Association between Metabolic Syndrome Diagnosis and the Physical Activity—Sedentary Profile of Adolescents with Obesity: A Complementary Analysis of the Beta-JUDO Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Anthropometry
2.3. Blood Pressure
2.4. Blood Sampling
2.5. Metabolic Syndrome Diagnosis
2.6. Continuous Cardiometabolic Syndrome Score
2.7. Physical Activity and Sedentary Time
2.8. Statistics
3. Results
3.1. Comparison SED+ vs. SED− Groups
3.2. Comparison MVPA− vs. MVPA+ Groups
3.3. Comparison between SED−/MVPA+, SED−/MVPA−, SED+/MVPA+ and SED+/MVPA− Groups
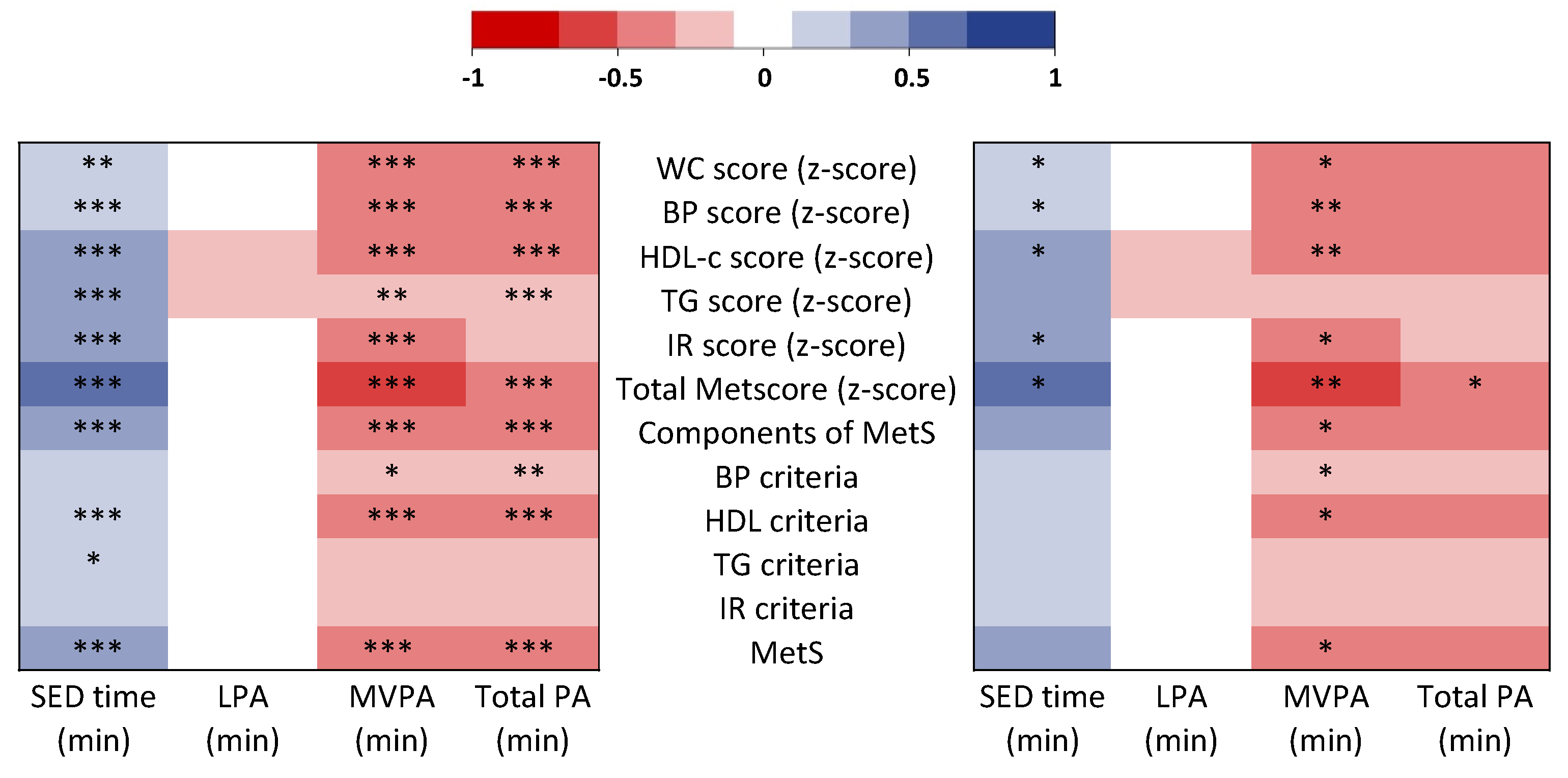
3.4. Correlations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- GBD 2015 Obesity Collaborators; Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef]
- Weihe, P.; Weihrauch-Blüher, S. Metabolic Syndrome in Children and Adolescents: Diagnostic Criteria, Therapeutic Options and Perspectives. Curr. Obes. Rep. 2019, 8, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Laurson, K.R.; Welk, G.J.; Eisenmann, J.C. Diagnostic Performance of BMI Percentiles to Identify Adolescents with Metabolic Syndrome. Pediatrics 2014, 133, e330–e338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Magnussen, C.G.; Cheriyan, S.; Sabin, M.A.; Juonala, M.; Koskinen, J.; Thomson, R.; Skilton, M.R.; Kähönen, M.; Laitinen, T.; Taittonen, L.; et al. Continuous and Dichotomous Metabolic Syndrome Definitions in Youth Predict Adult Type 2 Diabetes and Carotid Artery Intima Media Thickness: The Cardiovascular Risk in Young Finns Study. J. Pediatr. 2016, 171, 97–103.e3. [Google Scholar] [CrossRef]
- Morrison, J.A.; Friedman, L.A.; Gray-McGuire, C. Metabolic Syndrome in Childhood Predicts Adult Cardiovascular Disease 25 Years Later: The Princeton Lipid Research Clinics Follow-up Study. Pediatrics 2007, 120, 340–345. [Google Scholar] [CrossRef] [PubMed]
- DeBoer, M.D. Assessing and Managing the Metabolic Syndrome in Children and Adolescents. Nutrients 2019, 11, 1788. [Google Scholar] [CrossRef] [Green Version]
- Franks, P.W.; Hanson, R.L.; Knowler, W.C.; Sievers, M.L.; Bennett, P.H.; Looker, H.C. Childhood Obesity, Other Cardiovascular Risk Factors, and Premature Death. N. Engl. J. Med. 2010, 362, 485–493. [Google Scholar] [CrossRef] [PubMed]
- De Melo Boff, R.; Liboni RP, A.; de Azevedo Batista, I.P.; de Souza, L.H.; da Silva Oliveira, M. Weight Loss Interventions for Overweight and Obese Adolescents: A Systematic Review. Eat. Weight Disord. 2017, 22, 211–229. [Google Scholar] [CrossRef]
- Albert Pérez, E.; Mateu Olivares, V.; Martínez-Espinosa, R.M.; Molina Vila, M.D.; Reig García-Galbis, M. New Insights about How to Make an Intervention in Children and Adolescents with Metabolic Syndrome: Diet, Exercise vs. Changes in Body Composition. A Systematic Review of RCT. Nutrients 2018, 10, 878. [Google Scholar] [CrossRef] [Green Version]
