Impact of Mediterranean Diet Food Choices and Physical Activity on Serum Metabolic Profile in Healthy Adolescents: Findings from the DIMENU Project
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Nutritional History
2.3. Mediterranean Diet Adherence Test (KIDMED)
2.4. Anthropometric Parameters and Bioelectrical Impedance Analysis
2.5. Biochemical Measurements
2.6. Mediterranean Personalized Food Plan
2.7. Statistical Analysis
3. Results
3.1. General Characteristics and Metabolic Profile of the Study Population
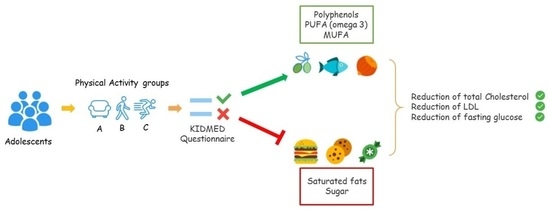
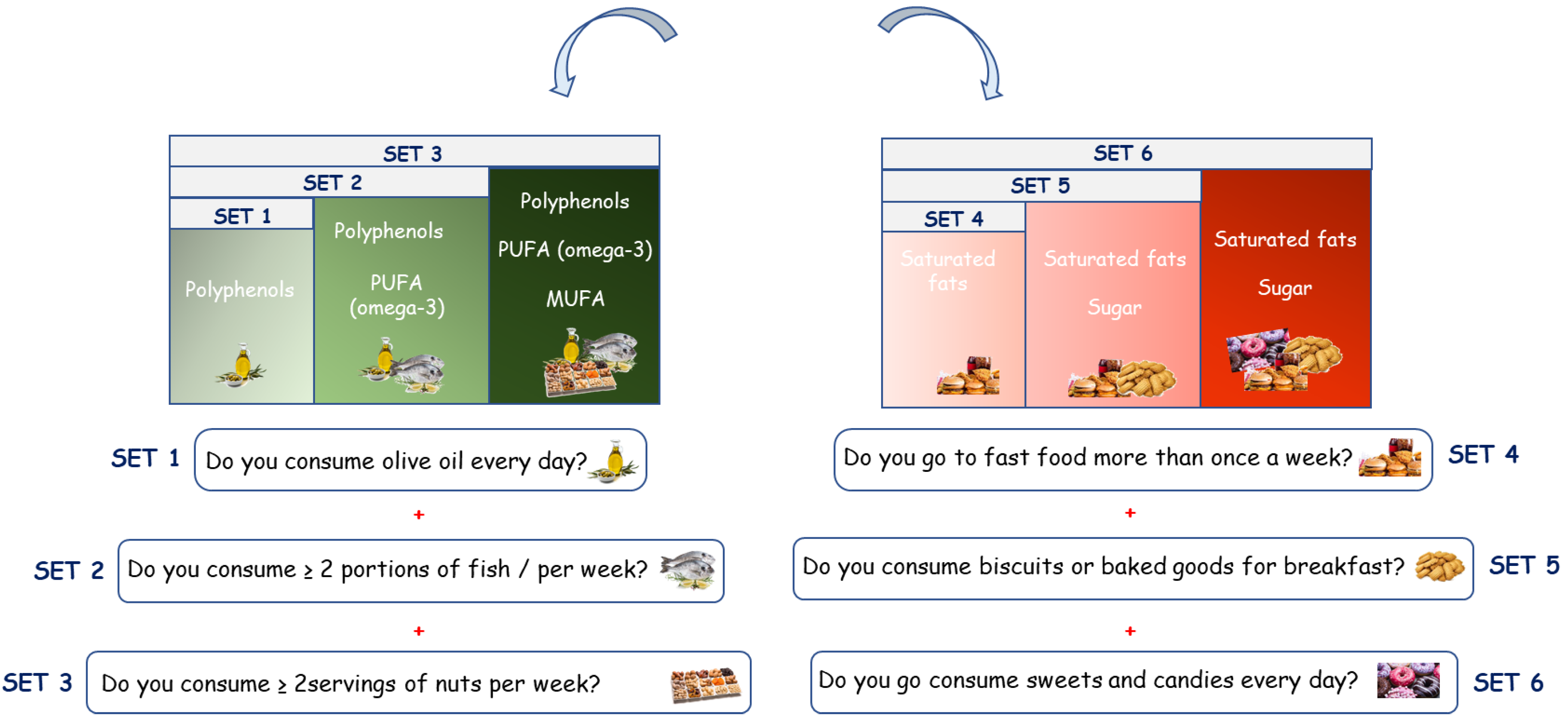
3.2. Impact of the Mediterranean Diet Food Choices on the Adolescent Metabolic Profile
3.3. Impact of the Mediterranean Diet Food Choices on Metabolic Profile in the Adolescents Grouped According to the Different Physical Activity Levels
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Keys, A.; Menott, A.; Karvonen, M.J.; Aravanjs, C.; Blackburn, H.; Buzina, R.; Djordjevic, B.S.; Dontas, A.S.; Fidanza, F.; Keys, M.H.; et al. The Diet and 15-Year Death Rate in the Seven Countries Study. Am. J. Epidemiol. 2017, 185, 1130–1142. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; Martin-Calvo, N. Mediterranean diet and life expectancy; beyond olive oil, fruits, and vegetables. Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 401–407. [Google Scholar] [CrossRef] [PubMed]
- Widmer, R.J.; Flammer, A.J.; Lerman, L.O.; Lerman, A. The Mediterranean diet, its components, and cardiovascular disease. Am. J. Med. 2015, 128, 229–238. [Google Scholar] [CrossRef] [Green Version]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and Mediterranean Diet: A Review. Nutrients 2019, 11, 2059. [Google Scholar] [CrossRef] [Green Version]
- Augimeri, G.; Montalto, F.I.; Giordano, C.; Barone, I.; Lanzino, M.; Catalano, S.; Ando, S.; De Amicis, F.; Bonofiglio, D. Nutraceuticals in the Mediterranean Diet: Potential Avenues for Breast Cancer Treatment. Nutrients 2021, 13, 2557. [Google Scholar] [CrossRef]
- Lotfi, K.; Saneei, P.; Hajhashemy, Z.; Esmaillzadeh, A. Adherence to the Mediterranean Diet, Five-Year Weight Change, and Risk of Overweight and Obesity: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2022, 13, 152–166. [Google Scholar] [CrossRef] [PubMed]
- Martin-Pelaez, S.; Fito, M.; Castaner, O. Mediterranean Diet Effects on Type 2 Diabetes Prevention, Disease Progression, and Related Mechanisms. A Review. Nutrients 2020, 12, 2236. [Google Scholar] [CrossRef] [PubMed]
- Malmir, H.; Saneei, P.; Larijani, B.; Esmaillzadeh, A. Adherence to Mediterranean diet in relation to bone mineral density and risk of fracture: A systematic review and meta-analysis of observational studies. Eur. J. Nutr. 2018, 57, 2147–2160. [Google Scholar] [CrossRef]
