Barriers and Facilitators Associated with the Adoption of and Adherence to a Mediterranean Style Diet in Adults: A Systematic Review of Published Observational and Qualitative Studies
Abstract
:1. Introduction
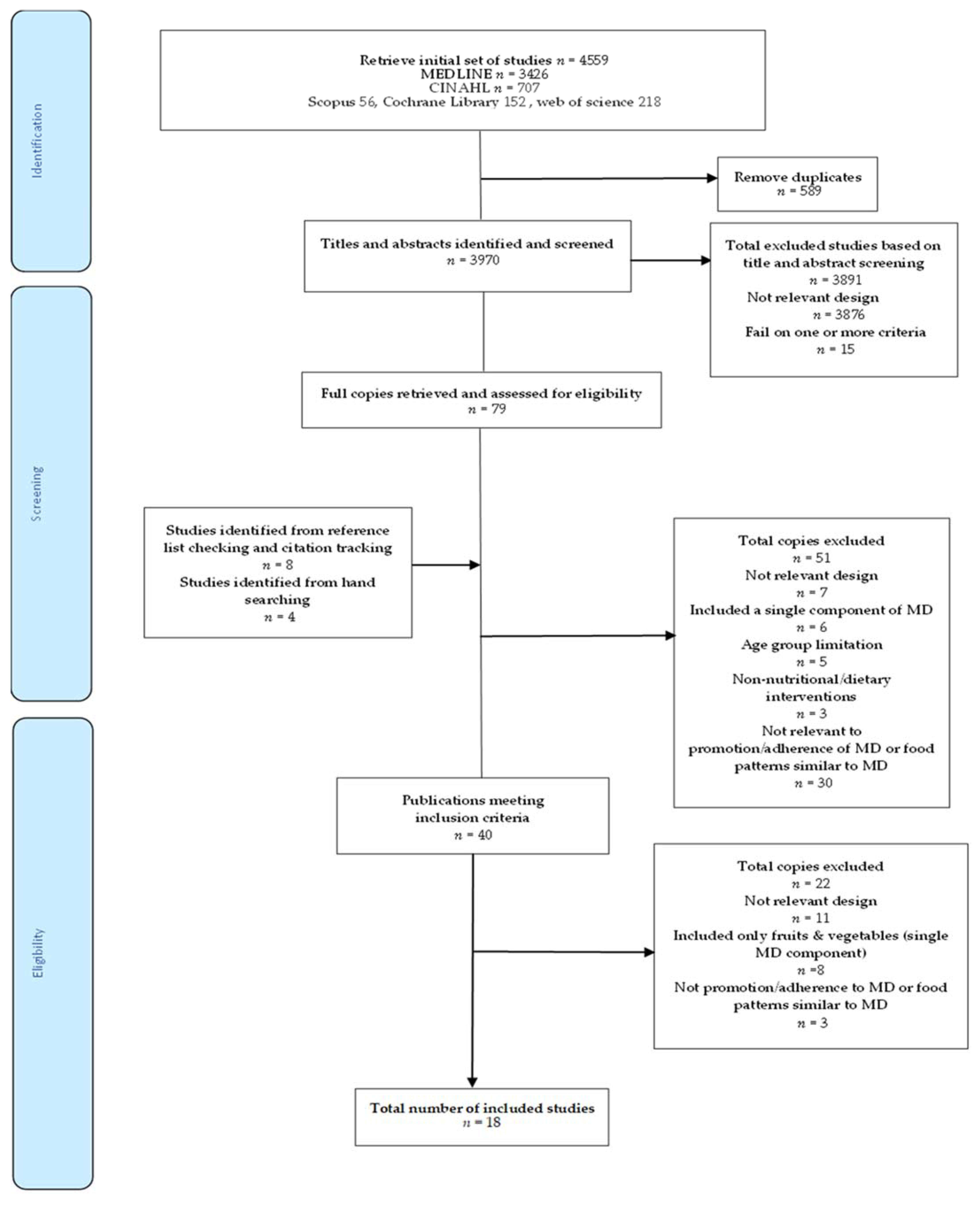
2. Materials and Methods
2.1. Systematic Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction
2.4. Risk of Bias
3. Results
3.1. Characteristics of Included Studies
3.2. Findings of Included Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Romaguera, D.; Norat, T.; Mouw, T.; May, A.M.; Bamia, C.; Slimani, N.; Travier, N.; Besson, H.; Luan, J.; Wareham, N.; et al. Adherence to the Mediterranean Diet Is Associated with Lower Abdominal Adiposity in European Men and Women. J. Nutr. 2009, 139, 1728–1737. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martínez-González, M.Á.; Hershey, M.S.; Zazpe, I.; Trichopoulou, A. Transferability of the Mediterranean Diet to Non-Mediterranean Countries. What Is and What Is Not the Mediterranean Diet. Nutrients 2017, 9, 1226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tortosa, A.; Bes-Rastrollo, M.; Sanchez-Villegas, A.; Basterra-Gortari, F.J.; Nuñez-Cordoba, J.M.; Martinez-Gonzalez, M.A. Mediterranean Diet Inversely Associated with the Incidence of Metabolic Syndrome: The Sun Prospective Cohort. Diabetes Care 2007, 30, 2957–2959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spadafranca, A.; Piuri, G.; Bulfoni, C.; Liguori, I.; Battezzati, A.; Bertoli, S.; Speciani, A.F.; Ferrazzi, E. Adherence to the Mediterranean Diet and Serum Adiponectin Levels in Pregnancy: Results from a Cohort Study in Normal Weight Caucasian Women. Nutrients 2018, 10, 928. [Google Scholar] [CrossRef] [Green Version]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N. Engl. J. Med. 2018, 378, 34. [Google Scholar] [CrossRef] [PubMed]
