The Negative Impact of Night Shifts on Diet in Emergency Healthcare Workers
Abstract
1. Introduction
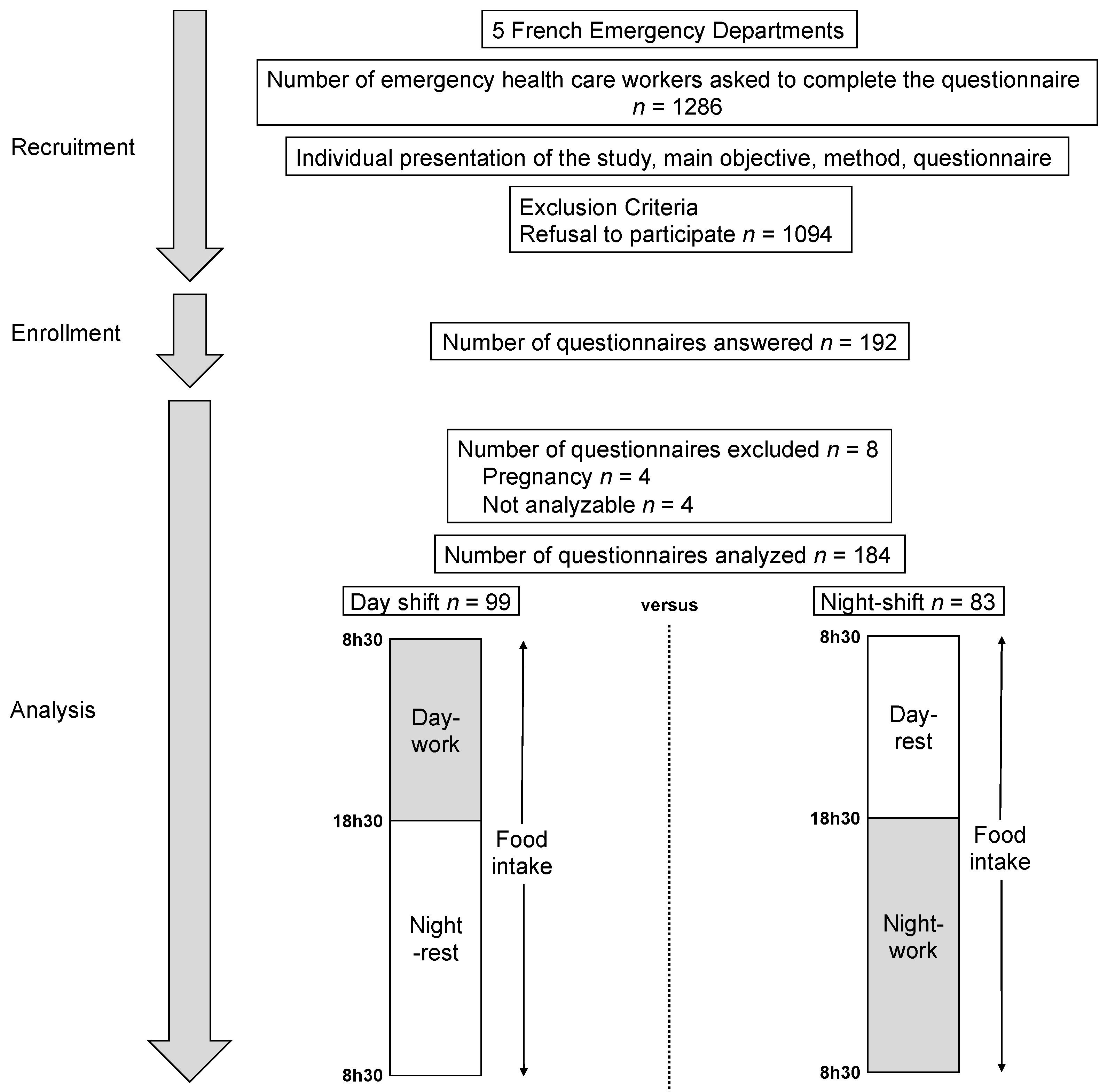
2. Materials and Methods
2.1. Study Design
2.2. Outcomes
2.3. Statistics
3. Results
3.1. Main Objective: Impact of Night Shift on Alimentation
3.1.1. Quantitative Data
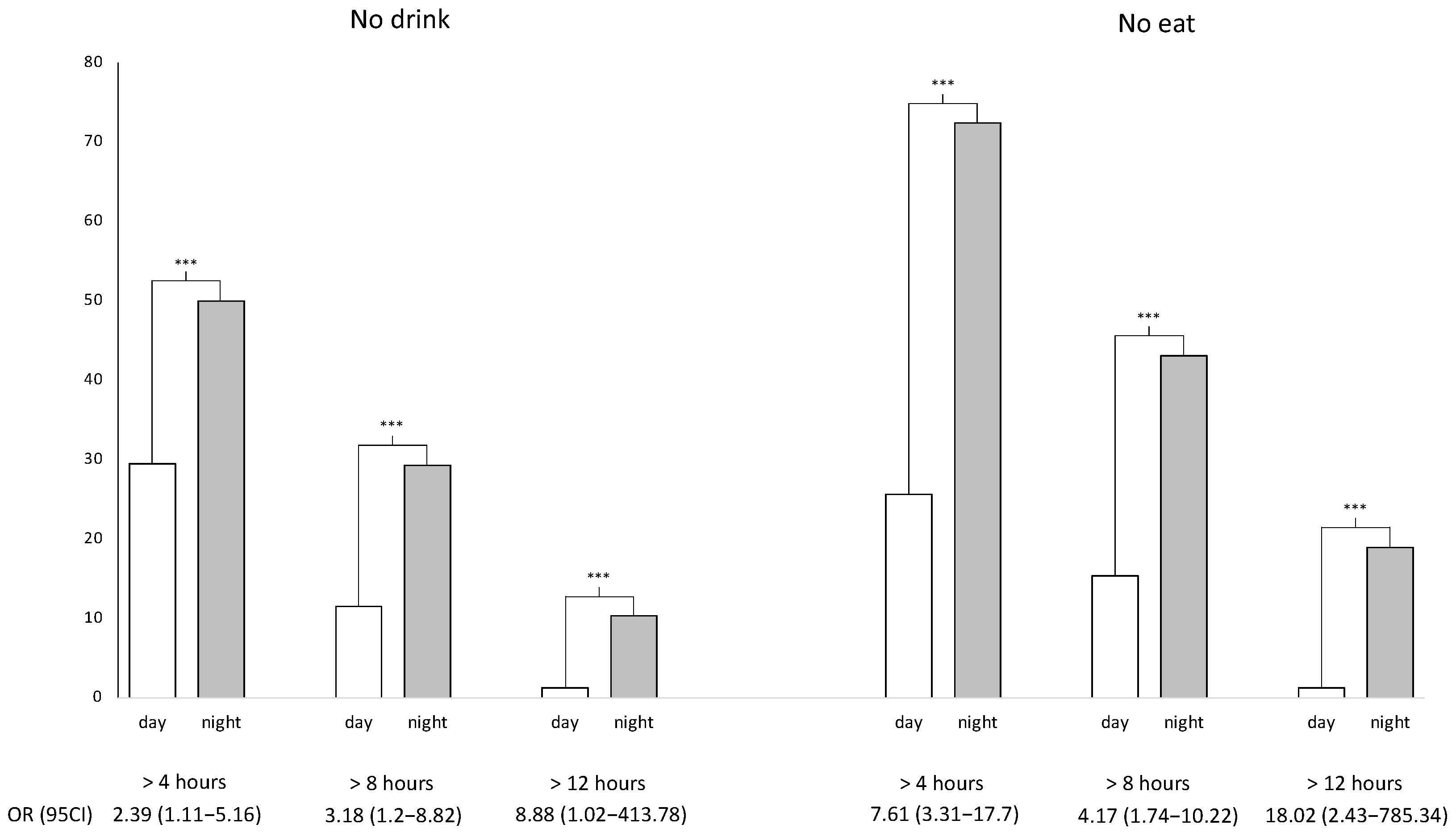
3.1.2. Qualitative Data
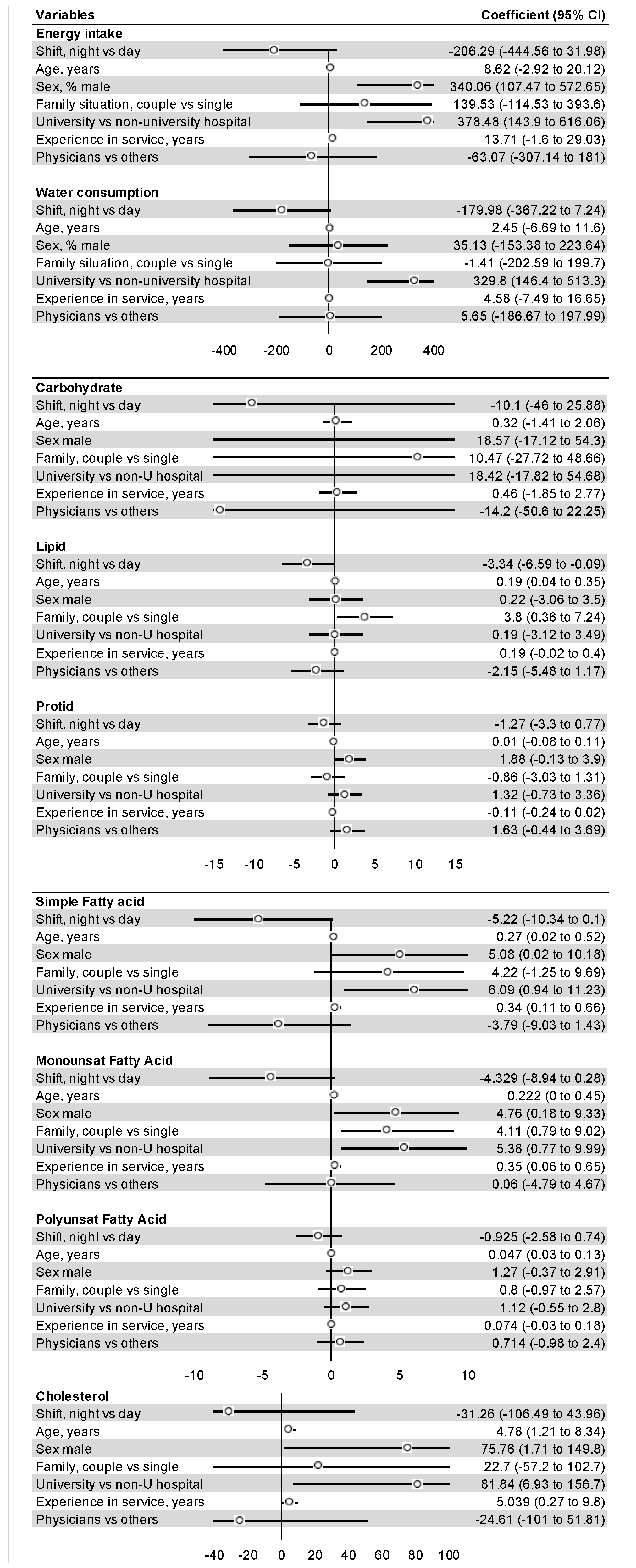
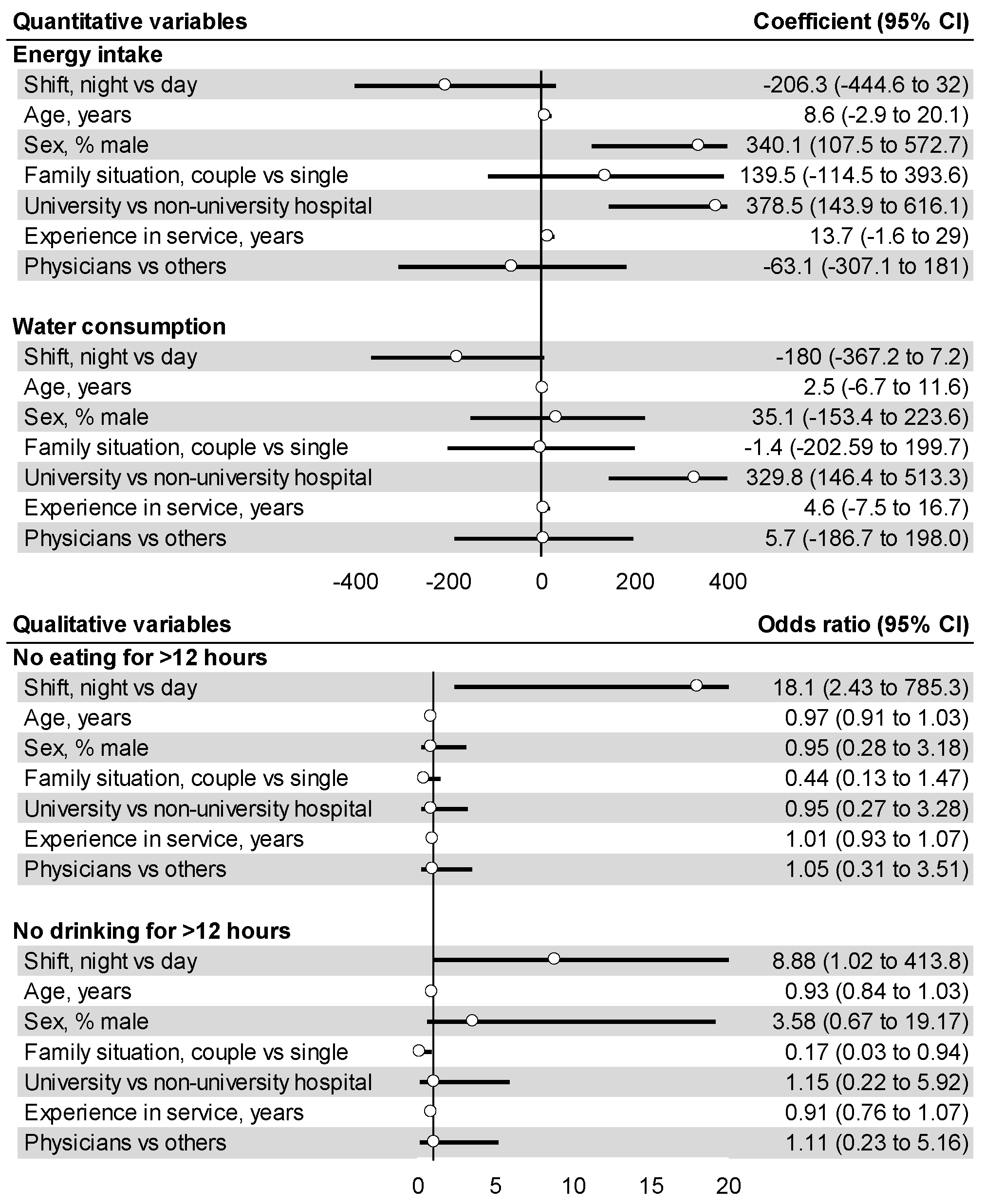
3.2. Regression Analysis
3.2.1. Quantitative Variables
3.2.2. Qualitative Variables
4. Discussion
4.1. The Negative Impact of Night Shift on Food Intake
4.2. The Amount and Quality of Nutrient Intake and Shifts
4.3. Other Influencing Variables
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Convention C171—Night Work Convention, 1990 (No. 171). Available online: https://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_INSTRUMENT_ID:312316 (accessed on 4 November 2021).
- Hansen, J. Night Shift Work and Risk of Breast Cancer. Curr. Environ. Health Rep. 2017, 4, 325–339. [Google Scholar] [CrossRef] [PubMed]
- Rajaratnam, S.M.; Arendt, J. Health in a 24-h Society. Lancet 2001, 358, 999–1005. [Google Scholar] [CrossRef]
- Boivin, D.B.; Boudreau, P. Impacts of Shift Work on Sleep and Circadian Rhythms. Pathol. Biol. 2014, 62, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, S.; Magee, M.; Stone, J.E.; Mulhall, M.D.; Collins, A.; Howard, M.E.; Lockley, S.W.; Rajaratnam, S.M.W.; Sletten, T.L. The Impact of Shift Work on Sleep, Alertness and Performance in Healthcare Workers. Sci. Rep. 2019, 9, 4635. [Google Scholar] [CrossRef]
