Abstract
The utilization of youth (older) and peer (same age) mentor-led interventions to improve nutrition and physical activity has been an emerging trend in recent years. This systematic review is intended to synthesize the effectiveness of these intervention programs on participants and mentors based on biometric, nutrition, physical activity, and psychosocial outcomes of youth and peer mentor-led interventions among children and adolescents. Online databases, including PubMed, ScienceDirect, EBSCOhost and Google Scholar, were searched, and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. A three-step screening process was used to meet the proposed eligibility criteria, and the risk-of-bias tool for randomized trials (RoB 2) was used to assess bias for the included studies. Nineteen unique intervention programs and twenty-five total studies were deemed eligible when considering the criteria required for review. Multiple studies demonstrated positive evidence of the biometric and physical activity outcomes that were considered significant. The findings regarding the nutritional outcomes across the included studies were mixed, as some studies reported significant changes in eating habits while others did not find a significant change. Overall, the utilization of youth and peer mentor-led models in nutrition- and physical-activity-related interventions may be successful in overweight and obesity prevention efforts for those children and adolescents receiving the intervention and the youths and peers leading the interventions. More research is needed to explore the impact on the youths and peers leading the interventions and disseminating more detailed implementation strategies, e.g., training mentors would allow for advancements in the field and the replicability of approaches. Terminology: In the current youth- and peer-led nutrition and physical activity intervention literature, a varying age differential exists between the targeted sample and the peers, and varying terminology with regards to how to name or refer to the youth. In some instances, the youth mentors were individuals of the same grade as the target sample who either volunteered to serve in the peer role or were selected by their fellow students or school staff. In other cases, the youth mentors were slightly older individuals, either in high school or college, who were selected based upon their experience, leadership skills, passion for the project, or demonstration of healthy lifestyle behaviors.
1. Introduction
Globally, rates of childhood overweight and obesity have risen dramatically over the past three decades, and the World Health Organization’s latest reports indicate that 18% of children and adolescents worldwide are experiencing overweight or obesity. In the United States (US) [1], the overall rates of childhood obesity are high, increasing steadily over the past couple of years, despite a previous plateau [2]. According to the National Health and Nutrition Examination Survey (NHANES) data from 2017 to March 2020, obesity affected 19.7% of US youths aged 2–19 years [3]. Hispanic and Non-Hispanic Black youth are more likely to be affected by obesity than Non-Hispanic White (26.2%, 24.8%, vs. 16.6%, respectively) [3]. The detrimental effects of overweight and obesity on youth developmental, physical, mental, and social health, as well as academic progress, speaks to the gravity of this nutritional public health issue [4,5]. Additionally, dietary habits, such as fruit and vegetable consumption, are developed earlier in life and maintained throughout adulthood [6]. Therefore, effective nutrition intervention strategies promoting health behaviors must be developed and implemented, specifically targeting youth, in order to prevent obesity along with its negative consequences.
The causes and factors related to overweight, and obesity are complex, especially among children and adolescents. In addition to excess calories, various obesogenic behaviors (i.e., low physical activity, sedentary behaviors, short sleep) further promote weight gain [7]. Changing these behaviors requires an understanding of the interplay between the multilevel factors that are influencing it, which can be explained through behavior change theories [7]. A common theoretical approach utilized in community nutrition and physical activity interventions to prevent overweight and obesity is the social cognitive theory (SCT) [8,9]. According to the SCT, behavioral changes can be learned through interactions comprising personal, behavioral, and environmental factors. Peer influence (of the same age) is one example of an environmental factor influencing behavior. The concept of peer influence is not limited to the SCT, but also plays a role in social inoculation and social norms theories [10,11]. The underlying similarities in each of these theories are that peers advise each other, peers are influenced by the expectations, attitudes, and behaviors of their friend groups, and that peer influence may be stronger than an adult or professional influence [12,13]. It is well known that peer influence increases substantially during adolescence, because it is at this life stage that youth attempt to establish independence from adults [14]. Peer dynamics are such a prominent environmental influence. Therefore, interventions with child and adolescent populations should utilize peers to promote healthy behaviors [14,15]. One way to do this is through peer mentorship programs.
Peer-led interventions have been utilized among youth in areas pertaining to the use of alcohol, tobacco, illegal drugs, violence, and sexual behavior [16,17,18,19,20,21,22,23]. Data indicate that mentored youth, when compared to unmentored youth are less likely to participate in these aforementioned risky behaviors and are more likely to succeed academically [24,25,26,27,28,29]. The use of peers as an intervention strategy to improve nutrition and physical activity, and ultimately weight status, had not been employed until more recently. Two previous systematic reviews have been published: one examining peer-led nutrition education programs and the other examining peer-led physical activity education programs [30,31]. These reviews were also limited to the school setting and the training of peer mentors was analyzed in one review but overlooked in the other [30,31]. The proper training of mentors and an analysis of the training are necessary to successfully implement and disseminate an intervention.
Due to the prevalence of overweight and obesity and the risk of weight gain throughout childhood and adolescence, coupled with the increased autonomy children and adolescents experience in making diet- and physical activity-related decisions, capitalizing on peer influence to promote diet and physical activity among adolescents is crucial. As Rhodes et al. acknowledged, the research findings from peer-based interventions can be complex given the potentially confounding—characteristics of multiple individuals involved, formed relationship quality, etc. [32]. Therefore, it is the responsibility of the scientific community to successfully analyze and communicate findings to the field [32]. To the best of the authors’ knowledge, no reviews have been published synthesizing child nutrition- and physical activity-related health intervention studies that utilize a peer-led model. Thus, the objectives of this study were to:
- Examine the training of peers and implementation of peer roles when developing peer-led nutrition and physical activity interventions.
- Evaluate the extent to which peer-led nutrition and physical activity interventions had an effect on biometrics, nutrition, physical activity, and psychosocial outcomes on child and adolescent intervention participants.
- Evaluate to what extent peer-led nutrition and physical activity interventions had an effect on biometrics, nutrition, physical activity, and psychosocial outcomes on the peers themselves.
- Evaluate process outcomes of the peer-led nutrition and physical activity interventions.
It is hypothesized that peer-led nutrition and physical activity interventions will have positive impacts on child biometric, nutrition, physical activity, and psychosocial outcomes, as well as the peers’ biometric, nutrition, physical activity, and psychosocial outcomes who are delivering the intervention activities.
2. Materials and Methods
2.1. Study Design
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline was employed during the literature review process for this study [33] An extensive search of online databases was conducted to gather articles pertaining to peer-led nutrition and physical activity interventions for children and adolescents to prevent obesity and chronic disease. PubMed, ScienceDirect, EBSCOhost, and GoogleScholar were thoroughly searched in 2018 and 2022 using key words, in varying combinations, including, but not limited to, the following: peer, peer mentor, peer mentor, youth leader, youth mentor, peer-led, mentor, mentoring, mentee, friend, nutrition, physical activity, exercise, support, social support, community, school, children, adolescent, diet, food, fruit, vegetable, prevention, health, obesity, overweight, and chronic disease. The references were also reviewed to identify additional, relevant articles. After removal of duplicates, these search procedures resulted in 667 potential studies. A schematic diagram of the PRISMA guideline is provided in Figure 1.
