Study Protocol for a Randomised Controlled Trial Investigating the Effects of Maternal Prebiotic Fibre Dietary Supplementation from Mid-Pregnancy to Six Months’ Post-Partum on Child Allergic Disease Outcomes
Abstract
:1. Introduction
2. Trial Population and Methods
2.1. Trial Design and Ethical Approvals
2.2. Participant Eligibility
2.3. Recruitment
2.4. Randomisation and Allocation to Treatment Groups
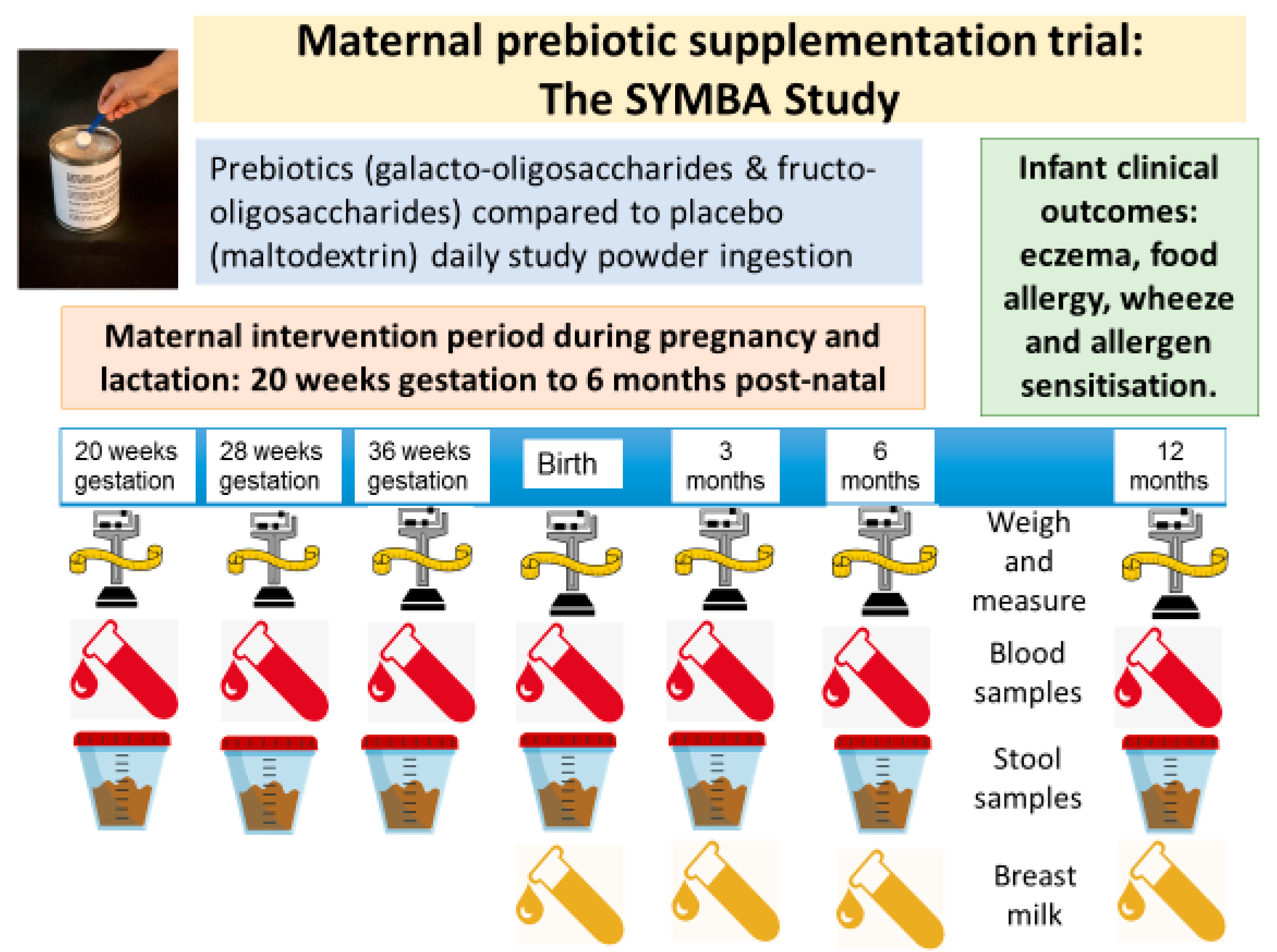
2.5. Interventions
- The prebiotics (intervention) group: women are asked to consume 14.2 g per day of prebiotic powder (Galacto-oligosaccharides (GOS) and Fructo-oligosaccharides (FOS) ratio 9:1) from <21 weeks gestation until 6 months’ postnatal infant age;
- The maltodextrin (control) group: women are asked to consume 8.7 g per day of maltodextrin powder from <21 weeks gestation until 6 months’ postnatal infant age.
