Cardiometabolic Biomarkers and Habitual Caffeine Consumption Associate with the Adverse Ambulatory Blood Pressure Response to Strenuous Physical Exertion among Firefighters
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Overview
2.2. Subjects
2.3. Study Design
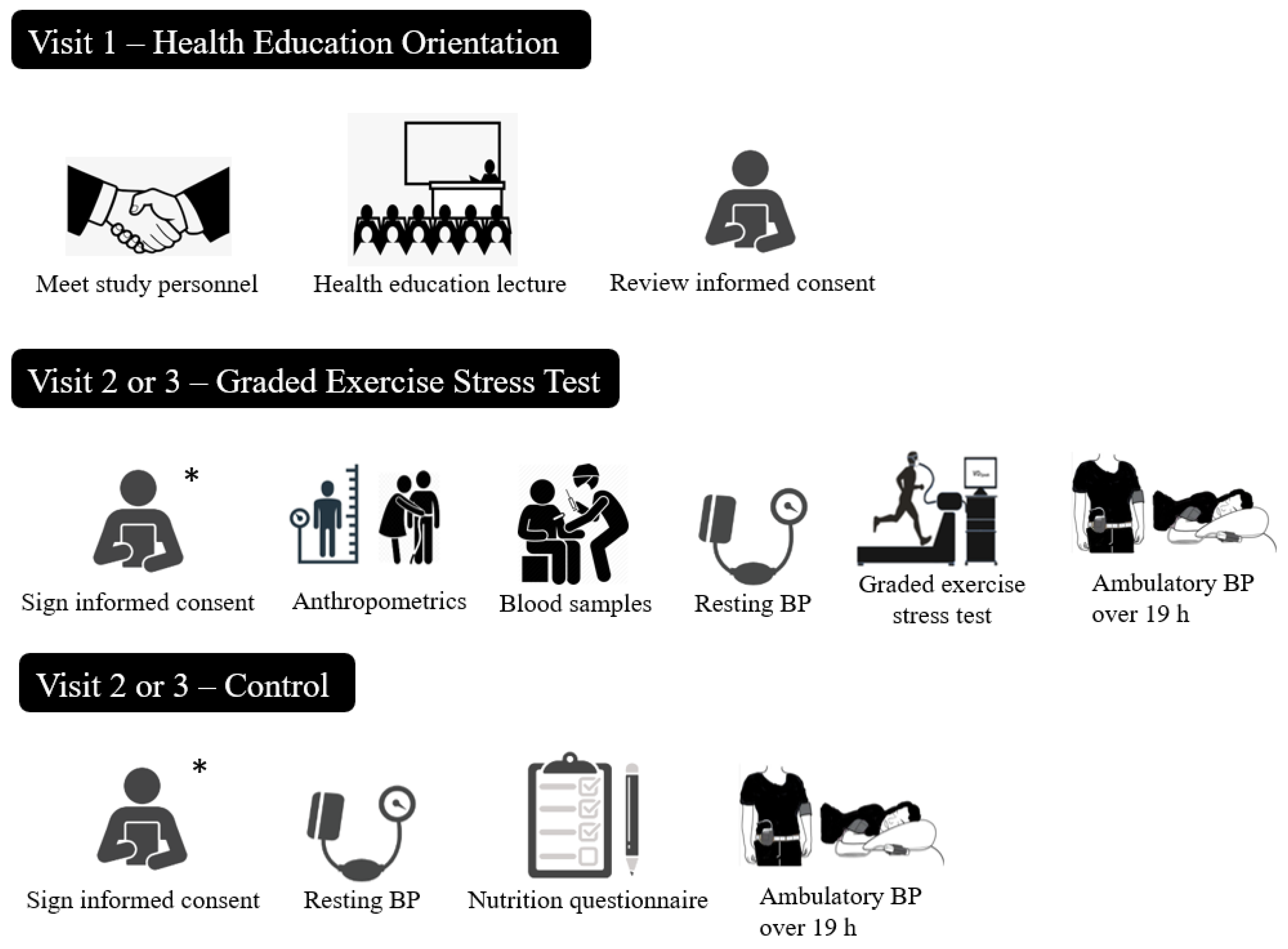
2.3.1. Visit 1: Health Education Orientation Session
2.3.2. Visit 2 or 3: Cardiovascular Health Testing
2.4. Study Procedures
2.4.1. Dietary Intake—Food-Frequency Questionnaire
2.4.2. Dietary Approaches to Stop Hypertension
2.4.3. Anthropometric Measurements
2.4.4. Resting Blood Pressure
2.4.5. Blood Sampling and Analysis
2.4.6. Ambulatory Blood Pressure
2.5. Statistical Analyses
3. Results
3.1. Subject Descriptive Characteristics
3.2. Nutrient Intake
3.3. Dietary Approaches to Stop Hypertension
3.4. The Ambulatory Blood Pressure Response to Exercise
3.5. The Influence of Dietary Intake and the Cardiometabolic Biomarkers on the Ambulatory Blood Pressure Response to Exercise
3.5.1. Caffeine
3.5.2. Calcium
3.5.3. Sodium
3.6. The Influence of Dietary Intake on Resting Blood Pressure
4. Discussion
4.1. Caffeine and the Cardiometabolic Biomarkers Associated with the ABP Response
4.2. Calcium and the Cardiometabolic Biomarkers Associated with the ABP Response
4.3. Sodium and the Cardiometabolic Biomarkers Associated with the ABP Response
4.4. Dietary Approaches to Stop Hypertension
4.5. Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Korre, M.; Sotos-Prieto, M.; Kales, S. Survival Mediterranean Style: Lifestyle Changes to Improve the Health of the US Fire Service. Front. Public Health 2017, 5, 331. [Google Scholar] [CrossRef] [PubMed]
