The Effect of Diet and Exercise Interventions on Body Composition in Liver Cirrhosis: A Systematic Review
Abstract
1. Introduction
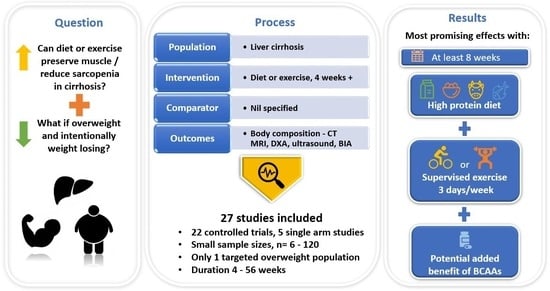
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Strategy
2.3. Data Extraction
2.4. Quality Assessment
2.5. Data Synthesis
3. Results
3.1. Characteristics of Studies
3.2. Quality Assessment
3.3. Outcomes for Combined Diet and Exercise Intervention Studies
3.4. Outcomes for Diet-Only Intervention Studies
3.5. Outcomes for Exercise-Only Interventions
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moon, A.M.; Singal, A.G.; Tapper, E.B. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin. Gastroenterol. Hepatol. 2020, 18, 2650–2666. [Google Scholar] [CrossRef] [PubMed]
- D’Amico, G.; Garcia-Tsao, G.; Pagliaro, L. Natural history and prognostic indicators of survival in cirrhosis: A systematic review of 118 studies. J. Hepatol. 2006, 44, 217–231. [Google Scholar] [CrossRef]
- Cheung, K.; Lee, S.S.; Raman, M. Prevalence and mechanisms of malnutrition in patients with advanced liver disease, and nutrition management strategies. Clin. Gastroenterol. Hepatol. 2012, 10, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Bhanji, R.A.; Carey, E.J.; Yang, L.; Watt, K.D. The long winding road to transplant: How sarcopenia and debility impact morbidity and mortality on the waitlist. Clin. Gastroenterol. Hepatol. 2017, 15, 1492–1497. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, M.; Poltavskiy, E.; Dodge, J.L.; Lai, J.C. Frailty is independently associated with increased hospitalisation days in patients on the liver transplant waitlist. World J. Gastroenterol. 2017, 23, 899. [Google Scholar] [CrossRef]
- Tandon, P.; Montano-Loza, A.J.; Lai, J.C.; Dasarathy, S.; Merli, M. Sarcopenia and frailty in decompensated cirrhosis. J. Hepatol. 2021, 75, S147–S162. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosisReport of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Laube, R.; Wang, H.; Park, L.; Heyman, J.K.; Vidot, H.; Majumdar, A.; Strasser, S.I.; McCaughan, G.W.; Liu, K. Frailty in advanced liver disease. Liver Int. 2018, 38, 2117–2128. [Google Scholar] [CrossRef]
- Kim, G.; Kang, S.H.; Kim, M.Y.; Baik, S.K. Prognostic value of sarcopenia in patients with liver cirrhosis: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0186990. [Google Scholar] [CrossRef]
- Van Vugt, J.; Levolger, S.; de Bruin, R.; van Rosmalen, J.; Metselaar, H.; IJzermans, J. Systematic review and meta-analysis of the impact of computed tomography–assessed skeletal muscle mass on outcome in patients awaiting or undergoing liver transplantation. Am. J. Transplant. 2016, 16, 2277–2292. [Google Scholar] [CrossRef]
- Berzigotti, A.; Garcia-Tsao, G.; Bosch, J.; Grace, N.D.; Burroughs, A.K.; Morillas, R.; Escorsell, A.; Garcia-Pagan, J.C.; Patch, D.; Matloff, D.S. Obesity is an independent risk factor for clinical decompensation in patients with cirrhosis. Hepatology 2011, 54, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Montano-Loza, A.J.; Angulo, P.; Meza-Junco, J.; Prado, C.M.; Sawyer, M.B.; Beaumont, C.; Esfandiari, N.; Ma, M.; Baracos, V.E. Sarcopenic obesity and myosteatosis are associated with higher mortality in patients with cirrhosis. J. Cachexia Sarcopenia Muscle 2016, 7, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Spengler, E.K.; O’Leary, J.G.; Te, H.S.; Rogal, S.; Pillai, A.A.; Al-Osaimi, A.; Desai, A.; Fleming, J.N.; Ganger, D.; Seetharam, A.; et al. Liver Transplantation in the Obese Cirrhotic Patient. Transplantation 2017, 101, 2288–2296. [Google Scholar] [CrossRef] [PubMed]
- Vidot, H.; Kline, K.; Cheng, R.; Finegan, L.; Lin, A.; Kempler, E.; Strasser, S.I.; Bowen, D.G.; McCaughan, G.W.; Carey, S. The relationship of obesity, nutritional status and muscle wasting in patients assessed for liver transplantation. Nutrients 2019, 11, 2097. [Google Scholar] [CrossRef]
- Calzadilla-Bertot, L.; Jeffrey, G.P.; Jacques, B.; McCaughan, G.; Crawford, M.; Angus, P.; Jones, R.; Gane, E.; Munn, S.; Macdonald, G. Increasing incidence of nonalcoholic steatohepatitis as an indication for liver transplantation in Australia and New Zealand. Liver Transpl. 2019, 25, 25–34. [Google Scholar] [CrossRef]
- Plauth, M.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Bischoff, S.C. European Society of Enteral and Parenteral Nutrition Guideline on Clinical Nutrition in Liver Disease. Clin. Nutr. 2019, 38, 485–521. [Google Scholar] [CrossRef]
- Morgan, M.Y.; Madden, A.M.; Soulsby, C.T.; Morris, R.W. Derivation and validation of a new global method for assessing nutritional status in patients with cirrhosis. Hepatology 2006, 44, 823–835. [Google Scholar] [CrossRef]
- Ulijaszek, S.J.; Kerr, D.A. Anthropometric measurement error and the assessment of nutritional status. Br. J. Nutr. 1999, 82, 165–177. [Google Scholar] [CrossRef]
- European Association for the Study of the Liver. EASL Clinical Practice Guidelines on nutrition in chronic liver disease. J. Hepatol. 2019, 70, 172–193. [Google Scholar] [CrossRef]
- Sinclair, M.; Hoermann, R.; Peterson, A.; Testro, A.; Angus, P.W.; Hey, P.; Chapman, B.; Gow, P.J. Use of dual X-ray absorptiometry in men with advanced cirrhosis to predict sarcopenia-associated mortality risk. Liver Int. 2019, 39, 1089–1097. [Google Scholar] [CrossRef]
