Individualised Nutritional Care for Disease-Related Malnutrition: Improving Outcomes by Focusing on What Matters to Patients
Abstract
:1. Introduction
2. Patients at the Centre of Their Care
2.1. Terminology
2.2. Defining Individualised Nutritional Care
3. The Inclusion of Individualised Nutritional Care in the Delivery of Nutritional Care to Manage Disease-Related Malnutrition
3.1. Individualised Nutritional Care in Nutrition Guidelines
3.2. Inclusion of Individualised Nutritional Care in Studies of Oral Nutritional Intervention
3.3. Studies Employing Individualised Nutritional Care in Specific Patient Groups
4. Delivering Individualised Nutritional Care in Practice
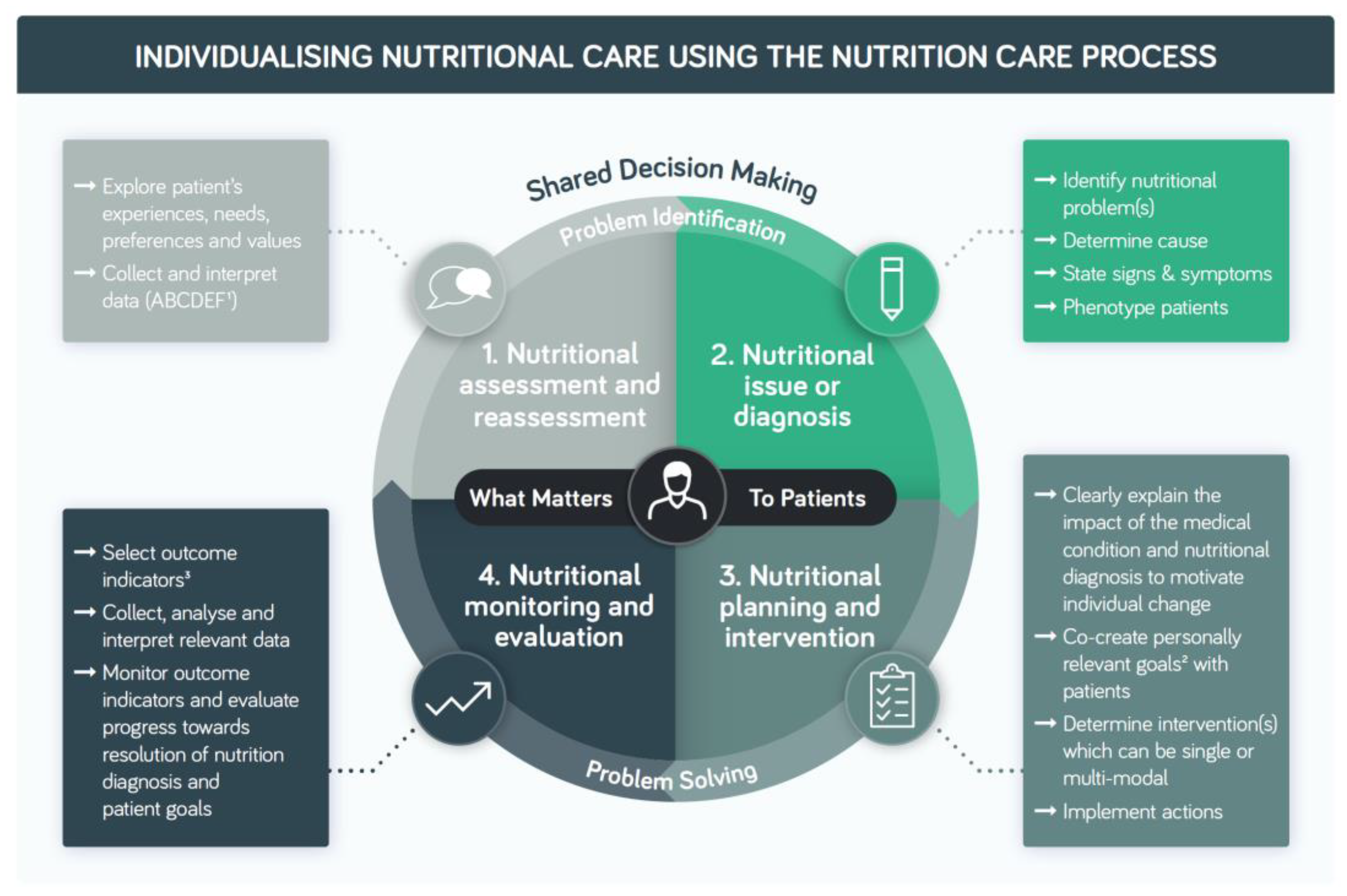
4.1. The Nutrition Care Process—A Practical Model to Individualise Nutritional Care
4.2. An Interdisciplinary Approach to Individualised Nutritional Care
4.3. Measuring What Matters: The Co-Creation of Care
5. Recommendations for Future Research
- ○
- Develop a consensus definition for INC as suggested in this review;
- ○
- In trials and nutrition guidelines, emphasise shared decision making and focusing on what matters to patients to encourage consideration of these key elements of individualised nutritional care in practice;
- ○
- Investigate the acceptability of the term and definition of INC to HCPs and patients;
- ○
- Increase the focus on outcomes that are meaningful to patients in trials;
- ○
- Investigate whether individualising nutritional care leads to better outcomes in different patient groups in different care settings compared to standard non-INC;
- ○
- Focus on models of care where evidenced-based nutritional care strategies are selected based on individual patient needs, preferences and goals rather than on pre-defined standard protocols where there is a hierarchy or stepwise approach to escalating nutrition intervention without any element of tailoring to patients’ specific needs;
- ○
- Investigate the optimal methods of delivery of INC—face to face, telehealth, patient-preferred methods of providing education: websites, videos, printed materials, etc., cultural preferences;
- ○
- Develop evidence-based decision aids to use with patients to assist with shared decision making for INC;
- ○
