Abstract
Approximately 20% of the community-dwelling Japanese elderly (≥65 years) experience falling annually, with injury frequency rising with age. Increased nursing home admission/hospitalization risk influences healthy aging and QOL. Nutrition for musculoskeletal health is necessary, though the relationship of falling with nutritional status in the elderly is largely unknown. We investigated falling incidents and nutritional status, including a Japanese-style diet in a community-dwelling cohort. Using a cross-sectional design, 186 subjects (median age 83.0 years, males/females 67/119) were analyzed. Oral and systemic health conditions were assessed. A brief-type self-administered diet history questionnaire (BDHQ) was given for nutritional status. Analysis of covariance (adjusted for gender, age, BMI, articular disease/osteoporosis history, present tooth number, educational level) and the Japanese-Mediterranean diet (jMD) score adapted for Japan were used. The jMD score and falling incidents were significantly associated, with point increases related to a significantly decreased falling risk of 28% (OR: 0.72; 95%CI: 0.57–0.91). Of the 13 jMD food components, fish, eggs, and potatoes had a significant relationship with reduced falling, while significant associations of intake of animal protein, potassium, magnesium, zinc, and cholesterol (p < 0.05) were also observed. The results suggest that the jMD dietary pattern is an important factor for the prevention of falling incidents in elderly individuals.
1. Introduction
Individuals over 65 years old in Japan number 36.2 million and comprise 28.9% of the population. It has been reported that one in every three elderly people experience falling, with approximately 6% of those falls leading to fractures and 24% to severe injuries [1]. In addition, the frequency of falls is known to increase with age, peaking in the 80s.
The annual incidence of falls at home among the elderly in Japan has been reported to range from 6.8% to 17.3% for men and 13.7% to 22.9% for women. Since bone health and muscle health are linked, sarcopenia, that is, age-related loss of muscle mass, strength, and function, should also be considered. Furthermore, osteosarcopenia can lead to a loss of independence and disability, as well as increased morbidity and mortality, and reduced quality of life [2].
Risk factors known to be associated with falling include advanced age, sarcopenia, osteoporosis, spinal arthritis and central nervous system disease, poor balance function, and depression [3]. Additionally, an association between oral status and falls has been reported [4], with a significantly increased risk of falling in individuals with 19 or fewer teeth and no dentures. Analyses of nutritional intake and bone health have also been summarized in several reviews [5]. Intake of vitamin D and protein, as well as calcium and magnesium, along with five servings of vegetables and fruits each day have been stated as important dietary recommendations for maintaining bone health. Furthermore, dietary patterns such as the Mediterranean diet (MED) are known to be associated with a lower risk of falling and fracture.
The MED was shown to be associated with a lower risk of falling in a Spanish report that studied older adults aged 60 years and older [6]. However, the association of the MED with falling incidents and fractures has yet to be established. According to a systematic review presented by Malmir et al. [7], there are few epidemiologic studies showing an association between the MED and bone mineral density or risk of fracture in older individuals in their 70s and 80s. Furthermore, though several related reports of subjects with similar ages have been presented, the results are likely biased due to the wide range of ages examined. On the other hand, a more recent epidemiological study of community-dwelling men aged 81 years found that adherence to the MED was associated with fewer falls, while consumption of higher levels of monounsaturated fatty acids and saturated fatty acids, and a higher ratio of monounsaturated fatty acids to saturated fatty acids, were associated with a reduced risk of falling [8]. In an epidemiological study of subjects with an average age of approximately 70 years, higher adherence to the MED was related to a lower risk of falling [6].
Previous studies presented findings that the consumption of animal protein led to greater muscle mass as compared to plant-sourced protein (e.g., soy and wheat) [9]. However, the details regarding the associations of the of plant- and animal-sourced diets with muscle and bone health were not clear [10]. The present study was conducted to investigate the effects of dietary patterns indicating nutrient intake on falling incidents in elderly individuals in Japan. We hypothesized that consumption of both animal protein and a Japanese-style dietary pattern by the elderly would lead to the prevention of falling incidents.
2. Materials and Methods
2.1. Study Design and Participants
This was a cross-sectional study conducted from April 2015 to November 2020. It was conducted with residents of Buzen, Fukuoka Prefecture, Japan, a city with a population of about 25,000, who are mainly engaged in agriculture and fishing. All participants were enrolled in the National Health Insurance and the Late-Stage Senior Citizens Health Insurance plans.