- Morgan, M.Y.; Madden, A.M.; Jennings, G.; Elia, M.; Fuller, N.J. Two-component models are of limited value for the assessment of body composition in patients with cirrhosis. Am. J. Clin. Nutr. 2006, 84, 1151–1162. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bowen, T.S.; Schuler, G.; Adams, V. Skeletal muscle wasting in cachexia and sarcopenia: Molecular pathophysiology and impact of exercise training. J. Cachexia Sarcopenia Muscle 2015, 6, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Williams, F.R.; Berzigotti, A.; Lord, J.M.; Lai, J.C.; Armstrong, M.J. Impact of exercise on physical frailty in patients with chronic liver disease. Aliment. Pharmacol. Ther. 2019, 50, 988–1000. [Google Scholar] [CrossRef] [PubMed]
- Toshikuni, N.; Arisawa, T.; Tsutsumi, M. Nutrition and exercise in the management of liver cirrhosis. World J. Gastroenterol. 2014, 20, 7286–7297. [Google Scholar] [CrossRef] [PubMed]
- Ooi, P.H.; Gilmour, S.M.; Yap, J.; Mager, D.R. Effects of branched chain amino acid supplementation on patient care outcomes in adults and children with liver cirrhosis: A systematic review. Clin. Nutr. ESPEN 2018, 28, 41–51. [Google Scholar] [CrossRef]
- Lai, J.C.; Tandon, P.; Bernal, W.; Tapper, E.B.; Ekong, U.; Dasarathy, S.; Carey, E.J. Malnutrition, Frailty, and Sarcopenia in Patients With Cirrhosis: 2021 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 2021, 74, 1611–1644. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- The EndNote Team. EndNote; Endnote X9; Clarivate: Philadelphia, PA, USA, 2013. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Sterne, J.A.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; McAleenan, A.; Reeves, B.C.; Higgins, J.P. ROBINS-I: A tool for assessing risk of bias in non-randomized studies of interventions. BMJ. 2016, 355, i4919. [Google Scholar] [CrossRef]
- Berzigotti, A.; Albillos, A.; Villanueva, C.; Genescá, J.; Ardevol, A.; Augustín, S.; Calleja, J.L.; Bañares, R.; García-Pagán, J.C.; Mesonero, F. Effects of an intensive lifestyle intervention program on portal hypertension in patients with cirrhosis and obesity: The SportDiet study. Hepatology 2017, 65, 1293–1305. [Google Scholar] [CrossRef] [PubMed]
- Román, E.; Torrades, M.T.; Nadal, M.J.; Cárdenas, G.; Nieto, J.C.; Vidal, S.; Bascunana, H.; Juárez, C.; Guarner, C.; Córdoba, J. Randomized pilot study: Effects of an exercise programme and leucine supplementation in patients with cirrhosis. Dig. Dis. Sci. 2014, 59, 1966–1975. [Google Scholar] [CrossRef] [PubMed]
- Manguso, F.; D’ambra, G.; Menchise, A.; Sollazzo, R.; D’agostino, L. Effects of an appropriate oral diet on the nutritional status of patients with HCV-related liver cirrhosis: A prospective study. Clin. Nutr. 2005, 24, 751–759. [Google Scholar] [CrossRef] [PubMed]
- Zenith, L.; Meena, N.; Ramadi, A.; Yavari, M.; Harvey, A.; Carbonneau, M.; Ma, M.; Abraldes, J.G.; Paterson, I.; Haykowsky, M.J. Eight weeks of exercise training increases aerobic capacity and muscle mass and reduces fatigue in patients with cirrhosis. Clin. Gastroenterol. Hepatol. 2014, 12, 1920–1926.e2. [Google Scholar] [CrossRef]
- Macías-Rodríguez, R.U.; Ilarraza-Lomelí, H.; Ruiz-Margáin, A.; Ponce-de-León-Rosales, S.; Vargas-Vorácková, F.; García-Flores, O.; Torre, A.; Duarte-Rojo, A. Changes in hepatic venous pressure gradient induced by physical exercise in cirrhosis: Results of a pilot randomized open clinical trial. Clin. Transl. Gastroenterol. 2016, 7, e180. [Google Scholar] [CrossRef]
- Macías-Rodríguez, R.U.; Ruiz-Margáin, A.; Román-Calleja, B.M.; Espin-Nasser, M.E.; Flores-García, N.C.; Torre, A.; Galicia-Hernández, G.; Rios-Torres, S.L.; Fernández-del-Rivero, G.; Orea-Tejeda, A. Effect of non-alcoholic beer, diet and exercise on endothelial function, nutrition and quality of life in patients with cirrhosis. World J. Hepatol. 2020, 12, 1299. [Google Scholar] [CrossRef]
- Lattanzi, B.; Bruni, A.; Di Cola, S.; Molfino, A.; De Santis, A.; Muscaritoli, M.; Merli, M. The Effects of 12-Week Beta-Hydroxy-Beta-Methylbutyrate Supplementation in Patients with Liver Cirrhosis: Results from a Randomized Controlled Single-Blind Pilot Study. Nutrients 2021, 13, 2296. [Google Scholar] [CrossRef]
- Hernández-Conde, M.; Llop, E.; Gómez-Pimpollo, L.; Carrillo, C.F.; Rodríguez, L.; Van Den Brule, E.; Perelló, C.; López-Gómez, M.; Abad, J.; Martínez-Porras, J.L. Adding Branched-Chain Amino Acids to an Enhanced Standard-of-Care Treatment Improves Muscle Mass of Cirrhotic Patients With Sarcopenia: A Placebo-Controlled Trial. Off. J. Am. Coll. Gastroenterol. 2021, 116, 2241–2249. [Google Scholar] [CrossRef]
- Aamann, L.; Dam, G.; Borre, M.; Drljevic-Nielsen, A.; Overgaard, K.; Andersen, H.; Vilstrup, H.; Aagaard, N.K. Resistance training increases muscle strength and muscle size in patients with liver cirrhosis. Clin. Gastroenterol. Hepatol. 2019, 18, 1179–1187. [Google Scholar] [CrossRef]
- Román, E.; García-Galcerán, C.; Torrades, T.; Herrera, S.; Marín, A.; Doñate, M.; Alvarado-Tapias, E.; Malouf, J.; Nácher, L.; Serra-Grima, R. Effects of an exercise programme on functional capacity, body composition and risk of falls in patients with cirrhosis: A randomized clinical trial. PLoS ONE 2016, 11, e0151652. [Google Scholar] [CrossRef]
- Schmidt, N.P.; Fernandes, S.A.; Silveira, A.T.; Rayn, R.G.; Henz, A.C.; Rossi, D.; Galant, L.H.; Marroni, C.A. Nutritional and functional rehabilitation in cirrhotic patients. J. Gastroenterol. Hepatol. Res. 2021, 10, 3470–3477. [Google Scholar]