- Kosmadopoulos, A.; Kervezee, L.; Boudreau, P.; Gonzales-Aste, F.; Vujovic, N.; Scheer, F.A.J.L.; Boivin, D.B. Effects of Shift Work on the Eating Behavior of Police Officers on Patrol. Nutrients 2020, 12, 999. [Google Scholar] [CrossRef][Green Version]
- Lim, Y.C.; Hoe, V.C.W.; Darus, A.; Bhoo-Pathy, N. Association between Night-Shift Work, Sleep Quality and Metabolic Syndrome. Occup. Environ. Med. 2018, 75, 716–723. [Google Scholar] [CrossRef]
- Vetter, C.; Devore, E.E.; Wegrzyn, L.R.; Massa, J.; Speizer, F.E.; Kawachi, I.; Rosner, B.; Stampfer, M.J.; Schernhammer, E.S. Association Between Rotating Night Shift Work and Risk of Coronary Heart Disease Among Women. JAMA 2016, 315, 1726–1734. [Google Scholar] [CrossRef]
- Dutheil, F.; Baker, J.S.; Mermillod, M.; De Cesare, M.; Vidal, A.; Moustafa, F.; Pereira, B.; Navel, V. Shift Work, and Particularly Permanent Night Shifts, Promote Dyslipidaemia: A Systematic Review and Meta-Analysis. Atherosclerosis 2020, 313, 156–169. [Google Scholar] [CrossRef]
- Sun, M.; Feng, W.; Wang, F.; Li, P.; Li, Z.; Li, M.; Tse, G.; Vlaanderen, J.; Vermeulen, R.; Tse, L.A. Meta-Analysis on Shift Work and Risks of Specific Obesity Types. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2018, 19, 28–40. [Google Scholar] [CrossRef]
