Efficacy and Safety of a Personalized Vitamin D3 Loading Dose Followed by Daily 2000 IU in Colorectal Cancer Patients with Vitamin D Insufficiency: Interim Analysis of a Randomized Controlled Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Intervention
2.3. Study Visits
2.4. Outcomes
- Mean difference in the serum 25(OH)D levels between the intervention and placebo groups at visits 1 and 2.
- Mean difference in the change of the serum 25(OH)D levels from screening to visits 1 and 2.
- Difference in prevalence of subjects with adequate serum 25(OH)D levels ≥ 50 nmol/L [2] in the intervention group and placebo group at visits 1 and 2.
- Difference in frequency of the hypervitaminosis D (25(OH)D levels > 150 nmol/L [2]), hypercalcemia (albumin-corrected serum calcium > 2.65 mmol/L [16]), hypercalciuria (random urine calcium ≥ 0.79 mmol/mmol creatinine [17]), and renal dysfunction (eGFR < 30 mL/min/1.73 m2 calculated with the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [18]) between the intervention and placebo group at visits 1 and 2.
- Mean differences in the levels of albumin-corrected serum calcium, urine calcium/creatinine ratio, and eGFR between the intervention and placebo groups at visits 1 and 2.
2.5. Laboratory Methods for 25(OH)D Measurements
2.6. Statistical Analysis
3. Results
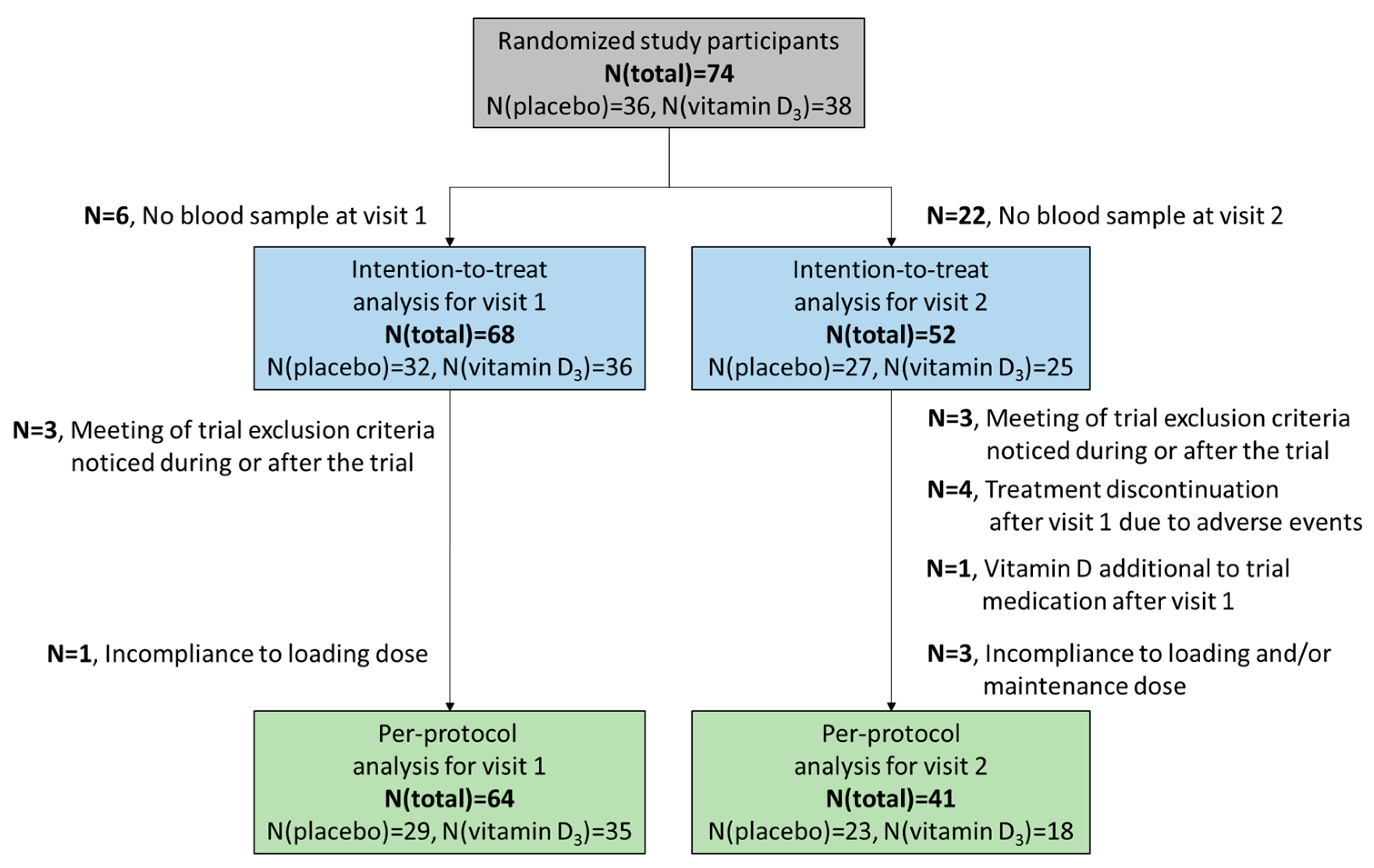
3.1. Participants’ Characteristics
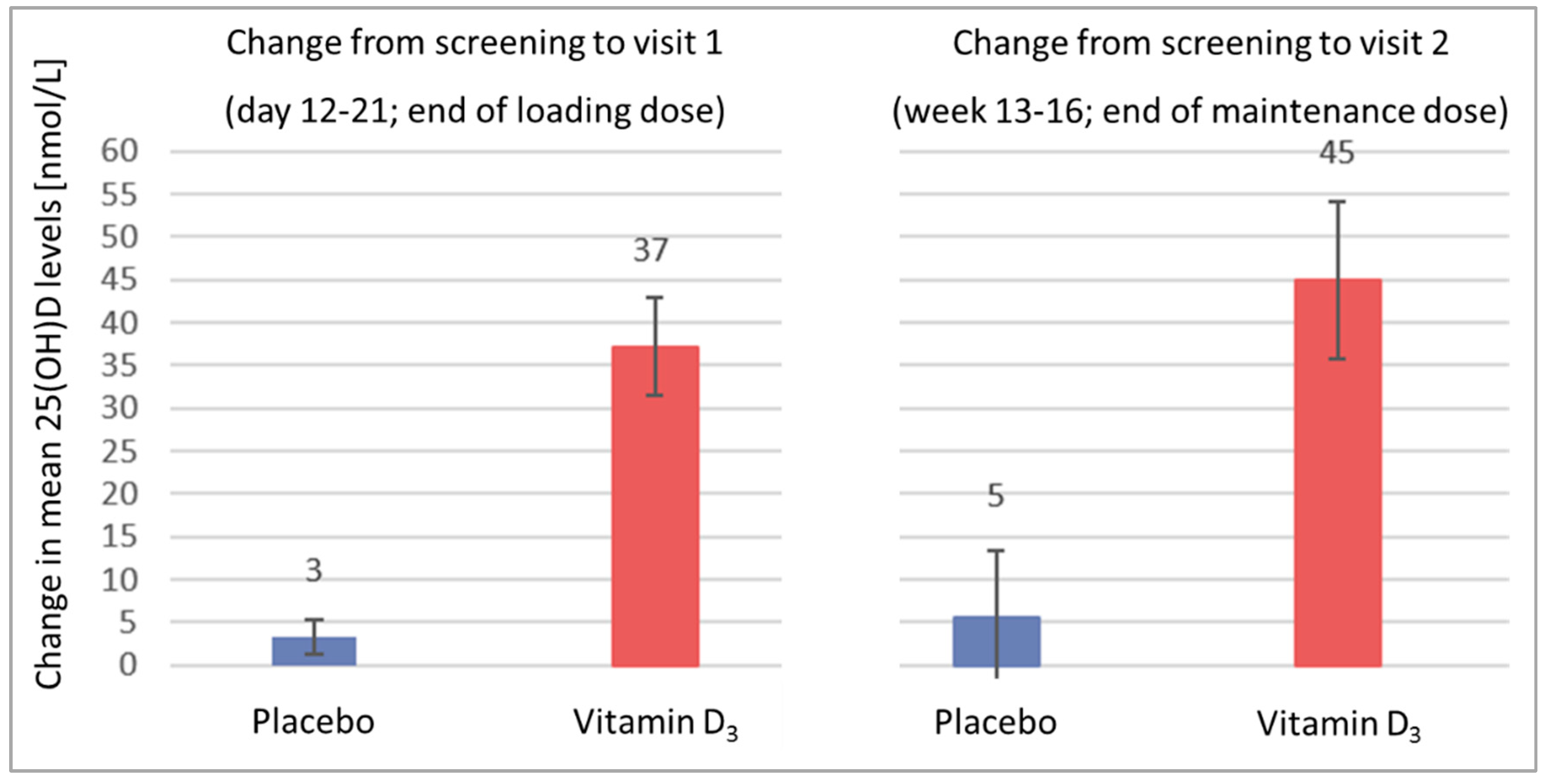
3.2. Efficacy Endpoints
3.2.1. Serum 25(OH)D Levels in the Total Trial Population
3.2.2. Serum 25(OH)D Levels in Patients with Vitamin D Deficiency at Enrolment
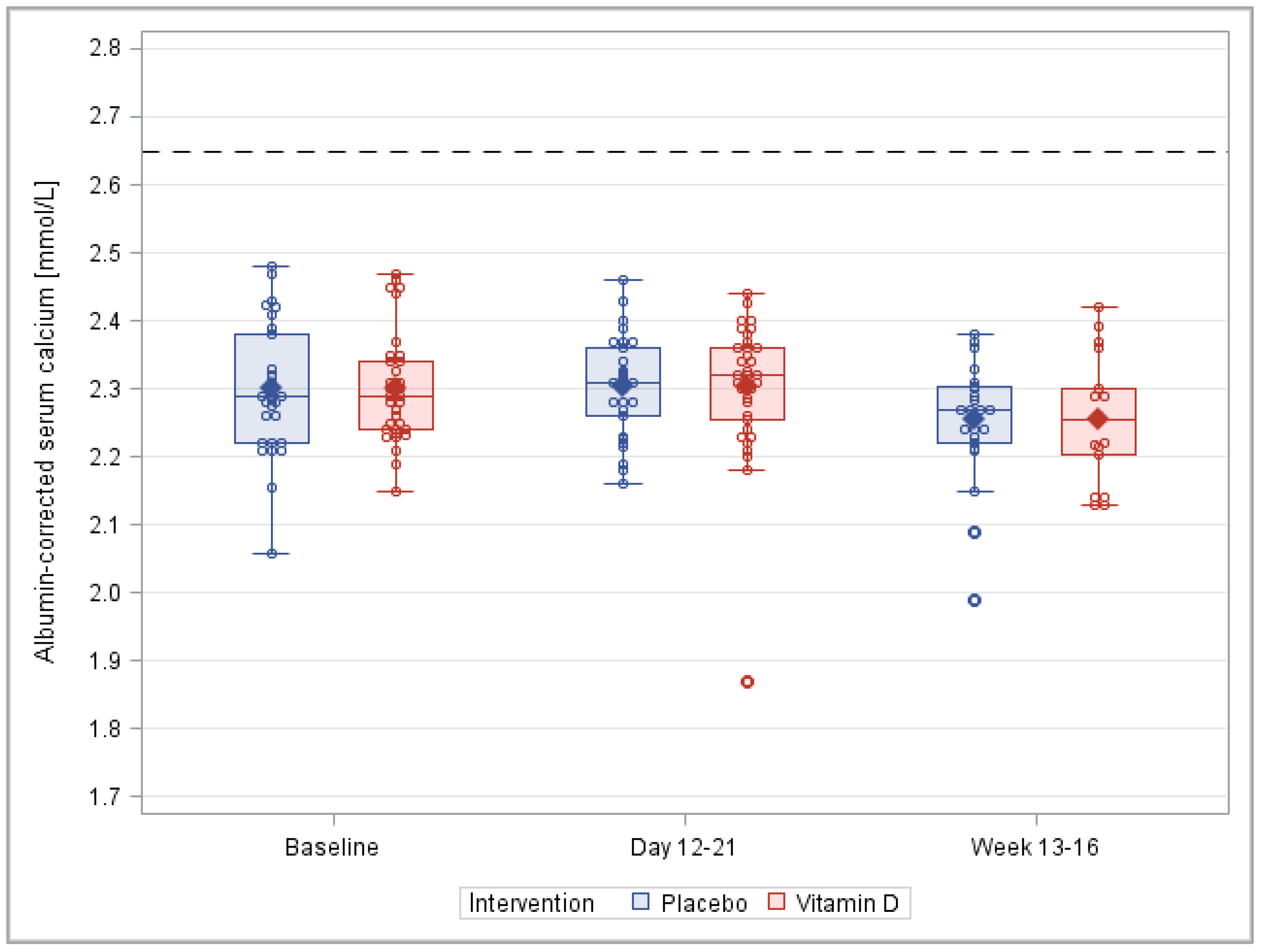
3.3. Safety Endpoints
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Robert-Koch-Institut. Darmkrebs in Deutschland 2018. Available online: https://www.krebsdaten.de/Krebs/DE/Content/Krebsarten/Darmkrebs/darmkrebs_node.html (accessed on 24 March 2022).
