Subclinical Cardiovascular Disease Markers in Relation to Serum and Dietary Magnesium in Individuals from the General Population: The KORA-MRI Study
Abstract
:1. Introduction
2. Materials and Methods
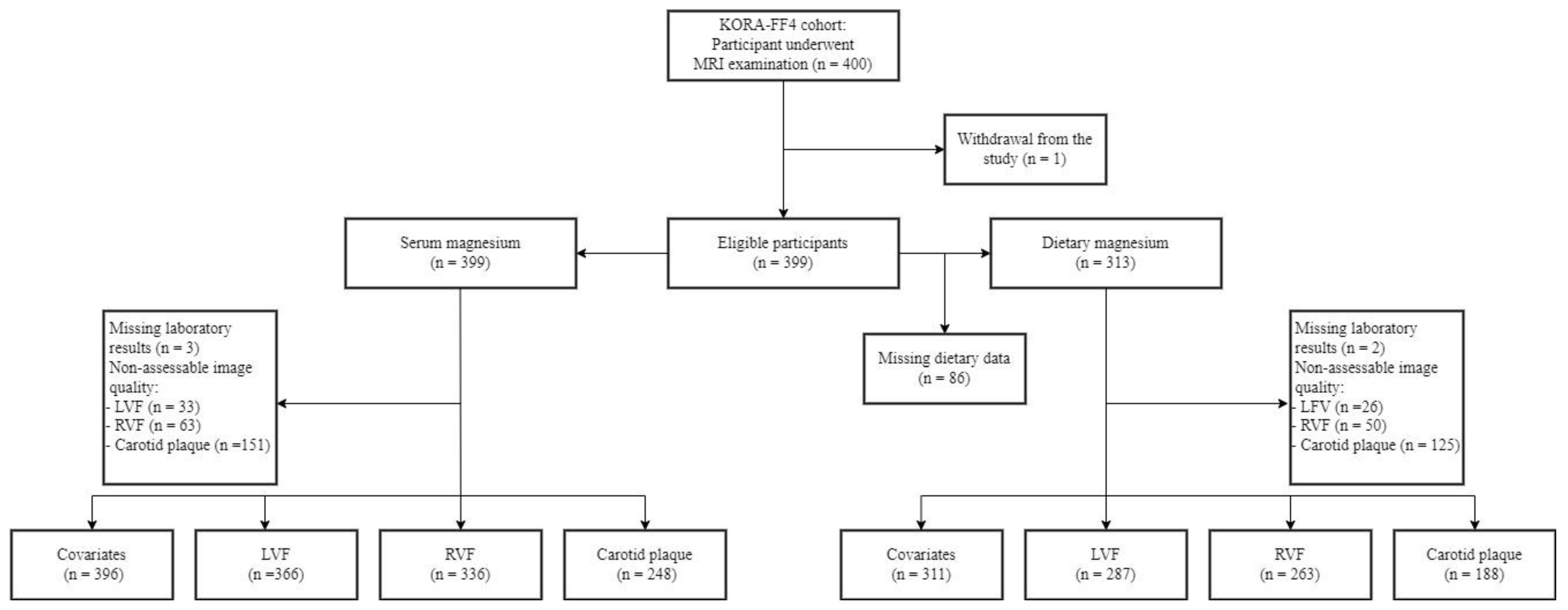
2.1. Study Design and Population
2.2. Assessment of Serum and Dietary Magnesium
2.3. Assessment of Subclinical Cardiovascular Disease Markers by MRI
2.3.1. Left Ventricular Structure and Function
2.3.2. Right Ventricular Structure and Function
2.3.3. Carotid Plaque
2.4. Assessment of Covariates
2.5. Statistical Analyses
3. Results
3.1. Study Population
3.2. Correlation between Serum and Dietary Magnesium with Clinical Characteristics and MRI-Derived Markers
3.3. Association between Magnesium and MRI-Derived Subclinical Cardiovascular Disease Markers
3.3.1. Serum Magnesium
3.3.2. Dietary Magnesium
4. Discussion
4.1. Main Findings
4.2. Correlation between Serum and Dietary Magnesium
4.3. Association of Magnesium with Overt and Early Cardiac Impairment
4.4. Association of Magnesium with Lipids and Preclinical Atherosclerosis
4.5. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mensah, G.A.; Roth, G.A.; Fuster, V. The Global Burden of Cardiovascular Diseases and Risk Factors: 2020 and Beyond. J. Am. Coll. Cardiol. 2019, 74, 2529–2532. [Google Scholar] [CrossRef] [PubMed]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.; Whitsel, L.; Khavjou, O.; Phelps, D.; Leib, A. Projections of Cardiovascular Disease Prevalence and Costs. RTI International. 2016. Available online: https://www.heart.org/-/media/Files/About-Us/Policy-Research/Fact-Sheets/Public-Health-Advocacy-and-Research/Projections-of-CVD-Prevalence-and-Costs-2015-2035.pdf (accessed on 30 September 2022).