- Petersson, S.D.; Philippou, E. Mediterranean Diet, Cognitive Function, and Dementia: A Systematic Review of the Evidence. Adv. Nutr. 2016, 7, 889–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marventano, S.; Vetrani, C.; Vitale, M.; Godos, J.; Riccardi, G.; Grosso, G. Whole Grain Intake and Glycaemic Control in Healthy Subjects: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutrients 2017, 9, 769. [Google Scholar] [CrossRef] [PubMed]
- Morrison, D.J.; Preston, T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes 2016, 7, 189–200. [Google Scholar] [CrossRef] [Green Version]
- Bullo, M.; Lamuela-Raventos, R.; Salas-Salvado, J. Mediterranean diet and oxidation: Nuts and olive oil as important sources of fat and antioxidants. Curr. Top Med. Chem. 2011, 11, 1797–1810. [Google Scholar] [CrossRef] [PubMed]
- Jimenez-Lopez, C.; Carpena, M.; Lourenco-Lopes, C.; Gallardo-Gomez, M.; Lorenzo, J.M.; Barba, F.J.; Prieto, M.A.; Simal-Gandara, J. Bioactive Compounds and Quality of Extra Virgin Olive Oil. Foods 2020, 9, 1014. [Google Scholar] [CrossRef]
- Bays, H.E.; Tighe, A.P.; Sadovsky, R.; Davidson, M.H. Prescription omega-3 fatty acids and their lipid effects: Physiologic mechanisms of action and clinical implications. Expert Rev. Cardiovasc. Ther. 2008, 6, 391–409. [Google Scholar] [CrossRef] [PubMed]
- Santos-Buelga, C.; Gonzalez-Manzano, S.; Gonzalez-Paramas, A.M. Wine, Polyphenols, and Mediterranean Diets. What Else Is There to Say? Molecules 2021, 26, 5537. [Google Scholar] [CrossRef] [PubMed]
- Subbaramaiah, K.; Michaluart, P.; Chung, W.J.; Tanabe, T.; Telang, N.; Dannenberg, A.J. Resveratrol inhibits cyclooxygenase-2 transcription in human mammary epithelial cells. Ann. N. Y. Acad. Sci. 1999, 889, 214–223. [Google Scholar] [CrossRef]
- Vivancos, M.; Moreno, J.J. Effect of resveratrol, tyrosol and beta-sitosterol on oxidised low-density lipoprotein-stimulated oxidative stress, arachidonic acid release and prostaglandin E2 synthesis by RAW 264.7 macrophages. Br. J. Nutr. 2008, 99, 1199–1207. [Google Scholar] [CrossRef] [Green Version]
- Altomare, R.; Cacciabaudo, F.; Damiano, G.; Palumbo, V.D.; Gioviale, M.C.; Bellavia, M.; Tomasello, G.; Lo Monte, A.I. The mediterranean diet: A history of health. Iran. J. Public Health 2013, 42, 449–457. [Google Scholar]
- Bach-Faig, A.; Berry, E.M.; Lairon, D.; Reguant, J.; Trichopoulou, A.; Dernini, S.; Medina, F.X.; Battino, M.; Belahsen, R.; Miranda, G.; et al. Mediterranean diet pyramid today. Science and cultural updates. Public Health Nutr. 2011, 14, 2274–2284. [Google Scholar] [CrossRef] [Green Version]
- Augimeri, G.; Bonofiglio, D. The Mediterranean Diet as a Source of Natural Compounds: Does It Represent a Protective Choice against Cancer? Pharmaceuticals 2021, 14, 920. [Google Scholar] [CrossRef]
