Obesity Risk-Factor Variation Based on Island Clusters: A Secondary Analysis of Indonesian Basic Health Research 2018
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Variables
2.3. Island Clusters
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
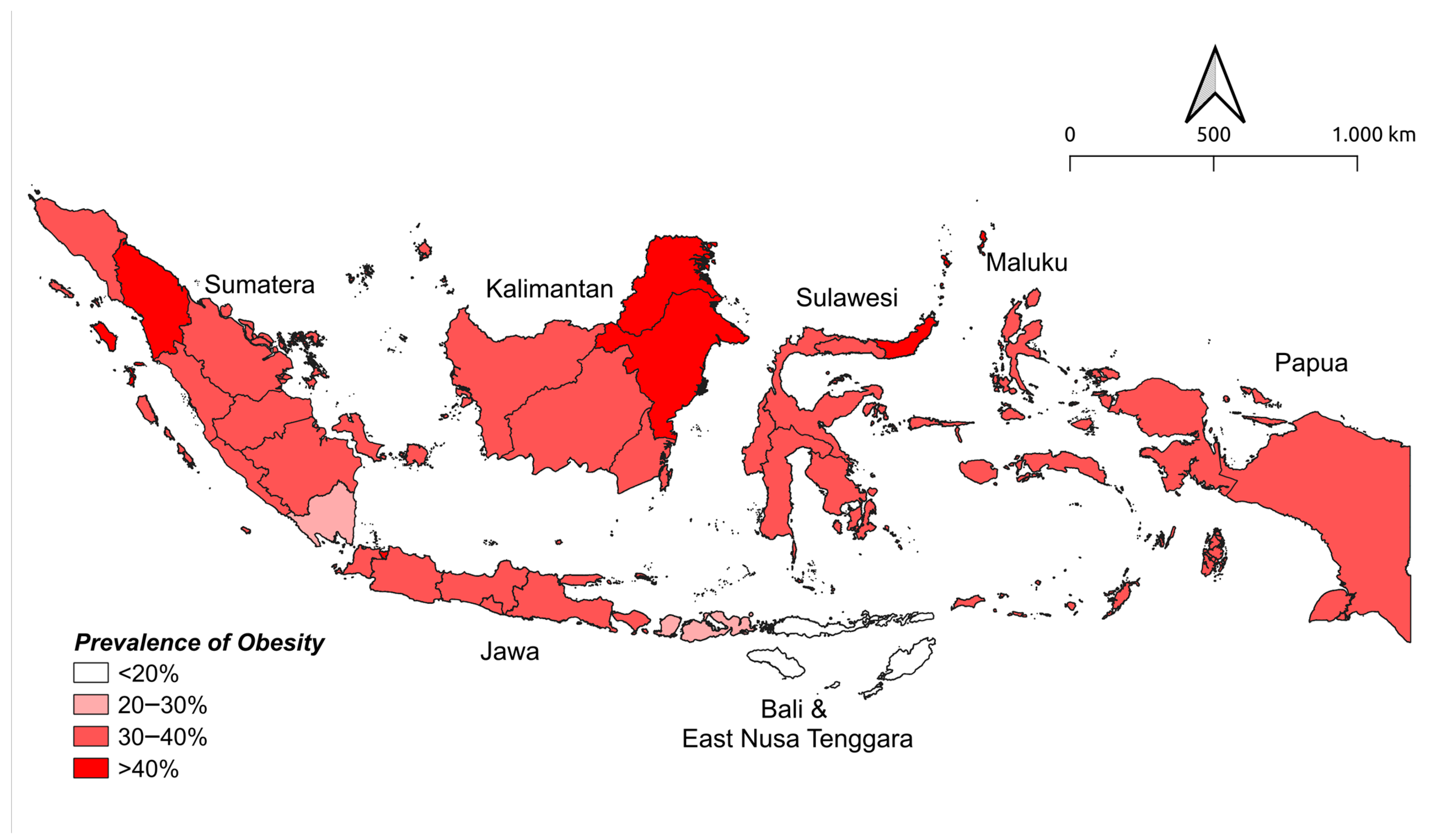
