The Influence of Obesity on Nutrition and Physical Activity during COVID-19 Pandemic: A Case-Control Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Data Collection
2.4. Instruments
2.4.1. Weight and Height Measurements
2.4.2. Eating Habit Assessments
2.4.3. Physical Activity Assessment
2.5. Ethical Considerations
2.6. Data Analysis
3. Results
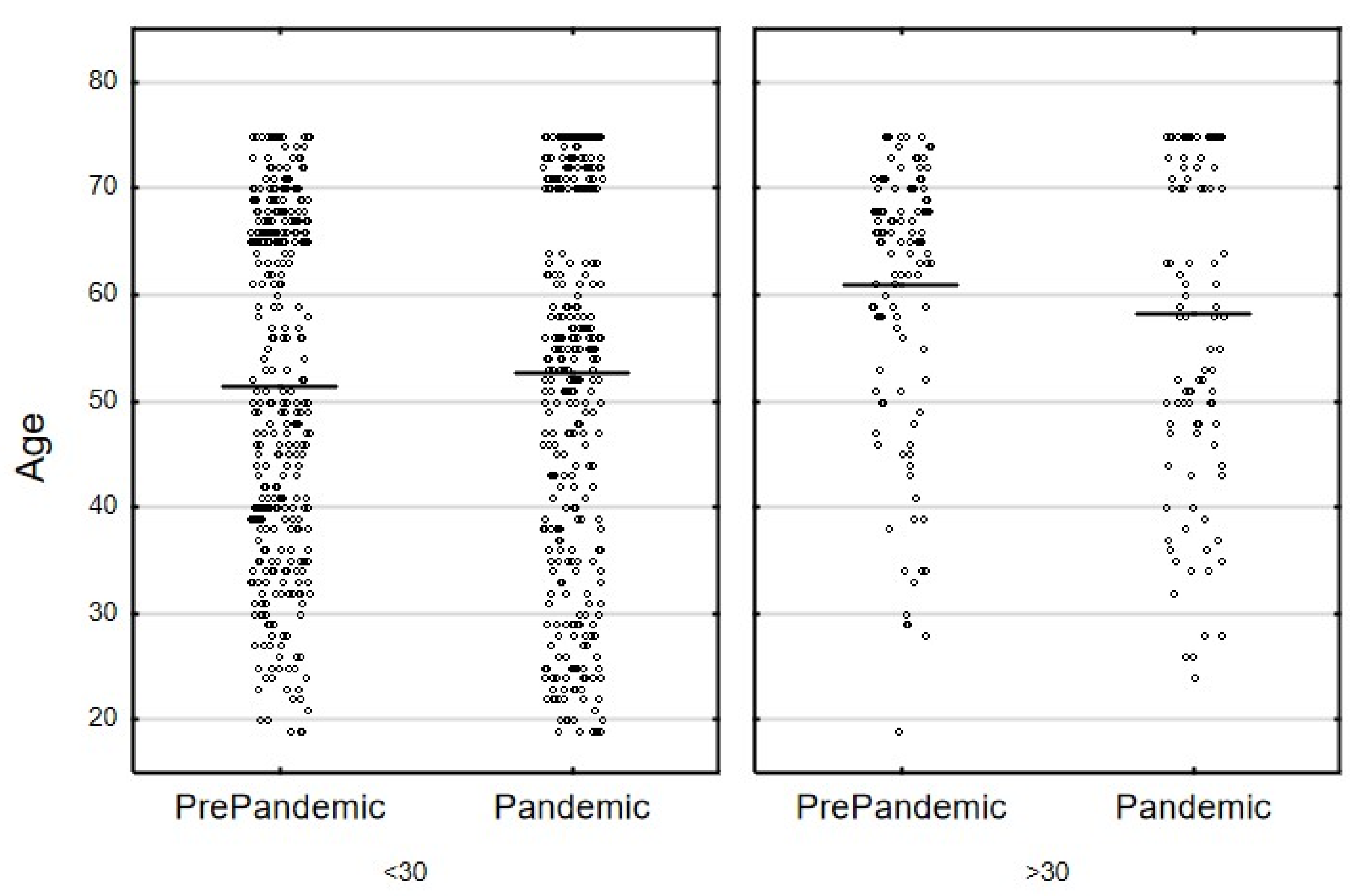
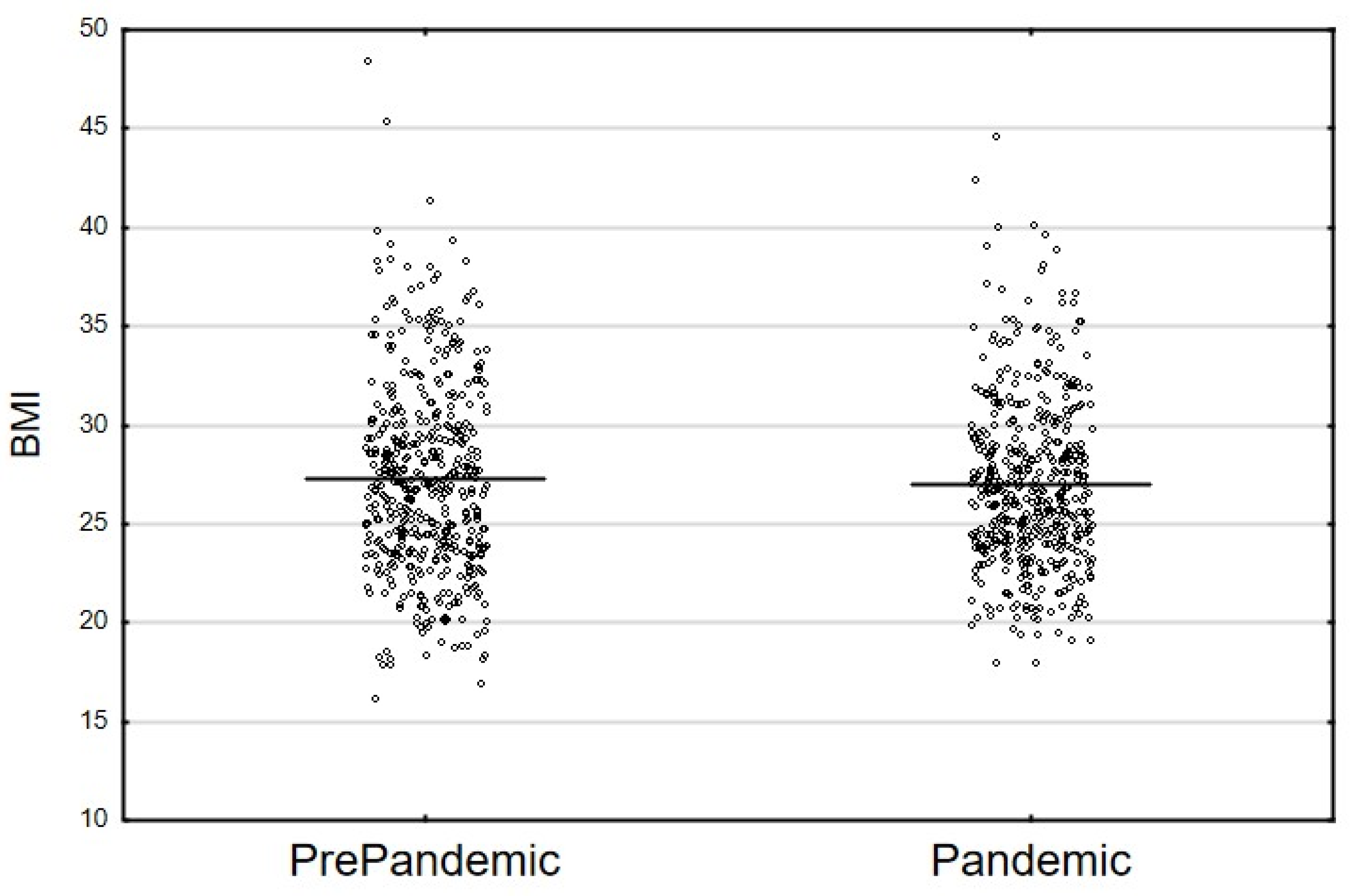
3.1. Participant Characteristics
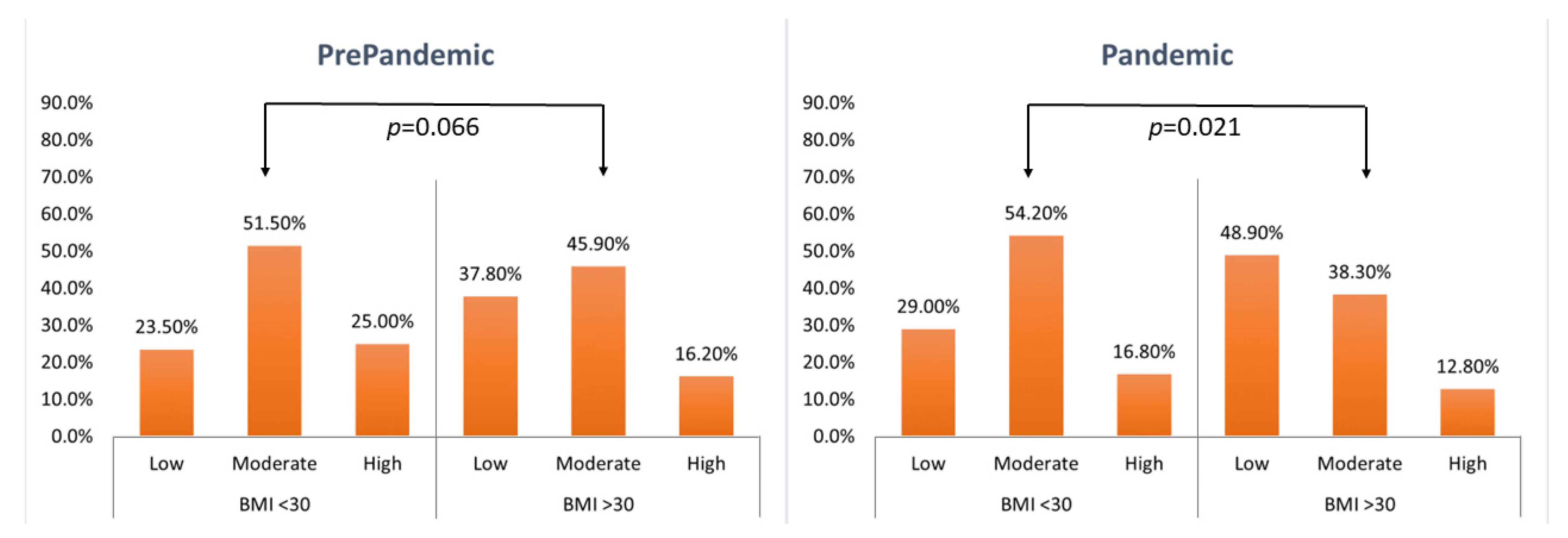
3.2. Physical Activity
3.3. Nutritional Changes
3.3.1. Qualitative Changes
3.3.2. Quantitative Changes
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Petrilli, C.M.; Jones, S.A.; Yang, J.; Rajagopalan, H.; O’Donnell, L.; Chernyak, Y.; Tobin, K.A.; Cerfolio, R.J.; Francois, F.; Horwitz, L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 2020, 369, m1966. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Du, S.; Green, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21, e13128. [Google Scholar] [CrossRef] [PubMed]
- Czernichow, S.; Beeker, N.; Rives-Lange, C.; Guerot, E.; Diehl, J.-L.; Katsahian, S.; Hulot, J.-S.; Poghosyan, T.; Carette, C.; Jannot, A.-S. Obesity Doubles Mortality in Patients Hospitalized for Severe Acute Respiratory Syndrome Coronavirus 2 in Paris Hospitals, France: A Cohort Study on 5795 Patients. Obesity 2020, 28, 2282–2289. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, M.; Ponzo, V.; Rosato, R.; Scumaci, E.; Goitre, I.; Benso, A.; Belcastro, S.; Crespi, C.; De Michieli, F.; Ghigo, E.; et al. Changes in Weight and Nutritional Habits in Adults with Obesity during the “Lockdown” Period Caused by the COVID-19 Virus Emergency. Nutrients 2020, 12, 2016. [Google Scholar] [CrossRef] [PubMed]