- Cardel, M.I.; Atkinson, M.A.; Taveras, E.M.; Holm, J.-C.; Kelly, A.S. Obesity Treatment Among Adolescents: A Review of Current Evidence and Future Directions. JAMA Pediatr. 2020, 174, 609–617. [Google Scholar] [CrossRef]
- Kumar, B.; Robinson, R.; Till, S. Physical Activity and Health in Adolescence. Clin. Med. 2015, 15, 267–272. [Google Scholar] [CrossRef] [Green Version]
- Poitras, V.J.; Gray, C.E.; Borghese, M.M.; Carson, V.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.T.; Pate, R.R.; Connor Gorber, S.; Kho, M.E.; et al. Systematic Review of the Relationships between Objectively Measured Physical Activity and Health Indicators in School-Aged Children and Youth. Appl. Physiol. Nutr. Metab. 2016, 41, S197–S239. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical Fitness in Childhood and Adolescence: A Powerful Marker of Health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janssen, I.; Leblanc, A.G. Systematic Review of the Health Benefits of Physical Activity and Fitness in School-Aged Children and Youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marson, E.C.; Delevatti, R.S.; Prado, A.K.G.; Netto, N.; Kruel, L.F.M. Effects of Aerobic, Resistance, and Combined Exercise Training on Insulin Resistance Markers in Overweight or Obese Children and Adolescents: A Systematic Review and Meta-Analysis. Prev. Med. 2016, 93, 211–218. [Google Scholar] [CrossRef]
- Stoner, L.; Rowlands, D.; Morrison, A.; Credeur, D.; Hamlin, M.; Gaffney, K.; Lambrick, D.; Matheson, A. Efficacy of Exercise Intervention for Weight Loss in Overweight and Obese Adolescents: Meta-Analysis and Implications. Sports Med. 2016, 46, 1737–1751. [Google Scholar] [CrossRef] [Green Version]
- Cesa, C.C.; Sbruzzi, G.; Ribeiro, R.A.; Barbiero, S.M.; de Oliveira Petkowicz, R.; Eibel, B.; Machado, N.B.; das Virgens Marques, R.; Tortato, G.; dos Santos, T.J.; et al. Physical Activity and Cardiovascular Risk Factors in Children: Meta-Analysis of Randomized Clinical Trials. Prev. Med. 2014, 69, 54–62. [Google Scholar] [CrossRef]
- Renninger, M.; Hansen, B.H.; Steene-Johannessen, J.; Kriemler, S.; Froberg, K.; Northstone, K.; Sardinha, L.; Anderssen, S.A.; Andersen, L.B.; Ekelund, U.; et al. Associations between Accelerometry Measured Physical Activity and Sedentary Time and the Metabolic Syndrome: A Meta-Analysis of More than 6000 Children and Adolescents. Pediatr. Obes. 2020, 15, e12578. [Google Scholar] [CrossRef] [Green Version]
