A Scoping Review of Food Insecurity and Related Factors among Cancer Survivors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Study Selection
2.3. Data Extraction
3. Results
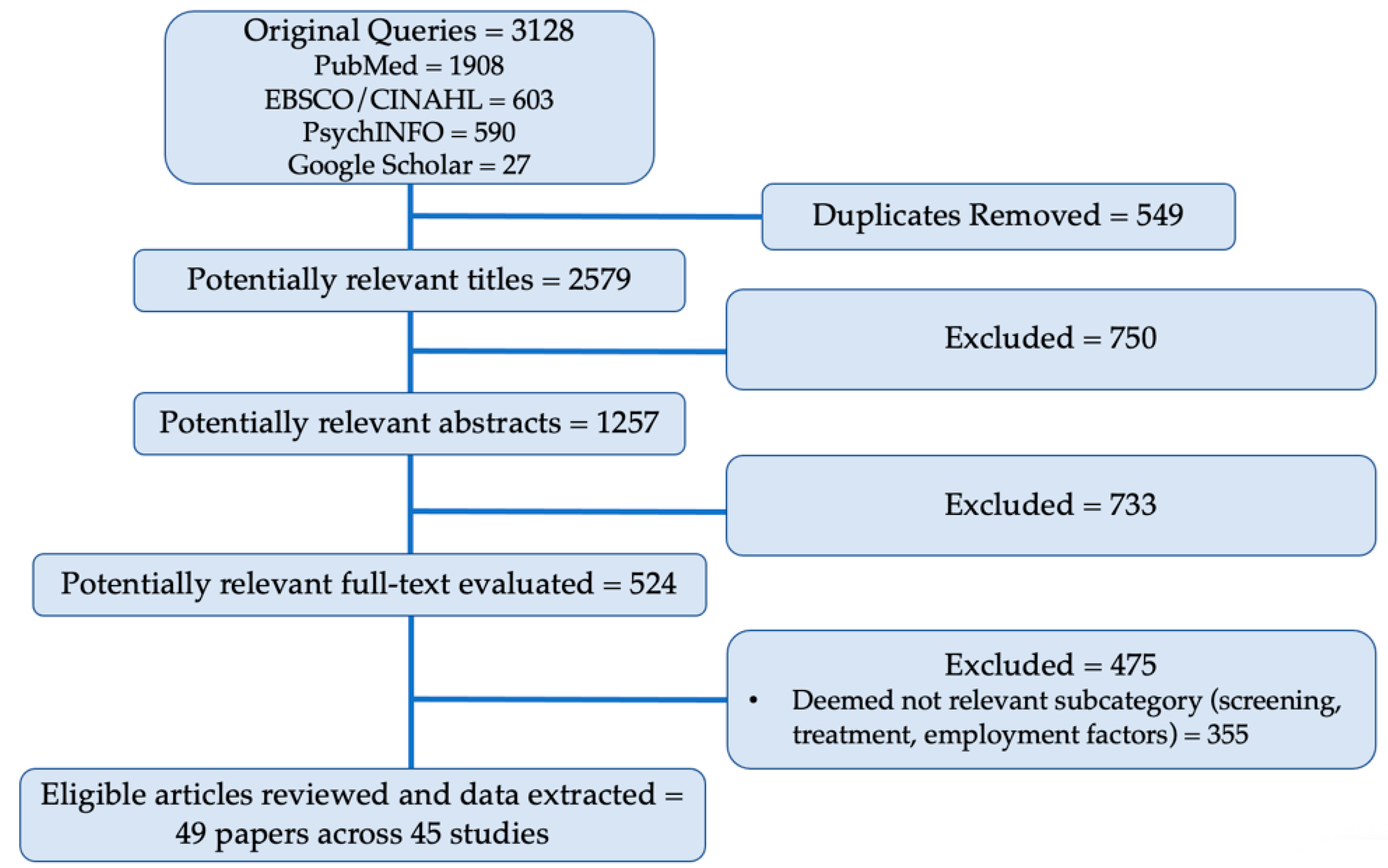
3.1. Study Selection
3.2. Study Characteristics
3.2.1. PN and Social Worker Role
3.2.2. Caregiver Role and Impact
3.2.3. Psychosocial Impacts
3.2.4. Food Insecurity and Financial Toxicity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Miller, K.D.; Siegel, R.L.; Lin, C.C.; Mariotto, A.B.; Kramer, J.L.; Rowland, J.H.; Stein, K.D.; Alteri, R.; Jemal, A. Cancer treatment and survivorship statistics, 2016. Cancer J. Clin. 2016, 66, 271–289. [Google Scholar] [CrossRef] [Green Version]
- Coleman-Jensen, A.; Rabbit, M.; Gregory, C.; Singh, A. Household Food Security in the United States in 2017, ERR-256; U.S.A. Department of Agriculture, Economic Research Service: Washington, DC, USA, 2018. Available online: https://www.ers.usda.gov/publications/pub-details/?pubid=90022 (accessed on 14 November 2018).
