Intakes of Folate, Vitamin B6, and Vitamin B12 in Relation to All-Cause and Cause-Specific Mortality: A National Population-Based Cohort
Abstract
:1. Introduction
2. Materials and Methods
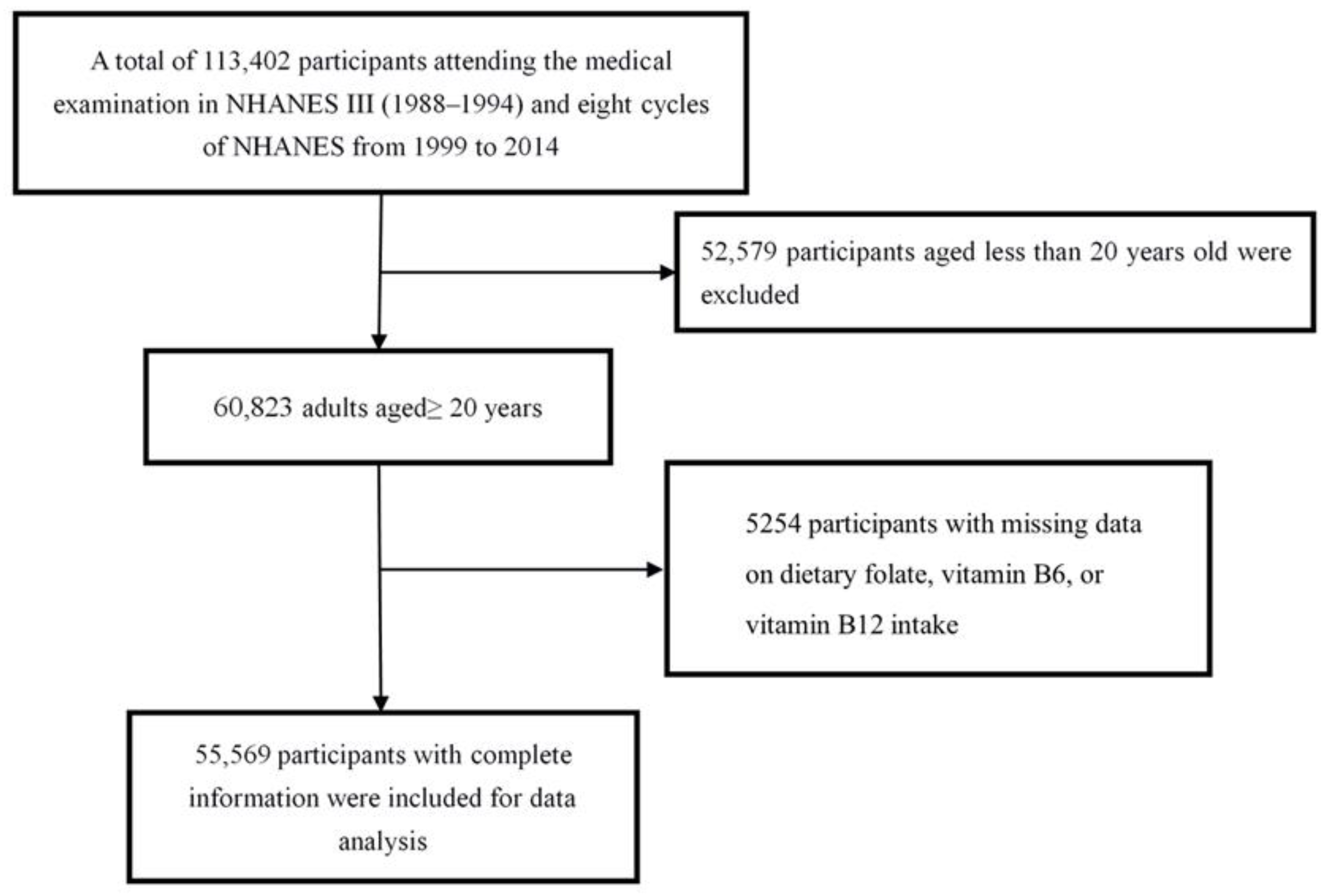
2.1. Study Population
2.2. Measurement of Dietary Folate, Vitamin B6, and Vitamin B12 Intake
2.3. Ascertainment of Mortality
2.4. Covariates
2.5. Statistical Analysis
3. Results
3.1. General Characteristics
3.2. Dietary Folate with All-Cause and Cause-Specific Mortality
3.3. Dietary Vitamin B6 with All-Cause and Cause-Specific Mortality
3.4. Dietary Vitamin B12 with All-Cause and Cause-Specific Mortality
3.5. Subgroup and Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tsai, M.Y.; Loria, C.M.; Cao, J.; Kim, Y.; Siscovick, D.S.; Schreiner, P.J.; Hanson, N.Q. Polygenic association with total homocysteine in the post-folic acid fortification era: The CARDIA study. Mol. Genet. Metab. 2009, 98, 181–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Looker, H.C.; Fagot-Campagna, A.; Gunter, E.W.; Pfeiffer, C.M.; Sievers, M.L.; Bennett, P.H.; Nelson, R.G.; Hanson, R.L.; Knowler, W.C. Homocysteine and vitamin B(12) concentrations and mortality rates in type 2 diabetes. Diabetes Metab. Res. Rev. 2007, 23, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Ntaios, G.; Savopoulos, C.; Grekas, D.; Hatzitolios, A. The controversial role of B-vitamins in cardiovascular risk: An update. Arch. Cardiovasc. Dis. 2009, 102, 847–854. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blount, B.C.; Mack, M.M.; Wehr, C.M.; MacGregor, J.T.; Hiatt, R.A.; Wang, G.; Wickramasinghe, S.N.; Everson, R.B.; Ames, B.N. Folate deficiency causes uracil misincorporation into human DNA and chromosome breakage: Implications for cancer and neuronal damage. Proc. Natl. Acad. Sci. USA 1997, 94, 3290–3295. [Google Scholar] [CrossRef] [Green Version]
- Um, H.J.; Ko, J.W.; Won, S.B.; Kwon, Y.H. Effects of Dietary Vitamin B6 Restriction on Hepatic Gene Expression Profile of Non-Obese and Obese Mice. Nutrients 2020, 12, 3821. [Google Scholar] [CrossRef]
- Persson, E.C.; Schwartz, L.M.; Park, Y.; Trabert, B.; Hollenbeck, A.R.; Graubard, B.I.; Freedman, N.D.; McGlynn, K.A. Alcohol consumption, folate intake, hepatocellular carcinoma, and liver disease mortality. Cancer Epidemiol. Biomark. Prev. 2013, 22, 415–421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, B.; Lu, Y.; Wang, L.; Zhang, C.X. Folate intake and breast cancer prognosis: A meta-analysis of prospective observational studies. Eur. J. Cancer Prev. 2015, 24, 113–121. [Google Scholar] [CrossRef]
