Assessing the Influence of Food Insecurity and Retail Environments as a Proxy for Structural Racism on the COVID-19 Pandemic in an Urban Setting
Abstract
:1. Introduction
Socially and Structurally Determined Outcomes: COVID-19, Food Insecurity, and Obesity
2. Materials and Methods
3. Analysis
4. Results
4.1. Regressions
4.1.1. Regression 1: Predicting Food Insecurity
4.1.2. Regression 2: Predicting Death Rates from COVID-19
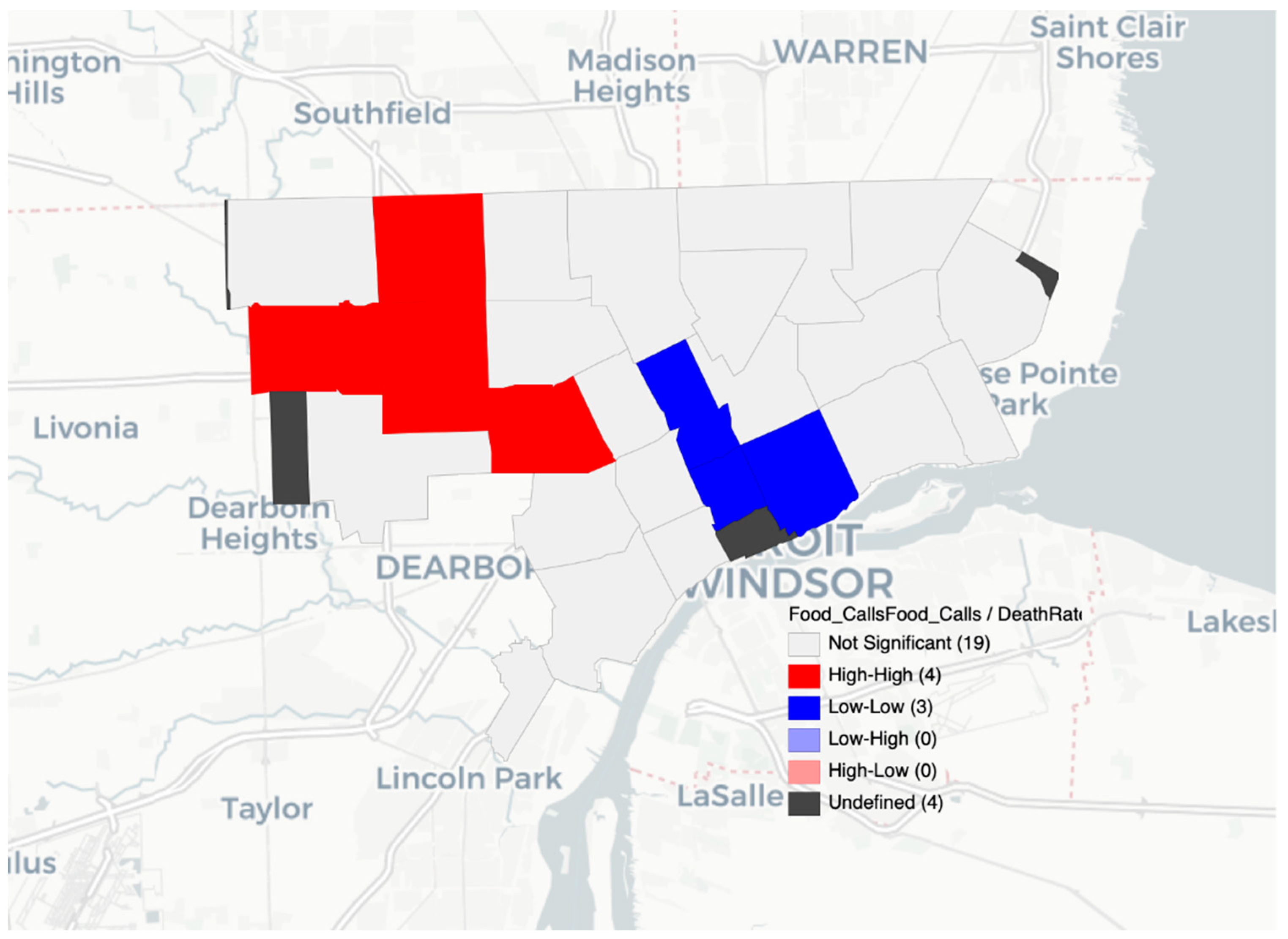
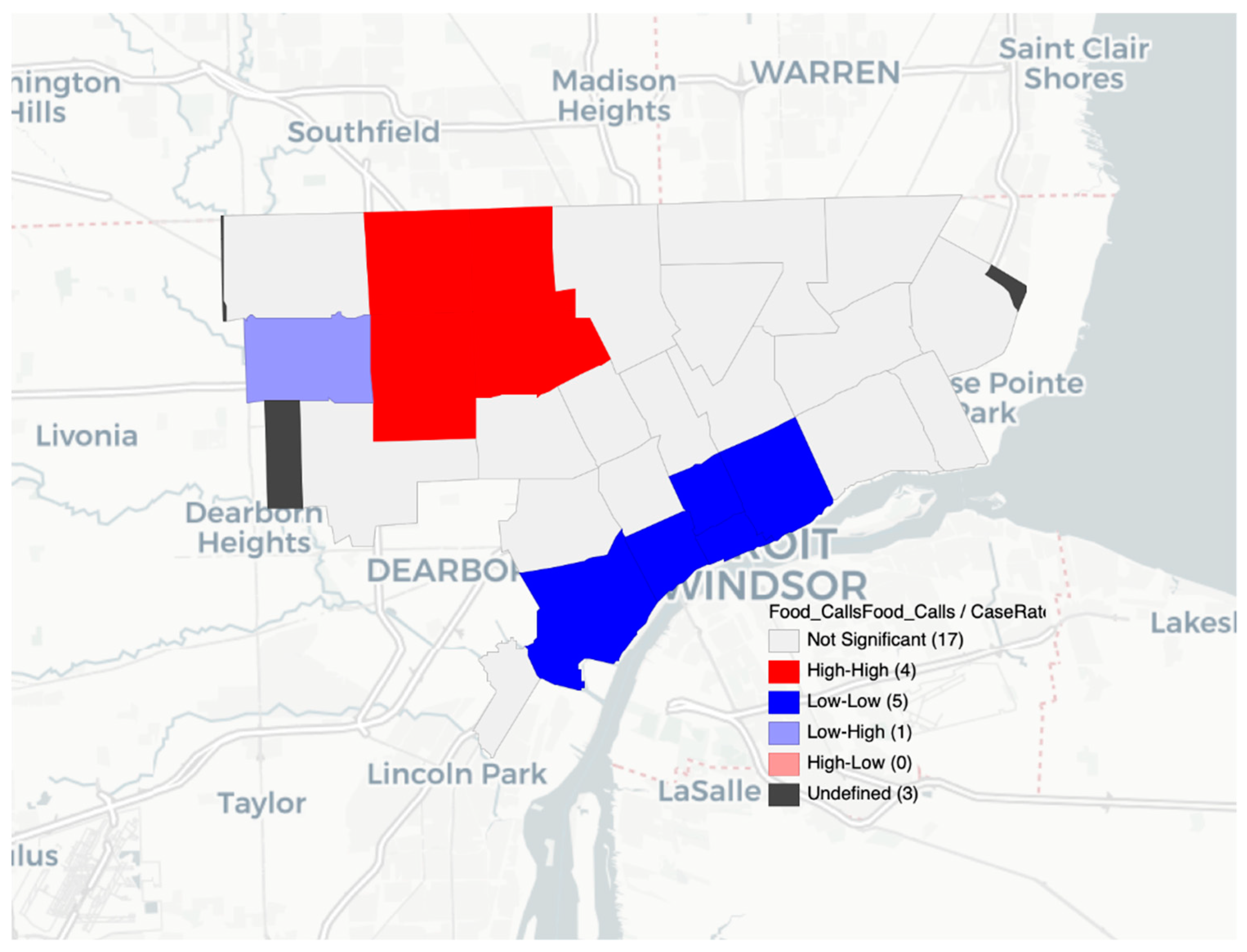
4.1.3. Spatial Analysis: Local Clustering with Empirical Bayes Rates
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. The Global Guardian of Public Health; WHO: Geneva, Switzerland, 2016; p. 12. [Google Scholar]
- Neumark-Sztainer, D.R.; Wall, M.M.; Haines, J.I.; Story, M.T.; Sherwood, N.E.; van den Berg, P.A. Shared Risk and Protective Factors for Overweight and Disordered Eating in Adolescents. Am. J. Prev. Med. 2007, 33, 359–369.e3. [Google Scholar] [CrossRef]
- Braveman, P.A.; Arkin, E.; Proctor, D.; Kauh, T.; Holm, N. Systemic and Structural Racism: Definitions, Examples, Health Damages, and Approaches to Dismantling: Study Examines Definitions, Examples, Health Damages, and Dismantling Systemic and Structural Racism. Health Aff. 2022, 41, 171–178. [Google Scholar] [CrossRef]
- WHO. Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 19 March 2022).
