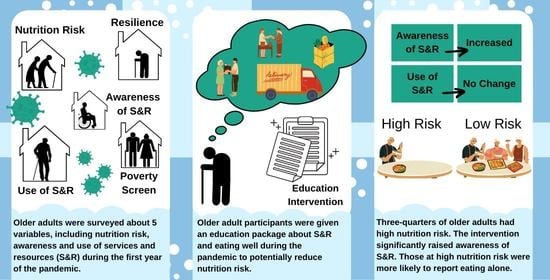
Nutrition Risk, Resilience and Effects of a Brief Education Intervention among Community-Dwelling Older Adults during the COVID-19 Pandemic in Alberta, Canada
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Design
2.3. Outcomes
2.4. Intervention
2.5. Statistical Analyses
3. Results
3.1. Baseline Characteristics
3.2. Effect of Intervention on Resilience, Nutrition Risk, S and R Awareness and Use
3.3. Nutrition Risk Behaviors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Borkent, J.W.; Keller, H.; Wham, C.; Wijers, F.; de van der Schueren, M.A.E. Cross-country differences and similarities in undernutrition prevalence and risk as measured by SCREEN II in community-dwelling older adults. Healthcare 2020, 8, 151. [Google Scholar] [CrossRef] [PubMed]
- Keller, H.H.; Ostbye, T. Nutritional risk and time to death; predictive validity of SCREEN (Seniors in the Community Risk Evaluation for Eating and Nutrition). J. Nutr. Health Aging 2003, 7, 274–279. [Google Scholar]
- Keller, H.H.; Ostbye, T.; Goy, R. Nutritional risk predicts quality of life in elderly community-living Canadians. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, M68–M74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keller, H.H.; Hedley, M.R.; Wong Brownlee, S. The development of Seniors in the Community: Risk Evaluation for Eating and Nutrition (SCREEN). Can. J. Diet. Pract. Res. 2000, 61, 67–72. [Google Scholar] [PubMed]
- Keller, H.H. Promoting food intake in older adults living in the community: A review. Appl. Physiol. Nutr. Metab. 2007, 32, 991–1000. [Google Scholar] [CrossRef]
- Sahyoun, N.R.; Zhang, X.L.; Serdula, M.K. Barriers to the consumption of fruits and vegetables among older adults. J. Nutr. Elder. 2006, 24, 5–21. [Google Scholar] [CrossRef]
- Appleton, K.M. Barriers to and facilitators of the consumption of animal-based protein-rich foods in older adults. Nutrients 2016, 8, 187. [Google Scholar] [CrossRef] [Green Version]
- Villalon, L.; Dupuis-Blanchard, S.; Gibbons, C.; Gould, O.; Simard, M. Food related challenges and issues faced by New Brunswick seniors living in their own home. J. Gerontol. Geriatr. Res. 2015, 4, 2. [Google Scholar]
- Wei, K.; Nyunt, M.; Gao, Q.; Wee, S.L.; Yap, K.B.; Ng, T.P. Association of frailty and malnutrition with long-term functional and mortality outcomes among community-dwelling older adults. Results from the Singapore Longitudinal Aging Study 1. JAMA Netw. Open 2018, 1, e180650. [Google Scholar] [CrossRef] [Green Version]
- De Biasio, J.C.; Mittel, A.M.; Mueller, A.L.; Ferrante, L.E.; Kim, D.H.; Shaefi, S. Frailty in critical care medicine: A review. Anesth. Analg. 2020, 130, 1462–1473. [Google Scholar] [CrossRef]
- Higgins, M.M.; Barkley, M.C. Improving effectiveness of nutrition education resources for older adults. J. Nutr. Elder. 2004, 23, 19–54. [Google Scholar] [CrossRef] [PubMed]
- Worsley, A. Nutrition knowledge and food consumption: Can nutrition knowledge change food behaviour? Asia Pac. J. Clin. Nutr. 2002, 11, S579–S585. [Google Scholar] [CrossRef] [Green Version]
- Di Santo, S.G.; Franchini, F.; Filiputti, B.; Martone, A.; Sannino, S. The effects of COVID-19 and quarantine measures on the lifestyles and mental health of people over 60 at increased risk of dementia. Front. Psychiatry 2020, 11, 578628. [Google Scholar] [CrossRef] [PubMed]
- Briguglio, M.; Giorgino, R.; Dell’Osso, B.; Cesari, M.; Porta, M.; Lattanzio, F.; Banfi, G.; Peretti, G.M. Consequences for the elderly after COVID-19 isolation: FEaR (Frail Elderly amid Restrictions). Front. Psychol. 2020, 28, 565052. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.; Monaco, A.; Kivipelto, M.; Onder, G.; Maggi, S.; Michel, J.-P.; Prieto, R.; Sykara, G.; Donde, S. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: Consequences for healthy ageing. Aging Clin. Exp. Res. 2020, 32, 1184–1194. [Google Scholar] [CrossRef]