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D; National Academy Press: Washington DC, USA, 2011; Available online: https://nap.nationalacademies.org/catalog/13050/dietary-reference-intakes-for-calcium-and-vitamin-d (accessed on 17 October 2022).
- Skender, S.; Bohm, J.; Schrotz-King, P.; Chang-Claude, J.; Siegel, E.M.; Steindorf, K.; Owen, R.W.; Ose, J.; Hoffmeister, M.; Brenner, H.; et al. Plasma 25-Hydroxyvitamin D3 Levels in Colorectal Cancer Patients and Associations with Physical Activity. Nutr. Cancer 2017, 69, 229–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maalmi, H.; Walter, V.; Jansen, L.; Chang-Claude, J.; Owen, R.W.; Ulrich, A.; Schöttker, B.; Hoffmeister, M.; Brenner, H. Relationship of very low serum 25-hydroxyvitamin D3 levels with long-term survival in a large cohort of colorectal cancer patients from Germany. Eur. J. Epidemiol. 2017, 32, 961–971. [Google Scholar] [CrossRef] [PubMed]
- Maalmi, H.; Walter, V.; Jansen, L.; Boakye, D.; Schöttker, B.; Hoffmeister, M.; Brenner, H. Association between Blood 25-Hydroxyvitamin D Levels and Survival in Colorectal Cancer Patients: An Updated Systematic Review and Meta-Analysis. Nutrients 2018, 10, 896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wesselink, E.; Kok, D.E.; de Wilt, J.H.W.; Bours, M.J.L.; van Zutphen, M.; Keulen, E.T.P.; Kruyt, F.M.; Breukink, S.O.; Kouwenhoven, E.A.; van den Ouweland, J.; et al. Sufficient 25-Hydroxyvitamin D Levels 2 Years after Colorectal Cancer Diagnosis are Associated with a Lower Risk of All-cause Mortality. Cancer Epidemiol. Biomark. Prev. 2021, 30, 765–773. [Google Scholar] [CrossRef]
- Zhou, J.; Ge, X.; Fan, X.; Wang, J.; Miao, L.; Hang, D. Associations of vitamin D status with colorectal cancer risk and survival. Int. J. Cancer 2021, 149, 606–614. [Google Scholar] [CrossRef]
