Geographic Variations in Dietary Patterns and Their Associations with Overweight/Obesity and Hypertension in China: Findings from China Nutrition and Health Surveillance (2015–2017)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Assessment of Dietary Intakes
2.3. Assessment of Dietary Patterns and Their Geographic Variations
2.4. Assessment of Overweight/Obesity and Hypertension
2.5. Socioeconomic Status (SES), Lifestyle, and Health Information
2.6. Statistical Analysis
3. Results
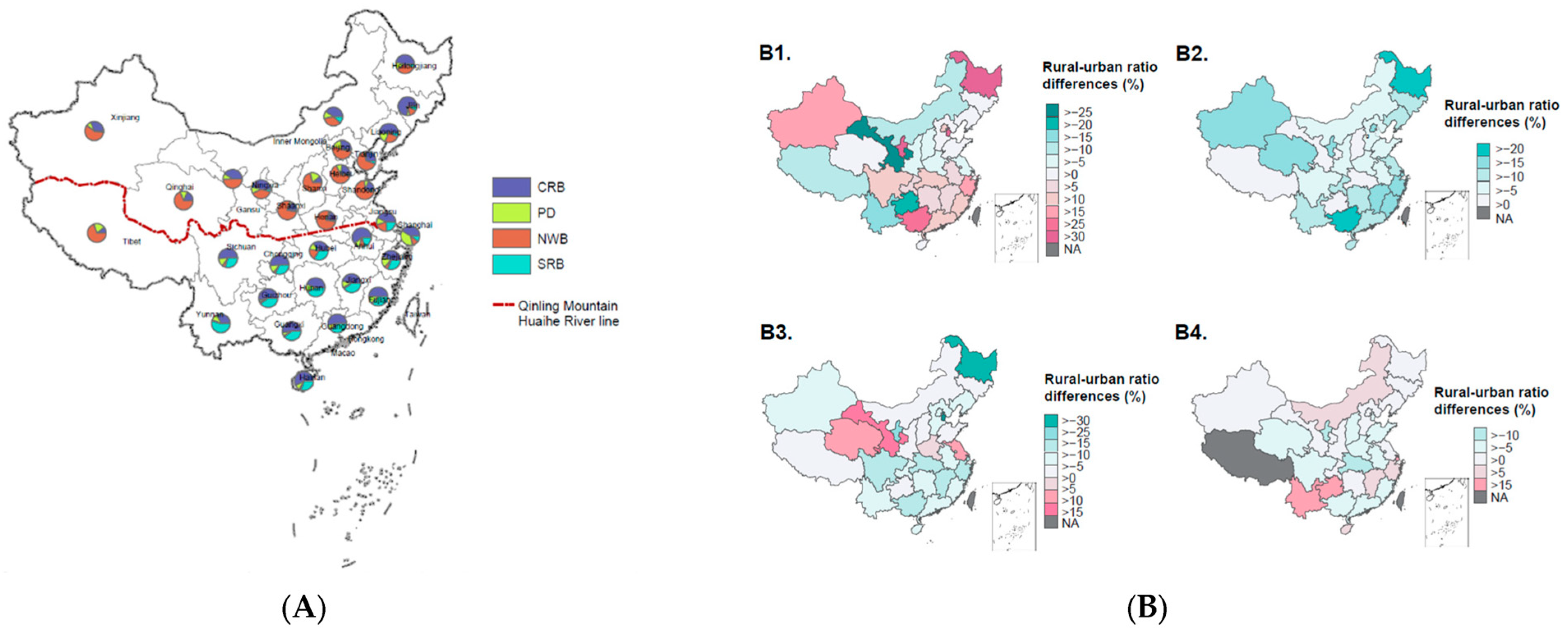
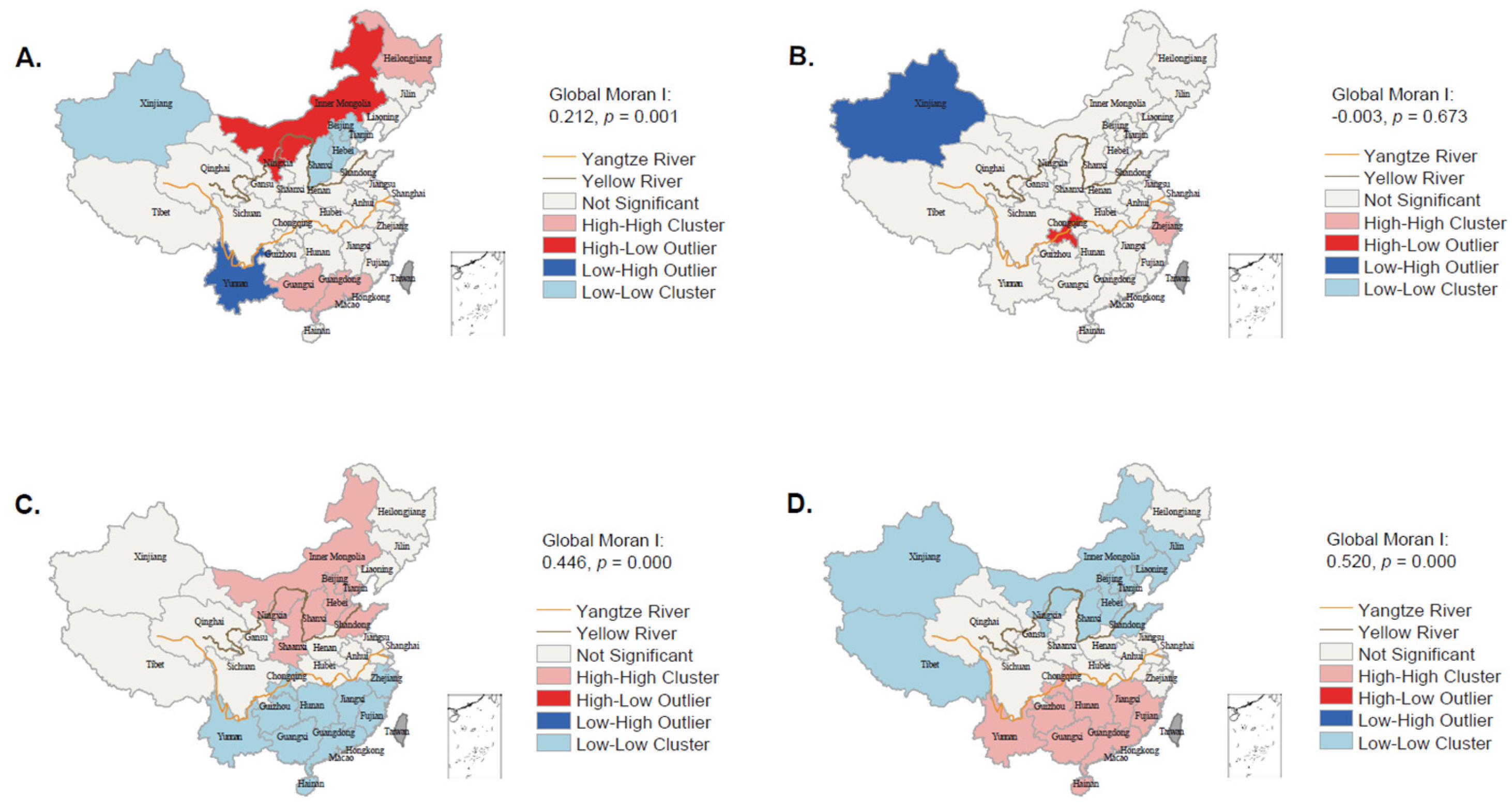
3.1. Geographic Variations in Dietary Patterns
3.2. Characteristics of Dietary Patterns
3.3. Socioeconomic and Lifestyle Factors Associated with Dietary Patterns
3.4. Association of Dietary Patterns with Overweight/Obesity and Hypertension
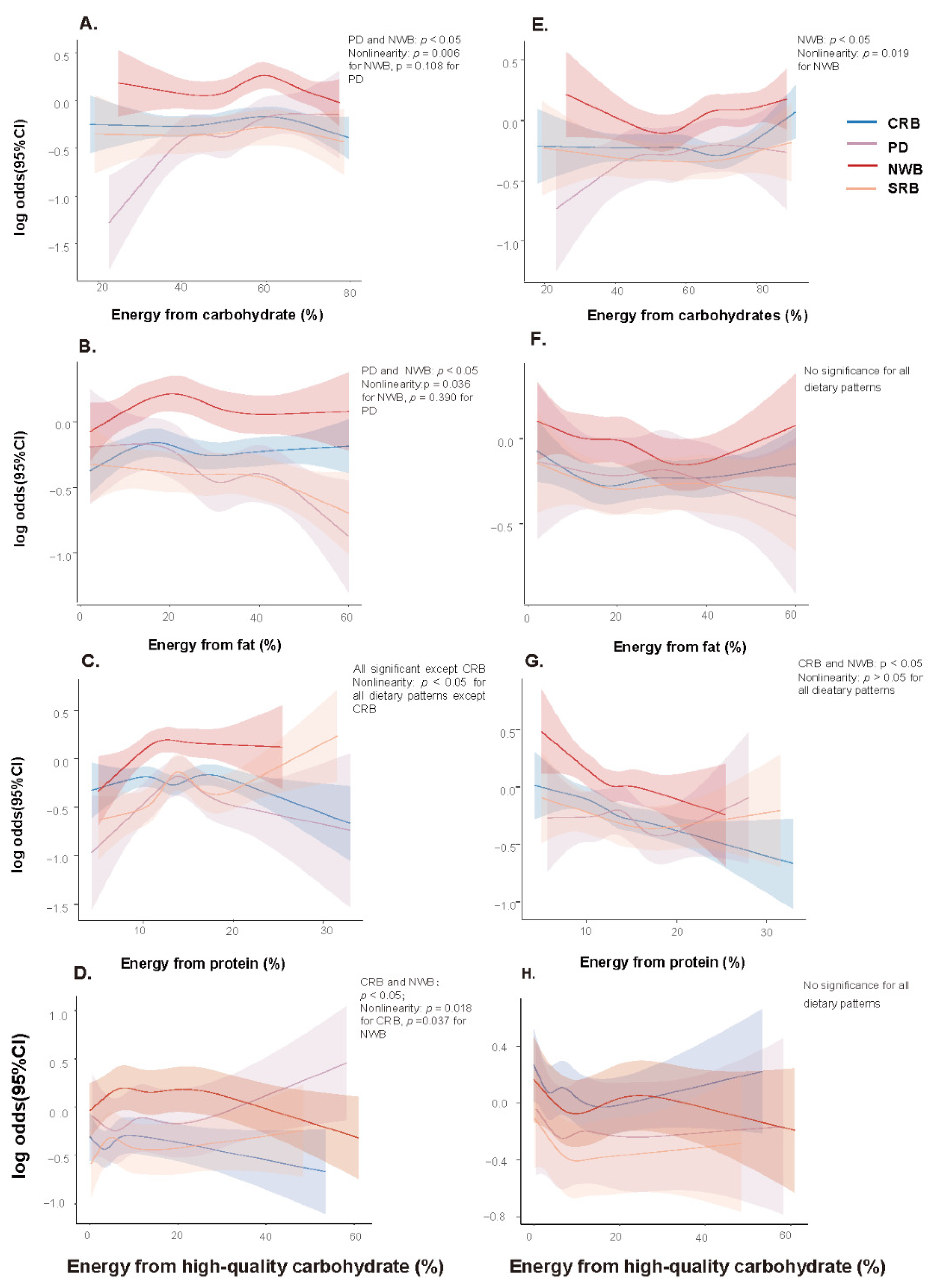
3.5. Associations of Estimated Percentage Energy from Macronutrients with Overweight/Obesity and Hypertension in Various Dietary Patterns
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wang, L.; Zhou, B.; Zhao, Z.; Yang, L.; Zhang, M.; Jiang, Y.; Li, Y.; Zhou, M.; Wang, L.; Huang, Z.; et al. Body-mass index and obesity in urban and rural China: Findings from consecutive nationally representative surveys during 2004–2018. Lancet 2021, 398, 53–63. [Google Scholar] [CrossRef]
- Zhou, M.; Wang, H.; Zeng, X.; Yin, P.; Zhu, J.; Chen, W.; Li, X.; Wang, L.; Wang, L.; Liu, Y.; et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 394, 1145–1158. [Google Scholar] [CrossRef]
- He, Y.; Li, Y.; Yang, X.; Hemler, E.C.; Fang, Y.; Zhao, L.; Zhang, J.; Yang, Z.; Wang, Z.; He, L.; et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982–2012: A cross-sectional population-based study. Lancet Diabetes Endocrinol. 2019, 7, 540–548. [Google Scholar] [CrossRef]