2.6. Intervention Duration
2.7. Blinding
2.8. Monitoring Adherence to Study Powder Ingestion
2.9. Trial Outcomes
- Infant medically diagnosed IgE-mediated food allergies by 1 year of age.
- Infant medically diagnosed recurrent wheeze by 1 year of age.
- Infant allergic sensitisation to food and environmental allergens at 1 year of age.
- Maternal and infant skin barrier permeability at 36 weeks (maternal only), 3–4 and 6 months post-natal, and at 1 year of age (infant only).
- Maternal weight gain during the pregnancy and lactation intervention period, gestational length, and pregnancy complications (including gestational diabetes mellitus, pre-eclampsia and gestational hypertension).
- Infant birth anthropometrics and body composition.
- Infant weight gain and growth during infancy.
- The secondary laboratory outcomes are:
- Maternal immune responses at 20, 28 and 36 weeks of gestation.
- Maternal gut microflora colonisation patterns and stool short-chain fatty acid levels and composition during the pregnancy and lactation intervention period.
- Infant gut microflora colonisation patterns and stool short-chain fatty acid profiles at 2, 3–4, 6 and 12 months of age.
- Infant immune responses at birth, 3–4, 6 and 12 months of age.
- Breast milk composition and immune components at 2, 3–4, 6 and 12 months of age.
2.10. Clinical Outcome Definitions and Clinical Assessment Methods
2.10.1. Infant Medically Diagnosed Eczema
2.10.2. Infant Medically Diagnosed Recurrent Wheeze
2.10.3. Infant Allergen Sensitisation
2.10.4. Infant IgE-Mediated Food Allergy
2.10.5. Skin Barrier Permeability
2.10.6. Body Composition
2.11. Laboratory Outcomes Assessment Methods
2.11.1. Blood Samples
2.11.2. Stool Samples
2.11.3. Breast Milk Samples
2.12. Study Timeline
2.13. Serious Adverse Event Monitoring
2.14. Data Collection and Management
2.15. Sample Size
2.16. Statistical Analysis
2.17. Current Trial Status
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Osborne, N.J.; Koplin, J.J.; Martin, P.E.; Gurrin, L.C.; Lowe, A.J.; Matheson, M.C.; Ponsonby, A.L.; Wake, M.; Tang, M.L.; Dharmage, S.C.; et al. Prevalence of challenge-proven IgE-mediated food allergy using population-based sampling and predetermined challenge criteria in infants. J. Allergy Clin. Immunol. 2011, 127, 668–676. [Google Scholar] [CrossRef] [PubMed]
- David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Button, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A.; et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leeming, E.R.; Johnson, A.J.; Spector, T.D.; Le Roy, C.I. Effect of Diet on the Gut Microbiota: Rethinking Intervention Duration. Nutrients 2019, 11, 2862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gill, P.A.; Inniss, S.; Kumagai, T.; Rahman, F.Z.; Smith, A.M. The Role of Diet and Gut Microbiota in Regulating Gastrointestinal and Inflammatory Disease. Front. Immunol. 2022, 13, 866059. [Google Scholar] [CrossRef] [PubMed]
- Gibson, G.R.; Hutkins, R.; Sanders, M.E.; Prescott, S.L.; Reimer, R.A.; Salminen, S.J.; Scott, K.; Stanton, C.; Swanson, K.S.; Cani, P.D.; et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 491–502. [Google Scholar] [CrossRef] [Green Version]