- De Luis Román, D.A.; Izaola, O.; Primo Martín, D.; Gómez Hoyos, E.; Torres Torres, B.; López Gómez, J.J. Effect of lockdown for COVID-19 on self-reported body weight gain in a sample of obese patients. Nutr. Hosp. 2020, 37, 1232–1237. [Google Scholar] [CrossRef]
- He, M.; Xian, Y.; Lv, X.; He, J.; Ren, Y. Changes in Body Weight, Physical Activity, and Lifestyle During the Semi-lockdown Period After the Outbreak of COVID-19 in China: An Online Survey. Disaster Med. Public Health Prep. 2020, 14, 1–6. [Google Scholar] [CrossRef]
- Kriaucioniene, V.; Bagdonaviciene, L.; Rodríguez-Pérez, C.; Petkeviciene, J. Associations between Changes in Health Behaviours and Body Weight during the COVID-19 Quarantine in Lithuania: The Lithuanian COVIDiet Study. Nutrients 2020, 12, 3119. [Google Scholar] [CrossRef]
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The Impact of COVID-19 Stay-At-Home Orders on Health Behaviors in Adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef]
- Sidor, A.; Rzymski, P. Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef]
- Błaszczyk-Bębenek, E.; Jagielski, P.; Bolesławska, I.; Jagielska, A. Nutrition Behaviors in Polish Adults before and during COVID-19 Lockdown. Nutrients 2020, 12, 3084. [Google Scholar] [CrossRef]
