrossRef]
- Ambrosini, G. Childhood dietary patterns and later obesity: A review of the evidence. Proc. Nutr. Soc. 2014, 73, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Devlin, U.M.; McNulty, B.; Nugent, A.; Gibney, M.J. The use of cluster analysis to derive dietary patterns: Methodological considerations, reproducibility, validity and the effect of energy mis-reporting. Proc. Nutr. Soc. 2012, 71, 599–609. [Google Scholar] [CrossRef] [Green Version]
- Aranceta-Bartrina, J.; Partearroyo, T.; López-Sobaler, A.M.; Ortega, R.M.; Varela-Moreiras, G.; Serra-Majem, L.; Pérez-Rodrigo, C. Updating the Food-Based Dietary Guidelines for the Spanish Population: The Spanish Society of Community Nutrition (SENC) Proposal. Nutrients 2019, 11, 2675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trichopoulos, D.; Lagiou, P. Mediterranean diet and overall mortality differences in the European Union. Public Health Nutr. 2004, 7, 949–951. [Google Scholar] [CrossRef] [Green Version]
- Cabrera, S.G.; Fernández, N.H.; Hernández, C.R.; Nissensohn, M.; Román-Viñas, B.; Serra-Majem, L. KIDMED test; Prevalence of low adherence to the mediterranean diet in children and young; A systematic review. Nutr. Hosp. 2015, 32, 2390–2399. [Google Scholar]
- Wu, X.Y.; Han, L.H.; Zhang, J.H.; Luo, S.; Hu, J.W.; Sun, K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE 2017, 12, e0187668. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leblanc, A.G.; Spence, J.C.; Carson, V.; Gorber, S.C.; Dillman, C.; Janssen, I.; Kho, M.; Stearns, J.; Timmons, B.W.; Tremblay, M.S. Systematic review of sedentary behaviour and health indicators in the early years (aged 0–4 years). Appl. Physiol. Nutr. Metab. 2012, 37, 753–772. [Google Scholar] [CrossRef] [Green Version]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behavior; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Lake, A.A.; Mathers, J.C.; Rugg-Gunn, A.J.; Adamson, A. Longitudinal change in food habits between adolescence (11–12 years) and adulthood (32–33 years): The ASH30 Study. J. Public Health 2006, 28, 10–16. [Google Scholar] [CrossRef]
- Telama, R. Tracking of Physical Activity from Childhood to Adulthood: A Review. Obes. Facts 2009, 2, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Plaza-Díaz, J.; Molina-Montes, E.; Soto-Méndez, M.J.; Madrigal, C.; Hernández-Ruiz, Á.; Valero, T.; Villoslada, F.L.; Leis, R.; De Victoria, E.M.; Moreno, J.M.; et al. Clustering of Dietary Patterns and Lifestyles Among Spanish Children in the EsNuPI Study. Nutrients 2020, 12, 2536. [Google Scholar] [CrossRef]