- Narang, A.K.; Nicholas, L.H. Out-of-pocket spending and financial burden among Medicare beneficiaries with cancer. JAMA Oncol. 2017, 3, 757–765. [Google Scholar] [CrossRef]
- Zitvogel, L.; Pietrocola, F.; Kroemer, G. Nutrition, inflammation and cancer. Nat. Immunol. 2017, 18, 843–850. [Google Scholar] [CrossRef]
- Olson, R.E.; Connor, J. When they don’t die: Prognosis ambiguity, role conflict and emotion work in cancer caregiving. J. Sociol. 2015, 51, 857–871. [Google Scholar] [CrossRef]
- Siegel, R.L.; Jemal, A.; Wender, R.C.; Gansler, T.; Ma, J.; Brawley, O.W. An assessment of progress in cancer control. Cancer J. Clin. 2018, 68, 329–339. [Google Scholar] [CrossRef] [Green Version]
- Singh, G.K.; Jemal, A. Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014: Over six decades of changing patterns and widening inequalities. J. Environ. Public Health 2017, 2017, 2819372. [Google Scholar] [CrossRef]
- Smith, R.A.; Andrews, K.S.; Brooks, D.; Fedewa, S.A.; Manassaram-Baptiste, D.; Saslow, D.; Saslow, D.; Wender, R.C. Cancer screening in the United States, 2018: A review of current American Cancer Society guidelines and current issues in cancer screening. CA Cancer J. Clin. 2018, 68, 297–316. [Google Scholar] [CrossRef]
- Ackerson, K.; Gretebeck, K. Factors influencing cancer screening practices of underserved women. J. Am. Acad. Nurse Pract. 2007, 19, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, S.S.; Caplan, L.; Young, L. A review of cancer outcomes among persons dually enrolled in Medicare and Medicaid. J. Hosp. Manag. Health Policy 2018, 2, 36. [Google Scholar] [CrossRef] [PubMed]
- Neal, C.D.; Weaver, D.T.; Raphel, T.J.; Lietz, A.P.; Flores, E.J.; Percac-Lima, S.; Knudsen, A.B.; Pandharipande, P.V. Patient navigation to improve cancer screening in underserved populations: Reported experiences, opportunities, and challenges. J. Am. Coll. Radiol. 2018, 15, 1565–1572. [Google Scholar] [CrossRef] [PubMed]
- Alfano, C.M.; Kent, E.E.; Padgett, L.S.; Grimes, M.; de Moor, J.S. Making cancer rehabilitation services work for cancer patients: Recommendations for research and practice to improve employment outcomes. Contemp. Issues Cancer Rehabil. 2017, 9, S398–S406. [Google Scholar] [CrossRef] [PubMed]
- De Boer, A.G.; Taskila, T.K.; Tamminga, S.J.; Feuerstein, M.; Frings-Dresen, M.H.; Verbeek, J.H. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst. Rev. 2015, 9, CD007569. [Google Scholar] [CrossRef] [PubMed]
- Duijts, S.; Bleiker, E.; Paalman, C.; van der Beek, A. A behavioural approach in the development of work-related interventions for cancer survivors: An exploratory review. Eur. J. Cancer Care 2017, 26, e12545. [Google Scholar] [CrossRef] [PubMed]
- Cockle-Hearne, J.; Faithfull, S. Self-management for men surviving prostate cancer: A review of behavioural and psychosocial interventions to understand what strategies can work, for whom and in what circumstances. Psycho-oncology 2010, 19, 909–922. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrell, B.R.; Kravitz, K. Cancer care: Supporting underserved and financially burdened family caregivers. J. Adv. Pract. Oncol. 2017, 8, 494–500. [Google Scholar]
- Cwikel, J.G.; Behar, L.C. Organizing social work services with adult cancer patients: Integrating empirical research. Soc. Work. Health Care 1999, 28, 55–76. [Google Scholar] [CrossRef]
- Hebert, J.R.; Braun, K.L.; Kaholokula, J.K.; Armstead, C.A.; Burch, J.B.; Thompson, B. Considering the role of stress in populations of high-risk, underserved community networks program centers. Prog. Community Health Partnersh. Res. Educ. Action 2015, 9, 71–82. [Google Scholar] [CrossRef] [Green Version]
- Ell, K.; Vourlekis, B.; Xie, B.; Nedjat-Haiem, F.R.; Lee, P.J.; Muderspach, L.; Russell, C.; Palinkas, L.A. Cancer treatment adherence among low-income women with breast or gynecologic cancer: A randomized controlled trial of patient navigation. Cancer 2009, 115, 4606–4615. [Google Scholar] [CrossRef] [Green Version]
- Ell, K.; Xie, B.; Quon, B.; Quinn, D.I.; Dwight-Johnson, M.; Lee, P.-J. Randomized controlled trial of collaborative care management of depression among low-income patients with cancer. J. Clin. Oncol. 2008, 26, 4488–4496. [Google Scholar] [CrossRef] [Green Version]
- Ell, K.; Xie, B.; Wells, A.; Nedjat-Haiem, F.; Lee, P.-J.; Vourlekis, B. Economic stress among low-income women with cancer: Effects on quality of life. Cancer 2008, 112, 616–625. [Google Scholar] [CrossRef]
- Martin, M.Y.; Evans, M.B.; Kratt, P.; Pollack, L.A.; Smith, J.L.; Oster, R.; Dingnan, M.; Prayor-Patterson, H.; Watson, C.; Houston, P.; et al. Meeting the information needs of lower income cancer survivors: Results of a randomized control trial evaluating the American cancer society’s “I Can Cope”. J. Health Commun. 2014, 19, 441–459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raich, P.C.; Whitley, E.M.; Thorland, W.; Valverde, P.; Fairclough, D. Patient navigation improves cancer diagnostic resolution: An individually randomized clinical trial in an underserved population. Cancer Epidemiol. Biomark. Prev. 2012, 21, 1629–1638. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raj, A.; Ko, N.; Battaglia, T.A.; Chabner, B.A.; Moy, B. Patient navigation for underserved patients diagnosed with breast cancer. Oncologist 2012, 17, 1027–1031. [Google Scholar] [CrossRef] [Green Version]