- CDC. COVID Data Tracker. Available online: https://covid.cdc.gov/covid-data-tracker (accessed on 19 March 2022).
- O’Hearn, M.; Liu, J.; Cudhea, F.; Micha, R.; Mozaffarian, D. Coronavirus Disease 2019 Hospitalizations Attributable to Cardiometabolic Conditions in the United States: A Comparative Risk Assessment Analysis. J. Am. Heart Assoc. 2021, 10, e019259. [Google Scholar] [CrossRef]
- Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 19 March 2022).
- Prevalence of Overweight and Obesity Among Adults with Diagnosed Diabetes—United States, 1988–1994 and 1999–2002. JAMA 2005, 293, 546. [CrossRef] [Green Version]
- NHANES—National Health and Nutrition Examination Survey Homepage. Available online: https://www.cdc.gov/nchs/nhanes/index.htm (accessed on 19 March 2022).
- FAO; IFAD; UNICEF; WFP; WHO. Transforming food systems for food security, improved nutrition and affordable healthy diets for all. In The State of Food Security and Nutrition in the World 2021; FAO: Rome, Italy, 2021. [Google Scholar] [CrossRef]
- USDA ERS-IFSA. Available online: https://www.ers.usda.gov/amber-waves/2021/september/food-insecurity-to-increase-in-2021-at-a-higher-rate-in-lower-income-countries/#:~:text=The%20number%20of%20food%20insecure%20people%20in%202021%20is%20estimated,2020%20(see%20figure%20below) (accessed on 19 March 2022).
- Kim, D.-G.; Grieco, E.; Bombelli, A.; Hickman, J.E.; Sanz-Cobena, A. Challenges and Opportunities for Enhancing Food Security and Greenhouse Gas Mitigation in Smallholder Farming in Sub-Saharan Africa. A Review. Food Secur. 2021, 13, 457–476. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Adult Obesity Facts. Centers for Disease Control and Prevention. 30 September 2021. Available online: https://www.cdc.gov/obesity/data/adult.html (accessed on 19 March 2022).
- Hill, L.; Artiga, S. COVID-19 Cases and Deaths by Race/Ethnicity: Current Data and Changes over Time. KFF. 22 February 2022. Available online: https://www.kff.org/coronavirus-covid-19/issue-brief/covid-19-cases-and-deaths-by-race-ethnicity-current-data-and-changes-over-time/#:~:text=These%20age%2Dstandardized%20data%20show,19%20infection%20than%20White%20people (accessed on 19 March 2022).
- Odoms-Young, A.; Bruce, M.A. Examining the Impact of Structural Racism on Food Insecurity: Implications for Addressing Racial/Ethnic Disparities. Fam. Community Health 2018, 41 (Suppl. S2), S3–S6. [Google Scholar] [CrossRef]
- Coleman-Jensen, A.; Rabbitt, M.P.; Gregory, C.A.; Singh, A. Household Food Security in the United States in 2020. Available online: http://www.ers.usda.gov/publications/pub-details/?pubid=102075 (accessed on 14 March 2022).
- Michigan|Feeding America. Available online: https://www.feedingamerica.org/hunger-in-america/michigan (accessed on 14 March 2022).