- Zhu, Z.; Yang, X.; Fang, Y.; Zhang, J.; Yang, Z.; Wang, Z.; Liu, A.; He, L.; Sun, J.; Lian, Y.; et al. Trends and Disparities of Energy Intake and Macronutrient Composition in China: A Series of National Surveys, 1982–2012. Nutrients 2020, 12, 2168. [Google Scholar] [CrossRef]
- Zhai, F.Y.; Du, S.F.; Wang, Z.H.; Zhang, J.G.; Du, W.W.; Popkin, B.M. Dynamics of the Chinese diet and the role of urbanicity, 1991–2011. Obes. Rev. 2014, 15 (Suppl. S1), S16–S26. [Google Scholar] [CrossRef]
- Popkin, B.M. Synthesis and implications: China’s nutrition transition in the context of changes across other low- and middle-income countries. Obes. Rev. 2014, 15 (Suppl. S1), S60–S67. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Shi, Y.; Shi, O.; Zhao, Z.; Zhang, X.; Li, C.; Huang, Z.; Zhao, L.; Wang, L.; Li, Y.; et al. Geographical variations in cardiovascular health in China: A nationwide population-based survey of 74,726 adults. Lancet Reg. Health West. Pac. 2020, 3, 100033. [Google Scholar] [CrossRef]
- Zhang, X.; Zhang, M.; Zhao, Z.; Huang, Z.; Deng, Q.; Li, Y.; Pan, A.; Li, C.; Chen, Z.; Zhou, M.; et al. Geographic Variation in Prevalence of Adult Obesity in China: Results From the 2013–2014 National Chronic Disease and Risk Factor Surveillance. Ann. Intern. Med. 2020, 172, 291–293. [Google Scholar] [CrossRef]
- Liu, S.; Li, Y.; Zeng, X.; Wang, H.; Yin, P.; Wang, L.; Liu, Y.; Liu, J.; Qi, J.; Ran, S.; et al. Burden of Cardiovascular Diseases in China, 1990–2016: Findings From the 2016 Global Burden of Disease Study. JAMA Cardiol. 2019, 4, 342–352. [Google Scholar] [CrossRef]