- Tremblay, M.S.; LeBlanc, A.G.; Kho, M.E.; Saunders, T.J.; Larouche, R.; Colley, R.C.; Goldfield, G.; Connor Gorber, S. Systematic Review of Sedentary Behaviour and Health Indicators in School-Aged Children and Youth. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 98. [Google Scholar] [CrossRef] [Green Version]
- Ekelund, U.; Tarp, J.; Steene-Johannessen, J.; Hansen, B.H.; Jefferis, B.; Fagerland, M.W.; Whincup, P.; Diaz, K.M.; Hooker, S.P.; Chernofsky, A.; et al. Dose-Response Associations between Accelerometry Measured Physical Activity and Sedentary Time and All Cause Mortality: Systematic Review and Harmonised Meta-Analysis. BMJ 2019, 366, l4570. [Google Scholar] [CrossRef] [Green Version]
- Carson, V.; Tremblay, M.S.; Chaput, J.-P.; Chastin, S.F.M. Associations between Sleep Duration, Sedentary Time, Physical Activity, and Health Indicators among Canadian Children and Youth Using Compositional Analyses. Appl. Physiol. Nutr. Metab. 2016, 41, S294–S302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carson, V.; Hunter, S.; Kuzik, N.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Saunders, T.J.; Katzmarzyk, P.T.; Okely, A.D.; Connor Gorber, S.; et al. Systematic Review of Sedentary Behaviour and Health Indicators in School-Aged Children and Youth: An Update. Appl. Physiol. Nutr. Metab. 2016, 41, S240–S265. [Google Scholar] [CrossRef] [PubMed]
- Katzmarzyk, P.T.; Barreira, T.V.; Broyles, S.T.; Champagne, C.M.; Chaput, J.-P.; Fogelholm, M.; Hu, G.; Johnson, W.D.; Kuriyan, R.; Kurpad, A.; et al. Physical Activity, Sedentary Time, and Obesity in an International Sample of Children. Med. Sci. Sports Exerc. 2015, 47, 2062–2069. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Rezende, L.F.M.; Rodrigues Lopes, M.; Rey-López, J.P.; Matsudo, V.K.R.; Luiz, O.D.C. Sedentary Behavior and Health Outcomes: An Overview of Systematic Reviews. PLoS ONE 2014, 9, e105620. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.-P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO Guidelines on Physical Activity and Sedentary Behaviour for Children and Adolescents Aged 5–17 Years: Summary of the Evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef] [PubMed]
- Bowden Davies, K.A.; Sprung, V.S.; Norman, J.A.; Thompson, A.; Mitchell, K.L.; Harrold, J.O.A.; Finlayson, G.; Gibbons, C.; Wilding, J.P.H.; Kemp, G.J.; et al. Physical Activity and Sedentary Time: Association with Metabolic Health and Liver Fat. Med. Sci. Sports Exerc. 2019, 51, 1169–1177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Final Report Summary-BETA-JUDO (Beta-Cell Function in Juvenile Diabetes and Obesity)|FP7|CORDIS|European Commission. Available online: https://cordis.europa.eu/project/id/279153/reporting/de (accessed on 15 December 2021).
