Relationship of Early Anemia with Neurodevelopment and Brain Injury in Very Low Birth Weight Preterm Infants—A Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Data Collection
2.4. Exposure and Outcome Variables
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics in the Early Anemia Group and the Control Group
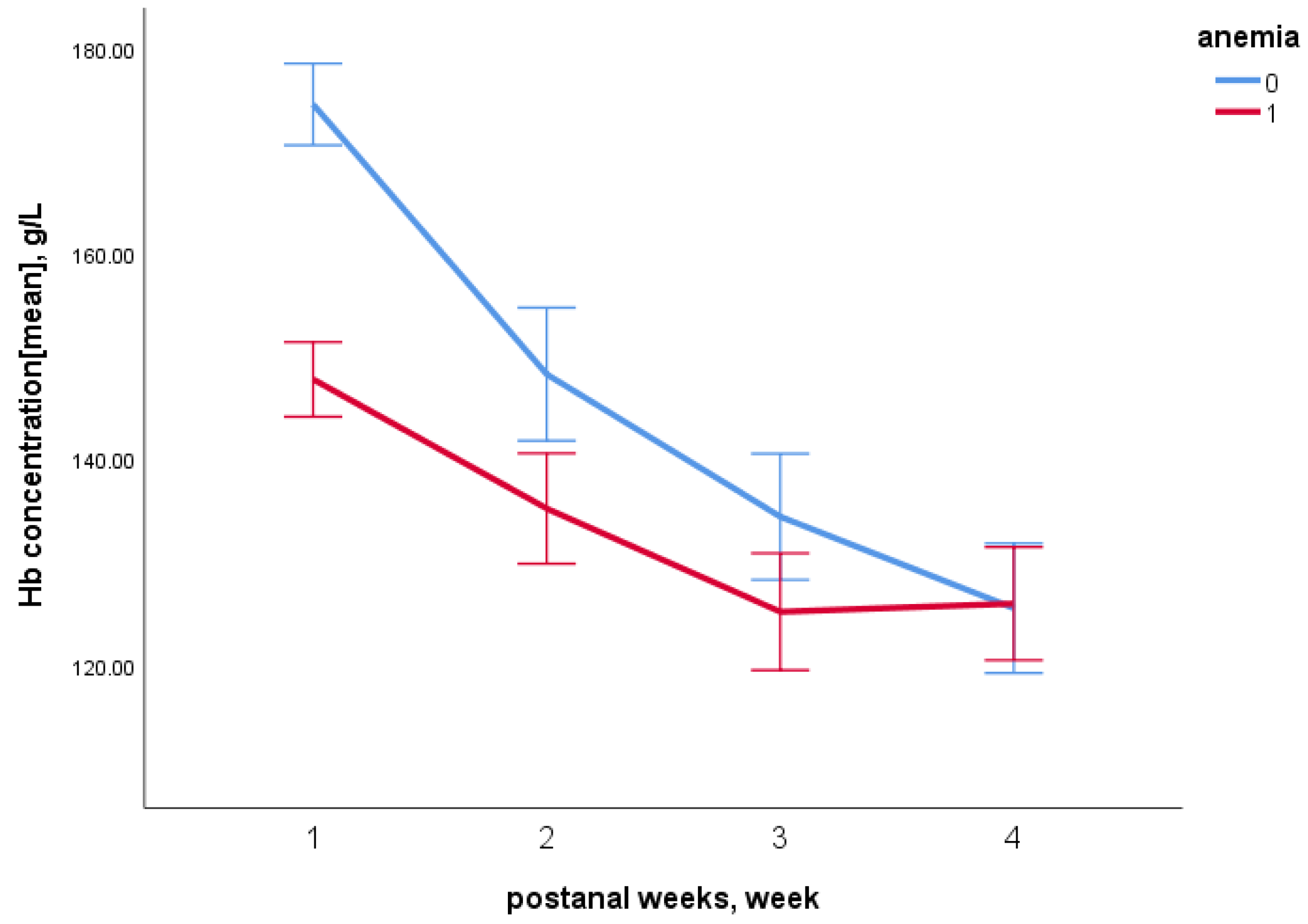
3.2. The Changes in Hb Concentration in VLBW Preterm Infants
3.3. The Relationship between Early Anemia and Neurodevelopment
3.4. The Relationship between Early Anemia and Brain Injury
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Preterm Birth Fact Sheet; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Widness, J.A. Pathophysiology of Anemia During the Neonatal Period, Including Anemia of Prematurity. NeoReviews 2008, 9, e520–e525. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rocha, G.; Pereira, S.; Antunes-Sarmento, J.; Flôr-De-Lima, F.; Soares, H.; Guimarães, H. Early anemia and neonatal morbidity in extremely low birth-weight preterm infants. J. Matern. Neonatal Med. 2021, 34, 3697–3703. [Google Scholar] [CrossRef] [PubMed]
- Aher, S.; Malwatkar, K.; Kadam, S. Neonatal anemia. Semin. Fetal Neonatal Med. 2008, 13, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Peng, H.; Tong, X. Study on the correlation between medical blood loss and the occurrence of anemia in preterm infants and the need for blood transfusion. Chin. J. Neonatol. 2008, 23, 197–200. [Google Scholar]
- Feng, S. Neonatal anemia. Foreign Med. Transfus. Hematol. 1986, 4, 279. [Google Scholar]
- Kadooka, M.; Kato, H.; Kato, A.; Ibara, S.; Minakami, H.; Maruyama, Y. Effect of neonatal hemoglobin concentration on long-term outcome of infants affected by fetomaternal hemorrhage. Early Hum. Dev. 2014, 90, 431–434. [Google Scholar] [CrossRef]
- Kirpalani, H.; Whyte, R.K.; Andersen, C.; Asztalos, E.V.; Heddle, N.; Blajchman, M.A.; Peliowski, A.; Rios, A.; LaCorte, M.; Connelly, R.; et al. The premature infants in need of transfusion (pint) study: A randomized, controlled trial of a restrictive (LOW) versus liberal (HIGH) transfusion threshold for extremely low birth weight infants. J. Pediatr. 2006, 149, 301–307.e3. [Google Scholar] [CrossRef]
- Kalteren, W.S.; Mebius, M.J.; Verhagen, E.A.; Tanis, J.C.; Kooi, E.M.; Bos, A.F. Neonatal Hemoglobin Levels in Preterm Infants Are Associated with Early Neurological Functioning. Neonatology 2021, 118, 593–599. [Google Scholar] [CrossRef]