- Ma, G. Food, eating behavior, and culture in Chinese society. J. Ethn. Foods 2015, 2, 195–199. [Google Scholar] [CrossRef]
- Wang, J.; Lin, X.; Bloomgarden, Z.T.; Ning, G. The Jiangnan diet, a healthy diet pattern for Chinese. J. Diabetes 2020, 12, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Keys, A.; Menotti, A.; Karvonen, M.J.; Aravanis, C.; Blackburn, H.; Buzina, R.; Djordjevic, B.S.; Dontas, A.S.; Fidanza, F.; Keys, M.H.; et al. The diet and 15-year death rate in the seven countries study. Am. J. Epidemiol. 1986, 124, 903–915. [Google Scholar] [CrossRef] [PubMed]
- James, W.P.; Nelson, M.; Ralph, A.; Leather, S. Socioeconomic determinants of health: The contribution of nutrition to inequalities in health. BMJ 1997, 314, 1545–1549. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Creger, T.; Howard, V.; Judd, S.E.; Harrington, K.F.; Fontaine, K.R. Geospatial analysis of Mediterranean diet adherence in the United States. Public Health Nutr. 2021, 24, 2920–2928. [Google Scholar] [CrossRef]
- Czarnocinska, J.; Wadolowska, L.; Lonnie, M.; Kowalkowska, J.; Jezewska-Zychowicz, M.; Babicz-Zielinska, E. Regional and socioeconomic variations in dietary patterns in a representative sample of young polish females: A cross-sectional study (GEBaHealth project). Nutr. J. 2020, 19, 26. [Google Scholar] [CrossRef]
- Gao, L.; Bhurtyal, A.; Wei, J.; Akhtar, P.; Wang, L.; Wang, Y. Double Burden of Malnutrition and Nutrition Transition in Asia: A Case Study of 4 Selected Countries with Different Socioeconomic Development. Adv. Nutr. 2020, 11, 1663–1670. [Google Scholar] [CrossRef] [PubMed]
- The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 14 May 2022).