- Medrano, M.J.; Sierra, M.J.; Almazán, J.; Olalla, M.T.; López-Abente, G. The association of dietary folate, B6, and B12 with cardiovascular mortality in Spain: An ecological analysis. Am. J. Public Health 2000, 90, 1636–1638. [Google Scholar] [CrossRef] [Green Version]
- Cui, R.; Iso, H.; Date, C.; Kikuchi, S.; Tamakoshi, A. Dietary folate and vitamin b6 and B12 intake in relation to mortality from cardiovascular diseases: Japan collaborative cohort study. Stroke 2010, 41, 1285–1289. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Gammon, M.D.; Wetmur, J.G.; Bradshaw, P.T.; Teitelbaum, S.L.; Neugut, A.I.; Santella, R.M.; Chen, J. B-vitamin intake, one-carbon metabolism, and survival in a population-based study of women with breast cancer. Cancer Epidemiol. Biomark. Prev. 2008, 17, 2109–2116. [Google Scholar] [CrossRef] [Green Version]
- Jenkins, D.J.A.; Spence, J.D.; Giovannucci, E.L.; Kim, Y.I.; Josse, R.; Vieth, R.; Blanco Mejia, S.; Viguiliouk, E.; Nishi, S.; Sahye-Pudaruth, S.; et al. Supplemental Vitamins and Minerals for CVD Prevention and Treatment. J. Am. Coll. Cardiol. 2018, 71, 2570–2584. [Google Scholar] [CrossRef] [PubMed]
- Ebbing, M.; Bønaa, K.H.; Nygård, O.; Arnesen, E.; Ueland, P.M.; Nordrehaug, J.E.; Rasmussen, K.; Njølstad, I.; Refsum, H.; Nilsen, D.W.; et al. Cancer incidence and mortality after treatment with folic acid and vitamin B12. JAMA 2009, 302, 2119–2126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roswall, N.; Olsen, A.; Christensen, J.; Hansen, L.; Dragsted, L.O.; Overvad, K.; Tjønneland, A. Micronutrient intake in relation to all-cause mortality in a prospective Danish cohort. Food Nutr. Res. 2012, 56, 5466–5474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mursu, J.; Robien, K.; Harnack, L.J.; Park, K.; Jacobs, D.R., Jr. Dietary supplements and mortality rate in older women: The Iowa Women’s Health Study. Arch. Intern. Med. 2011, 171, 1625–1633. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC); National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention: Hyattsville, MD, USA, 2022. Available online: https://www.cdc.gov/nchs/nhanes/index.htm (accessed on 9 May 2022).
- National Center for Health Statistics (NCHS). About the National Health and Nutrition Examination Survey; NCHS: Hyattsville, MD, USA, 2017. Available online: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx (accessed on 9 May 2022).
- U.S. Department of Agriculture Food Surveys Research Group. Food and Nutrient Database for Dietary Studies; U.S. Department of Agriculture Food Surveys Research Group: Beltsville, MD, USA, 2021. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fndds/ (accessed on 2 December 2021).
