Polyphenols and Cardiometabolic Health: Knowledge and Concern among Romanian People
Abstract
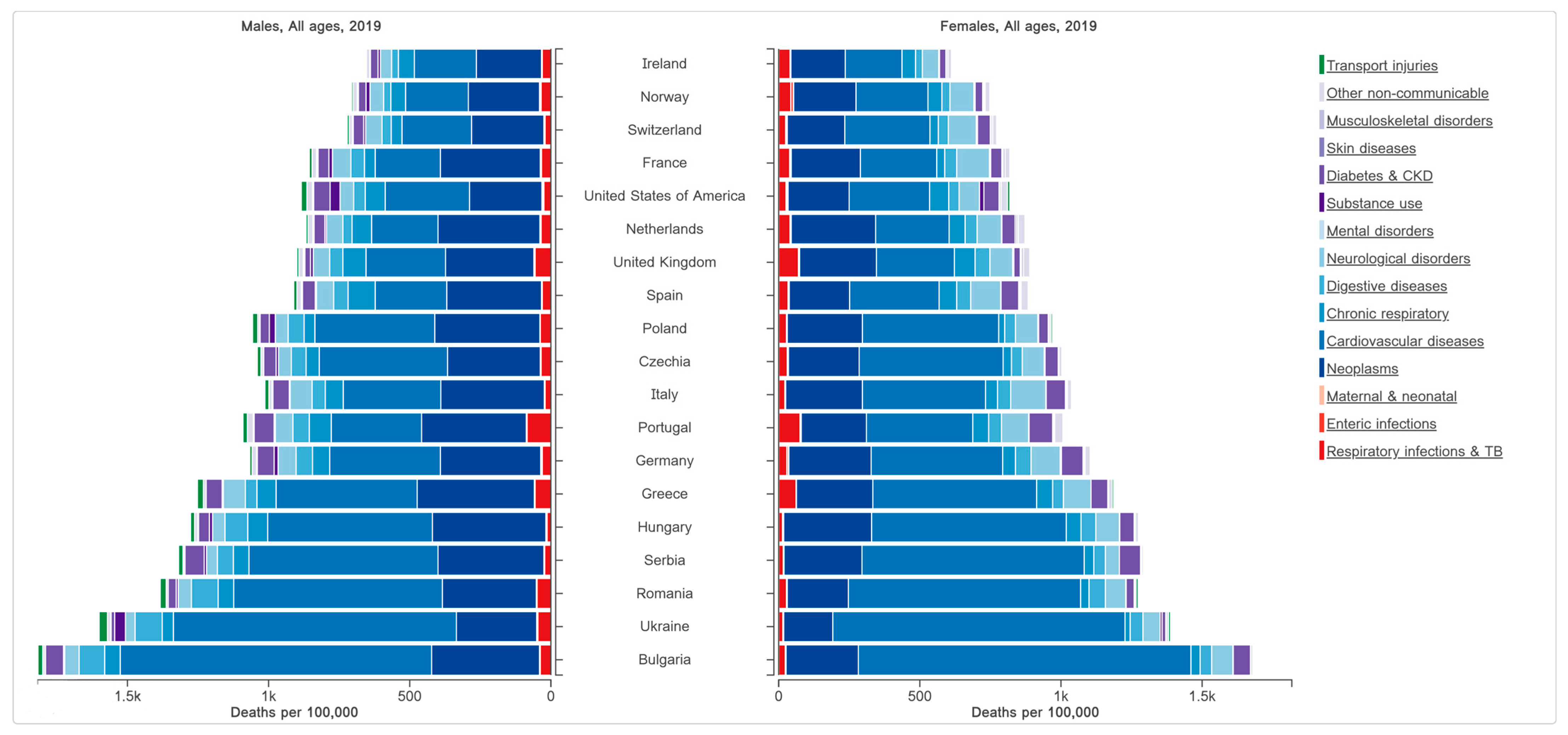
:1. Introduction
2. Materials and Methods
2.1. Online Survey
2.1.1. Participants
2.1.2. Survey Design
2.1.3. Questionnaire Instrument
2.1.4. Statistics
3. Results and Discussions
3.1. Respondents’ Characteristics
3.2. Health and Nutrition Concerns
3.3. CMR Awareness and Risk Knowledge
3.4. Polyphenol Knowledge
3.4.1. Consumption Frequency
3.4.2. General Knowledge of the Term “Polyphenols”
3.4.3. Health-Related Aspects of “Polyphenols”
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Questionnaire
References
- WHO World Health Organization: Noncommunicable Diseases: Mortality and Morbidity. Available online: https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/gho-ghe-ncd-mortality-and-morbidity (accessed on 27 February 2023).