- Explore optimum language and ways to explain to patients the link between nutrition diagnosis, e.g., an acceptable lay term for malnutrition and its sequelae, and outcome to actively engage patients in nutritional care and support adherence;
- ○
- Develop easy to use, practical tools or resources to enable patients to self-monitor and self-advocate for nutritional care and resources for HCPs to deliver these;
- ○
- Investigate the impact of INC on patients with multi-morbidity.
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organisation (WHO). Handbook for National Quality Policy and Strategy: A Practical Approach for Developing Policy and Strategy to Improve Quality of Care; World Health Organisation (WHO): Geneva, Switzerland, 2018; Available online: https://www.who.int/publications/i/item/9789241565561 (accessed on 27 June 2022).
- World Health Organisation (WHO). Continuity and Coordination of Care: A Practice Brief to Support Implementation of the WHO Framework on Integrated People-Centred Health Services; World Health Organisation (WHO): Geneva, Switzerland, 2018; Available online: https://www.who.int/publications/i/item/9789241514033 (accessed on 27 June 2022).
- Kuipers, S.J.; Cramm, J.M.; Nieboer, A.P. The importance of patient-centered care and co-creation of care for satisfaction with care and physical and social well-being of patients with multi-morbidity in the primary care setting. BMC Health Serv. Res. 2019, 19, 13. [Google Scholar] [CrossRef] [PubMed]
- The Organisation for Economic Co-operation and Development (OECD). Measuring What Matters: The Patient-Reported Indicator Surveys. Patient-Reported Indicators for Assessing Health System Performance. 2019. Available online: https://www.oecd.org/health/health-systems/Measuring-what-matters-the-Patient-Reported-Indicator-Surveys.pdf (accessed on 27 June 2022).
- Baldwin, C.; de van der Schueren, M.A.E.; Kruizenga, H.M.; Weekes, C.E. Dietary advice with or without oral nutritional supplements for disease-related malnutrition in adults. Cochrane Database Syst. Rev. 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation (WHO). Multimorbidity: Technical Series on Safer Primary Care; World Health Organisation (WHO): Geneva, Switzerland, 2016; Available online: https://apps.who.int/iris/bitstream/handle/10665/252275/9789241511650-eng.pdf (accessed on 27 June 2022).
