Impact of Geriatric Nutritional Risk Index and Modified Creatinine Index Combination on Mortality in Hemodialysis Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Baseline Data Collection
2.3. Index Calculation
2.4. Follow-Up
2.5. Statistics
3. Results
3.1. Baseline Characteristics
3.2. Clinical Outcomes
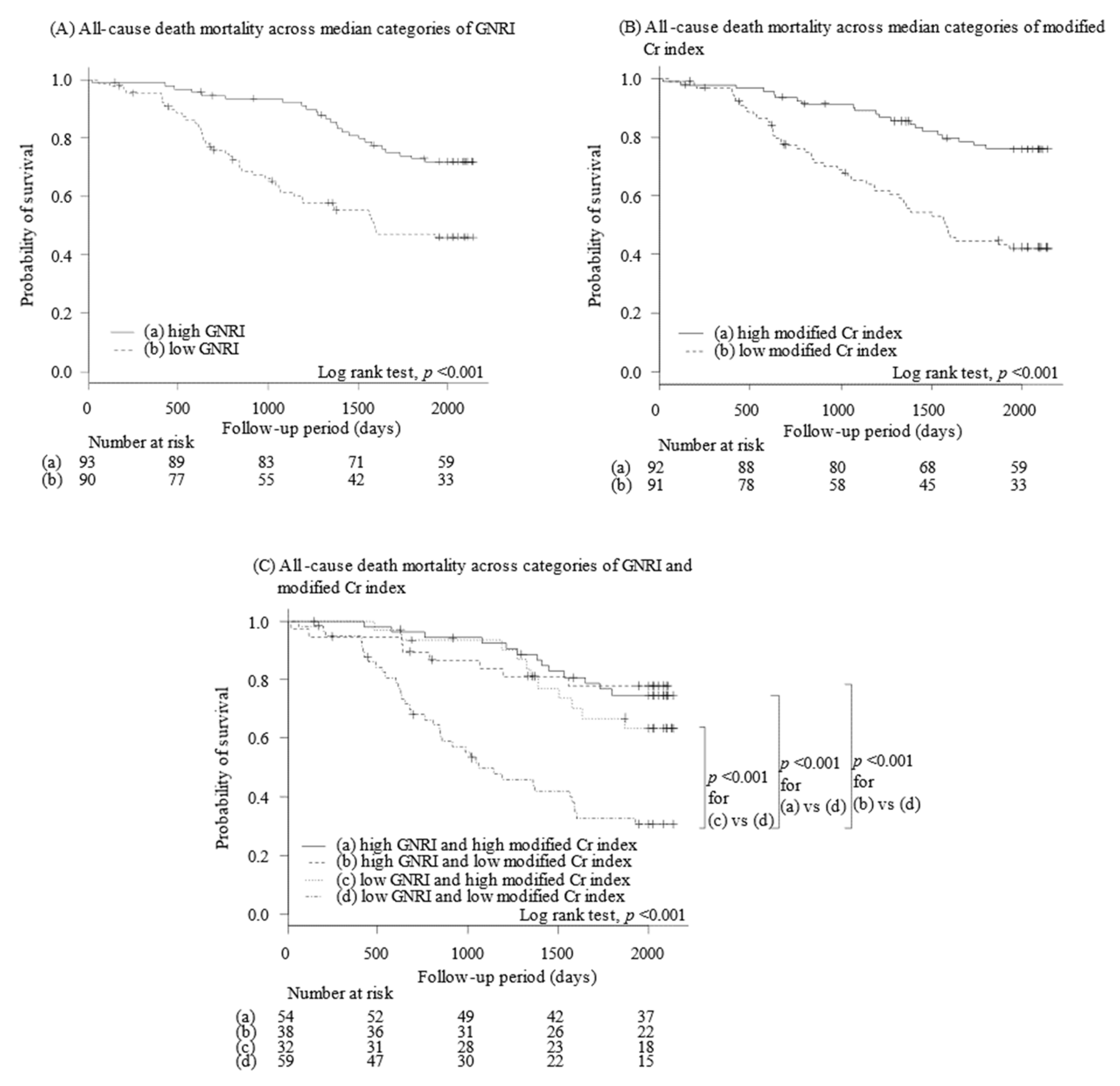
3.3. Stratification of Clinical Outcomes by GNRI
3.4. Stratification of Clinical Outcomes by Modified Cr Index
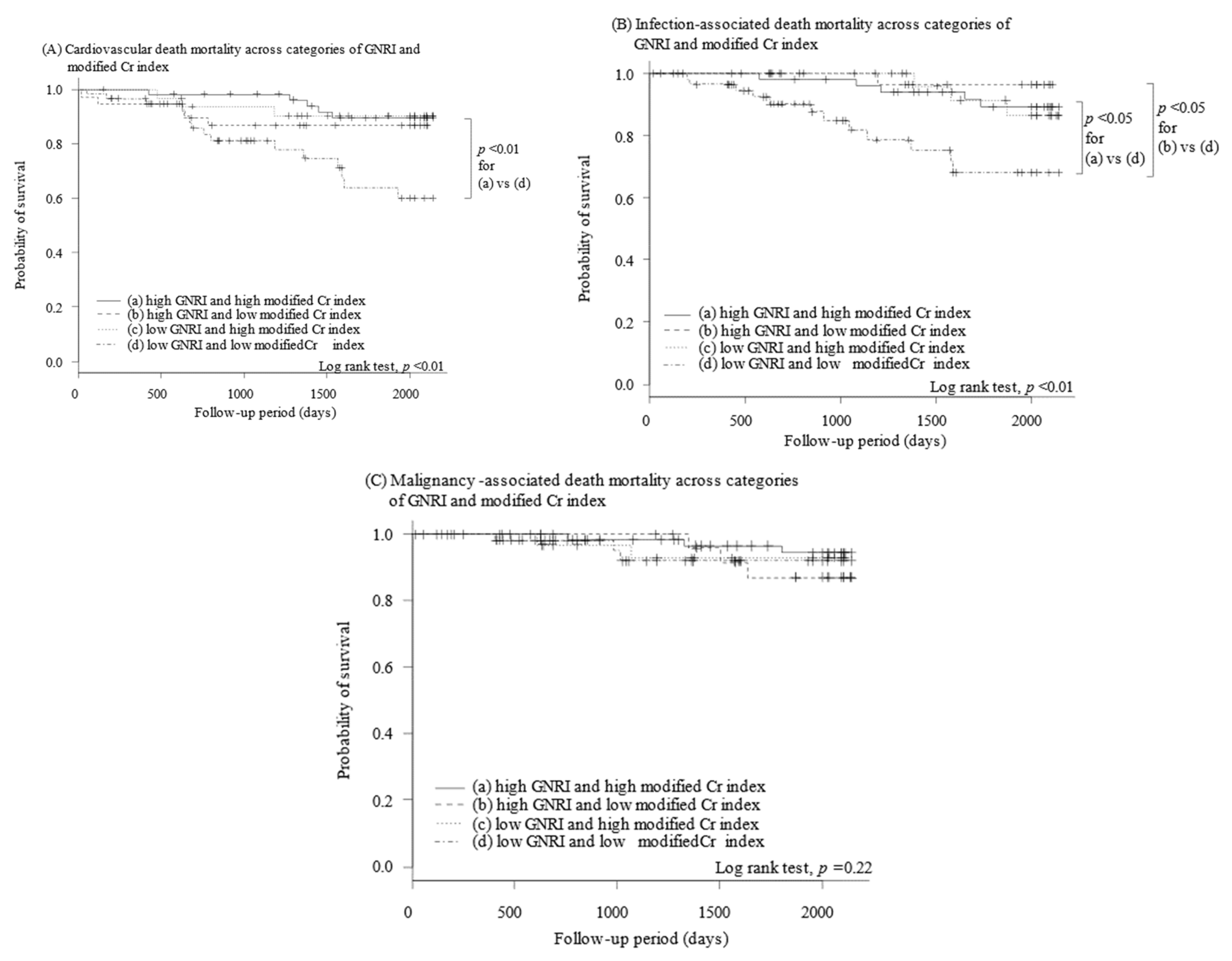
3.5. Stratification of Clinical Outcomes by Both Indexes
4. Discussion
4.1. GNRI and Modified Cr Index
4.2. Prognostic Impact of Both Indexes
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stenvinkel, P.; Heimbürger, O.; Lindholm, B.; Kaysen, G.A.; Bergström, J. Are there two types of malnutrition in chronic renal failure? Evidence for relationships between malnutrition, inflammation and atherosclerosis (MIA syndrome). Nephrol. Dial. Transplant. 2000, 15, 953–960. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalantar-Zadeh, K.; Kopple, J.D. Relative contributions of nutrition and inflammation to clinical outcome in dialysis patients. Am. J. Kidney Dis. 2001, 38, 1343–1350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ikizler, T.A.; Cano, N.J.; Franch, H.; Fouque, D.; Himmelfarb, J.; Kalantar-Zadeh, K.; Kuhlmann, M.K.; Stenvinkel, P.; TerWee, P.; Teta, D.; et al. Prevention and treatment of protein energy wasting in chronic kidney disease patients: A consensus statement by the International Society of Renal Nutrition and Metabolism. Kidney Int. 2013, 84, 1096–1107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Segall, L.; Moscalu, M.; Hogaş, S.; Mititiuc, I.; Nistor, I.; Veisa, G.; Covic, A. Protein-energy wasting, as well as overweight and obesity, is a long-term risk factor for mortality in chronic hemodialysis patients. Int. Urol. Nephrol. 2014, 46, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Fouque, D.; Kalantar-Zadeh, K.; Kopple, J.; Cano, N.; Chauveau, P.; Cuppari, L.; Franch, H.; Guarnieri, G.; Ikizler, T.A.; Kaysen, G.; et al. A proposed nomenclature and diagnostic criteria for protein-energy wasting in acute and chronic kidney disease. Kidney Int. 2008, 73, 391–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obi, Y.; Qader, H.; Kovesdy, C.P.; Kalantar-Zadeh, K. Latest consensus and update on protein-energy wasting in chronic kidney disease. Curr. Opin. Clin. Nutr. Metab. Care 2015, 18, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.