- Ottevaere, C.; the HELENA Study Group; Huybrechts, I.; Benser, J.; De Bourdeaudhuij, I.; Cuenca-Garcia, M.; Dallongeville, J.; Zaccaria, M.; Gottrand, F.; Kersting, M.; et al. Clustering patterns of physical activity, sedentary and dietary behavior among European adolescents: The HELENA study. BMC Public Health 2011, 11, 328. [Google Scholar] [CrossRef]
- Leech, R.M.; McNaughton, S.A.; Timperio, A. The clustering of diet, physical activity and sedentary behavior in children and adolescents: A review. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kowalski, K.C.; Crocker, P.R.; Donen, R.M. The Physical Activity Questionnaire for Older Children (PAQ-C) and Adolescents (PAQ-A) Manual; College of Kinesiology, University of Saskatchewan: Saskatoon, SK, Canada, 2004; Volume 87, pp. 1–38. [Google Scholar]
- Trinidad Rodríguez, I.; Fernández Ballart, J.; Cucó Pastor, G.; Biarnés Jordà, E.; Arija Val, V. Validación de un cuestionario de frecuencia de consumo alimentario corto: Reproducibilidad y validez. Nutr. Hosp. 2008, 23, 242–252. [Google Scholar]
- Lanfer, A.; Hebestreit, A.; Ahrens, W.; Krogh, V.; Sieri, S.; Lissner, L.; Eiben, G.; Siani, A.; Huybrechts, I.; Loit, H.-M. Reproducibility of food consumption frequencies derived from the Children’s Eating Habits Questionnaire used in the IDEFICS study. Int. J. Obes. 2011, 35, S61–S68. [Google Scholar] [CrossRef] [Green Version]
- Latorre-Millán, M.; Rupérez, A.; González-Gil, E.; Santaliestra-Pasías, A.; Vázquez-Cobela, R.; Gil-Campos, M.; Aguilera, C.; Gil, Á.; Moreno, L.; Leis, R.; et al. Dietary Patterns and Their Association with Body Composition and Cardiometabolic Markers in Children and Adolescents: Genobox Cohort. Nutrients 2020, 12, 3424. [Google Scholar] [CrossRef]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity world-wide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar] [CrossRef] [Green Version]
- Kyle, U.G.; Schutz, Y.; Dupertuis, Y.M.; Pichard, C. Body composition interpretation: Contributions of the fat-free mass index and the body fat mass index. Nutrition 2003, 19, 597–604. [Google Scholar] [CrossRef]
- Kalman, M.; Inchley, J.; Sigmundová, D.; Iannotti, R.J.; Tynjälä, J.A.; Hamrik, Z.; Haug, E.; Bucksch, J. Secular trends in moderate-to-vigorous physical activity in 32 countries from 2002 to 2010: A cross-national perspective. Eur. J. Public Health 2015, 25, 37–40. [Google Scholar] [CrossRef] [Green Version]
- Cunha, C.M.; Costa, P.R.F.; de Oliveira, L.P.M.; Queiroz, V.A.O.; Pitangueira, J.C.D.; Oliveira, A.M. Dietary patterns and cardiomet-abolic risk factors among adolescents: Systematic review and meta-analysis. Br. J. Nutr. 2018, 119, 859–879. [Google Scholar] [CrossRef]
