In-Hospital Patient Education Markedly Reduces Alcohol Consumption after Alcohol-Induced Acute Pancreatitis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting and Study Design
2.2. Patients
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. Intervention
2.4. Investigated Parameters
2.5. Outcome Parameters
2.6. Analysis
2.6.1. Subgroups
2.6.2. Statistical Analysis
2.7. Ethical Approval
3. Results
3.1. Basic Characteristics and Data Quality
3.2. Acute Pancreatitis Is Often Followed by Another Episode
3.3. Frequent Alcohol Drinkers Have Higher GGT Level
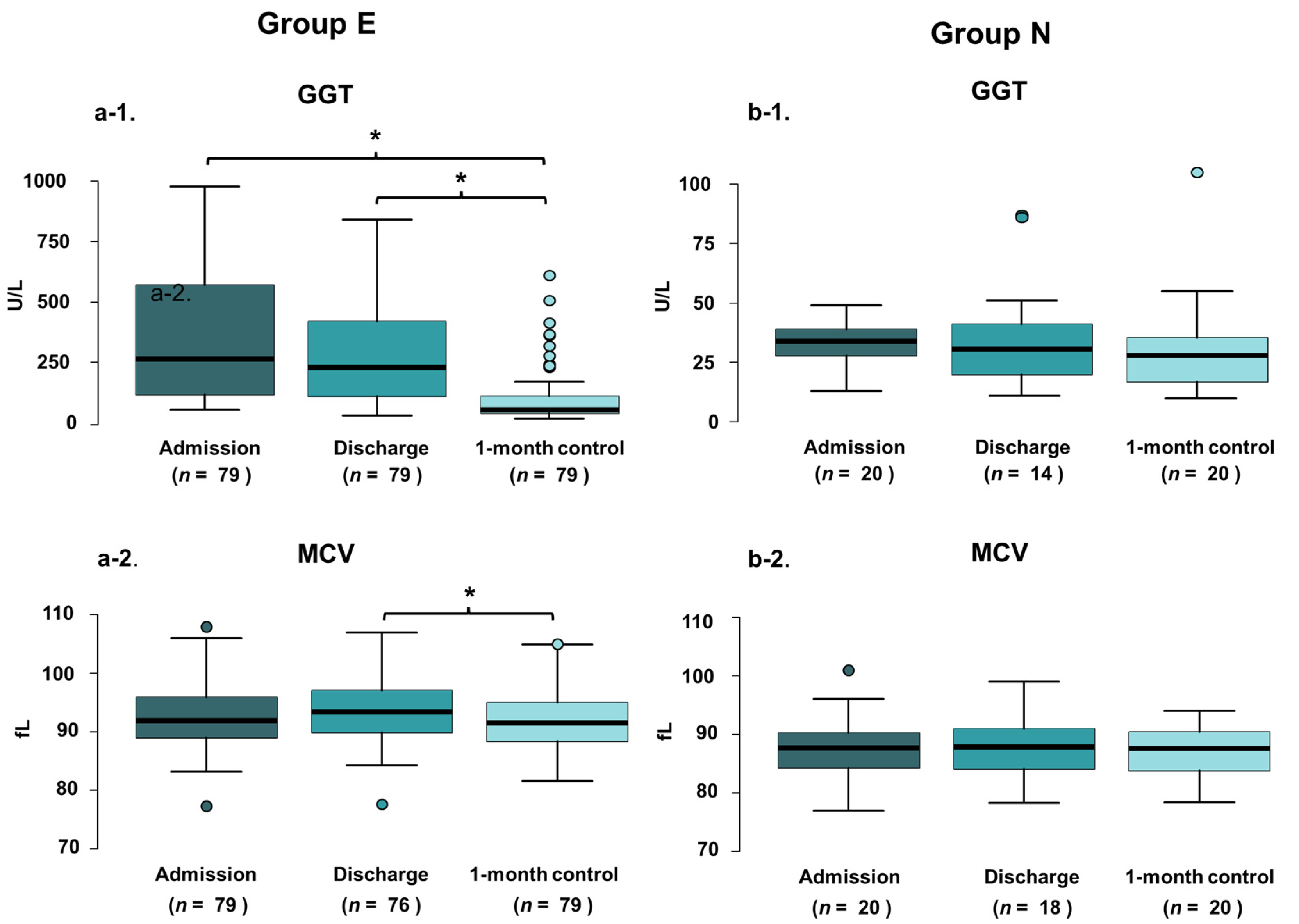
3.4. Significant Decrease Is Detected in GGT Value 1-Month Following In-Hospital Patient Education
3.5. MCV Value Showed Significant Reduction 1-Month Following In-Hospital Patient Education
3.6. 75–80% of the Patients Kept Abstinence 1-Month Following In-Hospital Patient Education
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Patients
4.3. Implications for Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peery, A.F.; Crockett, S.D.; Murphy, C.C.; Lund, J.L.; Dellon, E.S.; Williams, J.L.; Jensen, E.T.; Shaheen, N.J.; Barritt, A.S.; Lieber, S.R.; et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the united states: Update 2018. Gastroenterology 2019, 156, 254–272.e11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sekimoto, M.; Takada, T.; Kawarada, Y.; Hirata, K.; Mayumi, T.; Yoshida, M.; Hirota, M.; Kimura, Y.; Takeda, K.; Isaji, S.; et al. JPN Guidelines for the management of acute pancreatitis: Epidemiology, etiology, natural history, and outcome predictors in acute pancreatitis. J. Hepato-Biliary-Pancreat. Surg. 2006, 13, 10–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Párniczky, A.; Kui, B.; Szentesi, A.; Balázs, A.; Szűcs, Á.; Mosztbacher, D.; Czimmer, J.; Sarlós, P.; Bajor, J.; Gódi, S.; et al. Prospective, multicentre, nationwide clinical data from 600 cases of acute pancreatitis. PLoS ONE 2016, 11, e0165309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gullo, L.; Migliori, M.; Pezzilli, R.; Oláh, A.; Farkas, G.; Levy, P.; Arvanitakis, C.; Lankisch, P.; Beger, H. An update on recurrent acute pancreatitis: Data from five European countries. Am. J. Gastroenterol. 2002, 97, 1959–1962. [Google Scholar] [CrossRef]