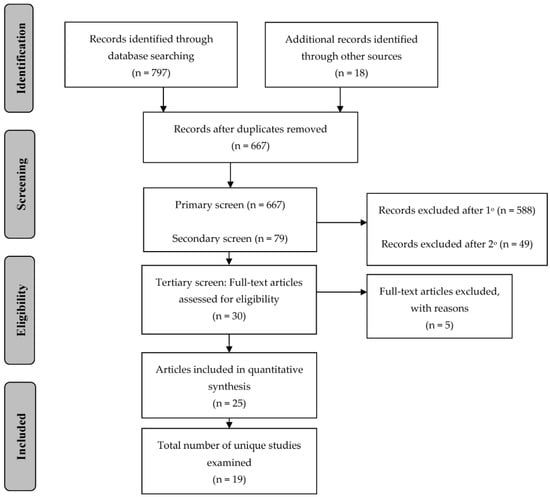
Figure 1.
Preferred Reporting Information for Systematic Reviews and Meta Analyses (PRISMA) schematic of article selection.
2.2. Inclusion and Exclusion Criteria
The following inclusion and exclusion criteria were used when screening the 667 articles for study eligibility. Overweight- and obesity-related health measures and behaviors, including weight, waist circumference, dietary intake and nutrition, and physical activity, were the outcomes of interest among school-aged children and adolescents (kindergarten through 12th grade). Individuals serving in “youth” or “peer” (defined below in Section 2.6) leadership roles must have been utilized in some manner during the delivery of the intervention. Studies in which the priority population had a pre-existing condition or disease, such as type 1 diabetes or cancer, were excluded. Studies in which extensive specificity of the target population limited the generalizability of the findings e.g., students attending boarding schools, were also excluded. Articles reviewing the same intervention trial were included due to the differing and contributory content of the articles. Studies presenting qualitative data were considered if the qualitative data augmented quantitative data collected for the same study.
2.3. Screening Protocol
A three-step screening process was conducted on the potential articles to determine article inclusion based on eligibility criteria (see Figure 1). The search and critical screening process were carried out by two authors (ML and LH). Discrepancies were discussed and a collective decision was made for inclusion or exclusion. The primary screening was conducted in which articles were eliminated due to irrelevancy based on title and a review of the abstract to identify the eligibility of the target population or outcomes of interest. This resulted in 79 potentially relevant articles. Next, a secondary screen was conducted in which articles were eliminated based on a review of the abstract and a brief scan of the entire article to match the remaining inclusion criteria, resulting in 30 potentially relevant articles. Major reasons for study exclusion during the secondary screen were limited generalizability based on the target population and the type of data presented (e.g., only qualitative data or process measures). Finally, the 30 articles were read in entirety for the tertiary screen and included if the inclusion criteria for the review were met, resulting in 25 articles addressing 19 unique studies.
2.4. Data Extraction
Following the tertiary screening process, the data were extracted in tabular format. Relevant information was extracted from the research articles including author(s) and year (included as the reference), study design, setting, participants, details regarding the use of youth or peer mentors, outcomes, and results. See Table 1.

Table 1.
Summary of Reviewed Studies Addressing Peer-Led Interventions to Improve Biometric, Nutrition, and Physical Activity Outcomes among Children and Adolescents.
2.5. Risk of Bias Assessment
The Cochrane risk-of-bias version 2 tool for randomized trials (RoB 2) was used to assess bias for included studies [57]. All studies were assessed with an overall bias judgement of ‘some concern’ [15,16,29,34,35,38,44,45,46,47,48,49,53,54,55,56] or ‘high risk’ [36,37,40,41,42,43,50,51,52,58]. The prevailing reason for bias was that participants or interventionists were aware of the treatment condition, which is a reality of social and behavioral intervention research. The prevailing reason that studies were assessed as ‘high risk’ was that the research designs were quasi-experimental in nature. See Table 2.

Table 2.
Risk of Bias Assessment for Included Studies using RoB 2 [57].
2.6. Definition of “Youth” and “Peer”
For the purposes of this literature review, the term ‘youth mentor’ will be used to refer to youth mentors that were older than the target sample and the term ‘peer mentor’ will be used to refer to youth mentors that were of similar age as the target sample, regardless of the terminology that was used by the investigators and authors of the interventions and studies.
3. Results
3.1. Overview of the Intervention Trials
Nineteen independent interventions were discussed in the final 25 selected articles. Table 1 contains an overview of each study included in this review, organized alphabetically by intervention trial name [See Appendix A for brief descriptions of each intervention].
The age range of the target populations as well as the settings for the interventions varied. Three of the interventions targeted elementary-school aged children, specifically children in kindergarten through sixth grade [42,43,44], while two interventions spanned the elementary-school and middle-school years [34,36]. Seven of the interventions concentrated on adolescents in middle school grades [16,38,39,40,48,49,50,52,54,55,56], while two interventions spanned both middle school and high school [35,47]. Finally, five interventions targeted solely high school-aged adolescents [15,37,41,45,46,53].
A majority of the studies were conducted in the US; however, three of the studies were conducted in Canada [37,42,43] and four were conducted in United Kingdom [48,49,51,56]. Almost all of the interventions took place either in school or after-school settings; one of the interventions took place in the homes of the participants [35]. More than half of the interventions were conducted in urban settings [29,34,35,36,37,38,39,40,41,42,43,47,50,52], several were conducted in suburban settings [15,16,38,39,48,49,51,53,54,55,56], and three were conducted in a rural setting [42,45,46]. The study designs varied across the interventions. Twelve of the studies were experimental [15,16,29,34,35,38,44,45,46,47,48,49,50,51,53,54,55,56], six were quasi-experimental [36,37,41,42,43,52], and one was a prospective observational study [40].
3.2. Training of Youth Mentors and Peer Mentors
Ten of the interventions utilized a youth mentor structure in which the peers were older than the target sample [29,34,36,37,40,41,42,44,51,56,58], while the other nine interventions utilized a peer mentor structure in which the peers were the same age as the target sample [15,16,38,39,43,46,48,49,50,51,52,53,54,55]. The amount of training that was provided to the youth mentors and peer mentors varied extensively, as did the amount of information and detail about the trainings. The most robust trainings and provisions of details were for the Challenge!, Fluids Used Effectively for Living (FUEL), Peer education About Weight Steadiness (PAWS), B’more Healthy Communities for Kids (BHCK), and HealthCorps interventions [29,34,35,37,41,50]. Intermediate amounts of training, spanning over several hours, and details were provided for the Healthy Hearty Kids Program (H2K), Just for Kids!, Move to Be Active (MBA), and Teens Eating for Eating for Energy and Nutrition at Schools (TEENS) interventions [16,43,44,45,46,54,55]. Finally, minimal training details were provided for the Cool Girls, Inc., Go Girls!, Girls Active Project (GAP), Healthy Buddies, MOVE Project, Peer-Led physical Activity iNterventions for Adolescent Girls (PLAN-A), Slice of Life, Students for Nutrition and eXercise (SNaX), Trying Alternative Cafeteria Options in Schools (TACOS), and the Walking in ScHools (WISH) interventions [15,36,37,38,39,40,47,48,49,53,56].
The most extensive information pertaining to the selection and training of youth mentors was provided for the Challenge! intervention. Inclusion criteria for project Challenge! mentors consisted of having a personal healthy lifestyle, expressing interest in being a role model, having experience with youth, and demonstrating commitment to the surrounding urban communities [29]. The mentee to mentor ratio was approximately 4–5:1 and a majority of the pairs were matched based on gender and race [29]. Training of mentors was approximately 40 h in length. During the training, mentors learned about the intervention, adolescent development, motivational interviewing, active listening, safety at home and in the surrounding neighborhoods, behavior management, and goal setting [29].