- Maslowski, K.M.; Mackay, C.R. Diet, gut microbiota and immune responses. Nat. Immunol. 2011, 12, 5–9. [Google Scholar] [CrossRef]
- McKenzie, C.; Tan, J.; Macia, L.; Mackay, C.R. The nutrition-gut microbiome-physiology axis and allergic diseases. Immunol. Rev. 2017, 278, 277–295. [Google Scholar] [CrossRef]
- Halnes, I.; Baines, K.J.; Berthon, B.S.; MacDonald-Wicks, L.K.; Gibson, P.G.; Wood, L.G. Soluble Fibre Meal Challenge Reduces Airway Inflammation and Expression of GPR43 and GPR41 in Asthma. Nutrients 2017, 9, 57. [Google Scholar] [CrossRef] [Green Version]
- Tan, J.K.; McKenzie, C.; Mariño, E.; Macia, L.; Mackay, C.R. Metabolite-Sensing G Protein-Coupled Receptors-Facilitators of Diet-Related Immune Regulation. Annu. Rev. Immunol. 2017, 35, 371–402. [Google Scholar] [CrossRef]
- Thorburn, A.N.; McKenzie, C.I.; Shen, S.; Stanley, D.; Macia, L.; Mason, L.J.; Roberts, L.K.; Wong, C.H.Y.; Shim, R.; Robert, R.; et al. Evidence that asthma is a developmental origin disease influenced by maternal diet and bacterial metabolites. Nat. Commun. 2015, 6, 7320. [Google Scholar] [CrossRef]
- Brogdon, J.L.; Xu, Y.; Szabo, S.J.; An, S.; Buxton, F.; Cohen, D.; Huang, Q. Histone deacetylase activities are required for innate immune cell control of Th1 but not Th2 effector cell function. Blood 2007, 109, 1123–1130. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.; Kim, M.; Kang, S.G.; Jannasch, A.H.; Cooper, B.; Patterson, J.; Kim, C.H. Short-chain fatty acids induce both effector and regulatory T cells by suppression of histone deacetylases and regulation of the mTOR–S6K pathway. Mucosal Immunol. 2015, 8, 80–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martins, G.N.; Ureta, M.M.; Tymczyszyn, E.E.; Castilho, P.C.; Gomez-Zavaglia, A. Technological Aspects of the Production of Fructo and Galacto-Oligosaccharides. Enzymatic Synthesis and Hydrolysis. Front. Nutr. 2019, 6, 78. [Google Scholar] [CrossRef] [PubMed]
- Knol, J.; Scholtens, P.; Kafka, C.; Steenbakkers, J.; Gro, S.; Helm, K.; Klarczyk, M.; Schöpfer, H.; Böckler, H.M.; Wells, J. Colon microflora in infants fed formula with galacto- and fructo-oligosaccharides: More like breast-fed infants. J. Pediatr. Gastroenterol. Nutr. 2005, 40, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Moro, G.; Minoli, I.; Mosca, M.; Fanaro, S.; Jelinek, J.; Stahl, B.; Boehm, G. Dosage-related bifidogenic effects of galacto- and fructooligosaccharides in formula-fed term infants. J. Pediatr. Gastroenterol. Nutr. 2002, 34, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Schmelzle, H.; Wirth, S.; Skopnik, H.; Radke, M.; Knol, J.; Böckler, H.M.; Brönstrup, A.; Wells, J.; Fusch, C. Randomized double-blind study of the nutritional efficacy and bifidogenicity of a new infant formula containing partially hydrolyzed protein, a high beta-palmitic acid level, and nondigestible oligosaccharides. J. Pediatr. Gastroenterol. Nutr. 2003, 36, 343–351. [Google Scholar] [CrossRef]
- Veereman-Wauters, G.; Staelens, S.; Van de Broek, H.; Plaskie, K.; Wesling, F.; Roger, L.C.; McCartney, A.L.; Assam, P. Physiological and bifidogenic effects of prebiotic supplements in infant formulae. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 763–771. [Google Scholar] [CrossRef]
