Association of Zinc with Anemia
Abstract
:1. Introduction
2. Anemia
3. Trace Elements Related to Anemia
3.1. Iron, Zinc, Copper, Manganese, Molybdenum, and Cobalt Are Related to Anemia
3.2. Iron-Deficiency Anemia
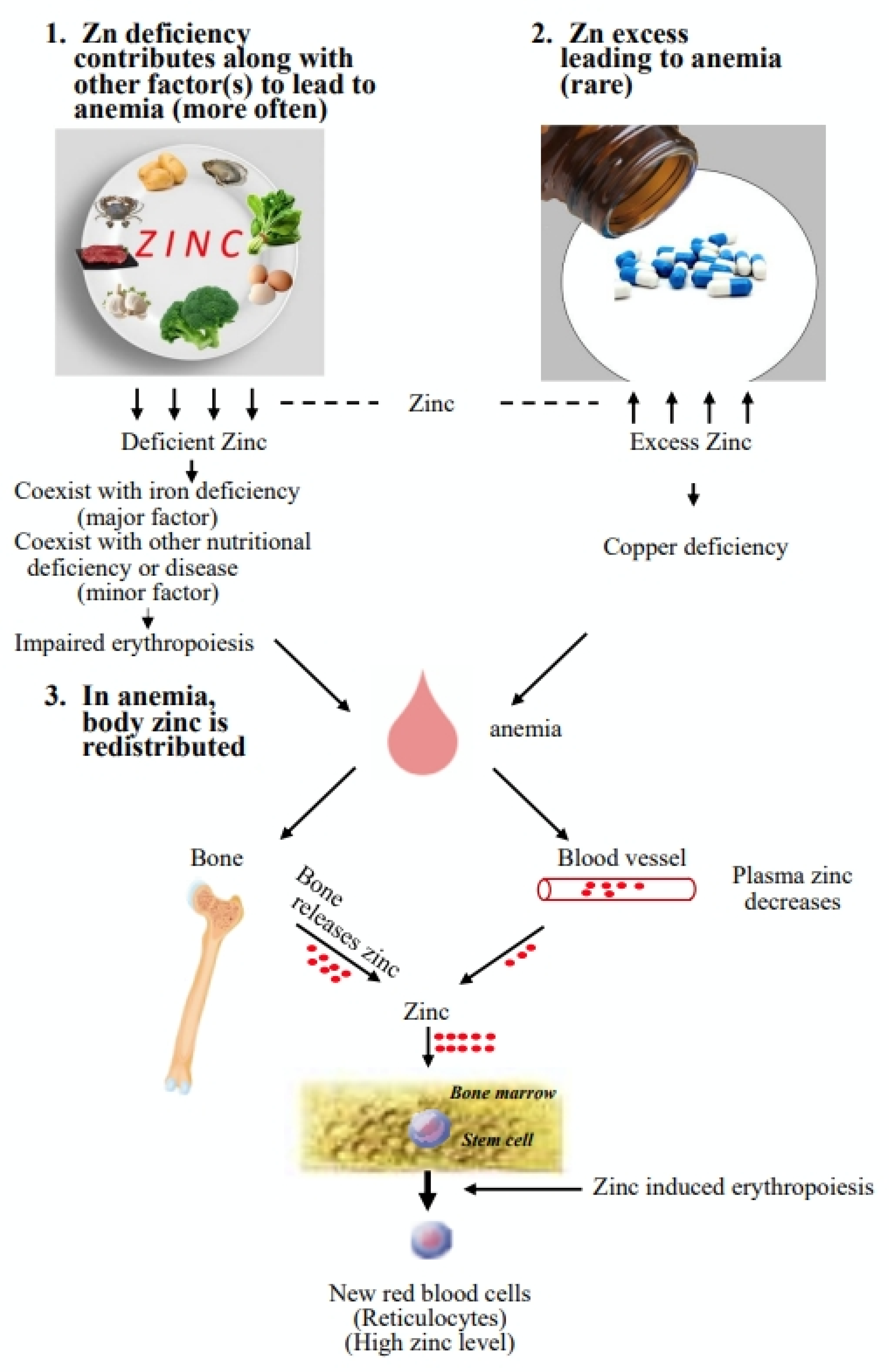
4. Association of Zinc with Anemia
5. Zinc Deficiency Contributing to Anemia
5.1. Zinc Deficiency Coexists with Iron-Deficiency Anemia
5.1.1. In Women of Reproductive Age
5.1.2. In Preschool-Aged Children
5.1.3. In Adults
5.2. Zinc and Iron Coexist in Food
5.3. In Anemia, Zinc Deficiency May Not Coexist with Iron Deficiency; However, It May Cooperate with Other Factors to Lead to Anemia
5.4. Zinc Is Essential for Erythropoiesis
5.5. Zinc Deficiency Alone Does Not Cause Anemia in Rats
5.6. Zinc Deficiency May Need to Cooperate with Other Factors to Lead to Anemia
5.7. Summary of the Association of Zinc Deficiency with Anemia
6. Excess Intake of Zinc Leads to Anemia
6.1. Types of Excess Intake
6.2. High Zinc Levels Induce Copper Deficiency
6.3. High Zinc Levels May Induce Iron Deficiency
6.4. Mechanism of Anemia Caused by Copper Deficiency
6.5. Summary of Excess Intake of Zinc Leading to Anemia
7. Anemia Leads to Abnormal Blood–Zinc Levels in the Body
7.1. High Prevalence of Anemia and Abnormal Blood–Zinc Levels in CKD Patients
7.2. Animal Model Studies Indicate That Abnormal Blood–Zinc Levels Might Be the Result of Anemia
7.3. In Anemia, Zinc Is Redistributed in the Body
7.4. Lower Plasma Zinc Levels in CKD Patients Could Be a Consequence of Anemia
7.5. Summary of Anemia Leading to Abnormal Blood—Zinc Levels in the Body
8. Supplementation of Zinc in Anemia
9. Conclusions
- The present review shows that zinc is highly associated with anemia, as shown in Figure 1. In humans at most ages, a significant proportion of cases of zinc deficiency coexist with iron deficiency, which might be the major cause of zinc deficiency contributing to anemia. Serum zinc levels should be evaluated in iron-deficient anemia patients, and combined iron and zinc supplementation should be considered if necessary.