3.1. Prevalence of Obesity across Island Clusters
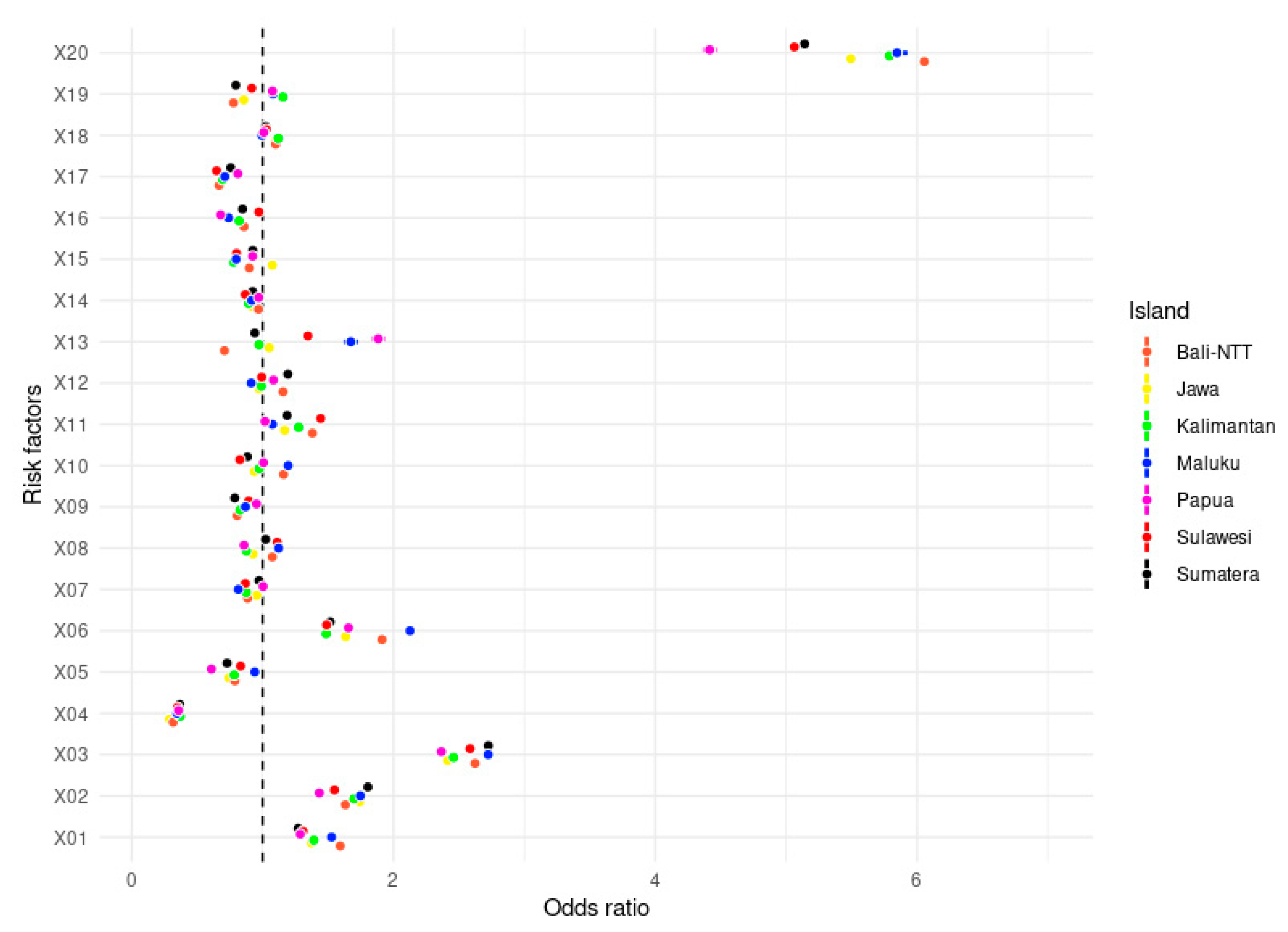
3.2. Cluster Variation of Obesity Risk Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 9 January 2022).
- MoH. Laporan Nasional Riset Kesehatan Dasar (Riskesdas) tahun 2018; MoH: Jakarta, Indonesia, 2019.