- Keski-Rahkonen, A.; Mustelin, L. Epidemiology of Eating Disorders in Europe: Prevalence, Incidence, Comorbidity, Course, Consequences, and Risk Factors. Curr. Opin. Psychiatry 2016, 29, 340–345. [Google Scholar] [CrossRef]
- Samhat, Z.; Attieh, R.; Sacre, Y. Relationship between Night Shift Work, Eating Habits and BMI among Nurses in Lebanon. BMC Nurs. 2020, 19, 25. [Google Scholar] [CrossRef][Green Version]
- Palla, L.; Almoosawi, S. Diurnal Patterns of Energy Intake Derived via Principal Component Analysis and Their Relationship with Adiposity Measures in Adolescents: Results from the National Diet and Nutrition Survey RP (2008–2012). Nutrients 2019, 11, 422. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bonham, M.P.; Kaias, E.; Zimberg, I.; Leung, G.K.W.; Davis, R.; Sletten, T.L.; Windsor-Aubrey, H.; Huggins, C.E. Effect of Night Time Eating on Postprandial Triglyceride Metabolism in Healthy Adults: A Systematic Literature Review. J. Biol. Rhythm. 2019, 34, 119–130. [Google Scholar] [CrossRef] [PubMed]
- Gupta, C.C.; Centofanti, S.; Dorrian, J.; Coates, A.; Stepien, J.M.; Kennaway, D.; Wittert, G.; Heilbronn, L.; Catcheside, P.; Noakes, M.; et al. Altering Meal Timing to Improve Cognitive Performance during Simulated Nightshifts. Chronobiol. Int. 2019, 36, 1691–1713. [Google Scholar] [CrossRef] [PubMed]
- Abdella, H.M.; Farssi, H.O.E.; Broom, D.R.; Hadden, D.A.; Dalton, C.F. Eating Behaviours and Food Cravings; Influence of Age, Sex, BMI and FTO Genotype. Nutrients 2019, 11, 377. [Google Scholar] [CrossRef][Green Version]