- For adults or those who have chronic diseases, zinc deficiency might contribute to anemia; at the same time, anemia might render abnormal zinc status. It may be necessary to examine zinc status in CKD patients and to provide zinc supplementation if necessary.
- The possibility of using zinc compounds as an erythrocyte stimulating agent is high, and further research is needed.
- The involvement of zinc in anemia is complex, and the interplay of zinc with other factors or diseases in anemia deserves much more attention.
Author Contributions
Funding
Conflicts of Interest
References
- Vallee, B.L. Biochemistry, physiology and pathology of zinc. Physiol. Rev. 1959, 39, 443–490. [Google Scholar] [CrossRef] [PubMed]
- Vallee, B.L.; Falchuk, K.H. The biochemical basis of zinc physiology. Physiol. Rev. 1993, 73, 79–118. [Google Scholar] [CrossRef] [PubMed]
- Prasad, A.S. Zinc: An overview. Nutrition 1995, 11 (Suppl. S1), 93–99. [Google Scholar]
- Salgueiro, M.J.; Zubillaga, M.; Lysionek, A.; Sarabia, M.I.; Caro, R.; De Paoli, T.; Hager, A.; Weill, R.; Boccio, J. Zinc as an essential micronutrient: A review. Nutr. Res. 2000, 20, 737–755. [Google Scholar] [CrossRef]
- Tapiero, H.; Tew, K.D. Trace elements in human physiology and pathology: Zinc and metallothioneins. Biomed. Pharmacother. 2003, 57, 399–411. [Google Scholar] [CrossRef]
- Solomons, N.W. Update on zinc biology. Ann. Nutr. Metab. 2013, 62 (Suppl. S1), 8–17. [Google Scholar] [CrossRef]
- Maret, W. Zinc biochemistry: From a single zinc enzyme to a key element of life. Adv. Nutr. 2013, 4, 82–91. [Google Scholar] [CrossRef] [Green Version]
- Kaur, K.; Gupta, R.; Saraf, S.A.; Saraf, S.K. Zinc: The metal of life. Compr. Rev. Food Sci. Food Saf. 2014, 13, 358–376. [Google Scholar] [CrossRef] [PubMed]
- Livingstone, C. Zinc: Physiology, deficiency, and parenteral nutrition. Nutr. Clin. Pract. 2015, 30, 371–382. [Google Scholar] [CrossRef]
- Maares, M.; Haase, H. A Guide to Human Zinc Absorption: General Overview and Recent Advances of In Vitro Intestinal Models. Nutrients 2020, 12, 762. [Google Scholar] [CrossRef] [Green Version]
- Prasad, A.S. Clinical manifestations of zinc deficiency. Annu. Rev. Nutr. 1985, 5, 341–363. [Google Scholar] [CrossRef] [PubMed]
- Yanagisawa, H. Zinc Deficiency and Clinical Practice—Validity of Zinc Preparations. Yakugaku Zasshi 2008, 128, 333–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cummings, J.E.; Kovacic, J.P. The ubiquitous role of zinc in health and disease. J. Vet. Emerg. Crit. Care 2009, 19, 215–240. [Google Scholar] [CrossRef] [PubMed]
- Plum, L.M.; Rink, L.; Haase, H. The essential toxin: Impact of zinc on human health. Int. J. Environ. Res. Public Health 2010, 7, 1342–1365. [Google Scholar] [CrossRef] [Green Version]
- Chasapis, C.T.; Loutsidou, A.C.; Spiliopoulou, C.A.; Stefanidou, M.E. Zinc and human health: An up-date. Arch. Toxicol. 2012, 86, 521–534. [Google Scholar] [CrossRef]
- Roohani, N.; Hurrell, R.; Kelishadi, R.; Schulin, R. Zinc and its importance for human health: An integrative review. J. Res. Med. Sci. Off. J. Isfahan Univ. Med. Sci. 2013, 18, 144. [Google Scholar]
- Prashanth, L.; Kattapagari, K.K.; Chitturi, R.T.; Baddam, V.R.R.; Prasad, L.K. A review on role of essential trace elements in health and disease. J. NTR Univ. Health Sci. 2015, 4, 75. [Google Scholar]
- Parveen, N.; Ansari, M.O.; Ahmad, M.F.; Jameel, S.; Shadab, G. Zinc: An element of extensive medical importance. Curr. Med. Res. Pract. 2017, 7, 90–98. [Google Scholar]
- Chasapis, C.T.; Ntoupa, P.-S.A.; Spiliopoulou, C.A.; Stefanidou, M.E. Recent aspects of the effects of zinc on human health. Arch. Toxicol. 2020, 94, 1443–1460. [Google Scholar] [CrossRef]
- Haas, J.D.; Brownlie, T., IV. Iron deficiency and reduced work capacity: A critical review of the research to determine a causal relationship. J. Nutr. 2001, 131, 676S–690S. [Google Scholar] [CrossRef] [Green Version]
- Lopez, A.; Cacoub, P.; Macdougall, I.C.; Peyrin-Biroulet, L. Iron deficiency anaemia. Lancet 2016, 387, 907–916. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Collaborators, G.A. The global burden of anemia. Hematol. Oncol. Clin. N. Am. 2016, 30, 247–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kassebaum, N.J.; Jasrasaria, R.; Naghavi, M.; Wulf, S.K.; Johns, N.; Lozano, R.; Regan, M.; Weatherall, D.; Chou, D.P.; Eisele, T.P. A systematic analysis of global anemia burden from 1990 to 2010. Blood J. Am. Soc. Hematol. 2014, 123, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Northrop-Clewes, C.A.; Thurnham, D.I. Biomarkers for the differentiation of anemia and their clinical usefulness. J. Blood Med. 2013, 4, 11. [Google Scholar]
- Maeda, M. Trace elements related to anemia. Biomed. Res. Trace Elem. 2005, 16, 19–24. [Google Scholar]
- Angelova, M.G.; Petkova-Marinova, T.V.; Pogorielov, M.V.; Loboda, A.N.; Nedkova-Kolarova, V.N.; Bozhinova, A.N. Trace element status (iron, zinc, copper, chromium, cobalt, and nickel) in iron-deficiency anaemia of children under 3 years. Anemia 2014, 2014, 718089. [Google Scholar] [CrossRef]
