Sleep Duration, Midday Napping, and Serum Homocysteine Levels: A Gene–Environment Interaction Study
Abstract
1. Introduction
2. Methods
2.1. Participant Inclusion
2.2. Ascertainment of Sleep
2.3. Measurement of Serum Homocysteine Levels
2.4. Covariates
2.5. Genotyping and Genetic Risk Score
2.6. Statistical Analyses
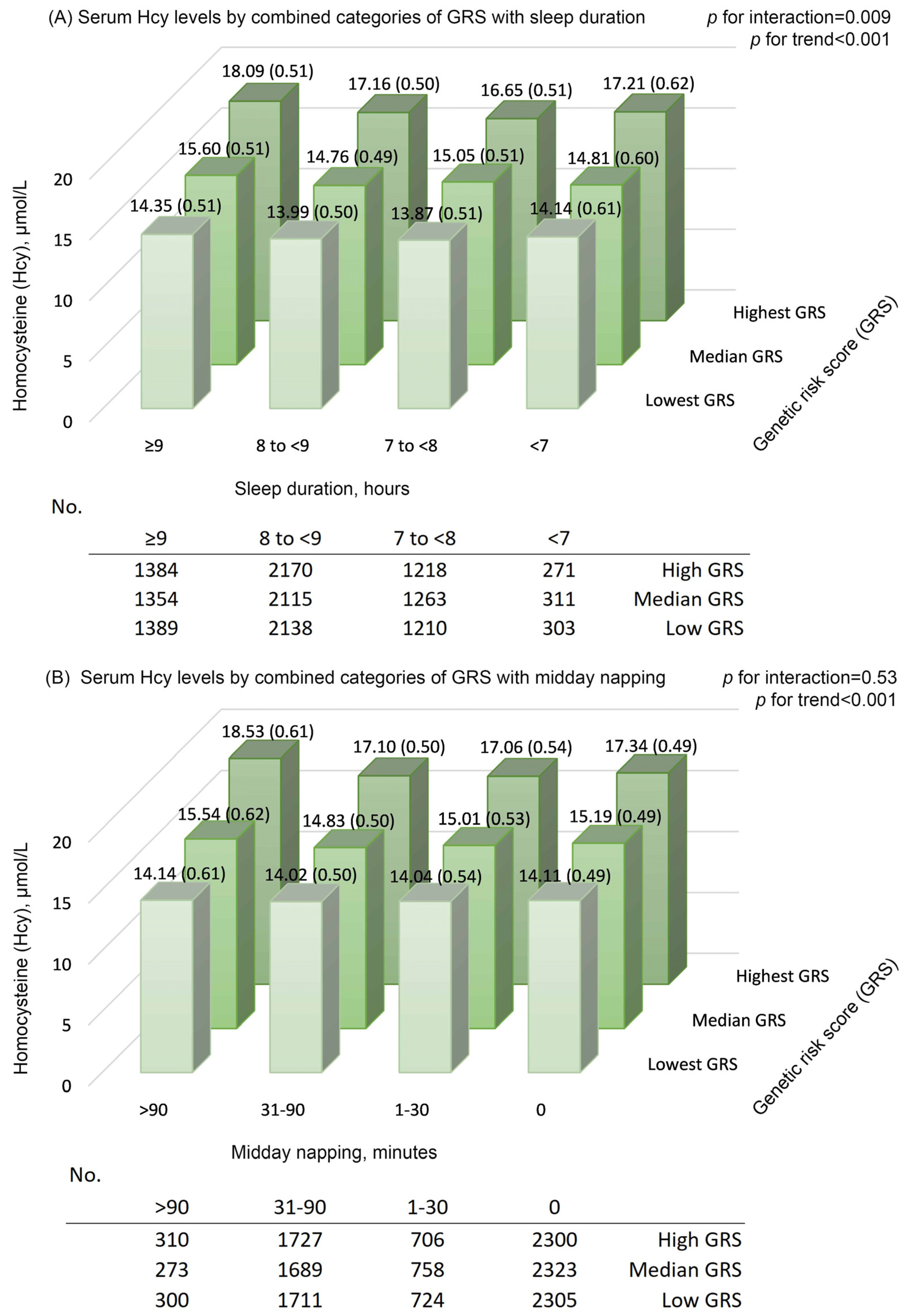
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mason, J.B. Biomarkers of nutrient exposure and status in one-carbon (methyl) metabolism. J. Nutr. 2003, 133 (Suppl. 3), 941s–947s. [Google Scholar] [CrossRef] [PubMed]
- Clare, C.E.; Brassington, A.H.; Kwong, W.Y.; Sinclair, K.D. One-carbon metabolism: Linking nutritional biochemistry to epigenetic programming of long-term development. Annu. Rev. Anim. Biosci. 2019, 7, 263–287. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.M.; Weir, D.G. Folic acid, homocysteine and one-carbon metabolism: A review of the essential biochemistry. J. Cardiovasc. Risk 1998, 5, 223–227. [Google Scholar] [CrossRef]
- Savage, D.G.; Lindenbaum, J.; Stabler, S.P.; Allen, R.H. Sensitivity of serum methylmalonic acid and total homocysteine determinations for diagnosing cobalamin and folate deficiencies. Am. J. Med. 1994, 96, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Abbenhardt, C.; Miller, J.W.; Song, X.; Brown, E.C.; Cheng, T.-Y.D.; Wener, M.H.; Zheng, Y.; Toriola, A.T.; Neuhouser, M.L.; Beresford, S.A.A.; et al. Biomarkers of one-carbon metabolism are associated with biomarkers of inflammation in women. J. Nutr. 2014, 144, 714–721. [Google Scholar] [CrossRef]
- Smith, A.D.; Refsum, H. Homocysteine—From disease biomarker to disease prevention. J. Intern. Med. 2021, 290, 826–854. [Google Scholar] [CrossRef] [PubMed]
- Ducker, G.S.; Rabinowitz, J.D. One-carbon metabolism in health and disease. Cell Metab. 2017, 25, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and stroke statistics-2020 update: A report from the american heart association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- Beydoun, M.A.; Gamaldo, A.A.; Canas, J.A.; Beydoun, H.A.; Shah, M.T.; McNeely, J.M.; Zonderman, A.B. Serum nutritional biomarkers and their associations with sleep among US adults in recent national surveys. PLoS ONE 2014, 9, e103490. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.Y.; Winkelman, J.W.; Mao, W.C.; Yeh, C.B.; Huang, S.Y.; Kao, T.W.; Yang, C.C.H.; Kuo, T.B.J.; Chen, W.L. Short sleep duration is associated with increased serum homocysteine: Insights from a national survey. J. Clin. Sleep Med. 2019, 15, 139–148. [Google Scholar] [CrossRef]