- Steinman, M.A.; Perry, L.; Perissinotto, C.M. Meeting the care needs of older adults isolated at home during the COVID-19 pandemic. JAMA Int. Med. 2020, 180, 819–820. [Google Scholar] [CrossRef] [Green Version]
- Akbar, A.N.; Gilroy, D.W. Aging immunity may exacerbate COVID-19. Science 2020, 369, 256–257. [Google Scholar] [CrossRef]
- Silverio, R.; Goncalves, D.C.; Andrade, M.F.; Seelaender, M. Coronavirus disease 2019 (COVID-19) and nutritional status: The missing link? Adv. Nutr. 2020, 12, 682–692. [Google Scholar] [CrossRef]
- Alberta211. 211 Data for System Navigation and Planning. 2020. Available online: https://ab.211.ca/how-we-help/211-data/.
- Kriaucioniene, V.; Bagdonaviciene, L.; Rodriguez-Perez, C.; Petkeviciene, J. Associations between changes in health behaviours and body weight during the COVID-19 quarantine in Lithuania: The Lithuanian COVIDiet Study. Nutrients 2020, 12, 3119. [Google Scholar] [CrossRef]
- Pfeifer, D.; Resetar, J.; Gajdos Kljuisuric, J.; Panjkota Krbavcic, I.; Vranesic Bender, D.; Rodriguez-Perez, C.; Ruiz-Lopez, M.D.; Satalic, Z. Cooking at home and adherence to the Mediterranean Diet during the COVID-19 confinement: The experience from the Croation COVIDiet Study. Front. Nutr. 2021, 8, 617721. [Google Scholar] [CrossRef]
- Rodriguez-Perez, C.; Molina-Montes, E.; Verardo, V.; Artacho, R.; Garcia-Villanova, B.; Guerra-Hernandez, E.J.; Ruiz-Lopez, M.D. Changes in dietary behaviours during the COVID-19 outbreak confinement in the Spanish COVIDiet Study. Nutrients 2020, 12, 1730. [Google Scholar] [CrossRef] [PubMed]
- Sulejmani, E.; Hyseni, A.; Xhabiri, G.; Rodriguez-Perez, C. Relationship in dietary habits variations during COVID-19 lockdown in Kosovo: The COVIDiet study. Appetite 2021, 164, 105244. [Google Scholar] [CrossRef] [PubMed]
- Giacalone, D.; Bom Frost, M.; Rodriguez-Perez, C. Reported changes in dietary habits during the COVID-19 lockdown in the Danish population: The Danish COVIDiet Study. Front. Nutr. 2020, 7, 592112. [Google Scholar] [CrossRef] [PubMed]
- Lamarche, B.; Brassard, D.; Lapointe, A.; Laramee, C.; Kearney, M.; Cote, M.; Belanger-Gravel, A.; Desroches, S.; Lemieux, S.; Plante, C. Changes in diet quality and food security among adults during the COVID-19-related early lockdown: Results from NutriQuébec. Am. J. Clin. Nutr. 2021, 113, 984–992. [Google Scholar] [CrossRef]
- Wu, G.; Feder, A.; Cohen, H.; Kim, J.J.; Calderon, S.; Charney, D.S.; Mathe, A.A. Understanding resilience. Front. Behav. Neurosci. 2013, 7, 10. [Google Scholar] [CrossRef] [Green Version]
- Mancini, A.D.; Bonanno, G.A. Predictors and parameters of resilience to loss: Toward an individual differences model. J. Pers. 2009, 77, 1805–1832. [Google Scholar] [CrossRef] [Green Version]
- Vesnaver, E.; Keller, H.H.; Payette, H.; Shatenstein, B. Dietary resilience as described by older community-dwelling adults from the NuAge study “If there is a will—There is a way!”. Appetite 2012, 58, 730–738. [Google Scholar] [CrossRef]
- Smith, B.W.; Dalen, J.; Wiggins, K.; Tooley, E.; Christopher, P.; Bernard, J. The brief resilience scale: Assessing the ability to bounce back. Int. J. Behav. Med. 2008, 15, 194–200. [Google Scholar] [CrossRef]
- World Health Organization. Regional Office for Europe. Survey Tool and Guidance: Rrapid, Simple, Flexible Behavioural Insights on COVID-19: 29 July 2020. Available online: https://apps.who.int/iris/handle/10665/333549 (accessed on 3 January 2022).
