Association between Quality of Maternal Prenatal Food Source and Preparation and Breastfeeding Duration in the Environmental Influences on Child Health Outcome (ECHO) Program
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
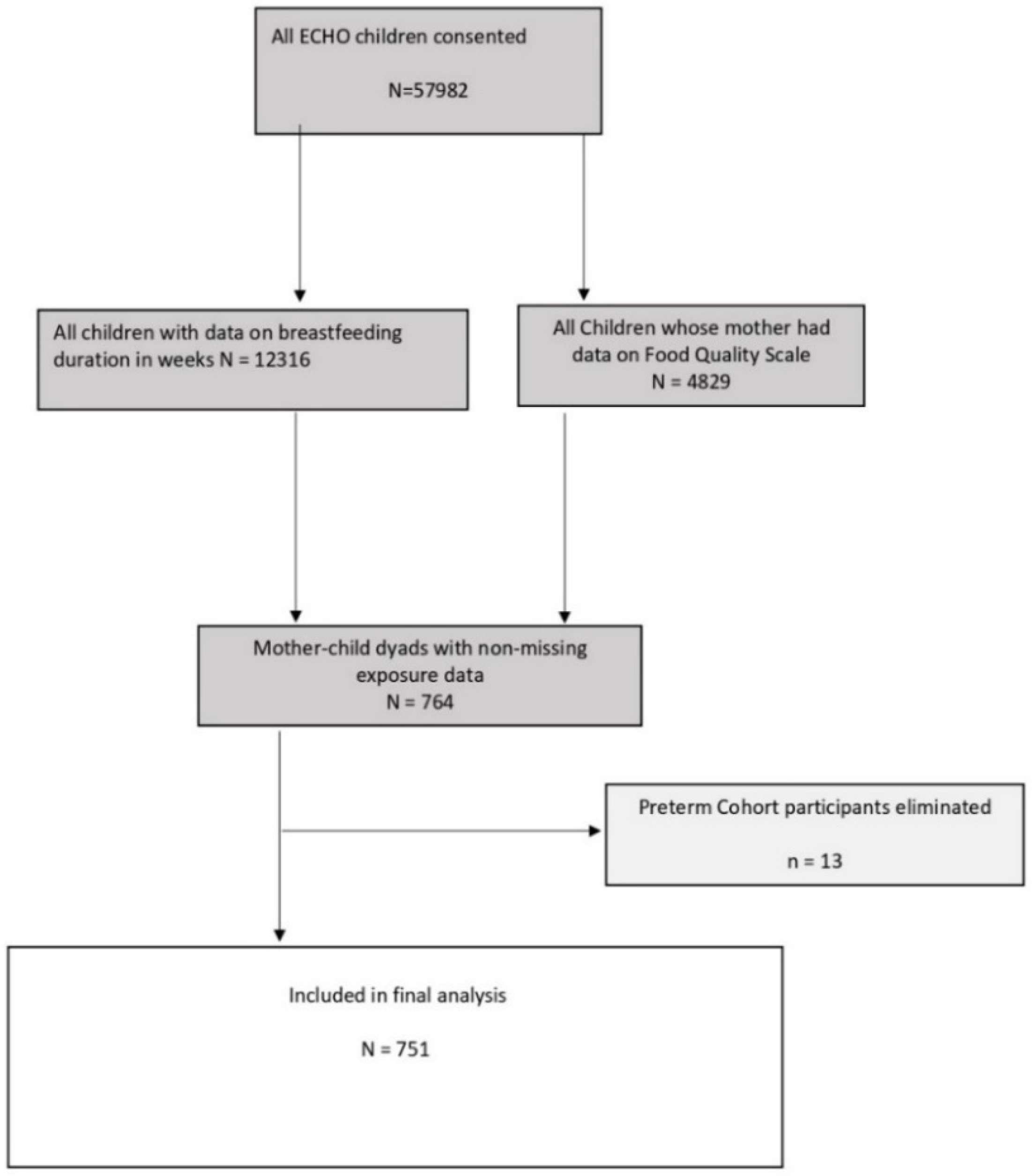
2.2. Sample
2.3. Measures
2.3.1. Breastfeeding Duration
2.3.2. Maternal Food Source Quality
2.3.3. Participant Characteristics
2.4. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Binns, C.; Lee, M.; Low, W.Y. The long-term public health benefits of breastfeeding. Asia Pac. J. Public Health 2016, 28, 7–14. [Google Scholar] [CrossRef] [Green Version]
- Bartick, M.C.; Jegier, B.J.; Green, B.D.; Schwarz, E.B.; Reinhold, A.G.; Stuebe, A.M. Disparities in breastfeeding: Impact on maternal and child health outcomes and costs. J. Pediatr. 2017, 181, 49–55.e46. [Google Scholar] [CrossRef]
- González, J.; Fernández, M. Exclusive breastfeeding reduces asthma in a group of children from the Caguas municipality of Puerto Rico. Bol. Asoc. Med. Puerto Rico 2010, 102, 10–12. [Google Scholar]
- Anderson, A.K.; Damio, G.; Himmelgreen, D.A.; Peng, Y.-K.; Segura-Pérez, S.; Pérez-Escamilla, R. Social capital, acculturation, and breastfeeding initiation among Puerto Rican women in the United States. J. Hum. Lact. 2004, 20, 39–45. [Google Scholar] [CrossRef] [PubMed]
- García-Fragoso, L.; Medina, M.; Ortiz, N. Factors associated to continuing breastfeeding after returning to work in a group of mothers in Puerto Rico. Bol. De La Asoc. Med. De Puerto Rico 2012, 104, 12–15. [Google Scholar]
- Rivera-Alvarado, I.; Vázquez-García, V.; Dávila-Torres, R.R.; Parrilla-Rodríguez, A.M. Exploratory study: Breastfeeding knowledge, attitudes towards sexuality and breastfeeding, and disposition towards supporting breastfeeding in future Puerto Rican male parents. P. R. Health Sci. J. 2006, 25, 337–341. [Google Scholar]
- Gregory, J.E.; Paxton, S.J.; Brozovic, A.M. Maternal feeding practices, child eating behaviour and body mass index in preschool-aged children: A prospective analysis. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 55. [Google Scholar] [CrossRef] [Green Version]
- Rodgers, R.F.; Paxton, S.J.; Massey, R.; Campbell, K.J.; Wertheim, E.H.; Skouteris, H.; Gibbons, K. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: A prospective study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 24. [Google Scholar] [CrossRef] [Green Version]
- Ventura, A.K.; Burch, L.L. Does parenting affect children’s eating and weight status? Int. J. Behav. Nutr. Phys. Act. 2008, 5, 15. [Google Scholar] [CrossRef] [Green Version]
- WHO. Ten Steps to Successful Breastfeeding; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Beckerman, J.P.; Slade, E.; Ventura, A.K. Maternal diet during lactation and breast-feeding practices have synergistic association with child diet at 6 years. Public Health Nutr. 2020, 23, 286–294. [Google Scholar] [CrossRef]
- Keikha, M.; Bahreynian, M.; Saleki, M.; Kelishadi, R. Macro-and micronutrients of human milk composition: Are they related to maternal diet? A comprehensive systematic review. Breastfeed. Med. 2017, 12, 517–527. [Google Scholar] [CrossRef] [PubMed]