- World Health Organisation (WHO). Planning and Implementing Palliative Care Services: A Guide for Programme Managers; World Health Organisation (WHO): Geneva, Switzerland, 2016; Available online: https://apps.who.int/iris/bitstream/handle/10665/250584/9789241565417-eng.pdf?sequence=1 (accessed on 27 June 2022).
- Rathert, C.; Wyrwich, M.D.; Boren, S.A. Patient-centered care and outcomes: A systematic review of the literature. Med. Care Res. Rev. 2013, 70, 351–379. [Google Scholar] [CrossRef] [PubMed]
- Payne, L.; Ghio, D.; Grey, E.; Slodkowska-Barabasz, J.; Harris, P.; Sutcliffe, M.; Green, S.; Roberts, H.C.; Childs, C.; Robinson, S.; et al. Optimising an intervention to support home-living older adults at risk of malnutrition: A qualitative study. BMC Fam. Pract. 2021, 22, 219. [Google Scholar] [CrossRef] [PubMed]
- Payne, C.; McIlfatrick, S.; Larkin, P.; Dunwoody, L.; Gracey, J. A qualitative exploration of patient and healthcare professionals' views and experiences of palliative rehabilitation during advanced lung cancer treatment. Palliat. Med. 2018, 32, 1624–1632. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, J. Jonathan Bradshaw on Social Policy: Selected Writings 1972–2011; Cookson, R.A., Sainsbury, R., Glendin-ning, C., Eds.; University of York: York, UK, 2013; Available online: https://www.york.ac.uk/inst/spru/pubs/pdf/JRB.pdf (accessed on 27 June 2022).
- National Library of Medicine. Patient Preference MeSH Descriptor Data. 2022. Available online: https://meshb.nlm.nih.gov/record/ui?ui=D057240 (accessed on 27 June 2022).
- Boyd, C.M.; Singh, S.; Varadhan, R.; Weiss, C.O.; Sharma, R.; Bass, E.B.; Puhan, M.A. Methods for Benefit and Harm Assessment in Systematic Reviews Methods Research Report. (Prepared by the Johns Hopkins University Evidence-based Practice Center under Contract No. 290-2007-10061-I). Rockville, MD: Agency for Healthcare Research and Quality. 2012. Available online: https://www.ncbi.nlm.nih.gov/books/NBK115751/#influence.s1 (accessed on 27 June 2022).
- National Library of Medicine. Goals MeSH Descriptor Data. 2022. Available online: https://meshb.nlm.nih.gov/record/ui?name=Goals (accessed on 27 June 2022).
- Johnstone, E.; Perry, S.; Davies, V.; Dassanayake, T. BDA Outcomes Guidance Document; The Association of UK Dietitians: Birmingham, UK, 2019. [Google Scholar]
- Levey, R.; Ball, L.; Chaboyer, W.; Sladdin, I. Dietitians’ perspectives of the barriers and enablers to delivering patient-centred care. J. Hum. Nutr. Diet. 2020, 33, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Sladdin, I.; Ball, L.; Bull, C.; Chaboyer, W. Patient-centred care to improve dietetic practice: An integrative review. J. Hum. Nutr. Diet. 2017, 30, 453–470. [Google Scholar] [CrossRef]
- Sladdin, I.; Chaboyer, W.; Ball, L. Patients’ perceptions and experiences of patient-centred care in dietetic consultations. J. Hum. Nutr. Diet. 2018, 31, 188–196. [Google Scholar] [CrossRef]
- Cereda, E.; Clave, P.; Collins, P.F.; Holdoway, A.; Wischmeyer, P.E. Recovery Focused Nutritional Therapy across the Continuum of Care: Learning from COVID-19. Nutrients 2021, 13, 3293. [Google Scholar] [CrossRef]
- Bischoff, S.C.; Austin, P.; Boeykens, K.; Chourdakis, M.; Cuerda, C.; Jonkers-Schuitema, C.; Lichota, M.; Nyulasi, I.; Schneider, S.M.; Stanga, Z.; et al. ESPEN practical guideline: Home enteral nutrition. Clin. Nutr. 2022, 41, 468–488. [Google Scholar] [CrossRef]