- MoH. Laporan Nasional Riset Kesehatan Dasar (RISKESDAS) tahun 2013; MoH: Jakarta, Indonesia, 2014.
- MoH. Laporan Nasional Riset Kesehatan Dasar (RISKESDAS) tahun 2007; MoH: Jakarta, Indonesia, 2008.
- Ferdowsy, F.; Rahi, K.S.A.; Jabiullah, M.I.; Habib, M.T. A machine learning approach for obesity risk prediction. Curr. Res. Behav. Sci. 2021, 2, 100053. [Google Scholar] [CrossRef]
- Safaei, M.; Sundararajan, E.A.; Driss, M.; Boulila, W.; Shapi’i, A. A systematic literature review on obesity: Understanding the causes & consequences of obesity and reviewing various machine learning approaches used to predict obesity. Comput. Biol. Med. 2021, 136, 104754. [Google Scholar] [CrossRef] [PubMed]
- Thamrin, S.A.; Arsyad, D.S.; Kuswanto, H.; Lawi, A.; Nasir, S. Predicting Obesity in Adults Using Machine Learning Techniques: An Analysis of Indonesian Basic Health. Front. Nutr. 2021, 8, 1–15. [Google Scholar] [CrossRef]
- Arundhana, A.I.; Utami, A.P.; Muqni, A.D.; Thalavera, M.T. Regional difference in obesity prevalence and associated factors among Indonesian adults. Malays. J. Nutr. 2018, 24, 193–201. [Google Scholar]
- MoH. Laporan Hasil Utama Riskesdas tahun 2018; MoH: Jakarta, Indonesia, 2019.
- WHO Regional Office for the Western Pacific. The Asia Pacific Perspective: Redefining Obesity and Its Treatment; Health Communications Australia Pty Limited: Sydney, Australia, 2000. [Google Scholar]
- Beusenberg, M.; Orley, J. A User’s Guide to the Self Reporting Questionnaire (SRQ); Division of Mental Health: Geneva, Switzerland, 1994. [Google Scholar]
- Ganihartono, I. Psychiatric morbidity among patients attending the Bangetayu community health centre in Indonesia. Bul. Penelit. Kesehat. 1996, 24, 42–51. [Google Scholar]
- Agudo, A. Measuring Intake of Fruit and Vegetables; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; LeFevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA-J. Am. Med. Assoc. 2014, 311, 507–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Romano, J.; Kromrev, D.; Coraggio, J.; Skowronek, J. Appropriate statistics for ordinal level data: Should we really be using t-test and cohen’s d for evaluating group differences on the NSSE and other surveys? In Proceedings of the Annual Meeting of the Florida Association of Institutional Research, Cocoa Beach, FL, USA, 1–3 February 2006. [Google Scholar]
- Karastergiou, K.; Smith, S.R.; Greenberg, A.S.; Fried, S.K. Sex differences in human adipose tissues—The biology of pear shape. Biol. Sex Differ. 2012, 3, 1. [Google Scholar] [CrossRef] [Green Version]
- Blaak, E. Gender differences in fat metabolism. Curr. Opin. Clin. Nutr. Metab. Care 2001, 4, 499–502. [Google Scholar] [CrossRef] [Green Version]
- Okeke, E.C.; Nnanyelugo, D.O.; Ngwu, E. The prevalence of obesity in adults by age, sex, and occupation in Anambra State, Nigeria. Growth 1983, 47, 263–271. [Google Scholar]