- Keller, H.; Goy, R.; Kane, S.L. Validity and reliability of SCREEN II (Seniors in the Community: Risk evaluation for eating and nutrition, Version II). Eur. J. Clin. Nutr. 2005, 59, 1149–1157. [Google Scholar] [CrossRef] [Green Version]
- Brcic, V.; Eberdt, C.; Kaczorowski, J. Development of a tool to identify poverty in a family practice setting: A pilot study. Int. J. Fam. Med. 2011, 2011, 812182. [Google Scholar] [CrossRef] [Green Version]
- Nutrition Resources. Stay Strong with Nutrition: Seniors and COVID-19. Available online: https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-stay-strong-with-nutrition-seniors.pdf (accessed on 10 February 2022).
- Nutrition Resources. COVID-19: Nutrition for Recovery. Available online: https://www.albertahealthservices.ca/assets/info/ppih/if-ppih-covid-19-nutrition-for-recovery.pdf (accessed on 10 February 2022).
- Alvarado, S.; Hussey, E.; Dobbs, B.M. A Guide to Mobility and Independence: A Comprehensive Listing of Essential Services and Transportation Providers in Edmonton and Outlying Communities, 10th ed.; The DR Group: Edmonton, AB, Canada, 2020. [Google Scholar]
- Kurtz, A.; Grant, K.; Marano, R.; Arrieta, A.; Grant, K., Jr.; Feaster, W.; Steele, C.; Ehwerhemuepha, L. Long-term effects of malnutrition on severity of COVID-19. Sci. Rep. 2021, 11, 14974. [Google Scholar] [CrossRef] [PubMed]
- Lengele, L.; Locquet, M.; Moutschen, M.; Beaudart, C.; Kaux, J.-F.; Gillain, S.; Reginster, J.-Y.; Bruyere, O. Frailty but not sarcopenia nor malnutrition increases the risk of developing COVID-19 in older community-dwelling adults. Aging Clin. Exp. Res. 2021, 34, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Ghanem, J.; Colicchio, B.; Andres, E.; Geny, B.; Dieterlen, A. Lockdown effect on elderly nutritional health. J. Clin. Med. 2021, 10, 5052. [Google Scholar] [CrossRef]
- Chmitorz, A.; Wenzel, M.; Stieglitz, R.-D.; Kunzler, A.; Bagusat, C.; Helmreich, I.; Gerlicher, A.; Kampa, M.; Kubiak, T.; Kalisch, R.; et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS ONE 2018, 13, e0192761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gilmore, H.; Ramage-Morin, P.L. Social isolation and mortality among Canadian seniors. Health Rep. 2020, 31, 27–38. [Google Scholar]
- Taylor, M.G.; Carr, D.C.; Jason, K. Financial hardship and psychological resilience during COVID-19: Differences by race/ethnicity. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021, gbab173. [Google Scholar] [CrossRef]
- McIntyre, L.; Dutton, D.J.; Kwok, C.; Emery, J.C.H. Reduction of food insecurity among low-income Canadian seniors as a likely impact of a Guaranteed Annual Income. Can. Public Policy 2016, 42, 274–286. [Google Scholar] [CrossRef]
- Statistics Canada. Table 11-10-0239-01 Income of Individuals by Age Group, Sex and Income Source, Canada, Provinces and Selected Census Metropolitan Areas; Statistics Canada: Ottawa, ON, Canada, 2021. [CrossRef]
- Bloom, I.; Lawrence, W.; Barker, M.; Baird, J.; Dennison, E.; Aihie Sayer, A.; Cooper, C.; Robinson, S. What influences diet quality in older people? A qualitative study among community-dwelling older adults from the Hertfordshire Cohort Study, UK. Public Health Nutr. 2017, 20, 2685–2693. [Google Scholar] [CrossRef] [Green Version]