- Pan, C.-F.; Lin, C.-J.; Chen, S.-H.; Huang, C.-F.; Lee, C.-C. Association between trace element concentrations and anemia in patients with chronic kidney disease: A cross-sectional population-based study. J. Investig. Med. 2019, 67, 995–1001. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Yin, Z.; Lv, Y.; Luo, J.; Shi, W.; Fang, J.; Shi, X. Plasma element levels and risk of chronic kidney disease in elderly populations (≥90 Years old). Chemosphere 2020, 254, 126809. [Google Scholar] [CrossRef]
- Cappellini, M.; Musallam, K.; Taher, A. Iron deficiency anaemia revisited. J. Intern. Med. 2020, 287, 153–170. [Google Scholar] [CrossRef] [Green Version]
- Frater, J.L. The Top 100 Cited Papers in the Field of Iron Deficiency in Humans: A Bibliometric Study. BioMed Res. Int. 2021, 2021, 5573790. [Google Scholar] [CrossRef]
- Greffeuille, V.; Fortin, S.; Gibson, R.; Rohner, F.; Williams, A.; Young, M.F.; Houghton, L.; Ou, J.; Dijkhuizen, M.A.; Wirth, J.P. Associations between Zinc and Hemoglobin Concentrations in Preschool Children and Women of Reproductive Age: An Analysis of Representative Survey Data from the Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) Project. J. Nutr. 2021, 151, 1277–1285. [Google Scholar] [CrossRef]
- Nishiyama, S.; Kiwaki, K.; Miyazaki, Y.; Hasuda, T. Zinc and IGF-I concentrations in pregnant women with anemia before and after supplementation with iron and/or zinc. J. Am. Coll. Nutr. 1999, 18, 261–267. [Google Scholar] [CrossRef]
- Ma, A.G.; Chen, X.C.; Xu, R.X.; Zheng, M.C.; Wang, Y.; Li, J.-S. Comparison of serum levels of iron, zinc and copper in anaemic and non-anaemic pregnant women in China. Asia Pac. J. Clin. Nutr. 2004, 13, 348–352. [Google Scholar]
- Gibson, R.S.; Abebe, Y.; Stabler, S.; Allen, R.H.; Westcott, J.E.; Stoecker, B.J.; Krebs, N.F.; Hambidge, K.M. Zinc, gravida, infection, and iron, but not vitamin B-12 or folate status, predict hemoglobin during pregnancy in Southern Ethiopia. J. Nutr. 2008, 138, 581–586. [Google Scholar] [CrossRef] [Green Version]
- Bushra, M.; Elhassan, E.M.; Ali, N.I.; Osman, E.; Bakheit, K.H.; Adam, I.I. Anaemia, zinc and copper deficiencies among pregnant women in central Sudan. Biol. Trace Elem. Res. 2010, 137, 255–261. [Google Scholar] [CrossRef]
- Ugwuja, E.; Ejikeme, B.; Ugwu, N.; Obidoa, O. A comparative study of plasma trace elements (copper, iron and zinc) status in anaemic and non-anaemic pregnant women in Abakaliki, Nigeria. Online J. Health Allied Sci. 2011, 10, 10. [Google Scholar]
- Özhan, O.; Erdem, N.; Aydoğdu, İ.; Erkurt, A.; Kuku, İ. Serum zinc levels in iron deficient women: A case-control study. Turk. J. Hematol. 2016, 33, 156. [Google Scholar] [CrossRef] [PubMed]
- Rasool, S.O.; Zaman, B.A.; Abdulah, D.M. Serum zinc levels in iron deficiency anemia, non-iron deficiency anemia, and normal pregnant women and its correlation with iron status and hematological parameters. Med. J. Babylon 2020, 17, 103. [Google Scholar]
- Olayanju, A.; Oboh, I.; Imaralu, J.; Ezigbo, E.; Enitan, S. Iron and Zinc deficiency and haematological correlates among anaemic pregnant women attending ante-natal clinic at Babcock University Teaching Hospital, Ilishan-Remo, Ogun State. J. Med. Lab. Sci. 2020, 30, 47–57. [Google Scholar]
- Yokoi, K.; Sandstead, H.H.; Egger, N.G.; Alcock, N.W.; Ramanujam, V.S.; Dayal, H.H.; Penland, J.G. Association between zinc pool sizes and iron stores in premenopausal women without anaemia. Br. J. Nutr. 2007, 98, 1214–1223. [Google Scholar] [CrossRef]
- Ece, A.; Uyamik, B.S.; IŞcan, A.; Ertan, P.; Yiğitolu, M.R. Increased serum copper and decreased serum zinc levels in children with iron deficiency anemia. Biol. Trace Elem. Res. 1997, 59, 31–39. [Google Scholar] [CrossRef]
- Gürgöze, M.K.; Ölçücü, A.; Aygün, A.D.; Taşkin, E.; Kiliç, M. Serum and hair levels of zinc, selenium, iron, and copper in children with iron-deficiency anemia. Biol. Trace Elem. Res. 2006, 111, 23–29. [Google Scholar] [CrossRef]
- Kelkitli, E.; Ozturk, N.; Aslan, N.A.; Kilic-Baygutalp, N.; Bayraktutan, Z.; Kurt, N.; Bakan, N.; Bakan, E. Serum zinc levels in patients with iron deficiency anemia and its association with symptoms of iron deficiency anemia. Ann. Hematol. 2016, 95, 751–756. [Google Scholar] [CrossRef] [PubMed]
- Soliman, J.S.A.; Amer, A.Y. Association of zinc deficiency with iron deficiency anemia and its symptoms: Results from a case-control study. Cureus 2019, 11, e3811. [Google Scholar] [CrossRef] [Green Version]
- Cole, C.R.; Grant, F.K.; Swaby-Ellis, E.D.; Smith, J.L.; Jacques, A.; Northrop-Clewes, C.A.; Caldwell, K.L.; Pfeiffer, C.M.; Ziegler, T.R. Zinc and iron deficiency and their interrelations in low-income African American and Hispanic children in Atlanta. Am. J. Clin. Nutr. 2010, 91, 1027–1034. [Google Scholar] [CrossRef] [Green Version]