-P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutritional Risk Index: A new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Canaud, B.; Granger Vallée, A.; Molinari, N.; Chenine, L.; Leray-Moragues, H.; Rodriguez, A.; Chalabi, L.; Morena, M.; Cristol, J.-P. Creatinine index as a surrogate of lean body mass derived from urea Kt/V, pre-dialysis serum levels and anthropometric characteristics of haemodialysis patients. PLoS ONE 2014, 9, e93286. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Furuya, R.; Takita, T.; Maruyama, Y.; Yamaguchi, Y.; Ohkawa, S.; Kumagai, H. Simplified nutritional screening tools for patients on maintenance hemodialysis. Am. J. Clin. Nutr. 2008, 87, 106–113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xiong, J.; Wang, M.; Zhang, Y.; Nie, L.; He, T.; Wang, Y.; Huang, Y.; Feng, B.; Zhang, J.; Zhao, J. Association of Geriatric Nutritional Risk Index with Mortality in Hemodialysis Patients: A Meta-Analysis of Cohort Studies. Kidney Blood Press Res. 2018, 43, 1878–1889. [Google Scholar] [CrossRef] [PubMed]
- Arase, H.; Yamada, S.; Yotsueda, R.; Taniguchi, M.; Yoshida, H.; Tokumoto, M.; Nakano, T.; Tsuruya, K.; Kitazono, T. Modified creatinine index and risk for cardiovascular events and all-cause mortality in patients undergoing hemodialysis: The Q-Cohort study. Atherosclerosis 2018, 275, 115–123. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Yamada, S.; Yamamoto, S.; Fukuma, S.; Nakano, T.; Tsuruya, K.; Inaba, M. Geriatric Nutritional Risk Index (GNRI) and Creatinine Index Equally Predict the Risk of Mortality in Hemodialysis Patients: J-DOPPS. Sci. Rep. 2020, 10, 5756. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, A.; Inaguma, D.; Shinjo, H.; Murata, M.; Takeda, A. Relationship between mortality and Geriatric Nutritional Risk Index (GNRI) at the time of dialysis initiation: A prospective multicenter cohort study. Ren. Replace Ther. 2017, 3, 27. [Google Scholar] [CrossRef]