- Diolintzi, A.; Panagiotakos, D.B.; Sidossis, L.S. From Mediterranean diet to Mediterranean lifestyle: A narrative review. Public Health Nutr. 2019, 22, 2703–2713. [Google Scholar] [CrossRef] [PubMed]
- Lake, A.A.; Mathers, J.C.; Rugg-Gunn, A.J.; Adamson, A.J. Longitudinal change in food habits between adolescence (11–12 years) and adulthood (32–33 years): The ASH30 Study. J. Public Health 2006, 28, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Strasser, B. Physical activity in obesity and metabolic syndrome. Ann. N. Y. Acad. Sci. 2013, 1281, 141–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morelli, C.; Avolio, E.; Galluccio, A.; Caparello, G.; Manes, E.; Ferraro, S.; Caruso, A.; De Rose, D.; Barone, I.; Adornetto, C.; et al. Nutrition Education Program and Physical Activity Improve the Adherence to the Mediterranean Diet: Impact on Inflammatory Biomarker Levels in Healthy Adolescents From the DIMENU Longitudinal Study. Front. Nutr. 2021, 8, 685247. [Google Scholar] [CrossRef]
- Morelli, C.; Avolio, E.; Galluccio, A.; Caparello, G.; Manes, E.; Ferraro, S.; De Rose, D.; Santoro, M.; Barone, I.; Catalano, S.; et al. Impact of Vigorous-Intensity Physical Activity on Body Composition Parameters, Lipid Profile Markers, and Irisin Levels in Adolescents: A Cross-Sectional Study. Nutrients 2020, 12, 742. [Google Scholar] [CrossRef] [Green Version]
- Augimeri, G.; Galluccio, A.; Caparello, G.; Avolio, E.; La Russa, D.; De Rose, D.; Morelli, C.; Barone, I.; Catalano, S.; Ando, S.; et al. Potential Antioxidant and Anti-Inflammatory Properties of Serum from Healthy Adolescents with Optimal Mediterranean Diet Adherence: Findings from DIMENU Cross-Sectional Study. Antioxidants 2021, 10, 1172. [Google Scholar] [CrossRef]
- Galluccio, A.; Caparello, G.; Avolio, E.; Manes, E.; Ferraro, S.; Giordano, C.; Sisci, D.; Bonofiglio, D. Self-Perceived Physical Activity and Adherence to the Mediterranean Diet in Healthy Adolescents during COVID-19: Findings from the DIMENU Pilot Study. Healthcare 2021, 9, 622. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. Available online: https://apps.who.int/iris/handle/10665/272722. (accessed on 24 January 2022).
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; Garcia, A.; Perez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef]
- World Health Organization. Physical Status: The Use and Interpretation of Anthropometry. Report of A WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995; Volume 854, pp. 1–452. [Google Scholar]
- Società Italiana Di Nutrizione Umana. Available online: https://sinu.it/2019/07/09/fabbisogno-energetico-medioar-nellintervallo-deta-1-17-anni (accessed on 28 October 2020).