- Wiggins, B.; Corsini, N.; Ramsey, I.; Edwards, S.; Ball, D.; Cocks, L.; Lill, J.; Sharplin, G.; Wilson, C. An evaluation of social work services in a cancer accommodation facility for rural South Australians. Supportive Care Cancer 2018, 26, 147–154. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Darby, K.; Likes, W.; Bell, J. Social workers as patient navigators for breast cancer survivors: What do African-American medically underserved women think of this idea? Soc. Work. Health Care 2009, 48, 561–578. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.K.; Cyr, J.; Carothers, B.J.; Mueller, N.B.; Anwuri, V.V.; James, A.I. Referrals among cancer services organizations serving underserved cancer patients in an urban area. Am. J. Public Health 2011, 101, 1248–1252. [Google Scholar] [CrossRef]
- Jean-Pierre, P.; Cheng, Y.; Wells, K.J.; Freund, K.M.; Snyder, F.R.; Fiscella, K.; Holden, A.E.; Paskett, E.; Dudley, D.; Simon, M.A.; et al. Satisfaction with cancer care among underserved racial-ethnic minorities and lower-income patients receiving patient navigation. Cancer 2016, 122, 1060–1067. [Google Scholar] [CrossRef] [Green Version]
- Townsend, D.; Accurso-Massana, C.; Lechman, C.; Duder, S.; Chasen, M. Cancer nutrition rehabilitation program: The role of social work. Curr. Oncol. 2010, 17, 12–17. [Google Scholar] [CrossRef] [Green Version]
- Wells, A.A.; Palinkas, L.A.; Williams, S.-L.L.; Ell, K. Retaining low-income minority cancer patients in a depression treatment intervention trial: Lessons learned. Community Ment. Health J. 2015, 51, 715–722. [Google Scholar] [CrossRef]
- Bona, K.; London, W.B.; Guo, D.; Frank, D.A.; Wolfe, J. Trajectory of material hardship and income poverty in families of children undergoing chemotherapy: A prospective cohort study. Pediatric Blood Cancer 2016, 63, 105–111. [Google Scholar] [CrossRef]
- Clarke, J.N. Fathers’ home health care work when a child has cancer: I’m her dad; I have to do it. Men Masc. 2005, 7, 385–404. [Google Scholar] [CrossRef]
- Clarke, J.N. Advocacy: Essential work for mothers of children living with cancer. J. Psychosoc. Oncol. 2006, 24, 31–47. [Google Scholar] [CrossRef] [PubMed]
- Clarke, J.N. Mother’s home healthcare: Emotion work when a child has cancer. Cancer Nurs. 2006, 29, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Dussel, V.; Bona, K.; Heath, J.A.; Hilden, J.M.; Weeks, J.C.; Wolfe, J. Unmeasured costs of a child’s death: Perceived financial burden, work disruptions, and economic coping strategies used by American and Australian families who lost children to cancer. J. Clin. Oncol. 2011, 29, 1007–1013. [Google Scholar] [CrossRef] [Green Version]
- Howard, A.F.; Hasan, H.; Bobinski, M.A.; Nurcombe, W.; Olson, R.; Parkinson, M.; Goddard, K. Parents’ perspectives of life challenges experienced by long-term paediatric brain tumour survivors: Work and finances, daily and social functioning, and legal difficulties. J. Cancer Surviv. 2014, 8, 372–383. [Google Scholar] [CrossRef]
- Lau, S.; Lu, X.; Balsamo, L.; Devidas, M.; Winick, N.; Hunger, S.P.; Carroll, W.; Stork, L.; Maloney, K.; Kadan-Lottick, N. Family life events in the first year of acute lymphoblastic leukemia therapy: A children’s oncology group report. Pediatric Blood Cancer 2014, 61, 2277–2284. [Google Scholar] [CrossRef] [Green Version]
- Mazanec, S.R.; Daly, B.J.; Douglas, S.L.; Lipson, A.R. Work productivity and health of informal caregivers of persons with advanced cancer. Res. Nurs. Health 2011, 34, 483–495. [Google Scholar] [CrossRef]
- Ashing-Giwa, K.T. Enhancing physical well-being and overall quality of life among underserved Latina-American cervical cancer survivors: Feasibility study. J. Cancer Surviv. 2008, 2, 215–223. [Google Scholar] [CrossRef]
- Boykoff, N.; Moieni, M.; Subramanian, S.K. Confronting chemobrain: An in-depth look at survivors’ reports of impact on work, social networks, and health care response. J. Cancer Surviv. 2009, 3, 223–232. [Google Scholar] [CrossRef] [Green Version]
- Brar, R.; Maliski, S.L.; Kwan, L.; Krupski, T.L.; Litwin, M.S. Changes in quality of life among low-income men treated for prostate cancer. Urology 2005, 66, 344–349. [Google Scholar] [CrossRef]
- Costas-Muniz, R.; Leng, J.; Aragones, A.; Ramirez, J.; Roberts, N.; Mujawar, M.I.; Gany, F. Association of socioeconomic and practical unmet needs with self-reported nonadherence to cancer treatment appointments in low-income Latino and Black cancer patients. Ethn. Health 2016, 21, 118–128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Orazio, L.M.; Meyerowitz, B.E.; Stone, P.J.; Felix, J.; Muderspach, L.I. Psychosocial adjustment among low-income Latina cervical cancer patients. J. Psychosoc. Oncol. 2011, 29, 515–533. [Google Scholar] [CrossRef] [PubMed]
- Darby, K.; Davis, C.; Likes, W.; Bell, J. Exploring the financial impact of breast cancer for African American medically underserved women: A qualitative study. J. Health Care Poor Underserved 2009, 20, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Gore, J.L.; Krupski, T.; Kwan, L.; Fink, A.; Litwin, M.S. Mental health of low income uninsured men with prostate cancer. J. Urol. 2005, 173, 1323–1326. [Google Scholar] [CrossRef]