- Green-Lapierre, R.J.; Williams, P.L.; Glanville, N.T.; Norris, D.; Hunter, H.C.; Watt, C.G. Learning from “knocks in life”: Food insecurity among low-income lone senior women. J. Aging Res. 2012, 2012, 450630. [Google Scholar] [CrossRef] [Green Version]
- Robinson, S.M. Improving nutrition to support healthy ageing: What are the opportunities for intervention? Proc. Nutr. Soc. 2018, 77, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Chan, C.B.; Popeski, N.; Gramlich, L.; Atkins, M.; Basualdo-Hammond, C.; Stadnyk, J.; Keller, H. Harnessing stakeholder perspectives and experience to address nutrition risk in community-dwelling older adults. Healthcare 2021, 9, 477. [Google Scholar] [CrossRef] [PubMed]
- Middleton, G.; Mehta, K.; McNaughton, D.; Booth, S. The experiences and perceptions of food banks amongst users in high-income countries: An international scoping review. Appetite 2018, 120, 698–708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarasuk, V.; Fafard St-Germain, A.A.; Loopstra, R. The relationship between food banks and food insecurity: Insights from Canada. Voluntas 2020, 31, 841–852. [Google Scholar] [CrossRef] [Green Version]
- Neter, J.E.; Kijkstra, S.C.; Twisk, J.; Visser, M.; Brouwer, I.A. Improving the dietary quality of food parcels leads to improved dietary intake in Dutch food bank recipients—Effects of a randomized controlled trial. Eur. J. Nutr. 2020, 59, 3491–3501. [Google Scholar] [CrossRef] [Green Version]
- Heasley, C.; Clayton, B.; Muileboom, J.; Schwanke, A.; Rathnayake, S.; Richter, A.; Little, M. “I was eating more fruits and veggies than I have in years”: A mixed methods evaluation of a fresh food prescription intervention. Arch. Public Health 2021, 79, 135. [Google Scholar] [CrossRef]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 151–171. [Google Scholar] [CrossRef] [Green Version]
- Donini, L.M.; Savina, C.; Cannella, C. Eating habits and appetite control in the elderly: The anorexia of aging. Int. Psychogeriatr. 2003, 15, 73–87. [Google Scholar] [CrossRef]
- Donnelly, R.; Keller, H. Challenges providing nutrition care during the COVID-19 pandemic: Canadian dietitian perspectives. J. Nutr. Health Aging 2021, 25, 710–711. [Google Scholar] [CrossRef]
- Taylor-Davis, S.; Smiciklas-Wright, H.; Warland, R.; Achterberg, C.; Jensen, G.L.; Sayer, A.; Shannon, B. Responses of older adults to theory-based nutrition newsletters. J. Am. Diet. Assoc. 2000, 100, 656–664. [Google Scholar] [CrossRef]
- Chan, C.B.; Popeski, N.; Fatehi-Hassanabad, M.; Sigal, R.J.; O’Connell, P.; Sargious, P. Use of virtual care for glycemic management in people with types 1 and 2 diabetes and diabetes in pregnancy: A rapid review. Can. J. Diabetes 2021, 45, 677–688. [Google Scholar] [CrossRef]
| Characteristic | Men (N = 13) | Women (N = 15) | Total (N = 28) | p-Value (Men vs. Women) |
|---|---|---|---|---|
| Age, years ± SD (range) | 73.5 ± 5.5 (65–82) | 71.7 ± 6.4 (65–86) | 72.6 ± 6.0 (65–86) | 0.44 |