- Mörwald, K.; Aigner, E.; Bergsten, P.; Brunner, S.M.; Forslund, A.; Kullberg, J.; Ahlström, H.; Manell, H.; Roomp, K.; Schütz, S.; et al. Serum Ferritin Correlates With Liver Fat in Male Adolescents With Obesity. Front. Endocrinol. 2020, 11, 340. [Google Scholar] [CrossRef]
- Furthner, D.; Weghuber, D.; Dalus, C.; Lukas, A.; Stundner-Ladenhauf, H.N.; Mangge, H.; Pixner, T. Nonalcoholic Fatty Liver Disease in Children with Obesity: Narrative Review and Research Gaps. Horm. Res. Paediatr. 2021, 94, 239–248. [Google Scholar] [CrossRef]
- Koutny, F.; Stein, R.; Kiess, W.; Weghuber, D.; Körner, A. Elevated Transaminases Potentiate the Risk for Emerging Dysglycemia in Children with Overweight and Obesity. Pediatr. Obes. 2021, 16, e12822. [Google Scholar] [CrossRef] [PubMed]
- Koutny, F.; Weghuber, D.; Bollow, E.; Greber-Platzer, S.; Hartmann, K.; Körner, A.; Reinehr, T.; Roebl, M.; Simic-Schleicher, G.; Wabitsch, M.; et al. Prevalence of Prediabetes and Type 2 Diabetes in Children with Obesity and Increased Transaminases in European German-Speaking Countries. Analysis of the APV Initiative. Pediatr. Obes. 2020, 15, e12601. [Google Scholar] [CrossRef] [Green Version]
- Feldman, A.; Aigner, E.; Weghuber, D.; Paulmichl, K. The Potential Role of Iron and Copper in Pediatric Obesity and Nonalcoholic Fatty Liver Disease. Biomed Res. Int. 2015, 2015, 287401. [Google Scholar] [CrossRef] [Green Version]
- Forslund, A.; Staaf, J.; Kullberg, J.; Ciba, I.; Dahlbom, M.; Bergsten, P. Uppsala Longitudinal Study of Childhood Obesity: Protocol Description. Pediatrics 2014, 133, e386–e393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henderson, M.; Rabasa-Lhoret, R.; Bastard, J.-P.; Chiasson, J.-L.; Baillargeon, J.-P.; Hanley, J.A.; Lambert, M. Measuring Insulin Sensitivity in Youth: How Do the Different Indices Compare with the Gold-Standard Method? Diabetes Metab. 2011, 37, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Chen, A.K.; Roberts, C.K.; Barnard, R.J. Effect of a Short-Term Diet and Exercise Intervention on Metabolic Syndrome in Overweight Children. Metabolism 2006, 55, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Julian, V.; Isacco, L.; Khammassi, M.; Fillon, A.; Miguet, M.; Dutheil, F.; Courteix, D.; Zak, M.; Bicki, J.; Głuszek, S.; et al. Appetite Control Might Not Be Improved after Weight Loss in Adolescents with Obesity, Despite Non-Persistent Metabolic Syndrome. Nutrients 2020, 12, 3885. [Google Scholar] [CrossRef] [PubMed]
- Thivel, D.; Malina, R.M.; Isacco, L.; Aucouturier, J.; Meyer, M.; Duché, P. Metabolic Syndrome in Obese Children and Adolescents: Dichotomous or Continuous? Metab. Syndr. Relat. Disord. 2009, 7, 549–555. [Google Scholar] [CrossRef]