- Kales, S.; Tsismenakis, A.; Zhang, C.; Soteriades, E. Blood Pressure in Firefighters, Police Officers, and Other Emergency Responders. Am. J. Hypertens. 2009, 22, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Rhoades, J.; Favorite, K. A Fire Department’s Guide to Implementing NFPA 1582; National Fire Protection Association: Quincy, MA, USA, 2013; p. 118. [Google Scholar]
- Smith, D.; DeBlois, J.; Kales, S.; Horn, G. Cardiovascular Strain of Firefighting and the Risk of Sudden Cardiac Events. Exerc. Sport Sci. Rev. 2016, 44, 90–97. [Google Scholar] [CrossRef]
- Khaja, S.; Mathias, K.; Bode, E.; Stewart, D.; Stewart, D.; Jack, K.; Moffatt, S.; Smith, D. Hypertension in the United States Fire Service. Int. J. Environ. Res. Public Health 2021, 18, 5432. [Google Scholar] [CrossRef]
- Smith, D.; Graham, E.; Douglas, J.; Jack, K.; Conner, M.; Arena, R.; Chaudhry, S. Subclinical Cardiac Dysfunction is Associated with Reduced Cardiorespiratory Fitness and Cardiometabolic Risk Factors in Firefighters. Am. J. Med. 2022, 135, 752–760. [Google Scholar] [CrossRef]
- Carey, M.; Al-Zaiti, S.; Liao, L.; Martin, H.; Butler, R. A Low-Glycemic Nutritional Fitness Program to Reverse Metabolic Syndrome in Professional Firefighters. J. Cardiovasc. Nurs. 2011, 26, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Markel, T. 2021 National Fire Service Research Agenda. 2022, pp. 1–93. Available online: www.everyonegoeshome.com (accessed on 7 February 2022).
