Implementing DASH-Aligned Meals and Self-Measured Blood Pressure to Reduce Hypertension at Senior Centers: A RE-AIM Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Ethics
2.2. Study Design
2.3. Study Aims
2.4. Study Participants and Settings
2.5. Study Interventions
2.6. Study Measures
3. Results
3.1. Reach: The Representativeness of Individuals Willing to Participate in Program, and Reasons Why or Why Not
Study Enrollment and Participant Demographics
3.2. Effectiveness
3.2.1. Change in BP
3.2.2. Change in Psychosocial and Health Behavior Measures/Surveys
3.3. Adoption
3.3.1. CBN, RU, and CDN Partnership
3.3.2. External Advisors
3.3.3. DFTA
3.3.4. Collaborative Study Workgroups
3.4. Implementation
3.4.1. Congregate Meal Fidelity: Delivery of Meals As-Served versus As-Planned
3.4.2. COVID Interruption/End of DASH Congregate Meals (Feasibility)
3.4.3. Client Engagement in Menu Development
3.4.4. DASH Congregate Meals Attendance and Satisfaction (Client Acceptability)
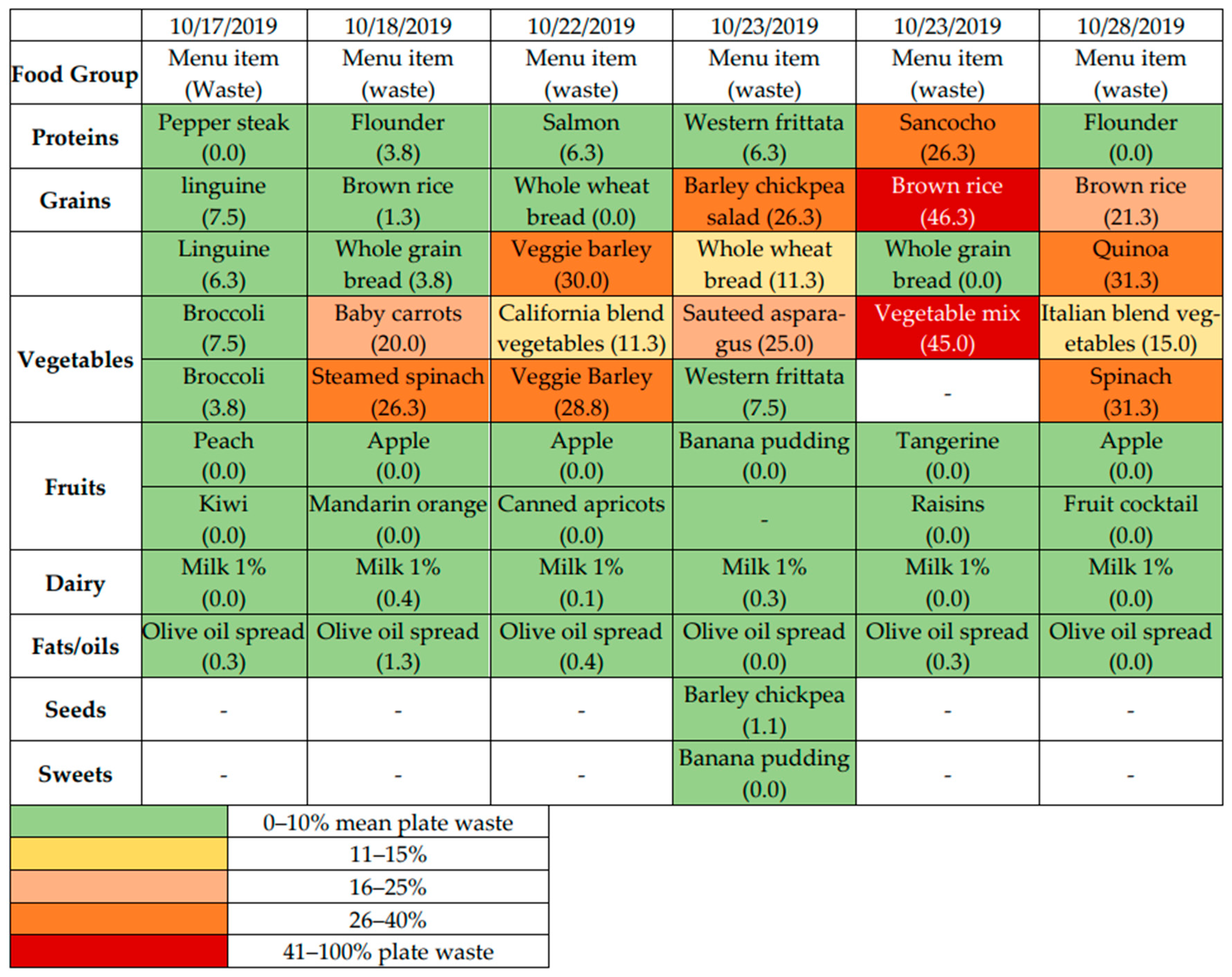
3.4.5. Plate Waste (Acceptability)
3.4.6. Food Cost (Feasibility)
3.4.7. Home Self-Measured Blood Pressure (SMBP) Implementation (Fidelity and Feasibility)
3.4.8. Health Education Program
3.5. Maintenance
4. Discussion
4.1. Reach
4.2. Effectiveness
4.3. Adoption
4.4. Implementation
4.5. Maintenance
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- Salt
- Removed saltshakers from tables;
- Eliminated adding high sodium prepared mixed seasonings while cooking;
- Food service staff made mixed spices on site that contained less salt and relied on herbs and spices for flavor;
- Onion powder, garlic powder, dried oregano, thyme, rosemary, chives, lemon zest, cumin, turmeric, pepper, cayenne, cinnamon, cloves, and nutmeg.
- Fats
- Replaced butter with olive oil;