- Burazeri, G.; Gofin, J.; Kark, J.D. Siesta and mortality in a Mediterranean population: A community study in Jerusalem. Sleep 2003, 26, 578–584. [Google Scholar] [CrossRef] [PubMed]
- Naska, A.; Oikonomou, E.; Trichopoulou, A.; Psaltopoulou, T.; Trichopoulos, D. Siesta in healthy adults and coronary mortality in the general population. Arch. Intern. Med. 2007, 167, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Bouscoulet, L.T.; Vázquez-García, J.C.; Muiño, A.; Márquez, M.; López, M.V.; de Oca, M.M.; Talamo, C.; Valdivia, G.; Pertuze, J.; Menezes, A.M.; et al. Prevalence of sleep related symptoms in four Latin American cities. J. Clin. Sleep Med. 2008, 4, 579–585. [Google Scholar] [CrossRef]
- Zhang, Z.; Xiao, X.; Ma, W.; Li, J. Napping in Older Adults: A Review of Current Literature. Curr. Sleep Med. Rep. 2020, 6, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Qi, Q.; Chu, A.Y.; Kang, J.H.; Huang, J.; Rose, L.M.; Jensen, M.K.; Liang, L.; Curhan, G.C.; Pasquale, L.R.; Wiggs, J.L.; et al. Fried food consumption, genetic risk, and body mass index: Gene-diet interaction analysis in three US cohort studies. BMJ 2014, 348, g1610. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Li, X.; Zhou, T.; Sun, D.; Liang, Z.; Li, Y.; Heianza, Y.; Qi, L. Glucosamine use, inflammation, and genetic susceptibility, and incidence of type 2 diabetes: A prospective study in UK Biobank. Diabetes Care 2020, 43, 719–725. [Google Scholar] [CrossRef]
- Van Meurs, J.B.; Pare, G.; Schwartz, S.M.; Hazra, A.; Tanaka, T.; Vermeulen, S.H.; Cotlarciuc, I.; Yuan, X.; Malarstig, A.; Bandinelli, S.; et al. Common genetic loci influencing plasma homocysteine concentrations and their effect on risk of coronary artery disease. Am. J. Clin. Nutr. 2013, 98, 668–676. [Google Scholar] [CrossRef]
- Wang, F.; Zhu, J.; Yao, P.; Li, X.; He, M.; Liu, Y.; Yuan, J.; Chen, W.; Zhou, L.; Min, X.; et al. Cohort profile: The Dongfeng-Tongji cohort study of retired workers. Int. J. Epidemiol. 2013, 42, 731–740. [Google Scholar] [CrossRef]
- Yang, L.; Yang, H.; He, M.; Pan, A.; Li, X.; Min, X.; Zhang, C.; Xu, C.; Zhu, X.; Yuan, J.; et al. Longer sleep duration and midday napping are associated with a higher risk of CHD incidence in middle-aged and older chinese: The Dongfeng-Tongji cohort study. Sleep 2016, 39, 645–652. [Google Scholar] [CrossRef]