- Brage, S.; Wedderkopp, N.; Ekelund, U.; Franks, P.W.; Wareham, N.J.; Andersen, L.B.; Froberg, K. European Youth Heart Study (EYHS) Features of the Metabolic Syndrome Are Associated with Objectively Measured Physical Activity and Fitness in Danish Children: The European Youth Heart Study (EYHS). Diabetes Care 2004, 27, 2141–2148. [Google Scholar] [CrossRef] [Green Version]
- Puyau, M.R.; Adolph, A.L.; Vohra, F.A.; Zakeri, I.; Butte, N.F. Prediction of Activity Energy Expenditure Using Accelerometers in Children. Med. Sci. Sports Exerc. 2004, 36, 1625–1631. [Google Scholar]
- Bendor, C.D.; Bardugo, A.; Pinhas-Hamiel, O.; Afek, A.; Twig, G. Cardiovascular Morbidity, Diabetes and Cancer Risk among Children and Adolescents with Severe Obesity. Cardiovasc. Diabetol. 2020, 19, 79. [Google Scholar] [CrossRef]
- Weiss, R.; Dziura, J.; Burgert, T.S.; Tamborlane, W.V.; Taksali, S.E.; Yeckel, C.W.; Allen, K.; Lopes, M.; Savoye, M.; Morrison, J.; et al. Obesity and the Metabolic Syndrome in Children and Adolescents. N. Engl. J. Med. 2004, 350, 2362–2374. [Google Scholar] [CrossRef] [Green Version]
- Roman-Viñas, B.; Chaput, J.-P.; Katzmarzyk, P.T.; Fogelholm, M.; Lambert, E.V.; Maher, C.; Maia, J.; Olds, T.; Onywera, V.; Sarmiento, O.L.; et al. Proportion of Children Meeting Recommendations for 24-Hour Movement Guidelines and Associations with Adiposity in a 12-Country Study. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Crowe, M.; Sampasa-Kanyinga, H.; Saunders, T.J.; Hamilton, H.A.; Benchimol, E.I.; Chaput, J.-P. Combinations of Physical Activity and Screen Time Recommendations and Their Association with Overweight/Obesity in Adolescents. Can. J. Public Health 2020, 111, 515–522. [Google Scholar] [CrossRef]
- Saunders, T.J.; Gray, C.E.; Poitras, V.J.; Chaput, J.-P.; Janssen, I.; Katzmarzyk, P.T.; Olds, T.; Connor Gorber, S.; Kho, M.E.; Sampson, M.; et al. Combinations of Physical Activity, Sedentary Behaviour and Sleep: Relationships with Health Indicators in School-Aged Children and Youth. Appl. Physiol. Nutr. Metab. 2016, 41, S283–S293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biswas, A.; Oh, P.I.; Faulkner, G.E.; Bajaj, R.R.; Silver, M.A.; Mitchell, M.S.; Alter, D.A. Sedentary Time and Its Association With Risk for Disease Incidence, Mortality, and Hospitalization in Adults. Ann. Intern. Med. 2015, 162, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Fridolfsson, J.; Buck, C.; Hunsberger, M.; Baran, J.; Lauria, F.; Molnar, D.; Moreno, L.A.; Börjesson, M.; Lissner, L.; Arvidsson, D.; et al. High-Intensity Activity Is More Strongly Associated with Metabolic Health in Children Compared to Sedentary Time: A Cross-Sectional Study of the I.Family Cohort. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 90. [Google Scholar] [CrossRef] [PubMed]
