Phase Angle Association with Dietary Habits and Metabolic Syndrome in Diabetic Hypertensive Patients: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
- Central adiposity defined as waist circumference (WC) ≥ 94 cm for European males and ≥ 80 cm for European females;
- Fasting blood glucose (FBG) ≥ 5.6 mmol/L or diagnosed diabetes;
- HDL cholesterol < 40 mg/dL (males) and < 50 mg/dL (females) or treatment for low HDL concentration;
- Serum TG > 150 mg/dL or treatment for hypertriglyceridemia;
- Blood pressure (BP) > 130/85 mmHg or treatment for hypertension.
2.2. Body Composition, Anthropometric and Blood Pressure, and Arterial Stiffness Measurement
2.3. Lifestyle Questionnaire and Mediterranean Diet Serving Score
2.4. Medical History and Clinical and Laboratory Parameters
2.5. Statistical Analysis
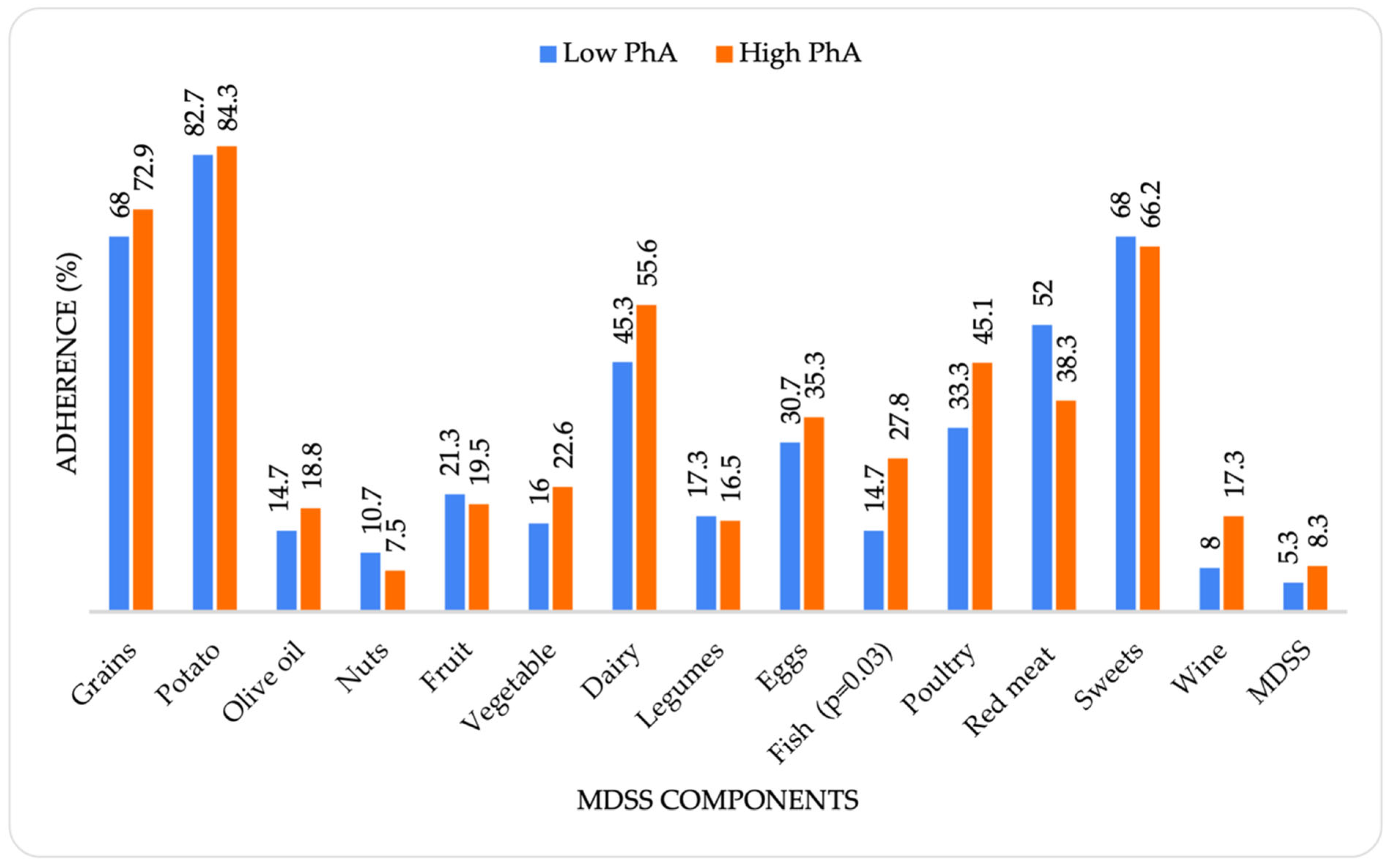
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cordain, L.; Eaton, S.B.; Sebastian, A.; Mann, N.; Lindeberg, S.; Watkins, B.A.; O’Keefe, J.H.; Brand-Miller, J. Origins and evolution of the Western diet: Health implications for the 21st century. Am. J. Clin. Nutr. 2005, 81, 341–354. [Google Scholar] [CrossRef] [Green Version]
- Kassi, E.; Pervanidou, P.; Kaltsas, G.; Chrousos, G. Metabolic syndrome: Definitions and controversies. BMC Med. 2011, 9, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Regufe, V.M.G.; Pinto, C.M.C.B.; Perez, P.M.V.H.C. Metabolic syndrome in type 2 diabetic patients: A review of current evidence. Porto Biomed. J. 2020, 5, e101. [Google Scholar] [CrossRef]
- Achari, A.; Jain, S. Adiponectin, a Therapeutic Target for Obesity, Diabetes, and Endothelial Dysfunction. Int. J. Mol. Sci. 2017, 18, 1321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdel-Daim, M.M.; El-Tawil, O.S.; Bungau, S.G.; Atanasov, A.G. Applications of Antioxidants in Metabolic Disorders and Degenerative Diseases: Mechanistic Approach. Oxid. Med. Cell. Longev. 2019, 2019, 4179676. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdel-Daim, M.M.; Zakhary, N.I.; Aleya, L.; Bungǎu, S.G.; Bohara, R.A.; Siddiqi, N.J. Aging, Metabolic, and Degenerative Disorders: Biomedical Value of Antioxidants. Oxid. Med. Cell. Longev. 2018, 2018, 2098123. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Zhong, J.; Ruan, Y.; Zhang, Z.; Sun, J.; Chen, H. The association between fat-to-muscle ratio and metabolic disorders in type 2 diabetes. Diabetol. Metab. Syndr. 2021, 13, 129. [Google Scholar] [CrossRef] [PubMed]