- Vaughan-Shaw, P.G.; Buijs, L.F.; Blackmur, J.P.; Theodoratou, E.; Zgaga, L.; Din, F.V.N.; Farrington, S.M.; Dunlop, M.G. The effect of vitamin D supplementation on survival in patients with colorectal cancer: Systematic review and meta-analysis of randomised controlled trials. Br. J. Cancer 2020, 123, 1705–1712. [Google Scholar] [CrossRef]
- Peng, J.; Liu, Y.; Xie, J.; Yang, G.; Huang, Z. Effects of vitamin D on drugs: Response and disposal. Nutrition 2020, 74, 110734. [Google Scholar] [CrossRef]
- van Groningen, L.; Opdenoordt, S.; van Sorge, A.; Telting, D.; Giesen, A.; de Boer, H. Cholecalciferol loading dose guideline for vitamin D-deficient adults. Eur. J. Endocrinol. 2010, 162, 805–811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffer, L.J.; Robitaille, L.; Swinton, N.; Agulnik, J.; Cohen, V.; Small, D.; Pepe, C.; Eintracht, S. Appropriate vitamin D loading regimen for patients with advanced lung cancer. Nutr. J. 2016, 15, 84. [Google Scholar] [CrossRef] [Green Version]
- Jansen, R.B.; Svendsen, O.L. The effect of oral loading doses of cholecalciferol on the serum concentration of 25-OH-vitamin-D. Int. J. Vitam. Nutr. Res. 2014, 84, 45–54. [Google Scholar] [CrossRef]
- Heaney, R.P.; Armas, L.A. Quantifying the vitamin D economy. Nutr. Rev. 2015, 73, 51–67. [Google Scholar] [CrossRef]
- Schöttker, B.; Kuznia, S.; Laetsch, D.C.; Czock, D.; Kopp-Schneider, A.; Caspari, R.; Brenner, H. Protocol of the VICTORIA study: Personalized vitamin D supplementation for reducing or preventing fatigue and enhancing quality of life of patients with colorectal tumor—randomized intervention trial. BMC Cancer 2020, 20, 739. [Google Scholar] [CrossRef]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [Green Version]
- Meng, Q.H.; Wagar, E.A. Laboratory approaches for the diagnosis and assessment of hypercalcemia. Crit. Rev. Clin. Lab. Sci. 2015, 52, 107–119. [Google Scholar] [CrossRef]