- Gore, J.L.; Krupski, T.; Kwan, L.; Maliski, S.; Litwin, M.S. Partnership status influences quality of life in low-income, uninsured men with prostate cancer. Cancer 2005, 104, 191–198. [Google Scholar] [CrossRef] [Green Version]
- Krupski, T.L.; Sonn, G.; Kwan, L.; Maliski, S.; Fink, A.; Litwin, M.S. Ethnic variation in health-related quality of life among low-income men with prostate cancer. Ethn. Dis. 2005, 15, 461–468. [Google Scholar]
- Lechner, S.C.; Whitehead, N.E.; Vargas, S.; Annane, D.W.; Robertson, B.R.; Carver, C.S.; Kobetz, E.; Antoni, M.H. Does a community-based stress management intervention affect psychological adaptation among underserved black breast cancer survivors? J. Natl. Cancer Inst. Monogr. 2014, 50, 315–322. [Google Scholar] [CrossRef] [Green Version]
- Lu, H.-Y.; Shaw, B.R.; Gustafson, D.H. Online health consultation: Examining uses of an interactive cancer communication tool by low-income women with breast cancer. Int. J. Med. Inform. 2011, 80, 518–528. [Google Scholar] [CrossRef] [Green Version]
- Marshall, C.A.; Weihs, K.L.; Larkey, L.K.; Badger, T.A.; Koerner, S.S.; Curran, M.A.; Pedroza, R.; Garcia, F.A.R. “Like a Mexican wedding”: Psychosocial intervention needs of predominately Hispanic low-income female co-survivors of cancer. J. Fam. Nurs. 2011, 17, 380–402. [Google Scholar] [CrossRef]
- Meraviglia, M.G.; Stuifbergen, A. Health-promoting behaviors of low-income cancer survivors. Clin. Nurse Spec. 2011, 25, 118–124. [Google Scholar] [CrossRef] [Green Version]
- Moadel, A.B.; Morgan, C.; Dutcher, J. Psychosocial needs assessment among an underserved, ethnically diverse cancer patient population. Cancer 2007, 109, 446–454. [Google Scholar] [CrossRef]
- Mosavel, M.; Sanders, K. Needs of low-income African American cancer survivors: Multifaceted and practical. J. Cancer Educ. 2011, 26, 717–723. [Google Scholar] [CrossRef] [PubMed]
- Wells, A.A.; Palinkas, L.A.; Shon, E.-J.; Ell, K. Low-income cancer patients in depression treatment: Dropouts and completers. J. Behav. Health Serv. Res. 2013, 40, 427–441. [Google Scholar] [CrossRef] [PubMed]
- Fenn, K.M.; Evans, S.B.; McCorkle, R.; DiGiovanna, M.P.; Pusztai, L.; Sanft, T.; Hofstatter, E.W.; Killelea, B.K.; Knobf, M.T.; Lannin, D.R.; et al. Impact of financial burden of cancer on survivors’ quality of life. J. Oncol. Pract. 2014, 10, 332–338. [Google Scholar] [CrossRef] [PubMed]
- Gany, F.; Lee, T.; Loeb, R.; Ramirez, J.; Moran, A.; Crist, M.; McNish, T.; Leng, J.C.F. Use of hospital-based food pantries among low-income urban cancer patients. J. Community Health 2015, 40, 1193–1200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gany, F.; Leng, J.; Ramirez, J.; Phillips, S.; Aragones, A.; Roberts, N.; Mujawar, M.I.; Costas-Muniz, R. Health-related quality of life of food-insecure ethnic minority patients with cancer. J. Oncol. Pract. 2015, 11, 396–402. [Google Scholar] [CrossRef] [Green Version]
- Kale, H.P.; Carroll, N.V. Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among US cancer survivors. Cancer 2016, 122, 283–289. [Google Scholar] [CrossRef]
- Lathan, C.S.; Cronin, A.; Tucker-Seeley, R.; Zafar, S.Y.; Ayanian, J.Z.; Schrag, D. Association of financial strain with symptom burden and quality of life for patients with lung or colorectal cancer. J. Clin. Oncol. 2016, 34, 1732–1740. [Google Scholar] [CrossRef] [Green Version]
- Meraviglia, M.; Stuifbergen, A.; Morgan, S.; Parsons, D. Low-income cancer survivors’ use of health-promoting behaviors. MEDSURG Nurs. 2015, 24, 101–106. [Google Scholar]
- Nekhlyudov, L.; Madden, J.; Graves, A.J.; Zhang, F.; Soumerai, S.B.; Ross-Degnan, D. Cost-related medication nonadherence and cost-saving strategies used by elderly Medicare cancer survivors. J. Cancer Surviv. 2011, 5, 395–404. [Google Scholar] [CrossRef]
- Nipp, R.D.; Zullig, L.L.; Samsa, G.; Peppercorn, J.M.; Schrag, D.; Taylor DHJr Abernethy, A.P.; Zafar, S.Y. Identifying cancer patients who alter care or lifestyle due to treatment-related financial distress. Psycho Oncol. 2016, 25, 719–725. [Google Scholar] [CrossRef] [PubMed]
- Simmons, L.A.; Modesitt, S.C.; Brody, A.C.; Leggin, A.B. Food insecurity among cancer patients in Kentucky: A pilot study. J. Oncol. Pract. 2006, 2, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Yabroff, K.R.; Dowling, E.C.; Guy, G.P.; Banegas, M.P.; Davidoff, A.; Han, X.; Virgo, K.S.; McNeel, T.S.; Chawla, N.; Blanch-Hartigan, D.; et al. Financial hardship associated with cancer in the United States: Findings from a population-based sample of adult cancer survivors. J. Clin. Oncol. 2016, 34, 259–267. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zafar, S.Y.; McNeil, R.B.; Thomas, C.M.; Lathan, C.S.; Ayanian, J.Z.; Provenzale, D. Population-based assessment of cancer survivors’ financial burden and quality of life: A prospective cohort study. J. Oncol. Pract. 2014, 11, 145–150. [Google Scholar] [CrossRef]
- Zafar, S.Y.; Peppercorn, J.M.; Schrag, D.; Taylor, D.H.; Goetzinger, A.M.; Zhong, X.; Abernethy, A.P. The financial toxicity of cancer treatment: A pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist 2013, 18, 381–390. [Google Scholar] [CrossRef] [Green Version]
- Institute of Medicine and National Research. From Cancer Patient to Cancer Survivor: Lost in Transition; The National Academies Press: Washington, DC, USA, 2006.