- Pi-Sunyer, X. Changes in body composition and metabolic disease risk. Eur. J. Clin. Nutr. 2019, 73, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Curvello-Silva, K.; Ramos, L.B.; Sousa, C.; Daltro, C. Phase angle and metabolic parameters in severely obese patients. Nutr. Hosp. 2020, 37, 1130–1134. [Google Scholar] [CrossRef] [PubMed]
- Norman, K.; Stobäus, N.; Zocher, D.; Bosy-Westphal, A.; Szramek, A.; Scheufele, R.; Smoliner, C.; Pirlich, M. Cutoff percentiles of bioelectrical phase angle predict functionality, quality of life, and mortality in patients with cancer. Am. J. Clin. Nutr. 2010, 92, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Dittmar, M.; Reber, H.; Kahaly, G.J. Bioimpedance phase angle indicates catabolism in Type 2 diabetes. Diabet. Med. 2015, 32, 1177–1185. [Google Scholar] [CrossRef] [PubMed]
- de Luis, D.A.; Aller, R.; Romero, E.; Dueñas, A.; Perez Castrillon, J.L. Relation of phase angle tertiles with blood adipocytokines levels, insulin resistance and cardiovascular risk factors in obese women patients. Eur. Rev. Med. Pharmacol. Sci. 2010, 14, 521–526. [Google Scholar] [PubMed]
- Xu, Y.; Xie, X.; Duan, Y.; Wang, L.; Cheng, Z.; Cheng, J. A review of impedance measurements of whole cells. Biosens. Bioelectron. 2016, 77, 824–836. [Google Scholar] [CrossRef] [PubMed]
- Barbosa-Silva, M.C.G.; Barros, A.J.; Wang, J.; Heymsfield, S.B.; Pierson, R.N. Bioelectrical impedance analysis: Population reference values for phase angle by age and sex. Am. J. Clin. Nutr. 2005, 82, 49–52. [Google Scholar] [CrossRef] [PubMed]
- Bosy-Westphal, A.; Danielzik, S.; Dörhöfer, R.-P.; Later, W.; Wiese, S.; Müller, M.J. Phase Angle From Bioelectrical Impedance Analysis: Population Reference Values by Age, Sex, and Body Mass Index. J. Parenter. Enter. Nutr. 2006, 30, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Stobäus, N.; Pirlich, M.; Valentini, L.; Schulzke, J.D.; Norman, K. Determinants of bioelectrical phase angle in disease. Br. J. Nutr. 2012, 107, 1217–1220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longo, G.Z.; Silva, D.A.S.; Gabiatti, M.P.; Martins, P.C.; Hansen, F. Phase angle association with metabolic profile in adults: A population-based study. Nutrition 2021, 90, 111233. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.-N.; Kim, K.-A.; Kim, Y.-S.; Yim, J.-E. Independent Association of Phase Angle with Fasting Blood Glucose and Hemoglobin A1c in Korean Type 2 Diabetes Patients. Clin. Nutr. Res. 2020, 9, 205. [Google Scholar] [CrossRef] [PubMed]
- de França, N.A.G.; Callegari, A.; Gondo, F.F.; Corrente, J.E.; Mclellan, K.C.P.; Burini, R.C.; de Oliveira, E.P. Higher dietary quality and muscle mass decrease the odds of low phase angle in bioelectrical impedance analysis in Brazilian individuals. Nutr. Diet. 2016, 73, 474–481. [Google Scholar] [CrossRef]
- Barrea, L.; Muscogiuri, G.; Macchia, P.; Di Somma, C.; Falco, A.; Savanelli, M.; Colao, A.; Savastano, S. Mediterranean Diet and Phase Angle in a Sample of Adult Population: Results of a Pilot Study. Nutrients 2017, 9, 151. [Google Scholar] [CrossRef] [PubMed]
- Mc780—User Manual. Available online: https://tanita.eu/media/wysiwyg/manuals/medical-approved-body-composition-monitors/mc-780-portable-instruction-manual.pdf (accessed on 12 December 2019).
- Monteagudo, C.; Mariscal-Arcas, M.; Rivas, A.; Lorenzo-Tovar, M.L.; Tur, J.A.; Olea-Serrano, F. Proposal of a mediterranean diet serving score. PLoS ONE 2015, 10, e0128594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [Green Version]
- Barrea, L.; Muscogiuri, G.; Laudisio, D.; Di Somma, C.; Salzano, C.; Pugliese, G.; De Alteriis, G.; Colao, A.; Savastano, S. Phase Angle: A Possible Biomarker to Quantify Inflammation in Subjects with Obesity and 25(OH)D Deficiency. Nutrients 2019, 11, 1747. [Google Scholar] [CrossRef] [Green Version]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean diet and health status: Meta-analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panagiotakos, D.B.; Polystipioti, A.; Papairakleous, N.; Polychronopoulos, E. Long-term adoption of a Mediterranean diet is associated with a better health status in elderly people; a cross-sectional survey in Cyprus. Asia Pac. J. Clin. Nutr. 2007, 16, 331–337. [Google Scholar]
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021; Available online: https://www.diabetesatlas.org (accessed on 21 September 2022).