2.2. Recruitment and Participants
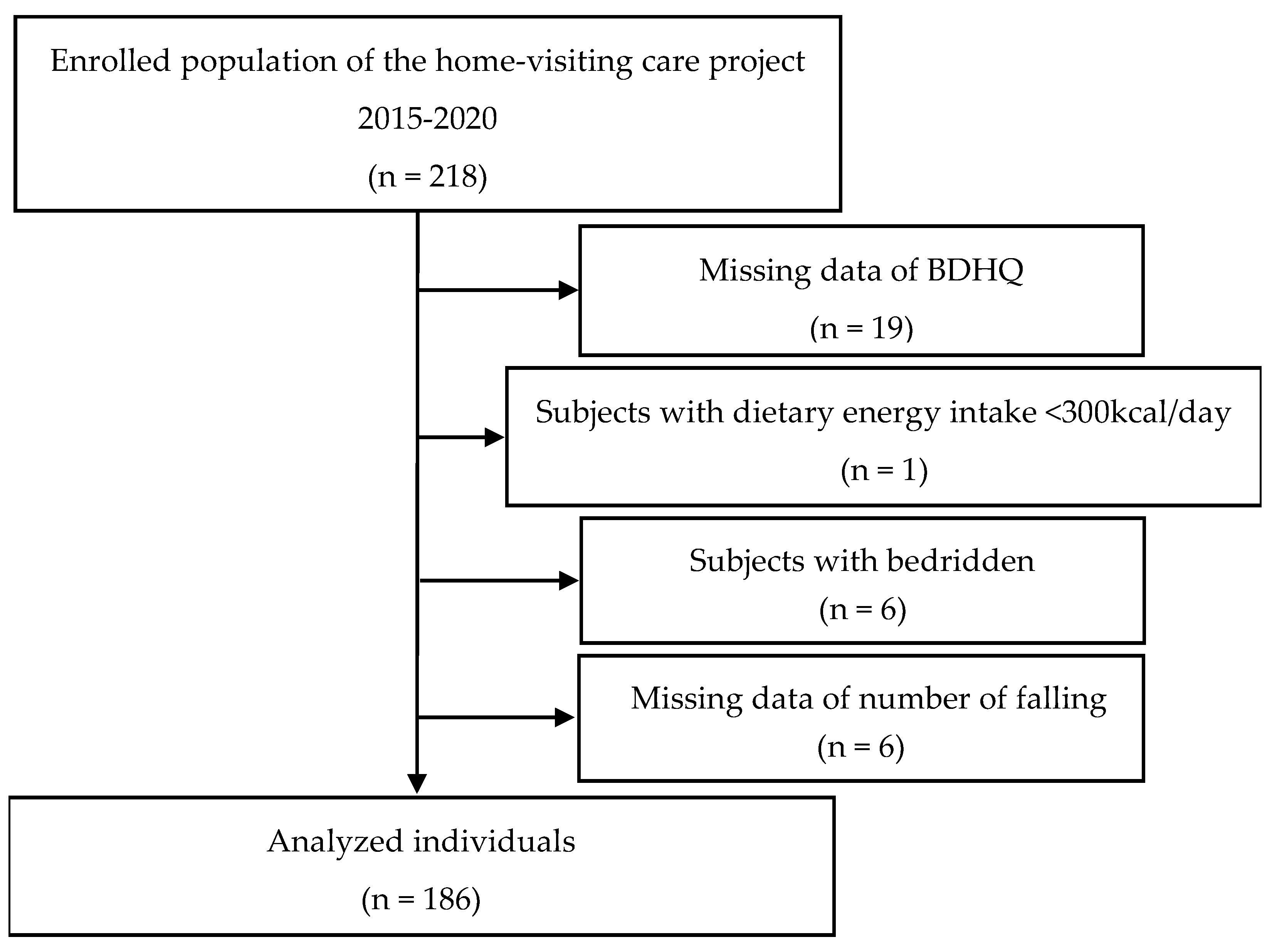
The Buzen City government sent an invitation by mail to elderly individuals aged 75 years and older based on the population composition rate, as the Late-Stage Senior Citizens Health Insurance Plan in Japan provides coverage for citizens of that age. At the time of the initial invitation in April 2015, the percentage of males and females aged 75 or older was reported to be 35.3% and 64.7%, respectively. A total of 218 age-qualified individuals (34% male, 66% female) gave consent to the invitation and were surveyed by a home visitation. Of those, 186 (36% male, 64% female) were included in the present analysis, after exclusion of individuals with incomplete data, a daily energy intake <300 kcal, or who were bedridden (Figure 1). The present survey was approved by the Ethics Committee of our university (No. 20-31).
