Exploring Overnutrition, Overweight, and Obesity in the Hospital Setting—A Point Prevalence Study
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Prevalence of Overweight and Obesity
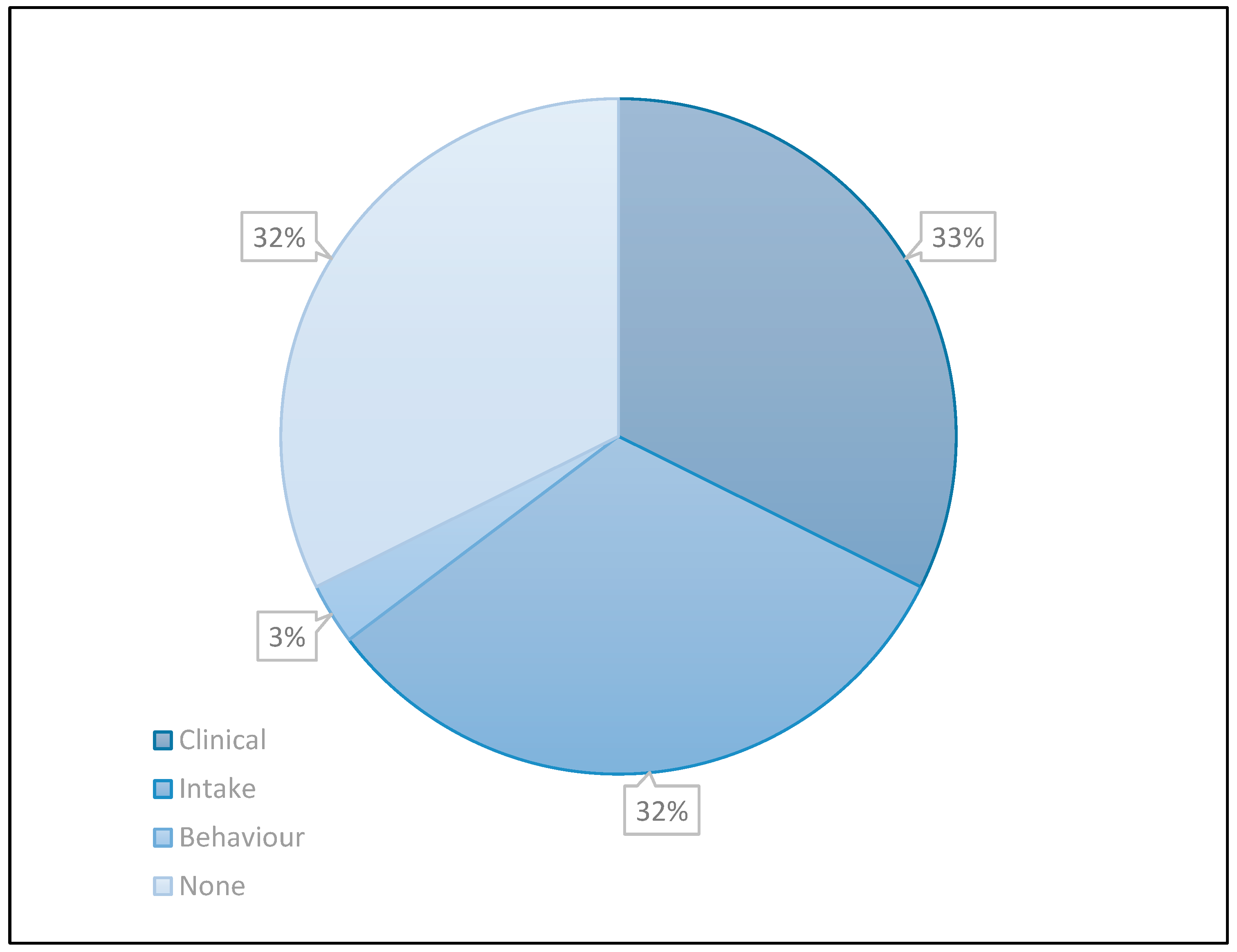
3.2. Nutrition Care Characteristics
3.3. Comparison to Population Data
3.4. Regression Analysis
4. Discussion
4.1. Strengths and Limitations
4.2. Implications for Clinical Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Classification of Weight Status by BMI Category, Adults > 18 Years | ||||||||
|---|---|---|---|---|---|---|---|---|
| Underweight | Normal | Total Underweight/ Normal | Overweight | Obese Class I | Obese Class II/III | Total Obese | Total Overweight/ Obese | |
| <18.5 kg/m2 | 18.5–24.9 kg/m2 | <24.99 kg/m2 | 25–29.9 kg/m2 | 30–34.9 kg/m2 | 35.0 kg/m2 | 30.00 kg/m2 | 25.00 kg/m2 or More | |
| Cohort % | 5.8 | 36.8 | 42.9 | 29.8 | 15.4 | 12.1 | 27.5 | 57.1 |
| Victoria [20] | 1.0 | 30.6 | 31.7 | 36.6 | 20.5 | 11.3 | 31.8 | 68.3 |
| National [20] | - | - | 34.2 | 36.6 | - | - | - | 65.8 |
References
- Agarwal, E.; Ferguson, M.; Banks, M.; Bauer, J.; Capra, S.; Isenring, E. Nutritional status and dietary intake of acute care patients: Results from the Nutrition Care Day Survey 2010. Clin. Nutr. 2012, 31, 41–47. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Curtis, L.J.; Bernier, P.; Jeejeebhoy, K.; Allard, J.; Duerksen, D.; Gramlich, L.; Laporte, M.; Keller, H.H. Costs of hospital malnutrition. Clin. Nutr. 2016, 36, 1391–1396. [Google Scholar] [CrossRef] [PubMed]