Similar to project Challenge!, training of youth mentors in the HealthCorps PAWS, and FUEL interventions spanned a course of weeks. Youth mentors in the HealthCorps study received a total of four weeks of training. Two weeks of the training pertained to nutrition, physical activity, and mental resilience, and the other two weeks pertained to professional development [41]. In the FUEL study, youth mentors received an “intensive” two-week training covering team building and curriculum content [37]. However, the total numbers of training hours for the HealthCorps or FUEL peer mentors were not noted [37,41].
The peer training for the H2K, Just for Kids!, PLAN-A, and TEENS, along with the interventions themselves were much shorter in length, ranging from one to two days. The peer mentors in the H2K study either volunteered or were recommended by school staff. These peer mentors underwent a 1-day, in-school training workshop that included leadership and team building training, as well as review of peer mentors’ responsibility in the H2K intervention [43]. In the Just for Kids! intervention trial, youth mentors were trained for six hours spanning a two-day period. Content of the training included learning about the intervention and responsibilities as a youth mentor, sharing viewpoints, discussing differing viewpoints as a group, motivating children, and practicing intervention delivery through role-playing [30]. In addition to pre-intervention training, youth mentors were supervised by an adult during the intervention sessions and debriefed after the sessions for reinforcement and subsequent weeks preparations [44]. Mentors in the PLAN-A study were selected by peers and participated in fifteen hours of training across 3 days [48,49]. In the TEENS study, a subset of seventh grade students were elected by their classmates to serve as peer mentors [16]. Peer mentors completed a 1-day training and their roles as peers included assisting with interactive sessions during classroom activities that were part of the intervention [16]. Similar to the HealthCorps and FUEL interventions, exact hours of training were not noted for the TEENS or H2K interventions.
Trainings of peers in the Cool Girls, Inc., Go Girls!, Healthy Buddies, MBA, MOVE Project, Slice of Life, SnaX, and TACOS interventions were extensively less compared to the aforementioned interventions. Cool Girls, Inc. participants were eligible to become youth mentors after participating in the program for one year [36]. Details of training the participants who served as mentors was not discussed [36]. In the Go Girls! intervention, youth mentors underwent training with the local Big Brothers Big Sisters agency [40]. The youth mentors In the Healthy Buddies intervention received a 45-min lesson per week from an intervention teacher then subsequently taught the same lesson to their mentees [42]. Peer mentor participants in MBA project received a four-hour training session [46]. In the MOVE Project, youth mentors attended a weekly training session immediately prior to their mentoring session [47]. The training sessions provided information about physical activity, behavior techniques, and mentoring techniques [47]. Peer mentor training in the Slice of Life intervention took place over the course of three days for a total of 16 h. The peer mentors learned about the program and engaged in role playing activities of social situations [52]. Peer mentors in the sNaX intervention attended a meeting to learn how to distribute healthy snacks and healthy messaging giveaways. No other information regarding peer mentor training was discussed [52].
Based on the articles pertaining to the studies discussing TACOS and GAP, formal training to youth and peer mentors did not seem to be provided [15,38,39,53]. In the TACOS study, mentors involved in the student groups were charged with creating promotional activities. Mentors were then classified as either low-involvement (<5 h; n = 343) or high-involvement (>5 h; n = 54) [peer mentors] based on the number of hours they dedicated to these promotional activities [15]. However, no other information was provided regarding the promotional activities or what constituted the extent of the students’ involvement [53]. In the BHCK study, extent of and format of training was not disclosed [34].
3.3. Child and Adolescent Participant Outcomes
3.3.1. Biometric Outcomes
Various biometric outcomes were assessed for study participants in several of the interventions including BMI (prevalence of overweight and obesity), body composition, blood pressure, and heart rate. BMI and prevalence of overweight and obesity were assessed in Challenge!, Just for Kids!, HealthCorps, PAWS, MBA and Healthy Buddies. Positive impacts on weight status due to the intervention were demonstrated in project Challenge!, MBA, and the Just for Kids! study. There was a 5.3% decrease in overweight and obesity status among Challenge! participants and an 11.3% increase in overweight and obesity status among control participants (p = 0.02) [35]. In the Just for Kids! study, mean change in BMI-percentile from pre- to post-intervention was significant in the intervention group (t = −2.2; p = 0.03) but not for the control group (t = 0.330; p = 0.743) [44]. In MBA, reduction of BMI in intervention group was significant across follow up data collection [46]. However, in the HealthCorps, PAWS, and Healthy Buddies interventions, changes in BMI and prevalence of overweight or obesity did not differ significantly between the intervention and control groups [41,42].
Body composition was only assessed in three interventions—Challenge!, Mentoring to be Active, and HealthCorps. Findings from project Challenge! indicated that fat-free mass was significantly higher at 10- and 24-month follow-ups among intervention male participants compared to control male participants [35]. However, similar results were not observed for female participants. When stratified by weight status (overweight/obese vs. normal weight) significant improvements in fat percentile (p = 0.003), fat mass (p = 0.025), and fat-free mass (p = 0.0205) were observed in overweight/obese participants at the 24-month follow-up [35]. Compared to the teacher-led program in the MBA study, participants had more fat loss when program was led by peer mentors [46]. In the HealthCorps study, body fat percent did not differ significantly between the intervention and control groups [41].Two intervention studies, Healthy Buddies and H2K, assessed cardiovascular biometrics. Both the intervention and control groups from the Healthy Buddies study had increased systolic blood pressure post-intervention; however, the increase in the intervention group was significantly lower compared to the control group for both younger children and peer mentors (p = 0.025; p = 0.006) [42]. Changes in diastolic blood pressure and heart rate did not significantly differ between the intervention and control groups for the younger children [42]. In the H2K study, both male and female intervention participants demonstrated significantly higher VO2 max compared to control participants (p = 0.038; p = 0.001), meaning there was a significant gain in cardiovascular fitness among participants in peer mentoring schools [43].
3.3.2. Nutrition Outcomes
Nutrition Outcomes: Dietary Intake
Outcomes related to dietary intake varied greatly across all studies reviewed. Only the Challenge!, Slice of Life, BHCK, PAWS and TEENS studies conducted a full dietary assessment. The most common dietary components that were assessed included fruits and vegetables, high or low-fat food options, and sugar-sweetened beverages (SSB) [16,29,34,35,50,51,54,55].
Challenge! [35] participants and Cool Girls, Inc. [36] participants demonstrated no significant changes related to fruit and vegetable consumption. Similarly, Cawley et al. found no significant differences in fruits and greens consumption between intervention and control groups in the HealthCorps studies [41]. The Slice of Life intervention appeared to improve overall dietary intake for females yet only improved salt intake for males [51]. TEENS participants exposed to classroom and school environment interventions improved their intake of fruit by a quarter serving per day (p = 0.052), vegetables by a quarter serving per day (p = 0.097), and combined fruit and vegetables by a half serving per day (p = 0.056) with marginal significance [16]. Youth participants in the PAWS study reported an increase of whole grain intake immediately and six months after intervention [50].