- Adair, T. Premature cardiovascular disease mortality with overweight and obesity as a risk factor: Estimating excess mortality in the United States during the COVID-19 pandemic. Int. J. Obes. 2023, 47, 273–279. [Google Scholar] [CrossRef]
- The Institute for Health Metrics and Evaluation (IHME). GBD Compare; IHME, University of Washington: Seattle, WA, USA, 2015. [Google Scholar]
- Sagastume, D.; Siero, I.; Mertens, E.; Cottam, J.; Colizzi, C.; Peñalvo, J.L. The effectiveness of lifestyle interventions on type 2 diabetes and gestational diabetes incidence and cardiometabolic outcomes: A systematic review and meta-analysis of evidence from low- and middle-income countries. eClinicalMedicine 2022, 53, 101650. [Google Scholar] [CrossRef]
- Kilkenny, M.F.; Dunstan, L.; Busingye, D.; Purvis, T.; Reyneke, M.; Orgill, M.; Cadilhac, D.A. Knowledge of risk factors for diabetes or cardiovascular disease (CVD) is poor among individuals with risk factors for CVD. PLoS ONE 2017, 12, e0172941. [Google Scholar] [CrossRef]
- Mitrea, L.; Nemes, S.-A.; Szabo, K.; Teleky, B.-E.; Vodnar, D.-C. Guts Imbalance Imbalances the Brain: A Review of Gut Microbiota Association With Neurological and Psychiatric Disorders. Front. Med. 2022, 9, 813204. [Google Scholar] [CrossRef] [PubMed]
- Teleky, B.-E.; Mitrea, L.; Călinoiu, L.-F.; Martău, G.-A.; Vodnar, D.-C. Microbial Processes to Produce Food Ingredients and Products. In Reference Module in Food Science; Elsevier: Amsterdam, The Netherlands, 2023; pp. 1–17. ISBN 9780081005965. [Google Scholar]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart disease and stroke statistics—2021 update: A report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- Rudrapal, M.; Khairnar, S.J.; Khan, J.; Dukhyil, A.B.; Ansari, M.A.; Alomary, M.N.; Alshabrmi, F.M.; Palai, S.; Deb, P.K.; Devi, R. Dietary Polyphenols and Their Role in Oxidative Stress-Induced Human Diseases: Insights Into Protective Effects, Antioxidant Potentials and Mechanism(s) of Action. Front. Pharmacol. 2022, 13, 806470. [Google Scholar] [CrossRef] [PubMed]
- Călinoiu, L.F.; Vodnar, D.C. Whole Grains and Phenolic Acids: A Review on Bioactivity, Functionality, Health Benefits and Bioavailability. Nutrients 2018, 10, 1615. [Google Scholar] [CrossRef] [PubMed]
- Martau, G.A.; Teleky, B.-E.; Ranga, F.; Pop, I.D.; Vodnar, D.C. Apple Pomace as a Sustainable Substrate in Sourdough Fermentation. Front. Microbiol. 2021, 12, 742020. [Google Scholar] [CrossRef] [PubMed]
- Teleky, B.-E.; Mitrea, L.; Plamada, D.; Nemes, S.A.; Călinoiu, L.-F.; Pascuta, M.S.; Varvara, R.-A.; Szabo, K.; Vajda, P.; Szekely, C.; et al. Development of Pectin and Poly(vinyl alcohol)-Based Active Packaging Enriched with Itaconic Acid and Apple Pomace-Derived Antioxidants. Antioxidants 2022, 11, 1729. [Google Scholar] [CrossRef]
- Plamada, D.; Vodnar, D.C. Polyphenols—Gut Microbiota Interrelationship: A Transition to a New Generation of Prebiotics. Nutrients 2022, 14, 137. [Google Scholar] [CrossRef]
- Szabo, K.; Mitrea, L.; Călinoiu, L.F.; Teleky, B.-E.; Adria, G.; Plamada, D.; Pascuta, M.S.; Nemeş, S.-A.; Varvara, R.; Vodnar, D.C. Natural Polyphenols Recovery from Apple-, Cereal-, and Tomato-Processing By-Products, and Related Health-Promoting Properties. Molecules 2022, 27, 7977. [Google Scholar] [CrossRef]
- Pallag, A.; Bungau, S.; Tit, D.M.; Jurca, T.; Sirbu, V.; Honiges, A.; Horhogea, C. Comparative study of polyphenols, flavonoids and chlorophylls in Equisetum ar vense L. populations. Rev. Chim. 2016, 67, 530–533. [Google Scholar]
- Tressera-Rimbau, A.; Arranz, S.; Eder, M.; Vallverdú-Queralt, A. Dietary polyphenols in the prevention of stroke. Oxid. Med. Cell. Longev. 2017, 2017, 7467962. [Google Scholar] [CrossRef]
- Fan, Y.; Pedersen, O. Gut microbiota in human metabolic health and disease. Nat. Rev. Microbiol. 2021, 19, 55–71. [Google Scholar] [CrossRef]
- de Paulo Farias, D.; de Araújo, F.F.; Neri-Numa, I.A.; Pastore, G.M. Antidiabetic potential of dietary polyphenols: A mechanistic review. Food Res. Int. 2021, 145, 110383. [Google Scholar] [CrossRef]
- Carnauba, R.A.; Chaves, D.F.S.; Baptistella, A.B.; Paschoal, V.; Naves, A.; Buehler, A.M. Association between high consumption of phytochemical-rich foods and anthropometric measures: A systematic review. Int. J. Food Sci. Nutr. 2017, 68, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Cháirez-Ramírez, M.H.; de la Cruz-López, K.G.; García-Carrancá, A. Polyphenols as Antitumor Agents Targeting Key Players in Cancer-Driving Signaling Pathways. Front. Pharmacol. 2021, 12, 710304. [Google Scholar] [CrossRef]
- Godos, J.; Castellano, S.; Ray, S.; Grosso, G.; Galvano, F. Dietary polyphenol intake and depression: Results from the mediterranean healthy eating, lifestyle and aging (MEAL) study. Molecules 2018, 23, 999. [Google Scholar] [CrossRef] [PubMed]
- Sarapis, K.; George, E.S.; Marx, W.; Mayr, H.L.; Willcox, J.; Esmaili, T.; Powell, K.L.; Folasire, O.S.; Lohning, A.E.; Garg, M.; et al. Extra virgin olive oil high in polyphenols improves antioxidant status in adults: A double-blind, randomized, controlled, cross-over study (OLIVAUS). Eur. J. Nutr. 2022, 61, 1073–1086. [Google Scholar] [CrossRef] [PubMed]
- Martău, G.A.; Teleky, B.-E.; Odocheanu, R.; Soporan, D.A.; Bochis, M.; Simon, E.; Vodnar, D.C. Vaccinium Species (Ericaceae): Phytochemistry and Biological Properties of Medicinal Plants. Molecules 2023, 28, 1533. [Google Scholar] [CrossRef]