- Rehm, C.D.; Peñalvo, J.L.; Afshin, A.; Mozaffarian, D. Dietary Intake Among US Adults, 1999–2012. JAMA 2016, 315, 2542–2553. [Google Scholar] [CrossRef]
- Huang, L.; Wang, H.; Wang, Z.; Zhang, J.; Zhang, B.; Ding, G. Regional Disparities in the Association between Cereal Consumption and Metabolic Syndrome: Results from the China Health and Nutrition Survey. Nutrients 2019, 11, 764. [Google Scholar] [CrossRef]
- Song, F.; Cho, M.S. Geography of Food Consumption Patterns between South and North China. Foods 2017, 6, 34. [Google Scholar] [CrossRef]
- Liu, Y.; Zhang, H.; Zhao, Y.; Chen, F.; Mi, B.; Zhou, J.; Chen, Y.; Wang, D.; Pei, L. Geographical variations in maternal dietary patterns during pregnancy associated with birth weight in Shaanxi province, Northwestern China. PLoS ONE 2021, 16, e0254891. [Google Scholar] [CrossRef]
- Lee, S.A.; Cai, H.; Yang, G.; Xu, W.H.; Zheng, W.; Li, H.; Gao, Y.T.; Xiang, Y.B.; Shu, X.O. Dietary patterns and blood pressure among middle-aged and elderly Chinese men in Shanghai. Br. J. Nutr. 2010, 104, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; He, Y.; Li, Y.; Luan, D.; Yang, X.; Zhai, F.; Ma, G. Dietary patterns and hypertension among Chinese adults: A nationally representative cross-sectional study. BMC Public Health 2011, 11, 925. [Google Scholar] [CrossRef]
- Xiao, X.; Qin, Z.; Lv, X.; Dai, Y.; Ciren, Z.; Yangla, Y.; Zeng, P.; Ma, Y.; Li, X.; Wang, L.; et al. Dietary patterns and cardiometabolic risks in diverse less-developed ethnic minority regions: Results from the China Multi-Ethnic Cohort (CMEC) Study. Lancet Reg. Health West. Pac. 2021, 15, 100252. [Google Scholar] [CrossRef]
- Krusekopf, C.C. Diversity in land-tenure arrangements under the household responsibility system in China. China Econ. Rev. 2002, 13, 297–312. [Google Scholar] [CrossRef]
- Giskes, K.; Avendano, M.; Brug, J.; Kunst, A.E. A systematic review of studies on socioeconomic inequalities in dietary intakes associated with weight gain and overweight/obesity conducted among European adults. Obes. Rev. 2010, 11, 413–429. [Google Scholar] [CrossRef] [PubMed]
- Kearney, J. Food consumption trends and drivers. Philos. Trans. R. Soc. B Biol. Sci. 2010, 365, 2793–2807. [Google Scholar] [CrossRef]
- He, Y.; Zhao, W.; Zhang, J.; Zhao, L.; Yang, Z.; Huo, J.; Yang, L.; Wang, J.; He, L.; Sun, J.; et al. Data Resource Profile: China National Nutrition Surveys. Int. J. Epidemiol. 2019, 48, 368. [Google Scholar] [CrossRef]
- Yu, D.; Zhao, L.; Zhang, J.; Yang, Z.; Yang, L.; Huang, J. China Nutrition and Health Surveys (1982–2017). China CDC Wkly. 2021, 3, 193–195. [Google Scholar] [CrossRef]
- Yang, Y.X.; Wang, G.Y.; Pan, X.C. China Food Composition Tables 2009; Beijing Medical University Publishing House: Beijing, China, 2009. [Google Scholar]
- Yang, Y.N.; Chinese Center for Disease Control and Prevention. China Food Composition Tables 2018; Beijing Medical University Publishing House: Beijing, China, 2018.