- Pescatello, L.S.; Buchner, D.M.; Jakicic, J.M.; Powell, K.E.; Kraus, W.E.; Bloodgood, B.; Campbell, W.W.; Dietz, S.; Dipietro, L.; George, S.M.; et al. Physical Activity to Prevent and Treat Hypertension: A Systematic Review. Med. Sci. Sports Exerc. 2019, 51, 1314–1323. [Google Scholar] [CrossRef]
- Pescatello, L.; Guidry, M.; Blanchard, B.; Kerra, A.; Taylor, A.; Johnson, A.; Maresha, C.; Rodriguez, N.; Thompson, P. Exercise Intensity Alters Postexercise Hypotension. J. Hypertens. 2004, 22, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Eicher, J.; Maresh, C.; Tsongalis, G.; Thompson, P.; Pescatello, S. The Additive Blood Pressure Lowering Effects of Exercise Intensity on Post-Exercise Hypotension. Am. Heart J. 2010, 160, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Pescatello, L.; MacDonald, H.; Lamberti, L.; Johnson, B. Exercise for Hypertension: A Prescription Update Integrating Existing Recommendations with Emerging Research. Curr. Hypertens. Rep. 2015, 17, 87. [Google Scholar] [CrossRef] [Green Version]
- Rynne, P.; Donahue, S.; Carty, M.; Dickinson, R.; Lashley, M.; Reeve, E.; Gilpin, J.; McMorrow, C.; Almeida, A.; Sherman, W.; et al. A High Physiological Stress Response is Dependent on Call Type in Firefighters. Circulation 2021, 144, A12778. [Google Scholar]
- Sarmento Da Nóbrega, T.; Moura Junior, J.; Bandeira Alves, N.; Da Cruz Santos, A.; Silva, A. The Coffee Intake Leads to Abolition of Aerobic Exercise Induced Hypotension: A Pilot Study. Rev. Da Educ. Fis. 2011, 22, 601–612. [Google Scholar]
- Notarius, C.; Morris, B.; Floras, J. Caffeine Attenuates Early Post-Exercise Hypotension in Middle-Aged Subjects. Am. J. Hypertens. 2006, 19, 184–188. [Google Scholar] [CrossRef]
- Pescatello, L.S.; Turner, D.; Rodriguez, N.; Blanchard, B.E.; Tsongalis, G.J.; Maresh, C.M.; Duffy, V.; Thompson, P.D. Dietary Calcium Intake and Renin Angiotensin System Polymorphisms Alter the Blood Pressure Response to Aerobic Exercise: A Randomized Control Design. Nutr. Metab. 2007, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Babcock, M.; Robinson, A.; Watso, J.; Migdal, K.; Martens, C.; Edwards, D.; Pescatello, L.; Farquhar, W. Salt Loading Blunts Central and Peripheral Postexercise Hypotension. Med. Sci. Sports Exerc. 2020, 52, 935–943. [Google Scholar] [CrossRef] [PubMed]
- Babcock, M.; Robinson, A.; Migdal, K.; Watso, J.; Martens, C.; Edwards, D.; Pescatello, L.; Farquhar, W. High Salt Intake Augments Blood Pressure Responses during Submaximal Aerobic Exercise. J. Am. Heart Assoc. 2020, 9, e015633. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.; Bakris, G.; Black, H.; Cushman, W.; Green, L.; Izzo, J.; Jones, D.; Materson, B.; Oparil, S.; Wright, J. Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef] [PubMed]
- Ash, G.; Walker, T.; Olson, K.; Stratton, J.; Gomez, A.; Kraemer, W.; Volek, J.; Pescatello, L. Reproducibility of Ambulatory Blood Pressure Changes from the Initial Values on Two Different Days. Clinics 2013, 68, 1509–1515. [Google Scholar] [CrossRef]
- Balke, B.; Ware, R. The Present Status of Physical Fitness in the Air Force. Proj. Rep. USAF Sch. Aviat. Med. 1959, 59, 1–9. [Google Scholar]
- Willett, W.; Reynolds, R.; Cottrell-Hoehner, S.; Sampson, L.; Browne, M. Validation of a Semi-Quantitative Food Frequency Questionnaire: Comparison with a 1-Year Diet Record. J. Am. Diet. Assoc. 1987, 87, 43–47. [Google Scholar] [CrossRef]