- Danielewicz, H.; Myszczyszyn, G.; Debinska, A.; Myszkal, A.; Boznanski, A.; Hirnle, L. Diet in pregnancy-more than food. Eur. J. Pediatr. 2017, 176, 1573–1579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gorman, K.S.; McCurdy, K.; Kisler, T.; Metallinos-Katsaras, E. Maternal Strategies to Access Food Differ by Food Security Status. J. Acad. Nutr. Diet. 2017, 117, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Gross, R.S.; Mendelsohn, A.L.; Arana, M.M.; Messito, M.J. Food insecurity during pregnancy and breastfeeding by low-income Hispanic mothers. Pediatrics 2019, 143, 6. [Google Scholar] [CrossRef]
- Dritsakou, K.; Massara, P.; Skourlis, N.; Liosis, G.; Skouroliakou, M. Maternal diet and breastfeeding duration of infants after NICU hospitalization in Greece: A cohort study. J. Matern.-Fetal Neonatal Med. 2017, 30, 2398–2403. [Google Scholar] [CrossRef] [PubMed]
- Gillman, M.W.; Blaisdell, C.J. Environmental influences on Child Health Outcomes, a Research Program of the National Institutes of Health. Curr. Opin. Pediatr. 2018, 30, 260–262. [Google Scholar] [CrossRef]
- Blaisdell, C.J.; Park, C.; Hanspal, M.; Roary, M.; Arteaga, S.S.; Laessig, S.; Luetkemeier, E.; Gillman, M.W. The NIH ECHO Program: Investigating how early environmental influences affect child health. Pediatr. Res. 2021, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Forrest, C.B.; Blackwell, C.K.; Camargo, C.A., Jr. Advancing the Science of Children’s Positive Health in the National Institutes of Health Environmental Influences on Child Health Outcomes (ECHO) Research Program. J. Pediatr. 2018, 196, 298–300. [Google Scholar] [CrossRef] [Green Version]
- Dennis, C.-L.; McQueen, K. The relationship between infant-feeding outcomes and postpartum depression: A qualitative systematic review. Pediatrics 2009, 123, e736–e751. [Google Scholar] [CrossRef] [Green Version]
- Thompson, A.L.; Mendez, M.A.; Borja, J.B.; Adair, L.S.; Zimmer, C.R.; Bentley, M.E. Development and validation of the Infant Feeding Style Questionnaire. Appetite 2009, 53, 210–221. [Google Scholar] [CrossRef] [Green Version]
- Blackwell, C.K.; Tang, X.; Elliott, A.J.; Thomes, T.; Louwagie, H.; Gershon, R.; Schalet, B.D.; Cella, D. Developing a common metric for depression across adulthood: Linking PROMIS depression with the Edinburgh Postnatal Depression Scale. Psychol. Assess. 2021, 33, 610–618. [Google Scholar] [CrossRef] [PubMed]
- Cox, D. Regression models and life tables. J. Roy. Stat. Soc. Ser. B (Stat. Method) 1972, 34, 187–220. [Google Scholar] [CrossRef]
- Breslow, N.E. Discussion of the paper by D.R. Cox. J. Roy. Stat. Soc. Ser. B (Stat. Method) 1972, 34, 216–217. [Google Scholar]
- Ghali-Zinoubi, Z. On linking socioeconomic status to consumer willingness to buy and pay for organic food. J. Food Sci. Technol. 2021, 58, 1042–1050. [Google Scholar] [CrossRef]
- Foley, W.; Ward, P.; Carter, P.; Coveney, J.; Tsourtos, G.; Taylor, A. An ecological analysis of factors associated with food insecurity in South Australia, 2002–2007. Public Health Nutr. 2010, 13, 215–221. [Google Scholar] [CrossRef] [Green Version]