- Mann, K.D.; Howe, L.D.; Basterfield, L.; Parkinson, K.N.; Pearce, M.S.; Reilly, J.K.; Adamson, A.J.; Reilly, J.J.; Janssen, X. Longitudinal Study of the Associations between Change in Sedentary Behavior and Change in Adiposity during Childhood and Adolescence: Gateshead Millennium Study. Int. J. Obes. 2017, 41, 1042–1047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwarzfischer, P.; Gruszfeld, D.; Socha, P.; Luque, V.; Closa-Monasterolo, R.; Rousseaux, D.; Moretti, M.; Mariani, B.; Verduci, E.; Koletzko, B.; et al. Longitudinal Analysis of Physical Activity, Sedentary Behaviour and Anthropometric Measures from Ages 6 to 11 Years. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 126. [Google Scholar] [CrossRef]
- Gába, A.; Dygrýn, J.; Štefelová, N.; Rubín, L.; Hron, K.; Jakubec, L. Replacing School and Out-of-School Sedentary Behaviors with Physical Activity and Its Associations with Adiposity in Children and Adolescents: A Compositional Isotemporal Substitution Analysis. Environ. Health Prev. Med. 2021, 26, 16. [Google Scholar] [CrossRef] [PubMed]
- Gába, A.; Pedišić, Ž.; Štefelová, N.; Dygrýn, J.; Hron, K.; Dumuid, D.; Tremblay, M. Sedentary Behavior Patterns and Adiposity in Children: A Study Based on Compositional Data Analysis. BMC Pediatr. 2020, 20, 147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wijndaele, K.; White, T.; Andersen, L.B.; Bugge, A.; Kolle, E.; Northstone, K.; Wedderkopp, N.; Ried-Larsen, M.; Kriemler, S.; Page, A.S.; et al. Substituting Prolonged Sedentary Time and Cardiovascular Risk in Children and Youth: A Meta-Analysis within the International Children’s Accelerometry Database (ICAD). Int. J. Behav. Nutr. Phys. Act. 2019, 16, 96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chastin, S.F.M.; McGregor, D.E.; Biddle, S.J.H.; Cardon, G.; Chaput, J.-P.; Dall, P.M.; Dempsey, P.C.; DiPietro, L.; Ekelund, U.; Katzmarzyk, P.T.; et al. Striking the Right Balance: Evidence to Inform Combined Physical Activity and Sedentary Behavior Recommendations. J. Phys. Act. Health 2021, 18, 631–637. [Google Scholar] [CrossRef]
- Ragland, D.R. Dichotomizing Continuous Outcome Variables: Dependence of the Magnitude of Association and Statistical Power on the Cutpoint. Epidemiology 1992, 3, 434–440. [Google Scholar] [CrossRef]
- Elmesmari, R.; Martin, A.; Reilly, J.J.; Paton, J.Y. Comparison of Accelerometer Measured Levels of Physical Activity and Sedentary Time between Obese and Non-Obese Children and Adolescents: A Systematic Review. BMC Pediatr. 2018, 18, 106. [Google Scholar] [CrossRef] [PubMed]