- Sharma, E.; Attri, D.C.; Sati, P.; Dhyani, P.; Szopa, A.; Sharifi-Rad, J.; Hano, C.; Calina, D.; Cho, W.C. Recent updates on anticancer mechanisms of polyphenols. Front. Cell Dev. Biol. 2022, 10, 1005910. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, G.V.; Alvares, T.S. Effect of curcumin on endothelial function in humans and their proposed physiological mechanism: Insights in formulating curcumin products supplementation. PharmaNutrition 2022, 22, 100313. [Google Scholar] [CrossRef]
- Nowrouzi-Sohrabi, P.; Hassanipour, S.; Sisakht, M.; Daryabeygi-Khotbehsara, R.; Savardashtaki, A.; Fathalipour, M. The effectiveness of pistachio on glycemic control and insulin sensitivity in patients with type 2 diabetes, prediabetes and metabolic syndrome: A systematic review and meta-analysis. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1589–1595. [Google Scholar] [CrossRef]
- Alves-Santos, A.M.; Sugizaki, C.S.A.; Lima, G.C.; Naves, M.M.V. Prebiotic effect of dietary polyphenols: A systematic review. J. Funct. Foods 2020, 74, 104169. [Google Scholar] [CrossRef]
- Liu, Y.C.; Li, X.Y.; Shen, L. Modulation effect of tea consumption on gut microbiota. Appl. Microbiol. Biotechnol. 2020, 104, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Precup, G.; Pocol, C.B.; Teleky, B.-E.; Vodnar, D.C. Awareness, Knowledge, and Interest about Prebiotics—A Study among Romanian Consumers. Int. J. Environ. Res. Public Health 2022, 19, 1208. [Google Scholar] [CrossRef]
- Teleky, B.E.; Martău, G.A.; Ranga, F.; Pop, I.D.; Vodnar, D.C. Biofunctional soy-based sourdough for improved rheological properties during storage. Sci. Rep. 2022, 12, 17535. [Google Scholar] [CrossRef] [PubMed]
- Smith, W.G. Does Gender Influence Online Survey Participation? A Record-Linkage Analysis of University Faculty Online Survey Response Behavior; San José State University: San Jose, CA, USA, 2008. [Google Scholar]
- Slauson-Blevins, K.; Johnson, K.M. Doing Gender, Doing Surveys? Women’s Gatekeeping and Men’s Non-Participation in Multi-Actor Reproductive Surveys. Sociol. Inq. 2016, 86, 427–449. [Google Scholar] [CrossRef]
- Ribot-Rodriguez, R.; Higuera-Gomez, A.; San-Cristobal, R.; Martín-Hernández, R.; Micó, V.; Espinosa-Salinas, I.; de Molina, A.R.; Martínez, J.A. Cardiometabolic Health Status, Ethnicity and Health-Related Quality of Life (HRQoL) Disparities in an Adult Population: NutrIMDEA Observational Web-Based Study. Int. J. Environ. Res. Public Health 2022, 19, 2948. [Google Scholar] [CrossRef]
- Sallis, J.F.; Floyd, M.F.; Rodríguez, D.A.; Saelens, B.E. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation 2012, 125, 729–737. [Google Scholar] [CrossRef]
- Zhang, N. Trends in urban/rural inequalities in cardiovascular risk bio-markers among Chinese adolescents in two decades of urbanisation: 1991–2011. Int. J. Equity Health 2018, 17, 101. [Google Scholar] [CrossRef]
- Gordon-Larsen, P.; Wang, H.; Popkin, B.M. Overweight dynamics in Chinese children and adults. Obes. Rev. 2014, 15, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Riha, J.; Karabarinde, A.; Ssenyomo, G.; Allender, S.; Asiki, G.; Kamali, A.; Young, E.H.; Sandhu, M.S.; Seeley, J. Urbanicity and Lifestyle Risk Factors for Cardiometabolic Diseases in Rural Uganda: A Cross-Sectional Study. PLoS Med. 2014, 11, e1001683. [Google Scholar] [CrossRef] [PubMed]
- Xiang, D.; Liu, Y.; Zhou, S.; Zhou, E.; Wang, Y. Protective Effects of Estrogen on Cardiovascular Disease Mediated by Oxidative Stress. Oxid. Med. Cell. Longev. 2021, 2021, 5523516. [Google Scholar] [CrossRef] [PubMed]
- Tit, D.M.; Bungau, S.; Iovan, C.; Cseppento, D.C.N.; Endres, L.; Sava, C.; Sabau, A.M.; Furau, G.; Furau, C. Effects of the hormone replacement therapy and of soy isoflavones on bone resorption in postmenopause. J. Clin. Med. 2018, 7, 297. [Google Scholar] [CrossRef] [PubMed]
- Fryar, C.D.; Ostchega, Y.; Hales, C.M.; Zhang, G.; Kruszon-Moran, D. Key findings Data from the National Health and Nutrition Examination Survey. Hypertens. Preval. Control. Adults USA 2015, 289, 2015–2016. [Google Scholar]
- Marques, A.; Peralta, M.; Naia, A.; Loureiro, N.; De Matos, M.G. Prevalence of adult overweight and obesity in 20 European countries, 2014. Eur. J. Public Health 2018, 28, 295–300. [Google Scholar] [CrossRef]
- Liu, J.; Fox, C.S.; Hickson, D.M.A.; May, W.D.; Hairston, K.G.; Carr, J.J.; Taylor, H.A. Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: The Jackson Heart Study. J. Clin. Endocrinol. Metab. 2010, 95, 5419–5426. [Google Scholar] [CrossRef]
- Montano, D. Education differences in cardiometabolic risk in England, Scotland and the United States between 1992 and 2019. BMC Cardiovasc. Disord. 2022, 22, 247. [Google Scholar] [CrossRef]
- Zajacova, A.; Lawrence, E.M. The Relationship between Education and Health: Reducing Disparities through a Contextual Approach. Annu. Rev. Public Health 2018, 39, 273–289. [Google Scholar] [CrossRef]
- Long, C.; Liu, P.; Yi, C. Does educational attainment affect residents’ health? Healthcare 2020, 8, 364. [Google Scholar] [CrossRef]
- Raghupathi, V.; Raghupathi, W. The influence of education on health: An empirical assessment of OECD countries for the period 1995–2015. Arch. Public Health 2020, 78, 20. [Google Scholar] [CrossRef] [PubMed]
- Health and Well-Being. Available online: https://www.who.int/data/gho/data/major-themes/health-and-well-being (accessed on 27 March 2023).