- Chatzi, L.; Rifas-Shiman, S.L.; Georgiou, V.; Joung, K.E.; Koinaki, S.; Chalkiadaki, G.; Margioris, A.; Sarri, K.; Vassilaki, M.; Vafeiadi, M.; et al. Adherence to the Mediterranean Diet during Pregnancy and Offspring Adiposity and Cardiometabolic Traits in Childhood. Pediatric Obes. 2017, 12, 47–56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Minhas, A.S.; Hong, X.; Wang, G.; Rhee, D.K.; Liu, T.; Zhang, M.; Michos, E.D.; Wang, X.; Mueller, N.T. Mediterranean-Style Diet and Risk of Preeclampsia by Race in the Boston Birth Cohort. J. Am. Heart Assoc. 2022, 11, e022589. [Google Scholar] [CrossRef]
- Timmermans, S.; Steegers-Theunissen, R.P.M.; Vujkovic, M.; Bakker, R.; den Breeijen, H.; Raat, H.; Russcher, H.; Lindemans, J.; Hofman, A.; Jaddoe, V.W.V.; et al. Major Dietary Patterns and Blood Pressure Patterns during Pregnancy: The Generation R Study. Am. J. Obstet. Gynecol. 2011, 205, 1–337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsofliou, F.; Theodoridis, X.; Arvanitidou, I. Chapter 14: Toward a Mediterranean-style diet outside the Mediterranean countries. In The Mediterranean Diet: An Evidence-Based Approach, 2nd ed.; Preedy, V., Watson, R., Eds.; Academic Press Elsevier: Cambridge, MA, USA, 2020. [Google Scholar]
- University of York. Centre for Reviews and Dissemination. Systematic Reviews: Crd’s Guidance for Undertaking Reviews in Health Care, 3rd ed.; Centre for Reviews and Dissemination: York, UK, 2009. [Google Scholar]
- Kellermeyer, L.; Harnke, B.; Knight, S. Covidence and Rayyan. J. Med. Libr. Assoc. 2018, 106, 580–583. [Google Scholar] [CrossRef] [Green Version]
- Hörnell, A.; Berg, C.; Forsum, E.; Larsson, C.; Sonestedt, E.; Akesson, A.; Lachat, C.; Hawwash, D.; Kolsteren, P.; Byrnes, G.; et al. Perspective: An Extension of the Strobe Statement for Observational Studies in Nutritional Epidemiology (strobe-Nut): Explanation and Elaboration. Adv. Nutr. 2017, 8, 652–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Critical Appraisal Skills Programme. Available online: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf (accessed on 1 January 2019).