- Replaced heavy cream with 1% milk in recipes;
- Butter removed from tables, replaced with olive oil spread;
- Started serving avocado;
- Premade spreads were expensive so initially CBN cooks made an olive oil spread on site which was messy and required extra labor. The seniors did not enjoy it and complained;
- In response to client response, the CBN Food Service Manager ordered Smart Balance spread through a restaurant supply website (it was not available through regular congregate meal vendors);
- Smart Balance was significantly more expensive (25 cents/serving versus 3 cents/serving for butter), but seniors were satisfied with the change and meal satisfaction ratings increased.
- Fruits and vegetables
- Additional serving of fruit and vegetables added to each meal—increased cost;
- Added mushrooms, peas, carrots and other vegetables to starches;
- Added spinach, mushrooms and other vegetables to omelets;
- Added more vegetables and fresh herbs to sofrito—peppers, parsley, scallions.
- Sugar
- Fruit juices and soda were replaced with lemon water.
- Grains
- Replaced highly processed grains and starches with whole grain options;
- Nuts, seeds, and legumes;
- Sesame, sunflower, and pumpkin seeds offered on the side; not incorporated into prepared foods out of concern for any dental issues the seniors might have;
- Nuts not offered as some clients were allergic.
Appendix B. Sample Menus


References
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; et al. Heart Disease and Stroke Statistics—2016 Update. Circulation 2016, 133, e38–e360. [Google Scholar] [CrossRef] [PubMed]
- CDC Hypertension Prevalence in the U.S. Million Hearts®. Available online: https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html (accessed on 16 July 2021).