- Masic, I. Public Health Aspects of Global Population Health and Well-being in the 21st Century Regarding Determinants of Health. Int. J. Prev. Med. 2018, 9, 4. [Google Scholar] [CrossRef]
- Masic, I. Determinants of Health and Health Concepts According toWHO Targets. Int. J. Biomed. Health 2015, 3, 16–21. [Google Scholar]
- De Oliveira Otto, M.C.; Afshin, A.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Singh, G.; Danaei, G.; Sichieri, R.; Monteiro, C.A.; Louzada, M.L.C.; et al. The Impact of dietary and metabolic risk factors on cardiovascular diseases and type 2 diabetes mortality in Brazil. PLoS ONE 2016, 11, e0151503. [Google Scholar] [CrossRef] [PubMed]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef] [PubMed]
- Kamphuis, C.B.M.; Oude Groeniger, J.; Van Lenthe, F.J. Does cultural capital contribute to educational inequalities in food consumption in the Netherlands? A cross-sectional analysis of the GLOBE-2011 survey. Int. J. Equity Health 2018, 17, 168. [Google Scholar] [CrossRef]
- Fernández-Alvira, J.M.; Mouratidou, T.; Bammann, K.; Hebestreit, A.; Barba, G.; Sieri, S.; Reisch, L.; Eiben, G.; Hadjigeorgiou, C.; Kovacs, E.; et al. Parental education and frequency of food consumption in European children: The IDEFICS study. Public Health Nutr. 2013, 16, 487–498. [Google Scholar] [CrossRef]
- Azizi Fard, N.; De Francisci Morales, G.; Mejova, Y.; Schifanella, R. On the interplay between educational attainment and nutrition: A spatially-aware perspective. EPJ Data Sci. 2021, 10, 18. [Google Scholar] [CrossRef]
- Baraldi, L.G.; Martinez Steele, E.; Canella, D.S.; Monteiro, C.A. Consumption of ultra-processed foods and associated sociodemographic factors in the USA between 2007 and 2012: Evidence from a nationally representative cross-sectional study. BMJ Open 2018, 8, e020574. [Google Scholar] [CrossRef]
- Aiello, L.M.; Schifanella, R.; Quercia, D.; Del Prete, L. Large-scale and high-resolution analysis of food purchases and health outcomes. EPJ Data Sci. 2019, 8, 14. [Google Scholar] [CrossRef]
- Cundiff, J.M.; Lin, S.S.H.; Faulk, R.D.; McDonough, I.M. Educational quality may be a closer correlate of cardiometabolic health than educational attainment. Sci. Rep. 2022, 12, 18105. [Google Scholar] [CrossRef] [PubMed]
- Ek, S. Gender differences in health information behaviour: A Finnish population-based survey. Health Promot. Int. 2015, 30, 736–745. [Google Scholar] [CrossRef]
- McGuigan, R.D.; Wilkinson, J.M. Obesity and Healthcare Avoidance: A Systematic Review. AIMS Public Health 2015, 2, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Mensinger, J.L.; Tylka, T.L.; Calamari, M.E. Mechanisms underlying weight status and healthcare avoidance in women: A study of weight stigma, body-related shame and guilt, and healthcare stress. Body Image 2018, 25, 139–147. [Google Scholar] [CrossRef]
- Wändell, P.E.; De Waard, A.K.M.; Holzmann, M.J.; Gornitzki, C.; Lionis, C.; De Wit, N.; Søndergaard, J.; Sønderlund, A.L.; Kral, N.; Seifert, B.; et al. Barriers and facilitators among health professionals in primary care to prevention of cardiometabolic diseases: A systematic review. Fam. Pract. 2018, 35, 383–398. [Google Scholar] [CrossRef]
- Jørgensen, T.; Jacobsen, R.K.; Toft, U.; Aadahl, M.; Glümer, C.; Pisinger, C. Effect of screening and lifestyle counselling on incidence of ischaemic heart disease in general population: Inter99 randomised trial. BMJ 2014, 348, g3617. [Google Scholar] [CrossRef]
- Stol, D.M.; Over, E.A.B.; Badenbroek, I.F.; Hollander, M.; Nielen, M.M.J.; Kraaijenhagen, R.A.; Schellevis, F.G.; de Wit, N.J.; de Wit, G.A. Cost-effectiveness of a stepwise cardiometabolic disease prevention program: Results of a randomized controlled trial in primary care. BMC Med. 2021, 19, 57. [Google Scholar] [CrossRef]
- Stol, D.M.; Badenbroek, I.F.; Hollander, M.; Nielen, M.M.J.; Kraaijenhagen, R.A.; Schellevis, F.G.; de Wit, N.J. Effectiveness of a stepwise cardiometabolic disease prevention program: Results of a randomized controlled trial in primary care. Prev. Med. 2020, 132, 105984. [Google Scholar] [CrossRef] [PubMed]
- Van Den Brekel-Dijkstra, K.; Rengers, A.H.; Niessen, M.A.J.; De Wit, N.J.; Kraaijenhagen, R.A. Personalized prevention approach with use of a web-based cardiovascular risk assessment with tailored lifestyle follow-up in primary care practice—A pilot study. Eur. J. Prev. Cardiol. 2016, 23, 544–551. [Google Scholar] [CrossRef] [PubMed]
- Forster, A.S.; Burgess, C.; Dodhia, H.; Fuller, F.; Miller, J.; McDermott, L.; Gulliford, M.C. Do health checks improve risk factor detection in primary care? Matched cohort study using electronic health records. J. Public Health 2016, 38, 552–559. [Google Scholar] [CrossRef]
- de Waard, A.K.M.; Korevaar, J.C.; Hollander, M.; Nielen, M.M.J.; Seifert, B.; Carlsson, A.C.; Lionis, C.; Søndergaard, J.; Schellevis, F.G.; de Wit, N.J.; et al. Unwillingness to participate in health checks for cardiometabolic diseases: A survey among primary health care patients in five European countries. Health Sci. Rep. 2021, 4, e256. [Google Scholar] [CrossRef] [PubMed]