- Gomes, F.; Emery, P.W.; Weekes, C.E. Risk of Malnutrition Is an Independent Predictor of Mortality, Length of Hospital Stay, and Hospitalization Costs in Stroke Patients. J. Stroke Cerebrovasc. Dis. 2016, 25, 799–806. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cass, A.R.; Charlton, K.E. Prevalence of hospital-acquired malnutrition and modifiable determinants of nutritional deterioration during inpatient admissions: A systematic review of the evidence. J. Hum. Nutr. Diet. 2022, 35, 1043–1058. [Google Scholar] [CrossRef]
- Marshall, K.M.; Loeliger, J.; Nolte, L.; Kelaart, A.; Kiss, N.K. Prevalence of malnutrition and impact on clinical outcomes in cancer services: A comparison of two time points. Clin. Nutr. 2018, 38, 644–651. [Google Scholar] [CrossRef]
- Tappenden, K.A.; Quatrara, B.; Parkhurst, M.L.; Malone, A.M.; Fanjiang, G.; Ziegler, T.R. Critical Role of Nutrition in Improving Quality of Care: An Interdisciplinary Call to Action to Address Adult Hospital Malnutrition. J. Parenter. Enter. Nutr. 2013, 37, 482–497. [Google Scholar] [CrossRef]
- Australian Commission on Safety and Quality in Health Care. National Safety and Quality Health Service Standards (Second Edition); 2021. Available online: https://www.safetyandquality.gov.au/publications-and-resources/resource-library/national-safety-and-quality-health-service-standards-second-edition (accessed on 13 March 2023).