- Robinson, E.; Gillespie, S.; Jones, A. Weight-related lifestyle behaviours and the COVID-19 crisis: An online survey study of UK adults during social lockdown. Obes. Sci. Pract. 2020, 6, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Aminian, A.; Fathalizadeh, A.; Tu, C.; Butsch, W.S.; Pantalone, K.M.; Griebeler, M.L.; Kashyap, S.R.; Rosenthal, R.J.; Burguera, B.; Nissen, S.E. Association of prior metabolic and bariatric surgery with severity of coronavirus disease 2019 (COVID-19) in patients with obesity. Surg. Obes. Relat. Dis. 2021, 17, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Iannelli, A.; Bouam, S.; Schneck, A.S.; Frey, S.; Zarca, K.; Gugenheim, J.; Alifano, M. The Impact of Previous History of Bariatric Surgery on Outcome of COVID-19. A Nationwide Medico-Administrative French Study. Obes. Surg. 2020, 18, 1–9. [Google Scholar] [CrossRef]
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Gazda, C.; Ofori, A.; Kukreja, S.; Messiah, S.E. Impact of COVID-19 stay-at-home orders on weight-related behaviours among patients with obesity. Clin. Obes. 2020, 10, e12386. [Google Scholar] [CrossRef] [PubMed]
- Traczyk, I.; Raciborski, F.; Kucharska, A.; Sińska, B.I.; Milewska, M.; Samoliński, B.; Szostak-Węgierek, D. A National Study of Nutrition and Nutritional Status of the Adult Polish Population in the Years 2017–2020 before and during the COVID-19 Pandemic—Design and Methods. Nutrients 2021, 13, 2568. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Obesity: Preventing and Managing the Global Epidemic; WHO: Geneva, Switzerland, 2000. [Google Scholar]
- Gibson, R.S. Principles of Nutritional Assessment, 2nd ed.; Oxford University Press: New York, NY, USA, 2005.
- Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES). Anthropometry Procedures. Available online: https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2007 (accessed on 26 September 2021).
- European Food Safety Authority (EFSA). General principles for the collection of national food consumption data in the view of a pan-European dietary survey. EFSA J. 2009, 7, 1435. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA). Guidance on the EU Menu methodology. EFSA J. 2014, 12, 3944–3977. [Google Scholar] [CrossRef] [Green Version]
- Przysławski, J.; Borawska, M.; Biernat, J. Adult Diet. Research Methods in the Dietary Research Methodological Guide; Gronowska-Senger, A., Ed.; The Committee of Human Nutrition Science, Polish Academy of Sciences: Warsaw, Poland, 2013; pp. 89–94. [Google Scholar]
- Brzozowska, A.; Roszkowski, W. Dietary Research Methods for Elderly People in the Dietary Research Methodological Guide; Gronowska-Senger, A., Ed.; The Committee of Human Nutrition Science, Polish Academy of Sciences: Warsaw, Poland, 2013; pp. 96–105. [Google Scholar]
- Wajszczyk, B.; Chwojnowska, Z.; Nasiadko, D.; Rybaczuk, M.; Charzewska, J. (Eds.) Instructions for the Use of the 6.0 Diet Program for Planning and Ongoing Evaluation of Individual and Collective Nutrition in Methodical Guide of Dietary Research; National Food and Nutrition Institute: Warsaw, Poland, 2018. Available online: https://www.pzh.gov.pl/uslugi/dieta-6/ (accessed on 26 September 2021).
- Wądołowska, L.; Krusińska, B. Kwestionariusz do Badania Poglądów i Zwyczajów Żywieniowych Oraz Procedura Opracowania Danych. In Procedura Opracowania Danych Żywieniowych z Kwestionariusza KomPAN; Rozdz. 3. Red; Gawęcki, J., Ed.; The Committee of Human Nutrition Science, Polish Academy of Sciences: Warsaw, Poland, 2014; pp. 34–51. Available online: http://www.knozc.pan.pl/ (accessed on 26 September 2021).
- Wolnicka, K. Talerz Zdrowego Żywienia. Available online: https://ncez.pl/abc-zywienia-/zasady-zdrowego-zywienia/talerz-zdrowego-zywienia (accessed on 26 September 2021).
- Jeżewska-Zychowicz, M.; Gawęcki, J.; Wadolowska, L.; Czarnocinska, J.; Galinski, G.; Kollajtis-Dolowy, A.; Krusinska, B. Dietary Habits and Nutrition Beliefs Questionnaire for people 15–65 years old, version 1.1.–interviewer administered questionnaire. In Dietary Habits and Nutrition Beliefs Questionnaire and the Manual for Developing of Nutritional Data; Gawęcki, J., Ed.; The Committee of Human Nutrition Science, Polish Academy of Sciences: Olsztyn, Poland, 2018; Chapter 1; pp. 3–20. Available online: https://knozc.pan.pl/index.php?option=com_content&view=article&id=137:dietary-habits-and-nutrition-beliefs-questionnaireand-the-manual-for-developing-of-nutritional-data-kompan-english-version-2nd-edition&catid=36&Itemid=129 (accessed on 15 September 2021).