- Kirpalani, H.; Bell, E.F.; Hintz, S.R.; Tan, S.; Schmidt, B.; Chaudhary, A.S.; Johnson, K.J.; Crawford, M.M.; Newman, J.E.; Vohr, B.R.; et al. Higher or Lower Hemoglobin Transfusion Thresholds for Preterm Infants. N. Engl. J. Med. 2020, 383, 2639–2651. [Google Scholar] [CrossRef]
- Kratimenos, P.; Christidis, P.; Kehinde, F.; Koutroulis, I.; Santana, S.; Mossabeb, R.; Fleishman, R. Association between hemoglobin concentrations at discharge from the neonatal intensive care unit with markers of neurodevelopmental outcomes in premature neonates. J. Neonatal Perinat. Med. 2019, 12, 221–230. [Google Scholar] [CrossRef]
- Kalteren, W.S.; Ter Horst, H.J.; Heijer, A.E.D.; De Vetten, L.; Kooi, E.M.; Bos, A.F. Perinatal Anemia is Associated with Neonatal and Neurodevelopmental Outcomes in Infants with Moderate to Severe Perinatal Asphyxia. Neonatology 2018, 114, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Zonnenberg, I.A.; Vermeulen, R.J.; Rohaan, M.W.; Van Weissenbruch, M.M.; Groenendaal, F.; De Vries, L.S. Severe Neonatal Anaemia, MRI Findings and Neurodevelopmental Outcome. Neonatology 2016, 109, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Fontana, C.; Raffaeli, G.; Pesenti, N.; Boggini, T.; Cortesi, V.; Manzoni, F.; Picciolini, O.; Fumagalli, M.; Mosca, F.; Ghirardello, S. Red blood cell transfusions in preterm newborns and neurodevelopmental outcomes at 2 and 5 years of age. Blood Transfus. 2022, 20, 40–49. [Google Scholar] [PubMed]
- Loureiro, B.; Martinez-Biarge, M.; Foti, F.; Papadaki, M.; Cowan, F.M.; Wusthoff, C.J. MRI Patterns of brain injury and neurodevelopmental outcomes in neonates with severe anaemia at birth. Early Hum. Dev. 2017, 105, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Brazelton, T.B. The Brazelton Neonatal Behavior Assessment Scale: Introduction. Monogr. Soc. Res. Child Dev. 1978, 43, 1–13. [Google Scholar] [CrossRef]
- Bao, X.L.; Liu, W.M. Application of neonatal behavioral neurological assessment and observation to the assessment of brain development and early intervention in preterm and young infants. Chin. J. Pract. Pediatr. 2017, 32, 820–822. (In Chinese) [Google Scholar]
- Harmat, G. Intracranial sonography in infancy. Acta Paediatr. Hung. 1985, 26, 15–29. [Google Scholar]
- Yamashita, H.; Kukita, J.; Ohga, S.; Nakayama, H.; Akazawa, K.; Ueda, K. Serum Erythropoietin Levels in Term and Preterm Infants During the First Year of Life. J. Pediatr. Hematol. 1994, 16, 213–218. [Google Scholar] [CrossRef]
- Colombatti, R.; Sainati, L.; Trevisanuto, D. Anemia and transfusion in the neonate. Semin. Fetal Neonatal Med. 2016, 21, 2–9. [Google Scholar] [CrossRef]