| Living situation, n (%) | ||||
| Alone | 5 (38%) | 7 (47%) | 12 (43%) | 0.72 |
| With spouse | 8 (62%) | 8 (53%) | 16 (57%) | |
| Currently or previously self-isolated because of COVID-19 restrictions, n (%) | ||||
| Currently | 8 (62%) | 14 (93%) | 22 (79%) | |
| Previously | 5 (38%) | 1 (7%) | 6 (21%) | 0.07 |
| Currently or previously quarantined because of COVID-19 restrictions, n (%) | ||||
| Currently | 0 (0%) | 2 (13%) | 2 (7%) | |
| Previously | 3 (23%) | 3 (20%) | 7 (25%) | |
| Never | 10 (77%) | 10 (67%) | 19 (68%) | 0.39 |
| Annual income, CAD $ ± SD | 94,367 ± 89,592 | 48,387 ± 27,783 | 69,734 ± 67,179 | 0.08 |
| Financial screen—Yes, n (%) | -- | -- | 3 (11%) | |
| Food insecurity screen—Yes, n (%) | -- | -- | ||
| Resilience ± SD (score) | 3.9 ± 0.5 | 3.3 ± 1.0 | 1 (4%) | 0.06 |
| Nutrition risk ± SD (score) | 44.9 ± 8.9 | 44.2 ± 10.3 | 44.6 ± 9.5 | 0.85 |
| Nutrition Risk | p-Value | ||||||
|---|---|---|---|---|---|---|---|
| Baseline | Post | ||||||
| Nutrition Risk Score | SCREEN-14 Score (Mean ± SD) | 44.6 ± 9.5 | 44.6 ± 9.7 | 0.96 | |||
| Awareness of S and R | p-Value | Use of S and R | p-Value | ||||
| Baseline | Post | Baseline | Post | ||||
| Services and Resources * | Composite score (mean ± SD) | 10 ± 4 | 11 ± 4 | 0.01 | 2 ± 2 | 3 ± 2 | 0.57 |
| N (%) | N (%) | N (%) | N (%) | ||||
| Transportation or Food Delivery | All (mean of 5 S and R) | 11 (39) | 21 (75) | 0.01 | 4 (14) | 3 (11) | 1.0 |
| Transportation services | 16 (57) | 18 (64) | 0.79 | 4 (14) | 3 (11) | 1.0 | |
| Restaurant or fast-food delivery | 28 (100) | 28 (100) | 1.0 | 8 (29) | 8 (29) | 1.0 | |
| Online grocery shopping and/or delivery | 27 (96) | 28 (100) | 1.0 | 6 (21) | 7 (25) | 1.0 | |
| Meals on WheelsTM | 26 (93) | 28 (100) | 0.49 | 0 (0) | 0 (0) | 1.0 | |
| Bag Half FullTM | 1 (4) | 2 (7) | 1.0 | 0 (0) | 0 (0) | 1.0 | |
| Telephone Services | All (mean of 3 S and R) | 15 (55) | 17 (62) | 0.79 | 5 (17) | 3 (11) | 0.71 |
| Alberta 211 Helpline | 17 (61) | 17 (61) | 1.0 | 2 (7) | 2 (7) | 1.0 | |
| Health Link 811 | 27 (96) | 27 (96) | 1.0 | 12 (28) | 8 (29) | 0.40 | |
| Rehabilitation Advice Line | 2 (7) | 4 (14) | 0.67 | 0 (0) | 0 (0) | 1.0 | |
| Websites | All (mean of 4 S and R) | 7 (25) | 9 (32) | 0.79 | 4 (14) | 4 (14) | 1.0 |
| Healthy Aging CORETM | 2 (7) | 4 (14) | 0.67 | 0 (0) | 1 (4) | 1.0 | |
| MyHealth Alberta | 15 (54) | 17 (61) | 0.79 | 11 (39) | 11 (39) | 1.0 | |
| AHS “Healthy Eating Starts Here” | 9 (32) | 11 (39) | 0.78 | 3 (11) | 4 (14) | 1.0 | |
| Communities ChoosewellTM | 1 (4) | 3 (11) | 0.61 | 0 (0) | 0 (0) | 1.0 | |
| Nutrition Counselling | All (mean of 5 S and R) | 13 (46) | 16 (57) | 0.59 | 3 (11) | 5 (18) | 0.71 |
| Family doctor | 18 (64) | 19 (68) | 1.0 | 7 (25) | 7 (25) | 1.0 | |
| AHS nutrition counselling | 13 (46) | 17 (61) | 0.42 | 3 (11) | 6 (21) | 0.47 | |
| City of Edmonton nutrition services | 3 (11) | 8 (29) | 0.18 | 0 (0) | 0 (0) | 1.0 | |
| Dietitians of Canada or other online directories to find a Registered Dietitian | 13 (46) | 17 (61) | 0.42 | 3 (11) | 4 (14) | 1.0 | |
| Primary care network-based nutrition counselling | 17 (61) | 17 (61) | 1.0 | 3 (11) | 7 (25) | 0.30 | |