- Song, P.; Fang, Z.; Wang, H.; Cai, Y.; Rahimi, K.; Zhu, Y.; Fowkes, F.G.R.; Fowkes, F.J.I.; Rudan, I. Global and regional prevalence, burden, and risk factors for carotid atherosclerosis: A systematic review, meta-analysis, and modelling study. Lancet Glob. Health 2020, 8, e721–e729. [Google Scholar] [CrossRef]
- Helfand, M.; Buckley, D.I.; Freeman, M.; Fu, R.; Rogers, K.; Fleming, C.; Humphrey, L.L. Emerging risk factors for coronary heart disease: A summary of systematic reviews conducted for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2009, 151, 496–507. [Google Scholar] [CrossRef] [PubMed]
- Kuo, F.; Gardener, H.; Dong, C.; Cabral, D.; Della-Morte, D.; Blanton, S.H.; Elkind, M.S.; Sacco, R.L.; Rundek, T. Traditional cardiovascular risk factors explain the minority of the variability in carotid plaque. Stroke 2012, 43, 1755–1760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qu, X.; Jin, F.; Hao, Y.; Li, H.; Tang, T.; Wang, H.; Yan, W.; Dai, K. Magnesium and the risk of cardiovascular events: A meta-analysis of prospective cohort studies. PLoS ONE 2013, 8, e57720. [Google Scholar] [CrossRef] [Green Version]
- Rodríguez-Ortiz, M.E.; Gómez-Delgado, F.; Arenas de Larriva, A.P.; Canalejo, A.; Gómez-Luna, P.; Herencia, C.; López-Moreno, J.; Rodríguez, M.; López-Miranda, J.; Almadén, Y. Serum Magnesium is associated with Carotid Atherosclerosis in patients with high cardiovascular risk (CORDIOPREV Study). Sci. Rep. 2019, 9, 8013. [Google Scholar] [CrossRef] [Green Version]
- Tangvoraphonkchai, K.; Davenport, A. Magnesium and Cardiovascular Disease. Adv. Chronic Kidney Dis. 2018, 25, 251–260. [Google Scholar] [CrossRef]
- Yamanaka, R.; Tabata, S.; Shindo, Y.; Hotta, K.; Suzuki, K.; Soga, T.; Oka, K. Mitochondrial Mg(2+) homeostasis decides cellular energy metabolism and vulnerability to stress. Sci. Rep. 2016, 6, 30027. [Google Scholar] [CrossRef]
- Liu, M.; Liu, H.; Feng, F.; Xie, A.; Kang, G.J.; Zhao, Y.; Hou, C.R.; Zhou, X.; Dudley, S.C., Jr. Magnesium Deficiency Causes a Reversible, Metabolic, Diastolic Cardiomyopathy. J. Am. Heart Assoc. 2021, 10, e020205. [Google Scholar] [CrossRef]
- Maier, J.A.; Malpuech-Brugère, C.; Zimowska, W.; Rayssiguier, Y.; Mazur, A. Low magnesium promotes endothelial cell dysfunction: Implications for atherosclerosis, inflammation and thrombosis. Biochim. Biophys. Acta 2004, 1689, 13–21. [Google Scholar] [CrossRef]
- Cazzola, R.; Della Porta, M.; Manoni, M.; Iotti, S.; Pinotti, L.; Maier, J.A. Going to the roots of reduced magnesium dietary intake: A tradeoff between climate changes and sources. Heliyon 2020, 6, e05390. [Google Scholar] [CrossRef]
- Fang, X.; Wang, K.; Han, D.; He, X.; Wei, J.; Zhao, L.; Imam, M.U.; Ping, Z.; Li, Y.; Xu, Y.; et al. Dietary magnesium intake and the risk of cardiovascular disease, type 2 diabetes, and all-cause mortality: A dose-response meta-analysis of prospective cohort studies. BMC Med. 2016, 14, 210. [Google Scholar] [CrossRef] [Green Version]
- Taveira, T.H.; Ouellette, D.; Gulum, A.; Choudhary, G.; Eaton, C.B.; Liu, S.; Wu, W.C. Relation of Magnesium Intake With Cardiac Function and Heart Failure Hospitalizations in Black Adults: The Jackson Heart Study. Circ. Heart Fail. 2016, 9, e002698. [Google Scholar] [CrossRef] [Green Version]
- Wu, W.C.; Huang, M.; Taveira, T.H.; Roberts, M.B.; Martin, L.W.; Wellenius, G.A.; Johnson, K.C.; Manson, J.E.; Liu, S.; Eaton, C.B. Relationship between Dietary Magnesium Intake and Incident Heart Failure Among Older Women: The WHI. J. Am. Heart Assoc. 2020, 9, e013570. [Google Scholar] [CrossRef]
- Reffelmann, T.; Dörr, M.; Ittermann, T.; Schwahn, C.; Völzke, H.; Ruppert, J.; Robinson, D.; Felix, S.B. Low serum magnesium concentrations predict increase in left ventricular mass over 5 years independently of common cardiovascular risk factors. Atherosclerosis 2010, 213, 563–569. [Google Scholar] [CrossRef]