- Fryar, C.D.; Ostchega, Y.; Hales, C.M.; Zhang, G.; Kruszon-Moran, D. Hypertension Prevalence and Control among Adults: United States, 2015-2016. NCHS Data Brief 2017, 289, 1–8. [Google Scholar]
- Raue, P.J.; Sirey, J.A.; Dawson, A.; Berman, J.; Bruce, M.L. Lay-Delivered Behavioral Activation for Depressed Senior Center Clients: Pilot RCT. Int. J. Geriatr. Psychiatry 2019, 34, 1715–1723. [Google Scholar] [CrossRef] [PubMed]
- What Is a Senior Center? Available online: https://www.ncoa.org/article/get-the-facts-on-senior-centers (accessed on 6 September 2022).
- LaTrella, P.; Bosnick, M.; Chin, J.; Di, J. NYC Department of Aging: Services Snapshot. 2020. Available online: https://www.nyc.gov/assets/dfta/downloads/pdf/reports/DFTASnapshotFY2019.pdf (accessed on 15 September 2021).
- Vasquez, K.; Guishard, D.; Dionne, W.; Jurenko, A.; Jiang, C.; Coffran, C.; Ronning, A.; George-Alexander, G.; Mofunanya, C.; Ceballo, O.C.; et al. A Community-Academic Partnership to Understand Correlates of Successful Aging in Place. Presented at the Translational Science 2018, Washington, DC, USA, 19–21 April 2018. [Google Scholar]
- Appel, L.J.; Brands, M.W.; Daniels, S.R.; Karanja, N.; Elmer, P.J.; Sacks, F.M.; American Heart Association. Dietary Approaches to Prevent and Treat Hypertension: A Scientific Statement from the American Heart Association. Hypertension 2006, 47, 296–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appel, L.J.; Moore, T.J.; Obarzanek, E.; Vollmer, W.M.; Svetkey, L.P.; Sacks, F.M.; Bray, G.A.; Vogt, T.M.; Cutler, J.A.; Windhauser, M.M.; et al. A Clinical Trial of the Effects of Dietary Patterns on Blood Pressure. DASH Collaborative Research Group. N. Engl. J. Med. 1997, 336, 1117–1124. [Google Scholar] [CrossRef] [Green Version]
- Sacks, F.M.; Svetkey, L.P.; Vollmer, W.M.; Appel, L.J.; Bray, G.A.; Harsha, D.; Obarzanek, E.; Conlin, P.R.; Miller, E.R.; Simons-Morton, D.G.; et al. Effects on Blood Pressure of Reduced Dietary Sodium and the Dietary Approaches to Stop Hypertension (DASH) Diet. DASH-Sodium Collaborative Research Group. N. Engl. J. Med. 2001, 344, 3–10. [Google Scholar] [CrossRef]
- Baker, E.A.; Barnidge, E.K.; Schootman, M.; Sawicki, M.; Motton-Kershaw, F.L. Adaptation of a Modified DASH Diet to a Rural African American Community Setting. Am. J. Prev. Med. 2016, 51, 967–974. [Google Scholar] [CrossRef] [Green Version]
- Ivery, J.M.; Benton, L.; Harrison, A.; Paul, M.; Cortés, M. The DASH Pilot Project: Developing Community-Based Nutrition Education for Older Adults. J. Gerontol. Soc. Work 2017, 60, 286–299. [Google Scholar] [CrossRef]
- McManus, R.J.; Mant, J.; Bray, E.P.; Holder, R.; Jones, M.I.; Greenfield, S.; Kaambwa, B.; Banting, M.; Bryan, S.; Little, P.; et al. Telemonitoring and Self-Management in the Control of Hypertension (TASMINH2): A Randomised Controlled Trial. Lancet 2010, 376, 163–172. [Google Scholar] [CrossRef]
- McManus, R.J.; Mant, J.; Haque, M.S.; Bray, E.P.; Bryan, S.; Greenfield, S.M.; Jones, M.I.; Jowett, S.; Little, P.; Penaloza, C.; et al. Effect of Self-Monitoring and Medication Self-Titration on Systolic Blood Pressure in Hypertensive Patients at High Risk of Cardiovascular Disease: The TASMIN-SR Randomized Clinical Trial. JAMA 2014, 312, 799–808. [Google Scholar] [CrossRef] [Green Version]