- Thibault, R.; Abbasoglu, O.; Ioannou, E.; Meija, L.; Ottens-Oussoren, K.; Pichard, C.; Rothenberg, E.; Rubin, D.; Siljamäki-Ojansuu, U.; Vaillant, M.-F.; et al. ESPEN guideline on hospital nutrition. Clin. Nutr. 2021, 40, 5684–5709. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, D.B.; Barrocas, A.; Annetta, M.G.; Stratton, K.; McGinnis, C.; Hardy, G.; Wong, T.; Arenas, D.; Turon-Findley, M.P.; Kliger, R.G.; et al. Ethical Aspects of Artificially Administered Nutrition and Hydration: An ASPEN Position Paper. Nutr. Clin. Pract. 2021, 36, 254–267. [Google Scholar] [CrossRef] [PubMed]
- Pironi, L.; Boeykens, K.; Bozzetti, F.; Joly, F.; Klek, S.; Lal, S.; Lichota, M.; Mühlebach, S.; Van Gossum, A.; Wanten, G.; et al. ESPEN guideline on home parenteral nutrition. Clin. Nutr. 2020, 39, 1645–1666. [Google Scholar] [CrossRef]
- Kovacevich, D.S.; Corrigan, M.; Ross, V.M.; McKeever, L.; Hall, A.M.; Braunschweig, C. American Society for Parenteral and Enteral Nutrition Guidelines for the Selection and Care of Central Venous Access Devices for Adult Home Parenteral Nutrition Administration. JPEN J. Parenter. Enter. Nutr. 2019, 43, 15–31. [Google Scholar] [CrossRef]
- Ukleja, A.; Gilbert, K.; Mogensen, K.M.; Walker, R.; Ward, C.T.; Ybarra, J.; Holcombe, B. Task Force on Standards for Nutrition Support: Adult Hospitalized Patients, the American Society for Parenteral and Enteral Nutrition. Standards for Nutrition Support: Adult Hospitalized Patients. Nutr. Clin. Pract. 2018, 33, 906–920. [Google Scholar] [CrossRef] [PubMed]
- Boullata, J.I.; Carrera, A.L.; Harvey, L.; Escuro, A.A.; Hudson, L.; Mays, A.; McGinnis, C.; Wessel, J.J.; Bajpai, S.; Beebe, M.L.; et al. ASPEN Safe Practices for Enteral Nutrition Therapy. J. Parenter. Enter. Nutr. 2017, 41, 15–103. [Google Scholar] [CrossRef] [PubMed]
- Compher, C.; Bingham, A.L.; McCall, M.; Patel, J.; Rice, T.W.; Braunschweig, C.; McKeever, L. Guidelines for the provision of nutrition support therapy in the adult critically ill patient: The American Society for Parenteral and Enteral Nutrition. JPEN J. Parenter. Enter. Nutr. 2021, 46, 12–41. [Google Scholar] [CrossRef]
- Singer, P.; Blaser, A.R.; Berger, M.M.; Alhazzani, W.; Calder, P.C.; Casaer, M.P.; Hiesmayr, M.; Mayer, K.; Montejo, J.C.; Pichard, C.; et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 2019, 38, 48–79. [Google Scholar] [CrossRef]
- Barazzoni, R.; Bischoff, S.C.; Busetto, L.; Cederholm, T.; Chourdakis, M.; Cuerda, C.; Delzenne, N.; Genton, L.; Schneider, S.; Singer, P.; et al. Nutritional management of individuals with obesity and COVID-19: ESPEN expert statements and practical guidance. Clin. Nutr. 2021; in press. [Google Scholar] [CrossRef]
- Barazzoni, R.; Bischoff, S.C.; Breda, J.; Wickramasinghe, K.; Krznaric, Z.; Nitzan, D.; Pirlich, M.; Singer, P. Endorsed by the ESPEN Council. ESPEN expert statements and practical guidance for nutritional management of individuals with SARS-CoV-2 infection. Clin. Nutr. 2020, 39, 1631–1638. [Google Scholar] [CrossRef]
- Chapple, L.S.; Fetterplace, K.; Asrani, V.; Burrell, A.; Cheng, A.C.; Collins, P.; Doola, R.; Ferrie, S.; Marshall, A.P.; Ridley, E.J. Nutrition management for critically and acutely unwell hospitalised patients with coronavirus disease 2019 (COVID-19) in Australia and New Zealand. Nutr. Diet. 2020, 77, 426–436. [Google Scholar] [CrossRef]
- Muscaritoli, M.; Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Hutterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr. 2021, 40, 2898–2913. [Google Scholar] [CrossRef]