- Lopez Sanchez, G.F.; Nicolas Lopez, J.; Diaz Suarez, A. Effects of a program of intense physical activity on the body compo-sition of adolescents from Murcia. SPORT TK-Rev. Euroam. Cienc. Deporte 2016, 5, 83–88. [Google Scholar] [CrossRef] [Green Version]
- Pereira, S.; Katzmarzyk, P.T.; Gomes, T.N.; Borges, A.; Santos, D.; Souza, M.; Santos, F.K.; Chaves, R.N.; Champagne, C.M.; Barreira, T.V.; et al. Profiling physical activity, diet, screen and sleep habits in Portuguese children. Nutrients 2015, 7, 4345–4362. [Google Scholar] [CrossRef] [Green Version]
- Landsberg, B.; Plachta-Danielzik, S.; Lange, D.; Johannsen, M.; Seiberl, J.; Müller, M.J. Clustering of lifestyle factors and associ-ation with overweight in adolescents of the Kiel Obesity Prevention Study. Public Health Nutr. 2010, 13, 1708–1715. [Google Scholar] [CrossRef] [Green Version]
- Hernáez, Á.; Soria-Florido, M.T.; Castañer, O.; Pintó, X.; Estruch, R.; Salas-Salvadó, J.; Corella, D.; Alonso-Gómez, A.; Martínez-González, M.A.; Schröder, H.; et al. Leisure time physical activity is associated with improved HDL func-tionality in high cardiovascular risk individuals: A cohort study. Eur. J. Prev. Cardiol. 2020. [Google Scholar] [CrossRef]
- Huffman, K.M.; Hawk, V.H.; Henes, S.T.; Ocampo, C.I.; Orenduff, M.C.; Slentz, C.A.; Johnson, J.L.; Houmard, J.A.; Samsa, G.P.; Kraus, W.E.; et al. Exercise effects on lipids in persons with varying dietary patterns—does diet matter if they exercise? Responses in Studies of a Targeted Risk Reduction Intervention through Defined Exercise I. Am. Heart J. 2012, 164, 117–124. [Google Scholar] [CrossRef] [Green Version]
- Fedewa, M.V.; Gist, N.H.; Evans, E.M.; Dishman, R.K. Exercise and Insulin Resistance in Youth: A Meta-Analysis. Pediatrics 2013, 133, e163–e174. [Google Scholar] [CrossRef] [Green Version]
- Peplies, J.; Börnhorst, C.; Günther, K.; Fraterman, A.; Russo, P.; Veidebaum, T.; Tornaritis, M.; de Henauw, S.; Marild, S.; Molnar, D.; et al. Longitudinal associations of lifestyle factors and weight status with insulin re-sistance (HOMA-IR) in preadolescent children: The large prospective cohort study IDEFICS. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madrigal, C.; Soto-Méndez, M.J.; Hernández-Ruiz, Á.; Ruiz, E.; Valero, T.; Ávila, J.M.; Lara-Villoslada, F.; Leis, R.; de Victoria, E.M.; Moreno, J.M.; et al. Dietary and Lifestyle Patterns in the Spanish Pediatric Popula-tion (One to <10 Years Old): Design, Protocol, and Methodology of the EsNuPI Study. Nutrients 2019, 11, 3050. [Google Scholar] [CrossRef] [Green Version]
- Aznar, S.; Naylor, P.J.; Silva, P.; Pérez, M.; Angulo, T.; Laguna, M.; Lara, M.T.; López-Chicharro, J. Patterns of physical activity in Spanish children: A descriptive pilot study. Child Care Health Dev. 2010, 37, 322–328. [Google Scholar] [CrossRef]