- Padilla, H.M.; Wilson, M.; Vandenberg, R.J.; Davis, M.; Clark, M.A. Health Behavior among Working Adults: Workload and Exhaustion Are Associated with Nutrition and Physical Activity Behaviors That Lead to Weight Gain. J. Health Psychol. 2021, 26, 892–904. [Google Scholar] [CrossRef]
- Nishitani, N.; Sakakibara, H.; Akiyama, I. Eating Behavior Related to Obesity and Job Stress in Male Japanese Workers. Nutrition 2009, 25, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Pepłońska, B.; Nowak, P.; Trafalska, E. The Association between Night Shift Work and Nutrition Patterns among Nurses: A Literature Review. Med. Pract. 2019, 70, 363–376. [Google Scholar] [CrossRef]
- Bouillon-Minois, J.-B.; Trousselard, M.; Pereira, B.; Schmidt, J.; Clinchamps, M.; Thivel, D.; Ugbolue, U.C.; Moustafa, F.; Occelli, C.; Vallet, G.; et al. Protocol of the Study on Emergency Health Care Workers’ Responses Evaluated by Karasek Questionnaire: The SEEK-Study Protocol. Int. J. Environ. Res. Public Health 2021, 18, 4068. [Google Scholar] [CrossRef]
- Durand, A.-C.; Bompard, C.; Sportiello, J.; Michelet, P.; Gentile, S. Stress and Burnout among Professionals Working in the Emergency Department in a French University Hospital: Prevalence and Associated Factors. Work Read. Mass 2019, 63, 57–67. [Google Scholar] [CrossRef]
- Bouillon-Minois, J.-B.; Roux, V.; Pereira, B.; Flannery, M.; Pelissier, C.; Occelli, C.; Schmidt, J.; Navel, V.; Dutheil, F. Stress among Emergency Health Care Workers on Nuclear or Radiation Disaster: A Preliminary State Survey. Int. J. Environ. Res. Public Health 2021, 18, 8384. [Google Scholar] [CrossRef] [PubMed]