- Ma, J.; Folsom, A.R.; Melnick, S.L.; Eckfeldt, J.H.; Sharrett, A.R.; Nabulsi, A.A.; Hutchinson, R.G.; Metcalf, P.A. Associations of serum and dietary magnesium with cardiovascular disease, hypertension, diabetes, insulin, and carotid arterial wall thickness: The ARIC study. Atherosclerosis Risk in Communities Study. J. Clin. Epidemiol. 1995, 48, 927–940. [Google Scholar] [CrossRef]
- Cao, Y.; Wang, C.; Guan, K.; Xu, Y.; Su, Y.X.; Chen, Y.M. Association of magnesium in serum and urine with carotid intima-media thickness and serum lipids in middle-aged and elderly Chinese: A community-based cross-sectional study. Eur. J. Nutr. 2016, 55, 219–226. [Google Scholar] [CrossRef]
- Hashimoto, T.; Hara, A.; Ohkubo, T.; Kikuya, M.; Shintani, Y.; Metoki, H.; Inoue, R.; Asayama, K.; Kanno, A.; Nakashita, M.; et al. Serum magnesium, ambulatory blood pressure, and carotid artery alteration: The Ohasama study. Am. J. Hypertens. 2010, 23, 1292–1298. [Google Scholar] [CrossRef]
- Darooghegi Mofrad, M.; Djafarian, K.; Mozaffari, H.; Shab-Bidar, S. Effect of magnesium supplementation on endothelial function: A systematic review and meta-analysis of randomized controlled trials. Atherosclerosis 2018, 273, 98–105. [Google Scholar] [CrossRef]
- Finn, A.V.; Kolodgie, F.D.; Virmani, R. Correlation between carotid intimal/medial thickness and atherosclerosis: A point of view from pathology. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 177–181. [Google Scholar] [CrossRef]
- Petersen, S.E.; Khanji, M.Y.; Plein, S.; Lancellotti, P.; Bucciarelli-Ducci, C. European Association of Cardiovascular Imaging expert consensus paper: A comprehensive review of cardiovascular magnetic resonance normal values of cardiac chamber size and aortic root in adults and recommendations for grading severity. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 1321–1331. [Google Scholar] [CrossRef] [Green Version]
- Holle, R.; Happich, M.; Löwel, H.; Wichmann, H.E. KORA--a research platform for population based health research. Gesundheitswesen 2005, 67 (Suppl. 1), 19–25. [Google Scholar] [CrossRef] [Green Version]
- Bamberg, F.; Hetterich, H.; Rospleszcz, S.; Lorbeer, R.; Auweter, S.D.; Schlett, C.L.; Schafnitzel, A.; Bayerl, C.; Schindler, A.; Saam, T.; et al. Subclinical Disease Burden as Assessed by Whole-Body MRI in Subjects With Prediabetes, Subjects with Diabetes, and Normal Control Subjects From the General Population: The KORA-MRI Study. Diabetes 2017, 66, 158–169. [Google Scholar] [CrossRef] [Green Version]
- Connerty, H.; Lau, H.; Briggs, A. Spectrophotometric determination of magnesium by use of methylthymol blue. In Clinical Chemistry; Amer Assoc Clinical Chemistry: Washington, DC, USA, 1971; p. 661. [Google Scholar]
- Costello, R.B.; Elin, R.J.; Rosanoff, A.; Wallace, T.C.; Guerrero-Romero, F.; Hruby, A.; Lutsey, P.L.; Nielsen, F.H.; Rodriguez-Moran, M.; Song, Y.; et al. Perspective: The Case for an Evidence-Based Reference Interval for Serum Magnesium: The Time has Come. Adv. Nutr. 2016, 7, 977–993. [Google Scholar] [CrossRef] [Green Version]
- Mitry, P.; Wawro, N.; Six-Merker, J.; Zoller, D.; Jourdan, C.; Meisinger, C.; Thierry, S.; Nöthlings, U.; Knüppel, S.; Boeing, H.; et al. Usual Dietary Intake Estimation Based on a Combination of Repeated 24-H Food Lists and a Food Frequency Questionnaire in the KORA FF4 Cross-Sectional Study. Front. Nutr. 2019, 6, 145. [Google Scholar] [CrossRef]
- Grover, S.; Leong, D.P.; Selvanayagam, J.B. Evaluation of left ventricular function using cardiac magnetic resonance imaging. J. Nucl. Cardiol. 2011, 18, 351–365. [Google Scholar] [CrossRef]
- Caudron, J.; Fares, J.; Bauer, F.; Dacher, J.N. Evaluation of left ventricular diastolic function with cardiac MR imaging. Radiographics 2011, 31, 239–259. [Google Scholar] [CrossRef]