- Lewis, S.J.; Rodbard, H.W.; Fox, K.M.; Grandy, S. Self-reported prevalence and awareness of metabolic syndrome: Findings from SHIELD. Int. J. Clin. Pract. 2008, 62, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Lo, S.W.S.; Chair, S.Y.; Lee, I.F.K. Knowledge of metabolic syndrome in Chinese adults: Implications for health education. Health Educ. J. 2016, 75, 589–599. [Google Scholar] [CrossRef]
- Wang, Q.; Chair, S.Y.; Wong, E.M.L.; Taylor-Piliae, R.E.; Qiu, X.C.H.; Li, X.M. Metabolic syndrome knowledge among adults with cardiometabolic risk factors: A cross-sectional study. Int. J. Environ. Res. Public Health 2019, 16, 159. [Google Scholar] [CrossRef] [PubMed]
- Altman, R.; Nunez De Ybarra, J.; Villablanca, A.C. Community-based cardiovascular disease prevention to reduce cardiometabolic risk in latina women: A pilot program. J. Womens Health 2014, 23, 350–357. [Google Scholar] [CrossRef]
- Jones, E.J.; Appel, S.J.; Eaves, Y.D.; Moneyham, L.; Oster, R.A.; Ovalle, F. Cardiometabolic Risk, Knowledge, Risk Perception, and Self-Efficacy among American Indian Women with Previous Gestational Diabetes. JOGNN J. Obstet. Gynecol. Neonatal Nurs. 2012, 41, 246–257. [Google Scholar] [CrossRef]
- Zhernakova, D.V.; Sinha, T.; Andreu-Sánchez, S.; Prins, J.R.; Kurilshikov, A.; Balder, J.-W.; Sanna, S.; Franke, L.; Kuivenhoven, J.A.; Zhernakova, A.; et al. Age-dependent sex differences in cardiometabolic risk factors. Nat. Cardiovasc. Res. 2022, 1, 844–854. [Google Scholar] [CrossRef]
- Bakhtiyari, M.; Kazemian, E.; Kabir, K.; Hadaegh, F.; Aghajanian, S.; Mardi, P.; Ghahfarokhi, N.T.; Ghanbari, A.; Mansournia, M.A.; Azizi, F. Contribution of obesity and cardiometabolic risk factors in developing cardiovascular disease: A population-based cohort study. Sci. Rep. 2022, 12, 1544. [Google Scholar] [CrossRef]
- Hägg, S.; Fall, T.; Ploner, A.; Mägi, R.; Fischer, K.; Draisma, H.H.M.; Kals, M.; De Vries, P.S.; Dehghan, A.; Willems, S.M.; et al. Adiposity as a cause of cardiovascular disease: A Mendelian randomization study. Int. J. Epidemiol. 2015, 44, 578–586. [Google Scholar] [CrossRef]
- Csige, I.; Ujvárosy, D.; Szabó, Z.; Lorincz, I.; Paragh, G.; Harangi, M.; Somodi, S.; Santulli, G. The Impact of Obesity on the Cardiovascular System. J. Diabetes Res. 2018, 2018, 3407306. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, F.D.; Whelton, P.K. High Blood Pressure and Cardiovascular Disease. Hypertension 2020, 75, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Lewington, S.; Clark, R.; Qizilbash, N.; Peto, R.; Collins, R. Mortality: A Meta-Analysis of Individual Data for One Million Adults in 61 Prospective Studies. Lancet 2002, 360, 1903–1913. [Google Scholar]
- World Health Organization: Hypertension. Available online: https://www.who.int/news-room/fact-sheets/detail/hypertension (accessed on 24 March 2023).
- WHO World Health Organization: Diabetes. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 22 March 2023).
- Poznyak, A.V.; Litvinova, L.; Poggio, P.; Sukhorukov, V.N.; Orekhov, A.N. Effect of Glucose Levels on Cardiovascular Risk. Cells 2022, 11, 3034. [Google Scholar] [CrossRef]
- Cristi-Montero, C.; Chillón, P.; Labayen, I.; Casajus, J.A.; Gonzalez-Gross, M.; Vanhelst, J.; Manios, Y.; Moreno, L.A.; Ortega, F.B.; Ruiz, J.R. Cardiometabolic risk through an integrative classification combining physical activity and sedentary behavior in European adolescents: HELENA study. J. Sport Health Sci. 2019, 8, 55–62. [Google Scholar] [CrossRef]
- Zhuang, Z.; Gao, M.; Yang, R.; Li, N.; Liu, Z.; Cao, W.; Huang, T. Association of physical activity, sedentary behaviours and sleep duration with cardiovascular diseases and lipid profiles: A Mendelian randomization analysis. Lipids Health Dis. 2020, 19, 86. [Google Scholar] [CrossRef]
- Kelishadi, R.; Noori, A.; Qorbani, M.; Rahimzadeh, S.; Djalalinia, S.; Shafiee, G.; Motlagh, M.E.; Ardalan, G.; Ansari, H.; Asayesh, H.; et al. Are active and passive smoking associated with cardiometabolic risk factors in adolescents? The CASPIAN-III Study. Paediatr. Int. Child Health 2016, 36, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Gastaldelli, A.; Folli, F.; Maffei, S. Impact of Tobacco Smoking on Lipid Metabolism, Body Weight and Cardiometabolic Risk. Curr. Pharm. Des. 2010, 16, 2526–2530. [Google Scholar] [CrossRef]
- Schiattarella, G.G.; Sannino, A.; Esposito, G.; Perrino, C. Diagnostics and therapeutic implications of gut microbiota alterations in cardiometabolic diseases. Trends Cardiovasc. Med. 2019, 29, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Leustean, A.M.; Ciocoiu, M.; Sava, A.; Costea, C.F.; Floria, M.; Tarniceriu, C.C.; Tanase, D.M. Implications of the intestinal microbiota in diagnosing the progression of diabetes and the presence of cardiovascular complications. J. Diabetes Res. 2018, 2018, 5205126. [Google Scholar] [CrossRef]
- Salari, A.; Mahdavi-Roshan, M.; Kheirkhah, J.; Ghorbani, Z. Probiotics supplementation and cardiometabolic risk factors: A new insight into recent advances, potential mechanisms, and clinical implications. PharmaNutrition 2021, 16, 100261. [Google Scholar] [CrossRef]
- WHO World Health Organization: Cardiovascular Diseases (CVDs) Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 20 March 2023).