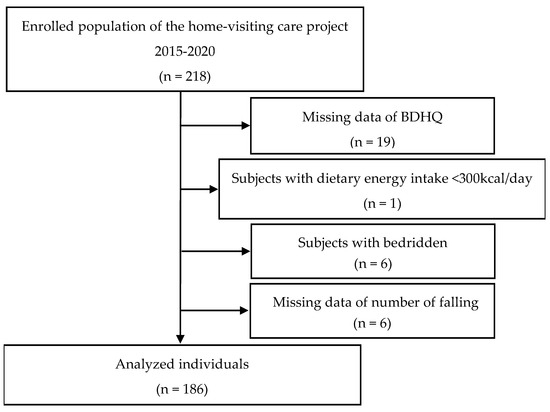
Figure 1.
Flow diagram of participants selection.
2.3. Sample Size Calculation
Sample size was estimated on the basis of a 30% prevalence of falling incidents by elderly individuals previously reported [1] and a relative 20% reduction in the non-faller group. Accordingly, a total of 156 individuals was estimated to achieve 80% power for a two-sided test at a statistical significance level of 5%.
2.4. Dietary Assessment
To assess intake of nutrients and food groups, a brief-type self-administered diet history questionnaire (BDHQ) was employed, which has been used in prior epidemiological studies, and confirmed for validity and accuracy by Kobayashi et al. [11]. The questionnaire asked respondents to indicate the frequency of consumption of specific foods among 58 food items, including beverages, by selecting from seven possible responses (twice a day or more, once a day, 4–6 times a week, 2–3 times a week, once a week, less than once a week, not eaten). This dietary survey method was designed to obtain information regarding an individual’s habitual intake of nutrients and foods during the past month’s meals [11]. Dietitians provided oral and written instructions on how to complete the BDHQ to the participants or their family members, and requested that they complete the form in advance. On the day of the home visit, a dietitian checked the BDHQ completed by the participant for errors or incompleteness, and also provided nutritional guidance, including food selection and cooking methods, as needed. For this study, the intake of each nutrient obtained from the BDHQ results was adjusted for energy using the density method (g/1000 kcal).
2.5. Japanese Modified Mediterranean Diet Score
According to the method reported by Kanauchi et al. [12], a Japanese-adapted MD (jMD) scoring system was used. Briefly, the jMD score was calculated based on the consumption of thirteen components (grains, vegetables, fruits, legumes, fish, dairy products, potatoes, poultry, eggs, red and processed meat, sweets, alcohol, ratio of monounsaturated to saturated fatty acids), with a value of 0 or 1 assigned to each of those thirteen components. One point was given for meeting each of the following consumption criteria; (1) three to seven servings of grains per day, (2) five or more servings of vegetables per day, (3) two or more servings of fruits per day, (4) 30 g or more of legumes per day, (5) 84 g or more of fish per day for men and 66 g or more for women, (6) 1.5–2.5 servings of dairy products per day, (7) potatoes consumed one to three times per week, (8) poultry two to three times per week, (9) eggs two to three times per week, (10) meat or meat products less than three times per week, (11) sweets less than two times per week, (12) 10–30 g of alcohol per day for men and 5–15 g for women, and (13) ratio of monounsaturated fatty acids to saturated fatty acids of 1.5 or greater. Otherwise, a score of zero was assigned. The range of possible total points was from 0 to 13, with a higher score indicating better adherence to the jMD.
2.6. Outcome Variable, Falling Incident
Incident falls were determined by the use of a short questionnaire. First the question “Have you had any falls over the previous 12 months?”, with a possible answer of “Yes” or “No”, was given. If “Yes” was answered, the subject was asked to report the number of falls. Those with more than two falls during that time were defined as “fallers”, as previous studies have found that single fallers are more similar to non-fallers than recurrent fallers in regard to a range of medical, physical, and psychological risk factors [13,14].