- Akamatsu, Y.; Kusakabe, T.; Arai, H.; Yamamoto, Y.; Nakao, K.; Ikeue, K.; Ishihara, Y.; Tagami, T.; Yasoda, A.; Ishii, K.; et al. Phase angle from bioelectrical impedance analysis is a useful indicator of muscle quality. J. Cachexia Sarcopenia Muscle 2022, 13, 180–189. [Google Scholar] [CrossRef]
- Dittmar, M. Reliability and variability of bioimpedance measures in normal adults: Effects of age, gender, and body mass. Am. J. Phys. Anthropol. 2003, 122, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Mullie, L.; Obrand, A.; Bendayan, M.; Trnkus, A.; Ouimet, M.; Moss, E.; Chen-Tournoux, A.; Rudski, L.G.; Afilalo, J. Phase Angle as a Biomarker for Frailty and Postoperative Mortality: The BICS Study. J. Am. Heart Assoc. 2018, 7, e008721. [Google Scholar] [CrossRef] [PubMed]
- Jaremków, A.; Markiewicz-Górka, I.; Hajdusianek, W.; Gać, P. Relationships between Body Composition Parameters and Phase Angle as Related to Lifestyle among Young People. J. Clin. Med. 2021, 11, 80. [Google Scholar] [CrossRef]
- Gonzalez, M.C.; Barbosa-Silva, T.G.; Bielemann, R.M.; Gallagher, D.; Heymsfield, S.B. Phase angle and its determinants in healthy subjects: Influence of body composition. Am. J. Clin. Nutr. 2016, 103, 712–716. [Google Scholar] [CrossRef] [Green Version]
- Siddiqui, N.I. Anthropometric Predictors of Bio- Impedance Analysis (BIA) Phase Angle in Healthy Adults. J. Clin. Diagn. Res. 2016, 10, CC01. [Google Scholar] [CrossRef] [PubMed]
- Dodig Novaković, M.; Lovrić Kojundžić, S.; Radić, M.; Vučković, M.; Gelemanović, A.; Roguljić, M.; Kovačević, K.; Orešković, J.; Radić, J. Number of Teeth and Nutritional Status Parameters Are Related to Intima-Media Thickness in Dalmatian Kidney Transplant Recipients. J. Pers. Med. 2022, 12, 984. [Google Scholar] [CrossRef]
- Langer, R.D.; Larsen, S.C.; Ward, L.C.; Heitmann, B.L. Phase angle measured by bioelectrical impedance analysis and the risk of cardiovascular disease among adult Danes. Nutrition 2021, 89, 111280. [Google Scholar] [CrossRef]
- Brown, A.; Guess, N.; Dornhorst, A.; Taheri, S.; Frost, G. Insulin-associated weight gain in obese type 2 diabetes mellitus patients: What can be done? Diabetes Obes. Metab. 2017, 19, 1655–1668. [Google Scholar] [CrossRef] [PubMed]
- Russell-Jones, D.; Khan, R. Insulin-associated weight gain in diabetes--causes, effects and coping strategies. Diabetes Obes. Metab. 2007, 9, 799–812. [Google Scholar] [CrossRef]
- Verissimo, T.; Faivre, A.; Rinaldi, A.; Lindenmeyer, M.; Delitsikou, V.; Veyrat-Durebex, C.; Heckenmeyer, C.; Fernandez, M.; Berchtold, L.; Dalga, D.; et al. Decreased Renal Gluconeogenesis Is a Hallmark of Chronic Kidney Disease. J. Am. Soc. Nephrol. 2022, 33, 810–827. [Google Scholar] [CrossRef]