- McManus, R.J.; Mant, J.; Franssen, M.; Nickless, A.; Schwartz, C.; Hodgkinson, J.; Bradburn, P.; Farmer, A.; Grant, S.; Greenfield, S.M.; et al. Efficacy of Self-Monitored Blood Pressure, with or without Telemonitoring, for Titration of Antihypertensive Medication (TASMINH4): An Unmasked Randomised Controlled Trial. Lancet 2018, 391, 949–959. [Google Scholar] [CrossRef]
- Bray, E.P.; Holder, R.; Mant, J.; McManus, R.J. Does Self-Monitoring Reduce Blood Pressure? Meta-Analysis with Meta-Regression of Randomized Controlled Trials. Ann. Med. 2010, 42, 371–386. [Google Scholar] [CrossRef] [PubMed]
- Uhlig, K.; Patel, K.; Ip, S.; Kitsios, G.D.; Balk, E.M. Self-Measured Blood Pressure Monitoring in the Management of Hypertension. Ann. Intern. Med. 2013, 159, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.; Papadopoulos, A.; Silvers, C.T.; Charness, N.; Boot, W.R.; Schlachta-Fairchild, L.; Crump, C.; Martinez, M.; Ent, C.B. Remote Health Monitoring for Older Adults and Those with Heart Failure: Adherence and System Usability. Telemed. J. e-Health 2016, 22, 480–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Truncali, A.; Dumanovsky, T.; Stollman, H.; Angell, S.Y. Keep on Track: A Volunteer-Run Community-Based Intervention to Lower Blood Pressure in Older Adults. J. Am. Geriatr. Soc. 2010, 58, 1177–1183. [Google Scholar] [CrossRef] [PubMed]
- Muldoon, M.F.; Einhorn, J.; Yabes, J.G.; Burton, D.; Irizarry, T.; Basse, J.; Forman, D.E.; Rollman, B.L.; Burke, L.E.; Kamarck, T.W.; et al. Randomized Feasibility Trial of a Digital Intervention for Hypertension Self-Management. J. Hum. Hypertens. 2021, 36, 718–725. [Google Scholar] [CrossRef]
- Felix, H.C.; Adams, B.; Cornell, C.E.; Fausett, J.K.; Krukowski, R.A.; Love, S.J.; Prewitt, T.E.; West, D.S. Barriers and Facilitators to Senior Centers Participating in Translational Research. Res. Aging 2014, 36, 22–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernandez, S.; Scales, K.L.; Pineiro, J.M.; Schoenthaler, A.M.; Ogedegbe, G. A Senior Center–Based Pilot Trial of the Effect of Lifestyle Intervention on Blood Pressure in Minority Elderly People with Hypertension. J. Am. Geriatr. Soc. 2008, 56, 1860–1866. [Google Scholar] [CrossRef]
- Glasgow, R.E.; Harden, S.M.; Gaglio, B.; Rabin, B.; Smith, M.L.; Porter, G.C.; Ory, M.G.; Estabrooks, P.A. RE-AIM Planning and Evaluation Framework: Adapting to New Science and Practice with a 20-Year Review. Front. Public Health 2019, 7, 64. [Google Scholar] [CrossRef] [Green Version]
- Hashemi, A.; Vasquez, K.; Guishard, D.; Naji, M.; Ronning, A.; George-Alexander, G.; Vasquez, D.; Sylvester, C.; Pagano, W.; Khalida, C.; et al. Implementing DASH-Aligned Congregate Meals and Self-Measured Blood Pressure in Two Senior Centers: An Open Label Study. Nutr. Metab. Cardiovasc. Dis. 2022, 32, 1998–2009. [Google Scholar] [CrossRef]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; LeFevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [PubMed]
- New York City’s Department for the Aging. Profile of Older New Yorkers. 2017. Available online: https://www1.nyc.gov/assets/dfta/downloads/pdf/reports/ProfileOlderNYers10262017.pdf (accessed on 16 July 2021).