- Hiatt, R.A.; Breen, N. The social determinants of cancer: A challenge for transdisciplinary science. Am. J. Prev. Med. 2008, 35, S141–S150. [Google Scholar] [CrossRef]
- Pooler, J.A.; Hartline-Grafton, H.; DeBor, M.; Sudore, R.L.; Seligman, H.K. Food insecurity: A key social determinant of health for older adults. J. Am. Geriatr. Soc. 2019, 67, 421–424. [Google Scholar] [CrossRef]
- Gregory, C.A.; Coleman-Jensen, A. Food Insecurity, Chronic Disease, and Health Among Working-Age Adults, ERR-235; U.S.A Department of Agriculture, Economic Research Service: Washington, DC, USA, 2017.
- Patel, K.G.; Borno, H.T.; Seligman, H.K. Food insecurity screening: A missing piece in cancer management. Cancer 2019, 125, 3494–3501. [Google Scholar] [CrossRef] [Green Version]
| Study/Year | Country | Purpose | Study Design/Participants | Summary of Results | Implications |
|---|---|---|---|---|---|
| Patient navigation (PN) and social worker role. | |||||
| Davis, 2009 [26] | US | Understand models of care facilitated by social workers. | Focus groups with cancer survivors in 3 Tennessee cities (n = 36). | PN programs need to address access to quality care, emotional, practical concerns. Participants reluctant to discuss emotional/practical distress with providers. | Oncology social workers have a unique opportunity to meet the needs of medically underserved survivors through PN. |
| Ell, 2007 [21]; Ell, 2008 [20]; Ell, 2009 [19] | US | Explore impact of economic stress on HRQOL of survivors and role of PN. | RCT involving surveys and follow-up interviews. Breast cancer patients at urban public safety-net medical center (n = 487 for RCT; n = 29 for interviews). | Unemployment/medical cost concerns, high at baseline, decline at 12 months. Lost wage worries increased baseline-6 months. Functional, emotional, physical, social-family well-being had positive linear improvement. | Managing depression among cancer survivors in a collaborative care system with PN shows promise. Future research can explore follow-up symptom monitoring and depression care in multi-site trials. |
| Determine effectiveness of depression treatment. | 12 months: 63% of intervention patients had ≥ 50% reduction in depressive symptoms; vs. 50% of control group. | ||||
| Comparison of written resource navigation vs. written information plus PN. | 24 months: 46% of intervention, 32% of control had ≥50% decrease in depression. Intervention patients had better social and functional well-being. Intervention patients more likely to receive treatment after 12 months. | ||||
| Harris, 2011 [27] | US | Describe referrals among organizations providing services to underserved cancer patients. | Survey with underserved cancer patients in St. Louis, MO, US (n = 33). | Those providing informational services were more likely to refer patients. Specialized services (e.g., prostheses) more likely to receive referrals. Few organizations provided housing services, smoking cessation, and were lacking in particular geographic areas. | Increased awareness building among provider organizations, broader geographic coverage, increased utilization of tobacco cessation, and financial assistance services are needed. |
| Jean-Pierre, 2016 [28] | US | Examine satisfaction with interpersonal relationship with PN. | Survey with cancer patients (n = 1345). | Increased age and minority race-ethnicity status associated with a higher satisfaction. Satisfaction with PN associated with satisfaction with cancer-related care. | There is a need to understanding role of interpersonal relationships and impact on care-related outcomes. |
| Martin, 2014 [22] | US | Determine impact of “I Can Cope” (ACS intervention). | Telephone survey among low-income cancer survivors (n = 140). | Intervention participants had lower information needs. Significant covariates with lower informational needs: higher self-efficacy, younger individuals, more educated, and higher income. | Supporting self-efficacy among cancer survivors may lead to lower information needs. |
| Raich, 2012 [23] | US | Evaluate the impact of lay PNs on time to resolution and follow-up testing. | Survey among medically underserved breast and prostate cancer survivors (n = 993). | PN positively impacts time to resolution of abnormal screening tests. Barriers experienced most by patients with low household income, low education attainment, high unemployment, high uninsured rate, and high comorbidity. | PN is an effective strategy for improving adherence to diagnostic evaluation and resolution, regardless of ethnicity, insurance status and education level. |
| Raj, 2012 [24] | US | Examine characteristics among women in a PN program. | Retrospective chart review of breast cancer patients (n = 168). | PN programs facilitated evidence-based quality care for vulnerable populations. | Need for improved processes and outcomes of PN in diverse underserved settings. |
| Townsend, 2010 [29] | Canada | Describe patients in a Cancer Nutrition Rehabilitation program. | Retrospective data from a cancer nutrition program (n = 75). | Lowest% of psychological problems were older survivors (63–94 years). Most patients (85.3%) were independent with activities of daily living. 55% needed assistance with basic needs (e.g., transportation, finances, groceries). | Supporting psychological needs for cancer survivors is important and may be more of a need among younger survivors. |
| Wells, 2015 [30] | US | Assess behavioral health intervention for retention among low-income minority cancer patients. | Interviews with behavioral health providers of a depression treatment program (n = 9). | Retention strategies clustered around five dropout barriers: (1) informational, (2) instrumental, (3) provider–patient therapeutic alliance, (4) clinic setting, and (5) depression treatment. | Further identification of simple, effective, feasible, and culturally sensitive means of retaining minorities in follow-up depression care is needed. |
| Wiggins, 2018 [25] | Australia | Evaluate social work service at a facility for cancer patients receiving treatment away from home. | Survey with cancer survivors utilizing a cancer council lodge while receiving treatment (n = 149). | Social work contact (n = 19) associated with reduction in distress, better able to manage challenges, and access services between arrival and departure compared with no contact (n = 56). | Type of support cancer survivors benefit from delivered by social workers has a wide range. |
| Caregiver (CG) role and impact | |||||
| Bona, 2016 [31] | US | Describe material hardship of families at a pediatric oncology center. | Surveys with families of children receiving chemo in MA, US (n = 99). | At baseline, 20% of families had low-income. At follow-up, work disruptions caused 25% of families to lose >40% household income and 29% to experience household material hardship. | Household material hardships are prevalent in newly diagnosed pediatric oncology families. |