- Morkane, C.M.; Kearney, O.; Bruce, D.A.; Melikian, C.N.; Martin, D.S. An outpatient hospital-based exercise training program for patients with cirrhotic liver disease awaiting transplantation: A feasibility trial. Transplantation 2020, 104, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.W.; Ferrando, A.; White, M.G.; Dennis, R.A.; Xie, J.; Pauly, M.; Park, S.; Bartter, T.; Dunn, M.A.; Ruiz-Margain, A. Home-Based Physical Activity and Diet Intervention to Improve Physical Function in Advanced Liver Disease: A Randomized Pilot Trial. Dig. Dis. Sci. 2020, 65, 3350–3359. [Google Scholar] [CrossRef] [PubMed]
- Dupont, B.; Dao, T.; Joubert, C.; Dupont-Lucas, C.; Gloro, R.; Nguyen-Khac, E.; Beaujard, E.; Mathurin, P.; Vastel, E.; Musikas, M. Randomised clinical trial: Enteral nutrition does not improve the long-term outcome of alcoholic cirrhotic patients with jaundice. Aliment. Pharmacol. Ther. 2012, 35, 1166–1174. [Google Scholar] [CrossRef]
- Debette-Gratien, M.; Tabouret, T.; Antonini, M.-T.; Dalmay, F.; Carrier, P.; Legros, R.; Jacques, J.; Vincent, F.; Sautereau, D.; Samuel, D. Personalized adapted physical activity before liver transplantation: Acceptability and results. Transplantation 2015, 99, 145–150. [Google Scholar] [CrossRef]
- Kruger, C.; McNeely, M.L.; Bailey, R.J.; Yavari, M.; Abraldes, J.G.; Carbonneau, M.; Newnham, K.; DenHeyer, V.; Ma, M.; Thompson, R. Home exercise training improves exercise capacity in cirrhosis patients: Role of exercise adherence. Sci. Rep. 2018, 8, 99. [Google Scholar] [CrossRef]
- Les, I.; Doval, E.; García-Martínez, R.; Planas, M.; Cárdenas, G.; Gómez, P.; Flavià, M.; Jacas, C.; Mínguez, B.; Vergara, M. Effects of branched-chain amino acids supplementation in patients with cirrhosis and a previous episode of hepatic encephalopathy: A randomized study. Off. J. Am. Coll. Gastroenterol. 2011, 106, 1081–1088. [Google Scholar] [CrossRef]
- Okabayashi, T.; Nishimori, I.; Sugimoto, T.; Iwasaki, S.; Akisawa, N.; Maeda, H.; Ito, S.; Onishi, S.; Ogawa, Y.; Kobayashi, M. The benefit of the supplementation of perioperative branched-chain amino acids in patients with surgical management for hepatocellular carcinoma: A preliminary study. Dig. Dis. Sci. 2008, 53, 204–209. [Google Scholar] [CrossRef]
- Poon, R.P.; Yu, W.C.; Fan, S.T.; Wong, J. Long-term oral branched chain amino acids in patients undergoing chemoembolization for hepatocellular carcinoma: A randomized trial. Aliment. Pharmacol. Ther. 2004, 19, 779–788. [Google Scholar] [CrossRef]
- Sorrentino, P.; Castaldo, G.; Tarantino, L.; Bracigliano, A.; Perrella, A.; Perrella, O.; Fiorentino, F.; Vecchione, R.; D’Angelo, S. Preservation of nutritional-status in patients with refractory ascites due to hepatic cirrhosis who are undergoing repeated paracentesis. J. Gastroenterol. Hepatol. 2012, 27, 813–822. [Google Scholar] [CrossRef]
- Hiraoka, A.; Michitaka, K.; Kiguchi, D.; Izumoto, H.; Ueki, H.; Kaneto, M.; Kitahata, S.; Aibiki, T.; Okudaira, T.; Tomida, H. Efficacy of branched-chain amino acid supplementation and walking exercise for preventing sarcopenia in patients with liver cirrhosis. Eur. J. Gastroenterol. Hepatol. 2017, 29, 1416–1423. [Google Scholar] [CrossRef] [PubMed]
- Nishida, Y.; Ide, Y.; Okada, M.; Otsuka, T.; Eguchi, Y.; Ozaki, I.; Tanaka, K.; Mizuta, T. Effects of home-based exercise and branched-chain amino acid supplementation on aerobic capacity and glycemic control in patients with cirrhosis. Hepatol. Res. 2017, 47, E193–E200. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, S.; Bunout, D.; De La Maza, P.; Iturriaga, H.; Petermann, M.; Icazar, G.; Gattas, V.; Ugarte, G. Controlled trial on nutrition supplementation in outpatients with symptomatic alcoholic cirrhosis. J. Parenter. Enter. Nutr. 1993, 17, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Le Cornu, K.A.; McKiernan, F.J.; Kapadia, S.A.; Neuberger, J.M. A prospective randomized study of preoperative nutritional supplementation in patients awaiting elective Orthotopic liver Transplantation. Transplantation 2000, 69, 1364–1369. [Google Scholar] [CrossRef]
- Okabayashi, T.; Iyoki, M.; Sugimoto, T.; Kobayashi, M.; Hanazaki, K. Oral supplementation with carbohydrate-and branched-chain amino acid-enriched nutrients improves postoperative quality of life in patients undergoing hepatic resection. Amino Acids 2011, 40, 1213–1220. [Google Scholar] [CrossRef]
- Tangkijvanich, P.; Mahachai, V.; Wittayalertpanya, S.; Ariyawongsopon, V.; Isarasena, S. Short-term effects of branched-chain amino acids on liver function tests in cirrhotic patients. Southeast Asian J. Trop. Med. Public Health 2000, 31, 152–157. [Google Scholar]
- Putadechakum, S.; Klangjareonchai, T.; Soponsaritsuk, A.; Roongpisuthipong, C. Nutritional status assessment in cirrhotic patients after protein supplementation. Int. Sch. Res. Not. 2012, 2012, 690402. [Google Scholar] [CrossRef]
- Kitajima, Y.; Takahashi, H.; Akiyama, T.; Murayama, K.; Iwane, S.; Kuwashiro, T.; Tanaka, K.; Kawazoe, S.; Ono, N.; Eguchi, T. Supplementation with branched-chain amino acids ameliorates hypoalbuminemia, prevents sarcopenia, and reduces fat accumulation in the skeletal muscles of patients with liver cirrhosis. J. Gastroenterol. 2018, 53, 427–437. [Google Scholar] [CrossRef]
