Protective Role of Chronic Exercise Training in Modulating the Impact of Hyperglycemia on Vascular Sensitivity to Ischemia-Reperfusion
Abstract
:1. Introduction
2. Methods
2.1. Population and Experimental Design
2.2. Femoral Artery Ischemia Reperfusion Protocol
2.3. Vascular Reactivity
2.4. ROS and NO Quantification
2.5. Statistics
3. Results
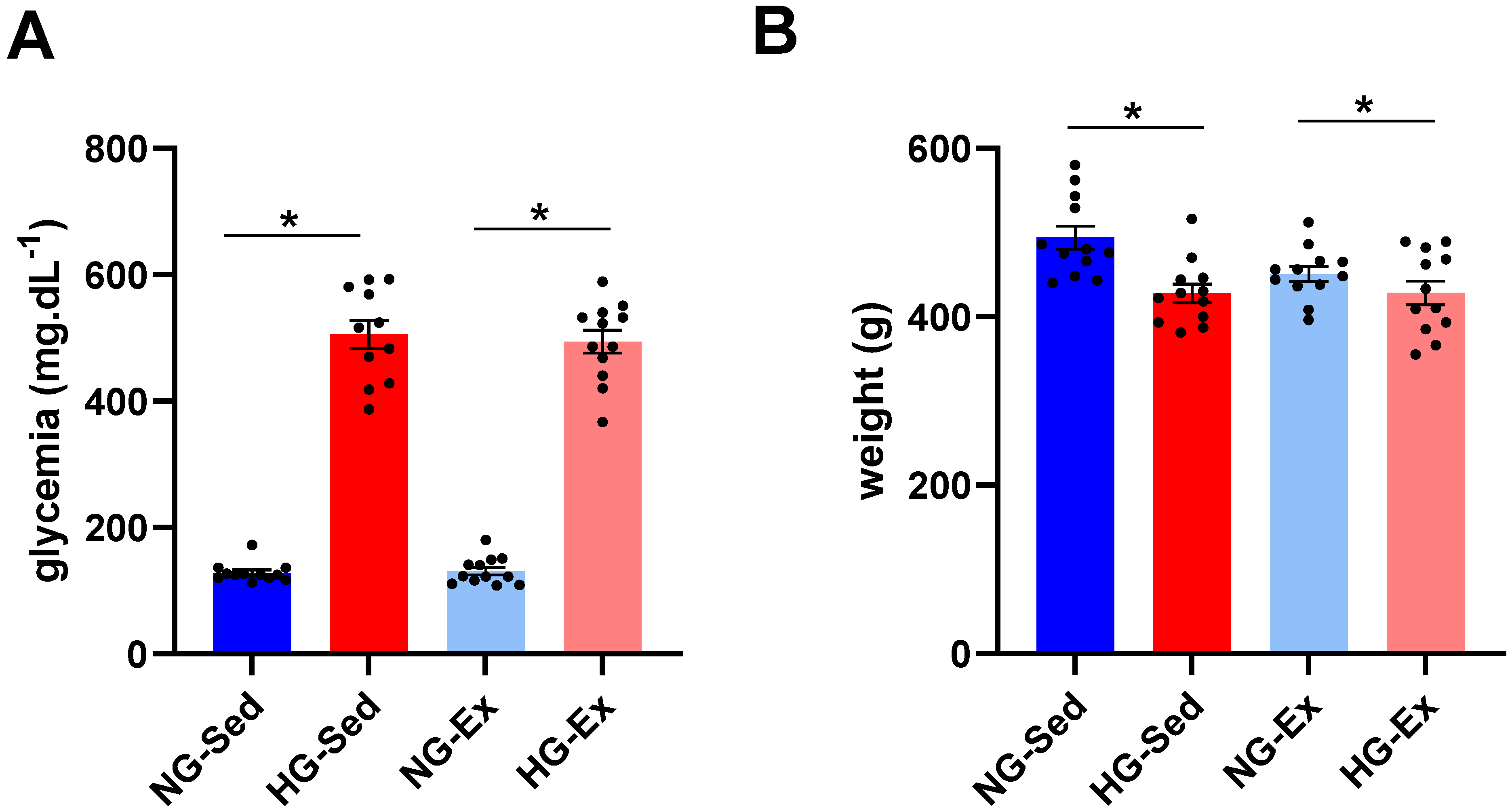
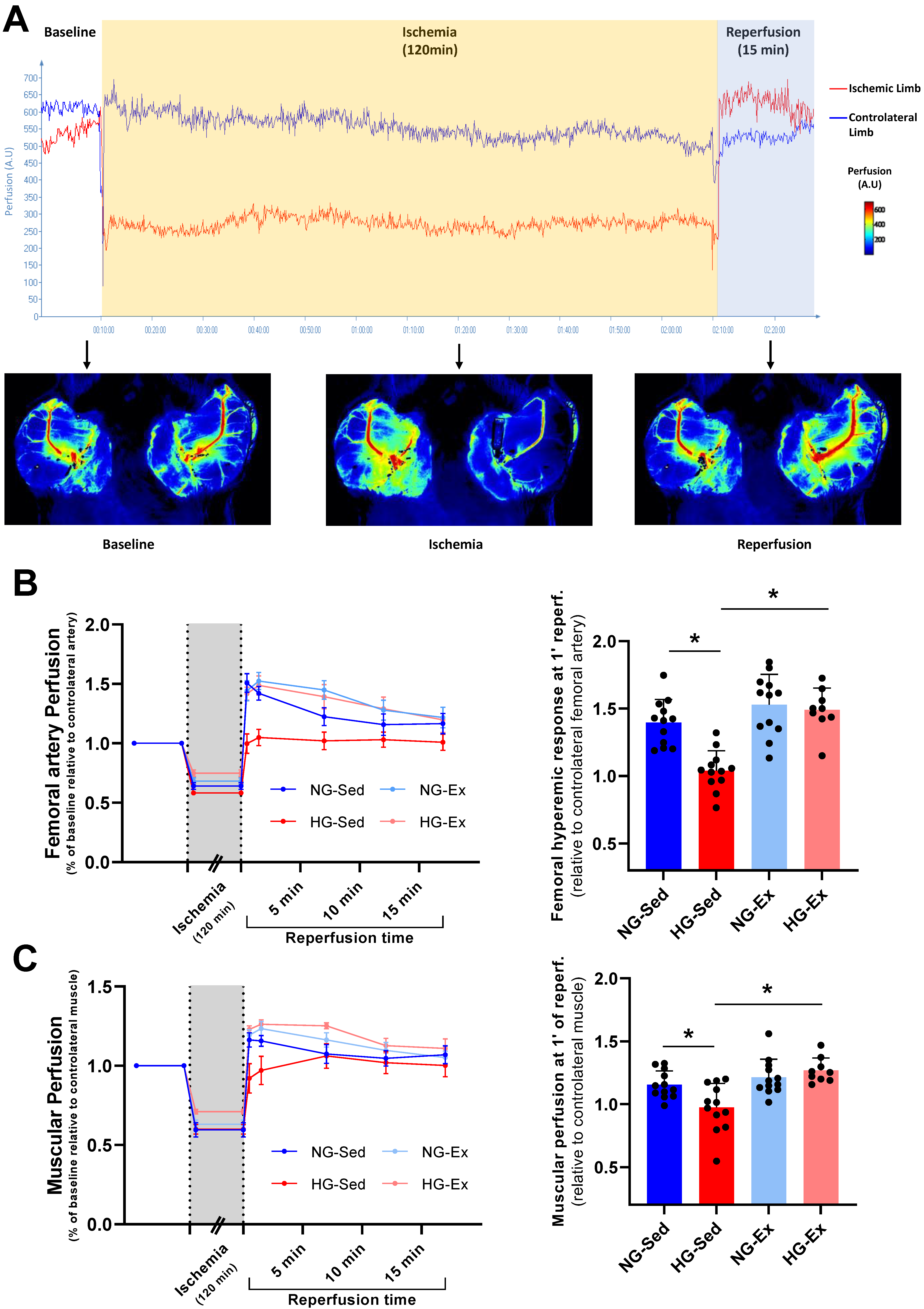
3.1. Impact of Hyperglycemia and Exercise Training on Vascular Function
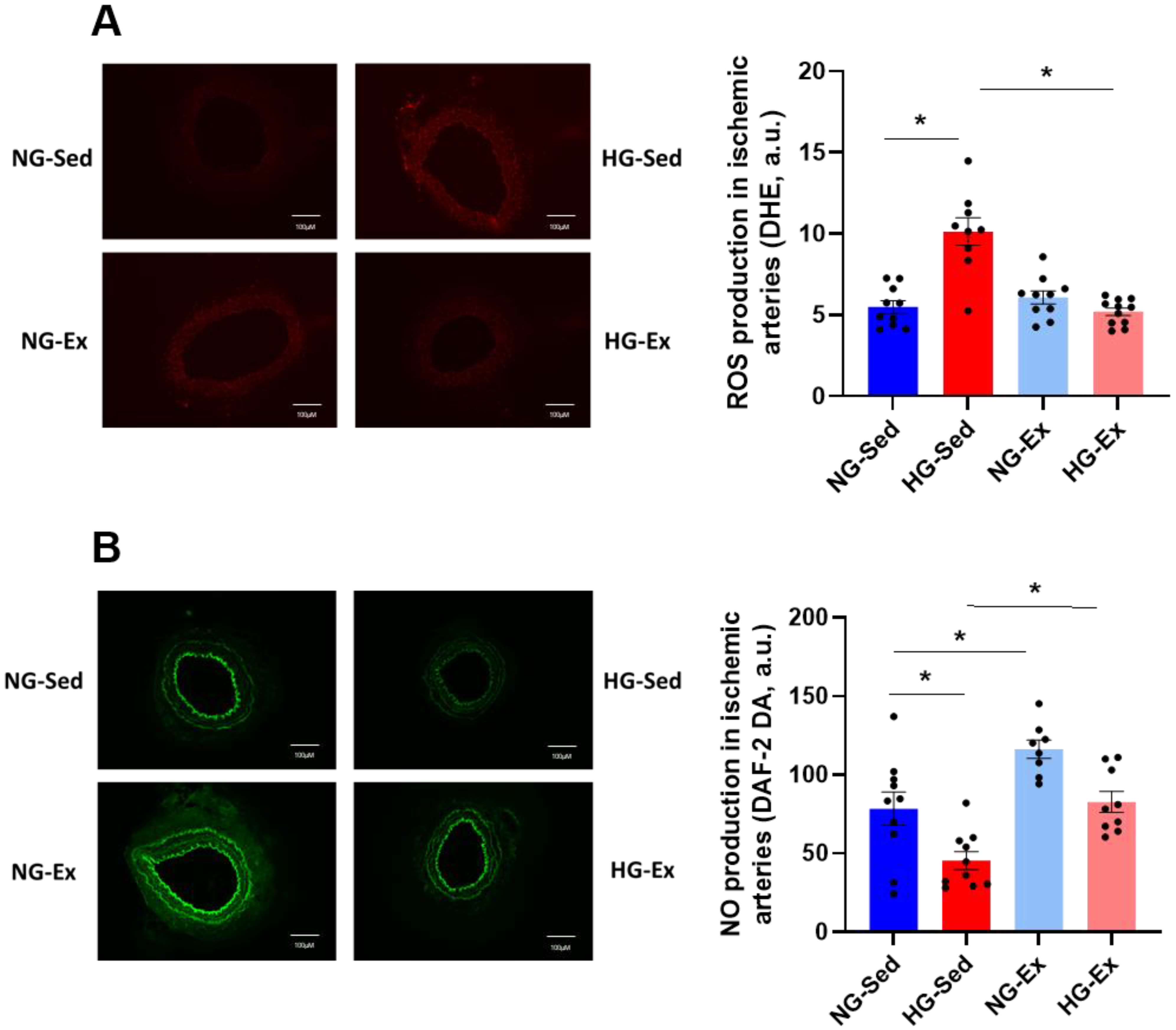
3.2. Impact of Hyperglycemia and Exercise Training on Arterial ROS Production and NO Availability
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Tsivgoulis, G.; Katsanos, A.H.; Mavridis, D.; Lambadiari, V.; Roffe, C.; Macleod, M.J.; Sevcik, P.; Cappellari, M.; Nevšímalová, M.; Toni, D.; et al. Association of Baseline Hyperglycemia with Outcomes of Patients with and without Diabetes with Acute Ischemic Stroke Treated with Intravenous Thrombolysis: A Propensity Score-Matched Analysis from the SITS-ISTR Registry. Diabetes 2019, 68, 1861–1869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ceriello, A. Acute Hyperglycaemia: A ‘New’ Risk Factor during Myocardial Infarction. Eur. Heart J. 2005, 26, 328–331. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, M.; Inoue, I.; Kawagoe, T.; Shimatani, Y.; Kurisu, S.; Nishioka, K.; Umemura, T.; Nakamura, S.; Yoshida, M. Impact of Acute Hyperglycemia on Left Ventricular Function after Reperfusion Therapy in Patients with a First Anterior Wall Acute Myocardial Infarction. Am. Heart J. 2003, 146, 674–678. [Google Scholar] [CrossRef] [PubMed]
- Kosiborod, M.; Rathore, S.S.; Inzucchi, S.E.; Masoudi, F.A.; Wang, Y.; Havranek, E.P.; Krumholz, H.M. Admission Glucose and Mortality in Elderly Patients Hospitalized With Acute Myocardial Infarction: Implications for Patients With and Without Recognized Diabetes. Circulation 2005, 111, 3078–3086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bruno, A.; Biller, J.; Adams, H.P.; Clarke, W.R.; Woolson, R.F.; Williams, L.S.; Hansen, M.D. Acute Blood Glucose Level and Outcome from Ischemic Stroke. Neurology 1999, 52, 280. [Google Scholar] [CrossRef] [PubMed]