| Clarke, 2005 [32] | Canada | Describe the health care activities of fathers of children with cancer. | Interviews with fathers of children with cancer (n = 18). | Home health care work of fathers included: monitoring and advocacy, collaboration with medical staff, scheduling, and administration/financial/emotional management. | Further research is needed on the work that fathers do when their children have cancer to inform specific tools for parents. |
| Clarke, 2006 [33]; Clarke, 2006 [34] | Canada | Describe the health care activities of mothers of children with cancer [33]. Describe the advocacy work these mothers engage in [34]. | Focus groups with mothers of children with cancer (n = 49). | Caring for children was a full-time job and left no time for outside employment or other activities. Home health care activities included: managing medications/side effects, administration, and emotional work [33]. | A paradigm shift is needed away from the psychological suffering to the strengths possessed by mothers. |
| Medical advocacy for children carried out in response to perceived errors, understaffing, and peer advice. Many coped by educating themselves, extensive notes, and sharing their experiences with other parents [34]. | |||||
| Dussel, 2011 [35] | US and Australia | Describe financial hardship, work disruptions, income loss, and coping of families. | Survey with bereaved parents of children lost to cancer (n = 230). | Financial hardship experienced by 24% (US) and 39% (Australia). Work disruptions led to reduction in income (60%). After accounting for income loss, 22% of families dropped below the poverty line. Fundraising and reduced spending were common coping strategies. | Existing health care, social, and work policies at three sites were not sufficient to prevent financial effects of a child’s death. |
| Howard, 2014 [36] | Canada | Describe parents of pediatric survivors perspectives of life challenges experienced by their now adult child. | Survey with parents of children that experienced a brain tumor in childhood (n = 46). | Participants had difficulty gaining/sustaining employment and independent living, some requiring continuous support. Support included help with grocery shopping and meal planning. Parents considered their children vulnerable and in need of protection. | Prospective longitudinal research is needed to explore factors such as: unemployment, financial challenges and legal difficulties, which appear to be poorly addressed by health and social programs. |
| Lau, 2014 [37] | US and Australia | Measure major life changes for parents at one year after child’s leukemia diagnosis. | Surveys (during the first 12 months of therapy) with parents of children with leukemia (n = 159). | Major life changes in first year of treatment is high: 13% divorced/separated, 27% relocated homes, 22% decided not to have more children, 51% declined job opportunities, 68% decreased work hours. | The steepest incidence of family burdens occurs at diagnosis. Social workers and others should help families anticipate these challenges and develop coping strategies. |
| Mazanec, 2011 [38] | US | Identify CGs differences in work productivity, CG burden, depression, anxiety, and social support. | Surveys with CGs (n = 69). | Work productivity loss for CGs associated with increased CG hours and cancer stage, marriage status, greater financial problems, disrupted schedule. 20% of CGs were unable to see their doctor when they needed. Work productivity loss related to anxiety, depression, financial burdens, disrupted schedule, health problems. | Health care providers are in a unique position to provide health promotion education to CGs, which may ultimately improve their health and reduce the economic impact of caregiving. |
| Olson, 2015 [5] | Australia | Understand variations in CGs emotional experiences. | Interviews with spousal CGs in Australia (n = 32). | A terminal (negative) prognosis facilitates clear priorities, unambiguous emotion management, and improved social bonds. An ambiguous (positive) prognosis fosters role conflict and ongoing guilt within spousal CGs. | To support CGs, it is imperative to consider characteristics of their experiences be examined to prepare health professionals to conduct psychological screening. |
| Psychosocial (PS) impacts | |||||
| Ashing-Giwa, 2008 [39] | US | Assess feasibility of implementing a culturally sensitive telephone intervention. | Surveys (pre-post) with Latina cervical cancer survivors. (Intervention n = 15, Control n = 8). | Increases in physical well-being and positive effects (e.g., outlook on life, hopefulness, energy level, family life, intimacy, spirituality, quality of care) found in intervention group. Social/family, emotional, and functional scores did not significantly improve in either group. | Intervention associated with changes in physical well-being and QOL. |
| Boykoff, 2009 [40] | US | Understand changes patients undergo to inform care. | Focus groups with African American cancer patients (n = 75). | Cognitive impairment influences interviewees’ ability to manage their social and professional lives. Coping strategies included use of tools such as notes and calendars, and having consistent behavioral patterns. | Greater knowledge of how “chemobrain” influences post-treatment HRQOL can inform strategies. |
| Brar, 2005 [41] | US | Investigate changes over time in general and disease-specific HRQOL. | Surveys with prostate cancer patients, <200% poverty level (n = 138). | Participants with advanced prostate cancer experienced more negative changes in health. Men with < high school education experienced greater improvement in mental well-being. | Findings from this study provide a unique view of HRQOL changes over time in the study population. |
| Costas-Muniz, 2016 [42] | US | Determine if unmet financial, logistic, and care needs predict adherence to cancer treatment. | Survey with low-income ethnic minority patients at a New York, NY, US cancer clinic (n = 1098). | ≥4 unmet needs increased likelihood of reporting missing appointments. For African Americans, unmet supportive care and health insurance needs increased missed appointments. For Latinos, legal health-related issues were a predictor of missed appointments. | There is a need to understand the impact of practical and supportive unmet needs on adherence and development of interventions aiming to improve adherence. |
| D’Orazio, 2011 [43] | US | Explain the PS adjustment in order to describe and identify predictors of PS outcomes. | Survey with Latina cervical cancer patients from a California cancer clinic (n = 54). | Patients reported depression yet adequate amounts of social support. Cancer-related PS resources, life stress, and optimism accounted for PS outcomes. Common life stressors: fears of deportation, navigating a foreign medical system, not speaking English. | There is a need to develop explanatory models of adjustment for low-income Latina cervical cancer patients that include cancer-related and contextual predictors of PS well-being. |