- Cavaliere, A.; Donzelli, F.; Banterle, A.; De Marchi, E. Is the Mediterranean Diet for All? An Analysis of Socioeconomic Inequalities and Food Consumption in Italy. Br. Food J. 2019, 121, 1327–1341. [Google Scholar] [CrossRef]
- Moreno-Gómez, C.; Romaguera-Bosch, D.; Tauler-Riera, P.; Bennasar-Veny, M.; Pericas-Beltran, J.; Martinez-Andreu, S.; Aguilo-Pons, A. Clustering of Lifestyle Factors in Spanish University Students: The Relationship between Smoking, Alcohol Consumption, Physical Activity and Diet Quality. Public Health Nutr. 2012, 15, 2131–2139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olmedo-Requena, R.; Fernández, J.G.; Prieto, C.A.; Moreno, J.M.; Bueno-Cavanillas, A.; Jiménez-Moleón, J.J. Factors Associated with a Low Adherence to a Mediterranean Diet Pattern in Healthy Spanish Women Before Pregnancy. Public Health Nutr. 2014, 17, 648–656. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Theodoridis, X.; Grammatikopoulou, M.G.; Gkiouras, K.; Papadopoulou, S.E.; Agorastou, T.; Gkika, I.; Maraki, M.I.; Dardavessis, T.; Chourdakis, M. Food Insecurity and Mediterranean Diet Adherence among Greek University Students. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 477–485. [Google Scholar] [CrossRef] [PubMed]
- Couto, R.M.; Frugé, A.D.; Greene, M.W. Adherence to the Mediterranean Diet in a Portuguese Immigrant Community in the Central Valley of California. Nutrients 2021, 13, 1989. [Google Scholar] [CrossRef]
- Dijkstra, S.C.; Neter, J.E.; van Stralen, M.M.; Knol, D.L.; Brouwer, I.A.; Huisman, M.; Visser, M. The Role of Perceived Barriers in Explaining Socio-Economic Status Differences in Adherence to the Fruit, Vegetable and Fish Guidelines in Older Adults: A Mediation Study. Public Health Nutr. 2015, 18, 797–808. [Google Scholar] [CrossRef] [Green Version]
- Greiner, B.H.; Croff, J.; Wheeler, D.; Miller, B. Mediterranean Diet Adherence in Cardiac Patients: A Cross-Sectional Study. Am. J. Health Behav. 2018, 42, 3–10. [Google Scholar] [CrossRef]
- Knight, C.J.; Jackson, O.; Rahman, I.; Burnett, D.O.; Frugé, A.D.; Greene, M.W. The Mediterranean Diet in the Stroke Belt: A Cross-Sectional Study on Adherence and Perceived Knowledge, Barriers, and Benefits. Nutrients 2019, 11, 1847. [Google Scholar] [CrossRef] [Green Version]
- Lara, J.; McCrum, L.-A.; Mathers, J.C. Association of Mediterranean Diet and Other Health Behaviours with Barriers to Healthy Eating and Perceived Health among British Adults of Retirement Age. Maturitas 2014, 79, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Papadaki, A.; Wood, L.; Sebire, S.J.; Jago, R. Adherence to the Mediterranean Diet among Employees in South West England: Formative Research to Inform a Web-Based, Work-Place Nutrition Intervention. Prev. Med. Rep. 2015, 2, 223–228. [Google Scholar] [CrossRef]
- Scannell, N.; Villani, A.; Swanepoel, L.; Mantzioris, E. Understanding the Self-Perceived Barriers and Enablers Toward Adopting a Mediterranean Diet in Australia: An Application of the Theory of Planned Behaviour Framework. Int. J. Environ. Res. Public Health 2020, 17, 9321. [Google Scholar] [CrossRef] [PubMed]
- Tong, T.Y.N.; Imamura, F.; Monsivais, P.; Brage, S.; Griffin, S.J.; Wareham, N.J.; Forouhi, N.G. Dietary Cost Associated with Adherence to the Mediterranean Diet, and Its Variation by Socio-Economic Factors in the Uk Fenland Study. Br. J. Nutr. 2018, 119, 685–694. [Google Scholar] [CrossRef] [Green Version]
- Haigh, L.; Bremner, S.; Houghton, D.; Henderson, E.; Avery, L.; Hardy, T.; Hallsworth, K.; McPherson, S.; Anstee, Q.M. Barriers and Facilitators to Mediterranean Diet Adoption by Patients with Nonalcoholic Fatty Liver Disease in Northern Europe. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2019, 17, 1364–1371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hardin-Fanning, F. Adherence to a Mediterranean Diet in a Rural Appalachian Food Desert. Rural Remote Health 2013, 13, 2293. [Google Scholar] [CrossRef]