- Zhou, L.; Yu, K.; Yang, L.; Wang, H.; Xiao, Y.; Qiu, G.; Liu, X.; Yuan, Y.; Bai, Y.; Li, X.; et al. Sleep duration, midday napping, and sleep quality and incident stroke: The Dongfeng-Tongji cohort. Neurology 2020, 94, e345–e356. [Google Scholar] [CrossRef]
- Long, P.; Liu, X.; Li, J.; He, S.; Chen, H.; Yuan, Y.; Qiu, G.; Yu, K.; Liu, K.; Jiang, J.; et al. Circulating folate concentrations and risk of coronary artery disease: A prospective cohort study in Chinese adults and a Mendelian randomization analysis. Am. J. Clin. Nutr. 2020, 111, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Hara, K.; Shojima, N.; Yamauchi, T.; Kadowaki, T. Daytime napping and the risk of cardiovascular disease and all-cause mortality: A prospective study and dose-response meta-analysis. Sleep 2015, 38, 1945–1953. [Google Scholar] [CrossRef]
- Kwok, C.S.; Kontopantelis, E.; Kuligowski, G.; Gray, M.; Muhyaldeen, A.; Gale, C.P.; Peat, G.M.; Cleator, J.; Chew-Graham, C.; Loke, Y.K.; et al. Self-reported sleep duration and quality and cardiovascular disease and mortality: A dose-response meta-analysis. J. Am. Heart Assoc. 2018, 7, e008552. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.C.; Chow, C.C.; Tellier, L.C.; Vattikuti, S.; Purcell, S.M.; Lee, J.J. Second-generation PLINK: Rising to the challenge of larger and richer datasets. Gigascience 2015, 4, 7. [Google Scholar] [CrossRef] [PubMed]
- Matsubayashi, H.; Nagai, M.; Dote, K.; Turana, Y.; Siddique, S.; Chia, Y.C.; Chen, C.H.; Cheng, H.M.; Van Minh, H.; Verma, N.; et al. Long sleep duration and cardiovascular disease: Associations with arterial stiffness and blood pressure variability. J. Clin. Hypertens. Greenwich Conn. 2021, 23, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Mo, X.; Wu, Z.; Guan, X. Systematic review and meta-analysis of the correlation between plasma homocysteine levels and coronary heart disease. J. Thorac. Dis. 2022, 14, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Bangdiwala, S.I.; Rangarajan, S.; Lear, S.A.; Al Habib, K.F.; Mohan, V.; Teo, K.; Poirier, P.; Tse, L.A.; Liu, Z.; et al. Association of estimated sleep duration and naps with mortality and cardiovascular events: A study of 116 632 people from 21 countries. Eur. Heart J. 2019, 40, 1620–1629. [Google Scholar] [CrossRef]
- Paganelli, F.; Mottola, G.; Fromonot, J.; Marlinge, M.; Deharo, P.; Guieu, R.; Ruf, J. Hyperhomocysteinemia and Cardiovascular Disease: Is the Adenosinergic System the Missing Link? Int. J. Mol. Sci. 2021, 22, 1690. [Google Scholar] [CrossRef]
- Ganguly, P.; Alam, S.F. Role of homocysteine in the development of cardiovascular disease. Nutr. J. 2015, 14, 6. [Google Scholar] [CrossRef]