- Arends, J.; Strasser, F.; Gonella, S.; Solheim, T.S.; Madeddu, C.; Ravasco, P.; Buonaccorso, L.; de van der Schueren, M.A.E.; Baldwin, C.; Chasen, M.; et al. Cancer cachexia in adult patients: ESMO Clinical Practice Guidelines. ESMO Open 2021, 6, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Kiss, N.; Loeliger, J.; Findlay, M.; Isenring, E.; Baguley, B.J.; Boltong, A.; Butler, A.; Deftereos, I.; Eisenhuth, M.; Fraser, S.F.; et al. Clinical Oncology Society of Australia: Position statement on cancer-related malnutrition and sarcopenia. Nutr. Diet. 2020, 77, 416–425. [Google Scholar] [CrossRef]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.C.; et al. ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin. Nutr. 2019, 38, 10–47. [Google Scholar] [CrossRef] [PubMed]
- Dorner, B.; Friedrich, E.K. Position of the Academy of Nutrition and Dietetics: Individualized Nutrition Approaches for Older Adults: Long-Term Care, Post-Acute Care, and Other Settings. J. Acad. Nutr. Diet. 2018, 118, 724–735. [Google Scholar] [CrossRef] [PubMed]
- Olufson, H.T.; Young, A.M.; Green, T.L. The delivery of patient centred dietetic care in subacute rehabilitation units: A scoping review. J. Hum. Nutr. Diet. 2022, 35, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.; Huang, Y.; Sowa, P.M.; Banks, M.D.; Bauer, J.D. Effectiveness of dietary counseling with or without nutrition supplementation in hospitalized patients who are malnourished or at risk of malnutrition: A systematic review and meta-analysis. JPEN J. Parenter. Enter. Nutr. 2022. [Google Scholar] [CrossRef]
- Schuetz, P.; Fehr, R.; Baechli, V.; Geiser, M.; Deiss, M.; Gomes, F.; Kutz, A.; Tribolet, P.; Bregenzer, T.; Braun, N.; et al. Individualised nutritional support in medical inpatients at nutritional risk: A randomised clinical trial. Lancet 2019, 393, 2312–2321. [Google Scholar] [CrossRef]
- Kaegi-Braun, N.; Mueller, M.; Schuetz, P.; Mueller, B.; Kutz, A. Evaluation of Nutritional Support and In-Hospital Mortality in Patients With Malnutrition. JAMA Netw. Open 2021, 4, e2033433. [Google Scholar] [CrossRef]
- Schuetz, P.; Sulo, S.; Walzer, S.; Vollmer, L.; Stanga, Z.; Gomes, F.; Rueda, R.; Mueller, B.; Partridge, J. Economic evaluation of individualized nutritional support in medical inpatients: Secondary analysis of the EFFORT trial. Clin. Nutr. 2020, 39, 3361–3368. [Google Scholar] [CrossRef]
- Baumgartner, A.; Pachnis, D.; Parra, L.; Hersberger, L.; Bargetzi, A.; Bargetzi, L.; Kaegi-Braun, N.; Tribolet, P.; Gomes, F.; Hoess, C.; et al. The impact of nutritional support on malnourished inpatients with aging-related vulnerability. Nutrition 2021, 89, 111279. [Google Scholar] [CrossRef] [PubMed]
- Baumgartner, A.; Hasenboehler, F.; Cantone, J.; Hersberger, L.; Bargetzi, A.; Bargetzi, L.; Kaegi-Braun, N.; Tribolet, P.; Gomes, F.; Hoess, C.; et al. Effect of nutritional support in patients with lower respiratory tract infection: Secondary analysis of a randomized clinical trial. Clin. Nutr. 2021, 40, 1843–1850. [Google Scholar] [CrossRef] [PubMed]
- Hersberger, L.; Dietz, A.; Bürgler, H.; Bargetzi, A.; Bargetzi, L.; Kägi-Braun, N.; Tribolet, P.; Gomes, F.; Hoess, C.; Pavlicek, V.; et al. Individualized Nutritional Support for Hospitalized Patients With Chronic Heart Failure. J. Am. Coll. Cardiol. 2021, 77, 2307–2319. [Google Scholar] [CrossRef] [PubMed]
- Bargetzi, L.; Brack, C.; Herrmann, J.; Bargetzi, A.; Hersberger, L.; Bargetzi, M.; Kaegi-Braun, N.; Tribolet, P.; Gomes, F.; Hoess, C.; et al. Nutritional support during the hospital stay reduces mortality in patients with different types of cancers: Secondary analysis of a prospective randomized trial. Ann. Oncol. 2021, 32, 1025–1033. [Google Scholar] [CrossRef]