- Agarwal, E.; Ferguson, M.; Banks, M.; Batterham, M.; Bauer, J.; Capra, S.; Isenring, E. Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: Results from the Nutrition Care Day Survey 2010. Clin. Nutr. 2013, 32, 737–745. [Google Scholar] [CrossRef][Green Version]
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.J.; et al. GLIM criteria for the diagnosis of malnutrition—A consensus report from the global clinical nutrition community. Clin. Nutr. 2019, 38, 1–9. [Google Scholar] [CrossRef][Green Version]
- Shetty, P. Malnutrition and undernutrition. Medicine 2006, 34, 524–529. [Google Scholar] [CrossRef]
- Nguyen, A.T.; Tsai, C.-L.; Hwang, L.-Y.; Lai, D.; Markham, C.; Patel, B. Obesity and Mortality, Length of Stay and Hospital Cost among Patients with Sepsis: A Nationwide Inpatient Retrospective Cohort Study. PLoS ONE 2016, 11, e0154599. [Google Scholar] [CrossRef]
- Hauck, K.; Hollingsworth, B. The Impact of Severe Obesity on Hospital Length of Stay. Med. Care 2010, 48, 335–340. [Google Scholar] [CrossRef]
- Fusco, K.; Thompson, C.; Woodman, R.; Horwood, C.; Hakendorf, P.; Sharma, Y. The Impact of Morbid Obesity on the Health Outcomes of Hospital Inpatients: An Observational Study. J. Clin. Med. 2021, 10, 4382. [Google Scholar] [CrossRef]
- Gil, J.A.; Durand, W.; Johnson, J.P.; Goodman, A.D.; Daniels, A.H. Effect of Obesity on Perioperative Complications, Hospital Costs, and Length of Stay in Patients With Open Ankle Fractures. J. Am. Acad. Orthop. Surg. 2019, 27, e529–e534. [Google Scholar] [CrossRef]
- Terada, T.; Johnson, J.A.; Norris, C.; Padwal, R.; Qiu, W.; Sharma, A.M.; Janzen, W.; Forhan, M. Severe Obesity Is Associated With Increased Risk of Early Complications and Extended Length of Stay Following Coronary Artery Bypass Grafting Surgery. J. Am. Heart Assoc. 2016, 5, e003282. [Google Scholar] [CrossRef][Green Version]
- Mathison, C. Skin and wound care challenges in the hospitalized morbidly obese patient. J. Wound Ostomy Cont. Nurs. 2003, 30, 78–83. [Google Scholar] [CrossRef]
- Bochicchio, G.V.; Joshi, M.; Bochicchio, K.; Nehman, S.; Tracy, K.J.; Scalea, T.M. Impact of Obesity in the Critically Ill Trauma Patient: A Prospective Study. J. Am. Coll. Surg. 2006, 203, 533–538. [Google Scholar] [CrossRef]
- Schetz, M.; De Jong, A.; Deane, A.M.; Druml, W.; Hemelaar, P.; Pelosi, P.; Pickkers, P.; Reintam-Blaser, A.; Roberts, J.; Sakr, Y.; et al. Obesity in the critically ill: A narrative review. Intensiv. Care Med. 2019, 45, 757–769. [Google Scholar] [CrossRef]
- Korda, R.J.; Joshy, G.; Paige, E.; Butler, J.R.G.; Jorm, L.R.; Liu, B.; Bauman, A.E.; Banks, E. The Relationship between Body Mass Index and Hospitalisation Rates, Days in Hospital and Costs: Findings from a Large Prospective Linked Data Study. PLoS ONE 2015, 10, e0118599. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. Overweight and Obesity; AIHW: Canberra, Australia, 2022. [Google Scholar]
- Eastern Health. Eastern Health Annual Report; Eastern Health: Mount Pearl, NL, Canada, 2019; Available online: https://www.easternhealth.org.au/component/cobalt/category-items/3-publications/2-annual-reports?Itemid=170 (accessed on 13 March 2023).
- National Health and Medical Research Council. Ethical Considerations in Quality Assurance and Evaluation Activities; National Health and Medical Research Council: Canberra, Australia, 2014. [Google Scholar]
- Nestle Nutrition Institute Nutritional Screening as Easy as MNA. Available online: http://www.mna-elderly.com/forms/mna_guide_english (accessed on 13 March 2023).