- Wuarlela, M.; Sangadji, H.; Putirulan, A.; Hiariej, C.; Sandanafu, S.P.; Ahar, J.V.; Pesiwarissa, S.I.; Latupeirissa, E.; Wariunsora, M.; Suatrat, R.H.; et al. Membaca Perempuan Maluku: Kalo Su Bisa Tuang Papeda Brarti Su Bisa Kaweng; Kantor Bahasa Maluku Badan Pengembangan Bahasa dan Perbukuan Kementerian Pendidikan dan Kebudayaan: Jakarta, Indonesia, 2019; ISBN 9786022631781. [Google Scholar]
- Bray, G.A.; Popkin, B.M. Dietary fat intake does affect obesity! Am. J. Clin. Nutr. 1998, 68, 1157–1173. [Google Scholar] [CrossRef] [PubMed]
- Beulen, Y.; Martínez-González, M.A.; van de Rest, O.; Salas-Salvadó, J.; Sorlí, J.V.; Gómez-Gracia, E.; Fiol, M.; Estruch, R.; Santos-Lozano, J.M.; Schröder, H.; et al. Quality of dietary fat intake and body weight and obesity in a mediterranean population: Secondary analyses within the PREDIMED trial. Nutrients 2018, 10, 2011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsieh, T.H.; Lee, J.J.; Yu, E.W.R.; Hu, H.Y.; Lin, S.Y.; Ho, C.Y. Association between obesity and education level among the elderly in Taipei, Taiwan between 2013 and 2015: A cross-sectional study. Sci. Rep. 2020, 10, 20285. [Google Scholar] [CrossRef] [PubMed]
- Malik, V.S.; Schulze, M.B.; Hu, F.B. Intake of sugar-sweetened beverages and weight gain: A systematic review. Am. J. Clin. Nutr. 2006, 84, 274–288. [Google Scholar] [CrossRef] [PubMed]
- Arundhana, A.I.; Najamuddin, U.; Ibrahim, W.; Semba, G.; Muqni, A.D.; Haning, M.T. Why consumption pattern of sugar-sweetened beverage is potential to increase the risk of overweight in school age children? Biomedicine 2018, 38, 55–59. [Google Scholar]
- Jürgens, H.; Haass, W.; Castañeda, T.R.; Schürmann, A.; Koebnick, C.; Dombrowski, F.; Otto, B.; Nawrocki, A.R.; Scherer, P.E.; Spranger, J.; et al. Consuming fructose-sweetened beverages increases body adiposity in mice. Obes. Res. 2005, 13, 1145–1156. [Google Scholar] [CrossRef] [Green Version]
- Bush, T.; Lovejoy, J.C.; Deprey, M.; Carpenter, K.M. The effect of tobacco cessation on weight gain, obesity and diabetes risk. Obesity 2016, 24, 1834–1841. [Google Scholar] [CrossRef]
- Hasegawa, K.; Komiyama, M.; Takahashi, Y. Obesity and cardiovascular risk after quitting smoking: The latest evidence. Eur. Cardiol. Rev. 2019, 14, 60–61. [Google Scholar] [CrossRef] [Green Version]
- Locker, D.; Payne, B.; Ford, J. Area variations in health behaviours. Can. J. Public Health 1996, 87, 125–129. [Google Scholar]
- Ecob, R.; Macintyre, S. Small area variations in health related behaviours; do these depend on the behaviour itself, its measurement, or on personal characteristics? Health Place 2000, 6, 261–274. [Google Scholar] [CrossRef]
- Tasevska, N.; DeLia, D.; Lorts, C.; Yedidia, M.; Ohri-Vachaspati, P. Determinants of Sugar-Sweetened Beverage Consumption among Low-Income Children: Are There Differences by Race/Ethnicity, Age, and Sex? J. Acad. Nutr. Diet. 2017, 117, 1900–1920. [Google Scholar] [CrossRef] [PubMed]