- Yajima, T.; Yajima, K.; Takahashi, H. Impact of Annual Change in Geriatric Nutritional Risk Index on Mortality in Patients Undergoing Hemodialysis. Nutrients 2020, 12, 3333. [Google Scholar] [CrossRef] [PubMed]
- Harada, T.; Sorimachi, H.; Obokata, M.; Sunaga, H.; Ishida, H.; Ito, K.; Ogawa, T.; Ando, Y.; Kurabayashi, M.; Negishi, K. The relationship between antecedent creatinine decreases and outcomes in patients undergoing hemodialysis. Hemodial. Int. 2020, 24, 89–98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lacson, E.; Wang, W.; Zebrowski, B.; Wingard, R.; Hakim, R.M. Outcomes associated with intradialytic oral nutritional supplements in patients undergoing maintenance hemodialysis: A quality improvement report. Am. J. Kidney Dis. 2012, 60, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Cheu, C.; Pearson, J.; Dahlerus, C.; Lantz, B.; Chowdhury, T.; Sauer, P.F.; Farrell, R.E.; Port, F.K.; Ramirez, S.P.B. Association between oral nutritional supplementation and clinical outcomes among patients with ESRD. Clin. J. Am. Soc. Nephrol. 2013, 8, 100–107. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiner, D.E.; Tighiouart, H.; Ladik, V.; Meyer, K.B.; Zager, P.G.; Johnson, D.S. Oral intradialytic nutritional supplement use and mortality in hemodialysis patients. Am. J. Kidney Dis. 2014, 63, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Endo, M.; Nakamura, Y.; Murakami, T.; Tsukahara, H.; Watanabe, Y.; Matsuoka, Y.; Ohsawa, I.; Gotoh, H.; Inagaki, T.; Oguchi, E. Rehabilitation improves prognosis and activities of daily living in hemodialysis patients with low activities of daily living. Phys. Ther. Res. 2017, 20, 9–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| N = 183 | |
|---|---|
| Demographics | |
| Males, n (%) | 98 (53.6) |
| Age, years | 68.3 ± 12.4 |
| Dialysis vintage, month | 97 ± 89 |
| Systolic blood pressure, mmHg | 150 ± 25 |
| Comorbidity | |
| Presence of diabetes, n (%) | 76 (41) |
| History of cardiovascular events, n (%) | 51 (27) |
| Charlson risk index | 3.5 ± 1.3 |
| Cause of end-stage renal disease | |
| Diabetic nephropathy, n (%) | 74 (40.4) |
| Chronic glomerulonephritis, n (%) | 48 (26.2) |
| Glomerulosclerosis, n (%) | 48 (26.2) |
| Polycystic disease, n (%) | 16 (8.7) |
| Others, n (%) | 16 (8.7) |
| Laboratory data | |
| Hemoglobin, g/dL | 10.0 ± 1.2 |
| Serum albumin, g/dL | 3.4 ± 0.4 |