- Pugh, R.; Murray-Lyon, I.; Dawson, J.; Pietroni, M.; Williams, R. Transection of the oesophagus for bleeding oesophageal varices. J. Br. Surg. 1973, 60, 646–649. [Google Scholar] [CrossRef]
- Molina Raya, A.; García Navarro, A.; San Miguel Méndez, C.; Domínguez Bastante, M.; Villegas Herrera, M.T.; Granero, K.; Becerra Massare, A.; Villar Del Moral, J.M.; Expósito, M.; Fundora Suárez, Y. Influence of Obesity on Liver Transplantation Outcomes. Transplant. Proc. 2016, 48, 2503–2505. [Google Scholar] [CrossRef]
- Johnston, H.E.; de Crom, T.; Hargrave, C.; Adhyaru, P.; Woodward, A.J.; Pang, S.; Ali, A.; Coombes, J.S.; Keating, S.E.; McLean, K. The inter-and intrarater reliability and feasibility of dietetic assessment of sarcopenia and frailty in potential liver transplant recipients: A mixed-methods study. Clin. Transplant. 2021, 35, e14185. [Google Scholar] [CrossRef]
- Georgiou, A.; Papatheodoridis, G.V.; Alexopoulou, A.; Deutsch, M.; Vlachogiannakos, I.; Ioannidou, P.; Papageorgiou, M.-V.; Papadopoulos, N.; Yannakoulia, M.; Kontogianni, M.D. Validation of cutoffs for skeletal muscle mass index based on computed tomography analysis against dual energy X-ray absorptiometry in patients with cirrhosis: The KIRRHOS study. Ann. Gastroenterol. 2020, 33, 80. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Margáin, A.; Xie, J.J.; Román-Calleja, B.M.; Pauly, M.; White, M.G.; Chapa-Ibargüengoitia, M.; Campos-Murguía, A.; González-Regueiro, J.A.; Macias-Rodríguez, R.U.; Duarte-Rojo, A. Phase Angle From Bioelectrical Impedance for the Assessment of Sarcopenia in Cirrhosis With or Without Ascites. Clin. Gastroenterol. Hepatol. 2021, 19, 1941–1949.e2. [Google Scholar] [CrossRef]
- Wallen, M.P.; Keating, S.E.; Hall, A.; Hickman, I.J.; Pavey, T.G.; Woodward, A.J.; Skinner, T.L.; Macdonald, G.A.; Coombes, J.S. Exercise training is safe and feasible in patients awaiting liver transplantation: A Pilot Randomized Controlled Trial. Liver Transpl. 2019, 25, 1576–1580. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.C.; Feng, S.; Terrault, N.A.; Lizaola, B.; Hayssen, H.; Covinsky, K. Frailty predicts waitlist mortality in liver transplant candidates. Am. J. Transplant. 2014, 14, 1870–1879. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, M.; Chapman, B.; Hoermann, R.; Angus, P.W.; Testro, A.; Scodellaro, T.; Gow, P.J. Handgrip strength adds more prognostic value to the Model for End-Stage Liver Disease score than imaging-based measures of muscle mass in men with cirrhosis. Liver Transpl. 2019, 25, 1480–1487. [Google Scholar] [CrossRef] [PubMed]
- Tandon, P.; Tangri, N.; Thomas, L.; Zenith, L.; Shaikh, T.; Carbonneau, M.; Ma, M.; Bailey, R.J.; Jayakumar, S.; Burak, K.W.; et al. A Rapid Bedside Screen to Predict Unplanned Hospitalization and Death in Outpatients With Cirrhosis: A Prospective Evaluation of the Clinical Frailty Scale. Am. J. Gastroenterol. 2016, 111, 1759–1767. [Google Scholar] [CrossRef]
- Lai, J.C.; Dodge, J.L.; Kappus, M.R.; Dunn, M.A.; Volk, M.L.; Duarte-Rojo, A.; Ganger, D.R.; Rahimi, R.S.; McCulloch, C.E.; Haugen, C.E. Changes in frailty are associated with waitlist mortality in patients with cirrhosis. J. Hepatol. 2020, 73, 575–581. [Google Scholar] [CrossRef]



| Criteria | Inclusion and Exclusion Details |
|---|---|
| Population |
|
| Intervention |
|
| Control |
|
| Outcomes |
|
| Study Design |
|
| Study Citation, Country | Study Design | Population | Exercise Intervention | Dietary Intervention | Control Group | Body Composition Outcomes ↑ = Significantly Increased or Higher ↓ = Significantly Decreased or Lower ↔ = No Significant Difference (Pre/Post or vs. Control) |
|---|---|---|---|---|---|---|
| Combined intervention studies (n = 9 RCTs, n = 2 non-randomised studies, n = 3 single arm intervention trials) | ||||||
| Aaman et al. [40] 2019 Denmark | RCT | Intervention n = 20 Age 61.7 ± 7.8 years 80% male BMI 26 ± 3.0 kg/m2 Child Pugh Class: A 50%, B 50% MELD 10.8 ± 2.7 Control n = 19 Age 63 ± 7 years 74% male BMI 25 ± 4.2 kg/m2 Child Pugh Class: A 53%, B 47% MELD 10.7 ± 2.8 Outpatients | Supervised resistance training 3 days/week for 60 min at a moderate level. 5 min warm up, then 7 whole body exercises, (3 sets for legs, 2 sets for arms/chest, 1 set lower back, 1 for abdominals), starting at 15–12 repetitions at the start down to 8 by week 12 Duration:12 weeks | Oral nutrition supplements (125 mL, 14.4 g protein and 2.9 g BCAA/100 g) provided if protein intake < 1.2 g/kg/day at baseline | No change to current exercise or diet | Intervention versus control: ↑ Cross sectional area of quadriceps via MRI ↑ Body cell mass via BIA ↔ Dry lean mass via BIA ↔ Lean mass via BIA ↔ Calf circumference ↔ MAC ↔ Thigh circumference ↔ Mid arm muscle area ↔ TSF |