- Altman, D.G.; Bland, J.M. Statistics notes: The normal distribution. BMJ 1995, 310, 298. [Google Scholar] [CrossRef] [Green Version]
- Ulrich-Lai, Y.M.; Fulton, S.; Wilson, M.; Petrovich, G.; Rinaman, L. Stress exposure, food intake and emotional state. Stress 2015, 18, 381–399. [Google Scholar]
- Clemente-Suárez, V.J.; Ramos-Campo, D.J.; Mielgo-Ayuso, J.; Dalamitros, A.A.; Nikolaidis, P.A.; Hormeño-Holgado, A.; Tornero-Aguilera, J.F. Nutrition in the Actual COVID-19 Pandemic. A Narrative Review. Nutrients 2021, 13, 1924. [Google Scholar] [CrossRef]
- Lamarche, B.; Brassard, D.; Lapointe, A.; Laramée, C.; Kearney, M.; Côté, M.; Bélanger-Gravel, A.; Desroches, S.; Lemieux, S.; Plante, C. Changes in diet quality and food security among adults during the COVID-19-related early lockdown: Results from NutriQuébec. Am. J. Clin. Nutr. 2021, 113, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Hills, A.P.; Byrne, N.M.; Lindstrom, R.; Hill, J.O. ‘Small changes’ to diet and physical activity behaviors for weight management. Obes. Facts 2013, 6, 228–238. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Cheikh, I.L.; Osaili, T.M.; Mohamad, M.N.; Al Marzouqi, A.; Jarrar, A.H.; Abu Jamous, D.O.; Magriplis, E.; Ali, H.I.; Al Sabbah, H.; Hasan, H.; et al. Eating Habits and Lifestyle during COVID-19 Lockdown in the United Arab Emirates: A Cross-Sectional Study. Nutrients 2020, 12, 3314. [Google Scholar] [CrossRef]
- Deschasaux-Tanguy, M.; Druesne-Pecollo, N.; Esseddik, Y.; De Edelenyi, F.S.; Allès, B.; Andreeva, V.A.; Baudry, J.; Charreire, H.; Deschamps, V.; Egnell, M.; et al. Diet and physical activity during the coronavirus disease 2019 (COVID-19) lockdown (March–May 2020): Results from the French NutriNet-Santé cohort study. Am. J. Clin. Nutr. 2021, 113, 924–938. [Google Scholar] [CrossRef]
- Freisling, H.; van Bakel, M.M.; Biessy, C.; May, A.M.; Byrnes, G.; Norat, T.; Rinaldi, S.; De Magistris, M.S.; Grioni, S.; Bueno-de-Mesquita, H.B.; et al. Dietary reporting errors on 24 h recalls and dietary questionnaires are associated with BMI across six European countries as evaluated with recovery biomarkers for protein and potassium intake. Br. J. Nutr. 2012, 107, 910–920. [Google Scholar] [CrossRef] [Green Version]
- Robinson, E.; Boyland, E.; Chisholm, A.; Harrold, J.; Maloney, N.G.; Marty, L.; Mead, B.R.; Noonan, R.; Hardman, C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite 2021, 156, 104853. [Google Scholar] [CrossRef]
- Giustino, V.; Parroco, A.M.; Gennaro, A.; Musumeci, G.; Palma, A.; Battaglia, G. Physical activity levels and related energy expenditure during COVID-19 quarantine among the sicilian active population: A cross-sectional online survey study. Sustainability 2020, 12, 4356. [Google Scholar] [CrossRef]
- Puccinelli, P.J.; da Costa, T.S.; Seffrin, A.; de Lira, C.A.B.; Vancini, R.L.; Nikolaidis, P.T.; Knechtle, B.; Rosemann, T.; Hill, L.; Andrade, M.S. Reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: An internet-based survey. BMC Public Health 2021, 21, 425. [Google Scholar]
- Amini, H.; Isanejad, A.; Chamani, N.; Movahedi-Fard, F.; Salimi, F.; Moezi, M.; Habibi, S. Physical activity during COVID-19 pandemic in the Iranian population: A brief report. Heliyon 2020, 6, e05411. [Google Scholar] [CrossRef]
- Dunton, G.F.; Wang, S.D.; Do, B.; Courtney, J. Early effects of the COVID-19 pandemic on physical activity locations and behaviors in adults living in the United States. Prev. Med. Rep. 2020, 20, 101241. [Google Scholar] [CrossRef] [PubMed]
- Górnicka, M.; Drywień, M.E.; Zielinska, M.A.; Hamułka, J. Dietary and Lifestyle Changes During COVID-19 and the Subsequent Lockdowns among Polish Adults: A Cross-Sectional Online Survey PLifeCOVID-19 Study. Nutrients 2020, 12, 2324. [Google Scholar] [CrossRef] [PubMed]