- Pina, A.F.; Borges, D.O.; Meneses, M.J.; Branco, P.; Birne, R.; Vilasi, A.; Macedo, M.P. Insulin: Trigger and Target of Renal Functions. Front. Cell Dev. Biol. 2020, 8, 519. [Google Scholar] [CrossRef] [PubMed]
- Zha, Y.; Qian, Q. Protein Nutrition and Malnutrition in CKD and ESRD. Nutrients 2017, 9, 208. [Google Scholar] [CrossRef]
- Panjeta, M.; Tahirović, I.; Sofić, E.; Ćorić, J.; Dervišević, A. Interpretation of Erythropoietin and Haemoglobin Levels in Patients with Various Stages of Chronic Kidney Disease. J. Med. Biochem. 2017, 36, 145–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohammed, M.A.; Sharew, N.T. Adherence to dietary recommendation and associated factors among diabetic patients in Ethiopian teaching hospitals. Pan Afr. Med. J. 2019, 33, 260. [Google Scholar] [CrossRef] [PubMed]
- Adriouch, S.; Lelong, H.; Kesse-Guyot, E.; Baudry, J.; Lampuré, A.; Galan, P.; Hercberg, S.; Touvier, M.; Fezeu, L. Compliance with Nutritional and Lifestyle Recommendations in 13,000 Patients with a Cardiometabolic Disease from the Nutrinet-Santé Study. Nutrients 2017, 9, 546. [Google Scholar] [CrossRef]
- Ahola, A.J.; Groop, P.-H. Barriers to self-management of diabetes. Diabet. Med. 2013, 30, 413–420. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015; ISBN 9789241565042. [Google Scholar]
- Zarei, M.; Qorbani, M.; Djalalinia, S.; Sulaiman, N.; Subashini, T.; Appanah, G.; Naderali, E. Food Insecurity and Dietary Intake Among Elderly Population: A Systematic Review. Int. J. Prev. Med. 2021, 12, 8. [Google Scholar] [CrossRef]
- Park, C.; Pagnini, F.; Langer, E. Glucose metabolism responds to perceived sugar intake more than actual sugar intake. Sci. Rep. 2020, 10, 15633. [Google Scholar] [CrossRef]
- Madden, M.; Morris, S.; Stewart, D.; Atkin, K.; Gough, B.; McCambridge, J. Conceptualising alcohol consumption in relation to long-term health conditions: Exploring risk in interviewee accounts of drinking and taking medications. PLoS ONE 2019, 14, e0224706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rondanelli, M.; Rigon, C.; Perna, S.; Gasparri, C.; Iannello, G.; Akber, R.; Alalwan, T.A.; Freije, A.M. Novel Insights on Intake of Fish and Prevention of Sarcopenia: All Reasons for an Adequate Consumption. Nutrients 2020, 12, 307. [Google Scholar] [CrossRef] [Green Version]
- Alhussain, M.H.; ALshammari, M.M. Association Between Fish Consumption and Muscle Mass and Function in Middle-Age and Older Adults. Front. Nutr. 2021, 8, 746880. [Google Scholar] [CrossRef]