| Chen et al. [44] 2020 USA | Pilot RCT | Intervention n = 9 Age 55 ± 7 years 56% male BMI 30 ± 6 kg/m2 Child Pugh Class: B 78%, C 22% MELD-Na 16 ± 4 Control n = 8 Age 54 ± 11 years 75% male BMI 31 ± 8 kg/m2 Child Pugh Class: B 50%, C 50% MELD-Na 19 ±3 Portal hypertension and MELD ≥ 10 Outpatients | Education on exercise, and behavioural counselling bi-weekly for first 8 weeks. Self-directed exercise increasing 500 steps/day weekly to biweekly. Daily to weekly motivational phone calls. Duration: 12 weeks | Standardised diet provided 1.2–1.5 g/kg/day of protein + late evening snack + oral nutrition supplement (6 g essential amino acids) twice a day | Standardised diet (same as intervention group) only | Intervention versus control: ↑ Psoas muscle index via CT ↔ Total skeletal muscle index via CT ↔ Intramuscular adipose tissue via CT ↔ Total abdominal adipose tissue via CT ↔ Total thigh muscle volume via CT ↔ Thigh muscle index via CT ↔ Cross sectional area, 50% of femur length via CT ↔ Thigh adipose tissue volume via CT ↔ Fat free mass via DXA ↔ Fat mass via DXA ↔ Lean muscle index via DXA ↔ Lower extremities lean muscle index via DXA ↔ Fat free mass via BIA ↔ Fat mass via BIA ↔ Skeletal muscle mass via BIA ↔ Skeletal muscle index via BIA ↔ Phase angle via BIA |
| Hernandez-Conde et al. [39] 2021 | Pilot, double-blind RCT | Intervention n = 15 Age 69 ± 9.7 years 86.7% male BMI 29 ± 4.6 kg/m2 MELD 10.7 ± 4.4 Child Pugh Class: A 78.6%, B 21.4% Control n = 17 Age 61 ± 9.4 years 88.2% male BMI 26 ± 4.7 kg/m2 MELD 11 ± 3.4 Child Pugh Class: A 59%, B 29%, C 12% Compensated outpatients | Personalised exercise instructions with use of accelerometers in wristbands or smartphones to include 5000–10,000 steps/day with gradual increments of 2000–2500 steps/day + moderate intensity exercise in 30-min sessions (goal at least 150 min/week) + verbal reinforcement at reviews. Duration: 12 weeks | Personalised diet recommendations + instructed to eat 7 meals/day including late evening snack plus BCAA supplement 100 g dissolved in 500 mL water throughout the day (15 g protein, 8.5 g fat, 68 g of carbohydrates, 2.61 g of leucine, 1.01 g of isoleucine, and 1.62 g of valine) + verbal reinforcement at reviews | Same exercise and diet recommendations as intervention group except took placebo supplement 100 g dissolved in 500 mL water throughout day (maltodextrin 99.63%) instead of BCAA | Intervention versus control: ↑ Skeletal muscle index via CT ↓ % total body fat via BIA ↔ Phase angle via BIA |
| Kruger et al. [47] 2018 Canada | RCT | Intervention n = 20 Age 53 ± 8 years 50% male MELD 9.05 Child Pugh Class: A 70%, B 30% Control n = 18 Age 56.4 ± 8.5 years 65% male MELD 9.7 Child Pugh Class: A 70%, B 30% BMI not reported Outpatients | Supervised at home, moderate to high intensity aerobic exercise (60–80% of heart rate reserve) on cycle ergometer 3 days/week (30 min sessions gradually increased to 60 min). Visited bi-weekly for session observation. Duration: 8 weeks | Dietary counselling on optimal protein (1.2–1.5 g/kg/day, ideal body weight for BMI > 30) and energy intake (35–40 kcal/kg for BMI 20–30, 25–35 kcal/kg for BMI 30–40, and 20–25 kcal/kg for BMI > 40. Advised on exercise days to consume an extra 250–300 kcal. | Usual care | Intervention versus control: ↔ Thigh muscle mass via ultrasound ↔ Thigh circumference |
| Lattanzi et al. [38] 2021 | Pilot single blind RCT | Intervention n = 14 Age: 59.2 ± 8.4 years 64% male BMI 29.8 ± 4.3 kg/m2 Child Pugh Class: A 86%, B 14% MELD 9 ± 2.7 Control n = 10 Age: 56 ± 4.6 years 60% male BMI 29.6 ± 6.8 kg/m2 Child Pugh Class: A 90%, B 10% MELD 9.8 ± 3.2 Outpatients with portal hypertension | Motivational interviewing with information on physical activity at baseline | Motivational interview at baseline with information and counselling on diet in line with EASL clinical guidelines (2019) + HMB supplement (3 g/day) | Same exercise and diet as intervention group + placebo supplement (Sorbitol 3 g/day) | Within group changes: ↑ Thigh muscle thickness via ultrasound ↔Fat free mass via BIA ↔Phase Angle via BIA |
| Macias-Rodriguez et al. [37] 2020 | RCT | Intervention n = 22 Age 53.5 ± 7.6 years 47% male BMI 29.8 ± 4.8 kg/m2 Child Pugh Class: A 82%, B 18% MELD 8.5 (7–10) Control n = 21 Age 53.7 ± 8.2 years 43% male BMI 29.2 ± 3.7 kg/m2 Child Pugh Class: A 95%, B 5% MELD 8 (7.5–9.5) Compensated cirrhosis, outpatients | Given wrist-worn accelerometer as activity tracker. Aim to gradually increase physical activity to reach >2500 steps/day above baseline. Total 5000 steps/day. Light to moderate intensity. Duration: 10 weeks | Harris–Benedict equation was utilised to calculate energy requirements + 10% extra for thermic effect of food and 20% extra for exercise. Diet 60% carbohydrates, 1.3–1.5 g protein/kg/day + remainder from fats + 1.5–2 g sodium restriction/day restriction + non-alcoholic beer at lunch (330 mL/day) | The same diet and exercise prescribed as intervention group without non-alcoholic beer (given a 330 mL bottle of water instead) | Within group changes: ↔ Phase Angle via BIA ↑ Thigh circumference ↔MAMC ↔TSF |
| Macias-Rodriguez et al. [36] 2016 Mexico | Pilot open RCT | Intervention n = 13 Age 53 (48–55) years 69% male BMI 27.5 (22.4–28.9) kg/m2 Child Pugh score 6 (5–7) MELD 9 (8–12) Control n = 12 Age 51 (38–57) years 83% male BMI 27.4 (25–30) kg/m2 Child Pugh score 6 (5–7) MELD: 12 (7–14) Compensated outpatients | Supervised exercise 3 days/week of 60–70% max heart rate, for 40 min of aerobic training using cycle ergometer + kinesiotherapy/rhythmic activities) Duration: 14 weeks | Instructed to consume 30% extra calories (65% carbohydrates, 1.2 g/kg/day protein) + no added salt diet of 1.5–2 g/day | Same recommendations as intervention; consume 10% extra calories (65% carbohydrates, 1.2 g/kg/day protein) + no added salt diet of 1.5–2 g/day. Continue regular activities, no new exercise | Intervention versus control: ↑ Phase angle via BIA |