- Dutheil, F.; Trousselard, M.; Perrier, C.; Lac, G.; Chamoux, A.; Duclos, M.; Naughton, G.; Mnatzaganian, G.; Schmidt, J. Urinary Interleukin-8 Is a Biomarker of Stress in Emergency Physicians, Especially with Advancing Age—The JOBSTRESS* Randomized Trial. PLoS ONE 2013, 8, e71658. [Google Scholar] [CrossRef] [PubMed]
- Dutheil, F.; Boudet, G.; Perrier, C.; Lac, G.; Ouchchane, L.; Chamoux, A.; Duclos, M.; Schmidt, J. JOBSTRESS Study: Comparison of Heart Rate Variability in Emergency Physicians Working a 24-Hour Shift or a 14-Hour Night Shift—A Randomized Trial. Int. J. Cardiol. 2012, 158, 322–325. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, M.; Mujahid, M.; Hutson, M.; Fukutome, A.; Robichaud, R.; Lopez, J. Investing in Public School Kitchens and Equipment as a Pathway to Healthy Eating and Equitable Access to Healthy Food. J. Sch. Health 2020, 90, 492–503. [Google Scholar] [CrossRef]
- Tremblay, A.; Clinchamps, M.; Pereira, B.; Courteix, D.; Lesourd, B.; Chapier, R.; Obert, P.; Vinet, A.; Walther, G.; Chaplais, E.; et al. Dietary Fibres and the Management of Obesity and Metabolic Syndrome: The RESOLVE Study. Nutrients 2020, 12, 2911. [Google Scholar] [CrossRef]
- Nutrient Recommendations: Dietary Reference Intakes (DRI). Available online: https://ods.od.nih.gov/HealthInformation/Dietary_Reference_Intakes.aspx (accessed on 19 November 2021).