- Kretowicz, H.; Hundley, V.; Tsofliou, F. Exploring the Perceived Barriers to Following a Mediterranean Style Diet in Childbearing Age: A Qualitative Study. Nutrients 2018, 10, 1694. [Google Scholar] [CrossRef] [Green Version]
- Middleton, G.; Keegan, R.; Smith, M.F.; Alkhatib, A.; Klonizakis, M. Implementing a Mediterranean Diet Intervention into a Rct: Lessons Learned from a Non-Mediterranean Based Country. J. Nutr. Health Aging 2015, 19, 1019–1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moore, S.E.; McEvoy, C.T.; Prior, L.; Lawton, J.; Patterson, C.C.; Kee, F.; Cupples, M.; Young, I.S.; Appleton, K.; McKinley, M.C.; et al. Barriers to Adopting a Mediterranean Diet in Northern European Adults at High Risk of Developing Cardiovascular Disease. J. Hum. Nutr. Diet. 2017, 31, 451–462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zacharia, K.; Patterson, A.J.; English, C.; MacDonald-Wicks, L. Feasibility of the Ausmed Diet Program: Translating the Mediterranean Diet for Older Australians. Nutrients 2020, 12, 1044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kihlstrom, L.; Long, A.; Himmelgreen, D. Barriers and Facilitators to the Consumption of Fresh Produce among Food Pantry Clients. J. Hunger Environ. Nutr. 2019, 14, 168–182. [Google Scholar] [CrossRef]
- Ashton, L.M.; Hutchesson, M.J.; Rollo, M.E.; Morgan, P.J.; Collins, C.E. Motivators and Barriers to Engaging in Healthy Eating and Physical Activity: A Cross-Sectional Survey in Young Adult Men. Am. J. Men’s Health 2017, 11, 330–343. [Google Scholar] [CrossRef] [Green Version]
- Ares, G.; Machín, L.; Girona, A.; Curutchet, M.R.; Giménez, A. Comparison of Motives Underlying Food Choice and Barriers to Healthy Eating among Low Medium Income Consumers in Uruguay. Cad. De Saúde Pública 2017, 33, e00213315. [Google Scholar] [CrossRef] [PubMed]
- Lopez, C.N.; Martinez-Gonzalez, M.A.; Sanchez-Villegas, A.; Alonso, A.; Pimenta, A.M.; Bes-Rastrollo, M. Costs of Mediterranean and Western Dietary Patterns in a Spanish Cohort and Their Relationship with Prospective Weight Change. J. Epidemiol. Community Health 2009, 63, 920–927. [Google Scholar] [CrossRef] [PubMed]
- Andajani-Sutjahjo, S.; Ball, K.; Warren, N.; Inglis, V.; Crawford, D. Perceived Personal, Social and Environmental Barriers to Weight Maintenance among Young Women: A Community Survey. Int. J. Behav. Nutr. Phys. Act. 2004, 1, 15. [Google Scholar] [CrossRef] [Green Version]
- Munt, A.E.; Partridge, S.R.; Allman-Farinelli, M. The Barriers and Enablers of Healthy Eating among Young Adults: A Missing Piece of the Obesity Puzzle: A Scoping Review. Obes. Rev. 2017, 18, 1–17. [Google Scholar] [CrossRef]
- Rydén, P.; Sydner, Y.M.; Hagfors, L. Counting the Cost of Healthy Eating: A Swedish Comparison of Mediterranean-Style and Ordinary Diets. Int. J. Consum. Stud. 2008, 32, 138–146. [Google Scholar] [CrossRef]
- Aggarwal, A.; Monsivais, P.; Drewnowski, A.; Cook, A.J. Does Diet Cost Mediate the Relation between Socioeconomic Position and Diet Quality? Eur. J. Clin. Nutr. 2011, 65, 1059–1066. [Google Scholar] [CrossRef] [Green Version]
- French, S.A.; Tangney, C.C.; Crane, M.M.; Wang, Y.; Appelhans, B.M. Nutrition Quality of Food Purchases Varies by Household Income: The Shopper Study. BMC Public Health 2019, 19, 231. [Google Scholar] [CrossRef] [Green Version]
- Goulet, J.; Lamarche, B.; Lemieux, S. A Nutritional Intervention Promoting a Mediterranean Food Pattern Does Not Affect Total Daily Dietary Cost in North American Women in Free-Living Conditions. J. Nutr. 2008, 138, 54–59. [Google Scholar] [CrossRef] [Green Version]
- Appleton, K.M.; McGill, R.; Woodside, J.V. Fruit and vegetable consumption in older individuals in Northern Ireland: Levels and patterns. Br. J. Nutr. 2009, 102, 949–953. [Google Scholar] [CrossRef] [Green Version]