- Patscheider, H.; Lorbeer, R.; Auweter, S.; Schafnitzel, A.; Bayerl, C.; Curta, A.; Rathmann, W.; Heier, M.; Meisinger, C.; Peters, A.; et al. Subclinical changes in MRI-determined right ventricular volumes and function in subjects with prediabetes and diabetes. Eur. Radiol. 2018, 28, 3105–3113. [Google Scholar] [CrossRef] [Green Version]
- Kerwin, W.; Xu, D.; Liu, F.; Saam, T.; Underhill, H.; Takaya, N.; Chu, B.; Hatsukami, T.; Yuan, C. Magnetic resonance imaging of carotid atherosclerosis: Plaque analysis. Top. Magn. Reason. Imaging 2007, 18, 371–378. [Google Scholar] [CrossRef]
- Cai, J.M.; Hatsukami, T.S.; Ferguson, M.S.; Small, R.; Polissar, N.L.; Yuan, C. Classification of human carotid atherosclerotic lesions with in vivo multicontrast magnetic resonance imaging. Circulation 2002, 106, 1368–1373. [Google Scholar] [CrossRef] [Green Version]
- WHO. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia: Report of a WHO/IDF Consultation; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- Seissler, J.; Feghelm, N.; Then, C.; Meisinger, C.; Herder, C.; Koenig, W.; Peters, A.; Roden, M.; Lechner, A.; Kowall, B.; et al. Vasoregulatory peptides pro-endothelin-1 and pro-adrenomedullin are associated with metabolic syndrome in the population-based KORA F4 study. Eur. J. Endocrinol. 2012, 167, 847–853. [Google Scholar] [CrossRef] [Green Version]
- Du Bois, D.; Du Bois, E.F. A formula to estimate the approximate surface area if height and weight be known. Nutrition 1989, 5, 303–311. [Google Scholar]
- Chiuve, S.E.; Sun, Q.; Curhan, G.C.; Taylor, E.N.; Spiegelman, D.; Willett, W.C.; Manson, J.E.; Rexrode, K.M.; Albert, C.M. Dietary and plasma magnesium and risk of coronary heart disease among women. J. Am. Heart Assoc. 2013, 2, e000114. [Google Scholar] [CrossRef] [Green Version]
- Kunutsor, S.K.; Whitehouse, M.R.; Blom, A.W.; Laukkanen, J.A. Low serum magnesium levels are associated with increased risk of fractures: A long-term prospective cohort study. Eur. J. Epidemiol. 2017, 32, 593–603. [Google Scholar] [CrossRef] [Green Version]
- Liao, F.; Folsom, A.R.; Brancati, F.L. Is low magnesium concentration a risk factor for coronary heart disease? The Atherosclerosis Risk in Communities (ARIC) Study. Am. Heart J. 1998, 136, 480–490. [Google Scholar] [CrossRef]
- Gant, C.M.; Soedamah-Muthu, S.S.; Binnenmars, S.H.; Bakker, S.J.L.; Navis, G.; Laverman, G.D. Higher Dietary Magnesium Intake and Higher Magnesium Status Are Associated with Lower Prevalence of Coronary Heart Disease in Patients with Type 2 Diabetes. Nutrients 2018, 10, 307. [Google Scholar] [CrossRef] [Green Version]
- Schuchardt, J.P.; Hahn, A. Intestinal Absorption and Factors Influencing Bioavailability of Magnesium-An Update. Curr. Nutr. Food Sci. 2017, 13, 260–278. [Google Scholar] [CrossRef]
- DiNicolantonio, J.J.; O’Keefe, J.H.; Wilson, W. Subclinical magnesium deficiency: A principal driver of cardiovascular disease and a public health crisis. Open Heart 2018, 5, e000668. [Google Scholar] [CrossRef]
- Nielsen, F.H.; Johnson, L.A. Data from Controlled Metabolic Ward Studies Provide Guidance for the Determination of Status Indicators and Dietary Requirements for Magnesium. Biol. Trace Elem. Res. 2017, 177, 43–52. [Google Scholar] [CrossRef]
- Del Gobbo, L.C.; Imamura, F.; Wu, J.H.; de Oliveira Otto, M.C.; Chiuve, S.E.; Mozaffarian, D. Circulating and dietary magnesium and risk of cardiovascular disease: A systematic review and meta-analysis of prospective studies. Am. J. Clin. Nutr. 2013, 98, 160–173. [Google Scholar] [CrossRef]
- Wang, D.; Zhu, Z.L.; Lin, D.C.; Zheng, S.Y.; Chuang, K.H.; Gui, L.X.; Yao, R.H.; Zhu, W.J.; Sham, J.S.K.; Lin, M.J. Magnesium Supplementation Attenuates Pulmonary Hypertension via Regulation of Magnesium Transporters. Hypertension 2021, 77, 617–631. [Google Scholar] [CrossRef]