2.7. Body Composition
Body composition was assessed using bioelectrical impedance analysis with an InBody S10 device (InBody Japan, Tokyo, Japan). A tetra-polar eight-point tactile electrode system was also used, according to the manufacturer’s guidelines. Measurements were performed with the participant in a lying posture between 2:00 and 4:00 PM, with the immediate postprandial period avoided. Skeletal muscle mass (SMM) calculations were performed according to a previously reported method [15]. Briefly, the extremity skeletal muscle mass index (SMI) was determined based on the sum of the upper and lower extremities, then the SMI was calculated by dividing the SMM by participant height in square meters (kg/m2).
2.8. Physical Function
A handgrip strength test was performed using a handheld dynamometer (T.K.K.5401, Takei Kiki Company, Niigata, Japan). Measurements were taken twice with each hand. After calculating the average value of each side, the larger value was used. Calf circumference (CC) on both sides was measured using a measuring tape with the largest circumference between the fibula head and outer edge of the lower leg noted.
2.9. Oral Examination
Assessments of tooth and/or denture conditions were performed by calibrated dentists, as described in our previous report [16].
2.10. Blood Examination
Blood tests were performed using a blood test kit (DEMECAL Leisure, Tokyo, Japan) [17]. Samples were collected from a fingertip and analyzed with a laboratory instrument (Demecal Healthcare Research Center, Yamanashi, Japan). The system provided results for 13 parameters; total protein, albumin, AST, ALT, γ-GTP, total cholesterol, HDL-C, triglycerides, BUN, creatinine, uric acid, glucose, and HbA1c.
2.11. Others
For medical history, information regarding hypertension, cardiovascular disease, cerebrovascular disease, cancer, dementia, articular disease, osteoporosis, and depression was obtained by letter from the primary care physician and the National Health Insurance database. Sarcopenia was assessed based on handgrip strength, CC, and SMI [15]. The Charlson Comorbidity Index, based on number of diseases noted in medical history records, was also calculated [18]. Information regarding alcohol consumption, smoking habit, and education level was obtained with a self-administered questionnaire.
2.12. Statistical Analyses
For comparisons between the faller and non-faller groups, a t-test was used when normality was observed, and the Mann–Whitney U-test was used when normality was not observed, with the Kolmogorov–Smirnov test used to test normality. When the distribution of nutrient intake did not follow a normal distribution, a log transformation was used to bring the analysis closer to a normal distribution. Mean differences between the groups were analyzed with analysis of covariance (ANCOVA), with covariates fed into the model selected based on previous studies. Risk factors related to falling were classified as internal or external [19]. Internal factors included age-related changes, such as muscle weakness, diseases such as arthritis, orthostatic hypotension, Parkinson’s disease, and hemiplegia, as well as medications taken, such as sleeping pills, antihypertensive drugs, and psychotropic drugs. External factors were considered to involve the living environment, such as house/apartment, clothing, and shoes. Other sociodemographic factors, such as educational history and assistive device use, in addition to gender and age, have also been reported to be associated [20]. Thus, the present model was adjusted for age, gender, body mass index (BMI), history of articular disease and/or osteoporosis, number of teeth, and educational level. All statistical analysis was executed using the SPSS software package, ver. 27 (IBM Corp., Armonk, NY, USA), with a p value < 0.05 considered to indicate significance.
3. Results
3.1. Basic Characteristics of Study Populations
The median age of the 186 subjects was 83.0 years, and there were 67 males and 119 females (36% and 64%, respectively). Table 1 shows the characteristics of the subjects according to falling status. Significant associations were observed in regard to history of articular disease (p = 0.02) and cancer (p = 0.04), while a significant tendency was observed between education level and falls (p = 0.05). No other significant association was found for the other variables.

Table 1.
Basic characteristics of study populations.
3.2. JMD Food Intake and Falling
Table 2 shows the intake of each of the 13 food groups in the jMD with relationship to falling. Significant associations were found in regard to the intake of fish, eggs, and potatoes (p = 0.01, 0.03, and 0.04, respectively). All of the foods, except for grains, dairy products, and sweets, tended to be consumed more in the non-faller than faller group.

Table 2.
Association of jMD food group components with falling.
3.3. Nutrient Intake and Falling
Table 3 shows nutrient intake according to falling incidents. Nutrients that still showed a reciprocal action after log transformation were excluded from the results. Significant associations were observed for the intake of protein (p = 0.01), animal protein (p < 0.01), potassium (p = 0.046), magnesium (p = 0.03), zinc (p = 0.02), and cholesterol (p < 0.01). Additionally, marginal associations were observed for iron, phosphorus, and vitamins D, E, and C.