- Appleton, K.M.; Dinnella, C.; Spinelli, S.; Morizet, D.; Saulais, L.; Hemingway, A.; Monteleone, E.; Depezay, L.; Perez-Cueto, F.J.A.; Hartwell, H. Consumption of a High Quantity and a Wide Variety of Vegetables Are Predicted by Different Food Choice Motives in Older Adults from France, Italy and the Uk. Nutrients 2017, 9, 923. [Google Scholar] [CrossRef]
- Arabshahi, S.; Lahmann, P.H.; Williams, G.M.; Marks, G.C.; van der Pols, J.C. Longitudinal Change in Diet Quality in Australian Adults Varies by Demographic, Socio-Economic, and Lifestyle Characteristics. J. Nutr. 2011, 141, 1871–1879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McMorrow, L.; Ludbrook, A.; Olajide, D.; Macdiarmid, J.I. Perceived Barriers Towards Healthy Eating and Their Association with Fruit and Vegetable Consumption. J. Public Health 2017, 39, 330–338. [Google Scholar] [CrossRef] [Green Version]
- Whitley, E.; Hunt, K.; Popham, F.; Benzeval, M.; Batty, G.D. The Role of Health Behaviours Across the Life Course in the Socioeconomic Patterning of All-Cause Mortality: The West of Scotland Twenty-07 Prospective Cohort Study. Ann. Behav. Med. 2014, 47, 148–157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schoufour, J.D.; de Jonge, E.A.L.; Kiefte-de Jong, J.C.; van Lenthe, F.J.; Hofman, A.; Nunn, S.P.T.; Franco, O.H. Socio-Economic Indicators and Diet Quality in an Older Population. Maturitas 2018, 107, 71–77. [Google Scholar] [CrossRef]
- Appleton, K.M.; McGill, R.; Neville, C.; Woodside, J.V. Barriers to Increasing Fruit and Vegetable Intakes in the Older Population of Northern Ireland: Low Levels of Liking and Low Awareness of Current Recommendations. Public Health Nutr. 2010, 13, 514–521. [Google Scholar] [CrossRef] [Green Version]
- Nagler, R.H. Adverse Outcomes Associated with Media Exposure to Contradictory Nutrition Messages. J. Health Commun. 2014, 19, 24–40. [Google Scholar] [CrossRef]
- Didinger, C.; Thompson, H. Motivating Pulse-Centric Eating Patterns to Benefit Human and Environmental Well-Being. Nutrients 2020, 12, 3500. [Google Scholar] [CrossRef]
- McEvoy, C.T.; Moore, S.E.; Erwin, C.M.; Kontogianni, M.; Wallace, S.M.; Appleton, K.M.; Cupples, M.E.; Hunter, S.J.; Kee, F.; McCance, D.; et al. Trial to Encourage Adoption and Maintenance of a Mediterranean Diet (team-Med): A Randomised Pilot Trial of a Peer Support Intervention for Dietary Behaviour Change in Adults from a Northern European Population at High Cardiovascular Disease Risk. Br. J. Nutr. 2021, 15, 1130. [Google Scholar] [CrossRef]
- McEvoy, C.T.; Moore, S.E.; Appleton, K.M.; Cupples, M.E.; Erwin, C.; Kee, F.; Prior, L.; Young, I.S.; McKinley, M.C.; Woodside, J.V. Development of a Peer Support Intervention to Encourage Dietary Behaviour Change Towards a Mediterranean Diet in Adults at High Cardiovascular Risk. BMC Public Health 2018, 18, 1194. [Google Scholar] [CrossRef]
- McEvoy, C.T.; Moore, S.E.; Appleton, K.M.; Cupples, M.E.; Erwin, C.M.; Hunter, S.J.; Kee, F.; McCance, D.; Patterson, C.C.; Young, I.S.; et al. Trial to Encourage Adoption and Maintenance of a Mediterranean Diet (team-Med): Protocol for a Randomised Feasibility Trial of a Peer Support Intervention for Dietary Behaviour Change in Adults at High Cardiovascular Disease Risk. Int. J. Environ. Res. Public Health 2018, 15, 1130. [Google Scholar] [CrossRef]
| Authors | Location | Aims | Participants | Data Collection Method | Risk of Bias |
|---|---|---|---|---|---|
| Mediterranean Countries | |||||
| Cavaliere et al., 2019 [14] | Italy | To analyse whether socioeconomic status (SES) is ultimately related to the overall level of adherence to the Mediterranean Diet (MD) of the Italian population | n = 36,032 Males and females aged ≥18 years | Italian household food survey questionnaire and adherence to MD pyramid recommendations by a study-based index | 21/22 |
| Moreno-Gomez et al., 2012 [15] | Spain | To ascertain the prevalence of and association between main lifestyle factors such as diet, physical activity, alcohol consumption, smoking in students | n = 987 Males and females Age (mean (SD) 21.4 (3.3) | Modified Mediterranean diet score adapted to diet patterns and needs of study’s population group | 21/22 |