- Grüber, C.; van Stuijvenberg, M.; Mosca, F.; Moro, G.; Chirico, G.; Braegger, C.P.; Riedler, J.; Boehm, G.; Wahn, U. Reduced occurrence of early atopic dermatitis because of immunoactive prebiotics among low-atopy-risk infants. J. Allergy Clin. Immunol. 2010, 126, 791–797. [Google Scholar] [CrossRef]
- Moro, G.; Arslanoglu, S.; Stahl, B.; Jelinek, J.; Wahn, U.; Boehm, G. A mixture of prebiotic oligosaccharides reduces the incidence of atopic dermatitis during the first six months of age. Arch. Dis. Child. 2006, 91, 814–819. [Google Scholar] [CrossRef] [Green Version]
- Boyle, R.J.; Tang, M.L.; Chiang, W.C.; Chua, M.C.; Ismail, I.; Nauta, A.; Hourihane, J.O.B.; Smith, P.; Gold, M.; Ziegler, J.; et al. Prebiotic-supplemented partially hydrolysed cow’s milk formula for the prevention of eczema in high-risk infants: A randomized controlled trial. Allergy 2016, 71, 701–710. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Larsen, V.; Ierodiakonou, D.; Jarrold, K.; Cunha, S.; Chivinge, J.; Robinson, Z.; Geoghegan, N.; Ruparelia, A.; Devani, P.; Trivella, M.; et al. Diet during pregnancy and infancy and risk of allergic or autoimmune disease: A systematic review and meta-analysis. PLoS Med. 2018, 15, e1002507. [Google Scholar] [CrossRef] [PubMed]
- Jenmalm, M.C.; Duchén, K. Timing of allergy-preventive and immunomodulatory dietary interventions-are prenatal, perinatal or postnatal strategies optimal? Clin. Exp. Allergy 2013, 43, 273–278. [Google Scholar] [CrossRef]
- Rautava, S.; Luoto, R.; Salminen, S.; Isolauri, E. Microbial contact during pregnancy, intestinal colonization and human disease. Nat. Rev. Gastroenterol. Hepatol. 2012, 9, 565–576. [Google Scholar] [CrossRef] [PubMed]
- Renz, H.; Brandtzaeg, P.; Hornef, M. The impact of perinatal immune development on mucosal homeostasis and chronic inflammation. Nat. Rev. Immunol. 2011, 12, 9–23. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.C.; Miles, E.A.; Warner, J.O.; Colwell, B.M.; Bryant, T.N.; Warner, J.A. Fetal peripheral blood mononuclear cell proliferative responses to mitogenic and allergenic stimuli during gestation. Pediatr. Allergy Immunol. 1996, 7, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Martino, D.J.; Bosco, A.; McKenna, K.L.; Hollams, E.; Mok, D.; Holt, P.G.; Prescott, S.L. T-cell activation genes differentially expressed at birth in CD4+ T-cells from children who develop IgE food allergy. Allergy 2012, 67, 191–200. [Google Scholar] [CrossRef]
- Prescott, S.L.; Macaubas, C.; Holt, B.J.; Smallacombe, T.B.; Loh, R.; Sly, P.D.; Holt, P.G. Transplacental priming of the human immune system to environmental allergens: Universal skewing of initial T cell responses toward the Th2 cytokine profile. J. Immunol. 1998, 160, 4730–4737. [Google Scholar]
- Tulic, M.K.; Hodder, M.; Forsberg, A.; McCarthy, S.; Richman, T.; D’Vaz, N.; van den Biggelaar, A.H.; Thornton, C.A.; Prescott, S.L. Differences in innate immune function between allergic and nonallergic children: New insights into immune ontogeny. J. Allergy Clin. Immunol. 2011, 127, 470–478.e471. [Google Scholar] [CrossRef]