- Velagaleti, R.S.; Vasan, R.S. Heart Failure in the Twenty-First Century: Is it a Coronary Artery Disease or Hypertension Problem? Cardiol. Clin. 2007, 25, 487–495. [Google Scholar] [CrossRef]
- Wright, N.D.; Barnhart, J.; Freeman, K.; Walker, E.A. Coronary heart disease risk underestimation in a minority population: The Bronx Coronary Risk Perception Study. Prev. Med. 2010, 51, 434–435. [Google Scholar] [CrossRef]
- Mukattash, T.L.; Shara, M.; Jarab, A.S.; Al-Azzam, S.I.; Almaaytah, A.; Al Hamarneh, Y.N. Public knowledge and awareness of cardiovascular disease and its risk factors: A cross-sectional study of 1000 Jordanians. Int. J. Pharm. Pract. 2012, 20, 367–376. [Google Scholar] [CrossRef]
- Nielsen, J.B.; Leppin, A.; Gyrd-Hansen, D.E.; Jarbøl, D.E.; Søndergaard, J.; Larsen, P.V. Barriers to lifestyle changes for prevention of cardiovascular disease—A survey among 40–60-year old Danes. BMC Cardiovasc. Disord. 2017, 17, 245. [Google Scholar] [CrossRef]
- Lutz, M.; Fuentes, E.; Ávila, F.; Alarcón, M.; Palomo, I. Roles of phenolic compounds in the reduction of risk factors of cardiovascular diseases. Molecules 2019, 24, 366. [Google Scholar] [CrossRef]
- Bouchenak, M.; Lamri-Senhadji, M. Nutritional quality of legumes, and their role in cardiometabolic risk prevention: A review. J. Med. Food 2013, 16, 185–198. [Google Scholar] [CrossRef] [PubMed]
- Vetrani, C.; Vitale, M.; Bozzetto, L.; Della Pepa, G.; Cocozza, S.; Costabile, G.; Mangione, A.; Cipriano, P.; Annuzzi, G.; Rivellese, A.A. Association between different dietary polyphenol subclasses and the improvement in cardiometabolic risk factors: Evidence from a randomized controlled clinical trial. Acta Diabetol. 2018, 55, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Eurostat. How Much Fruit and Vegetables Do You Eat Daily?—Products Eurostat News—Eurostat. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/ddn-20220104-1 (accessed on 18 April 2023).
- Lavefve, L.; Howard, L.R.; Carbonero, F. Berry polyphenols metabolism and impact on human gut microbiota and health. Food Funct. 2020, 11, 45–65. [Google Scholar] [CrossRef] [PubMed]
- Magrone, T.; Russo, M.A.; Jirillo, E. Cocoa and dark chocolate polyphenols: From biology to clinical applications. Front. Immunol. 2017, 8, 677. [Google Scholar] [CrossRef]
- Aneklaphakij, C.; Saigo, T.; Watanabe, M.; Naake, T.; Fernie, A.R.; Bunsupa, S.; Satitpatipan, V.; Tohge, T. Diversity of Chemical Structures and Biosynthesis of Polyphenols in Nut-Bearing Species. Front. Plant Sci. 2021, 12, 642581. [Google Scholar] [CrossRef] [PubMed]
- Nemes, S.A.; Florina, L.; Dulf, F.V.; Corina, A.; Vodnar, D.C. Integrated Technology for Cereal Bran Valorization: Perspectives for a Sustainable Industrial Approach. Antioxidants 2022, 11, 2159. [Google Scholar] [CrossRef] [PubMed]
- Vodnar, D.C.; Calinoiu, L.F.; Mitrea, L. Editorial: Exploiting the effect of dietary fibre on the gut microbiota in patients with pelvic radiotherapy. Br. J. Cancer 2022, 127, 1575–1576. [Google Scholar] [CrossRef] [PubMed]
- Jantan, I.; Haque, M.A.; Arshad, L.; Harikrishnan, H.; Septama, A.W.; Mohamed-Hussein, Z.A. Dietary polyphenols suppress chronic inflammation by modulation of multiple inflammation-associated cell signaling pathways. J. Nutr. Biochem. 2021, 93, 108634. [Google Scholar] [CrossRef]
- Plamada, D.; Teleky, B.-E.; Nemes, S.A.; Mitrea, L.; Szabo, K.; Calinoiu, L.-F.; Pascuta, M.S.; Varvara, R.-A.; Ciont, C.; Mărtau, G.A.; et al. Plant-Based Dairy Alternatives—A Future Direction to the Milky Way. Foods 2023, 12, 1883. [Google Scholar] [CrossRef]
- Behl, T.; Bungau, S.; Kumar, K.; Zengin, G.; Khan, F.; Kumar, A.; Kaur, R.; Venkatachalam, T.; Tit, D.M.; Vesa, C.M.; et al. Pleotropic Effects of Polyphenols in Cardiovascular System. Biomed. Pharmacother. 2020, 130, 110714. [Google Scholar] [CrossRef]
- Kolehmainen, M.; Mykkänen, O.; Kirjavainen, P.V.; Leppänen, T.; Moilanen, E.; Adriaens, M.; Laaksonen, D.E.; Hallikainen, M.; Puupponen-Pimiä, R.; Pulkkinen, L.; et al. Bilberries reduce low-grade inflammation in individuals with features of metabolic syndrome. Mol. Nutr. Food Res. 2012, 56, 1501–1510. [Google Scholar] [CrossRef]