- Zhang, Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann. Transl. Med. 2016, 4, 30. [Google Scholar] [CrossRef]
- Harris, H.R.; Bergkvist, L.; Wolk, A. Folate intake and breast cancer mortality in a cohort of Swedish women. Breast Cancer Res. Treat. 2012, 132, 243–250. [Google Scholar] [CrossRef] [Green Version]
- Xu, X.; Wei, W.; Jiang, W.; Song, Q.; Chen, Y.; Li, Y.; Zhao, Y.; Sun, H.; Yang, X. Association of folate intake with cardiovascular-disease mortality and all-cause mortality among people at high risk of cardiovascular-disease. Clin. Nutr. 2022, 41, 246–254. [Google Scholar] [CrossRef]
- Huang, Y.C.; Lee, M.S.; Wahlqvist, M.L. Prediction of all-cause mortality by B group vitamin status in the elderly. Clin. Nutr. 2012, 31, 191–198. [Google Scholar] [CrossRef]
- Kasperzyk, J.L.; Fall, K.; Mucci, L.A.; Håkansson, N.; Wolk, A.; Johansson, J.E.; Andersson, S.O.; Andrén, O. One-carbon metabolism-related nutrients and prostate cancer survival. Am. J. Clin. Nutr. 2009, 90, 561–569. [Google Scholar] [CrossRef] [Green Version]
- Zhao, L.G.; Shu, X.O.; Li, H.L.; Gao, J.; Han, L.H.; Wang, J.; Fang, J.; Gao, Y.T.; Zheng, W.; Xiang, Y.B. Prospective cohort studies of dietary vitamin B6 intake and risk of cause-specific mortality. Clin. Nutr. 2019, 38, 1180–1187. [Google Scholar] [CrossRef]
- Lochhead, P.; Nishihara, R.; Qian, Z.R.; Mima, K.; Cao, Y.; Sukawa, Y.; Kim, S.A.; Inamura, K.; Zhang, X.; Wu, K.; et al. Postdiagnostic intake of one-carbon nutrients and alcohol in relation to colorectal cancer survival. Am. J. Clin. Nutr. 2015, 102, 1134–1141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ricci, C.; Freisling, H.; Leitzmann, M.F.; Taljaard-Krugell, C.; Jacobs, I.; Kruger, H.S.; Smuts, C.M.; Pieters, M. Diet and sedentary behaviour in relation to cancer survival. A report from the national health and nutrition examination survey linked to the U.S. mortality registry. Clin. Nutr. 2020, 39, 3489–3496. [Google Scholar] [CrossRef] [PubMed]
- Galván-Portillo, M.V.; Oñate-Ocaña, L.F.; Pérez-Pérez, G.I.; Chen, J.; Herrera-Goepfert, R.; Chihu-Amparan, L.; Flores-Luna, L.; Mohar-Betancourt, A.; López-Carrillo, L. Dietary folate and vitamin B12 intake before diagnosis decreases gastric cancer mortality risk among susceptible MTHFR 677TT carriers. Nutrition 2010, 26, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C. Nutritional Epidemiology, 3rd ed.; Oxford University Press: New York, NY, USA, 2013. [Google Scholar]