| Foods to Be Promoted | Foods to Be Avoided |
|---|---|
| Dairy | Sugar, jam, cocoa |
| Fruits | Sweet snacks, salty sacks |
| Vegetables | Soft drinks |
| Whole grains and potatoes | Precooked food |
| Olive oil 1 | Margarine, butter, sunflower oil |
| Lean meats 2 | Sausages |
| Eggs | |
| Fish 3 | |
| Legumes |
| Sex | ES | 95% CI | |||
|---|---|---|---|---|---|
| Total | Female | Male | |||
| N | 549 | 296 (53.9%) | 253 (46.1%) | ||
| Age (years) | 10.52 (8.67–12.30) | 10.50 (8.42–12.33) | 10.53 (8.75–12.30) | −0.01 | −0.11–0.09 |
| BMI category | |||||
| Normal weight | 143 (26.0%) | 67 (22.6%) | 76 (30.0%) | −7.4% | −15.0–0.4% |
| Overweight | 131 (23.9%) | 77 (26.0%) | 54 (21.3%) | 4.7% | −2.8–12.0% |
| Obesity | 275 (50.1%) | 152 (51.4%) | 123 (48.6%) | 2.7% | −6.0–11.0% |
| Physical activity | |||||
| MVPA adherence | 139 (25.4%) | 66 (22.4%) | 73 (28.9%) | −6.5% | −14.0–1.2% |
| Full PA adherence | 38 (6.9%) | 16 (5.4%) | 22 (8.7%) | −3.3% | −8.0–1.4% |
| Moderate PA (min/week) | 180 (60–300) | 120 (60–300) | 180 (60–360) | −0.11 | −0.21–−0.02 |
| Vigorous PA (min/week) | 0 (0–0) | 0 (0–0) | 0 (0–60) | −0.10 | −0.20–0.00 |
| Dietary adherence | |||||
| Promoted foods (0–8 scale) | 3.89 (3.26–4.42) | 3.89 (3.32–4.39) | 3.84 (3.16–4.42) | 0.04 | −0.05–0.14 |
| Avoided foods (0–8 scale) | 6.68 (6.32–7.05) | 6.74 (6.37–7.05) | 6.68 (6.32–7.05) | 0.03 | −0.07–0.13 |
| Body mass | |||||
| Total fat mass (%) | 39.5 (31.8–45.0) | 41.0 (35.7–46.8) | 36.9 (28.1–43.1) | 0.28 | 0.16–0.38 |
| Abdominal fat (%) | 8.9 (8.0–10.1) | 9.2 (8.2–10.4) | 8.6 (7.8–9.9) | 0.18 | 0.04–0.31 |
| Total lean mass (%) | 59.3 (53.3–67.1) | 57.6 (51.2–62.9) | 61.9 (55.3–70.4) | −0.29 | −0.39–−0.18 |
| FFMI (kg/m2) | 13.3 (12.3–14.8) | 13.1 (12.0–14.5) | 13.6 (12.5–14.9) | −0.15 | −0.26–−0.03 |
| FMI (kg/m2) | 0.9 (0.7–1.2) | 1.0 (0.7–1.2) | 0.8 (0.5–1.1) | 0.22 | 0.10–0.33 |
| Cardiometabolic Risk Markers | |||||
| Triacylglycerols (mg/dL) | 62 (46–84) | 64 (52–90) | 55 (41–79) | 0.20 | 0.11–0.30 |
| Cholesterol (mg/dL) | 162 (144–181) | 163 (142–180) | 161 (144–182) | −0.01 | −0.11–0.08 |
| HDL−c (mg/dL) | 49 (41–60) | 48 (40–57) | 51 (43–62) | −0.14 | −0.23–−0.04 |
| LDL−c (mg/dL) | 94 (79–109) | 93 (79–109) | 94 (80–108) | −0.02 | −0.12–0.08 |
| Insulin (mU I/L) | 10.6 (6.1–15.7) | 12.3 (7.8–17.2) | 8.9 (4.7–13.7) | 0.26 | 0.17–0.35 |
| HOMA−IR | 2.09 (1.15–3.26) | 2.47 (1.52–3.55) | 1.64 (0.94–2.75) | 0.27 | 0.17–0.35 |
| SBP (mmHg) | 109 (100–118) | 109 (100–118) | 110 (100–117) | −0.01 | −0.11–0.09 |
| DBP (mmHg) | 65 (59–71) | 65 (60–71) | 64 (58–71) | 0.07 | −0.03–0.16 |