- World Health Organization (WHO). Obesity: Preventing and Managing the Global Epidemic Report of a WHO Consultation; WHO Technical Report Series 894; WHO: Geneva, Switzerland, 2000. [Google Scholar]
- Ferguson, M.; Capra, S.; Bauer, J.; Banks, M. Development of a valid and reliable malnutrition screening tool for adult acute hospital patients. Nutrition 1999, 15, 458–464. [Google Scholar] [CrossRef]
- Independent Health and Aged Care Pricing Authority. The International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM/ACHI/ACS), 12th ed.; Independent Health and Aged Care Pricing Authority: Darlinghurst, Australia, 2022.
- Swan, W.I.; Vivanti, A.; Hakel-Smith, N.A.; Hotson, B.; Orrevall, Y.; Trostler, N.; Howarter, K.B.; Papoutsakis, C. Nutrition Care Process and Model Update: Toward Realizing People-Centered Care and Outcomes Management. J. Acad. Nutr. Diet. 2017, 117, 2003–2014. [Google Scholar] [CrossRef]
- Academy of Nutrition and Dietetics. Nutrition Terminology Reference Manual (ENCPT): Dietetics Language for Nutrition Care; Academy of Nutrition and Dietetics: Cleveland, OH, USA, 2016. [Google Scholar]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef] [PubMed]
- Pallant, J. SPSS Survival Manual: A Step by Step Guide to Data Analysis Using IBM SPSS, 7th ed.; Routledge: London, UK, 2020; ISBN 978-1-00-311745-2. [Google Scholar]
- Di Bella, A.; Comans, T.; Gane, E.; Young, A.; Hickling, D.; Lucas, A.; Hickman, I.; Banks, M. Underreporting of Obesity in Hospital Inpatients: A Comparison of Body Mass Index and Administrative Documentation in Australian Hospitals. Healthcare 2020, 8, 334. [Google Scholar] [CrossRef] [PubMed]
- Dennis, D.M.; Carter, V.; Trevenen, M.; Tyler, J.; Perrella, L.; Lori, E.; Cooper, I. Do acute hospitalised patients in Australia have a different body mass index to the general Australian population: A point prevalence study? Aust. Health Rev. 2018, 42, 121–129. [Google Scholar] [CrossRef][Green Version]
- Inoue, Y.; Qin, B.; Poti, J.; Sokol, R.; Gordon-Larsen, P. Epidemiology of Obesity in Adults: Latest Trends. Curr. Obes. Rep. 2018, 7, 276–288. [Google Scholar] [CrossRef]
- Hossain, M.A.; Amin, A.; Paul, A.; Qaisar, H.; Akula, M.; Amirpour, A.; Gor, S.; Giglio, S.; Cheng, J.; Mathew, R.; et al. Recognizing Obesity in Adult Hospitalized Patients: A Retrospective Cohort Study Assessing Rates of Documentation and Prevalence of Obesity. J. Clin. Med. 2018, 7, 203. [Google Scholar] [CrossRef][Green Version]
- Gupta, T.; Kolte, D.; Mohananey, D.; Khera, S.; Goel, K.; Mondal, P.; Aronow, W.S.; Jain, D.; Cooper, H.A.; Iwai, S.; et al. Relation of Obesity to Survival After In-Hospital Cardiac Arrest. Am. J. Cardiol. 2016, 118, 662–667. [Google Scholar] [CrossRef]
- Cederholm, T.; Rothenberg, E.; Barazzoni, R. A Clinically Relevant Diagnosis Code for “Malnutrition in Adults” Is Needed in ICD-11. J. Nutr. Health Aging 2022, 26, 314–315. [Google Scholar] [CrossRef]