- Tunzi, L.; Funk, T.; Brown, T.; Findlay, M.; Bauer, J. Optimal frequency of individualised nutrition counselling in patients with head and neck cancer receiving radiotherapy: A systematic review. J. Hum. Nutr. Diet. 2022, 35, 223–233. [Google Scholar] [CrossRef]
- Isenring, E.A.; Capra, S.; Bauer, J.D. Nutrition intervention is beneficial in oncology outpatients receiving radiotherapy to the gastrointestinal or head and neck area. Br. J. Cancer 2004, 91, 447–452. [Google Scholar] [CrossRef]
- Isenring, E.A.; Bauer, J.D.; Capra, S. Nutrition support using the American Dietetic Association medical nutrition therapy protocol for radiation oncology patients improves dietary intake compared with standard practice. J. Am. Diet. Assoc. 2007, 107, 404–412. [Google Scholar] [CrossRef]
- Britton, B.; Baker, A.L.; Wolfenden, L.; Wratten, C.; Bauer, J.; Beck, A.K.; McCarter, K.; Harrowfield, J.; Isenring, E.; Tang, C.; et al. Eating As Treatment (EAT): A Stepped-Wedge, Randomized Controlled Trial of a Health Behavior Change Intervention Provided by Dietitians to Improve Nutrition in Patients with Head and Neck Cancer Undergoing Radiation Therapy (TROG 12.03). Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 353–362. [Google Scholar] [CrossRef]
- Ravasco, P.; Monteiro-Grillo, I.; Marques, V.P.; Camilo, M.E. Impact of nutrition on outcome: A prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy. Head Neck 2005, 27, 659–668. [Google Scholar] [CrossRef]
- Orell, H.; Schwab, U.; Saarilahti, K.; Osterlund, P.; Ravasco, P.; Makitie, A. Nutritional Counseling for Head and Neck Cancer Patients Undergoing (Chemo) Radiotherapy—A Prospective Randomized Trial. Front. Nutr. 2019, 6, 22. [Google Scholar] [CrossRef]
- Lacey, K.; Pritchett, E. Nutrition Care Process and Model: ADA adopts road map to quality care and outcomes management. J. Am. Diet. Assoc. 2003, 103, 1061–1072. [Google Scholar] [CrossRef]
- Cederholm, T.; Barazzoni, R.; Austin, P.; Ballmer, P.; Biolo, G.; Bischoff, S.C.; Compher, C.; Correia, I.; Higashiguchi, T.; Holst, M.; et al. ESPEN guidelines on definitions and terminology of clinical nutrition. Clin. Nutr. 2017, 36, 49–64. [Google Scholar] [CrossRef]
- Professional Practice Board. Model and Process for Nutrition and Dietetic Practice; The Association of UK Dietitians: Birmingham, UK, 2016. [Google Scholar]
- Gibbons, K. Toward International Best Outcomes: The Shared Path of the Nutrition Care Process, Informatics, and Research Translation. J. Acad. Nutr. Diet. 2017, 117, 1727–1730. [Google Scholar] [CrossRef]
- Swan, W.I.; Vivanti, A.; Hakel-Smith, N.A.; Hotson, B.; Orrevall, Y.; Trostler, N.; Beck Howarter, K.; Papoutsakis, C. Nutrition Care Process and Model Update: Toward Realizing People-Centered Care and Outcomes Management. J. Acad. Nutr. Diet. 2017, 117, 2003–2014. [Google Scholar] [CrossRef] [PubMed]
- Swan, W.I.; Pertel, D.G.; Hotson, B.; Lloyd, L.; Orrevall, Y.; Trostler, N.; Vivanti, A.; Howarter, K.B.; Papoutsakis, C. Nutrition Care Process (NCP) Update Part 2: Developing and Using the NCP Terminology to Demonstrate Efficacy of Nutrition Care and Related Outcomes. J. Acad. Nutr. Diet. 2019, 119, 840–855. [Google Scholar] [CrossRef] [PubMed]
- The Academy of Nutrition and Dietetics. Electronic Nutrition and Dietetic Process Terminology: International Collaboration and Translations. Available online: https://www.ncpro.org/international-collaboration (accessed on 27 June 2022).