| Olmedo-Rquena et al., 2014 [16] | Spain | To investigate the factors associated with the level of adherence to a Mediterranean dietary pattern in childbearing women before pregnancy | n = 1175 Females aged ≥18 years | Structured survey with FFQ and Mediterranean diet adherence index specific to Spanish MD guidelines | 22/22 |
| Thodoridis et al., 2018 [17] | Greece | To associate MedDiet adherence and food insecurity among university students in Greece | n = 236 Males and females aged 19–30 years | Household Food Insecurity Access Scale for MD barriers and MD adherence assessed with MEDAS questionnaire | 21/22 |
| Non-Mediterranean Countries | |||||
| Couto et al., 2021 [18] | USA | To examined MedDiet adherence and perceived knowledge, benefits, and barriers to the MedDiet in a Portuguese immigrant community | n = 208 Males and females 45 ≥ 75 years | Self-reported survey questionnaire on barriers and MEDAS score | 22/22 |
| Dijkstra et al., 2015 [19] | NL | To identify barriers for meeting the fruit, vegetable and fish guidelines in older Dutch adults and to investigate socio-economic status (SES) differences in these barriers | n = 1057 Males and females 55–85 years mean age of 68.9 (SD 6.2) years | Self reported food frequency questionnaire for MD adherence and lifestyle questionnaire | 21/22 |
| Greiner et al., 2018 [20] | USA | To examine adherence to the Mediterranean diet in patients diagnosed with cardiovascular disease based on social cognitive theory constructs | n = 337 Cardiac patients | Validated Food beliefs questionnaire and study-based 7-item MedDiet score | 22/22 |
| Knight et al., 2019 [21] | USA | To examine MedDiet adherence and perceived knowledge, benefits, and barriers to the MedDiet in the U.S. | n = 1447 Males and females, aged >18 years | Online questionnaire survey and MedDiet adherence evaluated by validated 14-point Mediterranean Diet Adherence Screener (MEDAS) | 22/22 |
| Lara et al., 2014 [22] | UK, England | To evaluate the association between perceived barriers to healthy eating and adherence to MD | n = 206 Males and females aged ≥50 years | Online Questionnaire-survey of 14-point Mediterranean Diet Adherence Screener (MEDAS) | 21/22 |
| Papadaki et al., 2015 [23] | UK, England | To assess internet usage patterns and adherence to the MedDiet among employees in South-West England, UK and their differences by personal characteristics | n = 590 Males and females mean age 43.8 years | Self-reported food frequency questionnaire of 11 main components of the Mediterranean diet | 22/22 |
| Scannell et al., 2020 [24] | Australia | To investigate the perceived beliefs, barriers, and enablers toward adherence to a MedDiet in Australian adults | n = 606 Females and males aged ≥18 years | Self-reported online questionnaire on barriers and adherence to a MedDiet via validated 14-item Mediterranean Diet Adherence Screener (MEDAS) | 22/22 |
| Tong et al., 2018 [25] | UK, England | To examine the dietary cost associated with adhering to the MedDiet in the United Kingdom and to assess the extent to which this association is influenced by socio-economic factors | n = 12417 Males and females 30–65 years | Self-reported food frequency questionnaire and study based Mediterranean diet score (MDS) | 22/22 |
| Authors | Location | Aims | Participants | Data Collection Method | Risk of Bias |
|---|---|---|---|---|---|
| Non-Mediterranean Countries | |||||
| Haigh et al., 2019 [26] | UK, England | To identify factors that affect Mediterranean diet adoption (and adherence/maintenance) in a northern European NAFLD population. | n = 19 Females, Age (mean(SD) 58.5 (10.6) | Semi structured interviews and MedDiet adherence via validated 14-point Mediterranean Diet Adherence Screener (MEDAS) | 10/10 |