- Lim, K.H.; Riddell, L.J.; Nowson, C.A.; Booth, A.O.; Szymlek-Gay, E.A. Iron and zinc nutrition in the economically-developed world: A review. Nutrients 2013, 5, 3184–3211. [Google Scholar] [CrossRef] [PubMed]
- Hallberg, L.; Brune, M.; Rossander, L. Iron absorption in man: Ascorbic acid and dose-dependent inhibition by phytate. Am. J. Clin. Nutr. 1989, 49, 140–144. [Google Scholar] [CrossRef] [PubMed]
- Lonnerdal, B. Dietary factors influencing zinc absorption. J. Nutr. 2000, 130, 1378S–1383S. [Google Scholar] [CrossRef] [Green Version]
- Sandstead, H.H.; Smith, J.C., Jr. Deliberations and evaluations of approaches, endpoints and paradigms for determining zinc dietary recommendations. J. Nutr. 1996, 126 (Suppl. S9), 2410S–2418S. [Google Scholar] [CrossRef] [Green Version]
- Graham, R.D.; Knez, M.; Welch, R.M. How much nutritional iron deficiency in humans globally is due to an underlying zinc deficiency? Adv. Agron. 2012, 115, 1–40. [Google Scholar]
- Houghton, L.A.; Parnell, W.R.; Thomson, C.D.; Green, T.J.; Gibson, R.S. Serum zinc is a major predictor of anemia and mediates the effect of selenium on hemoglobin in school-aged children in a nationally representative survey in New Zealand. J. Nutr. 2016, 146, 1670–1676. [Google Scholar] [CrossRef] [PubMed]
- Wieringa, F.T.; Dahl, M.; Chamnan, C.; Poirot, E.; Kuong, K.; Sophonneary, P.; Sinuon, M.; Greuffeille, V.; Hong, R.; Berger, J. The high prevalence of anemia in Cambodian children and women cannot be satisfactorily explained by nutritional deficiencies or hemoglobin disorders. Nutrients 2016, 8, 348. [Google Scholar] [CrossRef] [PubMed]
- Zivot, A.; Lipton, J.M.; Narla, A.; Blanc, L. Erythropoiesis: Insights into pathophysiology and treatments in 2017. Mol. Med. 2018, 24, 11. [Google Scholar] [CrossRef] [Green Version]
- Broxmeyer, H.E. Erythropoietin: Multiple targets, actions, and modifying influences for biological and clinical consideration. J. Exp. Med. 2013, 210, 205–208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bunn, H.F. Erythropoietin. Cold Spring Harb. Perspect. Med. 2013, 3, a011619. [Google Scholar] [CrossRef] [Green Version]
- Jelkmann, W. Physiology and pharmacology of erythropoietin. Transfus. Med. Hemother. 2013, 40, 302–309. [Google Scholar] [CrossRef] [Green Version]
- Huber, K.L.; Cousins, R.J. Zinc metabolism and metallothionein expression in bone marrow during erythropoiesis. Am. J. Physiol.-Endocrinol. Metab. 1993, 264, E770–E775. [Google Scholar] [CrossRef]
- Morgan, P.N.; Wehr, C.M.; MacGregor, J.T.; Woodhouse, L.R.; King, J.C. Zinc deficiency, erythrocyte production, and chromosomal damage in pregnant rats and their fetuses. J. Nutr. Biochem. 1995, 6, 263–268. [Google Scholar] [CrossRef]
- King, L.E.; Fraker, P.J. Zinc deficiency in mice alters myelopoiesis and hematopoiesis. J. Nutr. 2002, 132, 3301–3307. [Google Scholar] [CrossRef] [Green Version]
- King, L.E.; Frentzel, J.W.; Mann, J.J.; Fraker, P.J. Chronic zinc deficiency in mice disrupted T cell lymphopoiesis and erythropoiesis while B cell lymphopoiesis and myelopoiesis were maintained. J. Am. Coll. Nutr. 2005, 24, 494–502. [Google Scholar] [CrossRef]
- Konomi, A.; Yokoi, K. Zinc deficiency decreases plasma erythropoietin concentration in rats. Biol. Trace Elem. Res. 2005, 107, 289–292. [Google Scholar] [CrossRef]
- Chen, Y.H.; Feng, H.L.; Jeng, S.S. Zinc supplementation stimulates red blood cell formation in rats. Int. J. Mol. Sci. 2018, 19, 2824. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feng, H.L.; Chen, Y.H.; Jeng, S.S. Effect of zinc supplementation on renal anemia in 5/6-nephrectomized rats and a comparison with treatment with recombinant human erythropoietin. Int. J. Mol. Sci. 2019, 20, 4985. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.H.; Jeng, S.S.; Hsu, Y.C.; Liao, Y.M.; Wang, Y.X.; Cao, X.; Huang, L.-J. In anemia zinc is recruited from bone and plasma to produce new red blood cells. J. Inorg. Biochem. 2020, 210, 111172. [Google Scholar] [CrossRef]
- Paterson, P.G.; Bettger, W.J. Effect of dietary zinc intake on the hematological profile of the rat. Comp. Biochem. Physiol. A 1986, 83, 721–725. [Google Scholar] [CrossRef]
- Someya, Y.; Tanihata, J.; Sato, S.; Kawano, F.; Shirato, K.; Sugiyama, M.; Kawashima, Y.; Nomura, S.; Tachiyashiki, K.; Imaizumi, K. Zinc-deficiency induced changes in the distribution of rat white blood cells. J. Nutr. Sci. Vitaminol. 2009, 55, 162–169. [Google Scholar] [CrossRef] [Green Version]
- Chaparro, C.M.; Suchdev, P.S. Anemia epidemiology, pathophysiology, and etiology in low-and middle-income countries. Ann. N. Y. Acad. Sci. 2019, 1450, 15–31. [Google Scholar] [CrossRef] [Green Version]
- Trumbo, P.; Yates, A.A.; Schlicker, S.; Poos, M. Dietary reference intakes: Vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. J. Am. Diet. Assoc. 2001, 101, 294–301. [Google Scholar] [CrossRef]
- Hoffman, H.N., II; Phyliky, R.L.; Fleming, C.R. Zinc-induced copper deficiency. Gastroenterology 1988, 94, 508–512. [Google Scholar] [CrossRef]