- Reeves, S.L.; Newling-Ward, E.; Gissane, C. The Effect of Shift-work on Food Intake and Eating Habits. Nutr. Food Sci. 2004, 34, 216–221. [Google Scholar] [CrossRef]
- Sahu, S.; Dey, M. Changes in Food Intake Pattern of Nurses Working in Rapidly Rotating Shift. Al Ameen J. Med. Sci. 2011, 4, 9. [Google Scholar]
- Naghashpour, M.; Amani, R.; Nematpour, S.; Haghighizadeh, M.H. Dietary, Anthropometric, Biochemical and Psychiatric Indices in Shift Work Nurses. Food Nutr. Sci. 2013, 4, 1239–1246. [Google Scholar] [CrossRef][Green Version]
- Tada, Y.; Kawano, Y.; Maeda, I.; Yoshizaki, T.; Sunami, A.; Yokoyama, Y.; Matsumoto, H.; Hida, A.; Komatsu, T.; Togo, F. Association of Body Mass Index with Lifestyle and Rotating Shift Work in Japanese Female Nurses. Obesity 2014, 22, 2489–2493. [Google Scholar] [CrossRef]
- Beebe, D.; Chang, J.J.; Kress, K.; Mattfeldt-Beman, M. Diet Quality and Sleep Quality among Day and Night Shift Nurses. J. Nurs. Manag. 2017, 25, 549–557. [Google Scholar] [CrossRef]
- Ramin, C.; Devore, E.E.; Wang, W.; Pierre-Paul, J.; Wegrzyn, L.R.; Schernhammer, E.S. Night Shift Work at Specific Age Ranges and Chronic Disease Risk Factors. Occup. Environ. Med. 2015, 72, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.G.; Johnston, A.N.B.; Greenslade, J.H.; Wallis, M.; Elder, E.; Abraham, L.; Thom, O.; Carlström, E.; Crilly, J. Stressors and Coping Strategies of Emergency Department Nurses and Doctors: A Cross-Sectional Study. Australas. Emerg. Care 2019, 22, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Bouillon-Minois, J.-B.; Schmidt, J.; Dutheil, F. SARS-CoV-2 Pandemic and Emergency Medicine: The Worst Is yet to Come. Am. J. Emerg. Med. 2020, 42, 246–247. [Google Scholar] [CrossRef] [PubMed]
- Bouillon-Minois, J.-B.; Raconnat, J.; Clinchamps, M.; Schmidt, J.; Dutheil, F. Emergency Department and Overcrowding During COVID-19 Outbreak; a Letter to Editor. Arch. Acad. Emerg. Med. 2021, 9, e28. [Google Scholar] [CrossRef]
- Bremner, J.D.; Moazzami, K.; Wittbrodt, M.T.; Nye, J.A.; Lima, B.B.; Gillespie, C.F.; Rapaport, M.H.; Pearce, B.D.; Shah, A.J.; Vaccarino, V. Diet, Stress and Mental Health. Nutrients 2020, 12, 2428. [Google Scholar] [CrossRef] [PubMed]
- Bouillon-Minois, J.-B.; Trousselard, M.; Thivel, D.; Gordon, B.A.; Schmidt, J.; Moustafa, F.; Oris, C.; Dutheil, F. Ghrelin as a Biomarker of Stress: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 784. [Google Scholar] [CrossRef]
- Bouillon-Minois, J.-B.; Trousselard, M.; Thivel, D.; Benson, A.C.; Schmidt, J.; Moustafa, F.; Bouvier, D.; Dutheil, F. Leptin as a Biomarker of Stress: A Systematic Review and Meta-Analysis. Nutrients 2021, 13, 3350. [Google Scholar] [CrossRef]
- Dutheil, F.; de Saint Vincent, S.; Pereira, B.; Schmidt, J.; Moustafa, F.; Charkhabi, M.; Bouillon-Minois, J.-B.; Clinchamps, M. DHEA as a Biomarker of Stress: A Systematic Review and Meta-Analysis. Front. Psychiatry 2021, 12, 688367. [Google Scholar] [CrossRef]
- St-Onge, M.-P.; Pizinger, T.; Kovtun, K.; RoyChoudhury, A. Sleep and Meal Timing Influence Food Intake and Its Hormonal Regulation in Healthy Adults with Overweight/Obesity. Eur. J. Clin. Nutr. 2019, 72, 76–82. [Google Scholar] [CrossRef]