- Gaasch, W.H.; Zile, M.R. Left ventricular diastolic dysfunction and diastolic heart failure. Annu. Rev. Med. 2004, 55, 373–394. [Google Scholar] [CrossRef]
- Mizuguchi, Y.; Konishi, T.; Nagai, T.; Sato, T.; Takenaka, S.; Tada, A.; Kobayashi, Y.; Komoriyama, H.; Kato, Y.; Omote, K.; et al. Prognostic value of admission serum magnesium in acute myocardial infarction complicated by malignant ventricular arrhythmias. Am. J. Emerg. Med. 2021, 44, 100–105. [Google Scholar] [CrossRef]
- Shafiq, A.; Goyal, A.; Jones, P.G.; Sahil, S.; Hoffman, M.; Qintar, M.; Buchanan, D.M.; Kosiborod, M.; Arnold, S.V. Serum Magnesium Levels and In-Hospital Mortality in Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2017, 69, 2771–2772. [Google Scholar] [CrossRef]
- Larsson, S.C.; Burgess, S.; Michaëlsson, K. Serum magnesium levels and risk of coronary artery disease: Mendelian randomisation study. BMC Med. 2018, 16, 68. [Google Scholar] [CrossRef] [Green Version]
- He, B.; Xia, L.; Zhao, J.; Yin, L.; Zhang, M.; Quan, Z.; Ou, Y.; Huang, W. Causal Effect of Serum Magnesium on Osteoporosis and Cardiometabolic Diseases. Front. Nutr. 2021, 8, 738000. [Google Scholar] [CrossRef]
- De Oliveira Otto, M.C.; Alonso, A.; Lee, D.H.; Delclos, G.L.; Jenny, N.S.; Jiang, R.; Lima, J.A.; Symanski, E.; Jacobs, D.R., Jr.; Nettleton, J.A. Dietary micronutrient intakes are associated with markers of inflammation but not with markers of subclinical atherosclerosis. J. Nutr. 2011, 141, 1508–1515. [Google Scholar] [CrossRef] [Green Version]
- Inaba, Y.; Chen, J.A.; Bergmann, S.R. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: A meta-analysis. Atherosclerosis 2012, 220, 128–133. [Google Scholar] [CrossRef]
- Cambray, S.; Ibarz, M.; Bermudez-Lopez, M.; Marti-Antonio, M.; Bozic, M.; Fernandez, E.; Valdivielso, J.M. Magnesium Levels Modify the Effect of Lipid Parameters on Carotid Intima Media Thickness. Nutrients 2020, 12, 2631. [Google Scholar] [CrossRef]
- Randell, E.W.; Mathews, M.; Gadag, V.; Zhang, H.; Sun, G. Relationship between serum magnesium values, lipids and anthropometric risk factors. Atherosclerosis 2008, 196, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Merchant, T.E.; Glonek, T. 31P NMR of tissue phospholipids: Competition for Mg2+, Ca2+, Na+ and K+ cations. Lipids 1992, 27, 551–559. [Google Scholar] [CrossRef]


| (a) | ||||
|---|---|---|---|---|
| All | Mg ≤ 2.07 mg/dL | Mg > 2.07 mg/dL | p Value | |
| N = 396 (99.2%) | n = 181 (45.7%) | n = 215 (54.3%) | ||
| Age (years) | 56.34 (9.20) | 57.04 (9.65) | 55.75 (8.79) | 0.167 |
| Male sex | 229 (57.8) | 108 (59.7%) | 121 (56.3%) | 0.563 |
| Weight (kg) | 83.00 (16.63) | 83.60 (15.96) | 82.49 (17.19) | 0.508 |
| BMI (kg/m2) | 28.10 (4.91) | 28.21 (4.83) | 28.00 (4.99) | 0.67 |
| Smoking | 0.345 | |||
| Never smoker | 145 (36.6%) | 67 (37.0%) | 78 (36.3%) | |
| Ex-smoker | 171 (43.2%) | 83 (45.9%) | 88 (40.9%) | |
| Smoker | 80 (20.2%) | 31 (17.1%) | 49 (22.8%) | |
| Waist circumference (cm) | 98.56 (14.37) | 99.24 (14.17) | 98.00 (14.55) | 0.394 |
| Systolic BP (mmHg) | 120.54 (16.64) | 122.60 (16.31) | 118.81 (16.75) | 0.024 |
| Diastolic BP (mmHg) | 75.24 (9.99) | 75.93 (9.67) | 74.67 (10.24) | 0.514 |
| Physically active | 237 (59.8%) | 112 (61.9%) | 125 (58.1%) | 0.523 |
| Hypertension | 133 (33.6%) | 65 (35.9%) | 68 (31.6%) | 0.428 |
| Glucose (mg/dl) | 104.31 (22.63) | 107.36 (25.04) | 101.74 (20.08) | 0.014 |
| HbA1c (%) | 5.57 (0.72) | 5.63 (0.74) | 5.52 (0.71) | 0.121 |
| Diabetes | 0.022 | |||
| No | 242 (61.1%) | 105 (58.0%) | 137 (63.7%) | |
| Prediabetes | 102 (25.8%) | 43 (23.8%) | 59 (27.4%) | |
| Diabetes | 52 (13.1%) | 33 (18.2%) | 19 (8.8%) | |
| Total cholesterol (mg/dl) | 218.05 (36.31) | 215.12 (34.54) | 220.51 (37.65) | 0.141 |
| HDL-C (mg/dl) | 62.00 (17.68) | 62.14 (17.62) | 61.89 (17.76) | 0.888 |
| LDL-C (mg/dl) | 139.68 (32.98) | 136.71 (31.51) | 142.17 (34.04) | 0.101 |