- Kushi, L.; Fee, R.; Folsom, A.; Mink, P.; Anderson, K.; Sellers, T. Physical Activity and Mortality in Postmenopausal Women. JAMA 1997, 277, 1287–1292. [Google Scholar] [CrossRef] [PubMed]
- Munger, R.; Folsom, A.; Kushi, L.; Kaye, S.; Sellers, T. Dietary Assessment of Older Iowa Women with a Food Frequency Questionnaire: Nutrient Intake, Reproducibility, and Comparison with 24-Hour Dietary Recall Interviews. Am. J. Epidemiol. 1992, 136, 192–200. [Google Scholar] [CrossRef] [PubMed]
- Salvini, S.; Hunter, D.; Sampson, L.; Stampfer, M.; Colditz, G.; Rosner, B.; Willett, W. Food-Based Validation of a Dietary Questionnaire: The Effects of Week-to-Week Variation in Food Consumption. Int. J. Epidemiol. 1989, 18, 858–867. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Andrade, F. Diagnostic Status of Hypertension on the Adherence to the Dietary Approaches to Stop Hypertension (DASH) Diet. Prev. Med. Rep. 2016, 4, 525–531. [Google Scholar] [CrossRef]
- Mellen, P.; Gao, S.; Vitolins, M.; Goff, D. Deteriorating Dietary Habits among Adults with Hypertension: DASH Dietary Accordance, NHANES 1988–1994 and 1999–2004. Arch. Intern. Med. 2008, 168, 308–314. [Google Scholar] [CrossRef]
- Pickering, T.; Hall, J.; Appel, L.; Falkner, B.; Graves, J.; Hill, M.; Jones, D.; Kurtz, T.; Sheps, S.; Roccella, E. Recommendations for Blood Pressure Measurement in Humans and Experimental Animals: Part 1: Blood Pressure Measurement in Humans: A Statement for Professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005, 111, 697–716. [Google Scholar]
- Data Innovations. Total Allowable Error Table. 2020. Available online: https://datainnovations.com/allowable-total-error-table (accessed on 30 June 2020).
- Ibrahim, J.; Chen, M.; Lipsitz, S.; Herring, A. Missing-Data Methods for Generalized Linear Models: A Comparative Review. J. Am. Stat. Assoc. 2005, 100, 332–347. [Google Scholar] [CrossRef]
- Pescatello, L.; Schifano, E.; Ash, G.; Panza, G.; Corso, L.; Chen, M.; Deshpande, V.; Zaleski, A.; Cilhoroz, B.; Farinatti, P.; et al. Deep-Targeted Sequencing of Endothelial Nitric Oxide Synthase Gene Exons Uncovers Exercise Intensity and Ethnicity-Dependent Associations with Post-Exercise Hypotension. Physiol. Rep. 2017, 5, e13510. [Google Scholar] [CrossRef]
- Johnson, P.; Barry, S.; Ferguson, H.; Müller, P. Power Analysis for Generalized Linear Mixed Models in Ecology and Evolution. Methods Ecol. Evol. 2015, 6, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Holm, S. A Simple Sequentially Rejective Multiple Test Procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Sheather, S. A Modern Approach to Regression with R; Springer: New York, NY, USA, 2009. [Google Scholar]
- National Heart, Lung, and Blood Institute. Classification of Overweight and Obesity by BMI, Waist Circumference, and Associated Disease Risks. 2022. Available online: https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmi_dis.htm (accessed on 2 June 2022).
- Riebe, D. American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription, 10th ed.; Lippincott Williams & Wilkins: Philadelpha, PA, USA, 2018. [Google Scholar]
- O’Brien, E.; Parati, G.; Stergiou, G.; Asmar, R.; Beilin, L.; Bilo, G.; Clement, D.; de la Sierra, A. European Society of Hypertension Position Paper on Ambulatory Blood Pressure Monitoring. J. Hypertens. 2013, 31, 1731–1768. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Nutrient Recommendations: Dietary Reference Intakes (DRI). 2020. Available online: https://ods.od.nih.gov/HealthInformation/nutrientrecommendations.aspx (accessed on 7 August 2020).