- Danaei, G.; Ding, E.L.; Mozaffarian, D.; Taylor, B.; Rehm, J.; Murray, C.J.; Ezzati, M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009, 6, e1000058. [Google Scholar] [CrossRef] [PubMed]
- Menke, A.; Muntner, P.; Batuman, V.; Silbergeld, E.K.; Guallar, E. Blood lead below 0.48 micromol/L (10 microg/dL) and mortality among US adults. Circulation 2006, 114, 1388–1394. [Google Scholar] [CrossRef] [Green Version]
- Lavriša, Ž.; Hristov, H.; Hribar, M.; Žmitek, K.; Kušar, A.; Koroušić Seljak, B.; Gregorič, M.; Blaznik, U.; Gregorič, N.; Zaletel, K.; et al. Dietary Intake and Status of Vitamin B12 in Slovenian Population. Nutrients 2022, 14, 334. [Google Scholar] [CrossRef] [PubMed]
- Hustad, K.S.; Ottestad, I.; Olsen, T.; Sæther, T.; Ulven, S.M.; Holven, K.B. Salmon fish protein supplement increases serum vitamin B12 and selenium concentrations: Secondary analysis of a randomised controlled trial. Eur. J. Nutr. 2022, 1–9. [Google Scholar] [CrossRef]
- Pravst, I.; Lavriša, Ž.; Hribar, M.; Hristov, H.; Kvarantan, N.; Seljak, B.K.; Gregorič, M.; Blaznik, U.; Gregorič, N.; Zaletel, K.; et al. Dietary Intake of Folate and Assessment of the Folate Deficiency Prevalence in Slovenia Using Serum Biomarkers. Nutrients 2021, 13, 3860. [Google Scholar] [CrossRef]
| Variables | Total Sample n = 55,569 | Survivors n = 44,034 | Death n = 11,535 |
|---|---|---|---|
| Age, year | 49.0 (18.6) | 44.4 (16.5) | 66.4 (15.7) |
| Sex | |||
| Female | 26,566 (47.81%) | 20,343 (46.2%) | 6223 (53.95%) |
| Male | 29,003 (52.19%) | 23,691 (53.8%) | 5312 (46.05%) |
| Race | |||
| Hispanic | 14,402 (25.92%) | 12,011 (27.28%) | 2391 (20.73%) |
| Non-Hispanic white | 25,249 (45.44%) | 18,973 (43.09%) | 6276 (54.41%) |
| Non-Hispanic black | 12,658 (22.78%) | 10,090 (22.91%) | 2568 (22.26%) |
| Other race—including multi-racial | 3260 (5.87%) | 2960 (6.72%) | 300 (2.6%) |
| Drinking | |||
| Never | 14,732 (26.51%) | 10,410 (23.64%) | 4322 (37.47%) |
| Low to moderate | 11,607 (20.89%) | 8984 (20.4%) | 2623 (22.74%) |
| Heavy | 29,230 (52.60%) | 24,640 (55.96%) | 4590 (39.79%) |
| Smoking | |||
| Never | 12,662 (22.79%) | 10,050 (22.82%) | 2612 (22.64%) |
| Former | 13,919 (25.05%) | 9779 (22.21%) | 4140 (35.89%) |
| Current | 28,988 (52.17%) | 24,205 (54.97%) | 4783 (41.47%) |
| Ratio of family income to poverty | |||
| ≤1 | 12,048 (21.68%) | 9353 (21.24%) | 2695 (23.36%) |
| 1–3 | 24,021 (43.23%) | 18,178 (41.28%) | 5843 (50.65%) |
| >3 | 19,500 (35.09%) | 16,503 (37.48%) | 2997 (25.98%) |
| Diabetes | 6469 (11.64%) | 3975 (9.03%) | 2494 (21.62%) |
| Hypertension | 10,078 (18.14%) | 5814 (13.2%) | 4264 (36.97%) |
| Cardiovascular disease | 5705 (10.27%) | 2806 (6.37%) | 2899 (25.13%) |