| Metabolic syndrome | 76 (14.5%) | 47 (16.6%) | 29 (12.0%) | 4.6% | −1.8–11.0% |
| Cluster 1–Cluster 2 | Cluster 1–Cluster 3 | Cluster 2–Cluster 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Cluster 1 | Cluster 2 | Cluster 3 | ES | 95% CI | ES | 95% CI | ES | 95% CI | |
| N | 306 (55.7%) | 178 (32.4%) | 65 (11.8%) | ||||||
| Age (years) | 10.3 (8.3–12.3) | 10.5 (8.8–12.1) | 11.5 (10.1–13.4) | −0.05 | −0.15–0.06 | −0.28 | −0.42–−0.14 | −0.26 | −0.40–−0.10 |
| Sex | |||||||||
| Female | 165 (53.9%) | 106 (59.6%) | 25 (38.5%) | −5.6% | −15.0–3.9% | 15.0% | 1.4–29.0% | 21.0% | 6.2–36.0% |
| Male | 141 (46.1%) | 72 (40.4%) | 40 (61.5%) | 5.6% | −3.9–15.0% | −15.0% | −29.0–−1.4% | −21.0% | −36.0%–−6.2% |
| BMI category | |||||||||
| Normal weight | 86 (28.1%) | 32 (18.0%) | 25 (38.5%) | 10.0% | 2.1–18.0% | −10.0% | −24.0–3.4% | −20.0% | −35.0–−6.3% |
| Overweight | 72 (23.5%) | 44 (24.7%) | 15 (23.1%) | −1.2% | −9.6–7.2% | 0.5% | −11.0–12.0% | 1.6% | −11.0–15.0% |
| Obesity | 148 (48.4%) | 102 (57.3%) | 25 (38.5%) | −8.9% | −19.0–0.7% | 9.9% | −4.1–24.0% | 19.0% | 3.9–34.0% |
| Physical activity | |||||||||
| MVPA adherence | 64 (20.9%) | 23 (13.0%) | 52 (80.0%) | 7.9% | 0.7–15.0% | −59.0% | −71.0–−47.0% | −67.0% | −79.0–−55.0% |
| Full PA adherence | 3 (1.0%) | 1 (0.6%) | 34 (52.3%) | 0.4% | −1.6–2.4% | −51.0% | −64.0–−38.0% | −52.0% | −65.0–−38.0% |
| Moderate PA (min/week) | 180 (60–300) | 120 (0–300) | 240 (120–420) | 0.16 | 0.06–0.27 | −0.20 | −0.34–0.05 | −0.36 | −0.49–−0.21 |
| Vigorous PA (min/week) | 0 (0–0) | 0 (0–0) | 300 (240–360) | −0.03 | −0.13–0.08 | −1.00 | −1.00–−1.00 | −0.99 | −0.99–−0.98 |
| Dietary adherence | |||||||||
| Promoted foods (0–8 scale) | 3.47 (2.84–4.25) | 4.21 (3.95–4.63) | 3.74 (3.32–4.21) | −0.52 | −0.59–−0.44 | −0.16 | −0.31–−0.01 | 0.42 | 0.28–0.55 |
| Avoided foods (0–8 scale) | 6.42 (6.16–6.68) | 7.11 (6.89–7.42) | 6.74 (6.42–7.05) | −0.77 | −0.81–−0.73 | −0.31 | −0.44–−0.16 | 0.45 | 0.31–0.57 |
| Body mass | |||||||||
| Total fat mass (%) | 39.1 (30.0–44.3) | 40.7 (35.7–46.4) | 36.4 (29.4–42.1) | −0.15 | −0.27–−0.02 | 0.14 | −0.03–0.31 | 0.29 | 0.12–0.45 |
| Abdominal fat (%) | 9.0 (8.0–10.1) | 8.7 (7.9–9.8) | 9.3 (8.3–15.8) | 0.06 | −0.09–0.21 | −0.18 | −0.39–0.05 | −0.24 | −0.45–−0.01 |
| Total lean mass (%) | 59.7 (54.0–69.1) | 57.6 (51.4–63.4) | 61.9 (56.6–69.6) | 0.16 | 0.04–0.29 | −0.15 | −0.31–0.03 | −0.31 | −0.46–−0.14 |
| FFMI (kg/m2) | 13.0 (11.9–14.4) | 13.3 (12.5–14.8) | 14.4 (13.4–16.0) | −0.13 | −0.25–0.00 | −0.40 | −0.54–−0.25 | −0.31 | −0.47–−0.13 |
| FMI (kg/m2) | 0.9 (0.6–1.1) | 1.0 (0.8–1.2) | 0.9 (0.6–1.1) | −0.15 | −0.28–−0.03 | 0.03 | −0.14–0.20 | 0.18 | 0.00–0.35 |