- Drywień, M.E.; Hamulka, J.; Zielinska-Pukos, M.A.; Jeruszka-Bielak, M.; Górnicka, M. The COVID-19 Pandemic Lockdowns and Changes in Body Weight among Polish Women. A Cross-Sectional Online Survey PLifeCOVID-19 Study. Sustainability 2020, 12, 7768. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
- Kokko, S.; Martin, L.; Geidne, S.; Van Hoye, A.; Lane, A.; Meganck, J.; Scheerder, J.; Seghers, J.; Villberg, J.; Kudlacek, M.; et al. Does sports club participation contribute to physical activity among children and adolescents? A comparison across six European countries. Scand. J. Public Health 2019, 47, 851–858. [Google Scholar] [CrossRef]
- Visser, M.; Schaap, L.A.; Wijnhoven, H.A.H. Self-Reported Impact of the COVID-19 Pandemic on Nutrition and Physical Activity Behaviour in Dutch Older Adults Living Independently. Nutrients 2020, 12, 3708. [Google Scholar] [CrossRef]
- Schmier, J.K.; Halpern, M.T. Patient recall and recall bias of health state and health status. Expert Rev. Pharmacoecon. Outcomes Res. 2004, 4, 159–163. [Google Scholar] [CrossRef]
- Bates, C.H.J.; Bogin, B.; Holmes, B. Nutritional assessment methods. In Human Nutrition, 13th ed.; Geissler, C., Powers, H., Eds.; Oxford University Press: Oxford, UK, 2017; pp. 613–647. [Google Scholar]
- Vilallonga, R.; Garcia Ruiz de Gordejuela, A.; Cossio-Gil, Y.; Dominguez Gonzalez, J.M.; Martin Sanchez, R.; Armengol Carrasco, M. Transforming a surgical department during the outbreak of new coronavirus pandemic. Clinical implications. Langenbecks Arch. Surg. 2020, 405, 867–875. [Google Scholar] [CrossRef]

| Group of Products | Consumption Frequency (*) |
|---|---|
| Healthy groups of products—Pro-Healthy Diet (the higher the score, the better the nutrition) | |
| 1. Vegetables | Several times a day |
| 2. Fruits | At least once daily |
| 3. Whole grains | At least once daily |
| 4. Dairy products | At least once daily |
| 5. Legumes | At least several times a week |
| 6. Fish | At least once a week |
| 7. Water | At least once daily |
| 8. White meat | Several times a week or less frequently |
| Unhealthy groups of products—Non-Healthy Diet (the higher the score, the worse the nutrition) | |
| 1. Refined grains | Several times a day |
| 2. Red and processed meat | At least once a week |
| 3. Canned meat | At least once a week |
| 4. Butter | At least several times a week |
| 5. Lard | At least several times a week |
| 6. Fried food | At least once a week |
| 7. Fast food | At least once a week |
| 8. Sweets | At least several times a week |
| 9. Salty snacks | At least several times a week |
| 10. Sweetened drinks | At least once a week |
| 11. Energy drinks | At least once a week |
| 12. Alcohol | At least once a week |
| Physical Activity Domain | The Level of Physical Activity | ||
|---|---|---|---|
| Low | Moderate | High | |
| at work or in school | over 70% of time sitting | about 50% of time sitting and about 50% of time moving about | about 70% of time moving about or physical labor |
| during leisure time | mostly sedentary, watching TV, reading newspapers/books, light housework, walking for 1–2 h/week | walking, cycling, exercise, gardening or other light physical activity for 2–3 h/week | cycling, running, gardening and other sport/recreational activities that require physical activity for longer than 3 h/week |
| Variable * | BMI (kg/m2) | PrePandemic (n = 482) | Pandemic (n = 482) | χ2 | p-Value ** |
|---|---|---|---|---|---|
| Sex | |||||
| Male | <30 | 210 (83.00) | 208 (82.21) | 0.055 | 0.815 |
| ≥30 | 43 (17.00) | 45 (17.79) | |||
| Female | <30 | 150 (65.50) | 169 (73.80) | 3.729 | 0.053 |
| ≥30 | 79 (34.50) | 60 (26.20) | |||
| Education | |||||
| Primary/Junior high school | <30 | 23 (71.88) | 21 (75.00) | 0.075 | 0.785 |