- Gislason, H.; Horn, A.; Hoem, D.; Andrén-Sandberg, Å.; Imsland, A.K.; Søreide, O.; Viste, A. Acute pancreatitis in Bergen, Norway. A study on incidence, etiology and severity. Scand. J. Surg. 2004, 93, 29–33. [Google Scholar] [CrossRef] [Green Version]
- Bougard, M.; Barbier, L.; Godart, B.; Le Bayon-Bréard, A.-G.; Marques, F.; Salamé, E. Management of biliary acute pancreatitis. J. Visc. Surg. 2018, 156, 113–125. [Google Scholar] [CrossRef]
- Garg, R.; Rustagi, T. Management of hypertriglyceridemia induced acute pancreatitis. BioMed Res. Int. 2018, 2018, 4721357. [Google Scholar] [CrossRef] [Green Version]
- Ghazale, A.; Chari, S.T. Optimising corticosteroid treatment for autoimmune pancreatitis. Gut 2007, 56, 1650–1652. [Google Scholar] [CrossRef] [Green Version]
- Appelros, S.; Borgström, A. Incidence, aetiology and mortality rate of acute pancreatitis over 10 years in a defined urban population in Sweden. Br. J. Surg. 1999, 86, 465–470. [Google Scholar] [CrossRef]
- Hegyi, P.J.; Soós, A.; Tóth, E.; Ébert, A.; Venglovecz, V.; Márta, K.; Mátrai, P.; Mikó, A.; Bajor, J.; Sarlós, P.; et al. Evidence for diagnosis of early chronic pancreatitis after three episodes of acute pancreatitis: A cross-sectional multicentre international study with experimental animal model. Sci. Rep. 2021, 11, 1367. [Google Scholar] [CrossRef]
- Ocskay, K.; Juhász, M.F.; Farkas, N.; Zádori, N.; Szakó, L.; Szakács, Z.; Szentesi, A.; Erőss, B.; Miklós, E.; Zemplényi, A.; et al. Recurrent acute pancreatitis prevention by the elimination of alcohol and cigarette smoking (REAPPEAR): Protocol of a randomised controlled trial and a cohort study. BMJ Open 2022, 12, e050821. [Google Scholar] [CrossRef] [PubMed]
- Szentesi, A.; Farkas, N.; Sipos, Z.; Mátrai, P.; Vincze, Á.; Izbéki, F.; Párniczky, A.; Hegyi, P. Alcohol consumption and smoking dose-dependently and synergistically worsen local pancreas damage. Gut 2022. [Google Scholar] [CrossRef] [PubMed]
- Clemens, D.L.; Mahan, K.J. Alcoholic pancreatitis: Lessons from the liver. World J. Gastroenterol. 2010, 16, 20–26. [Google Scholar] [CrossRef] [PubMed]
- NIH. Drinking Levels Defined. Available online: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking (accessed on 22 February 2022).