- Broun, E.R.; Greist, A.; Tricot, G.; Hoffman, R. Excessive zinc ingestion: A reversible cause of sideroblastic anemia and bone marrow depression. Jama 1990, 264, 1441–1443. [Google Scholar] [CrossRef]
- Gyorffy, E.J.; Chan, H. Copper Deficiency and Microcytic Anemia Resulting from Prolonged Ingestion of Over-the-Counter Zinc. Am. J. Gastroenterol. 1992, 87, 1054–1055. [Google Scholar]
- Fiske, D.N.; McCoy, H.E., III; Kitchens, C.S. Zinc-induced sideroblastic anemia: Report of a case, review of the literature, and description of the hematologic syndrome. Am. J. Hematol. 1994, 46, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Porea, T.J.; Belmont, J.W.; Mahoney, D.H., Jr. Zinc-induced anemia and neutropenia in an adolescent. J. Pediatr. 2000, 136, 688–690. [Google Scholar] [CrossRef]
- Willis, M.S.; Monaghan, S.A.; Miller, M.L.; McKenna, R.W.; Perkins, W.D.; Levinson, B.S.; Bhushan, V.; Kroft, S.H. Zinc-induced copper deficiency: A report of three cases initially recognized on bone marrow examination. Am. J. Clin. Pathol. 2005, 123, 125–131. [Google Scholar] [CrossRef]
- Duncan, A.; Yacoubian, C.; Watson, N.; Morrison, I. The risk of copper deficiency in patients prescribed zinc supplements. J. Clin. Pathol. 2015, 68, 723–725. [Google Scholar] [CrossRef] [PubMed]
- Wahab, A.; Mushtaq, K.; Borak, S.G.; Bellam, N. Zinc-induced copper deficiency, sideroblastic anemia, and neutropenia: A perplexing facet of zinc excess. Clin. Case Rep. 2020, 8, 1666–1671. [Google Scholar] [CrossRef]
- Tatineni, V.; An, J.Y.; Leffew, M.R.; Mahesh, S.A. Anemia from A to zinc: Hypocupremia in the setting of gastric bypass and zinc excess. Clin. Case Rep. 2020, 8, 745–750. [Google Scholar] [CrossRef] [Green Version]
- Munie, S.; Pintavorn, P. Erythropoietin-Resistant Anemia Secondary to Zinc-Induced Hypocupremia in a Hemodialysis Patient. Case Rep. Nephrol. Dial. 2021, 11, 167–175. [Google Scholar] [CrossRef]
- Wahab, A.; Mushtaq, K.; Khan, A.; Khakwani, M.S.K.; Masood, A.; Henderson, J.; Malik, F. Zinc-induced hypocupremia and pancytopenia, from zinc supplementation to its toxicity, a case report. J. Community Hosp. Intern. Med. Perspect. 2021, 11, 843–846. [Google Scholar] [CrossRef]
- Cai, S.; Gong, J.-Y.; Yang, J.; Wang, J.-S. Anemia following zinc treatment for Wilson’s disease: A case report and literature review. BMC Gastroenterol. 2019, 19, 1–6. [Google Scholar] [CrossRef]
- Nations, S.; Boyer, P.; Love, L.; Burritt, M.; Butz, J.; Wolfe, G.; Hynan, L.; Reisch, J.; Trivedi, J. Denture cream: An unusual source of excess zinc, leading to hypocupremia and neurologic disease. Neurology 2008, 71, 639–643. [Google Scholar] [CrossRef]
- Doherty, K.; Connor, M.; Cruickshank, R. Zinc-containing denture adhesive: A potential source of excess zinc resulting in copper deficiency myelopathy. Br. Dent. J. 2011, 210, 523–525. [Google Scholar] [CrossRef] [PubMed]
- Cathcart, S.J.; Sofronescu, A.G. Clinically distinct presentations of copper deficiency myeloneuropathy and cytopenias in a patient using excessive zinc-containing denture adhesive. Clin. Biochem. 2017, 50, 733–736. [Google Scholar] [CrossRef] [PubMed]
- Dolcourt, B.A.; Paxton, J.H.; Bora, K.M.; Aaron, C.K. Pennies for your thoughts: A case series of pancytopenia due to zinc-induced copper deficiency in the same patient. Clin. Pract. Cases Emerg. Med. 2019, 3, 341. [Google Scholar] [CrossRef] [PubMed]
- Agnew, U.M.; Slesinger, T.L. Zinc Toxicity; Stat Pearls Publishing: Treasure Island, FL, USA, 2020; PMID32119435. [Google Scholar]
- Hill, C.H.; Matrone, G. Chemical parameters in the study of in vivo and in vitro interactions of transition elements. Fed. Proc. 1970, 29, 1474–1481. [Google Scholar]
- Ogiso, T.; Moriyama, K.; Sasaki, S.; Ishimura, Y.; Minato, A. Inhibitory effect of high dietary zinc on copper absorption in rats. Chem. Pharm. Bull. 1974, 22, 55–60. [Google Scholar] [CrossRef] [Green Version]
- 88. Fischer, P.W.; Giroux, A.; L’Abbe, M.R. Effects of zinc on mucosal copper binding and on the kinetics of copper absorption. J. Nutr. 1983, 113, 462–469. [Google Scholar] [CrossRef]
- Oestreicher, P.; Cousins, R.J. Copper and zinc absorption in the rat: Mechanism of mutual antagonism. J. Nutr. 1985, 115, 159–166. [Google Scholar] [CrossRef]
- Bremner, I.; Beattie, J.H. Copper and Zinc Metabolism in Health and Disease: Speciation and Interactions. Proc. Nutr. Soc. 1995, 54, 489–499. [Google Scholar] [CrossRef] [Green Version]
- Reeves, P.G.; Rossow, K.L.; Bobilya, D.J. Zinc-induced metallothionein and copper metabolism in intestinal mucosa, liver, and kidney of rats. Nutr. Res. 1993, 13, 1419–1431. [Google Scholar] [CrossRef]
- Wapnir, R.A.; Balkman, C. Inhibition of copper absorption by zinc. Biol. Trace Elem. Res. 1991, 29, 193–202. [Google Scholar] [CrossRef]
- Reeves, P.G.; Rossow, K.L. Zinc-and/or cadmium-induced intestinal metallothionein and copper metabolism in adult rats. J. Nutr. Biochem. 1996, 7, 128–134. [Google Scholar] [CrossRef]