| Hardin -Faning, 2013 [27] | USA | To identify factors that affect adoption and future adherence to a MedDiet in a rural Appalachian food desert | n = 43 Males and females aged ≥21 years | Self-reported open-ended questions | 9/10 |
| Kretowicz et al., 2018 [28] | UK, England | To investigate the perceived barriers to following a MedDiet in women of childbearing age | n = 20 Females aged 18–49 years | Focus groups and MEDAS | 9/10 |
| Middleton et al., 2015 [29] | UK, England | To examine the participants’ experiences regarding perceived barriers and facilitators which impact on consuming the MedDiet | n = 11 Males and females aged 50–65 years | Semi-structured focus groups | 9/10 |
| Moore et al., 2017 [30] | UK, Northern Ireland | To investigate attitudes towards adoption of a MedDiet in individuals at high CVD risk in a Northern European population | n = 67 Males and females, Age (mean (SD) 64.0 (10.0) | Semi-structured focus groups and adapted eight-item Food Frequency Questionnaire (FFQ) based on MEDAS | 10/10 |
| Zacharia et al., 2020 [31] | Australia | Τo assess perceived barriers and enablers in order to support older Australians to adhere to an AusMed diet pattern | n = 6 Males and females aged over 55 years | Individual Semi-Structured Interviews | 8/10 |
| Themes | Barriers | Facilitators |
|---|---|---|
| Availability/Accessibility | Difficult to purchase food items (e.g., little support to find and locate items in supermarket) [29,30] Seasonal availability of foods [24,28] Limited access, selection and choices [19,24,27] | Increased access to fresh foods [24] Availability of diet in catering outlets [24] Good access to budget supermarkets and good transport [26] |
| Cognitive | Absence of nutrition education (e.g., limited knowledge of the health benefits of MedDiet foods) [18,19,21,27,28,30] Lack of knowledge of how to incorporate the food components of the MedDiet into meals [24,27] Complex & contradictory dietary information (e.g., conflicting reports from media) [28,30] Complexity and size of meal plans [31] Concerns over specific foods (e.g., fats & oils) [28] Concerns over food safety (e.g., pesticide residues) [19] Low food literacy [24] Low health appeal and perceived healthfulness [18,21,24] Negative perceived outcomes, e.g., increased body weight [20,30] Lack of understanding of the importance of nutrition [26] Nutritional attitudes and beliefs [26,28] | Good nutrition knowledge and skills [26] Improved diet quality [24,29] Physical benefits, e.g., disease prevention [24,26,28,29] Appearance/body weight related benefits, inc. weight loss [18,21,26,28] Psychological benefits, e.g., improved well-being, mood [18,28] Natural content [18] Environmental benefits [24] Recipes to enable food incorporation [24] Understanding of links between diet and disease [26] Nutritional attitudes and beliefs [26] Trusted advice [26] Positive perceived outcomes [20] |
| Demographic | Lower education level [14,16,19,21] Lower SES [16] Gender: Being male [14] Gender: Males were less likely to understand the health implications of the MedDiet and less amenable to making chages [27] Age: Younger [14,16] Age: Younger people were concerned about the cost [27] | Higher education attainment [16,18,23,25] Lower education attainment [18] Gender: Being female [14,15,22] Age: Being older [16] |
| Financial | Increased food costs [19,24,27,28,29,30,31] Greater food expenses on high consumption items, e.g., legumes, Lower food expenses on low consumption items, e.g., meat [25] Wasteful/Foods easily spoil (e.g., fruits and vegetables) [19,24] Poor storage facilities [19] Lower incomes [14,19,27] High food insecurity [17] | Higher household income [25] Occupation (Professional/managerial) [25] Relative expense of plant-vs animal based foods [28] Good value for money [18,21,24,26] |
| Lifestyle | Sedentary lifestyle [16] Habit of smoking [16,17] Greater number of previous pregnancies [16] Medical concerns/poor health [19,26] Higher BMI [21] | Active lifestyle [16] Lower BMI [22] Higher number of meals consumed daily [15] |