| Triglycerides (mg/dl) | 131.41 (85.12) | 133.42 (92.51) | 129.73 (78.54) | 0.668 |
| eGFR (ml/min/1.73 m2) | 86.62 (12.96) | 86.18 (13.13) | 87.00 (12.83) | 0.531 |
| Serum potassium (mmol/L) | 4.29 (0.28) | 4.30 (0.29) | 4.27 (0.28) | 0.298 |
| Serum phosphate (mmol/L) | 1.04 (0.15) | 1.04 (0.15) | 1.05 (0.15) | 0.4 |
| Diabetic medication | 30 (7.6%) | 23 (12.7%) | 7 (3.3%) | 0.001 |
| Antihypertensive medication | 100 (25.3%) | 49 (27.1%) | 51 (23.7%) | 0.517 |
| Lipid lowering medication | 42 (10.6%) | 21 (11.6%) | 21 (9.8%) | 0.669 |
| Diuretics medication | 54 (13.6%) | 23 (12.7%) | 31(14.4%) | 0.728 |
| Anticoagulant therapy | 8 (2.0%) | 4 (2.2%) | 4 (1.9%) | 1 |
| (b) | ||||
| All | Dietary Mg ≤ 155.2 mg/1000 kcal/day | Dietary Mg > 155.2 mg/1000 kcal/day | p Value | |
| N = 311 (77.9%) | n = 154 (49.5%) | n = 157 (50.5%) | ||
| Age (years) | 56.39 (9.10) | 55.86 (9.23) | 56.91 (8.97) | 0.311 |
| Male sex | 175 (56.3%) | 118 (76.6%) | 57 (36.3%) | <0.001 |
| Weight (kg) | 82.23 (16.60) | 85.79 (15.81) | 78.74 (16.67) | <0.001 |
| BMI (kg/m2) | 27.95 (4.97) | 28.19 (4.64) | 27.71 (5.27) | 0.394 |
| Smoking | 0.495 | |||
| Never smoker | 115 (37.0%) | 52 (33.8%) | 63 (40.1%) | |
| Ex-smoker | 136 (43.7%) | 70 (45.5%) | 66 (42.0%) | |
| Smoker | 60 (19.3%) | 32 (20.8%) | 28 (17.8%) | |
| Waist circumference (cm) | 97.99 (14.56) | 100.86 (13.90) | 95.18 (14.69) | 0.001 |
| Systolic BP (mmHg) | 120.05 (16.36) | 123.13 (16.31) | 117.02 (15.89) | 0.001 |
| Diastolic BP (mmHg) | 74.80 (9.90) | 76.30 (9.97) | 73.34 (9.64) | 0.008 |
| Physically active | 189 (60.8%) | 88 (57.1%) | 101 (64.3%) | 0.237 |
| Hypertension | 108 (34.7%) | 60 (39.0%) | 48 (30.6%) | 0.151 |
| Glucose (mg/dl) | 103.44 (18.28) | 105.61 (20.96) | 101.31 (14.96) | 0.038 |
| HbA1c (%) | 5.53 (0.59) | 5.56 (0.63) | 5.51 (0.54) | 0.438 |
| Diabetes | 0.531 | |||
| No | 192 (61.7%) | 93 (60.4%) | 99 (63.1%) | |
| Prediabetes | 83 (26.7%) | 40 (26.0%) | 43 (27.4%) | |
| Diabetes | 36 (11.6%) | 21 (13.6%) | 15 (9.6%) | |
| Total cholesterol (mg/dl) | 217.67 (36.18) | 216.32 (37.37) | 218.89 (35.05) | 0.532 |
| HDL-C (mg/dl) | 62.63 (17.82) | 58.89 (16.89) | 66.29 (18.00) | <0.001 |
| LDL-C (mg/dl) | 139.31 (33.50) | 139.25 (34.12) | 139.36 (32.99) | 0.977 |
| Triglycerides (mg/dl) | 127.65 (79.43) | 144.12 (97.15) | 111.49 (52.43) | <0.001 |
| eGFR (ml/min/1.73 m2) | 86.63 (13.10) | 86.98 (13.34) | 86.28 (12.88) | 1 |
| Energy intake (kcal/day) | 1841.53 (414.39) | 2004.73 (383.37) | 1681.45 (380.79) | <0.001 |
| Dietary calcium (mg/day) | 763.29 (205.97) | 739.29 (193.76) | 786.83 (215.30) | <0.001 |
| Dietary potassium (mg/day) | 2532.28 (503.22) | 2515.33 (470.74) | 2548.91 (534.16) | 0.557 |
| Dietary phosphate (mg/day) | 1111.75 (263.84) | 1130.93 (244.04) | 1092.94 (281.43) | 0.205 |
| Diabetic medication | 23 (7.4%) | 13 (8.4%) | 10 (6.4%) | 0.630 |
| Antihypertensive medication | 84 (27.0%) | 45 (29.2%) | 39 (24.8%) | 0.458 |
| Lipid lowering medication | 34 (10.9%) | 21 (13.6%) | 13 (8.3%) | 0.183 |
| Diuretics medication | 49 (15.8%) | 22 (14.3%) | 27 (17.2%) | 0.583 |
| Anticoagulant therapy | 8 (2.6%) | 4 (2.6%) | 4 (2.5%) | 1 |
| (a) | ||||
|---|---|---|---|---|
| All | Mg ≤ 2.07 mg/dL | Mg > 2.07 mg/dL | p Value | |
| Left Ventricular Function | N = 366 (91.7%) | n = 168 (45.9%) | n = 198 (54.1%) | |
| Early diastolic filling rate (mL/s) | 226.11 (115.89) | 223.95 (115.97) | 227.93 (116.09) | 0.744 |
| Late diastolic filling rate (mL/s) | 225.90 (109.28) | 223.95 (113.18) | 227.56 (106.11) | 0.754 |
| End diastolic volume (mL/m2) | 66.14 (14.90) | 66.50 (16.21) | 65.84 (13.73) | 0.673 |
| End systolic volume (mL/m2) | 20.73 (8.65) | 20.87 (9.67) | 20.60 (7.70) | 0.764 |
| Stroke volume (mL/m2) | 45.43 (9.42) | 45.65 (10.06) | 45.24 (8.85) | 0.682 |