Table 3.
Association of nutrient intake with falling.
3.4. Logistic Regression Analysis
Table 4 shows the results of logistic regression analysis of the association between the jMD and falling, with falls as the dependent variable. The results were adjusted for gender, age, and BMI (Model 1: [OR] 0.77, 95% [CI] 0.62–0.95, p = 0.016), and further for history of articular disease and osteoporosis (Model 2: [OR] 0.76, [CI] 0.61–0.94, p = 0.013). Model 3 shows the results after adjusting for the other covariates, plus number of teeth and education level ([OR] 0.72, [CI] 0.57–0.91, p = 0.005). The results indicated that a point increase in the jMD score was associated with a 28% decrease in falling risk.

Table 4.
Multivariable adjusted OR and 95% CI for the association of jMD and falling.
4. Discussion
The results of this cross-sectional study of community-dwelling elderly individuals showed that a reduction in risk of falling was significantly associated with the intake of potassium, magnesium, zinc, and cholesterol, as well as protein, including animal as opposed to plant protein. In addition to use of the jMD as a dietary pattern, which is consistent with findings described in a review by Rizzoli et al. [5], this is the first known study to examine the association of nutrients and dietary patterns with the risk of falling in very old individuals, and also the first such examination conducted with an Asian population.
Dietary patterns have also been reported to be important for reducing fracture risk [5]. Other recent studies regarding the association of the MED as a dietary pattern with falls include systematic reviews presented by Ballesteros et al. [6] and Malmir et al. [7], both of which suggested that adherence to the MED lowered the risk of falling and fracture. Additionally, Ballesteros et al. [6] suggested that the accumulated or synergic impact of several foods, including fish and nuts, as well as vegetable intake, had a more beneficial effect as compared to a single food or nutrient.
The involvement of bioactive components such as polyphenols, carotenoids, and phytosterols has been pointed out as a pathway by which the MED can influence sarcopenia and osteoporosis [21,22]. Thus, it is plausible that adherence to the jMD may be a factor related to reducing the risk of falling, as shown in the present study.
On the other hand, there are some differences between the results of this and previous investigations. First, the present study found no association between vegetable intake and falling incidents, similar to the subgroup analysis findings presented by Lin et al. [23] of dark- and light-colored vegetables, though the reasons are unknown. Umezawa et al. [24] reported that the diet consumed in rural areas of Japan was characterized by higher intake of home-grown vegetables, as well as those given by neighboring farmers, as compared to such products purchased from a grocery store, likely due to cultural settings where vegetables are more readily available. This may explain why the present study found no significant difference between the faller and non-faller groups. Second, there was no significant association between calcium intake and falling shown in the present findings, while that between vitamin D and falling was only marginally significant. Many studies have reported that calcium intake is effective for reducing the risk of falls and fractures, though the optimal level of calcium remains to be firmly established. In particular, individuals over 75 years of age have decreased intestinal calcium absorption and the appropriate intake amount varies widely [5]. Lemming et al. [25] examined the associations of combinations of dietary calcium intake and the MED with the risk of hip fracture, and found that while calcium had some effect, calcium alone was not sufficient for the optimal prevention of a hip fracture.
Nutrients found to be significantly associated with falling incidents included potassium, magnesium and zinc, which have positive effects on bone health, as described previously [26]. According to a recent review [5], magnesium has a role in parathyroid hormone secretion and potassium homeostasis. Another report noted that hip bone mineral density was positively correlated with magnesium intake [27]. Also, zinc is an essential nutrient used by various signaling pathways in nearly all cells in the human body, including bone cells. Details regarding the effects of these nutrients are discussed in the following.