- Getts, K.M.; Quinn, E.L.; Johnson, D.B.; Otten, J.J. Validity and Interrater Reliability of the Visual Quarter-Waste Method for Assessing Food Waste in Middle School and High School Cafeteria Settings. J. Acad. Nutr. Diet 2017, 117, 1816–1821. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holtrop, J.S.; Estabrooks, P.A.; Gaglio, B.; Harden, S.M.; Kessler, R.S.; King, D.K.; Kwan, B.M.; Ory, M.G.; Rabin, B.A.; Shelton, R.C.; et al. Understanding and Applying the RE-AIM Framework: Clarifications and Resources. J. Clin. Transl. Sci. 2021, 5, e126. [Google Scholar] [CrossRef]
- N4a’s Aging Innovations and Achievement Awards Staff; National Association of Area Agencies on Aging: Washington, DC, USA, 2016; Available online: https://www.usaging.org/Files/2016AwardsBookFinal.pdf (accessed on 20 September 2022).



| RE AIM Dimension & Definition [29] | Study Data (Source) |
|---|---|
| Reach The absolute number, proportion, and representativeness of individuals who are willing to participate in a given initiative, intervention, or program, and reasons why or why not. |
|
| Effectiveness The impact of an intervention on important individual outcomes, including potential negative effects, and broader impact including quality of life and economic outcomes; and variability across subgroups (generalizability or heterogeneity of effects). |
|
| Adoption Multiple setting and staff levels: The absolute number, proportion, and representativeness of settings and intervention agents (people who deliver the program) who are willing to initiate a program, and why. Note that adoption can have many (nested) levels; e.g., staff under a supervisor under a clinic or school, under a system, under a community. |
|
| Implementation (Multiple settings and especially delivery staff level): The fidelity to the various elements of an intervention’s key functions or components, including consistency of delivery as intended and the time and cost of the implementation. Importantly, it also includes adaptations made to interventions and implementation strategies and reasons for the above results. | Congregate Meals
|
| Maintenance (Individual and setting levels): At the setting level, the extent to which a program or policy becomes institutionalized or part of the routine organizational practices and policies. At the individual level, maintenance has been defined as the long-term effects of a program on outcomes after a program is completed. The specific time frame for assessment of maintenance or sustainment varies across projects. |
|
| Demographic Characteristics | Study Participants, Both Sites (n = 84) | All Clients, Both Sites (n = 291) |
|---|---|---|
| Race | ||
| American/Indian/Alaskan Native | 1 (1%) | 1 (0.3%) |
| Asian | 2 (2%) | 58 (20%) |
| Black | 25 (30%) | 29 (10%) |
| Native Hawaiian or Other Pacific Islander | 0 (0%) | 1 (0.3%) |
| Multiple Races | 4 (5%) | 3 (1%) |
| White | 38 (45%) | 151 (52%) |
| Other | 5 (6%) | 5 (2%) |
| Unknown or Missing | 9 (11%) | 43 (15%) |
| Sex (Female) | 57 (68%) | 165 (57%) |
| Age | ||
| 60–74 | 47 (56%) | 149 (51%) |
| 75–84 | 30 (36%) | 97 (33%) |