- Yek, C. Risk Factors for Severe COVID-19 Outcomes Among Persons Aged ≥18 Years Who Completed a Primary COVID-19 Vaccination Series—465 Health Care Facilities, United States, December 2020–October 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 19–25. [Google Scholar] [CrossRef]
- Gayam, V.; Chobufo, M.D.; Merghani, M.A.; Lamichanne, S.; Garlapati, P.R.; Quist, J.; Adler, M.K. Clinical Characteristics and Predictors of Mortality in African Americans with COVID-19 from an Inner-City Community Hospital in New York. SSRN J. 2020, 93, 812–819. [Google Scholar] [CrossRef]
- Choi, S.L.; Men, F. Food Insecurity Associated with Higher COVID-19 Infection in Households with Older Adults. Public Health 2021, 200, 7–14. [Google Scholar] [CrossRef]
- Seligman, B.; Ferranna, M.; Bloom, D.E. Social Determinants of Mortality from COVID-19: A Simulation Study Using NHANES. PLoS Med. 2021, 18, e1003490. [Google Scholar] [CrossRef]
- Coronavirus—Michigan Data. Available online: https://www.michigan.gov/coronavirus/0,9753,7-406-98163_98173---,00.html (accessed on 19 March 2022).
- El Chaar, M.; King, K.; Galvez, L.A. Are Black and Hispanic Persons Disproportionately Affected by COVID-19 Because of Higher Obesity Rates? Surg. Obes. Relat. Dis. 2020, 16, 1096–1099. [Google Scholar] [CrossRef]
- COVID-19 Stats: COVID-19 Incidence, by Age Group—United States, March 1–November 14, 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 69, 1664. [CrossRef]
- Food Security Council (FSC). Food Security Council; Michigan.Gov: Lansing, MI, USA, 2022; p. 24.
- Coronavirus COVID-19. Available online: https://detroitmi.gov/departments/detroit-health-department/programs-and-services/communicable-disease/coronavirus-covid-19 (accessed on 19 March 2022).
- Myers, A. Michigan Primary Care Needs Assessment (PCNA); Policy and Planning Administration, Michigan Department of Health and Human Services: Lansing, MI, USA, 2020; p. 82.
- MDHHS Obesity. Available online: https://www.michigan.gov/mdhhs/0,5885,7-339-71550_63445_82471---,00.html?msclkid=615b4fa9a7bf11ec94a7c3a642465813 (accessed on 19 March 2022).
- Social Determinants of Health—Healthy People 2030|Health.Gov. Available online: https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed on 14 March 2022).
- Health-Related Quality of Life (HRQOL)|CDC. Available online: https://www.cdc.gov/hrqol/index.htm (accessed on 14 March 2022).
- Hill, A.B. Before Redlining and Beyond; Metropolitics: New York, NY, USA, 2021. [Google Scholar]
- Alkon, A.H.; Agyeman, J. (Eds.) Cultivating Food Justice: Race, Class, and Sustainability; Food, health, and the environment; MIT Press: Cambridge, MA, USA, 2011. [Google Scholar]
- Yearby, R.; Clark, B.; Figueroa, J.F. Structural Racism in Historical And Modern US Health Care Policy: Study Examines Structural Racism in Historical and Modern US Health Care Policy. Health Aff. 2022, 41, 187–194. [Google Scholar] [CrossRef]
- Bode, B. Exploring the Implications of School Food Policy Interpretation on Public Health Outcomes of School-Aged Youth. Ph.D. Dissertation, Wayne State University, Detroit, MI, USA, 2022. ProQuest Dissertations Publishing. [Google Scholar]
- Gaynor, T.S.; Wilson, M.E. Social Vulnerability and Equity: The Disproportionate Impact of COVID-19. Public Admin. Rev. 2020, 80, 832–838. [Google Scholar] [CrossRef]
- Russo, R.G.; Li, Y.; Doan, L.N.; Ali, S.H.; Siscovick, D.; Kwon, S.C.; Yi, S.S. COVID-19, Social Determinants of Health, and Opportunities for Preventing Cardiovascular Disease: A Conceptual Framework. JAHA 2021, 10, e022721. [Google Scholar] [CrossRef]