- Hoevenaar-Blom, M.P.; Spijkerman, A.M.W.; Kromhout, D.; van den Berg, J.F.; Verschuren, W.M.M. Sleep duration and sleep quality in relation to 12-year cardiovascular disease incidence: The MORGEN study. Sleep 2011, 34, 1487–1492. [Google Scholar] [CrossRef]
- Magee, C.A.; Kritharides, L.; Attia, J.; McElduff, P.; Banks, E. Short and long sleep duration are associated with prevalent cardiovascular disease in Australian adults. J. Sleep Res. 2012, 21, 441–447. [Google Scholar] [CrossRef]
- Fan, M.; Sun, D.; Zhou, T.; Heianza, Y.; Lv, J.; Li, L.; Qi, L. Sleep patterns, genetic susceptibility, and incident cardiovascular disease: A prospective study of 385 292 UK biobank participants. Eur. Heart J. 2020, 41, 1182–1189. [Google Scholar] [CrossRef]
- Xin, C.; Zhang, B.; Fang, S.; Zhou, J. Daytime napping and successful aging among older adults in China: A cross-sectional study. BMC Geriatr. 2020, 20, 2. [Google Scholar] [CrossRef] [PubMed]
- Picarsic, J.L.; Glynn, N.W.; Taylor, C.A.; Katula, J.A.; Goldman, S.E.; Studenski, S.A.; Newman, A.B. Self-reported napping and duration and quality of sleep in the lifestyle interventions and independence for elders pilot study. J. Am. Geriatr. Soc. 2008, 56, 1674–1680. [Google Scholar] [CrossRef]
- Häusler, N.; Marques-Vidal, P.; Haba-Rubio, J.; Heinzer, R. Does sleep predict next-day napping or does napping influence same-day nocturnal sleep? Results of a population-based ecological momentary assessment study. Sleep Med. 2019, 61, 31–36. [Google Scholar] [CrossRef]
- Fu, Y.; Wang, X.; Kong, W. Hyperhomocysteinaemia and vascular injury: Advances in mechanisms and drug targets. Br. J. Pharmacol. 2018, 175, 1173–1189. [Google Scholar] [CrossRef]
- Ji, X.; Grandner, M.A.; Liu, J. The relationship between micronutrient status and sleep patterns: A systematic review. Public Health Nutr. 2017, 20, 687–701. [Google Scholar] [CrossRef]
- Jansen, E.C.; Dolinoy, D.C.; O’Brien, L.M.; Peterson, K.E.; Chervin, R.D.; Banker, M.; Téllez-Rojo, M.M.; Cantoral, A.; Mercado-Garcia, A.; Sanchez, B.; et al. Sleep duration and fragmentation in relation to leukocyte DNA methylation in adolescents. Sleep 2019, 42, zsz121. [Google Scholar] [CrossRef] [PubMed]
- Smail, E.; Maher, B.; Moore, A.; Kuo, P.L.; Wu, M.; Low, D.; Stone, K.; Spira, A. Links ofsleep duration with biomarkers of accelerated aging: The Baltimore longitudinal study of aging. Innov. Aging 2021, 5, 665–666. [Google Scholar] [CrossRef]