- Weir, C.J.; Murray, G.D.; Dyker, A.G.; Lees, K.R. Is Hyperglycaemia an Independent Predictor of Poor Outcome after Acute Stroke? Results of a Long Term Follow up Study. BMJ 1997, 314, 1303. [Google Scholar] [CrossRef] [Green Version]
- Loader, J.; Montero, D.; Lorenzen, C.; Watts, R.; Méziat, C.; Reboul, C.; Stewart, S.; Walther, G. Acute Hyperglycemia Impairs Vascular Function in Healthy and Cardiometabolic Diseased Subjects: Systematic Review and Meta-Analysis. ATVB 2015, 35, 2060–2072. [Google Scholar] [CrossRef] [Green Version]
- Gutterman, D.D. Vascular Dysfunction in Hyperglycemia. Circ. Res. 2002, 90, 5–7. [Google Scholar] [CrossRef]
- Mah, E.; Bruno, R.S. Postprandial Hyperglycemia on Vascular Endothelial Function: Mechanisms and Consequences. Nutr. Res. 2012, 32, 727–740. [Google Scholar] [CrossRef]
- Mah, E.; Noh, S.K.; Ballard, K.D.; Matos, M.E.; Volek, J.S.; Bruno, R.S. Postprandial Hyperglycemia Impairs Vascular Endothelial Function in Healthy Men by Inducing Lipid Peroxidation and Increasing Asymmetric Dimethylarginine:Arginine. J. Nutr. 2011, 141, 1961–1968. [Google Scholar] [CrossRef] [Green Version]
- Loader, J.; Meziat, C.; Watts, R.; Lorenzen, C.; Sigaudo-Roussel, D.; Stewart, S.; Reboul, C.; Meyer, G.; Walther, G. Effects of Sugar-Sweetened Beverage Consumption on Microvascular and Macrovascular Function in a Healthy Population. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 1250–1260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Förstermann, U.; Münzel, T. Endothelial Nitric Oxide Synthase in Vascular Disease: From Marvel to Menace. Circulation 2006, 113, 1708–1714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsuruta, R.; Fujita, M.; Ono, T.; Koda, Y.; Koga, Y.; Yamamoto, T.; Nanba, M.; Shitara, M.; Kasaoka, S.; Maruyama, I.; et al. Hyperglycemia Enhances Excessive Superoxide Anion Radical Generation, Oxidative Stress, Early Inflammation, and Endothelial Injury in Forebrain Ischemia/Reperfusion Rats. Brain Res. 2010, 1309, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Fabian, R.H.; Kent, T.A. Hyperglycemia Accentuates Persistent “Functional Uncoupling” of Cerebral Microvascular Nitric Oxide and Superoxide Following Focal Ischemia/Reperfusion in Rats. Transl. Stroke Res. 2012, 3, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Murphy, E.; Steenbergen, C. Mechanisms Underlying Acute Protection from Cardiac Ischemia-Reperfusion Injury. Physiol. Rev. 2008, 88, 581–609. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maessen, M.F.H.; van Mil, A.C.C.M.; Straathof, Y.; Riksen, N.P.; Rongen, G.A.P.J.M.; Hopman, M.T.E.; Eijsvogels, T.M.H.; Thijssen, D.H.J. Impact of Lifelong Exercise Training on Endothelial Ischemia-Reperfusion and Ischemic Preconditioning in Humans. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2017, 312, R828–R834. [Google Scholar] [CrossRef] [Green Version]
- DeVan, A.E.; Umpierre, D.; Lin, H.-F.; Harrison, M.L.; Tarumi, T.; Dhindsa, M.; Hunter, S.D.; Sommerlad, S.M.; Tanaka, H. Habitual Resistance Exercise and Endothelial Ischemia–Reperfusion Injury in Young Adults. Atherosclerosis 2011, 219, 191–193. [Google Scholar] [CrossRef] [Green Version]
- Zanesco, A.; Delbin, M.A.; Davel, A.P.; Bau, F.R.; Priviero, F.B.; Rossoni, L.V.; Antunes, E. Effect of Exercise Training on Endothelium-Dependent Relaxing Response and CGMP Concentration in Pulmonary Artery from Rats Submitted to Lung Ischemia/Reperfusion. BMC Pharmacol. 2009, 9, P77. [Google Scholar] [CrossRef] [Green Version]