- Borghese, M.M.; Tremblay, M.S.; LeBlanc, A.G.; Leduc, G.; Boyer, C.; Chaput, J.P. Comparison of ActiGraph GT3X+ and Actical Accelerometer Data in 9–11-Year-Old Canadian Children. J. Sports Sci. 2017, 35, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Migueles, J.H.; Cadenas-Sanchez, C.; Tudor-Locke, C.; Löf, M.; Esteban-Cornejo, I.; Molina-Garcia, P.; Mora-Gonzalez, J.; Rodriguez-Ayllon, M.; Garcia-Marmol, E.; Ekelund, U.; et al. Comparability of Published Cut-Points for the Assessment of Physical Activity: Implications for Data Harmonization. Scand J. Med. Sci. Sports 2019, 29, 566–574. [Google Scholar] [CrossRef]
- Migueles, J.H.; Cadenas-Sanchez, C.; Ekelund, U.; Delisle Nyström, C.; Mora-Gonzalez, J.; Löf, M.; Labayen, I.; Ruiz, J.R.; Ortega, F.B. Accelerometer Data Collection and Processing Criteria to Assess Physical Activity and Other Outcomes: A Systematic Review and Practical Considerations. Sports Med. 2017, 47, 1821–1845. [Google Scholar] [CrossRef] [PubMed]
- Rosenberger, M.E.; Buman, M.P.; Haskell, W.L.; McConnell, M.V.; Carstensen, L.L. Twenty-Four Hours of Sleep, Sedentary Behavior, and Physical Activity with Nine Wearable Devices. Med. Sci. Sports Exerc. 2016, 48, 457–465. [Google Scholar] [CrossRef] [Green Version]

| Anthropometry variables | Mean ± SD |
| Age (year) | 13.4 ± 2.2 |
| Females (n, %) | 65 (48.5) |
| Tanner stage | 3.8 ± 1.3 |
| Height (cm) | 164.1 ± 13.6 |
| Weight (kg) | 93.2 ± 25.1 |
| BMI (kg⋅m−2) | 34.3 ± 5.2 |
| SDS-BMI (z-score) | 3.18 ± 0.48 |
| BMI (percentile) | 98.9 ± 0.7 |
| WC (cm) | 109.0 ± 13.8 |
| Accelerometry variables | Mean ± SD |
| Sedentary time (min⋅day−1) | 640 ± 116 |
| LPA (min⋅day−1) | 484 ± 107 |
| MPA (min⋅day−1) | 186 ± 76 |
| VPA (min⋅day−1) | 6 ± 10 |
| MVPA (min⋅day−1) | 192 ± 81 |
| Total PA (min⋅day−1) | 676 ± 139 |
| Cardiometabolic variables | Mean ± SD |
| Systolic BP (mmHg) | 119 ± 12 |
| Diastolic BP (mmHg) | 72 ± 9 |
| HDL-cholesterol (mmol⋅L−1) | 1.06 ± 0.23 |
| Triglycerides (mmol⋅L−1) | 1.22 ± 0.58 |
| LDL-cholesterol (mmol⋅L−1) | 2.61 ± 0.81 |
| Total cholesterol (mmol⋅L−1) | 3.92 ± 0.90 |
| Fast glucose (mmol⋅L−1) | 5.55 ± 0.59 |
| Fast insulin (mUI⋅L−1) | 24.12 ± 14.2 |
| HOMA-IR | 6.02 ± 3.91 |
| MetS status and components | |
| Components of MetS (mean ± SD) | 2.73 ± 0.86 |
| METS (≥3 criteria) (n, %) | 85 (63) |
| BP criteria (n, %) | 34 (25) |
| HDL criteria (n, %) | 75 (56) |
| TG criteria (n, %) | 41 (31) |
| IR criteria (n, %) | 116 (87) |
| SED− n = 67 | SED+ n = 67 | MVPA+ n = 67 | MVPA− n = 67 | SED−/MVPA+ n = 33 | SED−/MVPA− n = 34 | SED+ /MVPA+ n = 33 | SED+ /MVPA− n = 34 | |
|---|---|---|---|---|---|---|---|---|
| Components of MetS | 2.67 ± 1.10 | 3.29 ± 1.04 *** | 2.62 ± 1.13 | 3.34 ± 0.97 *** | 2.42 ± 1.14 | 2.91 ± 1.02 # | 3.23 ± 0.89 # | 3.36 ± 1.19 ### |