- Wu, G.; Fang, Y.-Z.; Yang, S.; Lupton, J.R.; Turner, N.D. Glutathione metabolism and its implications for health. J. Nutr. 2004, 134, 489–492. [Google Scholar] [CrossRef] [PubMed]
- Kropp, H.; Sundelof, J.G.; Hajdu, R.; Kahan, F.M. Metabolism of thienamycin and related carbapenem antibiotics by the renal dipeptidase, dehydropeptidase. Antimicrob. Agents Chemother. 1982, 22, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, H.; Inazawa, J.; Inoue, K.; Misawa, S.; Kashima, K.; Adachi, H.; Nakazato, H.; Abe, T. Assignment of the human renal dipeptidase gene (DPEP1) to band q24 of chromosome 16. Cytogenet. Cell. Genet. 1992, 59, 258–260. [Google Scholar] [CrossRef]
- Mayatepek, E.; Badiou, S.; Bellet, H.; Lehmann, W.D. A patient with neurological symptoms and abnormal leukotriene metabolism: A new defect in leukotriene biosynthesis. Ann. Neurol. 2005, 58, 968–970. [Google Scholar] [CrossRef] [PubMed]
- Verhoef, P.; Steenge, G.R.; Boelsma, E.; van Vliet, T.; Olthof, M.R.; Katan, M.B. Dietary serine and cystine attenuate the homocysteine-raising effect of dietary methionine: A randomized crossover trial in humans. Am. J. Clin. Nutr. 2004, 80, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, J.D.; Martin, J.J.; Harris, B.J. Methionine metabolism in mammals. The methionine-sparing effect of cystine. J. Biol. Chem. 1988, 263, 11750–11754. [Google Scholar] [CrossRef]
- Grandner, M.A.; Kripke, D.F.; Naidoo, N.; Langer, R.D. Relationships among dietary nutrients and subjective sleep, objective sleep, and napping in women. Sleep Med. 2010, 11, 180–184. [Google Scholar] [CrossRef]
- Chen, J.C.; Espeland, M.A.; Brunner, R.L.; Lovato, L.C.; Wallace, R.B.; Leng, X.; Phillips, L.S.; Robinson, J.G.; Kotchen, J.M.; Johnson, K.C.; et al. Sleep duration, cognitive decline, and dementia risk in older women. Alzheimers Dement. J. Alzheimers Assoc. 2016, 12, 21–33. [Google Scholar] [CrossRef]
- Xie, J.; Zhu, M.; Ji, M.; Fan, J.; Huang, Y.; Wei, X.; Jiang, X.; Xu, J.; Yin, R.; Wang, Y.; et al. Relationships between sleep traits and lung cancer risk: A prospective cohort study in UK Biobank. Sleep 2021, 44, zsab089. [Google Scholar] [CrossRef]
- Williams, C. Work-life balance of shift workers. Perspect. Labour Income 2008, 9, 5–16. [Google Scholar]
- Li, W.; Yu, K.; Jia, N.; Xu, X.; Yuan, Y.; Peng, R.; Niu, R.; You, X.; Yang, H.; Qiu, G.; et al. Past Shift Work and Incident Coronary Heart Disease in Retired Workers: A Prospective Cohort Study. Am. J. Epidemiol. 2021, 190, 1821–1829. [Google Scholar] [CrossRef]