- Farah, C.; Kleindienst, A.; Bolea, G.; Meyer, G.; Gayrard, S.; Geny, B.; Obert, P.; Cazorla, O.; Tanguy, S.; Reboul, C. Exercise-Induced Cardioprotection: A Role for ENOS Uncoupling and NO Metabolites. Basic. Res. Cardiol. 2013, 108, 389. [Google Scholar] [CrossRef]
- Laughlin, M.H. Joseph, B. Wolfe Memorial Lecture. Physical Activity in Prevention and Treatment of Coronary Disease: The Battle Line Is in Exercise Vascular Cell Biology. Med. Sci. Sports Exerc. 2004, 36, 352–362. [Google Scholar] [CrossRef]
- Rush, J.W.E.; Denniss, S.G.; Graham, D.A. Vascular Nitric Oxide and Oxidative Stress: Determinants of Endothelial Adaptations to Cardiovascular Disease and to Physical Activity. Can. J. Appl. Physiol. 2005, 30, 442–474. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meziat, C.; Boulghobra, D.; Strock, E.; Battault, S.; Bornard, I.; Walther, G.; Reboul, C. Exercise Training Restores ENOS Activation in the Perivascular Adipose Tissue of Obese Rats: Impact on Vascular Function. Nitric. Oxide. 2019, 86, 63–67. [Google Scholar] [CrossRef] [PubMed]
- Boulghobra, D.; Dubois, M.; Alpha-Bazin, B.; Coste, F.; Olmos, M.; Gayrard, S.; Bornard, I.; Meyer, G.; Gaillard, J.-C.; Armengaud, J.; et al. Increased Protein S-Nitrosylation in Mitochondria: A Key Mechanism of Exercise-Induced Cardioprotection. Basic. Res. Cardiol. 2021, 116, 66. [Google Scholar] [CrossRef] [PubMed]
- Quast, M.J.; Wei, J.; Huang, N.C.; Brunder, D.G.; Sell, S.L.; Gonzalez, J.M.; Hillman, G.R.; Kent, T.A. Perfusion Deficit Parallels Exacerbation of Cerebral Ischemia/Reperfusion Injury in Hyperglycemic Rats. J. Cereb. Blood Flow Metab. 1997, 17, 553–559. [Google Scholar] [CrossRef] [Green Version]
- Quast, M.J.; Wei, J.; Huang, N.C. Nitric Oxide Synthase InhibitorNG-Nitro-l-Arginine Methyl Ester Decreases Ischemic Damage in Reversible Focal Cerebral Ischemia in Hyperglycemic Rats. Brain Res. 1995, 677, 204–212. [Google Scholar] [CrossRef]