Methods of assessing consumption of higher or lower fat food options also varied across studies. In the TEENS studies, intake of higher- or lower-fat food options was assessed using food choice scores. In the TEENS peer mentor sub-study, participants exposed to classroom and school environment interventions significantly improved their intake of lower fat food options (p < 0.001), while participants exposed to only the school environment intervention improved their intake of lower fat food options with marginal significance (p < 0.058) [16]. In the larger TEENS study, intervention dose response analyses were conducted. High-dose students demonstrated significantly higher food choice scores—greater intake of lower-fat food options—compared to low-dose and control students (p < 0.01) [54]. Thus, greater levels of exposure resulted in significantly higher food choice scores or greater intake of lower-fat foods. In the BHCK study, the intervention group purchased a higher amount of healthier options (fruits, vegetables, and low-fat foods) per week compared to control (p = 0.01) [44]. In project Challenge!, snack and dessert consumption decreased significantly among intervention participants compared to control participants at 10-month (p = 0.001) and 24-month (p = 0.089) follow-ups [35]. HealthCorps participants, however, did not demonstrate any significant differences in fast food consumption, which is considered a higher-fat food source [41]. A final method of assessing higher or lower fat food intake in these peer-led interventions was the use of sales data. In the TACOS study, percentage of sales of low-fat options increased significantly in the intervention schools compared to the control schools at year 1 and year 2 (p = 0.096; p = 0.042), suggesting that participants have increased their low-fat food intake [15].
Findings related to SSB intake were fairly consistent across studies. Compared to the control participants, HealthCorps intervention participants significantly decreased their SSB intake by 17.5% (p = 0.04) [41]. Intervention participants in the FUEL study demonstrated a significant (p < 0.02) decrease in SSB consumption that sustained for three months post-intervention, whereas control participants in the FUEL study significantly (p < 0.02) increased juice consumption post intervention and continued to significantly increase juice consumption three- and twelve-months post-intervention [37]. Finally, in the SNaX study, SSB intake decreased for the non-peer mentor groups from 33% to 26% (p = 0.06) [52].
Go Girls! participants reported dietary behaviors with a 17-item Adolescent Food Habits Checklist [40]. Participants demonstrated a significant improvement in dietary behaviors (p < 0.05) from baseline to post-intervention [40].
3.3.3. Physical Activity Outcomes
Physical Activity Outcomes: Physical Activity Behaviors
Physical activity was assessed by a variety of means including accelerometry, pedometers, fitness tests, and self-reported behaviors. The Challenge!, GAP, PLAN-A, and the MOVE Project studies utilized accelerometry technology. Among overweight or obese participants in project Challenge!, control participants partook in, on average, 25.5 min less physical activity daily than intervention participants (p = 0.018) at the 10-month follow-up time point, but no significant findings were seen at the 24-month follow-up time point [35]. In PLAN-A, accelerometry data showed that participants increased physical activity by 6 min compared to average compared to the control group [48,49]. The GAP study determined there was small significant difference of 2.4 min per day in mean physical activity from baseline [38,39]. No intervention effects were demonstrated with the MOVE Project accelerometry data [47].
The H2K participants reported step counts per day utilizing pedometer technology. Compared to participants at control schools, H2K participants at intervention schools logged significantly more steps per school day (p < 0.001) [43]. A significant difference was also demonstrated between gender; males logged significantly more steps per day than females (p < 0.05), regardless of treatment group [43].
For both the intervention and control groups in the Healthy Buddies study, distance covered during the 9-min run increased significantly (p < 0.001; p < 0.001); however, there was no significant difference demonstrated between treatment groups [42].
Self-reported physical activity behavior measures were utilized in the Cool Girls, Inc., Go Girls!, and HealthCorps, studies. Cool Girls, Inc. participants reported a significant increase in physical activity behavior scores (p < 0.05), however, there were no additional effects among participants who were mentored and those who were not [36]. Go Girls! participants reported physical activity behaviors with a 2-item physical activity questionnaire and a 2-item survey for leisure-time physical activity [40]. Participants demonstrated a significant improvement in leisure-time physical activity (p < 0.01) from baseline to post-intervention and significant improvements in total physical activity (p < 0.001) and leisure-time physical activity (p < 0.001) at the 7-week follow-up [40]. HealthCorps intervention participants compared to the control participants were 45% more likely to report an increase in physical activity (p = 0.05) [41].
3.4. Youth and Peer Mentors Outcomes
The above outcomes discussed referred only to the participants of the studies and not the mentors themselves. Less than half of the intervention studies assessed the youth mentors or peer mentors to some extent. Two of the intervention studies, Healthy Buddies and Just for Kids!, reported on the youth mentors, and three of the intervention studies, TACOS, TEENS, and SNaX reported on differences between non-peer mentor participants and peer mentor participants. Data on youth mentors in the Challenge! study were qualitatively assessed post hoc.
3.4.1. Biometric Outcomes
In the Just for Kids! study, youth mentor BMI-percentiles and blood pressure were assessed [45]. A marginally significant decrease in BMI was observed from baseline to post intervention (p < 0.06) [45]. Additionally, a medium effect size (ES = 0.56) for improved diastolic blood pressure among youth mentors was observed [45].
3.4.2. Nutrition Outcomes
In the Healthy Buddies intervention, health knowledge, behaviors, attitudes, and perceptions of body image were assessed. Significant improvements in knowledge, health behaviors, and attitudes were seen for youth mentors (p < 0.001; p < 0.001; p < 0.001) and differences between youth mentor intervention and control groups were greater among the intervention group (p < 0.001; p = 0.025; p = 0.045) [42]. No significant improvements were seen among the youth mentor group with regards to body image perceptions [42].
In the Just for Kids! study, lifestyle behaviors, including a subscale for dietary behaviors, were measured [45]. A medium effect size (ES = 0.57) for improvements in dietary behaviors was demonstrated [45].
Recall, that in the TACOS study, no formal peer mentor training occurred. Rather, students that highly participated in student group promotion were assessed as leaders among their peers. Low-involved participants reported that TACOS did not change the way they chose foods and did not influence them to eat more fruits and vegetables significantly more than high-involved participants (p < 0.001) [53]. High-involved participants reported that their involvement in TACOS resulted in eating more lower-fat foods and paying more attention to what they eat significantly more than low-involved participants (p < 0.001) [53]. In addition to eating behaviors, significant differences were seen among all attitude, social norms, student involvement, and experience questions when comparing high-involved participants to low-involved participants (p < 0.001 for all questions) [53].
In the TEENS peer mentor sub-study, the peer mentors significantly improved their intake of fruit by a half serving per day (p = 0.01), combined fruit and vegetables by one serving per day (p = 0.012), and lower fat food options (p < 0.001). They also improved their intake of vegetables by a half serving per day with marginal significance (p = 0.059) [16]. Regarding benefits of being a peer mentor, 85% of peer mentors reported that they learned more about healthy eating and more than 64% believed that they ate healthier because of being a peer mentor [55].
In the SNaX intervention, attitudes about the cafeteria significantly improved among peer mentors (p = 0.03) [52]. When comparing the change in attitudes about the cafeteria between the peer mentors and non-peer mentors, peer mentors attitudes significantly improved compared to non-peer mentors (p < 0.001) [52]. Additionally, SSB intake significantly decreased for peer mentors from 33% to 21% (p = 0.03) [52].
3.4.3. Physical Activity Outcomes
Physical activity outcomes among mentors was only measured in one study, the Just for Kids! Study. A significant improvement in physical activity behaviors (p < 0.04) was observed among youth mentors from baseline to post-intervention [45].