- International Agency for Research on Cancer; W.H.O. Red Meat and Processed Meat; International Agency for Research on Cancer: Lyon, France, 2018. [Google Scholar]
- Wang, X.; Li, S.; Ma, Y.; Sun, J. Current situation of edible oil consumption of rural residents in China and its guidance. China Oils 2020, 45, 4. [Google Scholar] [CrossRef]
- Schulz, C.A.; Oluwagbemigun, K.; Nöthlings, U. Advances in dietary pattern analysis in nutritional epidemiology. Eur. J. Nutr. 2021, 60, 4115–4130. [Google Scholar] [CrossRef]
- Zhao, J.; Li, Z.; Gao, Q.; Zhao, H.; Chen, S.; Huang, L.; Wang, W.; Wang, T. A review of statistical methods for dietary pattern analysis. Nutr. J. 2021, 20, 37. [Google Scholar] [CrossRef] [PubMed]
- Fahey, M.T.; Thane, C.W.; Bramwell, G.D.; Coward, W.A. Conditional Gaussian mixture modelling for dietary pattern analysis. J. R. Stat. Society. Ser. A Stat. Soc. 2007, 170, 149–166. [Google Scholar] [CrossRef]
- Fraley, C.; Raftery, A.E. How Many Clusters? Which Clustering Method? Answers Via Model-Based Cluster Analysis. Comput. J. 1998, 41, 578–588. [Google Scholar] [CrossRef]
- Nutrition, C.S.O. Chinese Dietary Guidelines (2022); People’s Medical Publishing House: Beijing, China, 2022. [Google Scholar]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet. 2018, 118, 1591–1602. [Google Scholar] [CrossRef]
- Liese, A.D.; Nichols, M.; Sun, X.; D’Agostino, R.B., Jr.; Haffner, S.M. Adherence to the DASH Diet is inversely associated with incidence of type 2 diabetes: The insulin resistance atherosclerosis study. Diabetes Care 2009, 32, 1434–1436. [Google Scholar] [CrossRef]
- Chen, C.; Lu, F.C. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed. Environ. Sci. 2004, 17, 1–36. [Google Scholar]
- Liu, L.S. 2010 Chinese guidelines for the management of hypertension. Chin. J. Cardiovasc. Dis. 2011, 39, 579–615. [Google Scholar]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65 (Suppl. S4), 1220S–1228S, discussion 1229S–1231S. [Google Scholar] [CrossRef]
- Hall, J.E.; do Carmo, J.M.; da Silva, A.A.; Wang, Z.; Hall, M.E. Obesity-induced hypertension: Interaction of neurohumoral and renal mechanisms. Circ. Res. 2015, 116, 991–1006. [Google Scholar] [CrossRef]
- Vanderweele, T.J. Explanation in Causal Inference: Methods for Mediation and Interaction; Oxford University Press: New York, NY, USA, 2015. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing. 2022. Available online: https://www.R-project.org/ (accessed on 12 November 2020).
- Society, C.N. Chinese Dietary Reference Intakes (2013); Science Press: Beijing, China, 2013. [Google Scholar]
- Su, C.; Jia, X.F.; Wang, Z.H.; Wang, H.J.; Ouyang, Y.F.; Zhang, B. Longitudinal association of leisure time physical activity and sedentary behaviors with body weight among Chinese adults from China Health and Nutrition Survey 2004–2011. Eur. J. Clin. Nutr. 2017, 71, 383–388. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, Z.; Du, W.; Huang, F.; Jiang, H.; Bai, J.; Zhang, X.; Zhang, B.; Wang, H. Twenty-Five-Year Trends in Dietary Patterns among Chinese Adults from 1991 to 2015. Nutrients 2021, 13, 1327. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.; Wang, Z.; Wang, H.; Zhao, L.; Jiang, H.; Zhang, B.; Ding, G. Nutrition transition and related health challenges over decades in China. Eur. J. Clin. Nutr. 2021, 75, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Zhao, L.; Zhao, W. Status and trends in consumption of grains and dietary fiber among Chinese adults (1982–2015). Nutr. Rev. 2020, 78, 43–53. [Google Scholar] [CrossRef]
- Ma, P. The influence of geographical environment upon dietetic culture differences between the North and the South in China: A case study of Guanzhong of Shaanxi and southeast of Guizhou. J. Carey Coll. 2010, 28, 5. [Google Scholar]
- He, Y.; Ma, G.; Zhai, F.; Li, Y.; Hu, Y.; Feskens, E.J.; Yang, X. Dietary patterns and glucose tolerance abnormalities in Chinese adults. Diabetes Care 2009, 32, 1972–1976. [Google Scholar] [CrossRef]
- Zhang, J.; Wang, Z.; Wang, H.; Du, W.; Su, C.; Zhang, J.; Jiang, H.; Jia, X.; Huang, F.; Zhai, F.; et al. Association between dietary patterns and blood lipid profiles among Chinese women. Public Health Nutr. 2016, 19, 3361–3368. [Google Scholar] [CrossRef] [PubMed]