| Roman et al. [33] 2014 Spain | Pilot RCT | Intervention n = 8 Age 65.5 (46–72) years 62% male BMI 26.7 (18.3–34.7) kg/m2 Child Pugh Class: A 87%, B 13% MELD 9.5 (7–12) Control n = 9 Age 61 (43–75) years 78% male BMI 27.6 (19.5–35.3) kg/m2 Child Pugh Class: A 78%, B 22%, MELD 9 (7–13) Outpatients with a previous episode of decompensation | Supervised exercise 3 days/week, moderate intensity (60–70% max heart rate) for 60 min. Cycle ergometry and treadmill walking Duration: 12 weeks | 10 g oral leucine supplementation daily | 10 g oral leucine supplementation daily, no exercise recommendations | Within group changes: ↑ Lower thigh circumference (intervention compared to baseline, ↔ control) ↔ Mid or upper thigh circumference (intervention or control) ↔ MAMC (intervention or control) ↔ Mid-arm circumference (intervention or control) ↔ TSF (intervention or control) |
| Zenith et al. [35] 2014 Canada | RCT | Intervention n = 9 Age 56 ± 8 years 78% male BMI 27.7 ± 3.8 kg/m2 Child Pugh score: 6.2 ± 1.4 MELD 9.7 ± 2.4 Control n = 10 Age 59 ± 6 years 80% male BMI 28.9 ± 4.1 kg/m2 Child Pugh score: 6.3 ± 1.4 MELD 10.2 ± 1.9 Outpatients, Child Pugh A or B | Supervised exercise 3 days/week, 60–80% of peak VO2, 30 min session, increased by 2.5 min per session each week, 5 min warm up and cool down using cycle ergometer Duration: 8 weeks | Baseline dietetic counselling to reach 1.2–1.5 g/kg of protein (for BMI > 30 adjustments made based on ideal body weight), calories BMI specific (between 14 up to 30 kcal/kg) and instructed to consume an extra 250–300 calories on exercise days | Baseline counselling by dietitian (same as intervention) but no formal exercise regimen | Intervention versus control: ↑ Quadricep muscle thickness via ultrasound ↑ Thigh circumference |
| Morkane et al. [43] 2020 United Kingdom | Non-randomised controlled trial | Intervention n = 16 Age 55.6 ± 7.8 years 87.5% male MELD 13.7 ± 4.6 BMI 30.9 ± 5.6 kg/m2 Control n = 17 Age 55.6 ± 7.8 years 82.7% Male MELD 13.2 ± 3.7 BMI: 27 ± 4.6 kg/m2 Outpatients, transplant candidates | Supervised 40 min interval training on cycle ergometer (4–6 × 3 min intervals at 80% of AT (moderate intensity) and 4–6 × 2 min intervals at 50% of difference between VO2 at peak and VO2 at AT (‘severe’ intensity) with 5 min warm up and cool down) Duration: 6 weeks | Standardised nutrition assessment and advice by transplant dietitian at baseline and 6 weeks | Standard care, no initiation of exercise. Standardised nutrition assessment and advice by transplant dietitian at baseline and 6 weeks | Within group changes: ↔ Mid-arm circumference (intervention or control) ↔ MAMC (intervention or control) |
| Schmidt et al. [42] 2021 | Non-randomised controlled trial | Intervention n = 11 Age 56.6 ± 9.9 years 63.6% male BMI 30.3 ± 5.4 kg/m2 Child Pugh Class: A 91%, B 9% Control n = 22 Age 58.7 ± 12.9 years 59.1% male BMI 32.4 ± 5.1 kg/m2 Child Pugh Class: A 86%, B 14% MELD—not reported Compensated outpatients | Supervised exercise 3 days/week, aerobic, moderate intensity (5 min warm up, 30 min walking/running 60–70% VO2 max). Increasing session by 2 min until reaching 50 mins by week 8. Duration: 12 weeks | Diet advice to aim for 25–30 kcal/day and 1.2–1.5 g of protein/kg/day—using estimated dry body weight. | The same diet advice without any exercise intervention | Intervention versus control: ↔ Phase Angle via BIA ↔ Lean mass via BIA ↔ Fat mass via BIA ↔ MAMC ↓ MAC |
| Berzigotti et al. [32] 2017 Spain | Multi-centre single arm intervention pilot study | Total n = 50 Age 56 ± 8 years 62% male BMI 33.3 ± 3.2 kg/m2 MELD 9 ± 3 Child Pugh Class: A 92%, B 8% Compensated outpatients with BMI ≥ 26 kg/m2 | Supervised exercise 1 day/week for 60 min moderate intensity (10–12 Borg Scale of Perceived Effort) in groups of 1–5 + increase daily step activity Duration: 16 weeks | Reduction of 500–1000 kcal/day. Protein intake maintained at 20–50% of total kcal and within 0.8 g/kg ideal bodyweight/day. Carbohydrates 45–50% and fat <35% of total kcal. 20 g/day alimentary fibre recommended. | No control | ↓ Fat mass via BIA ↔ Lean mass via BIA |
| Hiraoka et al. [52] 2017 Japan | Single arm intervention study | Total n = 33 Age 67 (63–71) years 39% men BMI 23.2 (20.8–25.1) kg/m2 Child Pugh Class: A 90%, B 10% Compensated outpatients | Walking (an additional 2000 steps/day on top of usual average steps) Duration: 12 weeks | Late evening BCAA supplement provided once daily (13.5 g protein, 210 kcal/day) | No control | ↑ Muscle volume via BIA (reported as change ratio) |
| Nishida et al. [53] 2017 Japan | Single arm intervention study | Total n = 6 Age from 51–79 years 100% female BMI 24.3 (19.6–26.1) kg/m2 Child Pugh Class: A 100% Compensated outpatients | Instructed to undertake bench step activity at anaerobic threshold level at home. Aim 140 min/week. Duration: 12 months | BCAA supplement (3 sachets/day = 12.45 g of BCAA), no specific nutrition advice except to maintain usual dietary intake | No control | ↔ % fat via BIA ↔ Visceral fat area via CT ↔ Intramuscular adipose tissue content via CT |
| Diet-only intervention studies (n = 9 RCTs, n = 1 non-randomised study, n = 2 single arm interventions) | ||||||