- Haș, I.M.; Teleky, B.-E.; Szabo, K.; Simon, E.; Ranga, F.; Zorița, M.D.; Purza, A.L.; Vodnar, D.-C.; Tit, D.M.; Nițescu, M. Bioactive Potential of Elderberry (Sambucus nigra L.): Antioxidant, Antimicrobial Activity, Bioaccessibility and Prebiotic Potential. Molecules 2023, 28, 3099. [Google Scholar] [CrossRef]
- Sata, Y.; Marques, F.Z.; Kaye, D.M. The Emerging Role of Gut Dysbiosis in Cardio-metabolic Risk Factors for Heart Failure. Curr. Hypertens. Rep. 2020, 22, 38. [Google Scholar] [CrossRef]
- Arora, A.; Behl, T.; Sehgal, A.; Singh, S.; Sharma, N.; Bhatia, S.; Sobarzo-Sanchez, E.; Bungau, S. Unravelling the involvement of gut microbiota in type 2 diabetes mellitus. Life Sci. 2021, 273, 119311. [Google Scholar] [CrossRef]
- Simon, E.; Călinoiu, L.F.; Mitrea, L.; Vodnar, D.C. Probiotics, prebiotics, and synbiotics: Implications and beneficial effects against irritable bowel syndrome. Nutrients 2021, 13, 2112. [Google Scholar] [CrossRef] [PubMed]
- Hussain, H.; Green, I.R. A patent review of the therapeutic potential of isoflavones (2012-2016). Expert Opin. Ther. Pat. 2017, 27, 1135–1146. [Google Scholar] [CrossRef] [PubMed]
- Kunnumakkara, A.B.; Bordoloi, D.; Padmavathi, G.; Monisha, J.; Roy, N.K.; Prasad, S.; Aggarwal, B.B. Curcumin, the golden nutraceutical: Multitargeting for multiple chronic diseases. Br. J. Pharmacol. 2017, 174, 1325–1348. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Kianpour, P.; Mohtashami, R.; Jafari, R.; Simental-Mendiá, L.E.; Sahebkar, A. Curcumin Lowers Serum Lipids and Uric Acid in Subjects with Nonalcoholic Fatty Liver Disease: A Randomized Controlled Trial. J. Cardiovasc. Pharmacol. 2016, 68, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Kubota, S.; Tanaka, Y.; Nagaoka, S. Ellagic acid affects mRNA expression levels of genes that regulate cholesterol metabolism in HepG2 cells. Biosci. Biotechnol. Biochem. 2019, 83, 952–959. [Google Scholar] [CrossRef] [PubMed]
- Amarowicz, R. Natural phenolic compounds protect LDL against oxidation. Eur. J. Lipid Sci. Technol. 2016, 118, 677–679. [Google Scholar] [CrossRef]
- Serreli, G.; Deiana, M. Role of Dietary Polyphenols in the Activity and Expression of Nitric Oxide Synthases: A Review. Antioxidants 2023, 12, 147. [Google Scholar] [CrossRef]
- Furuuchi, R.; Shimizu, I.; Yoshida, Y.; Hayashi, Y.; Ikegami, R.; Minamino, T. Boysenberry polyphenol inhibits endothelial dysfunction and improves vascular health. PLoS ONE 2018, 13, e0202051. [Google Scholar] [CrossRef]
- De Bruyne, T.; Steenput, B.; Roth, L.; De Meyer, G.R.Y.; Dos Santos, C.N.; Valentová, K.; Dambrova, M.; Hermans, N. Dietary polyphenols targeting arterial stiffness: Interplay of contributing mechanisms and gut microbiome-related Metabolism. Nutrients 2019, 11, 578. [Google Scholar] [CrossRef]
- Stainer, A.R.; Sasikumar, P.; Bye, A.P.; Unsworth, A.J.; Holbrook, L.M.; Tindall, M.; Lovegrove, J.A.; Gibbins, J.M. The Metabolites of the Dietary Flavonoid Quercetin Possess Potent Antithrombotic Activity, and Interact with Aspirin to Enhance Antiplatelet Effects. Th Open 2019, 3, 244–258. [Google Scholar] [CrossRef]
- Ludovici, V.; Barthelmes, J.; Nägele, M.P.; Flammer, A.J.; Sudano, I. Polyphenols: Anti-Platelet Nutraceutical? Current Pharmaceutical Design 2018, 24, 146–157. [Google Scholar] [CrossRef]
- Kim, Y.; Cho, A.Y.; Kim, H.C.; Ryu, D.; Jo, S.A.; Jung, Y. Effects of Natural Polyphenols on Oxidative Stress-Mediated Blood-Brain Barrier Dysfunction. Antioxidants 2022, 11, 197. [Google Scholar] [CrossRef]
- Ahmadi, A.; Jamialahmadi, T.; Sahebkar, A. Polyphenols and atherosclerosis: A critical review of clinical effects on LDL oxidation. Pharmacol. Res. 2022, 184, 106414. [Google Scholar] [CrossRef]
- Sun, C.; Zhao, C.; Guven, E.C.; Simal-gandara, J.; Ramkumar, K.M.; Buleu, F.; Tomas, M.; Paoli, P.; Wang, S.; Pah, A.; et al. Dietary polyphenols as antidiabetic agents: Advances and opportunities. Food Frontiers 2020, 1, 18–44. [Google Scholar] [CrossRef]