- Sederer, L.I. The social determinants of mental health. Psychiatr. Serv. 2016, 67, 234–235. [Google Scholar] [CrossRef] [PubMed]
- Chigbu, C.O.; Parhofer, K.G.; Aniebue, U.U.; Berger, U. Prevalence and sociodemographic determinants of adult obesity: A large representative household survey in a resource-constrained African setting with double burden of undernutrition and overnutrition. J. Epidemiol. Community Health 2018, 72, 702–707. [Google Scholar] [CrossRef] [PubMed]
- Sartorius, B.; Veerman, L.J.; Manyema, M.; Chola, L.; Hofman, K. Determinants of obesity and associated population attributability, South Africa: Empirical evidence from a national panel survey, 2008–2012. PLoS ONE 2015, 10, e0130218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tekalegn, Y.; Engida, Z.T.; Sahiledengle, B.; Rogers, H.L.; Seyoum, K.; Woldeyohannes, D.; Legese, B.; Ayele, T.A. Individual and community-level determinants of overweight and obesity among urban men: Further analysis of the Ethiopian demographic and health survey. PLoS ONE 2021, 16, e0259412. [Google Scholar] [CrossRef] [PubMed]
- Sudikno; Julianti, E.D.; Sari, Y.D.; Sari, Y.P. The Relationship of Physical Activities on Obesity in Adults in Indonesia. In Proceedings of the 4th International Symposium on Health Research (ISHR 2019), Bali, Indonesia, 28–30 November 2019; Atlantis Press: Paris, France, 2020; Volume 22, pp. 96–100. [Google Scholar]
- Dewi, N.U.; Tanziha, I.; Solechah, S.A. Bohari Obesity determinants and the policy implications for the prevention and management of obesity in Indonesia. Curr. Res. Nutr. Food Sci. 2020, 8, 942–955. [Google Scholar] [CrossRef]
- Mulia, E.P.B.; Fauzia, K.A. Atika Abdominal Obesity is Associated with Physical Activity Index in Indonesian Middle-Aged Adult Rural Population: A Cross-Sectional Study. Indian J. Community Med. 2021, 46, 317–320. [Google Scholar] [CrossRef]
- Samouda, H.; Ruiz-Castell, M.; Bocquet, V.; Kuemmerle, A.; Chioti, A.; Dadoun, F.; Kandala, N.B.; Stranges, S. Geographical variation of overweight, obesity and related risk factors: Findings from the European Health examination Survey in Luxembourg, 2013–2015. PLoS ONE 2018, 13, e0197021. [Google Scholar] [CrossRef]
- Ramachandran, A.; Chamukuttan, S.; Shetty, S.A.; Arun, N.; Susairaj, P. Obesity in Asia—Is it different from rest of the world. Diabetes. Metab. Res. Rev. 2012, 28, 47–51. [Google Scholar] [CrossRef]
| Variables | Categories | Island Clusters | ||||||
|---|---|---|---|---|---|---|---|---|
| Sumatra | Java | Bali and Nusa Tenggara | Kalimantan | Sulawesi | Maluku | Papua | ||
| n = 180,292 | n = 204,768 | n = 50,484 | n = 59,654 | n = 85,006 | n = 18,531 | n = 20,175 | ||