- Malik, V.S.; Schulze, M.B.; Hu, F.B. Intake of sugar-sweetened beverages and weight gain: A systematic review. Am. J. Clin. Nutr. 2006, 84, 274–288. [Google Scholar] [CrossRef]
- Neovius, M.; Linne, Y.; Rossner, S. BMI, waist-circumference and waist-hip-ratio as diagnostic tests for fatness in adolescents. Int. J. Obes. 2005, 29, 163–169. [Google Scholar] [CrossRef] [Green Version]
- Velazquez-Lopez, L.; Santiago-Diaz, G.; Nava-Hernandez, J.; Munoz-Torres, A.V.; Medina-Bravo, P.; Torres-Tamayo, M. Mediterranean-style diet reduces metabolic syndrome components in obese children and adolescents with obesity. BMC Pediatr. 2014, 14, 175. [Google Scholar] [CrossRef] [Green Version]
- Fletcher, E.A.; McNaughton, S.A.; Crawford, D.; Cleland, V.; Della Gatta, J.; Hatt, J.; Dollman, J.; Timperio, A. Associations between sedentary behaviours and dietary intakes among adolescents. Public Health Nutr. 2018, 21, 1115–1122. [Google Scholar] [CrossRef] [Green Version]
- Bohara, S.S.; Thapa, K.; Bhatt, L.D.; Dhami, S.S.; Wagle, S. Determinants of Junk Food Consumption Among Adolescents in Pokhara Valley, Nepal. Front. Nutr. 2021, 8, 644650. [Google Scholar] [CrossRef] [PubMed]
- Ajala, O.; English, P.; Pinkney, J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am. J. Clin. Nutr. 2013, 97, 505–516. [Google Scholar] [CrossRef] [Green Version]
- Huo, R.; Du, T.; Xu, Y.; Xu, W.; Chen, X.; Sun, K.; Yu, X. Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: A meta-analysis. Eur. J. Clin. Nutr. 2015, 69, 1200–1208. [Google Scholar] [CrossRef] [PubMed]
- Lasa, A.; Miranda, J.; Bullo, M.; Casas, R.; Salas-Salvado, J.; Larretxi, I.; Estruch, R.; Ruiz-Gutierrez, V.; Portillo, M.P. Comparative effect of two Mediterranean diets versus a low-fat diet on glycaemic control in individuals with type 2 diabetes. Eur. J. Clin. Nutr. 2014, 68, 767–772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| T0 | T1 | ||||
|---|---|---|---|---|---|
| Anthropometric Parameters | Mean | SD | Mean | SD | p-Value |
| Weight (kg) | 62.426 | 12.39 | 63.518 | 12.483 | 0.5685 |
| Height (cm) | 165.854 | 7.818 | 167.134 | 8.508 | 0.3087 |
| BMI (kg/m2) | 22.685 | 3.685 | 23.75 | 2.252 | 0.0237 |
| BMI z-score | 0.48 | 0.86 | 0.53 | 0.76 | 0.6884 |
| WHR | 0.772 | 0.047 | 0.781 | 0.065 | 0.3024 |
| Bioimpedentiometric Parameters | |||||
| PhA (°) | 6.128 | 0.693 | 6.285 | 0.777 | 0.1860 |
| BCM (Kg) | 26.468 | 5.714 | 26.929 | 5.844 | 0.6043 |
| FFM (Kg) | 48.627 | 8.987 | 48.866 | 9.144 | 0.8632 |
| FM (Kg) | 13.799 | 7.448 | 15.291 | 7.057 | 0.1826 |
| TBW (%) | 36.241 | 6.587 | 36.015 | 6.962 | 0.8327 |
| Metabolic Profile | |||||
| Total cholesterol (mg/dL) | 155.24 | 27.7 | 139.89 | 24.31 | 0.0002 |
| LDL (mg/dL) | 83.4 | 25.96 | 71.576 | 19.02 | 0.0009 |
| HDL (mg/dL) | 58.93 | 14.19 | 56.76 | 13.42 | 0.3071 |
| Triglycerides (mg/dL) | 64.39 | 31.07 | 57.67 | 24.43 | 0.1189 |
| Glucose (mg/dL) | 83.46 | 7.47 | 77.41 | 8.48 | 0.0001 |
| Insulin (μIU/mL) | 10.35 | 4.89 | 11.03 | 6.1 | 0.4237 |