| ≥30 | 9 (28.13) | 7 (25.00) | |||
| Basic vocational | <30 | 128 (69.95) | 147(78.19) | 3.288 | 0.070 |
| ≥30 | 55 (30.05) | 41 (21.81) | |||
| High school | <30 | 136 (73.91) | 143 (79.01) | 1.314 | 0.252 |
| ≥30 | 48 (26.09) | 38 (20.99) | |||
| Higher | <30 | 73 (87.95) | 66 (77.65) | 3.122 | 0.077 |
| ≥30 | 10 (12.05) | 19 (22.35) | |||
| Marital status | |||||
| Single | <30 | 70 (92.11) | 69 (84.15) | 2.362 | 0.124 |
| ≥30 | 6 (7.89) | 13 (15.85) | |||
| Married\Civil partnership | <30 | 251 (74.70) | 245 (78.53) | 1.317 | 0.251 |
| ≥30 | 85 (25.30) | 67 (21.47) | |||
| Divorced\Separated | <30 | 14 (63.64) | 21 (80.77) | 1.771 | 0.183 |
| ≥30 | 8 (36.36) | 5 (19.23) | |||
| Widowed | <30 | 25 (52.08) | 42 (67.74) | 2.786 | 0.095 |
| ≥30 | 23 (47.92) | 20 (32.26) | |||
| Household financial situation | |||||
| Good | <30 | 326 (74.43) | 354 (79.91) | 3.218 | 0.073 |
| ≥30 | 112 (25.57) | 89 (20.09) | |||
| Bad | <30 | 34 (77.27) | 23 (58.97) | 3.757 | 0.053 |
| ≥30 | 10 (22.73) | 16 (41.03) | |||
| Number of people in the household | |||||
| 1 | <30 | 53 (76.56) | 64 (78.05) | 0.256 | 0.613 |
| ≥30 | 28 (23.44) | 17 (21.95) | |||
| >1 | <30.00 | 307 (65.43) | 313 (79.01) | 3.723 | 0.054 |
| ≥30.00 | 94 (34.57) | 88 (20.99) | |||
| Condition Types | BMI (kg/m2) | Affected | PrePandemic (n = 482) | Pandemic (n = 482) | χ2 | p-Value * | ||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | |||||
| Cardiovascular conditions | <30 | No | 304 | 84.44 | 316 | 83.82 | 0.054 | 0.817 |
| Yes | 56 | 15.56 | 61 | 16.18 | ||||
| ≥30 | No | 72 | 59.02 | 70 | 66.67 | 1.410 | 0.235 | |
| Yes | 50 | 40.98 | 35 | 33.33 | ||||
| Respiratory conditions | <30 | No | 356 | 98.89 | 361 | 95.76 | 6.846 | 0.009 |
| Yes | 4 | 1.11 | 16 | 4.24 | ||||
| ≥30 | No | 114 | 93.44 | 102 | 97.14 | 1.676 | 0.196 | |
| Yes | 8 | 6.56 | 3 | 2.86 | ||||
| Gastrointestinal conditions | <30 | No | 356 | 98.89 | 364 | 96.55 | 4.464 | 0.035 |
| Yes | 4 | 1.11 | 13 | 3.45 | ||||
| ≥30 | No | 113 | 92.62 | 101 | 96.19 | 1.330 | 0.249 | |
| Yes | 9 | 7.38 | 4 | 3.81 | ||||
| Endocrine conditions (excluding diabetes) | <30 | No | 353 | 98.06 | 363 | 96.29 | 2.082 | 0.149 |
| Yes | 7 | 1.94 | 14 | 3.71 | ||||
| ≥30 | No | 107 | 87.70 | 98 | 93.33 | 2.043 | 0.153 | |
| Yes | 15 | 12.30 | 7 | 6.67 | ||||
| Musculoskeletal conditions | <30 | No | 328 | 91.11 | 339 | 89.92 | 0.304 | 0.582 |
| Yes | 32 | 8.89 | 38 | 10.08 | ||||
| ≥30 | No | 110 | 90.16 | 90 | 85.71 | 1.066 | 0.302 | |
| Yes | 12 | 9.84 | 15 | 14.29 | ||||
| Malignancies | <30 | No | 358 | 99.44 | 374 | 99.20 | 0.158 | 0.691 |
| Yes | 2 | 0.56 | 3 | 0.80 | ||||
| ≥30 | No | 120 | 98.36 | 103 | 98.10 | 0.023 | 0.880 | |
| Yes | 2 | 1.64 | 2 | 1.90 | ||||
| Diabetes | <30 | No | 345 | 95.84 | 363 | 96.30 | 0.100 | 0.752 |
| Yes | 15 | 4.16 | 14 | 3.70 | ||||
| ≥30 | No | 105 | 86.10 | 91 | 86.70 | 0.017 | 0.895 | |
| Yes | 17 | 13.90 | 14 | 13.30 | ||||
| Allergy | <30 | No | 347 | 96.39 | 360 | 95.49 | 0.380 | 0.537 |
| Yes | 13 | 3.61 | 17 | 4.51 | ||||
| ≥30 | No | 116 | 95.08 | 102 | 97.14 | 0.629 | 0.428 | |
| Yes | 6 | 4.92 | 3 | 2.86 | ||||
| BMI (kg/m2) | Level of Physical Activity | PrePandemic (n = 482) | Pandemic (n = 482) | (z) p-Value * | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | (z) p-Value * | n | % | (z) p-Value * | |||
| <30 | Low | 105 | 29.2 | (4.693) <0.001 | 179 | 47.5 | (3.145) 0.002 | (5.969) <0.001 |
| Moderate | 209 | 58.1 | 185 | 49.1 | ||||
| High | 46 | 12.8 | 13 | 3.4 | ||||
| >30 | Low | 65 | 53.3 | 67 | 63.8 | (1.937) 0.053 | ||
| Moderate | 49 | 40.2 | 38 | 36.2 | ||||
| High | 8 | 6.6 | 0 | 0.0 | ||||
| BMI (kg/m2) | Level of Physical Activity | PrePandemic (n = 233#) | Pandemic (n = 261#) | (z) p-Value * | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | (z) p-Value * | n | % | (z) p-Value * | |||