| BMI, kg/m2 | 28.1 (6.0) | 28.2 (6.0) | 27.5 (5.7) |
| Leisure-time physical activity, MET | 18.5 (28.3) | 19.2 (29.0) | 15.5 (25.5) |
| Quartile of Nutrient Intake | Ptrend | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Men | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.89 (0.84–0.95) | 0.77 (0.72–0.83) | 0.65 (0.60–0.71) | <0.001 |
| Multivariable Model | Ref | 0.91 (0.86–0.97) | 0.86 (0.80–0.92) | 0.77 (0.71–0.85) | <0.001 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.80 (0.71–0.91) | 0.64 (0.55–0.75) | 0.53 (0.44–0.63) | <0.001 |
| Multivariable Model | Ref | 0.81 (0.71–0.92) | 0.71 (0.61–0.83) | 0.59 (0.48–0.72) | <0.001 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.82 (0.72–0.93) | 0.77 (0.66–0.89) | 0.57 (0.48–0.68) | <0.001 |
| Multivariable Model | Ref | 0.87 (0.77–0.99) | 0.89 (0.77–1.04) | 0.68 (0.56–0.84) | 0.001 |
| Women | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 1.01 (0.94–1.07) | 0.91 (0.84–0.98) | 0.85 (0.78–0.93) | <0.001 |
| Multivariable Model | Ref | 0.91 (0.85–0.97) | 0.87 (0.81–0.95) | 0.86 (0.78–0.95) | <0.001 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.91 (0.79–1.05) | 0.71 (0.59–0.86) | 0.58 (0.46–0.71) | <0.001 |
| Multivariable Model | Ref | 0.82 (0.70–0.95) | 0.69 (0.57–0.83) | 0.53 (0.41–0.69) | <0.001 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.97 (0.84–1.13) | 1.04 (0.88–1.24) | 0.79 (0.65–0.97) | 0.115 |
| Multivariable Model | Ref | 0.93 (0.80–1.08) | 1.05 (0.88–1.25) | 0.82 (0.66–1.03) | 0.342 |
| Quartile of Nutrient Intake | Ptrend | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Men | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.76 (0.72–0.81) | 0.65 (0.61–0.70) | 0.57 (0.53–0.62) | <0.001 |
| Multivariable Model | Ref | 0.94 (0.88–1.00) | 0.86 (0.80–0.93) | 0.79 (0.71–0.86) | <0.001 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.71 (0.62–0.80) | 0.55 (0.47–0.64) | 0.51 (0.43–0.61) | <0.001 |
| Multivariable Model | Ref | 0.87 (0.76–0.98) | 0.74 (0.63–0.86) | 0.69 (0.56–0.85) | <0.001 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.67 (0.59–0.76) | 0.70 (0.61–0.80) | 0.54 (0.45–0.64) | <0.001 |
| Multivariable Model | Ref | 0.85 (0.74–0.97) | 0.95 (0.82–1.10) | 0.73 (0.60–0.90) | 0.013 |
| Women | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.93 (0.87–0.99) | 0.85 (0.79–0.91) | 0.83 (0.76–0.91) | <0.001 |
| Multivariable Model | Ref | 0.93 (0.87–1.00) | 0.90 (0.84–0.98) | 0.88 (0.80–0.97) | 0.002 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.89 (0.77–1.03) | 0.71 (0.60–0.85) | 0.58 (0.47–0.72) | <0.001 |