| Serum urea nitrogen, mg/dL | 60.4 ± 14.5 |
| Serum creatinine, mg/dL | 10.6 ± 2.6 |
| Serum uric acid, mg/dL | 7.6 ± 1.2 |
| Corrected serum calcium, mg/dL | 9.3 ± 0.7 |
| Serum phosphate, mg/dL | 5.0 ± 1.2 |
| Serum C-reactive protein, mg/dL | 0.4 ± 0.7 |
| Serum total cholesterol, mg/dL | 148 ± 29 |
| Serum triglycerides, mg/dL | 109 ± 53 |
| Intact parathormone, pg/mL | 155 ± 167 |
| Kt/V ratio for urea | 1.43 ± 0.28 |
| Index | |
| GNRI | 91.2 ± 10.9 |
| Modified Cr index (male), mg/kg/day | 22.2 ± 2.5 |
| Modified Cr index (female), mg/kg/day | 19.6 ± 2.2 |
| Medication | |
| Angiotensin receptor blocker, n (%) | 81 (48) |
| Calcium channel blocker, n (%) | 101 (60) |
| Beta-blocker, n (%) | 34 (20) |
| Statin, n (%) | 25 (15) |
| Anti-platelets, n (%) | 82 (49) |
| Unadjusted Model | Multivariable Model 1 | Multivariable Model 2 | Multivariable Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | |
| GNRI | ||||||||
| High GNRI | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| Low GNRI | 2.59 (1.59–4.23) | <0.001 | 2.18 (1.31–3.64) | <0.01 | 2.19 (1.29–3.73) | <0.01 | 2.05 (1.17–3.60) | <0.05 |
| Modified Cr index | ||||||||
| High modified Cr index | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| Low modified Cr index | 3.15 (1.89–5.26) | <0.001 | 2.02 (1.11–3.68) | <0.05 | 1.81 (0.97–3.35) | 0.06 | 1.82 (0.94–3.50) | 0.07 |
| Men | Women | Total | |
|---|---|---|---|
| High GNRI and high modified Cr index, n (%) | 32 (32.7) | 22 (25.9) | 54 (29.5) |
| High GNRI and low modified Cr index, n (%) | 24 (24.5) | 14 (16.5) | 38 (20.8) |
| Low GNRI and high modified Cr index, n (%) | 16 (16.3) | 16 (18.8) | 32 (17.5) |
| Low GNRI and low modified Cr index, n (%) | 26 (26.5) | 33 (38.8) | 59 (32.2) |
| Unadjusted Model | Multivariable Model 1 | Multivariable Model 2 | Multivariable Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | Hazard Ratio (95% CI) | p-Value | |
| All-cause death | ||||||||
| High GNRI and high modified Cr index | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| High GNRI and low modified Cr index | 1.48 (0.66–3.29) | 0.34 | 0.92 (0.40–2.11) | 0.84 | 0.73 (0.31–1.78) | 0.62 | 0.69 (0.27–1.71) | 0.42 |
| Low GNRI and high modified Cr index | 1.04 (0.42–2.55) | 0.93 | 1.11 (0.45–2.72) | 0.83 | 1.06 (0.43–2.61) | 0.9 | 0.75 (0.29–1.93) | 0.55 |