| Dupont et al. [45] 2012 France | Multi-centre RCT | Intervention n = 44 Age 56.1 ± 9.6 years 68% male Child Pugh score: 11.2 ± 1.3 Control n = 55 Age 54.6 ± 9.6 years 64% male Child Pugh score: 10.5 ± 1.5 BMI or MELD—not reported Inpatients with ARLD and jaundice (without alcoholic hepatitis) | NA | Enteral nutrition 3–4 weeks (30–55 kcal/kg/day through nasogastric tube). Subsequent 3 oral nutrition supplements/day for 2 months Duration: 12 weeks with outcomes reported at 12 months | Standard hospital oral diet | Intervention versus control: ↔ MAMC ↔ TSF |
| Hirsh et al. [54] 1983 Chile | RCT | Intervention n = 26 Age 49.9 ± 8.6 years 81% male Control n = 25 Age 46.1 ± 8.0 years 84% male BMI, Child Pugh, or MELD—not reported Decompensated outpatients | NA | 1 L oral nutrition supplement /day (1000 kcal, 34 g protein) + usual diet Duration: 12 months | Placebo tablet daily | Intervention versus control: ↔ TSF ↔ Mid-arm circumference |
| Le Cornu et al. [55] 2000 England | RCT | Intervention n = 42 Age 52 (27–67) years 69% male Child Pugh Class: A 7%, B 48%, C 45% Control n = 40 Age 50 (24–68) years 78% male Child Pugh Class: A 10%, B 28%, C 62% BMI or MELD not reported Outpatient transplant candidates with MAMC < 25% percentile | NA | Oral nutrition supplement of 500 mL/day (750 kcal, 20 g protein) was given + dietary counselling to adapt/increase their calories and protein based on their medical condition until transplantation Duration: until transplantation. Median wait 77 (1–395) days intervention and 45 (1–424) control | Standard dietary advice to adapt/increase their calories and protein based on their medical condition until transplantation | Intervention versus control: ↔ MAMC ↔ Mid-arm circumference ↔ TSF |
| Les et al. [48] 2011 Spain | Multi-centre RCT | Intervention n = 58 Age 64.1 ± 10.4 years 78% male Child Pugh 8.3 ± 2.0 MELD 16.1 ± 4.5 Control n = 58 Age 62.5 ± 10.4 years 74% male Child Pugh 8.1 ± 1.7 MELD 16.2 ± 3.9 BMI—not reported Outpatients with previous episode of hepatic encephalopathy | NA | Diet of 35 kcal/kg + 0.7 g/kg of protein/day adjusted to ideal weight + late evening BCAA supplement 2/day (120 kcal). Enteral nutrition if admitted for episode of hepatic encephalopathy and oral intake in hospital was poor. Duration: mean 32 ± 22 weeks intervention and 36 ± 2 weeks control | Same diet but with maltodextrin supplement 2/day instead of BCAA. Enteral nutrition provided if episode of hepatic encephalopathy and oral intake was poor | Within group changes: ↑ MAMC (intervention compared to baseline) ↔ MAMC (control compared to baseline) |
| Manguso et al. [34] 2005 Italy | Random-ised, double period cross-over trial | Group 1: n = 45 Age 60 ± 9 years 67% male BMI 28.5 ± 3.2 kg/m2 Child Pugh Class: A 33%, B 77% Group 2: n = 45 Age 60 ± 7 years 49% male BMI 27.8 ± 2.1 kg/m2 Child Pugh Class: A 33%, B 77% Outpatients with HCV cirrhosis | NA | Group 1: Prescribed diet of 30–40 kcal/kg/day based on calculated desirable weight (total calories split into 16% protein, 55% carbohydrates, 28–30% fat) + low sodium 1000 mg/day Followed by usual diet after. Group 2: Usual diet first. Followed by prescribed diet second. Duration: 3 months per diet (6 months total) | Within group changes: ↑ MAMC (Group 1 at 3 months post prescribed diet vs baseline) ↑ MAMC (Group 2 at 6/12, post prescribed diet vs baseline and vs 3/12) ↓ MAMC (Group 1 at 6 months post usual diet vs 3 months post prescribed diet) ↔ MAMC (Group 2 at 3 months post usual diet vs baseline) ↔ TSF (Group 1 or Group 2 after both diet interventions at 3 and 6 months) | |
| Okabayashi et al. [56] 2011 Japan | RCT | Intervention n = 40 Age 68 ± 7.6 years 28% male BMI 23.6 ± 3.2 kg/m2 Child Pugh Class: A 70%, B 30% Control n = 36 Age 65.1 ± 11.3 years 31% male BMI 22.7 ± 3.2 kg/m2 Child Pugh Class: A 71%, B 29% Outpatients with scheduled HCC surgery | NA | Carbohydrate and BCAA enriched supplement morning and night. (420 kcal, 13 g free amino acids, 13 g of gelatine hydrolysate, 62 g carbohydrates, 7 g lipids) + dietitian education to modify intake to reduce 420 kcal/day to account for the supplement and match caloric intake to controls Duration: supplements for at least 6 months, with a follow up at 12 months | Usual diet. No supplements | Interventionversus control: ↑ MAMC (at 6, 8, 10, 12 months) ↔ TSF no change post-operatively in both groups (data not reported) |
| Poon et al. [50] 2004 China | RCT | Intervention n = 41 Age 59 (24–84) years 95% male Control n = 43 Age 59 (27–80) years 90% male. No BMI, Child Pugh or MELD reported. Outpatients with unresectable HCC | NA | BCAA supplement morning and night (420 kcal, 13 g amino acids, 13 g peptides, 62 g carbohydrates, 7 g lipids) + unrestricted diet unless HE—protein was restricted Duration: 1 week prior to surgery, up to 12 months | Usual diet | Intervention versus control: ↔ Mid-arm circumference ↔ TSF |