- Knueppel, D.; Demment, M.; Kaiser, L. Validation of the Household Food Insecurity Access Scale in rural Tanzania. Public Health Nutr. 2010, 13, 360–367. [Google Scholar] [CrossRef]
- Swanson, V.; Keely, A.; Denison, F.C. Does body image influence the relationship between body weight and breastfeeding maintenance in new mothers? Br. J. Health Psychol. 2017, 22, 557–576. [Google Scholar] [CrossRef] [Green Version]
- Morley-Hewitt, A.G.; Owen, A.L. A systematic review examining the association between female body image and the intention, initiation and duration of post-partum infant feeding methods (breastfeeding vs bottle-feeding). J. Health Psychol. 2020, 25, 207–226. [Google Scholar] [CrossRef]
- Butcher, L.M.; O’Sullivan, T.A.; Ryan, M.M.; Lo, J.; Nyanjom, J.; Wilkins, H.C.; Devine, A. To dine in or not to dine in: A comparison of food selection and preparation behaviours in those with and without food security. Health Promot. J. Aust. 2021, 32 Suppl. 2, 267–282. [Google Scholar] [CrossRef]
- Amir, L.H.; Donath, S. A systematic review of maternal obesity and breastfeeding intention, initiation and duration. BMC Pregnancy Childbirth 2007, 7, 9. [Google Scholar] [CrossRef] [Green Version]
- Donath, S.M.; Amir, L.H.; ALSPAC Study Team. Relationship between prenatal infant feeding intention and initiation and duration of breastfeeding: A cohort study. Acta Paediatr. 2007, 92, 352–356. [Google Scholar] [CrossRef]
- Clark, H.R.; Goyder, E.; Bissell, P.; Blank, L.; Peters, J. How do parents’ child-feeding behaviours influence child weight? Implications for childhood obesity policy. J. Public Health (Oxf.) 2007, 29, 132–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodgers, R.F.; O’Flynn, J.L.; Bourdeau, A.; Zimmerman, E. A biopsychosocial model of body image, disordered eating, and breastfeeding among postpartum women. Appetite 2018, 126, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, E.; Rodgers, R.F.; O’Flynn, J.; Bourdeau, A. Weight-Related Concerns as Barriers to Exclusive Breastfeeding at 6 Months. J. Hum. Lact. 2019, 35, 284–291. [Google Scholar] [CrossRef]
- Bayol, S.A.; Farrington, S.J.; Stickland, N.C. A maternal ‘junk food’ diet in pregnancy and lactation promotes an exacerbated taste for ‘junk food’ and a greater propensity for obesity in rat offspring. Br. J. Nutr. 2007, 98, 843–851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canned Food Alliance. Telephone Survey (Landline and Mobile Numbers) of 1007 American Adults by Caravan(r) Survey, April 4–7 2013; Margin of Error +/− 3.1%; Canned Food Alliance: Pittsburgh, PA, USA, 2013. [Google Scholar]
- Barański, M.; Srednicka-Tober, D.; Volakakis, N.; Seal, C.; Sanderson, R.; Stewart, G.B.; Benbrook, C.; Biavati, B.; Markellou, E.; Giotis, C.; et al. Higher antioxidant and lower cadmium concentrations and lower incidence of pesticide residues in organically grown crops: A systematiliterature review and me-ta-analyses. Br. J. Nutr. 2014, 112, 794–811. [Google Scholar] [CrossRef] [Green Version]