- Bouchaud, G.; Castan, L.; Chesné, J.; Braza, F.; Aubert, P.; Neunlist, M.; Magnan, A.; Bodinier, M. Maternal exposure to GOS/inulin mixture prevents food allergies and promotes tolerance in offspring in mice. Allergy 2016, 71, 68–76. [Google Scholar] [CrossRef]
- Brosseau, C.; Selle, A.; Duval, A.; Misme-Aucouturier, B.; Chesneau, M.; Brouard, S.; Cherbuy, C.; Cariou, V.; Bouchaud, G.; Mincham, K.T.; et al. Prebiotic Supplementation During Pregnancy Modifies the Gut Microbiota and Increases Metabolites in Amniotic Fluid, Driving a Tolerogenic Environment in Utero. Front. Immunol. 2021, 12, 712614. [Google Scholar] [CrossRef]
- Fujiwara, R.; Takemura, N.; Watanabe, J.; Sonoyama, K. Maternal consumption of fructo-oligosaccharide diminishes the severity of skin inflammation in offspring of NC/Nga mice. Br. J. Nutr. 2010, 103, 530–538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gourbeyre, P.; Desbuards, N.; Grémy, G.; Le Gall, S.; Champ, M.; Denery-Papini, S.; Bodinier, M. Exposure to a galactooligosaccharides/inulin prebiotic mix at different developmental time points differentially modulates immune responses in mice. J. Agric. Food Chem. 2012, 60, 11942–11951. [Google Scholar] [CrossRef] [PubMed]
- Hogenkamp, A.; Knippels, L.M.; Garssen, J.; van Esch, B.C. Supplementation of Mice with Specific Nondigestible Oligosaccharides during Pregnancy or Lactation Leads to Diminished Sensitization and Allergy in the Female Offspring. J. Nutr. 2015, 145, 996–1002. [Google Scholar] [CrossRef] [PubMed]
- Hogenkamp, A.; Thijssen, S.; van Vlies, N.; Garssen, J. Supplementing pregnant mice with a specific mixture of nondigestible oligosaccharides reduces symptoms of allergic asthma in male offspring. J. Nutr. 2015, 145, 640–646. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Selle, A.; Brosseau, C.; Dijk, W.; Duval, A.; Bouchaud, G.; Rousseaux, A.; Bruneau, A.; Cherbuy, C.; Mariadassou, M.; Cariou, V.; et al. Prebiotic Supplementation During Gestation Induces a Tolerogenic Environment and a Protective Microbiota in Offspring Mitigating Food Allergy. Front. Immunol. 2022, 12, 745535. [Google Scholar] [CrossRef] [PubMed]
- van Vlies, N.; Hogenkamp, A.; Thijssen, S.; Dingjan, G.M.; Knipping, K.; Garssen, J.; Knippels, L.M.J. Effects of short-chain galacto- and long-chain fructo-oligosaccharides on systemic and local immune status during pregnancy. J. Reprod. Immunol. 2012, 94, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Jinno, S.; Toshimitsu, T.; Nakamura, Y.; Kubota, T.; Igoshi, Y.; Ozawa, N.; Suzuki, S.; Nakano, T.; Morita, Y.; Arima, T.; et al. Maternal Prebiotic Ingestion Increased the Number of Fecal Bifidobacteria in Pregnant Women but Not in Their Neonates Aged One Month. Nutrients 2017, 9, 196. [Google Scholar] [CrossRef] [PubMed]
- Shadid, R.; Haarman, M.; Knol, J.; Theis, W.; Beermann, C.; Rjosk-Dendorfer, D.; Schendel, D.J.; Koletzko, B.V.; Krauss-Etschmann, S. Effects of galactooligosaccharide and long-chain fructooligosaccharide supplementation during pregnancy on maternal and neonatal microbiota and immunity-a randomized, double-blind, placebo-controlled study. Am. J. Clin. Nutr. 2007, 86, 1426–1437. [Google Scholar] [CrossRef]