| Sleep Duration, Hours | Midday Napping, Minutes | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| <7 | 7 to <8 | 8 to <9 | ≥9 | 0 | 1–30 | 31–60 | 61–90 | >90 | |
| Sample size, n | 1132 | 4695 | 8269 | 5330 | 8933 | 2797 | 4919 | 1631 | 1146 |
| Age, years | 63.0 (8.1) | 62.4 (7.7) | 62.9 (8.1) | 63.5 (8.8) | 61.9 (8.0) | 62.8 (8.1) | 64.1 (8.3) | 64.5 (8.4) | 64.2 (8.5) |
| Female, (%) | 57.9 | 59.1 | 59.1 | 55.5 | 64.1 | 62.3 | 51.5 | 43.9 | 48.3 |
| Male, (%) | 42.1 | 40.9 | 40.9 | 44.5 | 35.9 | 37.7 | 48.5 | 56.1 | 51.7 |
| Education level, (%) | |||||||||
| Primary school or below | 17.1 | 16.2 | 19.8 | 26.3 | 21.5 | 18.9 | 19.3 | 18.1 | 27.0 |
| Middle school | 36.2 | 36.2 | 37.8 | 38.2 | 38.7 | 34.1 | 37.2 | 36.8 | 37.6 |
| High school or beyond | 46.0 | 47.0 | 41.9 | 35.0 | 39.2 | 46.3 | 43.0 | 44.8 | 35.3 |
| BMI, kg/m2 | 24.3 (3.2) | 24.1 (3.0) | 23.9 (3.07) | 23.8 (3.2) | 23.9 (3.1) | 23.9 (3.1) | 24.1 (3.1) | 24.0 (3.1) | 24.2 (3.1) |
| eGFR, mL/min/1.73 m2 | 83.8 (16.1) | 84.0 (15.4) | 83.0 (16.2) | 81.7 (17.2) | 83.3 (16.3) | 83.4 (16.4) | 83.0 (15.9) | 81.5 (16.9) | 82.4 (17.0) |
| Hypertension, (%) | 56.8 | 58.1 | 58.3 | 59.7 | 54.8 | 58.4 | 62.5 | 62.7 | 65.5 |
| Dyslipidemia, (%) | 41.3 | 39.7 | 38.7 | 38.9 | 37.0 | 39.5 | 40.3 | 42.0 | 45.8 |
| Diabetes, (%) | 20.1 | 18.4 | 19.3 | 20.4 | 17.2 | 20.0 | 21.2 | 22.3 | 23.5 |
| Smoking status, (%) | |||||||||
| Current smoker | 19.7 | 16.0 | 15.5 | 17.8 | 15.6 | 13.4 | 17.2 | 20.3 | 22.8 |
| Former smoker | 10.9 | 10.0 | 9.5 | 11.0 | 7.7 | 9.0 | 12.3 | 15.2 | 14.7 |
| Never smoker | 69.4 | 74.1 | 75.0 | 71.2 | 76.7 | 77.5 | 70.5 | 64.5 | 62.6 |
| Drinking status, (%) | |||||||||
| Current drinker | 28.7 | 26.6 | 24.9 | 26.1 | 23.6 | 23.4 | 27.8 | 30.4 | 34.8 |
| Former drinker | 4.8 | 4.6 | 4.4 | 5.2 | 3.6 | 4.7 | 4.8 | 8.9 | 6.4 |
| Never drinker | 66.5 | 68.8 | 70.7 | 68.7 | 72.8 | 71.9 | 67.4 | 60.7 | 58.8 |
| Dietary intake a, (%) | |||||||||
| Meat | 53.7 | 53.2 | 53.9 | 49.8 | 54.9 | 52.2 | 53.0 | 51.2 | 52.1 |
| Milk or dairy products | 43.4 | 44.2 | 43.6 | 39.5 | 45.3 | 40.8 | 44.4 | 42.6 | 39.8 |
| Beans or soy products | 56.5 | 56.4 | 56.5 | 52.2 | 58.3 | 53.4 | 57.3 | 54.8 | 55.1 |
| Fish or seafood | 22.1 | 20.8 | 22.9 | 20.9 | 23.4 | 22.3 | 22.0 | 19.4 | 20.6 |
| Fruits or vegetables | 96.9 | 96.9 | 96.5 | 96.7 | 96.9 | 96.8 | 96.7 | 96.0 | 95.3 |
| Regular exercise b, (%) | 71.0 | 67.8 | 69.6 | 63.3 | 71.8 | 65.3 | 70.6 | 70.8 | 66.1 |