- Brandt, K.; Leifert, C.; Sanderson, R.; Seal, C.J. Agroecosystem Management and Nutritional Quality of Plant Foods: The Case of Organic Fruits and Vegetables. Crit. Rev. Plant Sci. 2011, 30, 177–197. [Google Scholar] [CrossRef]
- Asami, D.K.; Hong, Y.J.; Barrett, D.M.; Mitchell, A.E. Comparison of the total phenolic and ascorbic acid content of freeze-dried and air-dried marionberry, strawberry, and corn grown using conventional, organic, and sustainable agricultural practices. J. Agric. Food Chem. 2003, 51, 1237–1241. [Google Scholar] [CrossRef]
- Mardali, F.; Fatahi, S.; Alinaghizadeh, M.; Kord Varkaneh, H.; Sohouli, M.H.; Shidfar, F.; Găman, M.A. Association between abnormal maternal serum levels of vitamin B12 and preeclampsia: A systematic review and meta-analysis. Nutr. Rev. 2021, 79, 518–528. [Google Scholar] [CrossRef]

| Food Source Questions (MFSP) | Response Options | Food Source Classification | Food Source Score |
|---|---|---|---|
| How often did you eat canned foods of any kind (meat, fish, vegetables, fruit, beans, etc.)? | Never | Excellent | 1 |
| 1 time/month | Good | 2 | |
| 2–3 times/month | |||
| 1 time/week | Average | 3 | |
| 2 times/week | |||
| 3–4 times/week | |||
| 5–6 times/week | |||
| 1 time/day | Poor | 4 | |
| 2+ times/day | |||
| How often did you eat fast-food or take-out food from restaurants (such as McDonalds, Chipotle, Panera, Chinese food) or prepared foods from a grocery store or deli counter? | Never | Excellent | 1 |
| 1 time/month | Good | 2 | |
| 2–3 times/month | |||
| 1 time/week | Average | 3 | |
| 2 times/week | |||
| 3–4 times/week | |||
| 5–6 times/week | |||
| 1 time/day | Poor | 4 | |
| 2+ times/day | |||
| How often did you eat meals that you or someone else prepared at home? | Never | Poor | 4 |
| 1 time/month | Average | 3 | |
| 2–3 times/month | |||
| 1 time/week | Good | 2 | |
| 2 times/week | |||
| 3–4 times/week | |||
| 5–6 times/week | |||
| 1 time/day | Excellent | 1 | |
| 2+ times/day | |||
| How often did you consume the food groups below that were organic (either fresh produce or from a jar, a package, or homemade, or labeled ‘Certified Organic’)? | Never/Rarely | Poor | 4 |
| Sometimes | Average | 3 | |
| Often | Good | 2 | |
| Nearly always | Excellent | 1 |
| Food Source Quality | |
|---|---|
| Mean Score * | Category |
| 1.00–2.0 | High |
| 2.01–3.0 | Moderate |
| 3.01–4.0 | Low |
| Characteristics | High Food Source Quality N (%) | High Food Source Quality BF Duration Mean (SD) | Moderate Food Source Quality N (%) | Moderate Food Source Quality BF Duration Mean (SD) | Low Food Source Quality N (%) | Low Food Source Quality BF Duration Mean (SD) |
|---|---|---|---|---|---|---|
| Quality scale categories | 270 (100%) | 41.2 (32.9) | 341 (100%) | 27.2 (23) | 140 (100%) | 16 (16.4) |
| Maternal race/ethnicity | ||||||
| Non-Hispanic White | 128 (47.4%) | 48.2 (34.4) | 140 (41.1%) | 32.6 (22.7) | 52 (37.1%) | 25.1 (20.7) |
| Non-Hispanic Black | 16 (5.9%) | 26.8 (26.3) | 54 (15.8%) | 19.8 (16.6) | 20 (14.3%) | 9.6 (11.9) |
| Hispanic | 109 (40.4%) | 35.3 (30) | 122 (35.8%) | 26 (24.9) | 49 (35%) | 10.9 (9.3) |
| Other race | <15 | 45.3 (34.8) | 19 (5.6%) | 19.2 (20) | <20 | 11.5 (10.5) |
| Unknown or missing | <5 | 23.8 (33.5) | 6 (1.8%) | 18.9 (19.3) | <5 | 8.8 (12.3) |