| Darby, 2009 [44] | US | Explore the financial burden to inform culturally sensitivity. | Focus groups with African American survivors (n = 36). | Lack of insurance resulted in missed, delayed, or fewer treatment opportunities. Financial burden of cancer was not limited to the acute treatment phase. | Estimates regarding care costs should be interpreted with caution due to variations in measurement. |
| Gore, 2005 [45]; Gore, 2005 [46] | US | Evaluate the influence of partnership on HRQOL [45]. | Survey with low-income, uninsured men participating in a state-funded program that provides free prostate cancer treatment (n = 291). | Partnered patients vs. unpartnered patients: Hispanic ethnicity (58% vs. 34%); More likely to have elected surgical therapy (49% vs. 34%); Better mental health, higher spirituality, lower symptom distress [45]. | Single participants may represent an isolated cohort of men with prostate cancer. Coping and social support mechanisms to encourage the beneficial aspects of partnership and to overcome the detrimental effects of being single need to be addressed. |
| Evaluate mental health outcomes in low income men with prostate cancer [46]. | Prostate cancer patients report worse mental health. Hispanic ethnicity, urinary/bowel bother negatively associated with mental health. Spirituality and physical functioning positively associated with mental health [46]. | ||||
| Krupski, 2005 [47] | US | Describe and compare HRQOL among men with localized prostate cancer. | Survey with low-income, prostate cancer patients (n = 208). | Hispanic men with prostate cancer were less educated, more often in significant relationships, had variable income, and had worse sexual and physical function compared to other ethnicities. African-American and Hispanic men were more spiritual than Caucasian men. | Attention to demographic variations in HRQOL may improve outcomes for low- survivors across ethnicities with specialized counseling and referrals to social support systems. |
| Lechner, 2014 [48] | US | Examine participation in a cognitive-behavioral stress management program. | Surveys/interviews with underserved breast cancer patients (n = 487; n = 29 for interviews). | Participants in both conditions showed improvement on psychological well-being, HRQOL, intrusive thoughts, depressive symptoms, and stress levels. | Lack of differences between the programs may be due to the natural course of PS improvement, actual improvement from the intervention, or a result of nonspecific factors. |
| Lu, 2011 [49] | US | Examine how PS variables predicted use of an online health consultation service and how use affected those same variables. | Pre-post examination of consultation services among low-income breast cancer patients below 250% poverty level (n = 231). | Online health consultation positively associated with three variables: health self-efficacy, participation in health care, and doctor–patient relationship. No significant relationships with information seeking and perceived social support variables. | Online health consultation complements other resources and increases confidence to participate in health care. |
| Marshall, 2011 [50] | US | Identify specific PS intervention needs of co-survivors. | Interviews with co-survivors on PS impacts (n = 16). | Themes: family stress, coping, need for financial help, and reliance on faith. Tailoring intervention to family needs and delivering it in accessible ways. | Outreach and engagement with various populations impacted by cancer, including co-survivors is important. |
| Meraviglia, 2011 [51] | US | Explore health-promoting behaviors of low-income cancer survivors. | Surveys with cancer patients from an urban cancer clinic (n = 51). | Health-promoting behaviors: walking, positive mental attitude, dietary changes, spiritual growth through prayer. Participants interested in learning about effective exercise, diet, and stress management. | Low-income cancer survivors engage in various health-promoting behaviors and want to learn strategies to use after treatment. |
| Moadel, 2007 [52] | US | Describe the development of a PS needs survey and patterns/predictors of need. | Survey with ethnically diverse underserved cancer patient population in Bronx, NY, US (n = 248). | Racial-ethnic minority cancer survivors have greater need for various PS supports: Informational; Practical (e.g., finances, transportation); Supportive (e.g., emotional/coping support); Spiritual (e.g., finding meaning/hope and spiritual resources). | There is a need to determine what interventions are most effective to address the informational, emotional, practical, and spiritual needs of these patients. |
| Mosavel, 2011 [53] | US | Identify the needs of low-income, African American cancer survivors in an urban setting. | Interviews/surveys with cancer survivors (n = 12), CGs (n = 10), professionals (n = 10); town halls (n = 80). | Participants identified practical needs (e.g., transportation, financial), lifestyle information, post treatment plan, and social support. The ideal resource would be located within the survivor’s neighborhood and provide medical support and recreational services. | Accrual of minorities in clinical cancer trials, attitudes/beliefs about cancer, and participation in research are issues that may be addressed by cancer resource centers within minority communities. |
| Wells, 2013 [54] | US | Explore patient perspectives about depression treatment. | Interviews with Latina cancer survivors in a depression treatment program (n = 30). | Treatment barriers: (a) barriers to treatment; (b) disease features; (c) treatment regimens; (d) provider–patient relationship; and (e) clinical setting. Completers more motivated and satisfied with treatment. | Need for educational approaches to address negative perception of antidepressants. Intensive case management useful. |
| Food insecurity (FI) and financial toxicity | |||||
| Fenn, 2014 [55] | US | Examine association between financial problems and reported HRQOL in a population-based sample of cancer patients. | Survey with secondary analysis of cancer survivors using NHIS data oversampling in minority population (n = 2108). | Degree to which cancer caused financial issues was the strongest predictor of HRQOL. Patients who reported that cancer caused “a lot” of financial problems were four times less likely to rate HRQOL as at least “good”. Lack of insurance is associated with the degree of cancer-related financial problems. | There is a need to give more attention to the economic burden of cancer and the impact on a patient’s overall well-being. |
| Gany, 2015 [56] | US | Examine predictors of us of a novel emergency food system at 5 clinics. | Survey with patients who visited hospital pantries in New York, NY, US (n = 351). | Younger patients used pantry less. Immigrant (non US-born), prostate cancer, and Stage IV cancer patients used the pantry more. | Cancer patients most at risk (e.g., immigrants, later stage cancers) need to be considered in the development of interventions to address FI. |