| Snoring, (%) | 44.3 | 43.1 | 39.6 | 38.9 | 34.4 | 44.1 | 45.4 | 48.3 | 48.2 |
| Sleep quality, (%) | |||||||||
| Good | 30.5 | 35.2 | 37.0 | 38.2 | 37.5 | 34.1 | 35.7 | 35.1 | 40.1 |
| Fair | 44.3 | 50.0 | 50.9 | 48.8 | 46.9 | 51.1 | 52.7 | 55.0 | 47.9 |
| Poor | 25.3 | 14.8 | 12.1 | 13.0 | 15.6 | 14.8 | 11.7 | 9.9 | 12.0 |
| Job category, (%) | |||||||||
| Manufacturing or manual labor | 44.8 | 44.8 | 45.6 | 47.0 | 43.7 | 47.9 | 43.5 | 43.5 | 46.7 |
| Service or sales work | 28.9 | 27.7 | 29.0 | 28.3 | 30.6 | 27.6 | 29.9 | 28.3 | 28.1 |
| Office work | 14.0 | 15.5 | 12.3 | 10.3 | 13.6 | 11.4 | 12.9 | 15.4 | 10.7 |
| Past shift work, years | |||||||||
| None | 45.4 | 42.2 | 43.8 | 42.2 | 44.2 | 43.5 | 44.3 | 43.9 | 40.6 |
| ≤5.00 | 13.9 | 15.7 | 13.6 | 14.4 | 14.9 | 13.7 | 14.1 | 13.9 | 13.4 |
| 5.25–10.00 | 10.2 | 9.8 | 10.9 | 11.5 | 10.3 | 11.3 | 10.1 | 10.5 | 11.6 |
| 10.50–20.00 | 11.7 | 12.3 | 11.1 | 10.9 | 11.3 | 11.5 | 11.2 | 9.6 | 11.9 |
| >20.00 | 7.7 | 8.9 | 8.1 | 7.5 | 7.9 | 7.7 | 7.4 | 9.7 | 8.6 |
| Total Participants | Participants with Genetic Data | p | |
|---|---|---|---|
| Sample size, n | 19,426 | 15126 | |
| Age, years | 62.9 (8.2) | 63.2 (8.0) | 0.006 |
| Female, (%) | 11,272 (58.0) | 8602 (56.9) | 0.03 |
| Male, (%) | 8154 (42.0) | 6524 (43.1) | 0.03 |
| Education level, (%) | 0.72 | ||
| Primary school or below | 3998 (20.6) | 3143 (20.8) | |
| Middle school | 7272 (37.4) | 5724 (37.8) | |
| High school or beyond | 8052 (41.4) | 6177 (40.8) | |
| BMI, kg/m2 | 24.0 (3.1) | 24.0 (3.1) | 0.96 |
| eGFR, mL/min/1.73 m2 | 82.9 (16.3) | 82.8 (16.1) | 0.33 |
| Hypertension, (%) | 11,375 (58.6) | 9018 (59.6) | 0.05 |
| Dyslipidemia, (%) | 7601 (39.1) | 5890 (38.9) | 0.73 |
| Diabetes, (%) | 3775 (19.4) | 2939 (19.4) | 0.99 |
| Smoking status, (%) | 0.38 | ||
| Current smoker | 3207 (16.5) | 2521 (16.7) | |
| Former smoker | 1963 (10.1) | 1591 (10.5) | |
| Never smoker | 14,256 (73.4) | 11,014 (72.8) | |
| Alcohol intake status, (%) | 0.52 | ||
| Current drinker | 5030 (25.9) | 3915 (25.9) | |
| Former drinker | 906 (4.7) | 745 (4.9) | |
| Never drinker | 13,490 (69.4) | 10,466 (69.2) | |
| Dietary intake a, (%) | |||
| Meat | 10,231 (52.7) | 7930 (52.4) | 0.84 |
| Milk or dairy products | 8245 (42.4) | 6347 (42.0) | 0.66 |
| Beans or soy products | 10,746 (55.3) | 8367 (55.3) | 0.97 |
| Fish or seafood | 4282 (22.0) | 3322 (22.0) | 0.95 |
| Fruits or vegetables | 18,776 (96.7) | 14,618 (96.6) | 0.99 |
| Regular exercise b, (%) | 13,232 (68.1) | 10,375 (68.6) | 0.63 |