- Belfort, M.B.; Ehrenkranz, R.A. Neurodevelopmental outcomes and nutritional strategies in very low birth weight infants. Semin. Fetal Neonatal Med. 2017, 22, 42–48. [Google Scholar] [CrossRef]
- Zheng, J.; Liu, J.; Yang, W. Association of Iron-Deficiency Anemia and Non-Iron-Deficiency Anemia with Neurobehavioral Development in Children Aged 6–24 Months. Nutrients 2021, 13, 3423. [Google Scholar] [CrossRef] [PubMed]
- Okereafor, A.; Allsop, J.; Counsell, S.J.; Fitzpatrick, J.; Azzopardi, D.; Rutherford, M.A.; Cowan, F.M. Patterns of Brain Injury in Neonates Exposed to Perinatal Sentinel Events. Pediatrics 2008, 121, 906–914. [Google Scholar] [CrossRef] [PubMed]
- Whyte, R.K. Neurodevelopmental Outcome of Extremely Low-Birth-Weight Infants Randomly Assigned to Restrictive or Liberal Hemoglobin Thresholds for Blood Transfusion. Semin. Perinatol. 2012, 36, 290–293. [Google Scholar] [CrossRef] [PubMed]
- Rabe, H.; Diaz-Rossello, J.L.; Duley, L.; Dowswell, T. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst. Rev. 2019, 9, CD003248. [Google Scholar] [CrossRef]
| Variable | Early Anemia Group | Control Group | p-Value |
|---|---|---|---|
| N = 55 | N = 55 | ||
| Maternal factors | |||
| maternal age (year) ▲ | 30 (28–33) | 30 (27–35) | 0.575 |
| Gravidity ▲ | 2 (1–3) | 2 (1–3) | 0.593 |
| Parity ▲ | 1 (1–2) | 2 (1–2) | 0.404 |
| Cesarean section, n (%) | 33 (68.8%) | 47 (74.6%) | 0.528 |
| Singleton, n (%) | 24 (50.0%) | 44 (69.8%) | 0.103 |
| Neonatal factors | |||
| Gestational age (weeks) ▲ | 30.43 (29.29–32.29) | 30.43 (29.29–32) | 0.657 |
| Birth weight (g) ▲ | 1355 (1190–1420) | 1300 (1105–1400) | 0.274 |
| Birth head circumference (cm) ▲ | 27 (26–28) | 27 (26–28) | 0.690 |
| Birth length (cm) ▲ | 38 (37–40) | 38 (36–40) | 0.579 |
| Male, n (%) | 25 (52.1%) | 39 (61.9%) | 0.336 |
| Nutrition supply | |||
| Amino acid introduction (DOL) ▲ | 0 (0–0) | 0 (0–0) | 0.258 |
| Duration of amino acid (days) ▲ | 23 (16–34) | 21 (14–28) | 0.215 |
| Lipid introduction (DOL) ▲ | 1 (1–2) | 1 (1–2) | 0.791 |
| Duration of lipid (days) ▲ | 21 (15–32) | 18 (11–26) | 0.076 |
| Start enteral nutrition (DOL) ▲ | 1 (1–2) | 1 (1–2) | 0.794 |
| Enteral feeding volumes(DOL) ▲ | |||
| 20 mL·kg−1·d−1 | 7 (3–12) | 5 (4–8) | 0.323 |
| 50 mL·kg−1·d−1 | 12 (7–19) | 9 (7–16) | 0.187 |
| 80 mL·kg−1·d−1 | 15 (11–28) | 13 (9–22) | 0.099 |
| 120 mL·kg−1·d−1 | 22 (17–36) | 18 (13–28) | 0.045 * |
| 150 mL·kg−1·d−1 | 24 (20–41) | 23 (16–33) | 0.308 |
| Respiratory condition | |||
| Intubation ventilation (days) ▲ | 2 (0–7) | 0 (0–6) | 0.340 |
| Non-invasive ventilation, (days) ▲ | 0 (0–4) | 2 (0–6) | 0.159 |