| Cardiac output (mL/min/m2) | 3009.05 (586.74) | 3050.06 (617.36) | 2974.25 (558.66) | 0.219 |
| Ejection fraction (%) | 69.37 (7.78) | 69.52 (8.45) | 69.25 (7.18) | 0.741 |
| Peak ejection rate (mL/s) | 354.70 (132.64) | 352.74 (136.76) | 356.36 (129.37) | 0.795 |
| Myocardial mass (g/m2) | 71.46 (13.37) | 72.46 (13.80) | 70.61 (12.97) | 0.188 |
| LGE | 11 (3.0%) | 3 (1.8%) | 8 (4.0%) | 0.341 |
| Remodeling index (g/mL/m2) | 0.58 (0.15) | 0.59 (0.17) | 0.57 (0.14) | 0.418 |
| Mean diastolic thickness (mm/m2) | 4.85 (0.67) | 4.88 (0.72) | 4.82 (0.61) | 0.33 |
| Right ventricular function | N = 336 (84.2%) | n = 85 (25.3%) | n = 251 (74.7%) | |
| End diastolic volume (mL/m2) | 84.72 (17.46) | 87.63 (18.54) | 83.73 (17.00) | 0.075 |
| End systolic volume (mL/m2) | 40.33 (11.78) | 42.70 (12.16) | 39.52 (11.56) | 0.031 |
| Stroke volume (mL/m2) | 44.43 (9.11) | 44.95 (9.45) | 44.25 (9.00) | 0.539 |
| Cardiac output (mL/min/m2) | 2938.74 (574.20) | 3004.43 (575.29) | 2916.49 (573.27) | 0.223 |
| Ejection fraction (%) | 52.85 (7.01) | 51.80 (6.74) | 53.21 (7.08) | 0.109 |
| Carotid plaque | N = 248 (62.2%) | n = 76 (30.6%) | n = 172 (69.4%) | |
| Presence of plaque | 50 (20.2%) | 12 (15.8%) | 38 (22.1) | 0.333 |
| Presence of plaque type | 0.416 | |||
| AHA type I | 198 (79.8%) | 64 (84.2%) | 134 (77.9) | |
| AHA type III | 34 (13.7%) | 7 (9.2%) | 27 (15.7) | |
| AHA type V | 10 (4.0%) | 4 (5.3%) | 6 (3.5) | |
| AHA type VI or VII | 6 (2.4%) | 1 (1.3%) | 5 (2.9) | |
| Wall thickness left (mm) | 0.75 (0.11) | 0.76 (0.13) | 0.74 (0.10) | 0.112 |
| Wall thickness right (mm) | 0.76 (0.10) | 0.78 (0.10) | 0.75 (0.10) | 0.018 |
| (b) | ||||
| All | Dietary Mg ≤ 155.2 mg/1000 kcal/day | Dietary Mg > 155.2 mg/1000 kcal/day | p Value | |
| Left Ventricular Function | N = 287 (91.8%) | n = 141 (49.1%) | n = 146 (50.9%) | |
| Early diastolic filling rate (mL/s) | 229.48 (115.39) | 226.99 (110.31) | 231.87 (120.42) | 0.721 |
| Late diastolic filling rate (mL/s) | 227.74 (110.88) | 226.97 (118.89) | 228.48 (102.96) | 0.908 |
| End diastolic volume (mL/m2) | 66.65 (14.81) | 65.83 (14.37) | 67.45 (15.23) | 0.355 |
| End systolic volume (mL/m2) | 20.73 (8.08) | 20.48 (7.81) | 20.97 (8.35) | 0.607 |
| Stroke volume (mL/m2) | 45.94 (9.43) | 45.38 (9.17) | 46.47 (9.67) | 0.327 |
| Cardiac output (mL/min/m2) | 3041.45 (574.70) | 3047.67 (561.30) | 3035.44 (589.22) | 0.857 |
| Ejection fraction (%) | 69.53 (7.27) | 69.46 (6.93) | 69.60 (7.61) | 0.875 |
| Peak ejection rate (mL/s) | 356.40 (133.62) | 361.26 (136.96) | 351.71 (130.61) | 0.546 |
| Myocardial mass (g/m2) | 70.71 (12.72) | 73.57 (12.56) | 67.94 (12.29) | <0.001 |
| LGE | 9 (3.1%) | 3 (2.1%) | 6 (4.1%) | 0.532 |
| Remodeling index (g/mL/m2) | 0.57 (0.14) | 0.58 (0.15) | 0.56 (0.13) | 0.091 |
| Mean diastolic thickness (mm/m2) | 4.81 (0.63) | 4.88 (0.65) | 4.75 (0.61) | 0.090 |
| Right ventricular function | N = 263 (84.0%) | n = 128 (48.7%) | n = 135 (51.3%) | |
| End diastolic volume (mL/m2) | 85.66 (17.65) | 85.92 (17.27) | 85.41 (18.07) | 0.817 |
| End systolic volume (mL/m2) | 40.52 (12.03) | 41.36 (11.94) | 39.72 (12.10) | 0.271 |
| Stroke volume (mL/m2) | 45.18 (9.00) | 44.58 (8.65) | 45.74 (9.32) | 0.296 |
| Cardiac output (mL/min/m2) | 2974.97 (574.37) | 3000.75 (561.10) | 2950.51 (587.71) | 0.118 |
| Ejection fraction (%) | 53.21 (6.89) | 52.37 (6.83) | 54.01 (6.88) | <0.001 |
| Carotid plaque | N = 188 (60.1%) | n = 100 (53.2%) | n = 88 (46.8%) | |
| Presence of plaque | 41 (21.8%) | 23 (23.0%) | 18 (20.5%) | 0.807 |
| Presence of plaque type | 0.265 | |||
| AHA type I | 147 (78.2%) | 77 (77.0%) | 70 (79.5%) | |
| AHA type III | 28 (14.9%) | 15 (15.0%) | 13 (14.8%) | |
| AHA type V | 7 (3.7%) | 6 (6.0%) | 1 (1.1%) | |
| AHA type VI or VII | 6 (3.2%) | 2 (2.0%) | 4 (4.5%) | |
| Wall thickness left (mm) | 0.75 (0.11) | 0.75 (0.12) | 0.74 (0.10) | 0.463 |