- Musiał, K.; Wiski, M.; Lipert, A. Protein intake among healthy adults undertaking regular muscle strength training. Med. Sci. Pulse 2020, 14, 23–29. [Google Scholar] [CrossRef]
- Hernández-Díazcouder, A.; Romero-Nava, R.; Carbó, R.; Sánchez-Lozada, L.G.; Sánchez-Muñoz, F. High Fructose Intake and Adipogenesis. Int. J. Mol. Sci. 2019, 20, 2787. [Google Scholar] [CrossRef] [PubMed]


| Total (n = 208) | Low Phase Angle (n = 75) | High Phase Angle (n = 133) | p-Value * | |
|---|---|---|---|---|
| Age (years), median (IQR) | 68 (60–73) | 72 (65–76) | 65 (57–71) | <0.001 |
| Sex, M/F | 117/91 | 28/47 | 89/44 | <0.001 |
| Duration of DM treatment (years), median (IQR) | 10 (4.75–20) | 10 (5.75–20) | 10 (3–20) | 0.84 |
| Duration of AH treatment (years), median (IQR) | 10 (5–20) | 15 (6–20) | 10 (5–20) | 0.27 |
| Smoking, N (%) | 43 (20.7) | 15 (20) | 28 (21.1) | 0.74 |
| pSBP (mmHg), median (IQR) | 146 (134–160.5) | 149.5 (131.5–162) | 144 (134–160) | 0.41 |
| pDBP (mmHg), median (IQR) | 91 (80–100) | 89.5 (74–96.5) | 93 (82.5–101.5) | 0.04 |
| PWV (m/s), median (IQR) | 10.45 (9–11.8) | 11.2 (10.1–12.05) | 10 (8.68–11.43) | 0.006 |
| Pharmacological therapy | ||||
| BBs, N (%) | 97 (46.6) | 38 (52.1) | 59 (46.8) | 0.48 |
| ACE inhibitors, N (%) | 106 (51) | 32 (43.8) | 74 (58.7) | 0.04 |
| ARBs, N (%) | 31 (14.9) | 14 (19.2) | 17 (13.6) | 0.30 |
| Cas, N (%) | 114 (54.8) | 41 (56.2) | 73 (57.9) | 0.81 |
| Diuretics, N (%) | 137 (65.9) | 49 (67.1) | 88 (69.8) | 0.69 |
| Moxonidine, N (%) | 52 (25) | 15 (20.5) | 37 (29.4) | 0.17 |
| Urapidil, N (%) | 17 (8.2) | 6 (8.2) | 11 (8.8) | 0.89 |
| Oral antidiabetics, N (%) | 148 (71.2) | 63 (86.3) | 85 (67.5) | 0.003 |
| Insulin, N (%) | 51 (24.5) | 11 (15.1) | 40 (31.7) | 0.009 |
| Statin, N (%) | 101 (48.6) | 37 (50.7) | 64 (50.8) | 0.99 |
| Body composition | ||||
| Body fat (%), median (IQR) | 29.05 (23.6–36.55) | 30.5 (24.6–38.3) | 28 (22.95–34.65) | 0.04 |
| Body fat (kg), median (IQR) | 27.45 (20.18–35.85) | 29.22 (19.4–35.4) | 25.8 (20.25–36.8) | 0.55 |
| Fat free mass (kg), median (IQR) | 65.55 (58.15–74.6) | 59.7 (53.7–68.7) | 67.7 (60.6–77.15) | <0.001 |
| Trunk fat mass (kg), median (IQR) | 14.3 (10.13–18.5) | 14.1 (10.1–18) | 14.5 (10.15–18.8) | 0.60 |
| Trunk fat mass (%), median (IQR) | 28.3 (22.5–33.6) | 28.4 (23.2–34) | 28.2 (22–32.55) | 0.43 |
| Muscle mass (%), median (IQR) | 67.5 (59.75–72.98) | 66 (58.6–71.7) | 68.3 (61.45–73.7) | 0.06 |
| Muscle mass (kg), median (IQR) | 62.25 (55.25–70.75) | 56.9 (51–65.3) | 64.3 (57.55–73.3) | <0.001 |
| Skeletal muscle mass (%), median (IQR) | 37.05 (29.98–41.48) | 33.1 (26.7–37.9) | 38.6 (34.3–42.5) | <0.001 |