| KIDMED Items | SET 1 | SET 2 | SET 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Subjects | (78 vs. 78) | (51 vs. 53) | (20 vs. 17) | |||||||
| Parameters | Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Total cholesterol (mg/dl) | T0 | 155.00 | 27.30 | 0.0004 | 153.82 | 28.36 | 0.0173 | 159.45 | 26.72 | 0.0022 |
| T1 | 140.08 | 23.92 | 141.77 | 22.15 | 133.35 | 20.06 | ||||
| LDL (mg/dl) | T0 | 83.28 | 25.56 | 0.0012 | 82.84 | 26.26 | 0.0123 | 89.30 | 21.22 | 0.0086 |
| T1 | 71.44 | 18.92 | 72.00 | 16.12 | 71.47 | 17.02 | ||||
| HDL (mg/dl) | T0 | 59.04 | 14.25 | 0.3782 | 57.95 | 15.06 | 0.9508 | 57.05 | 13.44 | 0.1511 |
| T1 | 57.08 | 13.44 | 57.77 | 14.61 | 50.94 | 11.57 | ||||
| Triglycerides (mg/dl) | T0 | 63.31 | 27.21 | 0.1843 | 65.07 | 35.33 | 0.3659 | 65.15 | 26.66 | 0.1691 |
| T1 | 57.82 | 24.11 | 59.66 | 24.67 | 54.47 | 17.86 | ||||
| Glucose (mg/dl) | T0 | 83.46 | 7.40 | 0.0001 | 83.84 | 7.79 | 0.0001 | 83.84 | 7.79 | 0.0019 |
| T1 | 77.18 | 8.51 | 75.79 | 7.10 | 75.59 | 6.97 | ||||
| Insulin (μIU/mL) | T0 | 10.42 | 5.08 | 0.8056 | 9.42 | 4.69 | 0.3315 | 9.42 | 4.69 | 0.2151 |
| T1 | 10.63 | 5.55 | 10.26 | 6.00 | 12.02 | 7.69 | ||||
| KIDMED Items Subjects | SET 4 | SET 5 | SET 6 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (73 vs. 77) | (55 vs. 68) | (30 vs. 31) | ||||||||
| Parameters | Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Total cholesterol (mg/dl) | T0 | 153.96 | 27.28 | 0.0011 | 154.44 | 26.08 | 0.0026 | 155.57 | 25.92 | 0.0049 |
| T1 | 139.87 | 24.53 | 140.19 | 25.13 | 136.29 | 25.58 | ||||
| LDL (mg/dl) | T0 | 82.47 | 26.12 | 0.0047 | 81.40 | 25.42 | 0.0226 | 79.40 | 23.28 | 0.0344 |
| T1 | 71.79 | 18.99 | 72.07 | 19.35 | 67.58 | 19.22 | ||||
| HDL (mg/dl) | T0 | 58.41 | 14.51 | 0.4348 | 60.07 | 14.95 | 0.1791 | 63.07 | 16.08 | 0.1012 |
| T1 | 56.61 | 13.65 | 56.51 | 14.16 | 56.13 | 16.45 | ||||
| Triglycerides (mg/dl) | T0 | 65.45 | 33.15 | 0.0865 | 64.80 | 34.96 | 0.2076 | 65.63 | 27.59 | 0.7400 |
| T1 | 57.23 | 24.79 | 57.91 | 25.26 | 63.26 | 28.03 | ||||
| Glucose (mg/dl) | T0 | 83.92 | 7.00 | 0.0001 | 84.00 | 6.44 | 0.0001 | 82.73 | 6.28 | 0.0024 |
| T1 | 77.87 | 8.47 | 77.85 | 8.76 | 77.13 | 7.45 | ||||
| Insulin (μIU/mL) | T0 | 10.66 | 4.78 | 0.9079 | 10.58 | 4.95 | 0.8276 | 9.76 | 3.68 | 0.1587 |
| T1 | 10.76 | 5.99 | 10.80 | 6.26 | 11.60 | 6.07 | ||||
| Group A | Group B | Group C | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T0 | T1 | T0 | T1 | p-Value T0 | p-Value T1 | |||||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | A vs. B | A vs. C | B vs. C | A vs. B | A vs. C | B vs. C | |
| Total cholesterol (mg/dl) | 164.61 | 28.51 | 138.65 * | 19.65 | 154.85 | 29.25 | 139.29 * | 26.32 | 148.00 | 23.46 | 141.64 | 25.13 | 0.3854 | 0.0835 | 0.5885 | 0.9948 | 0.9021 | 0.9256 |
| LDL (mg/dl) | 97.87 | 30.08 | 74.35 * | 17.09 | 82.09 | 23.26 | 68.62 * | 21.26 | 73.11 | 20.19 | 72.89 | 16.98 | 0.0488 | 0.0015 | 0.3238 | 0.5094 | 0.9604 | 0.6557 |