| Maternal education | ||||||
| Less than high school, high school degree, GED or equivalent | 31 (11.5%) | 16.3 (12.1) | 58 (17%) | 20.5 (22.1) | 37 (26.4%) | 9.4 (10.2) |
| Some college, no degree, associate degree, trade school | 49 (18.1%) | 35.8 (33.4) | 88 (25.8%) | 25.5 (26.2) | 37 (26.4%) | 18.2 (16.1) |
| Bachelor’s degree | 85 (31.5%) | 49.2(37.1) | 92 (27%) | 31.4 (21.9) | 26 (18.6%) | 22.7 (19.9) |
| Masters, professional, or doctorate degree | 88 (32.6%) | 48 (28.9) | 61 (17.9%) | 36.3 (18.8) | 8 (5.7%) | 33.8 (24.6) |
| Unknown or missing | 17 (6.3%) | 27.9 (26) | 42 (12.3%) | 17.7 (18.3) | 32 (22.9%) | 11.1 (11.3) |
| Household income | ||||||
| <$30,000 | 38 (14.1%) | 25.2 (26.7) | 96 (28.2%) | 17.1 (20.4) | 57 (40.7%) | 11.8 (11.9) |
| $30,000–$99,999 | 42 (15.6%) | 28.7 (19.7) | 115 (33.7%) | 29 (20.1) | 37 (26.4%) | 19.7 (18.3) |
| $100,000–$199,999 | 69 (25.6%) | 50.6 (36.7) | 42 (12.3%) | 35.2 (23.1) | 10 (7.1%) | 36.3 (26.1) |
| $200,000 or more | 58 (21.5%) | 46 (27.9) | 8 (2.3%) | 24.6 (24.8) | ||
| Unknown or missing | 63 (23.3%) | 44.6 (37.5) | 80 (23.5%) | 32.9 (25.6) | 36 (25.7%) | 13.2 (12.7) |
| Marital status | ||||||
| Married or living with a partner | 221 (81.9%) | 43.9 (32.4) | 272 (79.8%) | 29.2 (23.1) | 97 (69.3%) | 19.2 (18.1) |
| Widowed, separated, divorced | 5 (1.9%) | 25.1 (13.5) | 11 (3.2%) | 30.2 (23.4) | 5 (3.6%) | 3.2 (1.3) |
| Not married, not living together | 37 (13.7%) | 31.4 (36.5) | 45 (13.2%) | 17.7 (21) | 15 (10.7%) | 11.1 (8.1) |
| Unknown or missing | 7 (2.6%) | 21 (18.2) | 13 (3.8%) | 15.7 (15.7) | 23 (16.4%) | 8.4 (8.9) |
| Pregnancy depression diagnosis | ||||||
| No | 96 (35.6%) | 46.6 (34.4) | 98 (28.7%) | 35.8 (26.2) | 40 (28.6%) | 25.3 (21.2) |
| Yes | 21 (7.8%) | 53 (46.5) | 27 (7.9%) | 27.4 (26.1) | 14 (10%) | 14.6 (15.9) |
| Unknown or Missing | 153 (56.7%) | 36.2 (28.7) | 216 (63.3%) | 23.3 (19.8) | 86 (61.4%) | 11.9 (11.8) |
| Pregnancy depression PROMIS T-score | ||||||
| Low score (Below 50%) | 43 (15.9%) | 22.4 (21.7) | 117 (34.3%) | 23.2 (22.1) | 65 (46.4%) | 10.9 (10.2) |
| High score (Above 50%) | 34 (12.6%) | 34.7 (23.7) | 136 (39.9%) | 23.8 (17.6) | 52 (37.1%) | 17.1 (16.9) |
| Unknown or missing | 193 (71.5%) | 46.6 (34.6) | 88 (25.8%) | 37.8 (27.9) | 23 (16.4%) | 27.7 (22.8) |
| Parity (pregnancies > 20 weeks) | ||||||
| 0 | 123 (45.6%) | 50.2 (33.9) | 39 (11.4%) | 41.7 (27.1) | 9 (6.4%) | 28.6 (20.8) |
| 1 | 39 (14.4%) | 40.6 (32.4) | 69 (20.2%) | 29.9 (22.9) | 32 (22.9%) | 22.8 (19.8) |
| 2 | 14 (5.2%) | 45.3 (37.5) | 24 (7%) | 35.2 (22) | 8 (5.7%) | 18.5 (18.7) |
| 3+ | 11 (4.1%) | 41 (31.3) | 15 (4.4%) | 27 (33.6) | 13 (9.3%) | 21.1 (23.2) |
| Unknown or missing | 83 (30.7%) | 27.5 (26.2) | 194 (56.9%) | 22.4 (19.6) | 78 (55.7%) | 10.6 (9.9) |
| Maternal age at birth (years) | ||||||
| 18–26 | 50 (18.5%) | 27.7 (26.1) | 93 (27.3%) | 19.3 (16.5) | 54 (38.6%) | 10.7 (8.8) |
| 27–30 | 44 (16.3%) | 41.7 (31.6) | 90 (26.4%) | 29.8 (24.5) | 45 (32.1%) | 16.3 (13.9) |
| 31–33 | 58 (21.5%) | 43.9 (31) | 66 (19.4%) | 33.4 (25.1) | 19 (13.6%) | 23.7 (26.8) |