- O’Hara, S.; Toussaint, E.C. Food Access in Crisis: Food Security and COVID-19. Ecol. Econ. 2021, 180, 106859. [Google Scholar] [CrossRef]
- Bell, C.; Kerr, J.; Young, J. Associations between Obesity, Obesogenic Environments, and Structural Racism Vary by County-Level Racial Composition. Int. J. Environ. Res. Public Health 2019, 16, 861. [Google Scholar] [CrossRef] [Green Version]
- Mackey, E.R.; Burton, E.T.; Cadieux, A.; Getzoff, E.; Santos, M.; Ward, W.; Beck, A.R. Addressing Structural Racism Is Critical for Ameliorating the Childhood Obesity Epidemic in Black Youth. Child. Obes. 2022, 18, 75–83. [Google Scholar] [CrossRef]
- Aaron, D.G.; Stanford, F.C. Medicine, Structural Racism, and Systems. Soc. Sci. Med. 2022, 298, 114856. [Google Scholar] [CrossRef]
- Bleich, S.N.; Ard, J.D. COVID-19, Obesity, and Structural Racism: Understanding the Past and Identifying Solutions for the Future. Cell Metab. 2021, 33, 234–241. [Google Scholar] [CrossRef]
- Niles, M.T.; Beavers, A.W.; Clay, L.A.; Dougan, M.M.; Pignotti, G.A.; Rogus, S.; Savoie-Roskos, M.R.; Schattman, R.E.; Zack, R.M.; Acciai, F.; et al. A Multi-Site Analysis of the Prevalence of Food Insecurity in the United States, before and during the COVID-19 Pandemic. Curr. Dev. Nutr. 2021, 5, nzab135. [Google Scholar] [CrossRef] [PubMed]
- Curtis Publishing Company. City Markets: A Study of Thirty-Five Cities, Philadelphia; Curtis Publishing Company—Advertising Department: Philadelphia, PA, USA, 1932. [Google Scholar]
- Story, M.; Kaphingst, K.M.; Robinson-O’Brien, R.; Glanz, K. Creating Healthy Food and Eating Environments: Policy and Environmental Approaches. Annu. Rev. Public Health 2008, 29, 253–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glanz, K.; Sallis, J.F.; Saelens, B.E.; Frank, L.D. Healthy Nutrition Environments: Concepts and Measures. Am. J. Health Promot. 2005, 19, 330–333. [Google Scholar] [CrossRef] [PubMed]
- Herforth, A.; Ahmed, S. The Food Environment, Its Effects on Dietary Consumption, and Potential for Measurement within Agriculture-Nutrition Interventions. Food Secur. 2015, 7, 505–520. [Google Scholar] [CrossRef] [Green Version]
- Morland, K.B.; Evenson, K.R. Obesity Prevalence and the Local Food Environment. Health Place 2009, 15, 491–495. [Google Scholar] [CrossRef] [Green Version]
- Moffat, T.; Mohammed, C.; Newbold, K.B. Cultural Dimensions of Food Insecurity among Immigrants and Refugees. Hum. Organ. 2017, 76, 15–27. [Google Scholar] [CrossRef]
- Lee-Kwan, S.H.; Goedkoop, S.; Yong, R.; Batorsky, B.; Hoffman, V.; Jeffries, J.; Hamouda, M.; Gittelsohn, J. Development and Implementation of the Baltimore Healthy Carry-Outs Feasibility Trial: Process Evaluation Results. BMC Public Health 2013, 13, 638. [Google Scholar] [CrossRef] [Green Version]
- Hartmann-Boyce, J.; Bianchi, F.; Piernas, C.; Riches, S.P.; Frie, K.; Nourse, R.; Jebb, S.A. Grocery Store Interventions to Change Food Purchasing Behaviors: A Systematic Review of Randomized Controlled Trials. Am. J. Clin. Nutr. 2018, 107, 1004–1016. [Google Scholar] [CrossRef]
- Ayala, G.X.; Baquero, B.; Pickrel, J.L.; Mayer, J.; Belch, G.; Rock, C.L.; Linnan, L.; Gittelsohn, J.; Sanchez-Flack, J.; Elder, J.P. A Store-Based Intervention to Increase Fruit and Vegetable Consumption: The El Valor de Nuestra Salud Cluster Randomized Controlled Trial. Contemp. Clin. Trials 2015, 42, 228–238. [Google Scholar] [CrossRef] [Green Version]