- Noh, J.; Lee, C.; Hyun, D.; Kim, W.; Kim, M.; Park, K.; Koh, S.; Chang, S.; Kim, C.; Park, S. Blood Pressure and the Risk of Major Adverse Cardiovascular Events among Firefighters. J. Hypertens. 2020, 38, 850–857. [Google Scholar] [CrossRef] [PubMed]
- Temple, J.; Hostler, D.; Martin-Gill, C.; Moore, C.; Weiss, P.; Sequeira, D.; Condle, J.; Lang, S.; Higgins, J.; Patterson, P. Systematic Review and Meta-Analysis of the Effects of Caffeine in Fatigued Shift Workers: Implications for Emergency Medical Services Personnel. Prehosp. Emerg. Care 2018, 22, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Caldwell, J.; Caldwell, J.; Thompson, L.; Lieberman, H. Fatigue and its Management in the Workplace. Neurosci. Biobehav. Rev. 2019, 96, 272–289. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Steptoe, A. Vascular Inflammation and Blood Pressure Response to Acute Exercise. Eur. J. Appl. Physiol. 2012, 112, 2375–2379. [Google Scholar] [CrossRef] [PubMed]
- Sesso, H.; Buring, J.; Rifai, N.; Blake, G.; Gaziano, J.; Ridker, P. C-Reactive Protein and the Risk of Developing Hypertension. JAMA 2003, 290, 2945–2951. [Google Scholar] [CrossRef] [PubMed]
- Brett, S.; Ritter, J.; Chowienczyk, P. Diastolic Blood Pressure Changes during Exercise Positively Correlate with Serum Cholesterol and Insulin Resistance. Circulation 2000, 101, 611–615. [Google Scholar] [CrossRef] [PubMed]
- Su, x.; Kong, Y.; Peng, D. Evidence for Changing Lipid Management Strategy to Focus on Non-High Density Lipoprotein Cholesterol. Lipids Health Dis. 2019, 18, 134. [Google Scholar] [CrossRef]
- Lopez-Jimenez, F. Mayo Clinic: Cholesterol Ratio or Non-HDL Cholesterol: Which Is Most Important? 2022. Available online: https://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/expert-answers/cholesterol-ratio/faq-20058006 (accessed on 14 February 2022).
- Jarrett, C.; Tucker, W.; Angadi, S.; Gaesser, G. Postexercise Hypotension is Delayed in Men with Obesity and Hypertension. Front. Physiol. 2022, 13. [Google Scholar] [CrossRef]
- Neter, J.; Stam, B.; Kok, F.; Grobbee, D.; Geleijnse, J. Influence of Weight Reduction on Blood Pressure. Hypertension 2003, 42, 878–884. [Google Scholar] [CrossRef] [PubMed]
- Zeigler, Z.; Swan, P.; Buman, M.; Mookadam, F.; Gaesser, G.; Angadi, S. Postexercise Hemodynamic Responses in Lean and Obese Men. Med. Sci. Sports Exerc. 2018, 50, 2292–2300. [Google Scholar] [CrossRef]
- Olson, K.; Augeri, A.; Seipd, R.; Tsongalis, G.; Thompson, P.; Pescatello, L. Correlates of Endothelial Function and the Peak Systolic Blood Pressure Response to a Graded Maximal Exercise Test. Atherosclerosis 2012, 222. [Google Scholar] [CrossRef]
- Villa-Etchegoyen, C.; Lombarte, C.; Villa-Etchegoyen, M.; Belizán, J.; Cormick, G. Mechanisms Involved in the Relationship between Low Calcium Intake and High Blood Pressure. Nutrients 2019, 11, 1112. [Google Scholar] [CrossRef]