- Williamson, G.; Sheedy, K. Effects of polyphenols on insulin resistance. Nutrients 2020, 12, 3135. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Miao, M. Dietary polyphenols modulate starch digestion and glycaemic level: A review. Crit. Rev. Food Sci. Nutr. 2019, 0, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Williamson, G. Effects of Polyphenols on Glucose-Induced Metabolic Changes in Healthy Human Subjects and on Glucose Transporters. Mol. Nutr. Food Res. 2022, 66, 2101113. [Google Scholar] [CrossRef]
- Golovinskaia, O.; Wang, C.K. The hypoglycemic potential of phenolics from functional foods and their mechanisms. Food Sci. Hum. Wellness 2023, 12, 986–1007. [Google Scholar] [CrossRef]
- Villa-rodriguez, J.A.; Ifie, I.; Gonzalez-aguilar, G.A.; Roopchand, D.E. The Gastrointestinal Tract as Prime Site for Cardiometabolic Protection by Dietary Polyphenols. Adv. Nutr. 2019, 10, 999–1011. [Google Scholar] [CrossRef] [PubMed]
- Fraga, C.G.; Croft, K.D.; Kennedy, D.O.; Tomás-Barberán, F.A. The effects of polyphenols and other bioactives on human health. Food Funct. 2019, 10, 514–528. [Google Scholar] [CrossRef]








| Demographics | n | % | n | % | |
|---|---|---|---|---|---|
| Gender | Elevated BP/treatment | ||||
| Female | 440 | 80.6 | Yes | 68 | 12.5 |
| Male | 106 | 19.4 | No | 478 | 87.5 |
| Provenience | Smoking | ||||
| Urban | 426 | 78 | Yes | 128 | 23.4 |
| Rural | 120 | 22 | No | 418 | 76.6 |
| Age | BMI (kg/m2) | ||||
| 18–29 years | 116 | 21.2 | Underweight | 15 | 2.7 |
| 30–39 years | 127 | 23.3 | Normal weight | 277 | 50.7 |
| 40–49 years | 217 | 39.7 | Overweight | 161 | 29.5 |
| >50 years | 86 | 15.8 | Obese | 93 | 17 |
| Education level | FH of CVD or Diabetes | ||||
| University | 469 | 85.9 | Yes | 394 | 72.2 |
| Post-secondary | 37 | 6.8 | No | 131 | 24 |
| High school | 33 | 6 | Don’t know | 21 | 3.9 |
| Vocational school | 7 | 1.3 | |||
| Hyperglycemia/treatment | Elevated LDL-c | ||||
| Yes | 20 | 3.7 | Yes | 85 | 15.6 |
| No | 526 | 96.3 | No | 461 | 84.4 |
| Elevated TG | |||||
| Yes | 42 | 7.7 | |||
| No | 504 | 923 |
| Food Products | Consumption Frequency (%) | |||||
|---|---|---|---|---|---|---|
| Daily | Once/ Week | Several Times/ Week | Several Times/ Month | 1–2 Times/ Year | Not at All | |
| Whole grains | 52 ± 1.3 b | 123 ± 2.2 b | 180 ± 2.4 b | 99 ± 1.6 c | 52 ± 1.3 b | 40 ± 1.1 a |
| Berries | 26 ± 1.8 c | 120 ± 2.8 b | 159 ± 1.2 c | 161 ± 2.1 a | 69 ± 1.5 b | 11 ± 0.9 b |
| Nuts | 39 ± 2.1 c | 133 ± 1.7 a | 150 ± 1.6 c | 155 ± 2.3 a | 58 ± 1.2 b | 11 ± 1.0 b |
| Seeds | 25 ± 1.2 c | 121 ± 3.3 b | 130 ± 2.7 d | 137 ± 2.7 b | 86 ± 1.7 a | 47 ± 1.4 a |
| Aromatic herbs/spices | 161 ± 3.1 a | 82 ± 1.5 c | 185 ± 3.0 b | 64 ± 1.5 d | 27 ± 0.9 c | 27 ± 1.3 a |
| Cocoa powder/dark chocolate | 17 ± 1.0 c | 155 ± 3.7 a | 176 ± 3.1 b | 117 ± 2.3 b | 55 ± 1.3 b | 26 ± 1.5 a |
| Olive oil | 129 ± 2.9 a | 93 ± 1.4 c | 191 ± 2.3 b | 64 ± 1.4 d | 37 ± 1.2 c | 32 ± 1.1 a |
| Onion/Garlic | 142 ± 1.8 a | 95 ± 1.7 c | 249 ± 2.7 a | 38 ± 1.2 e | 14 ± 0.8 c | 8 ± 0.5 b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haș, I.M.; Teleky, B.-E.; Vodnar, D.-C.; Ștefănescu, B.E.; Tit, D.M.; Nițescu, M. Polyphenols and Cardiometabolic Health: Knowledge and Concern among Romanian People. Nutrients 2023, 15, 2281. https://doi.org/10.3390/nu15102281
Haș IM, Teleky B-E, Vodnar D-C, Ștefănescu BE, Tit DM, Nițescu M. Polyphenols and Cardiometabolic Health: Knowledge and Concern among Romanian People. Nutrients. 2023; 15(10):2281. https://doi.org/10.3390/nu15102281
Chicago/Turabian StyleHaș, Ioana Mariana, Bernadette-Emőke Teleky, Dan-Cristian Vodnar, Bianca Eugenia Ștefănescu, Delia Mirela Tit, and Maria Nițescu. 2023. "Polyphenols and Cardiometabolic Health: Knowledge and Concern among Romanian People" Nutrients 15, no. 10: 2281. https://doi.org/10.3390/nu15102281
APA StyleHaș, I. M., Teleky, B.-E., Vodnar, D.-C., Ștefănescu, B. E., Tit, D. M., & Nițescu, M. (2023). Polyphenols and Cardiometabolic Health: Knowledge and Concern among Romanian People. Nutrients, 15(10), 2281. https://doi.org/10.3390/nu15102281