| Cardiometabolic Risk Markers | |||||||||
| Triacylglycerols (mg/dL) | 60 (46–83) | 63 (47–90) | 58 (47–74) | −0.05 | −0.16–0.05 | 0.05 | −0.10–0.21 | 0.10 | −0.06–0.26 |
| Cholesterol (mg/dL) | 160 (141–179) | 165 (147–184) | 163 (144–180) | −0.09 | −0.19–0.02 | −0.06 | −0.21–0.10 | 0.03 | −0.13–0.19 |
| HDL−c (mg/dL) | 50 (42–61) | 48 (40–56) | 50 (41–60) | 0.13 | 0.03–0.24 | 0.01 | −0.14–0.17 | −0.13 | −0.29–0.03 |
| LDL−c (mg/dL) | 92 (77–107) | 95 (81–116) | 95 (83–107) | −0.14 | −0.24–−0.03 | −0.07 | −0.22–0.08 | 0.06 | −0.10–0.22 |
| Insulin (mU/L) | 10.1 (5.6–15.5) | 11.6 (6.5–17.3) | 9.8 (6.8–13.9) | −0.06 | −0.17–0.05 | 0.00 | −0.16–0.16 | 0.08 | −0.10–0.24 |
| HOMA−IR | 2.01 (1.12–3.26) | 2.18 (1.23–3.40) | 1.97 (1.24–2.87) | −0.03 | −0.15–0.08 | 0.05 | −0.12–0.21 | 0.09 | −0.08–0.27 |
| SBP (mm Hg) | 108 (100–118) | 109 (101–117) | 110 (100–118) | −0.03 | −0.14–0.08 | −0.07 | −0.23–0.08 | −0.04 | −0.21–0.12 |
| DBP (mm Hg) | 65 (60–71) | 65 (58–71) | 65 (56–70) | 0.01 | −0.10–0.12 | 0.07 | −0.09–0.22 | 0.06 | −0.10–0.23 |
| Metabolic syndrome | 39 (13.5%) | 27 (15.9%) | 10 (15.4%) | −2.4% | −9.6–4.8% | −1.9% | −12.0–8.7% | 0.5% | −10.0–11.0% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gil-Campos, M.; Pérez-Ferreirós, A.; Llorente-Cantarero, F.J.; Anguita-Ruiz, A.; Bedoya-Carpente, J.J.; Kalén, A.; Moreno, L.A.; Bueno, G.; Gil, Á.; Aguilera, C.M.; et al. Association of Diet, Physical Activity Guidelines and Cardiometabolic Risk Markers in Children. Nutrients 2021, 13, 2954. https://doi.org/10.3390/nu13092954
Gil-Campos M, Pérez-Ferreirós A, Llorente-Cantarero FJ, Anguita-Ruiz A, Bedoya-Carpente JJ, Kalén A, Moreno LA, Bueno G, Gil Á, Aguilera CM, et al. Association of Diet, Physical Activity Guidelines and Cardiometabolic Risk Markers in Children. Nutrients. 2021; 13(9):2954. https://doi.org/10.3390/nu13092954
Chicago/Turabian StyleGil-Campos, Mercedes, Alexandra Pérez-Ferreirós, Francisco Jesús Llorente-Cantarero, Augusto Anguita-Ruiz, Juan José Bedoya-Carpente, Anton Kalén, Luis A. Moreno, Gloria Bueno, Ángel Gil, Concepción M. Aguilera, and et al. 2021. "Association of Diet, Physical Activity Guidelines and Cardiometabolic Risk Markers in Children" Nutrients 13, no. 9: 2954. https://doi.org/10.3390/nu13092954
APA StyleGil-Campos, M., Pérez-Ferreirós, A., Llorente-Cantarero, F. J., Anguita-Ruiz, A., Bedoya-Carpente, J. J., Kalén, A., Moreno, L. A., Bueno, G., Gil, Á., Aguilera, C. M., & Leis, R. (2021). Association of Diet, Physical Activity Guidelines and Cardiometabolic Risk Markers in Children. Nutrients, 13(9), 2954. https://doi.org/10.3390/nu13092954