- Geliebter, A.; Gluck, M.E.; Tanowitz, M.; Aronoff, N.J.; Zammit, G.K. Work-Shift Period and Weight Change. Nutrition 2000, 16, 27–29. [Google Scholar] [CrossRef]
- Roskoden, F.C.; Krüger, J.; Vogt, L.J.; Gärtner, S.; Hannich, H.J.; Steveling, A.; Lerch, M.M.; Aghdassi, A.A. Physical Activity, Energy Expenditure, Nutritional Habits, Quality of Sleep and Stress Levels in Shift-Working Health Care Personnel. PLoS ONE 2017, 12, e0169983. [Google Scholar] [CrossRef]
- Han, K.; Choi-Kwon, S.; Kim, K.S. Poor Dietary Behaviors among Hospital Nurses in Seoul, South Korea. Appl. Nurs. Res. ANR 2016, 30, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Almajwal, A.M. Stress, Shift Duty, and Eating Behavior among Nurses in Central Saudi Arabia. Saudi Med. J. 2016, 37, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Elizabeth, L.; Machado, P.; Zinöcker, M.; Baker, P.; Lawrence, M. Ultra-Processed Foods and Health Outcomes: A Narrative Review. Nutrients 2020, 12, 1955. [Google Scholar] [CrossRef]
- Jia, P.; Luo, M.; Li, Y.; Zheng, J.-S.; Xiao, Q.; Luo, J. Fast-Food Restaurant, Unhealthy Eating, and Childhood Obesity: A Systematic Review and Meta-Analysis. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2021, 22 (Suppl. 1), e12944. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heath, G.; Dorrian, J.; Coates, A. Associations between Shift Type, Sleep, Mood, and Diet in a Group of Shift Working Nurses. Scand. J. Work. Environ. Health 2019, 45, 402–412. [Google Scholar] [CrossRef]
- Bilski, B. Influence of shift work on the diet and gastrointestinal complains among nurses. A pilot study. Med. Pract. 2006, 57, 15–19. [Google Scholar]
- Morikawa, Y.; Miura, K.; Sasaki, S.; Yoshita, K.; Yoneyama, S.; Sakurai, M.; Ishizaki, M.; Kido, T.; Naruse, Y.; Suwazono, Y.; et al. Evaluation of the Effects of Shift Work on Nutrient Intake: A Cross-Sectional Study. J. Occup. Health 2008, 50, 270–278. [Google Scholar] [CrossRef][Green Version]
- Dietary Behavior and Its Relation with Lifestyle, Rotating Work Shifts and Job Satisfaction among Nurses of Ain Shams University Hospitals. Egypt. J. Community Med. 2016, 34, 75–86. [CrossRef]
- Grzymisławska, M.; Puch, E.A.; Zawada, A.; Grzymisławski, M. Do Nutritional Behaviors Depend on Biological Sex and Cultural Gender? Adv. Clin. Exp. Med. 2020, 29, 165–172. [Google Scholar] [CrossRef][Green Version]
- Dutheil, F.; Chaplais, E.; Vilmant, A.; Courteix, D.; Duche, P.; Abergel, A.; Pfabigan, D.M.; Han, S.; Mobdillon, L.; Vallet, G.T.; et al. Stress Management in Obesity during a Thermal Spa Residential Programme (ObesiStress): Protocol for a Randomised Controlled Trial Study. BMJ Open 2019, 9, e027058. [Google Scholar] [CrossRef] [PubMed]
- Santa Cecília Silva, A.A.; Lopes, T.D.V.C.; Teixeira, K.R.; Mendes, J.A.; de Souza Borba, M.E.; Mota, M.C.; Waterhouse, J.; Crispim, C.A. The Association between Anxiety, Hunger, the Enjoyment of Eating Foods and the Satiety after Food Intake in Individuals Working a Night Shift Compared with after Taking a Nocturnal Sleep: A Prospective and Observational Study. Appetite 2017, 108, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, R.; Perry, L.; Duffield, C.; Gallagher, R.; Pierce, H. Barriers and Facilitators to Healthy Eating for Nurses in the Workplace: An Integrative Review. J. Adv. Nurs. 2017, 73, 1051–1065. [Google Scholar] [CrossRef] [PubMed]