| MetS (≥3 criteria) (n, %) | 33 (49) | 52 (77) ** | 29 (43) | 56 (83) *** | 11 (33) | 22 (65) # | 25 (75) # | 27 (79) # |
| WC score (Z-score) | −0.29 ± 1.05 | 0.29 ± 0.84 * | −0.35 ± 1.04 | 0.35 ± 0.81 ** | −0.68 ± 0.88 | 0.07 ± 1.08 # | 0.24 ± 0.90 # | 0.35 ± 0.79 # |
| BP score (Z-score) | −0.26 ± 0.90 | 0.26 ± 1.03 * | −0.25 ± 0.91 | 0.25 ± 1.01 | −0.41 ± 0.88 | −0.09 ± 0.88 | 0.18 ± 0.89 # | 0.31 ± 0.92 ## |
| HDL score (Z-score) | −0.40 ± 1.00 | 0.40 ± 0.82 ** | −0.34 ± 1.02 | 0.34 ± 0.85 ** | −0.70 ± 1.01 | −0.13 ± 0.91 # | 0.36 ± 0.78 ###,$ | 0.45 ± 0.85 ###,$ |
| TG score (Z-score) | −0.23 ± 0.96 | 0.23 ± 0.99 | −0.27 ± 0.89 | 0.27 ± 1.02 * | −0.24 ± 1.01 | −0.21 ± 0.91 | 0.20 ± 0.93 | 0.25 ± 1.05 |
| IR score (Z-score) | −0.37 ± 0.75 | 0.37 ± 1.08 *** | −0.27 ± 0.95 | 0.27 ± 0.97 ** | −0.46 ± 0.68 | −0.28 ± 0.80 | 0.36 ± 1.20 ##,$ | 0.38 ± 0.96 ###,$ |
| Total MetScore (Z-score) | −0.31 ± 0.57 | 0.31 ± 0.56 *** | −0.30 ± 0.64 | 0.30 ± 0.49 *** | −0.50 ± 0.54 | −0.13 ± 0.55 | 0.27 ± 0.53 ###,$$ | 0.35 ± 0.48 ###,$$ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Julian, V.; Ciba, I.; Olsson, R.; Dahlbom, M.; Furthner, D.; Gomahr, J.; Maruszczak, K.; Morwald, K.; Pixner, T.; Schneider, A.; et al. Association between Metabolic Syndrome Diagnosis and the Physical Activity—Sedentary Profile of Adolescents with Obesity: A Complementary Analysis of the Beta-JUDO Study. Nutrients 2022, 14, 60. https://doi.org/10.3390/nu14010060
Julian V, Ciba I, Olsson R, Dahlbom M, Furthner D, Gomahr J, Maruszczak K, Morwald K, Pixner T, Schneider A, et al. Association between Metabolic Syndrome Diagnosis and the Physical Activity—Sedentary Profile of Adolescents with Obesity: A Complementary Analysis of the Beta-JUDO Study. Nutrients. 2022; 14(1):60. https://doi.org/10.3390/nu14010060
Chicago/Turabian StyleJulian, Valérie, Iris Ciba, Roger Olsson, Marie Dahlbom, Dieter Furthner, Julian Gomahr, Katharina Maruszczak, Katharina Morwald, Thomas Pixner, Anna Schneider, and et al. 2022. "Association between Metabolic Syndrome Diagnosis and the Physical Activity—Sedentary Profile of Adolescents with Obesity: A Complementary Analysis of the Beta-JUDO Study" Nutrients 14, no. 1: 60. https://doi.org/10.3390/nu14010060
APA StyleJulian, V., Ciba, I., Olsson, R., Dahlbom, M., Furthner, D., Gomahr, J., Maruszczak, K., Morwald, K., Pixner, T., Schneider, A., Pereira, B., Duclos, M., Weghuber, D., Thivel, D., Bergsten, P., & Forslund, A. (2022). Association between Metabolic Syndrome Diagnosis and the Physical Activity—Sedentary Profile of Adolescents with Obesity: A Complementary Analysis of the Beta-JUDO Study. Nutrients, 14(1), 60. https://doi.org/10.3390/nu14010060