Based on the BDHQ, the food group from which each nutrient was derived was determined. For example, in the non-faller group, magnesium was found to be obtained from fish in 21.2% and vegetables in 21.8%. In other words, this population obtained magnesium from consuming both fish and vegetables. However, the results shown in Table 2 indicate that it was fish, eggs, and potatoes that were associated with falls, with most of the difference in magnesium consumption thought to be derived from fish. Results obtained the 2019 National Health and Nutrition Survey in Japan [28] indicated that 8.4% of magnesium was obtained from fish and 13.5% from vegetables, indicating that the present subjects consumed a much higher quantity of fish. This was consistent with our expectation based on the geographical location of the study area, which is facing the sea. Zinc is contained in oysters, and other shellfish, as well as meat and eggs. Similar to magnesium, a study using BDHQ found that about 49.2% of zinc consumed by a non-faller was derived from fish, meat, eggs, and dairy products, while 28.6% was from grains, and 8.9% from vegetables. These results may indicate potential reasons why fish and eggs were associated with falling incidents in our study. In present non-fallers, 32.0% of the potassium intake came from vegetables and 14.4% from fish. Although there was a significant difference in potassium intake between the non-faller and faller groups, vegetables, the main type of food consumed, were not found to be associated with falls for reasons mentioned earlier. Cholesterol and its metabolites have complex functions in osteogenesis, osteoclastogenesis, and bone homeostasis, depending on the form consumed [29]. Thus, the present findings indicate that cholesterol can sometimes be beneficial for bones. In addition, cholesterol is known to be included in large quantity in eggs, fish and shellfish, meat, and dairy products.
Though the differential effects of protein sources on musculoskeletal health remains to be clarified, potato protein supplementation was reported to increase muscle protein synthesis, both at rest and following resistance exercise in healthy young women [30]. On the other hand, there are few known epidemiological studies that have examined differences between animal and plant proteins, particularly in elderly individuals. The present results indicated a significant association of protein and animal protein intake with falling, while no association was seen with the intake of plant-sourced protein (Table 3). Among the 13 components of the jMD, there was a significant difference for potatoes. In general, the ingestion of animal protein leads to greater muscle mass as compared to plant-sourced protein, though there may not be a large difference between plant and animal proteins, especially among the elderly [10]. In the present results, grain ingestion was the most common (estimated at approximately 70%), while that of potatoes had a low percentage. This may explain why there was no significant difference regarding plant protein between the two groups. These results suggest that animal proteins have an important role in preventing against falling incidents, even in the elderly. Nevertheless, further studies are needed for confirmation.
The present subgroup analysis showed a gender difference regarding nutrients and fall risk, with a stronger trend in males (data not shown). Epidemiological studies that examined the association of the combined effect of dietary patterns and nutrition with the risk of falling have been limited, and most focused on a single gender. Although the reason for the difference between genders seen in the present results is unclear, the BDHQ mentioned that errors regarding food intake reported may vary between them [31], which might have influenced our results. Another possible reason is that the limited number of subjects did not provide sufficient statistical power. This study targeted community-dwelling individuals and is an ongoing project. It is important to provide community-based care, including dietary and nutritional guidance, on a regular basis through health education and information provided to local residents by collaborating with local government agencies to prevent falling incidents.
Important aspects of the present results include the following. First, elderly individuals received focus, which has not been shown in previous studies. Second, the age range of the subjects was narrow and the cohort was homogenous. Furthermore, while associations of food components with the risks of falling and fracture have been examined, few epidemiological studies related to nutrients have been presented. In addition, there have been no studies regarding nutrients and the MED in Japanese individuals, except for the report by Kanauchi et al. [12].
This study had several limitations. Because of the cross-sectional nature, causality could not be analyzed. Furthermore, when using the BDHQ to examine nutrient intake in an epidemiological study, multiple surveys are desirable [11], while only a single BDHQ evaluation was used for the present analysis. In addition, some risk factors related to falling could not be investigated, as there was limited information regarding external factors, such as balance limiting activity, hearing impairment, or house structure, such as floors, lighting, and stepping obstacles like stairs. Finally, the enrolled subjects comprised approximately 3% of the elderly population aged 75 years or older in Buzen City; thus, generalizability is considered to be limited. The use of longitudinal cohorts with a larger sample size will be necessary to clarify the present results.
5. Conclusions
In the present study, the consumption of fish, eggs, and potatoes included in the diet were found to be associated with falling incidents in the elderly. Additionally, protein, especially animal protein, and the nutrients potassium, magnesium, zinc, and cholesterol were also associated with falls. Together, the results suggest that the jMD represents one of the healthiest dietary patterns and is an important factor for the prevention of falling incidents by elderly individuals.