| Multivariable Model | Ref | 0.89 (0.77–1.03) | 0.77 (0.64–0.92) | 0.56 (0.44–0.73) | <0.001 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.98 (0.84–1.13) | 0.85 (0.71–1.00) | 0.82 (0.68–1.00) | 0.017 |
| Multivariable Model | Ref | 1.01 (0.87–1.17) | 0.91 (0.76–1.08) | 0.89 (0.72–1.10) | 0.182 |
| Quartile of Nutrient Intake | Ptrend | ||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Men | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.88 (0.82–0.93) | 0.79 (0.73–0.84) | 0.66 (0.61–0.72) | <0.001 |
| Multivariable Model | Ref | 1.01 (0.95–1.08) | 1.01 (0.94–1.09) | 1.01 (0.92–1.11) | 0.719 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.78 (0.69–0.90) | 0.68 (0.59–0.79) | 0.56 (0.47–0.67) | <0.001 |
| Multivariable Model | Ref | 0.92 (0.80–1.05) | 0.91 (0.77–1.07) | 0.93 (0.76–1.13) | 0.311 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.84 (0.73–0.96) | 0.85 (0.73–0.98) | 0.65 (0.55–0.77) | <0.001 |
| Multivariable Model | Ref | 0.97 (0.84–1.11) | 1.08 (0.93–1.27) | 0.96 (0.79–1.16) | 0.895 |
| Women | |||||
| All-cause mortality | |||||
| Crude Model | Ref | 0.88 (0.82–0.95) | 0.83 (0.77–0.89) | 0.77 (0.71–0.84) | <0.001 |
| Multivariable Model | Ref | 1.04 (0.97–1.11) | 1.02 (0.94–1.11) | 1.07 (0.97–1.18) | 0.244 |
| Cardiovascular mortality | |||||
| Crude Model | Ref | 0.84 (0.72–0.97) | 0.66 (0.56–0.79) | 0.55 (0.45–0.68) | <0.001 |
| Multivariable Model | Ref | 1.11 (0.95–1.29) | 0.98 (0.81–1.19) | 1.05 (0.83–1.34) | 0.848 |
| Cancer mortality | |||||
| Crude Model | Ref | 0.93 (0.80–1.08) | 0.91 (0.77–1.07) | 0.84 (0.69–1.01) | 0.062 |
| Multivariable Model | Ref | 1.03 (0.88–1.20) | 1.05 (0.88–1.26) | 1.05 (0.84–1.31) | 0.598 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bo, Y.; Xu, H.; Zhang, H.; Zhang, J.; Wan, Z.; Zhao, X.; Yu, Z. Intakes of Folate, Vitamin B6, and Vitamin B12 in Relation to All-Cause and Cause-Specific Mortality: A National Population-Based Cohort. Nutrients 2022, 14, 2253. https://doi.org/10.3390/nu14112253
Bo Y, Xu H, Zhang H, Zhang J, Wan Z, Zhao X, Yu Z. Intakes of Folate, Vitamin B6, and Vitamin B12 in Relation to All-Cause and Cause-Specific Mortality: A National Population-Based Cohort. Nutrients. 2022; 14(11):2253. https://doi.org/10.3390/nu14112253
Chicago/Turabian StyleBo, Yacong, Huadong Xu, Huanhuan Zhang, Junxi Zhang, Zhongxiao Wan, Xin Zhao, and Zengli Yu. 2022. "Intakes of Folate, Vitamin B6, and Vitamin B12 in Relation to All-Cause and Cause-Specific Mortality: A National Population-Based Cohort" Nutrients 14, no. 11: 2253. https://doi.org/10.3390/nu14112253