| >33 | 118 (43.7%) | 45.5 (35.5) | 92 (27%) | 28.3 (23.7) | 22 (15.7%) | 21.9 (20.2) |
| Maternal pre-pregnancy BMI | ||||||
| <25 | 136 (50.4%) | 46.3 (34.9) | 80 (23.5%) | 28.5 (24) | 35 (25%) | 20.3 (18.1) |
| 25–30 | 46 (17%) | 34.1 (26.4) | 64 (18.8%) | 36.2 (31) | 36 (25.7%) | 15.8 (16.6) |
| >30 | 45 (16.7%) | 37.7 (35) | 77 (22.6%) | 20.7 (21.5) | 42 (30%) | 14.3 (13.2) |
| Unknown or missing | 43 (15.9%) | 36.5 (28.3) | 120 (35.2%) | 25.7 (15.7) | 27 (19.3%) | 13.3 (18.2) |
| Gestational age | ||||||
| 20–36 weeks | <25 | 28.6 (26.2) | 25 (7.3%) | 19.3 (17.3) | 17 (12.1%) | 13.5 (16.9) |
| 37–39 weeks | 139 (51.5%) | 41.6 (33.1) | 215 (63%) | 26.3 (21.9) | 81 (57.9%) | 17.3 (17.2) |
| 40+ weeks | 108 (40%) | 43.1 (33.6) | 93 (27.3%) | 30.8 (26.2) | 32 (22.9%) | 15.6 (15.9) |
| Unknown or missing | <5 | 46.6 (26) | 8 (2.3%) | 34.6 (20.4) | 10 (7.1%) | 10.6 (9.6) |
| Birth weight (grams) | ||||||
| 500–2500 | 11 (4.1%) | 31.7 (29.6) | 15 (4.4%) | 20.6 (17.3) | 9 (6.4%) | 12.1 (17) |
| 2501+ | 227 (84.1%) | 45.1 (33) | 282 (82.7%) | 29.2 (23.5) | 90 (64.3%) | 18.1 (17.9) |
| Unknown or missing | 32 (11.9%) | 17.3 (19.8) | 44 (12.9%) | 16.5 (16.9) | 41 (29.3%) | 12.3 (12) |
| Maternal and Birth Characteristics | N (%) with Data | Breastfeeding Duration, Weeks Mean (SD) | Bivariate HR Estimate | Bivariate 95% CI |
|---|---|---|---|---|
| Food source quality overall | 751 (100%) | 30.2 (27.6) | ||
| Food source quality categories | ||||
| High | 270 (36%) | 41.2 (32.9) | 0.8 | 0.66, 0.97 |
| Moderate | 341 (45%) | 27.2 (23.0) | 1 | Referent |
| Low | 140 (19%) | 16.0 (16.4) | 1.6 | 1.29, 1.98 |
| Maternal race/ethnicity | ||||
| Non-Hispanic White | 320 (43%) | 37.6 (29.1) | 1 | Referent |
| Non-Hispanic Black | 90 (12%) | 18.8 (18.5) | 1.37 | 1.03, 1.81 |
| Hispanic | 280 (37%) | 27 (26.5) | 1.14 | 0.93, 1.4 |
| Other race | 47 (6%) | 24 (26.4) | 1.39 | 1.01, 1.91 |
| Unknown or missing | 14 (2%) | 17.4 (21.8) | 1.55 | 0.87, 2.76 |
| Maternal education | ||||
| Less than high school, high school degree, GED or equivalent | 126 (17%) | 16.2 (17.6) | 1 | Referent |
| Some college, no degree, associate degree, trade school | 174 (23%) | 26.9 (27.4) | 0.67 | 0.53, 0.84 |
| Bachelor’s degree | 203 (27%) | 37.7 (30.7) | 0.55 | 0.43, 0.7 |
| Masters, professional, or doctorate degree | 157 (21%) | 42.7 (25.8) | 0.51 | 0.39, 0.66 |
| Unknown or missing | 91 (12%) | 17.3 (18.7) | 0.66 | 0.47, 0.92 |
| Household income | ||||
| <$30,000 | 191 (25%) | 17.1 (20.3) | 1 | Referent |
| $30,000–$99,999 | 194 (26%) | 27.1 (19.9) | 0.77 | 0.61, 0.98 |
| $100,000–$199,999 | 121 (16%) | 44.1 (32.5) | 0.6 | 0.45, 0.81 |
| $200,000 or more | 66 (9%) | 43.4 (28.3) | 0.74 | 0.51, 1.08 |
| Unknown or missing | 179 (24%) | 33.1 (30.7) | 0.69 | 0.52,0.91 |
| Marital status | ||||
| Married or living with a partner | 590 (79%) | 33.1 (27.8) | 1 | Referent |
| Widowed, separated, divorced | 21 (3%) | 22.6 (20.9) | 1.01 | 0.65, 1.58 |
| Not married, not living together | 97 (13%) | 21.9 (27.8) | 1.3 | 1.04, 1.63 |
| Unknown or missing | 43 (6%) | 12.7 (13.5) | 1.57 | 1.08, 2.27 |
| Pregnancy depression diagnosis | ||||