| HDL (mg/dl) | 54.65 | 12.58 | 52.48 | 11.98 | 58.53 | 15.84 | 58.88 | 15.06 | 62.93 | 12.58 | 57.71 | 11.43 | 0.5621 | 0.0955 | 0.4375 | 0.1822 | 0.3470 | 0.9370 |
| Triglycerides (mg/dl) | 60.70 | 21.10 | 59.13 | 21.68 | 70.50 | 39.47 | 59.21 | 28.13 | 60.00 | 25.64 | 54.61 | 21.10 | 0.4741 | 0.9965 | 0.3849 | >0.9999 | 0.7914 | 0.7454 |
| Glucose (mg/dl) | 82.61 | 6.34 | 76.57 * | 7.55 | 81.62 | 8.35 | 77.94 | 10.18 | 86.39 | 6.45 | 77.46 * | 6.60 | 0.8685 | 0.1585 | 0.0309 | 0.823 | 0.9262 | 0.9741 |
| Insulin (μIU/mL) | 12.43 | 6.04 | 15.58 | 8.00 | 9.04 | 4.24 | 10.04 | 3.92 | 10.20 | 4.07 | 8.51 | 4.19 | 0.0277 | 0.2243 | 0.6109 | 0.0009 | <0.0001 | 0.5181 |
| KIDMED | SET 1 | SET 2 | SET 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Subject Group A | (22 vs. 21) | (12 vs. 11) | (4 vs. 5) | |||||||
| Parameters | Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Total cholesterol (mg/dl) | T0 | 163.82 | 28.92 | 0.0032 | 163.42 | 30.66 | 0.0328 | 144.33 | 20.77 | 0.3039 |
| T1 | 139.90 | 20.24 | 137.64 | 22.35 | 128.20 | 22.33 | ||||
| LDL (mg/dl) | T0 | 75.19 | 17.73 | 0.0057 | 74.73 | 15.72 | 0.0737 | 82.00 | 24.60 | 0.6626 |
| T1 | 97.36 | 30.69 | 96.25 | 32.92 | 75.80 | 16.33 | ||||
| HDL (mg/dl) | T0 | 54.18 | 12.67 | 0.8071 | 55.25 | 13.50 | 0.4592 | 48.83 | 15.59 | 0.2687 |
| T1 | 53.24 | 12.40 | 50.82 | 14.68 | 39.40 | 7.57 | ||||
| Triglycerides (mg/dl) | T0 | 61.50 | 21.23 | 0.5205 | 60.08 | 22.17 | 0.9918 | 65.83 | 15.97 | 0.9176 |
| T1 | 57.52 | 18.90 | 60.00 | 13.13 | 64.80 | 12.95 | ||||
| Glucose (mg/dl) | T0 | 82.95 | 6.26 | 0.0019 | 83.17 | 6.78 | 0.0070 | 83.17 | 6.78 | 0.2497 |
| T1 | 75.90 | 7.63 | 73.91 | 8.08 | 75.80 | 9.98 | ||||
| Insulin (μIU/mL) | T0 | 15.58 | 8.18 | 0.6209 | 15.39 | 8.73 | 0.9080 | 19.45 | 4.78 | 0.2151 |
| T1 | 14.41 | 7.15 | 14.98 | 9.02 | 11.03 | 9.12 | ||||
| Subject Group B | (30 vs. 31) | (20 vs. 22) | (5 vs. 4) | |||||||
| Parameters | Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Total cholesterol (mg/dl) | T0 | 155.53 | 27.93 | 0.0135 | 151.75 | 31.21 | 0.2266 | 149.00 | 38.33 | 0.5062 |
| T1 | 137.97 | 25.89 | 141.95 | 18.23 | 134.250 | 18.428 | ||||
| LDL (mg/dl) | T0 | 83.10 | 22.35 | 0.0059 | 82.40 | 24.55 | 0.0636 | 83.80 | 37.83 | 0.6351 |
| T1 | 67.16 | 21.24 | 70.09 | 16.90 | 72.750 | 25.786 | ||||
| HDL (mg/dl) | T0 | 58.63 | 15.83 | 0.9520 | 54.90 | 16.98 | 0.4341 | 53.80 | 11.71 | 0.6138 |
| T1 | 58.87 | 15.18 | 58.91 | 15.91 | 50.250 | 7.182 | ||||
| Triglycerides (mg/dl) | T0 | 60.03 | 29.27 | 0.3411 | 64.82 | 29.91 | 0.4705 | 56.80 | 33.84 | 0.9918 |
| T1 | 68.27 | 32.17 | 71.20 | 35.19 | 57.000 | 17.010 | ||||
| Glucose (mg/dl) | T0 | 81.10 | 8.01 | 0.1882 | 81.50 | 8.31 | 0.0392 | 81.50 | 8.31 | 0.1367 |
| T1 | 77.94 | 10.34 | 76.27 | 7.59 | 72.75 | 8.34 | ||||
| Insulin (μIU/mL) | T0 | 9.04 | 4.51 | 0.3492 | 7.80 | 4.56 | 0.1327 | 7.80 | 4.56 | 0.1610 |
| T1 | 10.06 | 3.92 | 9.86 | 4.14 | 12.55 | 3.70 | ||||
| Subject Group C | (26 vs. 26) | (19 vs. 20) | (11 vs. 8) | |||||||