| Snoring, (%) | 7877 (40.5) | 6220 (41.1) | 0.56 |
| Sleep quality, (%) | 0.74 | ||
| Good | 7097 (36.5) | 5587 (36.9) | |
| Fair | 9651 (49.7) | 7473 (49.4) | |
| Poor | 2678 (13.8) | 2066 (13.7) | |
| Job category, (%) | 0.36 | ||
| Manufacturing or manual labor | 45.8 | 45.9 | |
| Service or sales work | 28.7 | 29.1 | |
| Office work | 12.4 | 12.4 | |
| Past shift work, years | 0.59 | ||
| None | 43.7 | 44.2 | |
| ≤5.00 | 14.0 | 13.8 | |
| 5.25–10.00 | 10.8 | 11.0 | |
| 10.50–20.00 | 11.3 | 11.3 | |
| >20.00 | 7.9 | 7.9 |
| Homocysteine a, β (95% Confidence Interval) | |||
|---|---|---|---|
| Model 1 b | Model 2 c | Model 3 d | |
| Sleep duration, hours | |||
| <7 | 0.004 (−0.024, 0.032) | 0.005 (−0.021, 0.031) | 0.005 (−0.021, 0.031) |
| 7 to <8 | 0.000 (ref) | 0.000 (ref) | 0.000 (ref) |
| 8 to <9 | 0.024 (0.009, 0.040) | 0.013 (−0.001, 0.027) | 0.013 (−0.001, 0.027) |
| ≥9 | 0.079 (0.062, 0.096) | 0.046 (0.030, 0.062) | 0.045 (0.029, 0.061) |
| Midday napping, minutes | |||
| 0 | 0.040 (0.021, 0.058) | 0.015 (−0.002, 0.032) | 0.013 (−0.004, 0.03) |
| 1–30 | 0.000 (ref) | 0.000 (ref) | 0.000 (ref) |
| 31–60 | 0.010 (−0.010, 0.030) | 0.005 (−0.014, 0.024) | 0.003 (−0.015, 0.022) |
| 61–90 | 0.006 (−0.020, 0.033) | −0.007 (−0.032, 0.017) | −0.008 (−0.033, 0.016) |
| >90 | 0.056 (0.027, 0.086) | 0.033 (0.005, 0.060) | 0.029 (0.001, 0.057) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mo, T.; Wang, Y.; Gao, H.; Li, W.; Zhou, L.; Yuan, Y.; Zhang, X.; He, M.; Guo, H.; Long, P.; et al. Sleep Duration, Midday Napping, and Serum Homocysteine Levels: A Gene–Environment Interaction Study. Nutrients 2023, 15, 210. https://doi.org/10.3390/nu15010210
Mo T, Wang Y, Gao H, Li W, Zhou L, Yuan Y, Zhang X, He M, Guo H, Long P, et al. Sleep Duration, Midday Napping, and Serum Homocysteine Levels: A Gene–Environment Interaction Study. Nutrients. 2023; 15(1):210. https://doi.org/10.3390/nu15010210
Chicago/Turabian StyleMo, Tingting, Yufei Wang, Hui Gao, Wending Li, Lue Zhou, Yu Yuan, Xiaomin Zhang, Meian He, Huan Guo, Pinpin Long, and et al. 2023. "Sleep Duration, Midday Napping, and Serum Homocysteine Levels: A Gene–Environment Interaction Study" Nutrients 15, no. 1: 210. https://doi.org/10.3390/nu15010210
APA StyleMo, T., Wang, Y., Gao, H., Li, W., Zhou, L., Yuan, Y., Zhang, X., He, M., Guo, H., Long, P., & Wu, T. (2023). Sleep Duration, Midday Napping, and Serum Homocysteine Levels: A Gene–Environment Interaction Study. Nutrients, 15(1), 210. https://doi.org/10.3390/nu15010210