- Yamada, M.; Lamping, K.G.; Duttaroy, A.; Zhang, W.; Cui, Y.; Bymaster, F.P.; McKinzie, D.L.; Felder, C.C.; Deng, C.-X.; Faraci, F.M.; et al. Cholinergic Dilation of Cerebral Blood Vessels Is Abolished in M5 Muscarinic Acetylcholine Receptor Knockout Mice. Proc. Natl. Acad. Sci. USA 2001, 98, 14096–14101. [Google Scholar] [CrossRef] [Green Version]
- Sobey, C.G.; Faraci, F.M. Effects of a Novel Inhibitor of Guanylyl Cyclase on Dilator Responses of Mouse Cerebral Arterioles. Stroke 1997, 28, 837–842. [Google Scholar] [CrossRef]
- Kitayama, J.; Kitazono, T.; Ibayashi, S.; Wakisaka, M.; Watanabe, Y.; Kamouchi, M.; Nagao, T.; Fujishima, M. Role of Phosphatidylinositol 3-Kinase in Acetylcholine-Induced Dilatation of Rat Basilar Artery. Stroke 2000, 31, 2487–2493. [Google Scholar] [CrossRef] [Green Version]
- de Wit, C.; von Bismarck, P.; Pohl, U. Mediator Role of Prostaglandins in Acetylcholine-Lnduced Vasodilation and Control of Resting Vascular Diameter in the Hamster Cremaster Microcirculation in Vivo. JVR 1993, 30, 272–278. [Google Scholar] [CrossRef]
- Dóra, E.; Kovách, A.G. Effect of Topically Administered Epinephrine, Norepinephrine, and Acetylcholine on Cerebrocortical Circulation and the NAD/NADH Redox State. J. Cereb. Blood Flow Metab. 1983, 3, 161–169. [Google Scholar] [CrossRef]
- Killey, C.; Cleary, S.; Orr, J.; Frisbee, J.C.; Jackson, D.; Twynstra, J. The Contribution of Muscarinic-Receptor-Mediated Responses to Epineurial Vascular Diameter at the Sciatic Nerve. Can. J. Physiol. Pharmacol. 2018, 96, 855–858. [Google Scholar] [CrossRef]
- Winter, E.M.; Abt, G.A.; Nevill, A.M. Metrics of Meaningfulness as Opposed to Sleights of Significance. J. Sport. Sci. 2014, 32, 901–902. [Google Scholar] [CrossRef]