| Parameters | Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Total cholesterol (mg/dl) | T0 | 146.92 | 23.48 | 0.5348 | 149.58 | 22.04 | 0.4678 | 151.73 | 19.98 | 0.1215 |
| T1 | 142.73 | 24.84 | 143.85 | 26.41 | 136.125 | 21.464 | ||||
| LDL (mg/dl) | T0 | 71.58 | 18.00 | 0.6898 | 73.68 | 17.42 | 0.8412 | 73.64 | 19.13 | 0.5001 |
| T1 | 73.50 | 16.45 | 72.60 | 16.01 | 68.125 | 14.066 | ||||
| HDL (mg/dl) | T0 | 63.62 | 12.55 | 0.1049 | 64.32 | 12.86 | 0.2770 | 65.36 | 14.04 | 0.2492 |
| T1 | 58,04 | 11,80 | 60,35 | 12,44 | 58,56 | 8.73 | ||||
| Triglycerides (mg/dl) | T0 | 59.12 | 25.50 | 0.5850 | 58.32 | 27.82 | 0.5363 | 64.18 | 32.79 | 0.1972 |
| T1 | 55.42 | 21.56 | 53.80 | 22.80 | 46.750 | 19.002 | ||||
| Glucose (mg/dl) | T0 | 86.62 | 6.64 | 0.0001 | 86.74 | 7.23 | 0.0001 | 86.74 | 7.23 | 0.0019 |
| T1 | 77.46 | 6.60 | 76.30 | 6.11 | 76.88 | 4.22 | ||||
| Insulin (μIU/mL) | T0 | 10.19 | 4.21 | 0.1555 | 10.03 | 4.49 | 0.1817 | 10.03 | 4.49 | 0.2151 |
| T1 | 8.51 | 4.19 | 8.11 | 4.32 | 7.10 | 3.81 | ||||
| KIDMED | SET 4 | SET 5 | SET 6 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Subject Group A | (21 vs. 22) | (17 vs. 21) | (7 vs. 10) | |||||||
| Parameters | Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Total cholesterol (mg/dl) | T0 | 160.38 | 25.18 | 0.0014 | 156.76 | 23.80 | 0.0066 | 161.14 | 20.71 | 0.0024 |
| T1 | 137.09 | 19.09 | 136.57 | 19.40 | 128.60 | 16.22 | ||||
| LDL (mg/dl) | T0 | 94.62 | 28.96 | 0.0052 | 89.94 | 27.97 | 0.0257 | 91.71 | 29.47 | 0.0251 |
| T1 | 73.32 | 17.16 | 72.71 | 17.34 | 66.00 | 12.42 | ||||
| HDL (mg/dl) | T0 | 53.67 | 12.68 | 0.6915 | 55.47 | 12.96 | 0.4449 | 57.57 | 16.28 | 0.3317 |
| T1 | 52.14 | 12.42 | 52.24 | 12.72 | 50.40 | 13.19 | ||||
| Triglycerides (mg/dl) | T0 | 60.86 | 22.10 | 0.6942 | 57.41 | 20.05 | 0.9232 | 61.14 | 24.33 | 0.9703 |
| T1 | 58.18 | 22.20 | 58.10 | 22.75 | 60.70 | 23.31 | ||||
| Glucose (mg/dl) | T0 | 83.29 | 6.20 | 0.0052 | 83.71 | 6.02 | 0.0034 | 82.43 | 4.58 | 0.0566 |
| T1 | 77.09 | 7.46 | 76.71 | 7.43 | 75.30 | 8.23 | ||||
| Insulin (μIU/mL) | T0 | 12.66 | 6.28 | 0.2699 | 13.00 | 6.69 | 0.4122 | 10.94 | 3.43 | 0.1042 |
| T1 | 15.14 | 8.09 | 15.06 | 8.28 | 16.40 | 7.77 | ||||
| Subject Group B | (29 vs. 29) | (22 vs. 27) | (11 vs. 12) | |||||||
| Parameters | Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Total cholesterol (mg/dl) | T0 | 155.41 | 30.90 | 0.0454 | 158.32 | 28.29 | 0.0406 | 168.64 | 26.09 | 0.0264 |
| T1 | 139.39 | 28.67 | 141.15 | 28.44 | 140.73 | 29.63 | ||||
| LDL (mg/dl) | T0 | 81.79 | 24.43 | 0.0437 | 82.82 | 22.78 | 0.0714 | 87.09 | 19.80 | 0.0473 |
| T1 | 69.04 | 22.63 | 70.88 | 22.32 | 67.82 | 23.67 | ||||
| HDL (mg/dl) | T0 | 58.93 | 16.51 | 0.9399 | 60.59 | 16.40 | 0.5877 | 66.27 | 17.98 | 0.4931 |
| T1 | 58.61 | 16.04 | 58.04 | 16.18 | 60.64 | 20.53 | ||||
| Triglycerides (mg/dl) | T0 | 72.97 | 42.15 | 0.1542 | 74.09 | 44.48 | 0.2355 | 75.18 | 30.10 | 0.4009 |
| T1 | 59.04 | 30.35 | 61.19 | 30.44 | 62.64 | 39.01 | ||||