| BMI category | Obese | 35.3 | 36.2 | 28.2 | 34.8 | 34.9 | 35.0 | 36.0 |
| Location | Rural | 31.6 | 29.9 | 21.4 | 29.7 | 31.6 | 30.5 | 32.4 |
| Urban | 40.1 | 39.6 | 36.2 | 40.7 | 39.9 | 42.2 | 43.7 | |
| Sex | Men | 26.3 | 26.8 | 22.3 | 26.8 | 26.2 | 26.8 | 31.3 |
| Women | 44.6 | 45.6 | 33.9 | 43.6 | 43.5 | 43.5 | 41.2 | |
| Marital status | Not Married | 18.2 | 20.6 | 16.3 | 19.7 | 19.7 | 18.5 | 22.2 |
| Married | 39.4 | 39.8 | 31.4 | 38.8 | 39.1 | 39.2 | 38.6 | |
| Divorced | 33.9 | 34.2 | 26.0 | 30.0 | 31.0 | 29.9 | 40.5 | |
| Widowed | 34.5 | 32.5 | 22.4 | 27.8 | 30.3 | 35.9 | 32.8 | |
| Age group | ≤47 years | 34.5 | 36.8 | 28.6 | 35.2 | 34.7 | 34.3 | 35.2 |
| 48–63 years | 41.0 | 40.1 | 31.9 | 36.9 | 39.6 | 40.4 | 40.9 | |
| ≥64 years | 25.2 | 22.1 | 16.1 | 23.3 | 23.8 | 26.5 | 24.5 | |
| Education level | Lower education | 46.6 | 46.4 | 40.1 | 45.5 | 43.7 | 47.2 | 53.4 |
| Medium education | 36.5 | 37.9 | 31.5 | 37.5 | 35.8 | 34.4 | 39.5 | |
| Higher education | 33.2 | 34.3 | 24.8 | 32.3 | 33.0 | 33.3 | 32.2 | |
| Occupational status | Unemployed | 41.8 | 42.7 | 30.1 | 41.8 | 40.3 | 36.5 | 40.2 |
| Students | 20.2 | 24.7 | 15.2 | 23.1 | 18.5 | 19.4 | 28.7 | |
| Government/civil workers | 53.9 | 54.7 | 49.3 | 50.6 | 52.4 | 55.4 | 57.2 | |
| Private company officer | 35.0 | 36.3 | 34.8 | 35.9 | 34.0 | 38.8 | 37.3 | |
| Entrepreneur | 40.1 | 42.3 | 42.9 | 38.4 | 41.8 | 46.9 | 40.9 | |
| Farmer | 25.7 | 22.9 | 16.6 | 23.2 | 22.4 | 24.6 | 28.5 | |
| Fisherman | 22.9 | 24.5 | 23.9 | 22.9 | 25.0 | 17.4 | 24.4 | |
| Daily labor/driver/ housekeeper | 27.6 | 27.8 | 24.1 | 26.3 | 29.8 | 29.8 | 30.7 | |
| Others | 39.9 | 39.9 | 28.5 | 39.0 | 39.5 | 42.8 | 42.8 | |
| Mental emotional status | No mental disorder | 35.3 | 36.2 | 28.8 | 35.2 | 35.3 | 35.8 | 35.9 |
| With mental disorder | 35.1 | 36.0 | 23.6 | 30.9 | 31.7 | 29.5 | 36.9 | |
| Sweet food | <3 times/month | 37.0 | 38.2 | 26.3 | 37.6 | 34.0 | 34.2 | 34.3 |
| 1–6 times/week | 35.2 | 35.9 | 28.8 | 35.0 | 34.8 | 35.3 | 36.3 | |
| >1 time/day | 33.7 | 35.3 | 29.2 | 32.6 | 35.6 | 34.7 | 37.4 | |
| Sugar-sweetened beverages | <3 times/month | 42.9 | 44.3 | 30.4 | 42.6 | 39.1 | 40.5 | 40.5 |
| 1–6 times/week | 36.3 | 37.5 | 29.1 | 36.2 | 35.4 | 35.1 | 34.4 | |
| >1 time/day | 30.5 | 31.2 | 23.8 | 30.6 | 31.8 | 32.5 | 37.4 | |
| Food high in salt | <3 times/month | 36.7 | 38.0 | 27.9 | 36.9 | 37.7 | 36.1 | 36.5 |
| 1–6 times/week | 35.0 | 35.4 | 28.5 | 34.1 | 32.9 | 34.0 | 34.6 | |
| >1 time/day | 32.4 | 36.2 | 28.9 | 33.9 | 33.1 | 35.1 | 40.5 | |
| High-fat food | <3 times/month | 34.1 | 34.4 | 23.6 | 32.1 | 31.0 | 34.6 | 32.4 |
| 1–6 times/week | 35.4 | 36.1 | 29.9 | 35.3 | 35.0 | 35.1 | 37.8 | |
| >1 time/day | 36.5 | 36.8 | 32.8 | 35.7 | 38.4 | 35.1 | 38.2 | |
| Meat | <3 times/month | 35.3 | 35.7 | 27.6 | 34.9 | 34.6 | 34.6 | 34.8 |
| 1–6 times/week | 34.8 | 37.6 | 31.4 | 34.6 | 36.0 | 36.5 | 39.1 | |