- Lacko, A.; Delamater, P.; Gordon-Larsen, P.; Ng, S.W. Geographic patterns and socioeconomic differences in the nutritional quality of household packaged food purchases in the United States. Health Place 2021, 69, 102567. [Google Scholar] [CrossRef]
- Allen, L.; Williams, J.; Townsend, N.; Mikkelsen, B.; Roberts, N.; Foster, C.; Wickramasinghe, K. Socioeconomic status and non-communicable disease behavioural risk factors in low-income and lower-middle-income countries: A systematic review. Lancet Glob. Health 2017, 5, e277–e289. [Google Scholar] [CrossRef]
- Dekker, L.H.; Rijnks, R.H.; Strijker, D.; Navis, G.J. A spatial analysis of dietary patterns in a large representative population in the north of The Netherlands-the Lifelines cohort study. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 166. [Google Scholar] [CrossRef]
- Springmann, M.; Wiebe, K.; Mason-D’Croz, D.; Sulser, T.B.; Rayner, M.; Scarborough, P. Health and nutritional aspects of sustainable diet strategies and their association with environmental impacts: A global modelling analysis with country-level detail. Lancet Planet. Health 2018, 2, e451–e461. [Google Scholar] [CrossRef]
- Cong, N.; Zhao, A.; Gong, P. Food Delivery Platform: A Potential Tool for Monitoring the Food Environment and Mitigating Overweight/Obesity in China. Front. Nutr. 2021, 8, 703090. [Google Scholar] [CrossRef] [PubMed]
- Lam, H.M.; Remais, J.; Fung, M.C.; Xu, L.; Sun, S.S. Food supply and food safety issues in China. Lancet 2013, 381, 2044–2053. [Google Scholar] [CrossRef]
- Kuehn, B.M. Heritage Diets and Culturally Appropriate Dietary Advice May Help Combat Chronic Diseases. JAMA 2019, 322, 2271–2273. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Wang, J.; Sun, L.; Gu, W.; Zong, G.; Song, B.; Shen, C.; Zhou, P.; Chen, Y.; Wu, Y.; et al. Isocaloric-restricted Mediterranean diet and Chinese diets high or low in plants in adults with prediabetes. J. Clin. Endocrinol. Metab. 2022, 107, 2216–2227. [Google Scholar] [CrossRef]
- Zhang, S. Geographic Research of Food Culture in China. Yunnan Geogr. Environ. Res. 2009, 21, 27–31. [Google Scholar]
- André, P.; Proctor, G.; Driollet, B.; Garcia-Esquinas, E.; Lopez-Garcia, E.; Gomez-Cabrero, D.; Neyraud, E.; Rodriguez-Artalejo, F.; Morzel, M.; Féart, C. The role of overweight in the association between the Mediterranean diet and the risk of type 2 diabetes mellitus: A mediation analysis among 21 585 UK biobank participants. Int. J. Epidemiol. 2020, 49, 1582–1590. [Google Scholar] [CrossRef] [PubMed]
- Schoenaker, D.A.; Soedamah-Muthu, S.S.; Mishra, G.D. Quantifying the mediating effect of body mass index on the relation between a Mediterranean diet and development of maternal pregnancy complications: The Australian Longitudinal Study on Women’s Health. Am. J. Clin. Nutr. 2016, 104, 638–645. [Google Scholar] [CrossRef]
- Naude, C.E.; Brand, A.; Schoonees, A.; Nguyen, K.A.; Chaplin, M.; Volmink, J. Low-carbohydrate versus balanced-carbohydrate diets for reducing weight and cardiovascular risk. Cochrane Database Syst. Rev. 2022, 2022, Cd013334. [Google Scholar] [CrossRef]
- Ge, L.; Sadeghirad, B.; Ball, G.D.C.; da Costa, B.R.; Hitchcock, C.L.; Svendrovski, A.; Kiflen, R.; Quadri, K.; Kwon, H.Y.; Karamouzian, M.; et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: Systematic review and network meta-analysis of randomised trials. Bmj 2020, 369, m696. [Google Scholar] [CrossRef]
- Wan, Y.; Wang, F.; Yuan, J.; Li, J.; Jiang, D.; Zhang, J.; Huang, T.; Zheng, J.; Mann, J.; Li, D. Effects of Macronutrient Distribution on Weight and Related Cardiometabolic Profile in Healthy Non-Obese Chinese: A 6-month, Randomized Controlled-Feeding Trial. EBioMedicine 2017, 22, 200–207. [Google Scholar] [CrossRef]
- Wan, Y.; Wang, F.; Yuan, J.; Li, J.; Jiang, D.; Zhang, J.; Li, H.; Wang, R.; Tang, J.; Huang, T.; et al. Effects of dietary fat on gut microbiota and faecal metabolites, and their relationship with cardiometabolic risk factors: A 6-month randomised controlled-feeding trial. Gut 2019, 68, 1417–1429. [Google Scholar] [CrossRef]
- Hall, K.D.; Farooqi, I.S.; Friedman, J.M.; Klein, S.; Loos, R.J.F.; Mangelsdorf, D.J.; O’Rahilly, S.; Ravussin, E.; Redman, L.M.; Ryan, D.H.; et al. The energy balance model of obesity: Beyond calories in, calories out. Am. J. Clin. Nutr. 2022, 115, 1243–1254. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, D.S.; Aronne, L.J.; Astrup, A.; de Cabo, R.; Cantley, L.C.; Friedman, M.I.; Heymsfield, S.B.; Johnson, J.D.; King, J.C.; Krauss, R.M.; et al. The carbohydrate-insulin model: A physiological perspective on the obesity pandemic. Am. J. Clin. Nutr. 2021, 114, 1873–1885. [Google Scholar] [CrossRef]