- Westman, J.; Wahlbeck, K.; Laursen, T.M.; Gissler, M.; Nordentoft, M.; Hällgren, J.; Arffman, M.; Osby, U. Mortality and life expectancy of people with alcohol use disorder in Denmark, Finland and Sweden. Acta Psychiatr. Scand. 2014, 131, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Razvodovsky, Y.E. Alcohol consumption and pancreatitis mortality in Russia. JOP J. Pancreas 2014, 15, 280–412. [Google Scholar]
- Jyani, G.; Prinja, S.; Ambekar, A.; Bahuguna, P.; Kumar, R. Health impact and economic burden of alcohol consumption in India. Int. J. Drug Policy 2019, 69, 34–42. [Google Scholar] [CrossRef]
- Rehm, J.; Shield, K.; Rehm, M.; Gmel, G.; Frick, U. Alcohol Consumption, Alcohol Dependence, and Attributable Burden of Disease in Europe: Potential Gains from Effective Interventions for Alcohol Dependence; CAMH: Toronto, ON, Canada, 2012. [Google Scholar]
- Crowley, P. Long-term drug treatment of patients with alcohol dependence. Aust. Prescr. 2015, 38, 41–43. [Google Scholar] [CrossRef] [Green Version]
- Jhanjee, S. Evidence based psychosocial interventions in substance use. Indian J. Psychol. Med. 2014, 36, 112–118. [Google Scholar] [CrossRef] [Green Version]
- Nordback, I.; Pelli, H.; Lappalainen–Lehto, R.; Järvinen, S.; Räty, S.; Sand, J. The recurrence of acute alcohol-associated pancreatitis can be reduced: A randomized controlled trial. Gastroenterology 2009, 136, 848–855. [Google Scholar] [CrossRef]
- Kaner, E.F.; Dickinson, H.O.; Beyer, F.R.; Campbell, F.; Schlesinger, C.; Heather, N.; Saunders, J.B.; Burnand, B.; Pienaar, E.D. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst. Rev. 2018, 2, CD004148. [Google Scholar] [CrossRef] [Green Version]
- Platt, L.; Melendez-Torres, G.J.; O’Donnell, A.; Bradley, J.; Newbury-Birch, D.; Kaner, E.; Ashton, C. How effective are brief interventions in reducing alcohol consumption: Do the setting, practitioner group and content matter? Findings from a systematic review and metaregression analysis. BMJ Open 2016, 6, e011473. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saunders, J.B.; Whitfield, J.B.; Conigrave, K.M. Diagnostic tests for alcohol consumption. Alcohol Alcohol. 1995, 30, 13–26. [Google Scholar] [CrossRef]
- Mundle, G.; Ackermann, K.; Munkes, J.; Steinle, D.; Mann, K. Influence of age, alcohol consumption and abstinence on the sensitivity of carbohydrate-deficient transferrin, gamma-glutamyltransferase and mean corpuscular volume. Alcohol Alcohol. 1999, 34, 760–766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Besselink, M.; van Santvoort, H.; Freeman, M.; Gardner, T.; Mayerle, J.; Vege, S.S.; Werner, J.; Banks, P.; McKay, C.; Fernandez-del Castillo, C.; et al. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 2013, 13 (Suppl. 2), e1–e15. [Google Scholar]