- Valdivia Espino, J.N.; Guerrero, N.; Rhoads, N.; Simon, N.-J.; Escaron, A.L.; Meinen, A.; Nieto, F.J.; Martinez-Donate, A.P. Community-Based Restaurant Interventions to Promote Healthy Eating: A Systematic Review. Prev. Chronic Dis. 2015, 12, 140455. [Google Scholar] [CrossRef] [Green Version]
- Campbell, N.; Duhaney, T.; Arango, M.; Ashley, L.A.; Bacon, S.L.; Gelfer, M.; Kaczorowski, J.; Mang, E.; Morris, D.; Nagpal, S.; et al. Healthy Food Procurement Policy: An Important Intervention to Aid the Reduction in Chronic Noncommunicable Diseases. Can. J. Cardiol. 2014, 30, 1456–1459. [Google Scholar] [CrossRef] [PubMed]
- Oropeza, S.; Sadile, M.G.; Phung, C.N.; Cabiles, M.; Spackman, S.; Abuan, M.; Seligman, F.; Araneta, M.R. STRIVE, San Diego! Methodology of a Community-Based Participatory Intervention to Enhance Healthy Dining at Asian and Pacific Islander Restaurants. J. Nutr. Educ. Behav. 2018, 50, 297–306.e1. [Google Scholar] [CrossRef] [PubMed]
- Gittelsohn, J.; Kim, E.M.; He, S.; Pardilla, M. A Food Store–Based Environmental Intervention Is Associated with Reduced BMI and Improved Psychosocial Factors and Food-Related Behaviors on the Navajo Nation. J. Nutr. 2013, 143, 1494–1500. [Google Scholar] [CrossRef] [PubMed]
- Drewnowski, A.; Aggarwal, A.; Hurvitz, P.M.; Monsivais, P.; Moudon, A.V. Obesity and Supermarket Access: Proximity or Price? Am. J. Public Health 2012, 102, e74–e80. [Google Scholar] [CrossRef] [PubMed]
- Detroit Food Map. Available online: https://detroitfoodmap.com/?og=1 (accessed on 19 March 2022).
- Hill, A. “Treat Everybody Right”: Examining Foodways to Improve Food Access. J. Agric. Food Syst. Community Dev. 2021, 10, 9–16. [Google Scholar] [CrossRef]
- Detroit Great Grocer Project—Detroit Food Policy Council. Available online: https://www.detroitfoodpc.org/committees/#dgc (accessed on 19 March 2022).
- Hill, A.B. Detroit Food Metrics Report 2019; Detroit Food Policy Council: Detroit, MI, USA, 2020. [Google Scholar]
- Bethell, C.; Simpson, L.; Stumbo, S.; Carle, A.C.; Gombojav, N. National, State, and Local Disparities in Childhood Obesity. Health Aff. 2010, 29, 347–356. [Google Scholar] [CrossRef]
- O’Brien, R.; Neman, T.; Seltzer, N.; Evans, L.; Venkataramani, A. Structural racism, economic opportunity and racial health disparities: Evidence from U.S. counties. SSM-Popul. Health 2020, 11, 100564. [Google Scholar] [CrossRef]
- Brown, T.; Homan, P. Structural Racism and Health Stratification in the U.S.: Connecting Theory to Measurement. SOCArXiv Pap. 2022. [Google Scholar] [CrossRef]
- Shaver, E.R.; Sadler, R.C.; Hill, A.B.; Bell, K.; Ray, M.; Choy-Shin, J.; Lerner, J.; Soldner, T.; Jones, A.D. The Flint Food Store Survey: Combining Spatial Analysis with a Modified Nutrition Environment Measures Survey in Stores (NEMS-S) to Measure the Community and Consumer Nutrition Environments. Public Health Nutr. 2018, 21, 1474–1485. [Google Scholar] [CrossRef] [Green Version]
- Glanz, K.; Sallis, J.F.; Saelens, B.E.; Frank, L.D. Nutrition Environment Measures Survey in Stores (NEMS-S) Development and Evaluation. Am. J. Prev. Med. 2007, 32, 282–289. [Google Scholar] [CrossRef]
- United Way for Southeastern Michigan. 2-1-1 Data Dashboard. Available online: https://app.powerbi.com/view?r=eyJrIjoiODRiYjJiZDAtZGUwMS00YTY1LTg1MWUtNWNhNzEwZTkzOGM0IiwidCI6ImIxNTJkZTI1LTYxZDMtNDlhMi1hMmY4LTczMWQ2ZTgxNDAyOSIsImMiOjN9&pageName=ReportSectiona99dfe17b930ed9503d2 (accessed on 19 March 2022).