- Li, Q.; Liu, C.; Zhang, S.; Li, R.; Zhang, Y.; He, P.; Zhang, Z.; Li, M.; Zhou, C.; Ye, Z.; et al. Dietary Carbohydrate Intake and New-Onset Hypertension: A Nationwide Cohort Study in China. Hypertension. 2021, 78, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Miyazawa, I.; Miura, K.; Miyagawa, N.; Kondo, K.; Kadota, A.; Okuda, N.; Fujiyoshi, A.; Chihara, I.; Nakamura, Y.; Hozawa, A.; et al. Relationship between carbohydrate and dietary fibre intake and the risk of cardiovascular disease mortality in Japanese: 24-year follow-up of NIPPON DATA80. Eur. J. Clin. Nutr. 2020, 74, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Yu, D.; Zhang, X.; Shu, X.O.; Cai, H.; Li, H.; Ding, D.; Hong, Z.; Xiang, Y.B.; Gao, Y.T.; Zheng, W.; et al. Dietary glycemic index, glycemic load, and refined carbohydrates are associated with risk of stroke: A prospective cohort study in urban Chinese women. Am. J. Clin. Nutr. 2016, 104, 1345–1351. [Google Scholar] [CrossRef]
- Kjølbæk, L.; Sørensen, L.B.; Søndertoft, N.B.; Rasmussen, C.K.; Lorenzen, J.K.; Serena, A.; Astrup, A.; Larsen, L.H. Protein supplements after weight loss do not improve weight maintenance compared with recommended dietary protein intake despite beneficial effects on appetite sensation and energy expenditure: A randomized, controlled, double-blinded trial. Am. J. Clin. Nutr. 2017, 106, 684–697. [Google Scholar] [CrossRef]
- Lotfi, K.; Mohammadi, S.; Mirzaei, S.; Asadi, A.; Akhlaghi, M.; Saneei, P. Dietary total, plant and animal protein intake in relation to metabolic health status in overweight and obese adolescents. Sci. Rep. 2022, 12, 10055. [Google Scholar] [CrossRef]
- Myrmel, L.S.; Fauske, K.R.; Fjære, E.; Bernhard, A.; Liisberg, U.; Hasselberg, A.E.; Øyen, J.; Kristiansen, K.; Madsen, L. The Impact of Different Animal-Derived Protein Sources on Adiposity and Glucose Homeostasis during Ad Libitum Feeding and Energy Restriction in Already Obese Mice. Nutrients 2019, 11, 1153. [Google Scholar] [CrossRef]
- Larsen, T.M.; Dalskov, S.M.; van Baak, M.; Jebb, S.A.; Papadaki, A.; Pfeiffer, A.F.; Martinez, J.A.; Handjieva-Darlenska, T.; Kunešová, M.; Pihlsgård, M.; et al. Diets with high or low protein content and glycemic index for weight-loss maintenance. N. Engl. J. Med. 2010, 363, 2102–2113. [Google Scholar] [CrossRef]
- Meng, S.; Cui, Z.; Li, M.; Li, T.; Wu, F.; Kang, T.; Meng, H. Associations between Dietary Animal and Plant Protein Intake and Cardiometabolic Risk Factors—A Cross-Sectional Study in China Health and Nutrition Survey. Nutrients 2021, 13, 336. [Google Scholar] [CrossRef] [PubMed]
- Rouhani, M.H.; Salehi-Abargouei, A.; Surkan, P.J.; Azadbakht, L. Is there a relationship between red or processed meat intake and obesity? A systematic review and meta-analysis of observational studies. Obes. Rev. 2014, 15, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Schlesinger, S.; Neuenschwander, M.; Schwedhelm, C.; Hoffmann, G.; Bechthold, A.; Boeing, H.; Schwingshackl, L. Food Groups and Risk of Overweight, Obesity, and Weight Gain: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2019, 10, 205–218. [Google Scholar] [CrossRef]
- Giromini, C.; Givens, D.I. Benefits and Risks Associated with Meat Consumption during Key Life Processes and in Relation to the Risk of Chronic Diseases. Foods 2022, 11, 2063. [Google Scholar] [CrossRef] [PubMed]
- Schwingshackl, L.; Schwedhelm, C.; Hoffmann, G.; Knüppel, S.; Iqbal, K.; Andriolo, V.; Bechthold, A.; Schlesinger, S.; Boeing, H. Food Groups and Risk of Hypertension: A Systematic Review and Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2017, 8, 793–803. [Google Scholar] [CrossRef]
- Li, P.; Zhang, M.; Zhu, Y.; Liu, W.; Zhang, Y.; Gao, Y.; Huang, G. Dietary patterns and changes in cardiovascular risk factors in apparently healthy Chinese women: A longitudinal study. J. Clin. Biochem. Nutr. 2016, 58, 232–239. [Google Scholar] [CrossRef]
- Wang, Z.; Zhang, B.; Zhai, F.; Wang, H.; Zhang, J.; Du, W.; Su, C.; Zhang, J.; Jiang, H.; Popkin, B.M. Fatty and lean red meat consumption in China: Differential association with Chinese abdominal obesity. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 869–876. [Google Scholar] [CrossRef]