| Extra oxygen supply, (days) ▲ | 10 (0–23) | 5 (0–14) | 0.234 |
| NBNA Results | Early Anemia Group | Control Group | p-Value |
|---|---|---|---|
| N = 55 | N = 55 | ||
| NBNA score qualified, n (%) | 23 (47.9%) | 40 (63.5%) | 0.075 |
| NBNA total score ▲ | 36 (35–37.5) | 37 (36–38) | 0.086 |
| Behavioral ability score ▲ | 10 (9.5–11) | 11 (10–12) | 0.033 * |
| Passive muscle tone score ▲ | 8 (8–8) | 8 (8–8) | 0.818 |
| Active muscle tone score ▲ | 6 (6–7) | 6 (6–7) | 0.568 |
| Original reflex score ▲ | 6 (6–6) | 6 (6–6) | 0.282 |
| General assessment score ▲ | 6 (6–6) | 6 (6–6) | 1.000 |
| NBNA Results | Model 1 | p | Model 2 | p | Model 3 | p |
|---|---|---|---|---|---|---|
| NBNA total score | −0.516 (−1.113–0.082) | 0.091 | −0.650 (−1.215–−0.085) | 0.024 * | −0.748 (−1.368–−0.129) | 0.018 * |
| Behavioral ability score | −0.485 (−0.890–−0.080) | 0.019 * | −0.606 (−0.995–−0.218) | 0.002 * | −0.457 (−0.840–−0.020) | 0.041 * |
| Passive muscle tone score | −0.036 (−0.197–0.126) | 0.666 | −0.065 (−0.226–0.096) | 0.428 | −0.068 (−0.238–0.101) | 0.427 |
| Active muscle tone score | −0.205 (−0.726–0.317) | 0.442 | −0.230 (−0.757–0.296) | 0.391 | −0.401 (−0.930–0.128) | 0.138 |
| Original reflex score | 0.847 (−0.054–1.747) | 0.065 | 0.756 (−0.144–1.656) | 0.100 | 0.115 (−0.695–0.925) | 0.780 |
| General assessment score | NA | NA | NA | NA | NA | NA |
| Brain Injury | Early Anemia Group | Control Group | p-Value |
|---|---|---|---|
| N = 40 | N = 55 | ||
| Intraventricular hemorrhage | 6 (15.0%) | 7 (12.7%) | 0.489 |
| Ventricular cyst | 9 (22.5%) | 6 (10.9%) | 0.107 |
| Ventricular widening | 8 (20.0%) | 5 (9.1%) | 0.111 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, X.; Jing, J.; Huang, S.; He, X.; Gao, P.; Li, H.; Lin, Z.; Sangild, P.T.; Zhu, Y. Relationship of Early Anemia with Neurodevelopment and Brain Injury in Very Low Birth Weight Preterm Infants—A Prospective Cohort Study. Nutrients 2022, 14, 4931. https://doi.org/10.3390/nu14224931
Wang X, Jing J, Huang S, He X, Gao P, Li H, Lin Z, Sangild PT, Zhu Y. Relationship of Early Anemia with Neurodevelopment and Brain Injury in Very Low Birth Weight Preterm Infants—A Prospective Cohort Study. Nutrients. 2022; 14(22):4931. https://doi.org/10.3390/nu14224931
Chicago/Turabian StyleWang, Xiaotong, Jiajia Jing, Saijun Huang, Xiaoying He, Pingming Gao, Hailin Li, Zongyu Lin, Per Torp Sangild, and Yanna Zhu. 2022. "Relationship of Early Anemia with Neurodevelopment and Brain Injury in Very Low Birth Weight Preterm Infants—A Prospective Cohort Study" Nutrients 14, no. 22: 4931. https://doi.org/10.3390/nu14224931