- Sen, C.K. Human Wounds and Its Burden: An Updated Compendium of Estimates. Adv. Wound Care 2019, 8, 39–48. [Google Scholar] [CrossRef][Green Version]
- Ness, S.J.; Hickling, D.F.; Bell, J.J.; Collins, P.F. The pressures of obesity: The relationship between obesity, malnutrition and pressure injuries in hospital inpatients. Clin. Nutr. 2017, 37, 1569–1574. [Google Scholar] [CrossRef]
- Nghiem, S.; Campbell, J.; Walker, R.M.; Byrnes, J.; Chaboyer, W. Pressure injuries in Australian public hospitals: A cost of illness study. Int. J. Nurs. Stud. 2022, 130, 104191. [Google Scholar] [CrossRef]
- Hannan, E.L.; Zhong, Y.; Lahey, S.J.; Culliford, A.T.; Gold, J.P.; Smith, C.R.; Higgins, R.S.; Jordan, D.; Wechsler, A. 30-Day Readmissions After Coronary Artery Bypass Graft Surgery in New York State. JACC Cardiovasc. Interv. 2011, 4, 569–576. [Google Scholar] [CrossRef][Green Version]
- Dickerson, R.N.; Andromalos, L.; Brown, J.C.; Correia, M.I.T.D.; Pritts, W.; Ridley, E.J.; Robinson, K.N.; Rosenthal, M.D.; van Zanten, A.R.H. Obesity and critical care nutrition: Current practice gaps and directions for future research. Crit. Care 2022, 26, 283. [Google Scholar] [CrossRef]
- Phruetthiphat, O.-A.; Otero, J.E.; Zampogna, B.; Vasta, S.; Gao, Y.; Callaghan, J.J. Predictors for readmission following primary total hip and total knee arthroplasty. J. Orthop. Surg. 2020, 28, 2309499020959160. [Google Scholar] [CrossRef]
- Ayyagari, R.; Revol, C.; Tang, W.; Faust, E.; Tuttle, E. Association of Obesity with 30-day readmission rates among patients Hospitalized with Acute Bacterial Skin and Skin-Structure Infections (ABSSSI). Value Health 2015, 18, A186. [Google Scholar] [CrossRef][Green Version]
- Manu, P.; Khan, S.; Radhakrishnan, R.; Russ, M.J.; Kane, J.M.; Correll, C.U. Body Mass Index Identified as an Independent Predictor of Psychiatric Readmission. J. Clin. Psychiatry 2014, 75, e573–e577. [Google Scholar] [CrossRef]
- Dietitians Australia (DA). The Leading Voice in Nutrition and Dietetics. Available online: https://dietitiansaustralia.org.au/ (accessed on 13 March 2023).
- British Dietetic Association (BDA). Available online: https://www.bda.uk.com/ (accessed on 13 March 2023).
- Academy of Nutrition and Dietetics, Eatright.Org. Available online: https://www.eatright.org/ (accessed on 13 March 2023).
- Vivanti, A.; Lewis, J.; O’Sullivan, T.A. The Nutrition Care Process Terminology: Changes in Perceptions, Attitudes, Knowledge and Implementation amongst Australian Dietitians after Three Years: Nutrition Care Process Terminology after Three Years. Nutr. Diet. 2018, 75, 87–97. [Google Scholar] [CrossRef]
- Kim, J.; Lim, H. Nutritional Management in Childhood Obesity. J. Obes. Metab. Syndr. 2019, 28, 225–235. [Google Scholar] [CrossRef][Green Version]
- Vo, R.; Smith, M.; Patton, N. The role of dietitian clinical judgement in the nutrition care process within the acute care setting: A qualitative study. J. Hum. Nutr. Diet. 2021, 34, 124–133. [Google Scholar] [CrossRef]