| No | 234 (31%) | 38.4 (30.1) | 1 | Referent |
| Yes | 62 (8%) | 33.2 (35.8) | 1.17 | 0.88, 1.56 |
| Unknown or missing | 455 (61%) | 25.5 (23.8) | 1.71 | 1.2, 2.44 |
| Pregnancy depression PROMIS T-score | ||||
| Low score (Below 50%) | 222 (30%) | 23.9 (19.2) | 1 | Referent |
| High score (Above 50%) | 225 (30%) | 19.5 (20) | 1.05 | 0.85, 1.3 |
| Missing | 304 (40%) | 42.6 (32.4) | 0.79 | 0.57, 1.1 |
| Parity (pregnancies > 20 weeks) | ||||
| 0 | 171 (23%) | 47.2 (32.3) | 1 | Referent |
| 1 | 140 (19%) | 31.3 (25.9) | 1.17 | 0.88, 1.54 |
| 2 | 46 (6%) | 35.4 (28.1) | 1.07 | 0.74, 1.55 |
| 3+ | 39 (5%) | 29 (30.1) | 1.11 | 0.75, 1.65 |
| Missing | 355 (47%) | 21 (20.6) | 1.6 | 1.16, 2.22 |
| Maternal Age at birth (years) | ||||
| 18–26 | 197 (26%) | 19 (18.9) | 1 | Referent |
| 27–30 | 179 (24%) | 29.3 (25.9) | 0.71 | 0.58, 0.88 |
| 31–33 | 143 (19%) | 36.4 (28.5) | 0.61 | 0.49, 0.77 |
| >33 | 232 (31%) | 36.4 (31.4) | 0.71 | 0.58, 0.88 |
| Maternal pre-pregnancy BMI | ||||
| <25 | 251 (33%) | 37 (31.5) | 1 | Referent |
| 25–30 | 146 (19%) | 30.5 (27.8) | 0.92 | 0.75, 1.15 |
| >30 | 164 (22%) | 23.7 (25.9) | 1.19 | 0.97, 1.47 |
| Missing | 190 (25%) | 26.4 (20.7) | 1.21 | 0.91, 1.62 |
| Gestational age | ||||
| 20–36 weeks | 63 (8%) | 20.9 (21.2) | 1.34 | 1.02, 1.75 |
| 37–39 weeks | 435 (58%) | 29.5 (26.8) | 1 | Referent |
| 40+ weeks | 233 (31%) | 34.4 (30.3) | 0.94 | 0.79, 1.1 |
| Missing | 20 (3%) | 23.8 (20.7) | 1.14 | 0.69, 1.89 |
| Birth weight (grams) | ||||
| 500–2500 | 35 (5%) | 21.9 (22.5) | 1.41 | 0.99, 2 |
| 2501+ | 599 (80%) | 33.6 (28.6) | 1 | Referent |
| Missing | 117 (16%) | 15.3 (16.3) | 1.43 | 0.97, 2.1 |
| Maternal and Birth Characteristics | N (%) | Full Model HR Estimate | Full Model 95% CI | Final Model HR Estimate | Final Model 95% CI |
|---|---|---|---|---|---|
| Food source quality overall | 751 (100%) | ||||
| Food source quality categories | |||||
| High | 270 (36%) | 0.75 | 0.62, 0.92 | 0.76 | 0.63, 0.92 |
| Moderate | 341 (45%) | 1 | Referent | 1 | Referent |
| Low | 140 (19%) | 1.46 | 1.16, 1.83 | 1.52 | 1.22, 1.89 |
| Maternal race/ethnicity | |||||
| Non-Hispanic White | 320 (43%) | 1 | Referent | ||
| Non-Hispanic Black | 90 (12%) | 1.19 | 0.89, 1.6 | ||
| Hispanic | 280 (37%) | 1.07 | 0.86, 1.32 | ||
| Other race | 47 (6%) | 1.12 | 0.8, 1.58 | ||
| Unknown or missing | 14 (2%) | 1.41 | 0.75, 2.62 | ||
| Maternal education | |||||
| Less than high school, high school degree, GED or equivalent | 126 (17%) | 1 | Referent | 1 | Referent |
| Some college, no degree, Associate degree, trade school | 174 (23%) | 0.74 | 0.58, 0.95 | 0.7 | 0.55, 0.9 |
| Bachelor’s degree | 203 (27%) | 0.65 | 0.49, 0.85 | 0.6 | 0.46, 0.77 |
| Masters, professional, or doctorate degree | 157 (21%) | 0.63 | 0.46, 0.87 | 0.58 | 0.44, 0.77 |
| Unknown or missing | 91 (12%) | 0.65 | 0.46, 0.92 | 0.68 | 0.49, 0.95 |
| Household income | |||||
| <$30,000 | 191 (25%) | 1 | Referent | ||
| $30,000–$99,999 | 194 (26%) | 1.03 | 0.79, 1.32 | ||
| $100,000–$199,999 | 121 (16%) | 0.9 | 0.65, 1.26 | ||
| $200,000 or more | 66 (9%) | 1.18 | 0.77, 1.81 | ||
| Unknown or missing | 179 (24%) | 0.86 | 0.65, 1.14 | ||