- Silva, D.T.; Hagemann, E.; Davis, J.A.; Gibson, L.Y.; Srinivasjois, R.; Palmer, D.J.; Colvin, L.; Tan, J.; Prescott, S.L. Introducing the ORIGINS project: A community-based interventional birth cohort. Rev. Environ. Health 2020, 35, 281–293. [Google Scholar] [CrossRef]
- Noakes, P.S.; Holt, P.G.; Prescott, S.L. Maternal smoking in pregnancy alters neonatal cytokine responses. Allergy 2003, 58, 1053–1058. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef] [PubMed]
- Hanifin, J.M.; Rajka, G. Diagnostic features of atopic dermatitis. Acta Derm. Venereol. 1980, 92, 44–47. [Google Scholar]
- Kunz, B.; Oranje, A.P.; Labreze, L.; Stalder, J.-F.; Ring, J.; Taieb, A. Clinical validation and guidelines for the SCORAD index: Consensus report, of the European Task Force on Atopic Dermatitis. Dermatology 1997, 195, 10–19. [Google Scholar] [CrossRef] [PubMed]
- D’Vaz, N.; Meldrum, S.J.; Dunstan, J.A.; Martino, D.; McCarthy, S.; Metcalfe, J.; Tulic, M.K.; Mori, T.A.; Prescott, S.L. Postnatal fish oil supplementation in high-risk infants to prevent allergy: Randomized controlled trial. Pediatrics 2012, 130, 674–682. [Google Scholar] [CrossRef] [Green Version]
- Palmer, D.J.; Sullivan, T.; Gold, M.S.; Prescott, S.L.; Heddle, R.; Gibson, R.A.; Makrides, M. Effect of n-3 long chain polyunsaturated fatty acid supplementation in pregnancy on infants’ allergies in first year of life: Randomised controlled trial. BMJ 2012, 344, e184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rautava, S.; Kainonen, E.; Salminen, S.; Isolauri, E. Maternal probiotic supplementation during pregnancy and breast-feeding reduces the risk of eczema in the infant. J. Allergy Clin. Immunol. 2012, 130, 1355–1360. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palmer, D.J.; Keelan, J.; Garssen, J.; Simmer, K.; Jenmalm, M.C.; Srinivasjois, R.; Silva, D.; Prescott, S.L. Study Protocol for a Randomised Controlled Trial Investigating the Effects of Maternal Prebiotic Fibre Dietary Supplementation from Mid-Pregnancy to Six Months’ Post-Partum on Child Allergic Disease Outcomes. Nutrients 2022, 14, 2753. https://doi.org/10.3390/nu14132753
Palmer DJ, Keelan J, Garssen J, Simmer K, Jenmalm MC, Srinivasjois R, Silva D, Prescott SL. Study Protocol for a Randomised Controlled Trial Investigating the Effects of Maternal Prebiotic Fibre Dietary Supplementation from Mid-Pregnancy to Six Months’ Post-Partum on Child Allergic Disease Outcomes. Nutrients. 2022; 14(13):2753. https://doi.org/10.3390/nu14132753
Chicago/Turabian StylePalmer, Debra J., Jeffrey Keelan, Johan Garssen, Karen Simmer, Maria C. Jenmalm, Ravisha Srinivasjois, Desiree Silva, and Susan L. Prescott. 2022. "Study Protocol for a Randomised Controlled Trial Investigating the Effects of Maternal Prebiotic Fibre Dietary Supplementation from Mid-Pregnancy to Six Months’ Post-Partum on Child Allergic Disease Outcomes" Nutrients 14, no. 13: 2753. https://doi.org/10.3390/nu14132753
APA StylePalmer, D. J., Keelan, J., Garssen, J., Simmer, K., Jenmalm, M. C., Srinivasjois, R., Silva, D., & Prescott, S. L. (2022). Study Protocol for a Randomised Controlled Trial Investigating the Effects of Maternal Prebiotic Fibre Dietary Supplementation from Mid-Pregnancy to Six Months’ Post-Partum on Child Allergic Disease Outcomes. Nutrients, 14(13), 2753. https://doi.org/10.3390/nu14132753