| Low GNRI and low modified Cr index | 4.60 (2.52–8.39) | <0.001 | 2.83 (1.41–5.69) | <0.01 | 2.54 (1.24–5.21) | <0.05 | 2.33 (1.06–5.13) | <0.05 |
| Cardiovascular death | ||||||||
| High GNRI and high modified Cr index | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| High GNRI and low modified Cr index | 1.54 (0.45–5.32) | 0.50 | 1.43 (0.41–4.94) | 0.57 | 1.41 (0.41–4.91) | 0.59 | 1.49 (0.41–5.39) | 0.54 |
| Low GNRI and high modified Cr index | 1.07 (0.26–4.49) | 0.92 | 0.87 (0.20–3.86) | 0.86 | 0.69 (0.15–3.14) | 0.63 | 0.69 (0.14–3.37) | 0.65 |
| Low GNRI and low modified Cr index | 4.30 (1.55–11.9) | <0.01 | 3.46 (1.07–11.1) | <0.05 | 3.08 (0.91–10.4) | 0.07 | 3.14 (0.89–11.0) | 0.07 |
| Infection-associated death | ||||||||
| High GNRI and high modified Cr index | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - | 1.00 (reference) | - |
| High GNRI and low modified Cr index | 0.31 (0.04–2.69) | 0.29 | 0.28 (0.03–2.42) | 0.25 | 0.25 (0.03–2.13) | 0.20 | 0.21 (0.02–2.01) | 0.17 |
| Low GNRI and high modified Cr index | 1.08 (0.26–4.52) | 0.92 | 0.80 (0.18–3.59) | 0.76 | 0.70 (0.15–3.28) | 0.65 | 1.35 (0.24–7.73) | 0.74 |
| Low GNRI and low modified Cr index | 3.95 (1.38–11.3) | <0.05 | 3.23 (0.98–10.7) | 0.05 | 2.99 (0.89–9.98) | 0.08 | 8.45 (1.80–39.7) | <0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujioka, H.; Koike, T.; Imamura, T.; Tomoda, F.; Kakeshita, K.; Yamazaki, H.; Kinugawa, K. Impact of Geriatric Nutritional Risk Index and Modified Creatinine Index Combination on Mortality in Hemodialysis Patients. Nutrients 2022, 14, 801. https://doi.org/10.3390/nu14040801
Fujioka H, Koike T, Imamura T, Tomoda F, Kakeshita K, Yamazaki H, Kinugawa K. Impact of Geriatric Nutritional Risk Index and Modified Creatinine Index Combination on Mortality in Hemodialysis Patients. Nutrients. 2022; 14(4):801. https://doi.org/10.3390/nu14040801
Chicago/Turabian StyleFujioka, Hayato, Tsutomu Koike, Teruhiko Imamura, Fumihiro Tomoda, Kota Kakeshita, Hidenori Yamazaki, and Koichiro Kinugawa. 2022. "Impact of Geriatric Nutritional Risk Index and Modified Creatinine Index Combination on Mortality in Hemodialysis Patients" Nutrients 14, no. 4: 801. https://doi.org/10.3390/nu14040801