3.5. Process Evaluation
Process evaluation outcomes were only reported in four of the studies—FUEL, PLAN-A, Slice of Life, and TEENS. In the FUEL study, participants rated their satisfaction with the course content and delivery of the intervention on a 5-point Likert scale [54]. Overall, 77% of the participants would recommend the program to others, with significantly higher levels of satisfaction among participants in the intervention classrooms (p < 0.05) [54].
In the PLAN-A study, quantitative and qualitative measures were conducted across peer mentors, participants, teachers, parents, and intervention trainers [48,49]. Based on analysis of semi structured interviews, parents, peer-supporters, and teachers discussed an increase in the participants confidence [48,49].Training satisfaction of peer mentors was determined to be sufficient based on qualitative and quantitative measures [48,49].
Three questionnaires were used to evaluate satisfaction and perceived impact of the program in the Slice of Life study and all question responses were on a 5-point Likert scale [51]. Overall, females were more satisfied with the program (p < 0.01), believed that the program impacted their eating patterns (p < 0.001), enjoyed the use of university staff leading the program (p < 0.01) more compared to males [51]. Having peer mentors teach the program scored high and there was no significant difference in the enjoyment of peer mentors teaching the program between males and females [51]. However, females viewed the peer mentors as more able to lead group discussions (p = 0.01) and encourage participation (p = 0.01) compared to males [51].
A multicomponent process evaluation, including surveys of peer, student, and teacher perceptions of the peer mentors, implementation observation, and interviews with teachers, was conducted to assess the feasibility and acceptability of the TEENS peer mentor sub-study [55]. In terms of feasibility of the peer-led component of the TEENS sub-study, peer mentors actually led the classroom portion, which was the intervention intent, 94% of the time and were able to keep the students on task 77.5% of that time [55]. Ninety percent of the peer mentors in the TEENS sub-study stated that they enjoyed being peer mentors and 80% said they would be a peer mentor again, whereas 18% said that they would not be a peer mentor again [55]. These mentors were not probed as to why they would not want to be a peer mentor again. Among students who did not serve as peer mentors, almost 58% reported that the peer mentors were helpful [55]. Approximately 93% of teachers reported that the peer mentors were helpful or very helpful; however, one teacher reported that about 10% of the peer mentors did not take the role seriously [55]. In the teacher interviews, it was mentioned that the one-day training was too long for the kids [55]. However, no suggestions were made as to how the training could be modified for improved feasibility.
4. Discussion
Youth- and peer mentor-led interventions have been utilized among youth in a gamut of child development areas for over a quarter of a century. But it was not until the past decade or so that the use of peer and youth-led interventions for nutrition, physical activity, and child weight status research was implemented. Efforts to synthesize the findings from these nutrition and physical activity intervention studies has been minimal. This paper was the first to provide a review of peer- and youth-led interventions targeting children and adolescents to improve biometric-, nutrition-, physical activity, and psychosocial related outcomes for childhood overweight and obesity prevention across settings. The purpose of this study was to explore the training and implementation of youth and peers in nutrition and physical activity education interventions, evaluate the impact of the interventions on biometric-, nutrition-, physical-activity, and psychosocial related outcomes on children and adolescents receiving the interventions as well as the youth and peers leading the interventions, and to evaluate process outcomes of the interventions.
The training of the youth and peer mentors varied greatly for each intervention. Descriptions of the training processes were discussed extensively for the Challenge!, Just for Kids!, TEENS, and H2K interventions only [16,29,35,43,44,45,54,55]. If it could be determined that the intervention effects seen were due to the use of either youth or peer mentors, it would be incredibly difficult to replicate and improve generalizability of the findings. Future interventions that utilized or intend to utilize mentor model intervention strategies to improve biometric-, nutrition-, and physical activity-related outcomes should extensively detail implementation approaches, including training of mentors.
In general, both behavioral and psychosocial nutritional outcomes varied across the studies. Unfortunately, inconsistencies in findings across studies, especially regarding psychosocial factors, are common due to use of non-validated and variety of assessment tools. However, positive findings were seen for participants, youth mentors and peer mentors. The most consistent improvements were seen for increasing intake of lower-fat food options or decreasing intake of higher-fat food options, SSB intake, and nutritional knowledge.
Overall, the biometric findings were positive. Significant improvements in BMI and weight status were demonstrated in the Challenge!, MBA, and Just for Kids! studies, and significant improvements in body composition were seen in the Challenge! and HealthCorps studies [35,41,44,45]. The Challenge! and Just for Kids! interventions were two of the three studies with the most extensive youth mentor training, which could have contributed to the success of the intervention [29,35,44,45]. Given the short nature (12 and 8 weeks) of the interventions, these significant changes in biometrics speak to the incredible potential of these interventions, particularly if approaches that ensure programmatic sustainability is in place.
All studies that assessed physical activity outcomes demonstrated significant improvements in physical activity behaviors [35,42,43,47], and differences between intervention and control participants were only insignificant in one [42] of the studies. In the Challenge! study, physical activity data were derived from accelerometers that participants wore for at least nine days at a time. It is plausible that survey bias may have been playing a role, in that participants knew their physical activity was being recorded, so they consequently engaged in more physical activity than they would have otherwise [35]. In the Healthy Buddies intervention, step counts were calculated for the school day [42]. Thus, this measure was more of a validation of the intervention itself rather than an assessment of prolonged increases in physical activity. Future studies should explore innovative and effective ways to assess sustained physical activity in child and adolescent populations. Similar to the nutritional psychosocial outcomes, the results for physical activity psychosocial outcomes were mixed. However, improved self-efficacy for physical activity was consistent across those studies in which it was measured [40,44].
All the interventions were multi-component in nature. Examples of the components from these interventions include, but are not limited to, nutrition education, physical activity, marketing and promotion, and use of youth mentors or peer mentors. While the multi-component approach is essential to elicit behavior change [58,59,60], it makes it difficult to determine which component of the intervention resulted in the intervention effect, if one is detected. Only one study, the TEENS peer mentor sub-study, utilized a factorial design, to determine whether or not the innovative use of peer mentors was responsible for the intervention effect [16]. This study found that peer mentors increased their fruit and vegetable intake significantly. However, these changes were not compared to participants who received classroom and school environment intervention components or to participants who received only school environment intervention components. Additionally, several factorials were missing from this design, and effects of the peer-led intervention on participants that were mentored were not able to be determined. Therefore, future studies should utilize more rigorous factorial designs to determine whether the use of peers as mentors is an effective intervention component.
In all the interventions included in this review, methods of intervention were described as they were intended to be implemented. Whether or to what extent the interventions were implemented as planned is unknown. Two studies, PLAN-A and TEENS, provided implementation fidelity measures for the peer mentor component of the intervention. According to the authors of the article, high intervention feasibility was demonstrated [55]. Conducting process evaluations is essential to report feasibility and acceptability of the intervention, as well as implementation fidelity of the intervention. In addition to feasibility, acceptability, and fidelity, process evaluation outcomes provide insight to the sustainability of intervention strategies. Therefore, in conjunction with outcome evaluations, process evaluation measures should also be assessed in future youth-led nutrition and physical activity interventions.