| Skeletal muscle mass (kg), median (IQR) | 34.2 (26.8–39.8) | 27.7 (23.5–35.2) | 36.8 (31.1–42.35) | <0.001 |
| SMI, median (IQR) | 9.08 (8.1–10.14) | 8.4 (7.85–9.45) | 9.28 (8.47–10.44) | <0.001 |
| Metabolic age (years), median (IQR) | 61 (54.25–66.75) | 62 (56–69) | 59 (53–65.5) | 0.02 |
| Anthropometric parameters | ||||
| WHtR, median (IQR) | 0.63 (0.59–0.69) | 0.64 (0.58–0.69) | 0.63 (0.59–0.7) | 0.61 |
| WHR, median (IQR) | 0.96 (0.91–1.02) | 0.94 (0.9–1.01) | 0.98 (0.93–1.02) | 0.16 |
| MUAC (cm), median (IQR) | 32.55 (29.6–35.5) | 32 (29.5–34) | 33 (30–36) | 0.04 |
| WC (cm), median (IQR) | 111 (103–120) | 110 (101–119) | 111.7 (104–120.5) | 0.08 |
| BMI (kg/m2) as categories, N (%) | ||||
| 18.5–24.9, normal weight | 20 (9.6) | 11 (15) | 9 (7) | 0.18 |
| 25–29.9, overweight | 74 (35.6) | 25 (33) | 49 (37) | |
| ≥30, obese | 114 (54.8) | 39 (52) | 75 (56) | |
| Total (n = 208) | Low Phase Angle (n = 75) | High Phase Angle (n = 133) | p-Value * | |
|---|---|---|---|---|
| FBG (mmol/L), median (IQR) | 7.4 (6.3–8.88) | 7.45 (6.2–9.2) | 7.3 (6.33–8.78) | 0.87 |
| HbA1c (%), median (IQR) | 6.8 (6.3–7.7) | 6.6 (6.3–7.2) | 6.9 (6.3–7.9) | 0.06 |
| Alb (g/L), median (IQR) | 43 (40–46) | 42 (40–45.3) | 43.1 (40–46) | 0.65 |
| Total cholesterol (mmol/L), median (IQR) | 4.7 (4.1–5.75) | 4.6 (4–5.3) | 4.8 (4.1–5.8) | 0.37 |
| LDL (mmol/L), median (IQR) | 2.7 (2.1–3.4) | 2.6 (2.1–3.1) | 2.8 (2.08–3.5) | 0.18 |
| HDL (mmol/L), median (IQR) | 1.1 (0.9–1.3) | 1.1 (0.9–1.3) | 1.1 (0.9–1.3) | 0.77 |
| Tgl (mmol/L), median (IQR) | 1.9 (1.4–2.5) | 1.9 (1.6–2.36) | 1.9 (1.4–2.68) | 0.58 |
| Uric acid (mmol/L), median (IQR) | 414 (351–474) | 419 (365.25–466.75) | 405 (343–477) | 0.60 |
| E (×1012/L), mean (SD) | 4.66 (4.24–5.03) | 4.43 (4.02–5.03) | 4.7 (4.33–5.04) | 0.04 |
| Hb (g/L), median (IQR) | 136 (123–148) | 128 (113–143) | 139 (130–152) | <0.001 |
| MCV (fL), median (IQR) | 88.8 (85.9–91.93) | 88.2 (85.1–91.1) | 89 (86.3–92.8) | 0.11 |
| Creatinine (mmol/L), median (IQR) | 114 (78.25–161.75) | 129 (78–179) | 110 (78–154) | 0.23 |
| Estimated GF using CKD-EPI (mL/min/1.73 m2), median (IQR) | 53 (31–76.7) | 40.93 (27.65–70.15) | 57.2 (36.5–81.25) | 0.02 |
| ACR (mg/g), median (IQR) | 2.89 (0.72–12.71) | 1.69 (0.7–14.08) | 3.15 (0.75–13.28) | 0.69 |
| Proteinuria (mg/24 h), median (IQR) | 347 (97–1018) | 425 (86–1447) | 338.5 (99.75–944.5) | 0.61 |
| Albuminuria (mg/24 h), median (IQR) | 97.5 (18.75–770) | 149 (18–983) | 76.5 (22.25–594.5) | 0.56 |
| R | p-Value * | |
|---|---|---|
| Age (years) | −0.308 | <0.001 |
| Body fat (%) | −0.184 | 0.01 |