- Genitsaridi, S.-M.; Giannios, C.; Karampatsou, S.; Papageorgiou, I.; Papadopoulos, G.; Farakla, I.; Koui, E.; Georgiou, A.; Romas, S.; Terzioglou, E.; et al. A Comprehensive Multidisciplinary Management Plan Is Effective in Reducing the Prevalence of Overweight and Obesity in Childhood and Adolescence. Horm. Res. Paediatr. 2020, 93, 94–107. [Google Scholar] [CrossRef]
- Picot, J.; Jones, J.; Colquitt, J.; Gospodarevskaya, E.; Loveman, E.; Baxter, L.; Clegg, A. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: A systematic review and economic evaluation. Health Technol. Assess. 2009, 13, 1–357. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Abbott, S.; Parretti, H.M.; Greenfield, S. Experiences and perceptions of dietitians for obesity management: A general practice qualitative study. J. Hum. Nutr. Diet. 2021, 34, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Madigan, C.D.; Graham, H.E.; Sturgiss, E.; Kettle, V.E.; Gokal, K.; Biddle, G.; Taylor, G.M.J.; Daley, A.J. Effectiveness of weight management interventions for adults delivered in primary care: Systematic review and meta-analysis of randomised controlled trials. BMJ 2022, 377, e069719. [Google Scholar] [CrossRef] [PubMed]
- Mold, F.; Forbes, A. Patients’ and Professionals’ Experiences and Perspectives of Obesity in Health-Care Settings: A Synthesis of Current Research: Patients’and Professionals’ Experiences. Health Expect. 2013, 16, 119–142. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Diversi, T.M.; Hughes, R.; Burke, K.J. The prevalence and practice impact of weight bias amongst Australian dietitians. Obes. Sci. Pract. 2016, 2, 456–465. [Google Scholar] [CrossRef]
- Panza, G.A.; Armstrong, L.E.; Taylor, B.A.; Puhl, R.M.; Livingston, J.; Pescatello, L.S. Weight Bias among Exercise and Nutrition Professionals: A Systematic Review: Weight Bias in Exercise and Nutrition. Obes. Rev. 2018, 19, 1492–1503. [Google Scholar] [CrossRef]
- Cassiano, G.S.; Carvalho-Ferreira, J.P.; Buckland, N.J.; da Cunha, D.T. Do Registered Dietitians, Nutrition Students, and Laypeople Perceive Individuals with Obesity Differently? Int. J. Environ. Res. Public Health 2021, 18, 8925. [Google Scholar] [CrossRef]
- Qvist, A.; Pazsa, F.; Hitch, D. Perceptions of clinical leaders and managers of inpatients with obesity in an Australian public health service. J. Hosp. Manag. Health Policy 2021, 5, 15. [Google Scholar] [CrossRef]
- Hales, C.; Coombs, M.; de Vries, K. The challenges in caring for morbidly obese patients in Intensive Care: A focused ethnographic study. Aust. Crit. Care 2018, 31, 37–41. [Google Scholar] [CrossRef]
- Elliott, A.; Gibson, S. Exploring stakeholder experiences of dietetic service and care delivery: A systematic qualitative review. J. Hum. Nutr. Diet. 2022, 36, 288–310. [Google Scholar] [CrossRef]