- Johnstone, E.; Perry, S.; Dassanayake, T.; Davies, V. Model and Process for Nutrition and Dietetic Practice; The Association of UK Dietitians: Birmingham, UK, 2021. [Google Scholar]
- Committee on Diagnostic Error in Health Care; Board on Health Care Services; Institute of Medicine; The National Acad-emies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care; Balogh, E.P., Miller, B.T., Ball, J.R., Eds.; National Academies Press: Washington, DC, USA, 2015. Available online: https://www.ncbi.nlm.nih.gov/books/NBK338596/ (accessed on 27 June 2022). [CrossRef]
- Joint Commission of Pharmacy Practitioners. Pharmacists’ Patient Care Process. 2014. Available online: https://jcpp.net/wp-content/uploads/2016/03/PatientCareProcess-with-supporting-organizations.pdf (accessed on 27 June 2022).
- Bell, J.J.; Geirsdóttir, Ó.G.; Hertz, K.; Santy-Tomlinson, J.; Skúladóttir, S.S.; Eleuteri, S.A.J. Nutritional Care of the Older Patient with Fragility Fracture: Opportunities for Systematised, Interdisciplinary Approaches Across Acute Care, Rehabilitation and Secondary Prevention Settings. In Orthogeriatrics: The Management of Older Patients with Fragility Fractures; Falaschi, P., Marsh, D., Eds.; Springer: Berlin/Heidelberg, Germany, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK565574/ (accessed on 27 June 2022).
- Bell, J.J.; Young, A.M.; Hill, J.M.; Banks, M.D.; Comans, T.A.; Barnes, R.; Keller, H.H. Systematised, Interdisciplinary Malnutrition Program for impLementation and Evaluation delivers improved hospital nutrition care processes and patient reported experiences—An implementation study. Nutr. Diet. 2021, 78, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Managing Adult Malnutrition in the Community—A Guide to Managing Disease-Related Malnutrition, Including a Pathway for the Appropriate use of Oral Nutritional Supplements (ONS) Produced by a UK Multi-Professional Consensus Panel. 2021. Available online: https://www.malnutritionpathway.co.uk/library/managing_malnutrition.pdf (accessed on 27 June 2022).