- U.S. ZIP Codes: Free Zip Code Map and ZIP Code Lookup. United States Zip Codes. 2018. Available online: https://www.unitedstateszipcodes.org/ (accessed on 6 April 2022).
- Leech, N.L.; Gliner, J.A.; Morgan, G.A.; Harmon, R.J. Use and Interpretation of Multiple Regression. J. Am. Acad. Child Adolesc. Psychiatry 2003, 42, 738–740. [Google Scholar] [CrossRef] [PubMed]
- Anselin, L. Local Indicators of Spatial Association-LISA. Geogr. Anal. 2010, 27, 93–115. [Google Scholar] [CrossRef]
- Ord, J.K.; Getis, A. Local Spatial Autocorrelation Statistics: Distributional Issues and an Application. Geogr. Anal. 2010, 27, 286–306. [Google Scholar] [CrossRef]
- GeoDa: An Introduction to Spatial Data Analysis|Spatial@UChicago|The University of Chicago. Available online: https://spatial.uchicago.edu/geoda (accessed on 19 March 2022).
- Sallis, J.F.; Glanz, K. Physical Activity and Food Environments: Solutions to the Obesity Epidemic. Milbank Q. 2009, 87, 123–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berge, J.M.; Wall, M.; Larson, N.; Forsyth, A.; Bauer, K.W.; Neumark-Sztainer, D. Youth Dietary Intake and Weight Status: Healthful Neighborhood Food Environments Enhance the Protective Role of Supportive Family Home Environments. Health Place 2014, 26, 69–77. [Google Scholar] [CrossRef] [Green Version]
- Burke, M.P.; Jones, S.J.; Frongillo, E.A.; Fram, M.S.; Blake, C.E.; Freedman, D.A. Severity of household food insecurity and lifetime racial discrimination among African-American households in South Carolina. Ethn. Health 2016, 23, 276–292. [Google Scholar] [CrossRef]
- The Digital Scholarship Lab; The National Community Reinvestment Coalition. Not Even Past: Social Vulnerability and the Legacy of Redlining; American Panorama; Nelson, R.K., Ayers, E.L., Eds.; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2021; Available online: https://dsl.richmond.edu/socialvulnerability (accessed on 28 February 2022).
- Bowen, S.; Elliott, S.; Hardison-Moody, A. The structural roots of food insecurity: How racism is a fundamental cause of food insecurity. Sociol. Compass 2021, 15, e12846. [Google Scholar] [CrossRef]
- Pryor, S.; Dietz, W. The COVID-19, Obesity, and Food Insecurity Syndemic. Curr. Obes. Rep. 2022. [Google Scholar] [CrossRef]
- Tipton, E.; Hallberg, K.; Hedges, L.V.; Chan, W. Implications of Small Samples for Generalization: Adjustments and Rules of Thumb. Eval. Rev. 2017, 41, 472–505. [Google Scholar] [CrossRef] [Green Version]

| ZIP Code | Race (%Black/African American; %White) [67] | Quality (Range 0–6) | Availability (Range 0–27) | Price (Range −8–16) | Total (Range −8–49) |
|---|---|---|---|---|---|
| 48201 | 70%; 20% | 6.00 | 22.00 | 0.00 | 28.00 |
| 48202 | 82%; 12% | 6.00 | 23.00 | −2.00 | 27.00 |
| 48203 | 92%; 5% | 6.00 | 27.00 | −3.00 | 30.00 |
| 48204 | 97%; 1% | 6.00 | 23.00 | −2.00 | 27.00 |