- Forman, J.; Giovannucci, E.; Holmes, M.; Bischoff-Ferrari, H.; Tworoger, S.; Willett, W.; Curhan, G. Plasma 25-Hydroxyvitamin D Levels and Risk of Incident Hypertension. Hypertension 2007, 49, 1063–1069. [Google Scholar] [CrossRef]
- Ni, W.; Watts, S.; Chen, S.; Glenn, D.; Gardner, D. Elimination of Vitamin D Receptor in Vascular Endothelial Cells Alters Vascular Function. Hypertension 2014, 64, 1290–1298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schulz, E.; Steven, S.; Münzel, T. Is at Least One Vitamin Helping our Vasculature? Evidence for an Important Role of the Endothelial Vitamin D Receptor in Regulating Endothelial Function and Blood Pressure. Hypertension 2014, 64, 1187–1188. [Google Scholar] [CrossRef]
- Shankar, A.; Wang, J.; Rochtchina, E.; Mitchell, P. Positive Association between Plasma Fibrinogen Level and Incident Hypertension among Men. Hypertension 2006, 48, 1043–1049. [Google Scholar] [CrossRef] [PubMed]
- Hanssen, H.; Boardman, H.; Deiseroth, A.; Moholdt, T.; Simonenko, M.; Kränkel, N.; Niebauer, J. Personalized Exercise Prescription in the Prevention and Treatment of Arterial Hypertension: A Consensus Document from the European Association of Preventive Cardiology (EAPC) and the ESC Council on Hypertension. Eur. J. Prev. Cardiol. 2021, 29, 205–215. [Google Scholar] [CrossRef]
- Wilder, J. Pitfalls in the Methodology of the Law of Initial Value. Am. J. Psychother. 1965, 19, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Kestenbaum, B.; Rudser, K.; de Boer, I.; Peralta, C.; Fried, L.; Shlipak, M.; Palmas, W.; Stehman-Breen, C.; Siscovick, D. Differences in Kidney Function and Incident Hypertension: The Multi-Ethnic Study of Atherosclerosis. Ann. Intern. Med. 2008, 148, 501–508. [Google Scholar] [CrossRef]
- Aronow, W. Association of Obesity with Hypertension. Ann. Transl. Med. 2017, 5, 350. [Google Scholar] [CrossRef] [PubMed]
- Lan, F.; Yiannakou, I.; Schiebler, C.; Hershey, M.; Cabrera, J.; Gaviola, G.; Fernandez-Montero, A.; Christophi, C. The Effects of Fire Academy Training and Probationary Firefighter Status on Select Basic Health and Fitness Measurements. Med. Sci. Sports Exerc. 2021, 53, 740–748. [Google Scholar] [CrossRef] [PubMed]
- Subar, A.; Freedman, L.; Tooze, J.; Kirkpatrick, S.; Boushey, C.; Neuhouser, M.; Thompson, F.; Potischman, N.; Guenther, P. Addressing Current Criticism regarding the Value of Self-Report Dietary Data. J. Nutr. 2015, 145, 2369–2645. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Total Sample (n = 15) | |
|---|---|
| Age (yr) | 40.2 ± 9.5 |
| BP medication use (Yes/No) | 2/13 |
| DASH accordance score | 2.8 ± 1.3 |
| BMI (kg/m2) | 29.0 ± 3.9 |
| Waist Circumference (cm) | 93.3 ± 11.1 |
| Resting SBP (mmHg) | 124.1 ± 10.3 |
| Resting DBP (mmHg) | 79.6 ± 11.5 |
| 19 h Ambulatory SBP (mmHg) | 134.8 ± 7.4 |
| 19 h Ambulatory DBP (mmHg) | 76.6 ± 4.7 |
| Total Cholesterol (mg/dL) | 186.7 ± 33.0 |
| LDL-C (mg/dL) | 114.5 ± 30.1 |
| HDL-C (mg/dL) | 48.4 ± 11.4 |
| Triglycerides (mg/dL) | 118.3 ± 86.8 |
| Non-HDL-C (mg/dL) | 138.3 ± 37.8 |