Author Contributions
T.A. was responsible for the study design, analysis, interpretation of results, and manuscript writing. S.K. was responsible for data cleaning, analysis, and manuscript editing. J.-W.P. carried out the data collection and wrote the first draft of the manuscript. R.S. and T.H. contributed toward analysis and interpretation of data. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported in part by Grants-in-Aid for Scientific Research number 16K11868 and 19K10449 (SK).
Institutional Review Board Statement
The study was approved by the ethics committee of Kyushu Dental University (7 October 2020 approved).
Informed Consent Statement
This study was conducted in accordance with the guidelines laid down in the Declaration of Helsinki, and written informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgments
Special thanks to all the staff involved in this study and the most tremendous respect to the participants.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Matsuda, R. Life-style choices and falls. An empirical study of older people. In Health Inequalities in Japan; Kondo, K., Ed.; Trans Pac. Press: Melbourne, Australia, 2010; pp. 37–50. [Google Scholar]
- Daly, R.M. Exercise and nutritional approaches to prevent frail bones, falls and fractures: An update. Climacteric 2017, 20, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Guideline for the Prevention of Falls in Older Persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J. Am. Geriatr. Soc. 2001, 49, 664–672. [Google Scholar]
- Yamamoto, T.; Kondo, K.; Misawa, J.; Hirai, H.; Nakade, M.; Aida, J.; Kondo, N.; Kawachi, I.; Hirata, Y. Dental status and incident falls among older Japanese: A prospective cohort study. BMJ Open 2012, 2, e001262. [Google Scholar] [CrossRef] [PubMed]
- Rizzoli, R.; Biver, E.; Brennan-Speranza, T.C. Nutritional intake and bone health. Lancet Diabetes Endocrinol. 2021, 9, 606–621. [Google Scholar] [CrossRef]
- Ballesteros, J.M.; Struijk, E.A.; Rodriguez-Artalejo, F.; Lopez-Garcia, E. Mediterranean diet and risk of falling in community-dwelling older adults. Clin. Nutr. 2020, 39, 276–281. [Google Scholar] [CrossRef]
- Malmir, H.; Saneei, P.; Larijani, B.; Esmaillzadeh, A. Adherence to Mediterranean diet in relation to bone mineral density and risk of fracture: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2018, 57, 2147–2160. [Google Scholar] [CrossRef]
- Cervo, M.M.C.; Scott, D.; Seibel, M.J.; Cumming, R.G.; Naganathan, V.; Blyth, F.M.; Le Couteur, D.G.; Handelsman, D.J.; Ribeiro, R.V.; Waite, L.M.; et al. Adherence to Mediterranean diet and its associations with circulating cytokines, musculoskeletal health and incident falls in community-dwelling older men: The Concord Health and Ageing in Men Project. Clin. Nutr. 2021, 40, 5753–5763. [Google Scholar] [CrossRef]
- van Vliet, S.; Burd, N.A.; van Loon, L.J. The Skeletal Muscle Anabolic Response to Plant- versus Animal-Based Protein Consumption. J. Nutr. 2015, 145, 1981–1991. [Google Scholar] [CrossRef]
- Putra, C.; Konow, N.; Gage, M.; York, C.G.; Mangano, K.M. Protein Source and Muscle Health in Older Adults: A Literature Review. Nutrients 2021, 13, 743. [Google Scholar] [CrossRef]
- Kobayashi, S.; Honda, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Both comprehensive and brief self-administered diet history questionnaires satisfactorily rank nutrient intakes in Japanese adults. J. Epidemiol. 2012, 22, 151–159. [Google Scholar] [CrossRef]
- Kanauchi, M.; Kanauchi, K. Development of a Mediterranean diet score adapted to Japan and its relation to obesity risk. Food Nutr. Res. 2016, 60, 32172. [Google Scholar] [CrossRef] [PubMed]
- Nevitt, M.C.; Cummings, S.R.; Kidd, S.; Black, D. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA 1989, 261, 2663–2668. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.R.; Clark, R.D.; Webster, I.W. Physiological factors associated with falls in an elderly population. J. Am. Geriatr. Soc. 1991, 39, 1194–1200. [Google Scholar] [CrossRef]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e302. [Google Scholar] [CrossRef]