- Hachisuka, E.; Kido, T.; Suka, M.; Yanagisawa, H. Ingestion of Excess Zinc Augments the Osmotic Fragility of Red Blood Cells via An Increase in Oxidative Stress. Biomed. Res. Trace Elem. 2021, 31, 117–125. [Google Scholar]
- Yanagisawa, H.; Miyakoshi, Y.; Kobayashi, K.; Sakae, K.; Kawasaki, I.; Suzuki, Y.; Tamura, J.i. Long-term intake of a high zinc diet causes iron deficiency anemia accompanied by reticulocytosis and extra-medullary erythropoiesis. Toxicol. Lett. 2009, 191, 15–19. [Google Scholar] [CrossRef]
- Peled, T.; Landau, E.; Prus, E.; Treves, A.J.; Fibach, E. Cellular copper content modulates differentiation and self-renewal in cultures of cord blood-derived CD34+ cells. Br. J. Haematol. 2002, 116, 655–661. [Google Scholar] [CrossRef] [Green Version]
- Myint, Z.W.; Oo, T.H.; Thein, K.Z.; Tun, A.M.; Saeed, H. Copper deficiency anemia. Ann. Hematol. 2018, 97, 1527–1534. [Google Scholar] [CrossRef]
- Prohaska, J.R. Impact of copper limitation on expression and function of multicopper oxidases (ferroxidases). Adv. Nutr. 2011, 2, 89–95. [Google Scholar] [CrossRef] [Green Version]
- Helman, S.L.; Zhou, J.; Fuqua, B.K.; Lu, Y.; Collins, J.F.; Chen, H.; Vulpe, C.D.; Anderson, G.J.; Frazer, D.M. The biology of mammalian multi-copper ferroxidases. Biometals 2022. [Google Scholar] [CrossRef] [PubMed]
- Halfdanarson, T.R.; Kumar, N.; Li, C.Y.; Phyliky, R.L.; Hogan, W.J. Hematological manifestations of copper deficiency: A retrospective review. Eur. J. Haematol. 2008, 80, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Weiss, G.; Goodnough, L.T. Anemia of chronic disease. N. Engl. J. Med. 2005, 352, 1011–1023. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dvornik, Š.; Ćuk, M.; Rački, S.; Zaputović, L. Serum zinc concentrations in the maintenance hemodialysis patients. Coll. Antropol. 2006, 30, 125–129. [Google Scholar] [PubMed]
- Lee, S.H.; Huang, J.W.; Hung, K.Y.; Leu, L.J.; Kan, Y.T.; Yang, C.S.; Huang, C.L.; Chen, P.Y.; Chen, J.S.; Chen, W.Y. Trace Metals’ abnormalities in hemodialysis patients: Relationship with medications. Artif. Organs 2000, 24, 841–844. [Google Scholar] [CrossRef]
- Vikbladh, I. Studies on zinc in blood. Scand. J. Clin. Lab. Investig. 1950, 2, 143–148. [Google Scholar] [CrossRef]
- Condon, C.J.; Freeman, R.M. Zinc metabolism in renal failure. Ann. Intern. Med. 1970, 73, 531–536. [Google Scholar] [CrossRef]
- Mahajan, S.; Gardiner, W.; Abbasi, A.; Briggs, W.; Prasad, A.; McDonald, F. Abnormal plasma and erythrocyte zinc distribution in uremia. ASAIO J. 1978, 24, 50–54. [Google Scholar]
- Mahajan, S.; Prasad, A.; Rabbani, P.; Briggs, W.; McDonald, F. Zinc metabolism in uremia. J. Lab. Clin. Med. 1979, 94, 693–698. [Google Scholar] [CrossRef]
- Beerbower, K.S.; Raess, B.U. Erythrocyte, plasma, urine and dialysate zinc levels in patients on continuous ambulatory peritoneal dialysis. Am. J. Clin. Nutr. 1985, 41, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Lin, T.; Chen, J.; Liaw, J.; Juang, J. Trace elements and lipid peroxidation in uremic patients on hemodialysis. Biol. Trace Elem. Res. 1996, 51, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Mafra, D.; Cuppari, L.; Fávaro, D.I.; Cozzolino, S.M. Zinc levels after iron supplementation in patients with chronic kidney disease. J. Ren. Nutr. 2004, 14, 164–169. [Google Scholar] [CrossRef]
- Batista, M.N.; Cuppari, L.; Pedrosa, L.d.F.C.; Almeida, M.d.G.; De Almeida, J.B.; de Medeiros, A.C.Q.; Canziani, M.E.F. Effect of end-stage renal disease and diabetes on zinc and copper status. Biol. Trace Elem. Res. 2006, 112, 1–12. [Google Scholar] [CrossRef]
- Mahajan, S.K. Zinc in kidney disease. J. Am. Coll. Nutr. 1989, 8, 296–304. [Google Scholar] [CrossRef]
- Kimmel, P.L. Zinc and chronic renal disease. In Seminars in Dialysis; 1989; Volume 2, pp. 253–259. [Google Scholar]
- Tonelli, M.; Wiebe, N.; Hemmelgarn, B.; Klarenbach, S.; Field, C.; Manns, B.; Thadhani, R.; Gill, J. Trace elements in hemodialysis patients: A systematic review and meta-analysis. BMC Med. 2009, 7, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neto, L.; Bacci, M.; Sverzutt, L.; Costa, M.; Alves, B.; Fonseca, F. The role of zinc in chronic kidney disease patients on hemodialysis: A systematic review. Health 2016, 8, 344. [Google Scholar] [CrossRef] [Green Version]
- Lowe, N.M.; Fekete, K.; Decsi, T. Methods of assessment of zinc status in humans: A systematic review. Am. J. Clin. Nutr. 2009, 89, 2040S–2051S. [Google Scholar] [CrossRef] [Green Version]
- King, J.C.; Brown, K.H.; Gibson, R.S.; Krebs, N.F.; Lowe, N.M.; Siekmann, J.H.; Raiten, D.J. Biomarkers of Nutrition for Development (BOND)—Zinc review. J. Nutr. 2015, 146, 858S–885S. [Google Scholar] [CrossRef] [PubMed]
- Piechota, W.; Dobrucki, T.; Symonowicz, N.; Wadowska, E.; Murkowska, E. Zinc in patients with chronic renal failure. Int. Urol. Nephrol. 1983, 15, 377–382. [Google Scholar] [CrossRef]