- Tellioglu, A.; Basaran, S.; Guzel, R.; Seydaoglu, G. Efficacy and safety of high dose intramuscular or oral cholecalciferol in vitamin D deficient/insufficient elderly. Maturitas 2012, 72, 332–338. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., III; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van, L.F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Romagnoli, E.; Mascia, M.L.; Cipriani, C.; Fassino, V.; Mazzei, F.; D’Erasmo, E.; Carnevale, V.; Scillitani, A.; Minisola, S. Short and long-term variations in serum calciotropic hormones after a single very large dose of ergocalciferol (vitamin D2) or cholecalciferol (vitamin D3) in the elderly. J. Clin. Endocrinol. Metab. 2008, 93, 3015–3020. [Google Scholar] [CrossRef]
- Leventis, P.; Kiely, P.D. The tolerability and biochemical effects of high-dose bolus vitamin D2 and D3 supplementation in patients with vitamin D insufficiency. Scand. J. Rheumatol. 2009, 38, 149–153. [Google Scholar] [CrossRef]
- Kaur, P.; Mishra, S.K.; Mithal, A. Vitamin D toxicity resulting from overzealous correction of vitamin D deficiency. Clin. Endocrinol. 2015, 83, 327–331. [Google Scholar] [CrossRef]
- Chen, P.Z.; Li, M.; Duan, X.H.; Jia, J.Y.; Li, J.Q.; Chu, R.A.; Yu, C.; Han, J.H.; Wang, H. Pharmacokinetics and effects of demographic factors on blood 25(OH)D3 levels after a single orally administered high dose of vitamin D3. Acta Pharmacol. Sin. 2016, 37, 1509–1515. [Google Scholar] [CrossRef]
- Pludowski, P.; Holick, M.F.; Grant, W.B.; Konstantynowicz, J.; Mascarenhas, M.R.; Haq, A.; Povoroznyuk, V.; Balatska, N.; Barbosa, A.P.; Karonova, T.; et al. Vitamin D supplementation guidelines. J. Steroid Biochem. Mol. Biol. 2018, 175, 125–135. [Google Scholar] [CrossRef] [Green Version]