| >1 time/day | 37.8 | 36.1 | 35.2 | 34.3 | 34.7 | 36.1 | 37.8 | |
| Soft or carbonated drinks | <3 times/month | 35.9 | 36.8 | 28.0 | 35.7 | 35.5 | 35.5 | 36.1 |
| 1–6 times/week | 30.2 | 31.0 | 29.6 | 29.2 | 31.5 | 32.3 | 34.7 | |
| >1 time/day | 28.0 | 32.8 | 20.2 | 27.8 | 35.7 | 38.6 | 48.8 | |
| Energy drinks | <3 times/month | 36.0 | 36.9 | 28.8 | 36.1 | 36.3 | 36.3 | 36.5 |
| 1–6 times/week | 26.9 | 27.2 | 22.5 | 25.3 | 24.9 | 30.2 | 33.4 | |
| >1 time/day | 26.9 | 27.2 | 18.7 | 24.2 | 26.5 | 31.1 | 37.7 | |
| Instant foods | <3 times/month | 38.0 | 37.7 | 29.6 | 36.8 | 37.9 | 38.8 | 36.7 |
| 1–6 times/week | 33.5 | 35.2 | 27.0 | 34.2 | 33.5 | 33.6 | 35.6 | |
| >1 time/day | 31.8 | 36.3 | 25.3 | 26.8 | 29.2 | 28.2 | 35.5 | |
| Vegetable and fruit consumption | Sufficient | 42.5 | 42.7 | 35.3 | 41.7 | 37.8 | 43.2 | 47.4 |
| Insufficient | 35.0 | 35.9 | 27.8 | 34.5 | 34.7 | 34.4 | 35.2 | |
| Smoking | Never smoked | 41.7 | 43.4 | 32.7 | 40.9 | 41.5 | 41.2 | 39.4 |
| Quit smoking | 37.1 | 37.2 | 30.9 | 37.6 | 34.0 | 47.2 | 39.1 | |
| Currently smoking | 24.0 | 23.5 | 19.1 | 22.7 | 22.9 | 23.7 | 28.7 | |
| Physical activity | Adequate | 32.2 | 32.4 | 24.6 | 29.9 | 31.1 | 31.9 | 33.0 |
| Not adequate | 37.8 | 39.0 | 31.0 | 38.4 | 37.6 | 36.8 | 38.9 | |
| Alcohol consumption | Yes | 28.4 | 27.2 | 24.5 | 20.7 | 25.1 | 23.6 | 29.2 |
| No | 35.5 | 36.4 | 28.7 | 35.6 | 35.9 | 36.6 | 36.5 | |
| Blood pressure | Normal | 22.3 | 21.5 | 16.4 | 19.9 | 21.6 | 22.5 | 24.1 |
| Pre-hypertension | 34.6 | 34.2 | 28.7 | 31.4 | 35.2 | 35.4 | 36.3 | |
| Hypertension stage 1 | 46.1 | 45.1 | 38.5 | 43.8 | 44.9 | 45.9 | 49.2 | |
| Hypertension stage 2 | 54.7 | 52.4 | 44.8 | 51.2 | 51.3 | 55.9 | 58.5 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thamrin, S.A.; Arsyad, D.S.; Kuswanto, H.; Lawi, A.; Arundhana, A.I. Obesity Risk-Factor Variation Based on Island Clusters: A Secondary Analysis of Indonesian Basic Health Research 2018. Nutrients 2022, 14, 971. https://doi.org/10.3390/nu14050971
Thamrin SA, Arsyad DS, Kuswanto H, Lawi A, Arundhana AI. Obesity Risk-Factor Variation Based on Island Clusters: A Secondary Analysis of Indonesian Basic Health Research 2018. Nutrients. 2022; 14(5):971. https://doi.org/10.3390/nu14050971
Chicago/Turabian StyleThamrin, Sri Astuti, Dian Sidik Arsyad, Hedi Kuswanto, Armin Lawi, and Andi Imam Arundhana. 2022. "Obesity Risk-Factor Variation Based on Island Clusters: A Secondary Analysis of Indonesian Basic Health Research 2018" Nutrients 14, no. 5: 971. https://doi.org/10.3390/nu14050971
APA StyleThamrin, S. A., Arsyad, D. S., Kuswanto, H., Lawi, A., & Arundhana, A. I. (2022). Obesity Risk-Factor Variation Based on Island Clusters: A Secondary Analysis of Indonesian Basic Health Research 2018. Nutrients, 14(5), 971. https://doi.org/10.3390/nu14050971