- Nasima, A.; Raghib, A.; Abdul, W.; Mostafa, C.; Sakhi, C.; Hai, M. Relationship between zinc and anaemia in chronic haemodialysis patients. J. Teach. Assoc. RMC 2003, 16, 1019–8555. [Google Scholar]
- Goriki, K. The relationship between carbonic anhydrases and zinc concentration of erythrocytes in patients under chronic hemodialysis. Hiroshima J. Med. Sci. 1982, 31, 123–127. [Google Scholar]
- Mafra, D.; Cozzolino, S.M. Erythrocyte zinc and carbonic anhydrase levels in nondialyzed chronic kidney disease patients. Clin. Biochem. 2004, 37, 67–71. [Google Scholar] [CrossRef]
- Mafra, D.; Cuppari, L.; Cozzolino, S.M. Iron and zinc status of patients with chronic renal failure who are not on dialysis. J. Ren. Nutr. 2002, 12, 38–41. [Google Scholar] [CrossRef]
- Mahajan, S.K. Zinc metabolism in uremia. Int. J. Artif. Organs 1988, 11, 223–228. [Google Scholar] [CrossRef]
- Anagnostou, A.; Vercellotti, G.; Barone, J.; Fried, W. Factors which affect erythropoiesis in partially nephrectomized and sham-operated rats. Blood 1976, 48, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Mason, C.; Thomas, T. A model for erythropoiesis in experimental chronic renal failure. Br. J. Haematol. 1984, 58, 729–740. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.C.; Zuo, Y.; Fogo, A.B. Models of chronic kidney disease. Drug Discov. Today Dis. Model. 2010, 7, 13–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flanagan, J.P.; Lessler, M.A. Controlled phenylhydrazine-induced reticulocytosis in the rat. Ohio J. Sci. 1970, 75, 300. [Google Scholar]
- Berger, J. Phenylhydrazine haematotoxicity. J. Appl. Biomed. 2007, 5, 125–130. [Google Scholar] [CrossRef] [Green Version]
- Giugliano, R.; Millward, D. Growth and zinc homeostasis in the severely Zn-deficient rat. Br. J. Nutr. 1984, 52, 545–560. [Google Scholar] [CrossRef] [Green Version]
- Harland, B.; Fox, M.S.; Fry, B.E., Jr. Protection against zinc deficiency by prior excess dietary zinc in young Japanese quail. J. Nutr. 1975, 105, 1509–1518. [Google Scholar] [CrossRef]
- Brown, E.D.; Chan, W.; Smith, J.C., Jr. Bone Mineralization During a Developing Zinc Deficiency. Proc. Soc. Exp. Biol. Med. 1978, 157, 211–214. [Google Scholar] [CrossRef]
- Zhou, J.R.; Canar, M.M.; Erdman, J.W., Jr. Bone zinc is poorly released in young, growing rats fed marginally zinc-restricted diet. J. Nutr. 1993, 123, 1383–1388. [Google Scholar] [PubMed]
- King, J.C. Assessment of zinc status. J. Nutr. 1990, 120 (Suppl. S11), 1474–1479. [Google Scholar] [CrossRef]
- Kolsteren, P.; Rahman, S.; Hilberbrand, K.; Dintz, A. Treatment for iron deficiency anaemia with a combined supplementation of iron, vitamin A and zinc in women of Dinajpur, Bangladesh. Eur. J. Clin. Nutr. 1999, 53, 102–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alarcon, K.; Kolsteren, P.W.; Prada, A.M.; Chian, A.M.; Velarde, R.E.; Pecho, I.L.; Hoeree, T.F. Effects of separate delivery of zinc or zinc and vitamin A on hemoglobin response, growth, and diarrhea in young Peruvian children receiving iron therapy for anemia. Am. J. Clin. Nutr. 2004, 80, 1276–1282. [Google Scholar] [CrossRef] [Green Version]
- Mahmoudian, A.; Khademlou, M. The effect of simultaneous administration of zinc sulfate and ferrous sulfate in the treatment of anemic pregnant women. J. Res. Med. Sci. 2005, 10, 205–209. [Google Scholar]
- Walker, C.F.; Kordas, K.; Stoltzfus, R.J.; Black, R.E. Interactive effects of iron and zinc on biochemical and functional outcomes in supplementation trials–. Am. J. Clin. Nutr. 2005, 82, 5–12. [Google Scholar] [CrossRef]
- Berger, J.; Ninh, N.; Khan, N.; Nhien, N.; Lien, D.; Trung, N.; Khoi, H. Efficacy of combined iron and zinc supplementation on micronutrient status and growth in Vietnamese infants. Eur. J. Clin. Nutr. 2006, 60, 443–454. [Google Scholar] [CrossRef] [Green Version]
- Yalda, M.A.; Ibrahiem, A.A. The effect of combined supplementation of iron and zinc versus iron alone on anemic pregnant patients in Dohuk. Jordan Med. J. 2010, 44, 9–16. [Google Scholar]
- Chen, L.; Liu, Y.F.; Gong, M.; Jiang, W.; Fan, Z.; Qu, P.; Chen, J.; Liu, Y.X.; Li, T.Y. Effects of vitamin A, vitamin A plus zinc, and multiple micronutrients on anemia in preschool children in Chongqing, China. Asia Pac. J. Clin. Nutr. 2012, 21, 3–11. [Google Scholar] [PubMed]
- Mujica-Coopman, M.F.; Borja, A.; Pizarro, F.; Olivares, M. Effect of daily supplementation with iron and zinc on iron status of childbearing age women. Biol. Trace Elem. Res. 2015, 165, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Nakatani, S.; Mori, K.; Shoji, T.; Emoto, M. Association of Zinc Deficiency with Development of CVD Events in Patients with CKD. Nutrients 2021, 13, 1680. [Google Scholar] [CrossRef] [PubMed]