| Muscle mass (kg) | 0.388 | <0.001 |
| Muscle mass (%) | 0.194 | 0.01 |
| Fat-free mass (kg) | 0.393 | <0.001 |
| Skeletal muscle mass (kg) | 0.504 | <0.001 |
| Skeletal muscle mass (%) | 0.42 | <0.001 |
| SMI | 0.346 | <0.001 |
| WC (cm) | 0.147 | 0.04 |
| Metabolic age (years) | −0.184 | 0.01 |
| pDBP (mmHg) | 0.224 | 0.01 |
| E (×1012/L) | 0.187 | 0.02 |
| Hb (g/L) | 0.31 | <0.001 |
| HbA1c (%) | 0.16 | 0.04 |
| Estimated GF using CKD-EPI (mL/min/1.73 m2) | 0.169 | 0.02 |
| PWV (m/s) | −0.192 | 0.04 |
| Deli meats intake (frequency) | 0.203 | <0.001 |
| Eggs intake (frequency) | 0.147 | 0.03 |
| Cheese intake (frequency) | 0.147 | 0.03 |
| Fruit intake (frequency) | −0.166 | 0.02 |
| Red meat intake (MeDi adherence) | −0.141 | 0.04 |
| Adjusted for Age, Gender and BMI | |||
|---|---|---|---|
| Beta | p-Value | 95% CI | |
| Body fat (%) | −0.04 | 0.57 | 0.96 (0.85–1.09) |
| Fat-free mass (kg) | 0.09 | 0.52 | 1.09 (0.83–1.44) |
| Muscle mass (kg) | −0.07 | 0.24 | 0.93 (0.83–1.05) |
| Skeletal muscle mass (kg) | 0.16 | <0.001 | 1.18 (1.09–1.27) |
| MUAC (cm) | 0.18 | 0.03 | 1.20 (1.02–1.42) |
| HC (cm) | −0.04 | 0.27 | 0.96 (0.90–1.03) |
| pDBP (mmHg) | 0.01 | 0.33 | 1.01 (0.99–1.04) |
| PWV (m/s) | −0.01 | 0.96 | 0.99 (0.63–1.56) |
| Hb (g/L) | 0.03 | 0.01 | 1.03 (1.01–1.05) |
| HbA1c (%) | 0.37 | 0.04 | 1.45 (1.01–2.08) |
| ACE inhibitors | 0.48 | 0.15 | 1.62 (0.83–3.15) |
| Oral hypoglycemics | −0.81 | 0.08 | 0.45 (0.18–3.15) |
| Insulin | 0.62 | 0.16 | 1.86 (0.79–4.40) |
| Red meat intake (frequency) | 0.27 | 0.14 | 1.31 (0.92–1.86) |
| White meat intake (frequency) | 0.46 | 0.06 | 1.59 (0.98–2.59) |
| Fast food intake (frequency) | 0.38 | 0.10 | 1.46 (0.93–2.30) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bučan Nenadić, D.; Radić, J.; Kolak, E.; Vučković, M.; Novak, I.; Selak, M.; Radić, M. Phase Angle Association with Dietary Habits and Metabolic Syndrome in Diabetic Hypertensive Patients: A Cross-Sectional Study. Nutrients 2022, 14, 5058. https://doi.org/10.3390/nu14235058
Bučan Nenadić D, Radić J, Kolak E, Vučković M, Novak I, Selak M, Radić M. Phase Angle Association with Dietary Habits and Metabolic Syndrome in Diabetic Hypertensive Patients: A Cross-Sectional Study. Nutrients. 2022; 14(23):5058. https://doi.org/10.3390/nu14235058
Chicago/Turabian StyleBučan Nenadić, Dora, Josipa Radić, Ela Kolak, Marijana Vučković, Ivana Novak, Marija Selak, and Mislav Radić. 2022. "Phase Angle Association with Dietary Habits and Metabolic Syndrome in Diabetic Hypertensive Patients: A Cross-Sectional Study" Nutrients 14, no. 23: 5058. https://doi.org/10.3390/nu14235058