| Marital status | |||||
| Married or living with a partner | 590 (79%) | 1 | Referent | ||
| Widowed, separated, divorced | 21 (3%) | 1.02 | 0.64, 1.62 | ||
| Not married, not living together | 97 (13%) | 1.03 | 0.81, 1.32 | ||
| Unknown or missing | 43 (6%) | 1.52 | 1.03, 2.26 | ||
| Pregnancy depression diagnosis | |||||
| No | 234 (31%) | 1 | Referent | ||
| Yes | 62 (8%) | 1.17 | 0.87, 1.57 | ||
| Unknown or Missing | 455 (61%) | 1.54 | 1.02, 2.31 | ||
| Pregnancy depression PROMIS T-score | |||||
| Low score (below 50%) | 222 (30%) | 1 | Referent | ||
| High score (above 50%) | 225 (30%) | 0.96 | 0.77, 1.2 | ||
| Missing | 304 (40%) | 0.85 | 0.62, 1.16 | ||
| Parity (pregnancies > 20 weeks) | |||||
| 0 | 171 (23%) | 1 | Referent | ||
| 1 | 140 (19%) | 1.15 | 0.86, 1.55 | ||
| 2 | 46 (6%) | 1.07 | 0.73, 1.56 | ||
| 3+ | 39 (5%) | 1.08 | 0.69, 1.67 | ||
| Missing | 355 (47%) | 1.19 | 0.81, 1.74 | ||
| Maternal age at birth (years) | |||||
| 18–26 | 197 (26%) | 1 | Referent | 1 | Referent |
| 27–30 | 179 (24%) | 0.75 | 0.59, 0.94 | 0.76 | 0.61, 0.94 |
| 31–33 | 143 (19%) | 0.67 | 0.52, 0.87 | 0.67 | 0.53, 0.85 |
| >33 | 232 (31%) | 0.75 | 0.59, 0.95 | 0.78 | 0.62, 0.97 |
| Maternal pre-pregnancy BMI | |||||
| <25 | 251 (33%) | 1 | Referent | 1 | Referent |
| 25–30 | 146 (19%) | 0.9 | 0.72, 1.14 | 0.85 | 0.68, 1.06 |
| >30 | 164 (22%) | 1.2 | 0.96, 1.5 | 1.17 | 0.94, 1.44 |
| Missing | 190 (25%) | 0.94 | 0.69, 1.29 | 1.02 | 0.76, 1.37 |
| Gestational age | |||||
| 20–36 weeks | 63 (8%) | 1.24 | 0.89, 1.74 | ||
| 37–39 weeks | 435 (58%) | 1 | Referent | ||
| 40+ weeks | 233 (31%) | 0.93 | 0.78, 1.1 | ||
| Missing | 20 (3%) | 1.08 | 0.63, 1.87 | ||
| Birth weight (grams) | |||||
| 500–2500 | 35 (5%) | 1.07 | 0.68, 1.67 | ||
| 2501+ | 599 (80%) | 1 | Referent | ||
| Missing | 117 (16%) | 0.99 | 0.66, 1.48 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zimmerman, E.; Gachigi, K.K.; Rodgers, R.F.; Watkins, D.J.; Woodbury, M.; Cordero, J.F.; Alshawabkeh, A.; Meeker, J.D.; Huerta-Montañez, G.; Pabon, Z.R.; et al. Association between Quality of Maternal Prenatal Food Source and Preparation and Breastfeeding Duration in the Environmental Influences on Child Health Outcome (ECHO) Program. Nutrients 2022, 14, 4922. https://doi.org/10.3390/nu14224922
Zimmerman E, Gachigi KK, Rodgers RF, Watkins DJ, Woodbury M, Cordero JF, Alshawabkeh A, Meeker JD, Huerta-Montañez G, Pabon ZR, et al. Association between Quality of Maternal Prenatal Food Source and Preparation and Breastfeeding Duration in the Environmental Influences on Child Health Outcome (ECHO) Program. Nutrients. 2022; 14(22):4922. https://doi.org/10.3390/nu14224922
Chicago/Turabian StyleZimmerman, Emily, Kennedy K. Gachigi, Rachel F. Rodgers, Deborah J. Watkins, Megan Woodbury, José F. Cordero, Akram Alshawabkeh, John D. Meeker, Gredia Huerta-Montañez, Zaira Rosario Pabon, and et al. 2022. "Association between Quality of Maternal Prenatal Food Source and Preparation and Breastfeeding Duration in the Environmental Influences on Child Health Outcome (ECHO) Program" Nutrients 14, no. 22: 4922. https://doi.org/10.3390/nu14224922