- Hiroshimaya, T.; Iwasaki, M.; Sakai, R.; Kakuta, S.; Hamasaki, T.; Kataoka, S.; Tutsui, S.; Ansai, T. A pilot study of the relationship between whole-body skeletal mass and tongue pressure in ≥75-year-ols individualas requiring home-based support. J. Dent. Health 2018, 68, 145–152. (In Japanese) [Google Scholar] [CrossRef]
- Horita, M.; Sugimoto, S.; Hokazono, E.; Osawa, S. Establishment of mail medical examination system using immediate plasma separating device by the self-collection blood--the method of dilution ratio calculation by using Internal standard for the sample with different amount of collecting blood. Rinsho Byori 2008, 56, 577–583. [Google Scholar] [PubMed]
- Quan, H.; Li, B.; Couris, C.M.; Fushimi, K.; Graham, P.; Hider, P.; Januel, J.M.; Sundararajan, V. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am. J. Epidemiol. 2011, 173, 676–682. [Google Scholar] [CrossRef]
- Hagino, H. Epidemiology and evidence of prevention for falls. Jpn J. Rehabil. Med. 2018, 55, 898–904. [Google Scholar] [CrossRef][Green Version]
- Sharif, S.I.; Al-Harbi, A.B.; Al-Shihabi, A.M.; Al-Daour, D.S.; Sharif, R.S. Falls in the elderly: Assessment of prevalence and risk factors. Pharm Pr. 2018, 16, 1206. [Google Scholar] [CrossRef]
- Cederholm, T.; Cruz-Jentoft, A.J.; Maggi, S. Sarcopenia and fragility fractures. Eur J. Phys. Rehabil. Med. 2013, 49, 111–117. [Google Scholar]
- Romero, A.; Rivas, A. Adherence to Mediterranean diet and bone health. Nutr. Hosp. 2014, 29, 989–996. [Google Scholar]
- Lin, C.H.; Chen, K.H.; Chen, C.M.; Chang, C.H.; Huang, T.J.; Hsu, H.C.; Huang, S.Y. Low vegetable intake increases the risk of fall-related fragility fracture in postmenopausal Taiwanese women, a prospective pilot study in the community. Biomed. J. 2016, 39, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Umezawa, A.; Miwa, T.; Shibui, E.; Namikawa, T.; Tanaka, N.; Ishikawa, M. Total vegetable intake and homegrown vegetable intake in the rural area residents of Hokkaido. Jpn. J. Nutr. Diet. 2012, 70, 283–293. [Google Scholar] [CrossRef][Green Version]
- Lemming, E.; Byberg, L.; Höijer, J.; Larsson, S.C.; Wolk, A.; Michaësson, K. Combinations of dietary calcium intake and Mediterranean-style diet on risk of hip fracture: A longitudinal cohort study of 82,000 women and men. Clin. Nutr. 2021, 40, 4161–4170. [Google Scholar] [CrossRef] [PubMed]
- Tucker, K.L.; Hannan, M.T.; Chen, H.; Cupples, L.A.; Wilson, P.W.; Kiel, D.P. Potassium, magnesium, and fruit and vegetable intakes are associated with greater bone mineral density in elderly men and women. Am. J. Clin. Nutr 1999, 69, 727–736. [Google Scholar] [CrossRef]
- Orchard, T.S.; Larson, J.C.; Alghothani, N.; Bout-Tabaku, S.; Cauley, J.A.; Chen, Z.; LaCroix, A.Z.; Wactawski-Wende, J.; Jackson, R.D. Magnesium intake, bone mineral density, and fractures: Results from the Women’s Health Initiative Observational Study. Am. J. Clin. Nutr. 2014, 99, 926–933. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. National Health and Nutrition Survey. Available online: https://www.mhlw.go.jp/bunya/kenkou/kenkou_eiyou_chousa.html (accessed on 11 October 2022).
- Yin, W.; Li, Z.; Zhang, W. Modulation of Bone and Marrow Niche by Cholesterol. Nutrients 2019, 11, 1394. [Google Scholar] [CrossRef]
- Oikawa, S.Y.; Bahniwal, R.; Holloway, T.M.; Lim, C.; McLeod, J.C.; McGlory, C.; Baker, S.K.; Phillips, S.M. Potato Protein Isolate Stimulates Muscle Protein Synthesis at Rest and with Resistance Exercise in Young Women. Nutrients 2020, 12, 1235. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Murakami, K.; Sasaki, S.; Okubo, H.; Hirota, N.; Notsu, A.; Fukui, M.; Date, C. Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011, 14, 1200–1211. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).