- Lee, J.E.; McLerran, D.F.; Rolland, B.; Chen, Y.; Grant, E.J.; Vedanthan, R.; Inoue, M.; Tsugane, S.; Gao, Y.T.; Tsuji, I.; et al. Meat intake and cause-specific mortality: A pooled analysis of Asian prospective cohort studies. Am. J. Clin. Nutr. 2013, 98, 1032–1041. [Google Scholar] [CrossRef]
- Nestel, P.J. Dietary Fat and Blood Pressure. Curr. Hypertens. Rep. 2019, 21, 17. [Google Scholar] [CrossRef]
- Steur, M.; Johnson, L.; Sharp, S.J.; Imamura, F.; Sluijs, I.; Key, T.J.; Wood, A.; Chowdhury, R.; Guevara, M.; Jakobsen, M.U.; et al. Dietary Fatty Acids, Macronutrient Substitutions, Food Sources and Incidence of Coronary Heart Disease: Findings From the EPIC-CVD Case-Cohort Study Across Nine European Countries. J. Am. Heart Assoc. 2021, 10, e019814. [Google Scholar] [CrossRef]
- Li, Y.P.; He, Y.N.; Zhai, F.Y.; Yang, X.G.; Hu, X.Q.; Zhao, W.H.; Ma, G.S. Comparison of assessment of food intakes by using 3 dietary survey methods. Chin. J. Prev. Med. 2006, 40, 273–280. [Google Scholar]



| Indicators | CRB | PD | NWB | SRB |
|---|---|---|---|---|
| Energy, kcal | 1395 (1058,1801) | 1530 (1220, 1927) | 1495 (1171, 1899) | 1540 (1165, 1978) |
| Protein, g | 45.6 (33.8, 60.4) | 53.2 (40.1, 68.9) | 46.7 (36.0, 59.8) | 52.1 (39.0, 67.5) |
| Protein, % kcal, mean (SD) | 13.5 (4.0) | 14.2 (3.9) | 12.8 (2.8) | 14.0 (4.0) |
| Animal protein, % | 35.3 (19.9, 50.2) | 41.7 (26.9, 54.5) | 20.3 (8.4, 35.0) | 42.3 (28.6, 55.0) |
| Total fat, g | 40.6 (22.4,66.6) | 50.4 (31.3, 75.6) | 34.9 (18.1, 59.3) | 46.4 (26.7, 74.2) |
| Total fat, % kcal | 26.9 (16.8, 38.1) | 30.6 (21.0, 39.7) | 21.5 (12.7, 32.0) | 27.8 (18.9, 38.3) |
| MUFA, % kcal | 9.4 (5.5, 14.2) | 10.7 (7.0, 15.5) | 7.0 (3.7, 11.1) | 10.4 (6.7, 15.0) |
| Animal MUFA, % kcal | 4.6 (2.0, 7.8) | 4.9 (2.6, 7.6) | 2.3 (0.6, 4.6) | 7.5 (4.4, 11.8) |
| PUFA, % kcal | 4.3 (2.7, 8.9) | 5.4 (2.9, 9.5) | 4.4 (2.4, 8.9) | 3.6 (2.4, 5.6) |
| SFA, % kcal | 6.6 (4.3, 9.1) | 7.5 (5.4, 9.7) | 5.4 (3.4, 7.7) | 8.4 (5.7, 11.6) |
| Total carbohydrate, g | 196.4 (147.3, 261.4) | 207.3 (160.6, 268.4) | 240.5 (184.7, 304.7) | 209.5 (156.0, 276.0) |
| Total carbohydrate, % kcal | 59.3 (48.3, 69.8) | 55.8 (46.3, 65.5) | 66.6 (56.2, 75.5) | 57.1 (46.7, 67.0) |
| High-quality carbohydrate, % | 10.5 (6.3, 18.6) | 18.7 (11.1, 30.1) | 19.4 (10.6, 30.7) | 13.9 (7.8, 23.0) |
| Fiber, g | 6.8 (5.8, 18.2) | 8.4 (5.9, 12.1) | 9.5 (6.9, 12.9) | 7.4 (5.4, 10.7) |
| Dietary Pattern | Mediator | ORNIE (95%CI) | ORNDE (95%CI) | ORTE (95%CI) a | PM (%) b |
|---|---|---|---|---|---|
| PD | Overweight/obesity | 0.98 (0.97–1.00) | 0.86 (0.80–0.93) | 0.85 (0.78–0.91) | 9.9 |
| NWB | Overweight/obesity | 1.07 (1.06–1.08) | 1.09 (1.03–1.15) | 1.17 (1.10–1.23) | 43.2 |
| SRB | Overweight/obesity | 0.97 (0.96–0.98) | 0.92 (0.87–0.97) | 0.89 (0.84–0.95) | 27.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, R.; Zhao, L.; Gao, X.; Yang, F.; Yang, Y.; Fang, H.; Ju, L.; Xu, X.; Guo, Q.; Li, S.; et al. Geographic Variations in Dietary Patterns and Their Associations with Overweight/Obesity and Hypertension in China: Findings from China Nutrition and Health Surveillance (2015–2017). Nutrients 2022, 14, 3949. https://doi.org/10.3390/nu14193949
Zhao R, Zhao L, Gao X, Yang F, Yang Y, Fang H, Ju L, Xu X, Guo Q, Li S, et al. Geographic Variations in Dietary Patterns and Their Associations with Overweight/Obesity and Hypertension in China: Findings from China Nutrition and Health Surveillance (2015–2017). Nutrients. 2022; 14(19):3949. https://doi.org/10.3390/nu14193949
Chicago/Turabian StyleZhao, Rongping, Liyun Zhao, Xiang Gao, Fan Yang, Yuxiang Yang, Hongyun Fang, Lahong Ju, Xiaoli Xu, Qiya Guo, Shujuan Li, and et al. 2022. "Geographic Variations in Dietary Patterns and Their Associations with Overweight/Obesity and Hypertension in China: Findings from China Nutrition and Health Surveillance (2015–2017)" Nutrients 14, no. 19: 3949. https://doi.org/10.3390/nu14193949
APA StyleZhao, R., Zhao, L., Gao, X., Yang, F., Yang, Y., Fang, H., Ju, L., Xu, X., Guo, Q., Li, S., Cheng, X., Cai, S., Yu, D., & Ding, G. (2022). Geographic Variations in Dietary Patterns and Their Associations with Overweight/Obesity and Hypertension in China: Findings from China Nutrition and Health Surveillance (2015–2017). Nutrients, 14(19), 3949. https://doi.org/10.3390/nu14193949