| Wall thickness right (mm) | 0.76 (0.10) | 0.76 (0.10) | 0.75 (0.11) | 0.248 |
| Serum Magnesium | Dietary Magnesium | |||||
|---|---|---|---|---|---|---|
| Estimate | 95% CI | p Value | Estimate | 95% CI | p Value | |
| Left Ventricular Function | N = 366 | N = 287 | ||||
| Early diastolic filling rate (mL/s) | −3.29 | (−14.24, 7.67) | 0.556 | 0.17 | (−0.217, 0.556) | 0.388 |
| Late diastolic filling rate (mL/s) | −0.18 | (−11.17, 10.81) | 0.975 | 0.05 | (−0.347, 0.453) | 0.794 |
| End diastolic volume (mL/m2) | −0.86 | (−2.32, 0.58) | 0.239 | 0.06 | (0.014, 0.114) | 0.013 |
| End systolic volume (mL/m2) | −0.07 | (−0.94, 0.79) | 0.871 | 0.04 | (0.008, 0.065) | 0.011 |
| Stroke volume (mL/m2) | −0.81 | (−1.72, 0.10) | 0.082 | 0.03 | (−0.006, 0.059) | 0.104 |
| Cardiac output (mL/min/m2) | −52.73 | (−111.58, 6.11) | 0.078 | 1.42 | (−0.631, 3.471) | 0.174 |
| Ejection fraction (%) | −0.38 | (−1.16, 0.41) | 0.341 | −0.02 | (−0.048, 0.004) | 0.101 |
| Peak ejection rate (mL/s) | 5.38 | (−7.66, 18.42) | 0.418 | −0.22 | (−0.685, 0.253) | 0.365 |
| Myocardial mass (g/m2) | 0.003 | (−1.17, 1.18) | 0.995 | −0.01 | (−0.052, 0.028) | 0.546 |
| LGE | OR 3.06 | (1.27, 8.32) | 0.018 | OR 1.01 | (0.988, 1.036) | 0.434 |
| Remodeling index (g/mL/m2) | 0.005 | (−0.009, 0.019) | 0.479 | −0.001 | (−0.001. −0.0002) | 0.004 |
| Mean diastolic thickness (mm/m2) | 0.02 | (−0.04, 0.08) | 0.565 | −0.002 | (−0.004, −0.0002) | 0.029 |
| Right ventricular function | (N = 336) | (N = 236) | ||||
| End diastolic volume (mL/m2) | −1.74 | (−3.50, 0.02) | 0.053 | 0.05 | (−0.011, 0.114) | 0.105 |
| End systolic volume (mL/m2) | −1.21 | (−2.39, −0.04) | 0.043 | 0.03 | (−0.011, 0.071) | 0.171 |
| Stroke volume (mL/m2) | −0.53 | (−1.47, 0.41) | 0.268 | 0.02 | (−0.011, 0.056) | 0.187 |
| Cardiac output (mL/min/m2) | −32.62 | (−93.93, 28.70) | 0.296 | 1.51 | (−0.852, 3.474) | 0.169 |
| Ejection fraction (%) | 0.33 | (−0.38, 1.04) | 0.362 | −0.01 | (−0.034, 0.014) | 0.441 |
| Carotid plaque | (N = 248) | (N = 188) | ||||
| Presence of plaque | OR 1.62 | (1.07, 2.56) | 0.033 | OR 0.99 | (0.975,1.000) | 0.056 |
| Presence of plaque type | OR 1.58 | (1.19, 2.11) | 0.002 | OR 0.99 | (0.980, 0.996) | 0.004 |
| Wall thickness left (mm) | −0.003 | (−0.016, 0.009) | 0.66 | −0.0001 | (−0.0006, 0.0003) | 0.562 |
| Wall thickness right (mm) | −0.008 | (−0.019, 0.004) | 0.211 | −0.0001 | (−0.0006, 0.0002) | 0.381 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shugaa Addin, N.; Schlett, C.L.; Bamberg, F.; Thorand, B.; Linseisen, J.; Seissler, J.; Peters, A.; Rospleszcz, S. Subclinical Cardiovascular Disease Markers in Relation to Serum and Dietary Magnesium in Individuals from the General Population: The KORA-MRI Study. Nutrients 2022, 14, 4954. https://doi.org/10.3390/nu14234954
Shugaa Addin N, Schlett CL, Bamberg F, Thorand B, Linseisen J, Seissler J, Peters A, Rospleszcz S. Subclinical Cardiovascular Disease Markers in Relation to Serum and Dietary Magnesium in Individuals from the General Population: The KORA-MRI Study. Nutrients. 2022; 14(23):4954. https://doi.org/10.3390/nu14234954
Chicago/Turabian StyleShugaa Addin, Nuha, Christopher L. Schlett, Fabian Bamberg, Barbara Thorand, Jakob Linseisen, Jochen Seissler, Annette Peters, and Susanne Rospleszcz. 2022. "Subclinical Cardiovascular Disease Markers in Relation to Serum and Dietary Magnesium in Individuals from the General Population: The KORA-MRI Study" Nutrients 14, no. 23: 4954. https://doi.org/10.3390/nu14234954
APA StyleShugaa Addin, N., Schlett, C. L., Bamberg, F., Thorand, B., Linseisen, J., Seissler, J., Peters, A., & Rospleszcz, S. (2022). Subclinical Cardiovascular Disease Markers in Relation to Serum and Dietary Magnesium in Individuals from the General Population: The KORA-MRI Study. Nutrients, 14(23), 4954. https://doi.org/10.3390/nu14234954