| Total Cholesterol/Triglycerides (U) | 2.1 ± 0.8 |
| Total Cholesterol/HDL-C (U) | 4.1 ± 1.5 |
| Glucose (mg/dL) | 98.7 ± 16.9 |
| Insulin (ulU/mL) | 6.5 ± 4.1 |
| Relative peak oxygen consumption (mL/kg·min−1) | 41.5 ± 6.8 |
| Daily Intake (n = 15) | Dietary Reference Intake | |
|---|---|---|
| Carbohydrate (g) | 171.9 ± 64.8 | 130 |
| Protein (g) | 80.0 ± 30.4 | 56 |
| Fat (g) | 68.3 ± 28.5 | 56 |
| Fiber (g) | 14.1 ± 6.0 | 38 |
| Cholesterol (mg) | 222.4 ± 84.5 | <200 |
| Vitamin D—Calciferol (mcg) | 4.1 ± 2.6 | 15 |
| Caffeine (mg) | 542.0 ± 348.9 | 400 |
| Calcium (mg) | 840.7 ± 369.8 | 1000 |
| Potassium (mg) | 3070.5 ± 971.5 | 4700 |
| Magnesium (mg) | 331.6 ± 116.4 | 420 |
| Sodium (mg) | 2642.9 ± 1004.9 | 1500 |
| Trans Fatty Acids (g) | 3.0 ± 1.1 | 2 |
| Total Number of Fruit Servings | 1.7 ± 1.1 | 4 |
| Total Number of Vegetable Servings | 2.8 ± 1.3 | 5 |
| Lean Meat Equivalent from Nuts/Seeds (Oz) | 0.5 ± 0.5 | 0.7 |
| Lean Meat from Fish/Other Seafood (Oz) | 0.5 ± 0.5 | 0.3–0.4 |
| Number of Whole Grain Servings | 0.7 ± 0.4 | 3 |
| Alcohol (g) | 12.9 ± 10.5 | ≤28 |
| Total Caloric Intake (kcal) | 1683.2 ± 621.4 | 2538 |
| Total Sample Intake (n = 15) | DASH Score Target (1 Point) | DASH Score Intermediate Target (0.5 Points) | DASH Score Not Meeting Target or Intermediate (0 Points) | |
|---|---|---|---|---|
| DASH accordance score | 2.8 ± 1.3 | |||
| DASH nutrients | ||||
| Sodium (mg/d) | 2642.9 ± 1001.9 | <2300.0 | 2300–2650 b | >2650 |
| Cholesterol (mg/d) | 222.4 ± 84.5 | <149.1 | 149.1–224.7 b | >224.7 |
| Saturated fat (% of kcal/d) | 11.6 ± 2.6 | <6.0 | 6–11 | >11 c |
| Total fat (% of kcal/d) | 36.5 ± 5.0 | <27.0 | 27–32 | >32 c |
| Protein (% of kcal/d) | 19.2 ± 2.6 | >18.0 a | 16.5–18.0 | <16.5 |
| Calcium (mg/d) | 840.7 ± 369.8 | >1240.0 | 842.3–1240.0 | <842.3 c |
| Magnesium (mg/d) | 331.6 ± 116.4 | >496.7 | 330.3–496.7 b | <330.3 |
| Potassium (mg/d) | 3070.5 ± 971.5 | >4673.3 | 3198.3–4673.3 | <3198.3 c |
| Fiber (g/d) | 14.1 ± 6.0 | >30.0 | 19.5–30.0 | <19.5 c |
| Predictors | Β | T | Partial PVE | VIF | Power |
|---|---|---|---|---|---|
| Caffeine | |||||
| ASBP | 0.696 † * | 1.000 ¶ | |||
| C-reactive Protein | −8.75 | −8.78 | 0.444 * | 4.91486 | 1.000 |
| Non-HDL-C | −0.22 | −7.44 | 0.346 * | 1.95318 | 1.000 |
| Caffeine | 0.02 | 5.66 | 0.236 c | 2.63521 | 0.991 |
| Body Mass Index | 1.97 | 5.80 | 0.228 c | 3.06201 | 0.994 |
| Glucose | 0.18 | 2.80 | 0.062 a | 2.09854 | 0.771 |
| Heart Rate | −0.17 | −1.96 | 0.033 # | 1.58699 | 0.610 |
| ADBP | 0.742 † * | 1.000 ¶ | |||
| Non-HDL-C | −0.29 | −67.58 | 0.446 * | 1.29845 | 1.000 |
| Glucose | −0.11 | −17.17 | 0.375 * | 1.20414 | 1.000 |
| Body Mass Index | 0.51 | 14.58 | 0.315 * | 1.20949 | 1.000 |
| Caffeine | −0.01 | −13.52 | 0.111 * | 1.11281 | 1.000 |
| Calcium | |||||
| ASBP | 0.464 † c | 1.000 ¶ | |||
| Vitamin D | 4.24 | 5.54 | 0.285 c | 1.59214 | 0.998 |
| Calcium | −0.02 | −5.04 | 0.237 c | 1.62399 | 0.992 |