- Zhu, A.; Kuznia, S.; Niedermaier, T.; Holleczek, B.; Schöttker, B.; Brenner, H. Vitamin D-binding protein, total, “nonbioavailable,” bioavailable, and free 25-hydroxyvitamin D, and mortality in a large population-based cohort of older adults. J. Intern. Med. 2022, 292, 463–476. [Google Scholar] [CrossRef]
- Fan, X.; Wang, J.; Song, M.; Giovannucci, E.L.; Ma, H.; Jin, G.; Hu, Z.; Shen, H.; Hang, D. Vitamin D Status and Risk of All-Cause and Cause-Specific Mortality in a Large Cohort: Results From the UK Biobank. J. Clin. Endocrinol. Metab. 2020, 105, e3606–e3619. [Google Scholar] [CrossRef]
- Wijnen, H.; Salemink, D.; Roovers, L.; Taekema, D.; de Boer, H. Vitamin D supplementation in nursing home patients: Randomized controlled trial of standard daily dose versus individualized loading dose regimen. Drugs Aging 2015, 32, 371–378. [Google Scholar] [CrossRef]
- Mazess, R.B.; Bischoff-Ferrari, H.A.; Dawson-Hughes, B. Vitamin D: Bolus Is Bogus-A Narrative Review. JBMR Plus 2021, 5, e10567. [Google Scholar] [CrossRef]
- Keum, N.; Chen, Q.Y.; Lee, D.H.; Manson, J.E.; Giovannucci, E. Vitamin D supplementation and total cancer incidence and mortality by daily vs. infrequent large-bolus dosing strategies: A meta-analysis of randomised controlled trials. Br. J. Cancer 2022, 127, 872–878. [Google Scholar] [CrossRef]
- Wimalawansa, S.J.; Whittle, R. Vitamin D: A single initial dose is not bogus if followed by an appropriate maintenance intake. JBMR Plus 2022, 6, e10606. [Google Scholar] [CrossRef]
- Holick, M.F. Vitamin D: A d-lightful solution for health. J. Investig. Med. 2011, 59, 872–880. [Google Scholar] [CrossRef]
- Holick, M.F.; Biancuzzo, R.M.; Chen, T.C.; Klein, E.K.; Young, A.; Bibuld, D.; Reitz, R.; Salameh, W.; Ameri, A.; Tannenbaum, A.D. Vitamin D2 is as effective as vitamin D3 in maintaining circulating concentrations of 25-hydroxyvitamin D. J. Clin. Endocrinol. Metab. 2008, 93, 677–681. [Google Scholar] [CrossRef]