- Yinusa, G.; Scammell, J.; Murphy, J.; Ford, G.; Baron, S. Multidisciplinary Provision of Food and Nutritional Care to Hospitalized Adult In-Patients: A Scoping Review. J. Multidiscip. Healthc. 2021, 14, 459–491. [Google Scholar] [CrossRef]


| Term | Definition | Comment |
|---|---|---|
| Needs | Wants that are essential, felt or expressed by the individual, rather than normative needs as defined by experts and compared against standards [11] | This should not be taken to mean that needs expressed or felt by patients cannot be measured |
| Preferences | An individual’s expression of desirability of one course of action, outcome or selection in contrast to others [12] | Patient preferences can be context specific, whereas patient values are not generally context specific Preferences are a consequence of values, and values are expressed through preferences |
| Values | A person’s beliefs or expectations about what is right or wrong. Values are latent traits [13] | |
| Goals | The end result or objective, which may be specified in advance [14]. It can also refer to a measurable short-term aim set to be achieved by the next consultation or episode of care [15] | Ideally, co-create goals with patients |
| Topic, Reference | Organisation, Resource Type, Year | Summary or Recommendations Relating to Aspects of INC 1 |
|---|---|---|
| General: relating to provision of nutrition support relevant to multiple patient groups | ||
| Home enteral nutrition [20] | ESPEN Practical Guideline 2022 |
|
| Hospital nutrition [21] | ESPEN Guideline 2021 |
|
| Ethical aspects of artificially administered nutrition and hydration [22] | ASPEN Position Paper 2021 |
|
| Home parenteral nutrition (HPN) [23] | ESPEN Guideline 2020 |
|
| Selection and care of central venous access devices for adult home parenteral nutrition administration [24] | ASPEN Guideline 2019 |
|
| Nutrition support: adult hospitalised patients [25] | ASPEN Standard 2018 |
|
| Safe practices for enteral nutrition therapy [26] | ASPEN Consensus Recommendations2017 |
|
| Intensive care | ||
| Provision of nutrition support therapy in the adult critically ill patient [27] | ASPEN Guideline 2021 |
|
| Clinical nutrition in the intensive care unit [28] | ESPEN Guideline 2019 |
|
| COVID-19 | ||
| Nutritional management of individuals with obesity and COVID-19: ESPEN [29] | ESPEN Expert Statements and Practical Guidance 2021 |
|
| Nutritional management of individuals with SARS-CoV-2 infection [30] | ESPEN Expert Statements and Practical Guidance 2020 |
|
| Nutrition management for critically and acutely unwell hospitalised patients with coronavirus disease 2019 (COVID-19) in Australia and New Zealand [31] | Guideline 2020 |
|
| Cancer | ||
| Clinical nutrition in cancer [32] | ESPEN Practical Guideline 2021 |
|
| Cancer cachexia in adult patients [33] | ESMO Clinical Practice Guidelines 2021 |
|
| Cancer-related malnutrition and sarcopenia [34] | COSA Position Statement 2020 |
|
| Older people | ||
| Clinical nutrition and hydration in geriatrics [35] | ESPEN Guideline 2019 |
|
| Individualised nutrition approaches for older adults: long-term care, post-acute care and other settings [36] | The AND Position Paper 2018 |
|
| Comparison | Individualised | Not Individualised |
|---|---|---|
| 15 | 9 |
| 2 | 10 |
| 6 1 | 16 |
| 28 | 3 |
| 12 2 | 1 |
| Total 3 | 63 | 39 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holdoway, A.; Page, F.; Bauer, J.; Dervan, N.; Maier, A.B. Individualised Nutritional Care for Disease-Related Malnutrition: Improving Outcomes by Focusing on What Matters to Patients. Nutrients 2022, 14, 3534. https://doi.org/10.3390/nu14173534
Holdoway A, Page F, Bauer J, Dervan N, Maier AB. Individualised Nutritional Care for Disease-Related Malnutrition: Improving Outcomes by Focusing on What Matters to Patients. Nutrients. 2022; 14(17):3534. https://doi.org/10.3390/nu14173534
Chicago/Turabian StyleHoldoway, Anne, Fionna Page, Judy Bauer, Nicola Dervan, and Andrea B. Maier. 2022. "Individualised Nutritional Care for Disease-Related Malnutrition: Improving Outcomes by Focusing on What Matters to Patients" Nutrients 14, no. 17: 3534. https://doi.org/10.3390/nu14173534
APA StyleHoldoway, A., Page, F., Bauer, J., Dervan, N., & Maier, A. B. (2022). Individualised Nutritional Care for Disease-Related Malnutrition: Improving Outcomes by Focusing on What Matters to Patients. Nutrients, 14(17), 3534. https://doi.org/10.3390/nu14173534