| Food Security | All (mean of 3 S and R) | 14 (50) | 17 (61) | 0.59 | <1 (1) | 1 (4) | 1.0 |
| Food banks/food hampers | 24 (86) | 25 (89) | 1.0 | 0 (0) | 0 (0) | 1.0 | |
| Community groups providing low-cost prepared or frozen meals | 17 (61) | 21 (75) | 0.39 | 1 (4) | 2 (7) | 1.0 | |
| Free Food in Alberta directory | 1 (4) | 6 (21) | 0.10 | 0 (0) | 1 (4) | 1.0 | |
| Nutrition Risk Factor | Education Provided in Handouts | High Risk (N = 21) | Low Risk (N = 7) | p-Value |
|---|---|---|---|---|
| Inadequate servings of milk, milk products, soy | Yes | 1.2 ± 1.2 | 2.6±1.0 | 0.02 |
| Perception that weight is more/less than it should be | Yes | 1.3 ± 0.19 | 1.1 ± 2.0 | 0.82 |
| Inadequate servings of fruits and vegetables | Yes | 1.9 ± 1.3 | 3.7 ± 0.5 | <0.01 |
| Eating alone | No | 1.9 ± 1.8 | 2.9 ± 2.0 | 0.24 |
| Limiting or avoiding foods | No | 2.0 ± 1.3 | 2.9 ± 1.1 | 0.12 |
| Inadequate protein intake | Yes | 2.0 ± 1.3 | 3.6 ± 0.5 | <0.01 |
| Weight gain/loss ≥ 5 l b | Yes | 2.6 ± 1.6 | 3.1 ± 1.5 | 0.41 |
| Skipping meals | Yes | 2.7 ± 1.5 | 4.0 ± 0 | 0.04 |
| Inadequate fluid intake | Yes | 2.9 ± 0.8 | 3.7 ± 0.5 | 0.02 |
| Difficulty with meal preparation | * | 3.0 ± 1.5 | 3.4 ± 1.0 | 0.44 |
| Coughing, choking or pain swallowing when eating | * | 3.1 ± 1.3 | 3.9 ± 0.4 | 0.16 |
| Unintentional weight gain/loss | Yes | 3.4 ± 1.4 | 4.0 ± 0 | 0.31 |
| Poor appetite | * | 3.5 ± 1.0 | 3.0 ± 0.8 | 0.23 |
| Difficulty chewing | * | 3.5 ± 1.0 | 4.0 ± 0 | 0.22 |
| Problems obtaining groceries | *# | 3.5 ± 1.0 | 4.0 ± 0 | 0.24 |
| Uses commercial meal replacements or supplements | Yes | 3.9 ± 0.9 | 3.7 ± 0.8 | 0.47 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capicio, M.; Panesar, S.; Keller, H.; Gramlich, L.; Popeski, N.; Basualdo-Hammond, C.; Atkins, M.; Chan, C.B. Nutrition Risk, Resilience and Effects of a Brief Education Intervention among Community-Dwelling Older Adults during the COVID-19 Pandemic in Alberta, Canada. Nutrients 2022, 14, 1110. https://doi.org/10.3390/nu14051110
Capicio M, Panesar S, Keller H, Gramlich L, Popeski N, Basualdo-Hammond C, Atkins M, Chan CB. Nutrition Risk, Resilience and Effects of a Brief Education Intervention among Community-Dwelling Older Adults during the COVID-19 Pandemic in Alberta, Canada. Nutrients. 2022; 14(5):1110. https://doi.org/10.3390/nu14051110
Chicago/Turabian StyleCapicio, Michelle, Simran Panesar, Heather Keller, Leah Gramlich, Naomi Popeski, Carlota Basualdo-Hammond, Marlis Atkins, and Catherine B. Chan. 2022. "Nutrition Risk, Resilience and Effects of a Brief Education Intervention among Community-Dwelling Older Adults during the COVID-19 Pandemic in Alberta, Canada" Nutrients 14, no. 5: 1110. https://doi.org/10.3390/nu14051110
APA StyleCapicio, M., Panesar, S., Keller, H., Gramlich, L., Popeski, N., Basualdo-Hammond, C., Atkins, M., & Chan, C. B. (2022). Nutrition Risk, Resilience and Effects of a Brief Education Intervention among Community-Dwelling Older Adults during the COVID-19 Pandemic in Alberta, Canada. Nutrients, 14(5), 1110. https://doi.org/10.3390/nu14051110