- Jenkins, D.J.A.; Spence, J.D.; Giovannucci, E.L.; Kim, Y.-i.; Josse, R.; Vieth, R.; Blanco Mejia, S.; Viguiliouk, E.; Nishi, S.; Sahye-Pudaruth, S.; et al. Supplemental Vitamins and Minerals for CVD Prevention and Treatment. J. Am. Coll. Cardiol. 2018, 71, 2570–2584. [Google Scholar] [CrossRef]
- Khan, S.U.; Khan, M.U.; Riaz, H.; Valavoor, S.; Zhao, D.; Vaughan, L.; Okunrintemi, V.; Riaz, I.B.; Khan, M.S.; Kaluski, E.; et al. Effects of Nutritional Supplements and Dietary Interventions on Cardiovascular Outcomes: An Umbrella Review and Evidence Map. Ann. Intern. Med. 2019, 171, 190–198. [Google Scholar] [CrossRef]




| All Randomized (N = 74) | Vitamin D3 (N = 38) | Placebo (N = 36) | |
|---|---|---|---|
| Age [years], mean (SD) | 61.8 (9.8) | 62.1 (9.9) | 61.6 (9.7) |
| Sex | |||
| Female, n, % | 24 (32.4) | 14 (36.8) | 10 (27.8) |
| Male, n, % | 50 (67.6) | 24 (63.2) | 26 (72.2) |
| Cancer stage | |||
| I, n, % | 25 (33.8) | 8 (21.1) | 17 (47.2) |
| II, n, % | 22 (29.7) | 17 (44.7) | 5 (13.9) |
| III, n, % | 22 (29.7) | 11 (28.9) | 11 (30.6) |
| Unknown, n, % | 5 (6.8) | 2 (5.3) | 3 (8.3) |
| BMI (kg/m2), mean (SD) | 28.2 (5.8) | 28.5 (6.1) | 28.0 (5.5) |
| 25(OH)D level (nmol/L), mean (SD) | 27.3 (10.7) | 26.5 (9.9) | 28.2 (11.6) |
| Albumin-corrected serum calcium (mmol/L), mean (SD) | 2.29 (0.10) | 2.29 (0.09) | 2.29 (0.11) |
| Urinary calcium-to-creatinine ratio (mmol/mmol), mean (SD) | 0.28 (0.19) | 0.28 (0.20) | 0.28 (0.17) |
| Estimated glomerular filtration rate (ml/min/1.73 m2), mean (SD) | 87.8 (15.0) | 89.0 (15.4) | 86.5 (14.6) |
| Trial Arm | N | Vitamin D Insufficiency | p a | |
|---|---|---|---|---|
| (25(OH)D < 50 nmoL/L) | ||||
| No N (%) | Yes N (%) | |||
| Visit 1 (Days 12–21; end of loading dose) | ||||
| Placebo | 29 | 1 (3.5) | 28 (96.6) | <0.001 |
| Vitamin D3 | 35 | 28 (80.0) | 7 (20.0) | |