4.1. Strengths and Limitations
Overall, positive findings were demonstrated for biometric-, nutrition-, and physical activity-related outcomes in the nineteen peer-led interventions reviewed for both participants and the peers themselves. The scoping nature of the review including the examination of the child and adolescent recipients of the interventions as well as the youth and peers that delivered the interventions, as well as the inclusion of diverse settings (e.g., school, community, etc.) is a major strength of the current study. Another major strength of the interventions reviewed in this paper was the rigor of study designs employed and the ability to interpret the findings. All the studies were either quasi-experimental, randomized controlled trials, or prospective and longitudinal in design. However, a major limitation was that the number of research studies that explored the impact on the youth and peers leading the interventions was small. Therefore, conclusions that can be drawn about the impact on the youth and peers leading the interventions themselves are limited. Additionally, a meta-analysis was not performed for the current systematic literature review. Finally, all studies included in this literature review had some or high risk for bias per the risk of bias assessment that was completed. However, prevailing reasons for these biases were realities of community-based social and behavioral interventions research, i.e., participants being aware of their treatment assignment.
4.2. Conclusions
Public health and nutrition professionals conducting future research engaging youth and peer mentors should utilize rigorous, factorial design to determine the impact of peers alone as an effective intervention strategy. Additionally, if youth and peer mentors are determined to be effective in improving diet and physical activity among children and adolescents, successful strategies for training and employing youth mentors and peer mentors must be understood. Finally, the impact of youth and peer mentor models on the youth and peer mentors themselves need to be more thoroughly investigated in nutrition and physical activity intervention research.
Author Contributions
Conceptualization, C.W.G. and L.C.H.; methodology, M.A.L., C.W.G. and L.C.H.; formal analysis, M.A.L., M.K., C.W.G. and L.C.H.; writing—original draft preparation, M.A.L., M.K., C.W.G. and L.C.H.; writing—review and editing, M.A.L., M.K., C.W.G. and L.C.H.; supervision, C.W.G. and L.C.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to no collection of primary data.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
Appendix A.1. B’more Healthy Communities for Kids (BHCK) [34]
The B’more Healthy Communities for Kids program was a group randomized control trial in 30 low-income areas in Baltimore, Maryland. Children aged 9–15 who were primarily African American participated in 14-h long sessions that occurred every other week for six months. Groups were divided into two based on age of 9–12 and 13–15 years old. College students of Baltimore City were selected to serve as youth mentors for the study and were trained by program leaders. Food and beverage intake and purchasing behavior habits were recorded pre- and post- intervention. The intervention aimed to improve overall health outcomes of youth by increasing access of alternatives to unhealthy choices at local stores as well as promote healthy eating choices through the youth-mentor intervention.
Appendix A.2. Challenge! [29,35]
Project Challenge! was a two-year randomized control trial for low-income, urban, adolescents aged 11–16 in Baltimore, MD to promote health and prevent overweight and obesity. Data on BMI, body composition, physical activity, and diet were collected on study participants pre- and post-intervention, as well as 10- and 24-months after the intervention. The project incorporated the use of college-aged students to serve as peer mentors to the study participants. The peer mentors engaged with the participants approximately once weekly for 12 weeks at the homes of the participants. Activities during this contact time included participatory education, physical activity, and dietary and physical activity goal setting.
Appendix A.3. Cool Girls, Inc. [36]
The Cool Girls, Inc. study utilized a convenience sample to produce a quasi-experimental design examining fruit and vegetable consumption and physical activity pre and post intervention in 175 female students aged 9 to 15 years compared to a control group. Intervention took place using youth mentors, who were Cool Girls, Inc. participants for less than one year. Youth mentors worked to improve frequency of healthy lifestyles of peers through a comprehensive life skills curriculum and participating in workshops and fieldtrips across a summer.
Appendix A.4. Fluids Used Effectively for Living (FUEL) [37]
The FUEL study was quasi-experimental in design consisting of four ninth grade classes, two intervention and two control, totaling 113 students from 3 high schools (one high school had intervention and control classes) in Saskatchewan, Canada. Data pertaining to beverage intake and attitudes were collected from the participants pre- and post-intervention, as well as three months after the intervention. The schools and classes from which participants were drawn were purposefully sampled. Intervention classes received six nutrition education lessons over a six-week period pertaining to beverage consumption from peer mentors and leaders in two educator models—multiple educators and a single educator. Students in the control classes self-taught the nutrition lessons.
Appendix A.5. Girls Active Project [38,39]
The Girls Active Project was a two-arm cluster randomized control in secondary state schools across the Midlands, United Kingdom. Girls currently attending the schools aged 11–14 years old were participants in the study, and fellow classmates who were considered to have leadership qualities were selected to be peer mentors. The goal of the program was to improve the intensity of physical activity in peers by increasing physical activity culture in the school setting. This includes increased opportunities to participate in physical activity. Body composition, psychosocial outcomes, and physical activity level data were taken at baseline, as well as seven and 14 months post-intervention.
Appendix A.6. HealthCorps [41]
The HealthCorps study, which took place in eleven high schools in New York City, was quasi-experimental design with 6 intervention schools and 5 control schools. The high schools were purposefully chosen. Diet, physical activity, health knowledge, BMI, and body fat percent data were collected from study participants pre- and post intervention. The intervention was delivered by peer mentors and consisted of classroom workshops, weekly seminars at lunch, office hours, and after-school group fitness activities.
Appendix A.7. Healthy Buddies [42]
The Healthy Buddies intervention was a quasi-experimental study in two elementary schools in British Columbia, Canada that included nutrition, physical activity, and body image education. Peer mentors taught the 30-min nutrition lessons to their kindergarten through third grade mentees. In addition to the lesson, the mentors and mentees engaged in 30 min of structured physical activity weekly. The schools that participated in the study were chosen based on their interest and support from the superintendent. Data from the study participants, as well as the peer mentors, pertaining to healthy living knowledge, behavior, and attitudes, fitness, BMI, blood pressure, and heart rate were collected pre- and post-intervention.
Appendix A.8. Heart Healthy Kids Program (H2K) [43]
The H2K intervention was a quasi-experimental study design with ten schools to improve obesity and cardiovascular disease outcomes among 4th–6th graders in Nova Scotia, Canada. The schools were selected based on expressed need and willingness to participate, and then matched based on size, demography, urbanity, and current physical activity programming. Fitness and physical activity data were collected on all participants, including peer mentors, pre- and post-intervention. However, comparisons between participants and peer mentor participants were not made. Control schools received a physical activity challenge and educational components, and intervention schools received an additional peer mentor component.
Appendix A.9. Just for Kids! [44,45]
Just for Kids! was a randomized control nutrition education trial for elementary school-aged children led by high school-aged, trained peer mentors in rural, Appalachian, OH. Several psychosocial factors were assessed including nutrition knowledge, as well as eating healthy and being active attitudes, self-efficacy, perceived autonomy support, and intentions. These constructs in addition to BMI were collected pre- and post-intervention. The Just for Kids! intervention consisted of nutrition education and structured physical activity one hour per week for eight weeks. Control participants were attention-controlled, thus they received education led by teens pertaining to non-nutritional topics such as hygiene, bike safety, and tobacco use.
Appendix A.10. Mentoring to Be Active (MBA) [46]
Mentoring to be Active was a group randomized control trial in twenty rural Appalachian high schools of southern Ohio that lasted for 10 weeks. Data was collected pre-and post- intervention, as well as follow up data taken at 3 and 6 months. BMI, weight, BMI percentile, and body fat percentage were gathered at all points of data collection in the study. Males and females aged 14–17 participated in a 10-lesson unit that involved completion of workbooks, homework, and setting of weekly goals. The peer mentors utilized in the study were juniors and seniors who participated in a four-hour paid training session. The peer mentors were assigned up to four adolescents to monitor progress and demonstrate healthy living.