| Gany, 2015 [57] | US | Determine the relationship between FI and HRQOL. | Survey with ethnic minority cancer patients (n = 1390). | 41.8% food secure, 41.1% with low food security, 17.1% very low food security. HRQOL decreased with food security level. Inverse relationship: physical, functional, social, emotional well-being with FI. | Minority cancer survivors at higher risk for FI and suffer lower HRQOL. Services to support food security among these survivors are needed. |
| Kale, 2016 [58] | US | Determine prevalence and assess predictors of cancer-related financial burden and HRQOL. | Survey with a national panel involving multiple agencies surveying cancer survivors. (n = 1380). | 28.7% reported financial burden. Physical/mental HRQOL were lower for those with financial burden than those without. Survivors with financial burden had lower HRQOL, increased depression, and increased worry about cancer recurrence. | Future research should assess the role of value-based reimbursement, clinical practice guidelines, and physician-patient communication regarding reducing the cost of cancer care to help improve HRQOL. |
| Lathan, 2016 [59] | US | Measure association between financial strain, symptom burden, and HRQOL. | Survey with patients 5 Veterans Health Associations (n = 208). | Patients with lung (40%) and colorectal cancer (33%) reported limited financial reserves (≤2 months). Dose-response relationship was present across all measures of well-being with decreasing financial reserves. | Evaluation of financial strain could be performed by social workers, nurses, or physicians. |
| Meraviglia, 2015 [60] | US | Determine the feasibility of a health-promoting intervention. | Survey with low-income cancer survivors (n = 51). | >50% engaged in health-promoting behaviors (e.g., unusual symptoms, questioning health professionals, inspecting bodies for physical changes). Greater education related to health-promoting behaviors. | There is a need to understand the use of health-promoting behaviors and feasibility of interventions after treatment. |
| Nekhlyud, 2011 [61] | US | Compare cost-related medication nonadherence. | Survey with cancer survivors >65 (n = 9818). | Survivors who reported cost-related medication nonadherence tended to have lower income, be African-American, and have non-employer-based medication insurance. | Elderly Medicare cancer survivors may not face a greater perceived burden of medication costs than their peers. |
| Nipp, 2016 [62] | US | Describe patients at highest risk for using strategies to cope with treatment-related costs. | Survey with cancer survivors utilizing financial assistance from a non-profit organization (n = 174). | Younger patients more likely to use coping strategies. Strategies: spending less on leisure activities/basics, borrowing money, spending savings, not filling a prescription, and taking less medication than prescribed. Higher more education and shorter duration of chemotherapy used lifestyle-altering strategies more. | Qualitative assessments may help to better understand cancer survivors’ unique perspectives about financial burden. |
| Simmons, 2006 [63] | US | Examine the construct and correlates of FI in a sample of cancer patients. | Survey with patients at a university cancer clinic in Kentucky (n = 115). | FI rates higher than the general pop (25%). Patients with FI had greater nutritional risk, depression, financial strain, and lower HRQOL. 55% of FI patients did not take a prescribed medication because they could not afford it, versus 12.8% of food secure patients. | Understanding factors (including food insecurity) that may be associated with patient noncompliance is an important element of oncology care. |
| Yabroff, 2016 [64] | US | Estimate the prevalence of financial hardship associated with cancer. | Survey with cancer survivor’s data from the Medical Expenditure Panel Survey (n = 565). | Material psychological financial hardship greater among 18–64 than >65 years of age. Younger, female, nonwhite, treated recently, and changed employment because of cancer more likely to report financial hardship. | Further exploration on the financial hardship associated with cancer treatment as the health insurance landscape changes is needed. |
| Zafar, 2013 [65] | US | Describe experiences of patients using copayment assistance and the impact on well-being and treatment. | Surveys (pre and post) with patients that utilized a national copayment assistance foundation (n = 245). | Coping strategies: copayment assistance, reduced spending on food/clothing/leisure, used savings, partially filled prescriptions, avoided filling prescriptions. Greater financial burden associated with: younger age, larger household size, applying for copayment assistance, and communicating with physicians about costs. | Health insurance does not eliminate financial distress or health disparities among cancer patients. Financial distress as a result of disease or treatment decisions might be considered. |
| Zafar, 2014 [66] | US | Describe financial burden, disease status, HRQOL, comorbidities, and quality of care. | Survey from a large cohort of cancer survivors (n = 1000). | 48% reported difficulties living on their household income. Financial burden associated with lower household income, younger age, and poorer HRQOL. Better HRQOL was associated with fewer perceptions of poorer quality of care. | Financial burden is prevalent among survivors and associated with HRQOL. Need for interventions to improve patient education and engagement with regard to financial burden. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Parks, C.A.; Carpenter, L.R.; Sullivan, K.R.; Clausen, W.; Gargano, T.; Wiedt, T.L.; Doyle, C.; Kashima, K.; Yaroch, A.L. A Scoping Review of Food Insecurity and Related Factors among Cancer Survivors. Nutrients 2022, 14, 2723. https://doi.org/10.3390/nu14132723
Parks CA, Carpenter LR, Sullivan KR, Clausen W, Gargano T, Wiedt TL, Doyle C, Kashima K, Yaroch AL. A Scoping Review of Food Insecurity and Related Factors among Cancer Survivors. Nutrients. 2022; 14(13):2723. https://doi.org/10.3390/nu14132723
Chicago/Turabian StyleParks, Courtney A., Leah R. Carpenter, Kristen R. Sullivan, Whitney Clausen, Tony Gargano, Tracy L. Wiedt, Colleen Doyle, Kanako Kashima, and Amy L. Yaroch. 2022. "A Scoping Review of Food Insecurity and Related Factors among Cancer Survivors" Nutrients 14, no. 13: 2723. https://doi.org/10.3390/nu14132723
APA StyleParks, C. A., Carpenter, L. R., Sullivan, K. R., Clausen, W., Gargano, T., Wiedt, T. L., Doyle, C., Kashima, K., & Yaroch, A. L. (2022). A Scoping Review of Food Insecurity and Related Factors among Cancer Survivors. Nutrients, 14(13), 2723. https://doi.org/10.3390/nu14132723