| 85+ | 6 (7%) | 39 (13%) |
| Unknown | 1 (1%) | 6 (2%) |
| Site 1 (Breakfast and Lunch) | ||||
|---|---|---|---|---|
| As-Planned | As-Served Number of Servings (% of Goal) | |||
| Week 1 | Week 2 | Week 3 | ||
| Protein (1) | 15–30 | 23 (100%) | 21 (100%) | 23 (100%) |
| Grains | 20 | 23 (115%) | 21 (105%) | 18 (90%) |
| Vegetables | 15 | 16 (107%) | 20 (133%) | 21 (140%) |
| Fruit | 20 | 17 (85%) | 14 (70%) | 19 (95%) |
| Dairy | 10 | 10 (100%) | 10 (100%) | 10 (100%) |
| FAT | 10 | 11 (110%) | 7 (70%) | 8.5 (85%) |
| Sweets (2) | 4 | 1 (25%) | 1 (25%) | 0 (0%) |
| Nuts, legumes, dried peas and beans | 4 | 3 (75%) | 5 (125%) | 3 (75%) |
| Site 2 (Lunch) | ||||
| As-Planned | As-Served Number of Servings (% of Goal) | |||
| Week 1 | Week 2 | Week 3 | ||
| Protein (1) | 10–20 | 14 (100%) | 15 (100%) | 15 (100%) |
| Grains | 10 | 9 (90%) | 10 (100%) | 10 (100%) |
| Vegetables | 10 | 10 (100%) | 11 (110%) | 11 (110%) |
| Fruit | 10 | 8 (80%) | 11 (110%) | 11 (110%) |
| Dairy | 5 | 5 (100%) | 5 (100%) | 5 (100%) |
| FAT | 5 | 6 (120%) | 5 (100%) | 5 (100%) |
| Sweets (2) | 2–3 | 0 (0%) | 1 (50%) | 1 (50%) |
| Nuts, legumes, dried peas and beans | 4 | 3 (75%) | 3 (75%) | 3 (75%) |
| Excerpt of Responses from Research Town Hall ParticipantsWhat Did You Think of the Samples? | ||
|---|---|---|
| Site | Sample 1: Spinach | Sample 2: Barley Pilaf |
| Site 1 n = 30 |
|
|
| Site 2 n = 53 |
|
|
| Participant Reported Barriers and Facilitators during Self-Home Blood Pressure Monitoring | |
|---|---|
| Barriers | Facilitators |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hashemi-Arend, A.; Vasquez, K.S.; Guishard, D.; Naji, M.; Ronning, A.; George-Alexander, G.; Vasquez, D.; Sylvester, C.; Pagano, W.; Khalida, C.; et al. Implementing DASH-Aligned Meals and Self-Measured Blood Pressure to Reduce Hypertension at Senior Centers: A RE-AIM Analysis. Nutrients 2022, 14, 4890. https://doi.org/10.3390/nu14224890
Hashemi-Arend A, Vasquez KS, Guishard D, Naji M, Ronning A, George-Alexander G, Vasquez D, Sylvester C, Pagano W, Khalida C, et al. Implementing DASH-Aligned Meals and Self-Measured Blood Pressure to Reduce Hypertension at Senior Centers: A RE-AIM Analysis. Nutrients. 2022; 14(22):4890. https://doi.org/10.3390/nu14224890
Chicago/Turabian StyleHashemi-Arend, Anuradha, Kimberly S. Vasquez, Dozene Guishard, Moufdi Naji, Andrea Ronning, Glenis George-Alexander, Dacia Vasquez, Clewert Sylvester, William Pagano, Chamanara Khalida, and et al. 2022. "Implementing DASH-Aligned Meals and Self-Measured Blood Pressure to Reduce Hypertension at Senior Centers: A RE-AIM Analysis" Nutrients 14, no. 22: 4890. https://doi.org/10.3390/nu14224890
APA StyleHashemi-Arend, A., Vasquez, K. S., Guishard, D., Naji, M., Ronning, A., George-Alexander, G., Vasquez, D., Sylvester, C., Pagano, W., Khalida, C., Coffran, C., Ezeonu, T., Fofana, K., Bielopolski, D., Vaughan, R., Qureshi, A., Tobin, J. N., & Kost, R. G. (2022). Implementing DASH-Aligned Meals and Self-Measured Blood Pressure to Reduce Hypertension at Senior Centers: A RE-AIM Analysis. Nutrients, 14(22), 4890. https://doi.org/10.3390/nu14224890