- Swinburn, B.A.; Kraak, V.I.; Allender, S.; Atkins, V.J.; Baker, P.I.; Bogard, J.R.; Brinsden, H.; Calvillo, A.; De Schutter, O.; Devarajan, R.; et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. Lancet 2019, 393, 791–846. [Google Scholar] [CrossRef]
- Jaacks, L.M.; Vandevijvere, S.; Pan, A.; McGowan, C.J.; Wallace, C.; Imamura, F.; Mozaffarian, D.; Swinburn, B.; Ezzati, M. The obesity transition: Stages of the global epidemic. Lancet Diabetes Endocrinol. 2019, 7, 231–240. [Google Scholar] [CrossRef]

| Classification of Weight Status by BMI Category | p * | |||||||
|---|---|---|---|---|---|---|---|---|
| All | Underweight | Normal | Overweight | Obese Class I | Obese Class II | Obese Class III | ||
| <18.5 kg/m2 | 18.5–24.9kg/m2 | 25–29.9 kg/m2 | 30–34.9 kg/m2 | 35–39.9 kg/m2 | ≥40 kg/m2 | |||
| Characteristics | 513 (100%) | 30 (5.8%) | 189 (36.8%) | 153 (29.8%) | 79 (15.4%) | 35 (6.8%) | 27 (5.3%) | – |
| Age (years) Median (IQR) | 73 (59–83) | 89 (74–94) | 78 (65–84) | 73 (54–82) | 69 (58–79) | 72 (57–82) | 64 (59–73) | <0.001 |
| Sex (female) n (%) | 255 (49.7%) | 17 (56.7%) | 91 (47.9%) | 60 (39.5%) | 45 (56.3%) | 21 (61.8%) | 21 (77.8%) | 0.002 |
| BMI (kg/m2) Median (IQR) | 25.7 (22.2–30.4) | 17.2 (16.4–18.2) | 22.2 (20.7–23.7) | 27.3 (25.7–28.5) | 31.8 (30.7–33.2) | 37.0 (35.9–38.2) | 46.1 (43.8–50.6) | <0.001 |
| Min-Max | 13.9–78.1 | 13.9 –19.0 | 18.5–24.9 | 25.0–29.9 | 27.9–34.9 | 35.0–39.6 | 40.3–78.1 | |
| Nutrition risk score | 0.767 | |||||||
| Not at risk n (%) | 249 (68.8%) | 12 (40%) | 82 (43.4%) | 73 (47.7%) | 41 (51.9%) | 23 (65.7%) | 18 (66.7%) | |
| At risk n (%) | 113 (31.2%) | 11 (36.6%) | 56 (29.7%) | 32 (20.9%) | 8 (10.1%) | 3 (8.6%) | 3 (11.1%) | |
| Incomplete n (%) | 151 (29.4%) | 7 (23.4%) | 51 (27.0%) | 48 (31.4%) | 30 (38.0%) | 8 (23.5%) | 6 (22.2%) | |
| Malnutrition Diagnosis | <0.001 | |||||||
| Yes n (%) | 86 (16.8%) | 21 (70%) | 47 (24.9%) | 14(9.2%) | 1 (1.3%) | 2 (5.7%) | 1 (3.7%) | |
| Dietetic intervention | <0.001 | |||||||
| Yes n (%) | 191 (37.2%) | 22 (73.3%) | 77 (40.7%) | 58 (37.9%) | 19 (24.1%) | 7 (20.0%) | 8 (29.6%) | |
| Classification of Weight Status by BMI Category | p # | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| All | Underweight | Normal | Overweight | Obese Class I | Obese Class II | Obese Class III | |||
| Program | Characteristics | <18.5 kg/m2 | 18.5–24.9 kg/m2 | 25–29.9 kg/m2 | 30–34.9 kg/m2 | 35–39.9 kg/m2 | ≥40 kg/m2 | ||
| Acute * | n (%) | 330 (100%) | 16 (4.8%) | 107 (32.4%) | 105 (31.8%) | 60 (18.2%) | 26 (7.9%) | 16 (4.8%) | |
| 64.3% | Age (years) | ||||||||
| Median (IQR) | 70 (55–81) | 78 (69–89) | 74 (59–83) | 70 (48–82) | 68 (57–77) | 69 (48–73) | 62 (48–70) | 0.015 | |
| Sex (female) | |||||||||
| n (%) | 147 (44.5%) | 6 (4.1%) | 45 (30.6%) | 38 (25.9%) | 33 (22.4%) | 14 (9.5%) | 11 (7.5%) | 0.053 | |
| BMI (kg/m2) | |||||||||
| Median (IQR) | 26.7 (23.1–31) | 17.9 (17.1–18.3) | 22.2 (20.8–23.8) | 27.3 (25.7–28.7) | 31.7 (30.7–32.9) | 37.1 (36.1–38.3) | 46.2 (41.4–51.9) | <0.001 | |