- Hopkins, W.G.; Marshall, S.W.; Batterham, A.M.; Hanin, J. Progressive Statistics for Studies in Sports Medicine and Exercise Science. Med. Sci. Sports Exerc. 2009, 41, 3–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ikebe, K.; Kato, T.; Yamaga, M.; Hirose, J.; Tsuchida, T.; Takagi, K. Increased Ischemia-Reperfusion Blood Flow Impairs the Skeletal Muscle Contractile Function. J. Surg. Res. 2001, 99, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Traupe, H.; Kruse, E.; Heiss, W.D. Reperfusion of Focal Ischemia of Varying Duration: Postischemic Hyper- and Hypo-Perfusion. Stroke 1982, 13, 615–622. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsuchidate, R.; He, Q.-P.; Smith, M.-L.; Siesjö, B.K. Regional Cerebral Blood Flow during and after 2 Hours of Middle Cerebral Artery Occlusion in the Rat. J. Cereb. Blood Flow Metab. 1997, 17, 1066–1073. [Google Scholar] [CrossRef] [Green Version]
- Tamura, A.; Asano, T.; Sano, K. Correlation between RCBF and Histological Changes Following Temporary Middle Cerebral Artery Occlusion. Stroke 1980, 11, 487–493. [Google Scholar] [CrossRef] [Green Version]
- Brownlee, M. Biochemistry and Molecular Cell Biology of Diabetic Complications. Nature 2001, 414, 813–820. [Google Scholar] [CrossRef]
- Thijssen, D.H.J.; Uthman, L.; Somani, Y.; van Royen, N. Short-term Exercise-induced Protection of Cardiovascular Function and Health: Why and How Fast Does the Heart Benefit from Exercise? J. Physiol. 2022, 600, 1339–1355. [Google Scholar] [CrossRef]
- Farah, C.; Nascimento, A.; Bolea, G.; Meyer, G.; Gayrard, S.; Lacampagne, A.; Cazorla, O.; Reboul, C. Key Role of Endothelium in the ENOS-Dependent Cardioprotection with Exercise Training. J. Mol. Cell. Cardiol. 2017, 102, 26–30. [Google Scholar] [CrossRef]
- Khalafi, M.; Sakhaei, M.H.; Kazeminasab, F.; Symonds, M.E.; Rosenkranz, S.K. The Impact of High-Intensity Interval Training on Vascular Function in Adults: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med. 2022, 9, 679–692. [Google Scholar] [CrossRef] [PubMed]