- Garagarza, C.; Valente, A.; Caetano, C.; Ramos, I.; Sebastião, J.; Pinto, M.; Oliveira, T.; Ferreira, A.; Guerreiro, C.S. Zinc Deficient Intake in Hemodialysis Patients: A Path to a High Mortality Risk. J. Ren. Nutr. 2022, 32, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Mafra, D. Can Outcomes be Improved in Dialysis Patients by Optimizing Trace Mineral, Micronutrient, and Antioxidant Status?: The Role of Trace Elements. Semin. Dial. 2015, 29, 48–50. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.J.; Wang, M.Q.; Hu, R.; Yang, Y.; Huang, Y.S.; Xian, S.X.; Lu, L. Effect of zinc supplementation on maintenance hemodialysis patients: A systematic review and meta-analysis of 15 randomized controlled trials. BioMed Res. Int. 2017, 1024769. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.-J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J. KDOQI clinical practice guideline for nutrition in CKD: 2020 up-date. Am. J. Kidney Dis. 2020, 76, S1–S107. [Google Scholar] [CrossRef]
- Fukushima, T.; Horike, H.; Fujiki, S.; Kitada, S.; Sasaki, T.; Kashihara, N. Zinc deficiency anemia and effects of zinc therapy in maintenance hemodialysis patients. Ther. Apher. Dial. 2009, 13, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.; Abe, M.; Okada, K.; Tei, R.; Maruyama, N.; Kikuchi, F.; Higuchi, T.; Soma, M. Oral zinc supplementation reduces the erythropoietin responsiveness index in patients on hemodialysis. Nutrients 2015, 7, 3783–3795. [Google Scholar] [CrossRef] [PubMed]
| References |
| (1) In most cases, zinc deficiency coexists with iron-deficiency anemia | |
| [33,34,35,36,37,38,39,40] |
| [26,41,42] |
| [43,44] |
| [10,45,46] |
| (2). To a lesser extent, zinc deficiency may cooperate with other factors to lead to anemia | [31,45,51,52] |
| (3). No reports in humans recognize zinc as a primary factor | [31,45,51] |
| |
| (1). Zinc is essential for erythropoiesis | [57,58,59,60,61,62,63,64] |
| (2). In rats, iron deficiency or iron+zinc deficiency results in anemia, but not zinc deficiency alone | [61,65,66] |
|
| References |
| a. Excess and prolonged intake of oral zinc supplement | [69,70,71,72,73,74,75,76,77,78,79] |
| b. High-dose one-time zinc administration (for Wilson’s disease) | [80] |
| c. Use of denture cream (containing a high zinc concentration of 17,000–34,000 (µg/g) | [81,82,83] |
| d. Ingestion of coins (by individual with mental disease) | [70,84] |
| |
| (High zinc induces metallothionein, zinc and copper compete to bind metallothionein, and copper is preferentially bound by metallothionein) | [14,72,85,86,87,88,89,90] |
| (another suggested mechanism is that high zinc in the intestinal lumen directly interfered with the transport of copper across the mucosal cells) | [91,92,93] |
| |
| (Copper is essential for normal hematopoiesis) | [74,96,97] |
| ||||
| Controls | CKD patients | p value | Reference |
| (µg/mL plasma) | a. 1.07 ± 4 (n = 11) | 0.82 ± 0.04 (n = 10) | <0.01 | [105] |
| b. 1.016 ± 0.022(n = 50) | 0.80 ± 0.03 (n = 10) | <0.001 | [106] | |
| c. 1.14 ± 0.11 (n = 25) | 0.95 ± 0.10 (n = 26) | <0.001 | [109] | |
| d. 1.105 ± 0.175(n= 152) | 0.705 ± 0.128 (n = 456) | <0.0001 | [103] | |
| e. 0.93 ± 0.12 (n = 20) | 0.81 ± 0.19 (n = 30) | <0.05 | [110] | |
| f. 0.98 ± 0.15 (n = 11) | 0.49 ± 0.18 (n = 127) | <0.0001 | [64] | |
| -----Lower plasma zinc levels in CKD patients----- | ||||
| ||||
| (µg/g Hb) | a. 44.1 ± 1.1 (n = 50) | 55.0 ± 2.0 (n = 10) | <0.001 | [106] |
| b. 41.8 ± 63.0 (n = 20) | 51.3 ± 10.3 (n = 30) | <0.05 | [110] | |
| (µmoles/L) | c. 148 ± 13 (n = 10) | 198 ± 8 (n = 10) | <0.05 | [108] |
| (mg/L) | d. 12.1 ± 1.2 (n = 25) | 13.4 ± 3.1 (n = 26) | <0.001 | [109] |
| (µg/109 RBC) | e. 0.63 ± 0.06 (n = 21) | 0.72 ± 0.18 (n = 127) | <0.05 | [64] |
| -----Higher erythrocyte zinc levels in CKD patients----- | ||||
| ||||
| (1) Plasma zinc levels (µg/mL plasma) | Controls | Anemic rats | p value | Reference |
| a. 5/6 nephrectomized anemic rats | ||||
| 1.90 ± 0.3 (n = 6) | 1.40 ± 0.2 (n = 6) | <0.05 | [64] | |
| b. Phenylhydrazine induced anemic rats | ||||
| 1.45 ± 0.06 (n = 6) | 1.29 ± 0.03(n = 6) | <0.001 | [64] | |
| -----Lower plasma zinc levels in anemic rats----- | ||||
| (2) Erythrocyte zinc levels (µg/109 RBC) | ||||
| a. 5/6 nephrectomized anemic rats | ||||
| 0.50 ± 0.08 (n = 6) | 0.90 ± 0.01 (n = 6) | <0.001 | [64] | |
| b. Phenylhydrazine induced anemic rats | ||||
| 0.70 ± 0.21 (n = 6) | 0.86 ± 0.10 (n = 6) | <0.01 | [64] | |
| -----Higher erythrocyte zinc levels in anemic rats----- | ||||
| ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeng, S.-S.; Chen, Y.-H. Association of Zinc with Anemia. Nutrients 2022, 14, 4918. https://doi.org/10.3390/nu14224918
Jeng S-S, Chen Y-H. Association of Zinc with Anemia. Nutrients. 2022; 14(22):4918. https://doi.org/10.3390/nu14224918
Chicago/Turabian StyleJeng, Sen-Shyong, and Yen-Hua Chen. 2022. "Association of Zinc with Anemia" Nutrients 14, no. 22: 4918. https://doi.org/10.3390/nu14224918
APA StyleJeng, S.-S., & Chen, Y.-H. (2022). Association of Zinc with Anemia. Nutrients, 14(22), 4918. https://doi.org/10.3390/nu14224918