Appendix A.11. Peer Education about Weight Steadiness [50]
Peer Education about Weight Steadiness was a 12-week cluster randomized control in 4 east central Illinois middle schools. Data on BMI, blood pressure, physical activity, dietary intake, and social cognitive understandings were collected at baseline, post-intervention, and six months after intervention. Children aged 11–14 participated in a 12-week afterschool course of 90-min sessions that involved increments of dedicated time to physical activity, cooking classes, goal setting, and discussions of healthy living. Peer mentors used from the eighth-grade class were selected based on teacher references and participated in twelve training sessions for mentors.
Appendix A.12. Peer-Led Physical Activity iNtervention for Adolescent Girls (PLAN-A) [48,49]
Peer-Led physical Activity iNtervention for Adolescent girls was a two-arm randomized control study in six secondary schools in southwest England. Year 8 girls aged 12–13 who were considered to be more physical active and identified as influential from their peers. Participants in the study included year 8 girls aged 12–13. The peer mentors were trained for 15 h over the span of 3 days and were given various training booklets and activities to complete. The goal of the intervention was to informally provide support to peers to encourage physical activity. Data on physical activity and psychosocial measures were recorded pre- and post- intervention, and 4–5 months after completion of the intervention program.
Appendix A.13. Slice of Life [51]
The Slice of Life intervention was a one group pre- and post-test pilot study, lasting one year, in a high school in Minneapolis, MN. Data were collected from all participants, including peer mentors, pertaining to dietary intake, healthy knowledge and awareness, self-reported exercise, and behavioral intentions. Comparisons were not made between study participants and peer mentor participants. The intervention included a 10-lesson nutrition and physical activity curriculum led by student-selected peer mentors approximately half of the time.
Appendix A.14. Students for Nutrition and Exercise (SNaX) [52]
SNaX was a five-week pilot intervention in two Los Angeles city schools that aimed to translate policy into action regarding obesity prevention strategies. The schools were neither randomly selected nor randomly assigned. Pre- and post-surveys were collected from participants, including the peer mentors, from the intervention schools pertaining to cafeteria attitudes and sales data were collected from both schools. Components of the intervention included selling more appealing produce (i.e., sliced fruit instead of whole fruit), marketing nutrition and health information, disseminating health information to students, and training peer mentors to engage in discussion with fellow students about food and nutrition.
Appendix A.15. Trying Alternative Cafeteria Options in Schools (TACOS) [15,53]
The TACOS study was a group randomized control trial of twenty high schools in suburban, St. Paul, MN. Student-reported food choices, perceptions of the food environment, and behavioral intentions data from participants were collected pre- and post-intervention. Additionally, sale of low-fat à la carte items were compared pre- and post-intervention. A post hoc analysis of students that were less involved and highly involved in the peer-led promotional activities was conducted to assess differences in outcomes based on peer involvement. The intervention aimed to improve the food environment at high schools by increasing the availability of low-fat à la carte options and promoting the low-fat options through peer student group activities.
Appendix A.16. Teens Eating for Energy and Nutrition at School (TEENS) [16,54,55]
The TEENS intervention was a group randomized control trial in sixteen schools in St. Paul and Minneapolis, MN aiming to improve intakes of fruits, vegetables, and lower-fat food options among 7th and 8th graders. Fruit and vegetable intake, as well as data from usual food choice surveys were collected from all participants, including peer mentors, pre- and post-intervention. The TEENS intervention included educating through ten nutrition lessons, engaging families through parent packets, increasing availability of lower-fat options in school cafeterias, and developing, in 75% of intervention schools, Student Nutrition Advisory Councils (SNACs) comprised of teachers, staff, parents, and students aiming to improve the food environment at schools through policy changes.
Appendix A.17. The WISH Study [56]
The WISH Study was a 12-week randomized control trial used in six post primary schools in Northern Ireland in aged 11–13 girls to promote an increase of physical activity using youth mentors. Students from the same school in higher academic levels, aged 15–17, were selected to be the youth mentors. Data on physical activity, BMI, cardiorespiratory fitness, and psychosocial methods were collected pre- and post- intervention, as well as six months after the program had ended. Youth mentors would participate in daily walks with the participants for 10–15 min across the 12-week period.
References
- World Health Organization. Obesity and Overweight; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of Childhood and Adult Obesity in the United States, 2011–2012. J. Am. Med. Assoc. 2014, 311, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Bryan, S.; Afful, J.; Carroll, M.; Te-Ching, C.; Orlando, D.; Fink, S.; Fryar, C. NHSR 158. National Health and Nutrition Examination Survey 2017–March 2020 Pre-pandemic Data Files; NHSR: Hyattsville, MD, USA, 2021. [CrossRef]
- Halfon, N.; Larson, K.; Slusser, W. Associations Between Obesity and Comorbid Mental Health, Developmental, and Physical Health Conditions in a Nationally Representative Sample of US Children Aged 10 to 17. Acad. Pediatr. 2013, 13, 6–13. [Google Scholar] [CrossRef] [PubMed]
- Taras, H.; Potts-Datema, W. Obesity and Student Performance at School. J. Sch. Health 2005, 75, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Ashcroft, J.; Semmler, C.; Carnell, S.; Van Jaarsveld, C.H.; Wardle, J. Continuity and stability of eating behaviour traits in children. Eur. J. Clin. Nutr. 2008, 62, 985–990. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.D.; Fu, E.; Kobayashi, M.A. Prevention and Management of Childhood Obesity and Its Psychological and Health Comorbidities. Annu. Rev. Clin. Psychol. 2020, 16, 351–378. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations of Thought and Action: A Social Cognitive Theory; Prentice Hall: Engelwood, NJ, USA, 1986. [Google Scholar]
- Bandura, A. Social Learning Theory; Prentice Hall: Engelwood, NJ, USA, 1977. [Google Scholar]
- McGuire, W.J. Inducing Resistance to Persuasion: Some Contemporary Approaches; Elesiver: Amsterdam, The Netherlands, 1964; pp. 191–212. [Google Scholar] [CrossRef]
- Baric, L.; Harrison, A. Social Pressure and Health Education. J. Inst. Health Educ. 1977, 15, 12–18. [Google Scholar] [CrossRef]