| Glucose (mg/dl) | T0 | 81.97 | 8.29 | 0.2480 | 82.50 | 7.28 | 0.2710 | 78.73 | 6.12 | 0.6824 |
| T1 | 79.04 | 10.67 | 79.46 | 10.97 | 77.45 | 8.31 | ||||
| Insulin (μIU/mL) | T0 | 9.11 | 4.23 | 0.7112 | 8.52 | 3.41 | 0.3300 | 8.05 | 3.52 | 0.3027 |
| T1 | 9.50 | 3.74 | 9.56 | 3.87 | 9.58 | 3.39 | ||||
| Subject Group C | (23 vs. 26) | (16 vs. 20) | (12 vs. 9) | |||||||
| Parameters | Mean | SD | p-Value | Mean | SD | p-Value | Mean | SD | p-Value | |
| Total cholesterol (mg/dl) | T0 | 146.26 | 23.22 | 0.6615 | 146.63 | 25.11 | 0.7159 | 140.33 | 21.80 | 0.9923 |
| T1 | 143.23 | 24.70 | 143.40 | 27.03 | 140.44 | 30.50 | ||||
| LDL (mg/dl) | T0 | 72.22 | 21.45 | 0.7994 | 70.38 | 23.43 | 0.6938 | 65.17 | 14.90 | 0.6434 |
| T1 | 73.62 | 16.79 | 73.15 | 18.53 | 69.00 | 22.49 | ||||
| HDL (mg/dl) | T0 | 62.09 | 12.64 | 0.3165 | 64.25 | 14.34 | 0.2951 | 63.33 | 14.60 | 0.4158 |
| T1 | 58.62 | 11.37 | 59.50 | 12.45 | 58.00 | 14.46 | ||||
| Triglycerides (mg/dl) | T0 | 60.17 | 27.71 | 0.4246 | 59.88 | 31.40 | 0.4767 | 59.50 | 26.75 | 0.4517 |
| T1 | 54.54 | 21.15 | 53.55 | 21.24 | 67.67 | 19.89 | ||||
| Glucose (mg/dl) | T0 | 86.96 | 4.78 | 0.0001 | 86.38 | 5.21 | 0.0001 | 86.58 | 5.12 | 0.0054 |
| T1 | 77.35 | 6.79 | 77.05 | 6.96 | 78.89 | 6.11 | ||||
| Insulin (μIU/mL) | T0 | 10.78 | 3.04 | 0.0274 | 10.83 | 3.37 | 0.0338 | 10.63 | 3.65 | 0.3497 |
| T1 | 8.51 | 3.85 | 8.06 | 3.98 | 9.10 | 3.60 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ceraudo, F.; Caparello, G.; Galluccio, A.; Avolio, E.; Augimeri, G.; De Rose, D.; Vivacqua, A.; Morelli, C.; Barone, I.; Catalano, S.; et al. Impact of Mediterranean Diet Food Choices and Physical Activity on Serum Metabolic Profile in Healthy Adolescents: Findings from the DIMENU Project. Nutrients 2022, 14, 881. https://doi.org/10.3390/nu14040881
Ceraudo F, Caparello G, Galluccio A, Avolio E, Augimeri G, De Rose D, Vivacqua A, Morelli C, Barone I, Catalano S, et al. Impact of Mediterranean Diet Food Choices and Physical Activity on Serum Metabolic Profile in Healthy Adolescents: Findings from the DIMENU Project. Nutrients. 2022; 14(4):881. https://doi.org/10.3390/nu14040881
Chicago/Turabian StyleCeraudo, Fabrizio, Giovanna Caparello, Angelo Galluccio, Ennio Avolio, Giuseppina Augimeri, Daniela De Rose, Adele Vivacqua, Catia Morelli, Ines Barone, Stefania Catalano, and et al. 2022. "Impact of Mediterranean Diet Food Choices and Physical Activity on Serum Metabolic Profile in Healthy Adolescents: Findings from the DIMENU Project" Nutrients 14, no. 4: 881. https://doi.org/10.3390/nu14040881
APA StyleCeraudo, F., Caparello, G., Galluccio, A., Avolio, E., Augimeri, G., De Rose, D., Vivacqua, A., Morelli, C., Barone, I., Catalano, S., Giordano, C., Sisci, D., & Bonofiglio, D. (2022). Impact of Mediterranean Diet Food Choices and Physical Activity on Serum Metabolic Profile in Healthy Adolescents: Findings from the DIMENU Project. Nutrients, 14(4), 881. https://doi.org/10.3390/nu14040881