| 48205 | 92%; 5% | 5.00 | 19.33 | 1.00 | 25.33 |
| 48206 | 95%; 2% | 6.00 | 19.00 | 4.50 | 29.50 |
| 48207 | 89%; 7% | 5.14 | 22.29 | 3.00 | 30.00 |
| 48209 | 10%; 50% | 5.25 | 17.00 | 3.25 | 25.50 |
| 48210 | 28%; 42% | 6.00 | 16.50 | 3.50 | 26.00 |
| 48212 | 37%; 37% | 6.00 | 18.00 | 1.00 | 25.00 |
| 48213 | 96%; 2% | 6.00 | 25.00 | 3.00 | 34.00 |
| 48214 | 91%; 6% | 6.00 | 26.00 | 2.50 | 34.50 |
| 48215 | 92%; 5% | 4.50 | 22.00 | 2.00 | 28.50 |
| 48216 | 42%; 38% | 6.00 | 18.00 | −3.00 | 21.00 |
| 48219 | 91%; 7% | 3.75 | 22.25 | 0.50 | 26.50 |
| 48221 | 93%; 4% | 5.00 | 23.00 | 0.67 | 28.67 |
| 48223 | 89%; 8% | 6.00 | 0.00 | 0.00 | 6.00 |
| 48224 | 90%; 8% | 6.00 | 17.50 | 3.00 | 26.50 |
| 48227 | 96%; 2% | 4.50 | 20.17 | 2.00 | 26.67 |
| 48228 | 79%; 17% | 6.00 | 19.20 | 2.75 | 27.00 |
| 48234 | 94%; 4% | 6.00 | 17.33 | 0.00 | 23.30 |
| 48235 | 97%; 1% | 4.50 | 9.50 | 3.00 | 17.00 |
| 48238 | 97%; 1% | 4.00 | 10.00 | 0.33 | 14.33 |
| Regression | B | 95% CI | β | p |
|---|---|---|---|---|
| Analysis 1 | ||||
| Constant | 136.97 | −178.49, 452.40 | - | 0.37 |
| Case Counts | 0.047 | 0.008, 0.086 | 0.47 | 0.02 |
| Death Counts | 1.89 | 0.34, 3.43 | 0.47 | 0.02 |
| NEMS | −0.36 | −10.77, 10.06 | −0.008 | 0.94 |
| Analysis 2 | ||||
| Constant | 218.74 | −159.85, 597.33 | - | 0.24 |
| Case Rates | −0.002 | −0.02, 0.02 | −0.06 | 0.83 |
| NEMS | 3.05 | −5.35, 11.44 | 0.17 | 0.45 |
| Calls to 2-1-1 | 0.19 | −0.03, 0.40 | 0.45 | 0.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dombrowski, R.D.; Hill, A.B.; Bode, B.; Knoff, K.A.G.; Dastgerdizad, H.; Kulik, N.; Mallare, J.; Blount-Dorn, K.; Bynum, W. Assessing the Influence of Food Insecurity and Retail Environments as a Proxy for Structural Racism on the COVID-19 Pandemic in an Urban Setting. Nutrients 2022, 14, 2130. https://doi.org/10.3390/nu14102130
Dombrowski RD, Hill AB, Bode B, Knoff KAG, Dastgerdizad H, Kulik N, Mallare J, Blount-Dorn K, Bynum W. Assessing the Influence of Food Insecurity and Retail Environments as a Proxy for Structural Racism on the COVID-19 Pandemic in an Urban Setting. Nutrients. 2022; 14(10):2130. https://doi.org/10.3390/nu14102130
Chicago/Turabian StyleDombrowski, Rachael D., Alex B. Hill, Bree Bode, Kathryn A. G. Knoff, Hadis Dastgerdizad, Noel Kulik, James Mallare, Kibibi Blount-Dorn, and Winona Bynum. 2022. "Assessing the Influence of Food Insecurity and Retail Environments as a Proxy for Structural Racism on the COVID-19 Pandemic in an Urban Setting" Nutrients 14, no. 10: 2130. https://doi.org/10.3390/nu14102130
APA StyleDombrowski, R. D., Hill, A. B., Bode, B., Knoff, K. A. G., Dastgerdizad, H., Kulik, N., Mallare, J., Blount-Dorn, K., & Bynum, W. (2022). Assessing the Influence of Food Insecurity and Retail Environments as a Proxy for Structural Racism on the COVID-19 Pandemic in an Urban Setting. Nutrients, 14(10), 2130. https://doi.org/10.3390/nu14102130