| All | Male | Female | |
|---|---|---|---|
| n = 184 | n = 81 | n = 103 | |
| Age, years | 37.2 ± 10.2 | 37.8 ± 10.4 | 36.8 ± 10.1 |
| Body Mass Index, kg/m2 | 23.2 ± 3.9 | 24.3 ± 3.8 | 22.3 ± 3.7 |
| Family situation | |||
| Married/in couple | 127 (69%) | 57 (71.3%) | 70 (68.0%) |
| Single | 56 (30.4%) | 23 (28.7%) | 33 (32.0%) |
| Missing data | 1 (0.6%) | 1 (1.2%) | - |
| Children | |||
| No children | 86 (46.7%) | 40 (49.4%) | 46 (44.7%) |
| ≥1 children | 63 (42.3%) | 27 (33.3%) | 36 (34.8%) |
| Missing data | 34 (18.4%) | 14 (17.3%) | 21 (20.4%) |
| Seniority, years | |||
| As a provider | 10.5 ± 10 | 10.5 ± 9.6 | 10.6 ± 10.4 |
| In the hospital | 9.9 ± 9.8 | 9.0 ± 9.0 | 10.6 ± 10.3 |
| In the emergency department | 6.4 ± 10 | 5.6 ± 6.5 | 6.9 ± 8.3 |
| All | Day-Shift | Night-Shift | Comparisons between Shifts | |
|---|---|---|---|---|
| n = 184 | n = 101 | n = 83 | p-Value | |
| Energy Intake (kcal) | 1523.1 ± 737.0 | 1606.7 ± 748.2 | 1400.4 ± 708.3 | 0.049 * |
| Carbohydrates (g/day) | 172.1 ± 83.5 | 178.8 ± 81.5 | 163.3 ± 86.0 | 0.120 |
| Lipids (g/day) | 69.1 ± 35.1 | 75.1 ± 35.9 | 61.13 ± 32.7 | 0.030 * |
| Simple fatty acid | 29.3 ± 15.4 | 31.8 ± 16.1 | 26.0 ± 13.4 | 0.056 |
| Monounsaturated fatty acid | 23.4 ± 14.4 | 25.6 ± 14.2 | 20.7 ± 14.2 | 0.049 * |
| Polyunsaturated fatty acid | 7.0 ± 4.7 | 7.7 ± 4.8 | 6.13 ± 4.5 | 0.050 * |
| Protein (g/day) | 74.5 ± 33.7 | 80.6 ± 30.3 | 66.4 ± 36.4 | <0.001 * |
| Cholesterol (mg/day) | 301.3 ± 240.5 | 318.7 ± 238.9 | 278.7 ± 243.0 | 0.161 |
| Fiber (g/day) | 15.0 ± 7.6 | 15.8 ± 7.1 | 13.9 ± 8.2 | 0.171 |
| Calcium (mg/day) | 625.5 ± 274.2 | 665.6 ± 249.3 | 573.3 ± 297.9 | 0.049 * |
| Water (mL/day) | 1345.8 ± 516.6 | 1451.4 ± 496.8 | 1208.3 ± 513.9 | 0.010 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bouillon-Minois, J.-B.; Thivel, D.; Croizier, C.; Ajebo, É.; Cambier, S.; Boudet, G.; Adeyemi, O.J.; Ugbolue, U.C.; Bagheri, R.; Vallet, G.T.; et al. The Negative Impact of Night Shifts on Diet in Emergency Healthcare Workers. Nutrients 2022, 14, 829. https://doi.org/10.3390/nu14040829
Bouillon-Minois J-B, Thivel D, Croizier C, Ajebo É, Cambier S, Boudet G, Adeyemi OJ, Ugbolue UC, Bagheri R, Vallet GT, et al. The Negative Impact of Night Shifts on Diet in Emergency Healthcare Workers. Nutrients. 2022; 14(4):829. https://doi.org/10.3390/nu14040829
Chicago/Turabian StyleBouillon-Minois, Jean-Baptiste, David Thivel, Carolyne Croizier, Éric Ajebo, Sébastien Cambier, Gil Boudet, Oluwaseun John Adeyemi, Ukadike Chris Ugbolue, Reza Bagheri, Guillaume T. Vallet, and et al. 2022. "The Negative Impact of Night Shifts on Diet in Emergency Healthcare Workers" Nutrients 14, no. 4: 829. https://doi.org/10.3390/nu14040829
APA StyleBouillon-Minois, J.-B., Thivel, D., Croizier, C., Ajebo, É., Cambier, S., Boudet, G., Adeyemi, O. J., Ugbolue, U. C., Bagheri, R., Vallet, G. T., Schmidt, J., Trousselard, M., & Dutheil, F. (2022). The Negative Impact of Night Shifts on Diet in Emergency Healthcare Workers. Nutrients, 14(4), 829. https://doi.org/10.3390/nu14040829