| Motivational | Lack of willpower/motivation to cook healthy foods [24,26] Resistance to dietary change [27,30] The term “diet” elicited ideas of restriction [28] Low abilities to adhere, due to the restrictive nature [24] Low willingness for self-care [26] Perceived helplessness [26] Impacts of poor adherence [26] High responsiveness to external food cues [25] | High self-efficacy/self-determination [20,26] Good self-regulation to consume healthy foods and avoid unhealthy foods [20,26] Higher stage of dietary change [18,21] Desire to increase healthy choices [24] High motivation [26] Balanced relationship with food [26] |
| Sensory and Hedonic | Low sensory appeal [18,21] Not liking the taste/smell [19,24,26] Trouble with chewing fruits (especially in older adults) [19] Components of the diet were unappealing (e.g., lentils) [28,31] Finding it hard to give-up liked foods [28] Poor appetite [19] | Enjoyable and pleasurable eating experience (i.e., sense of pleasure and fulfilment to meal times) [26,29] High taste/sensory appeal [18,21,24,26,31] Satisfaction (fillingness) with the foods [31] Varied [26,28] Familiarity with foods [18,21] |
| Socio-cultural | Negative influence of family members/dining partners [19,26,27,28] Upbringing and family [28] Usual habits [19,26,28] Acceptability of a MedDiet: Difficulties in adapting a new eating pattern and changing personal established eating habits [24,29,30] Stress, stressors, work and time pressures (e.g., irregular working hours) [26,29] Working night shifts [17] Impractical [18,19,21,28] Culture and cultural differences (e.g., British culture has a tradition of eating a lot of red meat) [24,26,29,30] Perceived difficulty of living in a colder climate (e.g., some food patterns of MedDiet are being eaten cold and people prefer warmer foods) [28,29,30] Not convenient to prepare and cook fresh food [26,27,28] Lack of cooking skills/equipment [24,26,27,28,30] Time to plan, purchase and prepare foods [24,27,28,29,30] References to mothers as responsible for their offspring [28] Climate—cold weather [24] Obesogenic environment [26] | Being married or cohabiting [14,23] Family/friend support [24,26] Shared responsibility of food preparation [23] Upbringing and family [28] Broadens the food repertoire [29] Redefines cultural eating habits, e.g., eating together [24,29] Increased time availability [24] Increased cooking skills/equipment [24] Climate—warm weather [24] Coverage in the media [26] Higher number of meals/day [15] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsofliou, F.; Vlachos, D.; Hughes, C.; Appleton, K.M. Barriers and Facilitators Associated with the Adoption of and Adherence to a Mediterranean Style Diet in Adults: A Systematic Review of Published Observational and Qualitative Studies. Nutrients 2022, 14, 4314. https://doi.org/10.3390/nu14204314
Tsofliou F, Vlachos D, Hughes C, Appleton KM. Barriers and Facilitators Associated with the Adoption of and Adherence to a Mediterranean Style Diet in Adults: A Systematic Review of Published Observational and Qualitative Studies. Nutrients. 2022; 14(20):4314. https://doi.org/10.3390/nu14204314
Chicago/Turabian StyleTsofliou, Fotini, Dimitrios Vlachos, Christina Hughes, and Katherine M. Appleton. 2022. "Barriers and Facilitators Associated with the Adoption of and Adherence to a Mediterranean Style Diet in Adults: A Systematic Review of Published Observational and Qualitative Studies" Nutrients 14, no. 20: 4314. https://doi.org/10.3390/nu14204314
APA StyleTsofliou, F., Vlachos, D., Hughes, C., & Appleton, K. M. (2022). Barriers and Facilitators Associated with the Adoption of and Adherence to a Mediterranean Style Diet in Adults: A Systematic Review of Published Observational and Qualitative Studies. Nutrients, 14(20), 4314. https://doi.org/10.3390/nu14204314