| Sorrentino et al. [51] 2012 Italy | RCT | Group A: n = 40 Age 64 ± 6.3 years 65% male Child Pugh Class: B 28%, C 72% MELD 12.1 ± 0.7 Group B: n = 40 Age 66 ± 7.5 years 67% male Child Pugh Class: B 30%, C 70% MELD 11.7 ± 0.7 Group C: n = 40 Age: 65 ± 7.6 years 70% male Child Pugh Class: B 25%, C 75% MELD 12.4 ± 0.9 BMI not reported In/outpatients with refractory ascites | NA | Group A: Instructed to consume 1–1.3 g protein/kg/day, 30–35 kcal/kg/day + low sodium diet (80 mEq/day) + BCAA evening snack (210 kcal, 13.5 g protein, 3.5 g fat) + instructed to adjust energy intake to account for BCAA supplement + post LVP parenteral nutrition for 24 hrs post paracentesis during hospital admission + Dietitian advice monthly. Group B: same as group A without parenteral nutrition post paracentesis. Duration: 12 months, follow up at 3, 6, 12 months | Group C: Low sodium diet (80 mEq /day) + Dietitian advice monthly | Between group changes: ↓ TSF (Group C versus Group A at 3, 6, and 12 months and Group C versus Group B at 6 months only) ↓ MAC (Group C versus Group A and Group B at 6 and 12 months) |
| Tangkijvanich et al. [57] 2000 Thailand | RCT | Group 1: n = 14 Age: 53 ± 11 years 71% male BMI 23.7 ± 3.4 kg/m2 Child Pugh score: 5–7: 64%, score 8–15: 36%. Group 2: n = 15 Age: 53 ± 13 years 80% male BMI: 25 ± 4.1 kg/m2 Child Pugh score: 5–7: 60%, score 8–15: 40% Outpatients | NA | Group 1: received standard diet (40 g protein/day) + 150 g BCAA supplement/day = total of ~2000 kcal/day. Duration: 4 weeks | Group 2: standard diet (80 g protein/day = total of ~2000 kcal/day) | Within group changes: ↔ MAMC (Group 1 or Group 2) |
| Okabayashi et al. [49] 2008 Japan | Non-randomised study with historical control group | Intervention n = 13 Age 66.2 ± 9.1 years 54% male Child Pugh Class: A 77%, B 23% Control n = 28 Age 65.6 ± 8.2 yrs 75% male Child Pugh Class: A 82%, B 18% BMI not reported Outpatients for HCC surgery | NA | Carbohydrate and BCAA enriched supplement morning and night. (420 kcal, 13 g free amino acids, 13 g gelatin hydrolysate, 62 g carbohydrates, 7 g lipids) Duration: 2 weeks prior to surgery and at least 6 months post | Usual care—no supplementation | Within group changes: ↑ MAMC (baseline to 6 months for intervention, not reported for control) |
| Kitajima et al. [59] 2018 Japan | Single arm intervention study | Total n = 21 Age 71.3 ± 7.9 years 42% male BMI 23.9 ± 4.0 kg/m2 Child Pugh Class: A 48%, B 52% MELD—not reported Outpatients with hypoalbuminaemia | NA | BCAA supplement 3/day after meals. Dietitian advised intakes of 25–35 kcal/kg/day and protein 1–1.4 g/kg/day. Adherence monitored monthly. Duration: 48 weeks | No control | ↔ Skeletal muscle index via CT ↔ Intramuscular adipose tissue content via CT ↔ Subcutaneous fat area via CT ↔ Visceral fat area via CT |
| Putadechakum et al. [58] 2012 Thailand | Single arm intervention study | n = 22 Age 52.9 ± 12.8 years 55% male BMI 21.4 ± 0.6 kg/m2 Child Pugh Class: A 63%, B 23%, C 14% Outpatients with ARLD | NA | 20 g protein (soy based) oral nutrition supplement daily (420 kcal, 20 g protein, 65 g CHO, 10.6 g fat) + regular diet. Duration: 8 weeks | No control | ↑ Lean mass via BIA ↔ Fat mass via BIA ↔ TSF |
| Exercise only intervention (n = 1 RCT) | ||||||
| Roman et al. [41] 2016 Spain | RCT | Intervention n = 14 Age 62 ± 2.4 years 71% male BMI 31.5 ± 1.6 kg/m2 Child Pugh score: 5.4 ± 0.2 MELD 8.2 ± 0.4 Control n = 9 Age 63.1 ± 2.3 years 85% male BMI 30.3 ± 1.4 kg/m2 Child Pugh score: 5.4 ± 0.2 MELD 9.1 ± 0.4 Outpatients with a previous episode of decompensation | Supervised exercise 3 days/week, 60 min of cycle ergometry and treadmill walking + 5–10 min of upper body resistance exercise + 10–15 min balance, coordination, stretching and relaxation. Moderate intensity (60–70%) of max heart rate. Duration: 12 weeks | NA | Sham intervention 1 h 3 days/week of cephalocaudal muscle relaxation, and breathing, visualisation, and concentration exercises | Within group changes: ↑ Lean appendicular mass via DXA (intervention compared to baseline, ↔ control) ↑ Lean leg mass via DXA (intervention compared to baseline, ↔ control) ↑ Lean body mass via DXA (intervention compared to baseline, ↔ control) ↓ Fat body mass via DXA (intervention compared to baseline, ↔ control) ↑ Upper thigh circumference (intervention compared to baseline, ↔ control) ↔ Lower thigh circumference (intervention or control) ↓ Mid-arm circumference and mid-arm skinfold thickness (intervention compared to baseline, ↔ control) ↓ Mid-thigh skinfold thickness (intervention compared to baseline, ↔ control) ↔ MAMC (intervention or control) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Johnston, H.E.; Takefala, T.G.; Kelly, J.T.; Keating, S.E.; Coombes, J.S.; Macdonald, G.A.; Hickman, I.J.; Mayr, H.L. The Effect of Diet and Exercise Interventions on Body Composition in Liver Cirrhosis: A Systematic Review. Nutrients 2022, 14, 3365. https://doi.org/10.3390/nu14163365
Johnston HE, Takefala TG, Kelly JT, Keating SE, Coombes JS, Macdonald GA, Hickman IJ, Mayr HL. The Effect of Diet and Exercise Interventions on Body Composition in Liver Cirrhosis: A Systematic Review. Nutrients. 2022; 14(16):3365. https://doi.org/10.3390/nu14163365
Chicago/Turabian StyleJohnston, Heidi E., Tahnie G. Takefala, Jaimon T. Kelly, Shelley E. Keating, Jeff S. Coombes, Graeme A. Macdonald, Ingrid J. Hickman, and Hannah L. Mayr. 2022. "The Effect of Diet and Exercise Interventions on Body Composition in Liver Cirrhosis: A Systematic Review" Nutrients 14, no. 16: 3365. https://doi.org/10.3390/nu14163365
APA StyleJohnston, H. E., Takefala, T. G., Kelly, J. T., Keating, S. E., Coombes, J. S., Macdonald, G. A., Hickman, I. J., & Mayr, H. L. (2022). The Effect of Diet and Exercise Interventions on Body Composition in Liver Cirrhosis: A Systematic Review. Nutrients, 14(16), 3365. https://doi.org/10.3390/nu14163365