- Mattoo, S.K.; Prasad, S.; Ghosh, A. Brief intervention in substance use disorders. Indian J. Psychiatry 2018, 60, S466–S472. [Google Scholar] [CrossRef]
- Pelli, H.; Sand, J.; Laippala, P.; Nordback, I. Long-term follow-up after the first episode of acute alcoholic pancreatitis: Time course and risk factors for recurrence. Scand. J. Gastroenterol. 2000, 35, 552–555. [Google Scholar]
- Ali, U.A.; Issa, Y.; Hagenaars, J.C.; Bakker, O.J.; van Goor, H.; Nieuwenhuijs, V.B.; Bollen, T.L.; van Ramshorst, B.; Witteman, B.J.; Brink, M.A.; et al. Risk of recurrent pancreatitis and progression to chronic pancreatitis after a first episode of acute pancreatitis. Clin. Gastroenterol. Hepatol. 2016, 14, 738–746. [Google Scholar]
- Pelli, H.; Lappalainen-Lehto, R.; Piironen, A.; Sand, J.; Nordback, I. Risk factors for recurrent acute alcohol-associated pancreatitis: A prospective analysis. Scand. J. Gastroenterol. 2008, 43, 614–621. [Google Scholar] [CrossRef]
- Orrego, H.; Blake, J.E.; Israel, Y. Relationship between gamma-glutamyl transpeptidase and mean urinary alcohol levels in alcoholics while drinking and after alcohol withdrawal. Alcohol. Clin. Exp. Res. 1985, 9, 10–13. [Google Scholar] [CrossRef]

| Unit | Overall | Elevated Admission GGT | Non-Elevated Admission GGT | |
|---|---|---|---|---|
| Patients | n | 99 | 79 | 20 |
| Epidemiology | ||||
| Gender | ||||
| Male | n (%) | 88 (89) | 68 (86) | 20 (100) |
| Female | n (%) | 11 (11) | 11 (14) | 0 |
| Age (year) | Mean ± SD | 50.05 ± 11.37 | 48.84 ± 11.21 | 54.85 ± 10.96 |
| Median (IQR) | 50 (44–57) | 50 (41–56) | 54 (49–59) | |
| Outcomes | ||||
| Length of hospitalization (days) | Mean ± SD | 9.94 ± 10.53 | 9.56 ± 9.65 | 11.45 ± 13.66 |
| Median (IQR) | 6 (5–9) | 6 (5–9) | 7 (4–10) | |
| Severity | ||||
| Mild | n (%) | 61 (62) | 50 (63) | 11 (55) |
| Moderate | n (%) | 28 (28) | 21 (27) | 7 (35) |
| Severe | n (%) | 8 (8) | 6 (8) | 2 (10) |
| Medical history | ||||
| Previous acute pancreatitis | n (%) | 40 (40) | 31 (39) | 9 (45) |
| Chronic pancreatitis | n (%) | 14 (14) | 9 (11) | 5 (25) |
| Hypertriglyceridemia | n (%) | 17 (17) | 15 (20) | 2 (10) |
| Alcohol consumption (frequency) | ||||
| None | n (%) | 6 (6) | 5 (6) | 1 (5) |
| Occasionally | n (%) | 24 (24) | 14 (18) | 10 (50) |
| Monthly | n (%) | 2 (2) | 2 (3) | 0 (0) |
| Weekly | n (%) | 13 (13) | 9 (11) | 4 (20) |
| Daily | n (%) | 54 (54) | 49 (62) | 5 (25) |
| Alcohol consumption (gram/occasion) | Mean ± SD | 81.06 ± 65.26 | 84.43 ± 69.25 | 67.55 ± 44.88 |
| Laboratory parameters | ||||
| Admission GGT (U/L) | Mean ± SD | 364.57 ± 471.14 | 448.58 ± 493.43 | 32.7 ± 10.34 |