| Heart Rate | −0.43 | −3.76 | 0.192 b | 1.09861 | 0.954 |
| Fibrinogen | 0.09 | 2.93 | 0.143 a | 1.08374 | 0.888 |
| ADBP | 0.821 † * | 1.000 ¶ | |||
| Resting DBP | −0.72 | −48.00 | 0.582 * | 1.35211 | 1.000 |
| Fibrinogen | 0.08 | 14.81 | 0.309 * | 1.16022 | 1.000 |
| Calcium | −0.01 | −12.28 | 0.228 * | 1.83184 | 1.000 |
| TC/TG | −2.34 | −5.34 | 0.093 c | 1.23754 | 0.984 |
| Vitamin D | 0.79 | 4.68 | 0.070 b | 1.76900 | 1.000 |
| Sodium | |||||
| ASBP | 0.508 † c | 1.000 ¶ | |||
| C-reactive Protein | −4.91 | −4.97 | 0.302 c | 1.84193 | 0.966 |
| Non-HDL-C | −0.16 | −4.27 | 0.234 b | 1.51272 | 0.925 |
| Body Mass Index | 1.02 | 2.33 | 0.068 a | 2.55082 | 0.619 |
| Sodium | −0.00 | −1.83 | 0.050 # | 1.11441 | 0.507 |
| ADBP | 0.688 † * | 1.000 ¶ | |||
| Cystatin C | 46.81 | 23.18 | 0.270 * | 2.90843 | 1.000 |
| Body Mass Index | 1.37 | 17.62 | 0.263 * | 1.64401 | 1.000 |
| Sodium | 0.01 | 19.86 | 0.229 * | 2.77005 | 1.000 |
| Resting DBP | −0.20 | −8.83 | 0.118 * | 2.16846 | 1.000 |
| TC/HDL-C | −7.01 | −11.24 | 0.095 * | 1.77217 | 1.000 |
| Predictors | Β | T | Partial PVE | VIF |
|---|---|---|---|---|
| SBP | 0.860 † b | |||
| Non-HDL-C | 0.68 | 5.00 | 0.351 a | 1.332 |
| C-reactive Protein | 0.56 | 3.85 | 0.209 a | 1.490 |
| Body Mass Index | −0.33 | −2.17 | 0.066 # | 1.635 |
| DASH Score | −0.18 | −1.23 | 0.022 # | 1.470 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berkowsky, R.S.; Zaleski, A.L.; Taylor, B.A.; Chen, M.-H.; Gans, K.M.; Wu, Y.; Parducci, P.M.; Zhang, Y.; Fernandez, A.B.; Pescatello, L.S. Cardiometabolic Biomarkers and Habitual Caffeine Consumption Associate with the Adverse Ambulatory Blood Pressure Response to Strenuous Physical Exertion among Firefighters. Nutrients 2022, 14, 4025. https://doi.org/10.3390/nu14194025
Berkowsky RS, Zaleski AL, Taylor BA, Chen M-H, Gans KM, Wu Y, Parducci PM, Zhang Y, Fernandez AB, Pescatello LS. Cardiometabolic Biomarkers and Habitual Caffeine Consumption Associate with the Adverse Ambulatory Blood Pressure Response to Strenuous Physical Exertion among Firefighters. Nutrients. 2022; 14(19):4025. https://doi.org/10.3390/nu14194025
Chicago/Turabian StyleBerkowsky, Rachel S., Amanda L. Zaleski, Beth A. Taylor, Ming-Hui Chen, Kim M. Gans, Yin Wu, Paul M. Parducci, Yiming Zhang, Antonio B. Fernandez, and Linda S. Pescatello. 2022. "Cardiometabolic Biomarkers and Habitual Caffeine Consumption Associate with the Adverse Ambulatory Blood Pressure Response to Strenuous Physical Exertion among Firefighters" Nutrients 14, no. 19: 4025. https://doi.org/10.3390/nu14194025
APA StyleBerkowsky, R. S., Zaleski, A. L., Taylor, B. A., Chen, M.-H., Gans, K. M., Wu, Y., Parducci, P. M., Zhang, Y., Fernandez, A. B., & Pescatello, L. S. (2022). Cardiometabolic Biomarkers and Habitual Caffeine Consumption Associate with the Adverse Ambulatory Blood Pressure Response to Strenuous Physical Exertion among Firefighters. Nutrients, 14(19), 4025. https://doi.org/10.3390/nu14194025