| <30 | Low | 46 | 23.5 | 1.840 (0.066) | 62 | 29.0 | (2.300) 0.021 | (2.001) 0.045 |
| Moderate | 101 | 51.5 | 116 | 54.2 | ||||
| High | 49 | 25.0 | 36 | 16.8 | ||||
| >30 | Low | 14 | 37.8 | 23 | 48.9 | (0.974) 0.330 | ||
| Moderate | 17 | 45.9 | 18 | 38.3 | ||||
| High | 6 | 16.2 | 6 | 12.8 | ||||
| BMI | PrePandemic (n = 482) | Pandemic (n = 482) | p-Value ** | |||||
|---|---|---|---|---|---|---|---|---|
| M | SD | p-Value * | M | SD | p-Value * | |||
| Pro-Healthy Diet Indicator | <30 | 2.92 | 1.43 | 0.294 | 2.73 | 1.30 | 0.970 | 0.057 |
| ≥30 | 2.77 | 1.41 | 2.72 | 1.18 | 0.796 | |||
| Non-Healthy Diet Indicator | <30 | 4.84 | 2.13 | 0.003 | 4.67 | 2.01 | 0.685 | 0.267 |
| ≥30 | 4.06 | 1.48 | 4.58 | 2.16 | 0.049 | |||
| Food Types | BMI | PrePandemic (n = 482) | Pandemic (n = 482) | p-Value | ||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| Refined grains | <30 | 1.37 | 0.77 | 1.20 | 0.79 | 0.003 |
| ≥30 | 1.27 | 0.78 | 1.34 | 0.76 | 0.49 | |
| Fried foods | <30 | 0.35 | 0.23 | 0.35 | 0.24 | 0.74 |
| ≥30 | 0.30 | 0.20 | 0.38 | 0.33 | 0.002 | |
| Lard | <30 | 0.20 | 0.29 | 0.12 | 0.24 | 0.000 |
| ≥30 | 0.10 | 0.17 | 0.11 | 0.18 | 0.83 | |
| Processed meat | <30 | 0.95 | 0.69 | 0.74 | 0.54 | 0.000 |
| ≥30 | 0.78 | 0.54 | 0.86 | 0.56 | 0.32 | |
| Red meat | <30 | 0.32 | 0.24 | 0.26 | 0.22 | 0.000 |
| ≥30 | 0.28 | 0.21 | 0.28 | 0.24 | 0.8 | |
| BMI (kg/m2) | PrePandemic | Pandemic | p ** | |||
|---|---|---|---|---|---|---|
| M ± SD | p * | M ± SD | p * | |||
| Calories (kcal) | <30 | 2194 ± 789 | 0.005 | 2217 ± 695 | 0.370 | 0.680 |
| ≥30 | 1971 ± 880 | 2290 ± 591 | 0.001 | |||
| Total carbohydrates (g) | <30 | 283.1 ± 96.8 | 0.002 | 280.2 ± 93.3 | 0.060 | 0.670 |
| ≥30 | 252.0 ± 101.5 | 299.3 ± 83.8 | 0.000 | |||
| Sucrose (g) | <30 | 58.3 ± 33.0 | 0.009 | 62.6 ± 39.5 | 0.030 | 0.120 |
| ≥30 | 51.7 ± 30.0 | 71.6 ± 49.9 | 0.000 | |||
| Plant protein (g) | <30 | 29.8 ± 11.4 | 0.002 | 29.00 ± 10.8 | 0.820 | 0.290 |
| ≥30 | 26.3 ± 12.1 | 29.3 ± 8.3 | 0.040 | |||
| Total fat (g) | <30 | 80.2 ± 36.6 | 0.053 | 82.6 ± 30.9 | 0.557 | 0.335 |
| ≥30 | 73.1 ± 42.6 | 84.9 ± 29.6 | 0.011 | |||
| Saturated fatty acids (g) | <30 | 30.8 ± 14.5 | 0.421 | 32.4 ± 13.3 | 0.247 | 0.112 |
| ≥30 | 29.5 ± 16.4 | 34.3 ± 13.9 | 0.014 | |||
| Total protein (g) | <30 | 82.7 ± 31.8 | 0.055 | 82.6 ± 25.1 | 0.976 | 0.993 |
| ≥30 | 76.8 ± 37.8 | 82.7 ± 22.3 | 0.128 | |||
| Animal protein (g) | <30 | 51.7 ± 23.6 | 0.510 | 52.4 ± 9.5 | 0.999 | 0.637 |
| ≥30 | 50.1 ± 29.2 | 52.4 ± 17.7 | 0.434 | |||
| Dietary fiber (g) | <30 | 18.5 ± 6.5 | 0.176 | 17.9 ± 6.5 | 0.395 | 0.218 |
| ≥30 | 17.6 ± 7.6 | 18.5 ± 5.4 | 0.276 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wyleżoł, M.; Sińska, B.I.; Kucharska, A.; Panczyk, M.; Raciborski, F.; Szostak-Węgierek, D.; Milewska, M.; Samoliński, B.; Frączek, M.; Traczyk, I. The Influence of Obesity on Nutrition and Physical Activity during COVID-19 Pandemic: A Case-Control Study. Nutrients 2022, 14, 2236. https://doi.org/10.3390/nu14112236
Wyleżoł M, Sińska BI, Kucharska A, Panczyk M, Raciborski F, Szostak-Węgierek D, Milewska M, Samoliński B, Frączek M, Traczyk I. The Influence of Obesity on Nutrition and Physical Activity during COVID-19 Pandemic: A Case-Control Study. Nutrients. 2022; 14(11):2236. https://doi.org/10.3390/nu14112236
Chicago/Turabian StyleWyleżoł, Mariusz, Beata I. Sińska, Alicja Kucharska, Mariusz Panczyk, Filip Raciborski, Dorota Szostak-Węgierek, Magdalena Milewska, Bolesław Samoliński, Mariusz Frączek, and Iwona Traczyk. 2022. "The Influence of Obesity on Nutrition and Physical Activity during COVID-19 Pandemic: A Case-Control Study" Nutrients 14, no. 11: 2236. https://doi.org/10.3390/nu14112236