| Visit 2 (Weeks 13–16; end of maintenance dose) | ||||
| Placebo | 23 | 4 (17.4) | 19 (82.6) | <0.001 |
| Vitamin D3 | 18 | 18 (100.0) | 0 (0.0) | |
| Trial Arm | N | Hypervitaminosis D 1 | Hypercalcemia 2 | Hypercalciuria 3 | Renal Dysfunction 4 |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | ||
| Visit 1; end of loading dose; days 12–21 | |||||
| Placebo | 29 | 0 (0) | 0 (0) | 1 (3.4) | 0 (0) |
| Vitamin D3 | 35 | 0 (0) | 0 (0) | 5 (14.3) | 0 (0) |
| Visit 2; end of maintenance dose; weeks 13–16 | |||||
| Placebo | 23 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Vitamin D3 | 18 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuznia, S.; Czock, D.; Kopp-Schneider, A.; Caspari, R.; Fischer, H.; Laetsch, D.C.; Slavic, M.; Brenner, H.; Schöttker, B. Efficacy and Safety of a Personalized Vitamin D3 Loading Dose Followed by Daily 2000 IU in Colorectal Cancer Patients with Vitamin D Insufficiency: Interim Analysis of a Randomized Controlled Trial. Nutrients 2022, 14, 4546. https://doi.org/10.3390/nu14214546
Kuznia S, Czock D, Kopp-Schneider A, Caspari R, Fischer H, Laetsch DC, Slavic M, Brenner H, Schöttker B. Efficacy and Safety of a Personalized Vitamin D3 Loading Dose Followed by Daily 2000 IU in Colorectal Cancer Patients with Vitamin D Insufficiency: Interim Analysis of a Randomized Controlled Trial. Nutrients. 2022; 14(21):4546. https://doi.org/10.3390/nu14214546
Chicago/Turabian StyleKuznia, Sabine, David Czock, Annette Kopp-Schneider, Reiner Caspari, Harald Fischer, Dana Clarissa Laetsch, Marija Slavic, Hermann Brenner, and Ben Schöttker. 2022. "Efficacy and Safety of a Personalized Vitamin D3 Loading Dose Followed by Daily 2000 IU in Colorectal Cancer Patients with Vitamin D Insufficiency: Interim Analysis of a Randomized Controlled Trial" Nutrients 14, no. 21: 4546. https://doi.org/10.3390/nu14214546