- Lennon, S.L.; Quindry, J.C.; French, J.P.; Kim, S.; Mehta, J.L.; Powers, S.K. Exercise and Myocardial Tolerance to Ischaemia-Reperfusion. Acta Physiol. Scand. 2004, 182, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Thijssen, D.H.J.; Benda, N.M.M.; Kerstens, T.P.; Seeger, J.P.H.; van Dijk, A.P.J.; Hopman, M.T.E. 12-Week Exercise Training, Independent of the Type of Exercise, Attenuates Endothelial Ischaemia-Reperfusion Injury in Heart Failure Patients. Front. Physiol. 2019, 10, 264. [Google Scholar] [CrossRef] [Green Version]
- Pearson, M.J.; Smart, N.A. Effect of Exercise Training on Endothelial Function in Heart Failure Patients: A Systematic Review Meta-Analysis. Int. J. Cardiol. 2017, 231, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Chakraphan, D.; Sridulyakul, P.; Thipakorn, B.; Bunnag, S.; Huxley, V.H.; Patumraj, S. Attenuation of Endothelial Dysfunction by Exercise Training in STZ-Induced Diabetic Rats. Clin. Hemorheol. Microcirc. 2005, 32, 217–226. [Google Scholar]
- Piepoli, M.F. Exercise Training in Chronic Heart Failure: Mechanisms and Therapies. Neth. Heart J. 2013, 21, 85–90. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grandperrin, A.; Bourgoin, M.; Gayrard, S.; Boulghobra, D.; Walther, G.; Reboul, C.; Meyer, G. Protective Role of Chronic Exercise Training in Modulating the Impact of Hyperglycemia on Vascular Sensitivity to Ischemia-Reperfusion. Nutrients 2023, 15, 212. https://doi.org/10.3390/nu15010212
Grandperrin A, Bourgoin M, Gayrard S, Boulghobra D, Walther G, Reboul C, Meyer G. Protective Role of Chronic Exercise Training in Modulating the Impact of Hyperglycemia on Vascular Sensitivity to Ischemia-Reperfusion. Nutrients. 2023; 15(1):212. https://doi.org/10.3390/nu15010212
Chicago/Turabian StyleGrandperrin, Antoine, Mathilde Bourgoin, Sandrine Gayrard, Doria Boulghobra, Guillaume Walther, Cyril Reboul, and Grégory Meyer. 2023. "Protective Role of Chronic Exercise Training in Modulating the Impact of Hyperglycemia on Vascular Sensitivity to Ischemia-Reperfusion" Nutrients 15, no. 1: 212. https://doi.org/10.3390/nu15010212