| Median (IQR) | 166 (64–493) | 263 (115.5–571) | 34 (28.5–39) | |
| Discharge GGT (U/L) | Mean ± SD | 255.28 ± 248.88 | 294 ± 250.75 | 36.79 ± 23.78 |
| Median (IQR) | 194 (70–399) | 229 (108–419) | 30.50 (21.25–40.25) | |
| 1-month GGT (U/L) | Mean ± SD | 88.55 ± 105.80 | 103.2 ± 113.5 | 30.65 ± 20.90 |
| Median (IQR) | 91 (87.3–94) | 53 (41–108) | 28 (18–35.25) | |
| Admission MCV (fL) | Mean ± SD | 91.45 ± 6.04 | 92.51 ± 5.69 | 97.29 ± 5.70 |
| Median (IQR) | 166 (87.8–94.65) | 92 (89–95.90) | 35 (28.5–39) | |
| Discharge MCV (fL) | Mean ± SD | 92.58 ± 5.79 | 93.73 ± 5.3 | 97.74 ± 5.34 |
| Median (IQR) | 92.5 (88.93–96.25) | 93.4 (89.95–97.03) | 87.85 (84.25–90.95) | |
| 1-month MCV (fL) | Mean ± SD | 91.02 ± 5.34 | 92.07 ± 5.10 | 86.9 ± 4.22 |
| Median (IQR) | 90.9 (87.3–94) | 91.5 (88.35–95) | 87.6 (83.92–90.33) | |
| 1-month GGT change (U/L) | Mean ± SD | 152.67 ± 195.94 | 190 ± 202.16 | 2.05 ± 17.69 |
| 1-month GGT change (U/L; %) | Mean ± SD | 40.92 ± 71.13 | 49.25 ± 74.50 | 8.04 ± 43.42 |
| 1-month MCV change (fL) | Mean ± SD | 1.50 ± 2.95 | 1.79 ± 2.93 | 0.38 ± 2.83 |
| 1-month MCV change (fL; %) | Mean ± SD | 1.53 ± 3.16 | 1.85 ± 3.12 | 0.31 ± 3.06 |
| Self-reporting | ||||
| 1-month abstinence | n (%) | 74 (79) | 60 (80) | 14 (70) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nagy, R.; Ocskay, K.; Váradi, A.; Papp, M.; Vitális, Z.; Izbéki, F.; Boros, E.; Gajdán, L.; Szentesi, A.; Erőss, B.; et al. In-Hospital Patient Education Markedly Reduces Alcohol Consumption after Alcohol-Induced Acute Pancreatitis. Nutrients 2022, 14, 2131. https://doi.org/10.3390/nu14102131
Nagy R, Ocskay K, Váradi A, Papp M, Vitális Z, Izbéki F, Boros E, Gajdán L, Szentesi A, Erőss B, et al. In-Hospital Patient Education Markedly Reduces Alcohol Consumption after Alcohol-Induced Acute Pancreatitis. Nutrients. 2022; 14(10):2131. https://doi.org/10.3390/nu14102131
Chicago/Turabian StyleNagy, Rita, Klementina Ocskay, Alex Váradi, Mária Papp, Zsuzsanna Vitális, Ferenc Izbéki, Eszter Boros, László Gajdán, Andrea Szentesi, Bálint Erőss, and et al. 2022. "In-Hospital Patient Education Markedly Reduces Alcohol Consumption after Alcohol-Induced Acute Pancreatitis" Nutrients 14, no. 10: 2131. https://doi.org/10.3390/nu14102131
APA StyleNagy, R., Ocskay, K., Váradi, A., Papp, M., Vitális, Z., Izbéki, F., Boros, E., Gajdán, L., Szentesi, A., Erőss, B., Hegyi, P. J., Vincze, Á., Bajor, J., Sarlos, P., Mikó, A., Márta, K., Pécsi, D., Párniczky, A., & Hegyi, P. (2022). In-Hospital Patient Education Markedly Reduces Alcohol Consumption after Alcohol-Induced Acute Pancreatitis. Nutrients, 14(10), 2131. https://doi.org/10.3390/nu14102131