| Subacute * | n (%) | 153 (100%) | 14 (9.2%) | 63(41.2%) | 42 (27.5%) | 17 (11.1%) | 6 (3.9%) | 11 (7.2%) | |
| 29.8% | Age (years) | ||||||||
| Median (IQR) | 79 (65–86) | 93 (89–96) | 82 (71–86) | 76 (64–84) | 73 (58–82) | 67 (60–81) | 68 (60–82) | <0.001 | |
| Sex (female) | |||||||||
| n (%) | 90 (58.8%) | 11 (12.2%) | 34 (37.8%) | 20 (22.2%) | 10 (11.1%) | 5 (5.6%) | 10 (11.1%) | 0.047 | |
| BMI (kg/m2) | |||||||||
| Median (IQR) | 25 (21.8–29.3) | 16.45 (15.5–17.5) | 22.3 (20.6–23.6) | 27.6 (26.0–28.4) | 32.7 (31.6–33.3) | 36.9 (35.8–37.2) | 46.0 (45.0–49.7) | <0.001 | |
| Transition Care * | n (%) | 30 (100%) | 0 (0.0%) | 19 (63.3%) | 6 (20.0%) | 2 (6.7%) | 3 (10.0%) | 0 (0.0%) | |
| 5.8% | Age (years) | 0.730 | |||||||
| Median (IQR) | 81 (73–86) | – | 81 (72–86) | 83 (80–86) | 79 (68–89) | 81 (72–81) | – | ||
| Sex (female) | 0.355 | ||||||||
| n (%) | 18 (60%) | 0 (0.0%) | 12 (66.7%) | 2 (11.1%) | 2 (11.1%) | 2 (11.1%) | 0 (0.0%) | ||
| BMI (kg/m2) | |||||||||
| Median (IQR) | 23.5 (21–25.5) | – | 21.4 (20.5–23.5) | 25.4 (25.2–25.7) | 30.0 (29.6–30.3) | 35.0 (35.0–38.8) | <0.001 | ||
| Domain | Diagnosis | Number of Patients with Diagnosis |
|---|---|---|
| Clinical | Morbid obesity | 3 |
| Well-nourished | 7 | |
| Severely malnourished | 1 | |
| Intake | Inadequate intake | 8 |
| Inadequate carbohydrate intake | 1 | |
| Adequate intake | 1 | |
| Excessive intake | 1 | |
| Behavior | Nutrition knowledge deficit | 1 |
| No diagnosis | 11 |
| Dependent Variable: BMI kgm−2 | |||
|---|---|---|---|
| Independent Variables: | Β | Sig | Contribution% |
| Age Sex | −0.217 −0.136 | <0.001 0.000 | 4.12% 1.77% |
| Clinical Program | −0.042 | 0.239 | 0.23% |
| Malnutrition Screen (yes/no) | 0.093 | 0.076 | 0.52% |
| Nutrition risk score | −0.165 | 0.020 | 1.56% |
| Malnutrition diagnosis (yes/no) | −0.277 | <0.001 | 5.15% |
| Assessment and care by a Dietitian (yes/no) | 0.014 | 0.775 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elliott, A.; Gibson, S.; Bauer, J.; Cardamis, A.; Davidson, Z. Exploring Overnutrition, Overweight, and Obesity in the Hospital Setting—A Point Prevalence Study. Nutrients 2023, 15, 2315. https://doi.org/10.3390/nu15102315
Elliott A, Gibson S, Bauer J, Cardamis A, Davidson Z. Exploring Overnutrition, Overweight, and Obesity in the Hospital Setting—A Point Prevalence Study. Nutrients. 2023; 15(10):2315. https://doi.org/10.3390/nu15102315
Chicago/Turabian StyleElliott, Andrea, Simone Gibson, Judy Bauer, Anna Cardamis, and Zoe Davidson. 2023. "Exploring Overnutrition, Overweight, and Obesity in the Hospital Setting—A Point Prevalence Study" Nutrients 15, no. 10: 2315. https://doi.org/10.3390/nu15102315
APA StyleElliott, A., Gibson, S., Bauer, J., Cardamis, A., & Davidson, Z. (2023). Exploring Overnutrition, Overweight, and Obesity in the Hospital Setting—A Point Prevalence Study. Nutrients, 15(10), 2315. https://doi.org/10.3390/nu15102315