- Lindsey, B.J. Peer Education: A Viewpoint and Critique. J. Am. Coll. Health 1997, 45, 187–189. [Google Scholar] [CrossRef]
- Mellanby, A.R.; Rees, J.B.; Tripp, J.H. Peer-led and adult-led school health education: A critical review of available comparative research. Health Educ. Res. 2000, 15, 533–545. [Google Scholar] [CrossRef]
- Perry, C.; Kelder, S.; Komro, K. The Social World of Adolescents: Families, Peers, School, and the Community. In Promoting the Health of Adolescents: New Directions for the Twenty-First Century; Millstein, S., Petersen, A., Nightingale, E., Eds.; Oxford University Press, Inc.: New York, NY, USA, 1993; pp. 73–96. [Google Scholar]
- French, S.A.; Story, M.; Fulkerson, J.A.; Hannan, P. An Environmental Intervention to Promote Lower-Fat Food Choices in Secondary Schools: Outcomes of the TACOS Study. Am. J. Public Health 2004, 94, 1507–1512. [Google Scholar] [CrossRef]
- Birnbaum, A.S.; Lytle, L.A.; Story, M.; Perry, C.L.; Murray, D.M. Are Differences in Exposure to a Multicomponent School-Based Intervention Associated with Varying Dietary Outcomes in Adolescents? Health Educ. Behav. 2002, 29, 427–443. [Google Scholar] [CrossRef]
- Black, D.R.; Tobler, N.S.; Sciacca, J.P. Peer helping/involvement: An efficacious way to meet the challenge of reducing alcohol, tobacco, and other drug use among youth? J. Sch. Health 1998, 68, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Fors, S.W.; Jarvis, S. Evaluation of a Peer-Led Drug Abuse Risk Reduction Project for Runaway/Homeless Youths. J. Drug Educ. 1995, 25, 321–333. [Google Scholar] [CrossRef] [PubMed]
- Klepp, K.-I.; Halper, A.; Perry, C.L. The Efficacy of Peer Leaders in Drug Abuse Prevention. J. Sch. Health 1986, 56, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Komro, K.A.; Perry, C.L.; Murray, D.M.; Veblen-Mortenson, S.; Williams, C.L.; Anstine, P.S. Peer-Planned Social Activities for Preventing Alcohol Use among Young Adolescents. J. Sch. Health 1996, 66, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Orpinas, P.; Parcel, G.S.; Mcalister, A.; Frankowski, R. Violence prevention in middle schools: A pilot evaluation. J. Adolesc. Health 1995, 17, 360–371. [Google Scholar] [CrossRef] [PubMed]
- Perry, C.L. Prevention of Alcohol Use and Abuse in Adolescence: Teacher- vs Peer-led Intervention. Crisis 1989, 10, 52–61. [Google Scholar]
- Sawyer, R.G.; Pinciaro, P.; Bedwell, D. How Peer Education Changed Peer Sexuality Educators’ Self-Esteem, Personal Development, and Sexual Behavior. J. Am. Coll. Health 1997, 45, 211–217. [Google Scholar] [CrossRef]
- Beier, S.R.; Rosenfeld, W.D.; Spitalny, K.C.; Zansky, S.M.; Bontempo, A.N. The Potential Role of an Adult Mentor in Influencing High-Risk Behaviors in Adolescents. Arch. Pediatr. Adolesc. Med. 2000, 154, 327–331. [Google Scholar] [CrossRef]
- Zimmerman, M.A.; Bingenheimer, J.B.; Notaro, P.C. Natural Mentors and Adolescent Resiliency: A Study with Urban Youth. Am. J. Community Psychol. 2002, 30, 221–243. [Google Scholar] [CrossRef]
- DuBois, D.L.; Silverthorn, N. Natural Mentoring Relationships and Adolescent Health: Evidence from a National Study. Am. J. Public Health 2005, 95, 518–524. [Google Scholar] [CrossRef]
- Klaw, E.L.; Rhodes, J.E. Mentor Relationships and the Career Development of Pregnant and Parenting African-American Teenagers. Psychol. Women Q. 1995, 19, 551–562. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, J.E.; Grossman, J.B.; Resch, N.L. Agents of change: Pathways through which mentoring relationships influence adolescents’ academic adjustment. Child Dev. 2000, 71, 1662–1671. [Google Scholar] [CrossRef] [PubMed]
- Black, M.M.; Arteaga, S.S.; Sanders, J.; Hager, E.R.; Anliker, J.A.; Gittelsohn, J.; Wang, Y. College Mentors. Health Promot. Pract. 2010, 13, 238–244. [Google Scholar] [CrossRef] [PubMed]
- McHale, F.; Ng, K.; Taylor, S.; Bengoechea, E.; Norton, C.; O’shea, D.; Woods, C. A Systematic Literature Review of Peer-led Strategies for Promoting Physical Activity Levels of Adolescents. Health Educ. Behav. 2021, 49, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Yip, C.; Gates, M.; Gates, A.; Hanning, R.M. Peer-led nutrition education programs for school-aged youth: A systematic review of the literature. Health Educ. Res. 2015, 31, cyv063. [Google Scholar] [CrossRef] [PubMed]
- Rhodes, J.E. Improving Youth Mentoring Interventions Through Research-based Practice. Am. J. Community Psychol. 2008, 41, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Liberati, M.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Trude, A.C.B.; Surkan, P.J.; Cheskin, L.J.; Gittelsohn, J. A multilevel, multicomponent childhood obesity prevention group-randomized controlled trial improves healthier food purchasing and reduces sweet-snack consumption among low-income African-American youth. Nutr. J. 2018, 17, 96. [Google Scholar] [CrossRef]
- Black, M.M.; Hager, E.R.; Le, K.; Anliker, J.; Arteaga, S.S.; DiClemente, C.; Gittelsohn, J.; Magder, L.; Papas, M.; Snitker, S.; et al. Challenge! Health Promotion/Obesity Prevention Mentorship Model among Urban, Black Adolescents. Pediatrics 2010, 126, 280–288. [Google Scholar] [CrossRef]
- Kuperminc, G.P.; Thomason, J.; DiMeo, M.; Broomfield-Massey, K. Cool Girls, Inc.: Promoting the Positive Development of Urban Preadolescent and Early Adolescent Girls. J. Prim. Prev. 2011, 32, 171–183. [Google Scholar] [CrossRef]
- Lo, E.; Coles, R.; Humbert, M.L.; Polowski, J.; Henry, C.J.; Whiting, S.J. Beverage intake improvement by high school students in Saskatchewan, Canada. Nutr. Res. 2008, 28, 144–150. [Google Scholar] [CrossRef] [PubMed]
- McQuinn, S.; Belton, S.; Staines, A.; Sweeney, M.R. Co-design of a school-based physical activity intervention for adolescent females in a disadvantaged community: Insights from the Girls Active Project (GAP). BMC Public Health 2022, 22, 615. [Google Scholar] [CrossRef] [PubMed]
- Harrington, D.M.; Davies, M.J.; Bodicoat, D.; Charles, J.M.; Chudasama, Y.V.; Gorely, T.; Khunti, K.; Rowlands, A.V.; Sherar, L.B.; Tudor-Edwards, R.; et al. A school-based intervention (‘Girls Active’) to increase physical activity levels among 11- to 14-year-old girls: Cluster RCT. Public Health Res. 2019, 7, 1–162. [Google Scholar] [CrossRef]
- Dowd, A.J.; Chen, M.Y.; Jung, M.E.; Beauchamp, M.R. “Go Girls!”: Psychological and behavioral outcomes associated with a group-based healthy lifestyle program for adolescent girls. Transl. Behav. Med. 2014, 5, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Cawley, J.; Cisek-Gillman, L.; Roberts, R.; Cocotas, C.; Smith-Cook, T.; Bouchard, M.; Oz, M. Effect of HealthCorps, a High School Peer Mentoring Program, on Youth Diet and Physical Activity. Child. Obes. 2011, 7, 364–371. [Google Scholar] [CrossRef]
- Stock, S.; Miranda, C.; Evans, S.; Plessis, S.; Ridley, J.; Yeh, S.; Chanoine, J.-P. Healthy Buddies: A Novel, Peer-Led Health Promotion Program for the Prevention of Obesity and Eating Disorders in Children in Elementary School. Pediatrics 2007, 120, e1059–e1068. [Google Scholar] [CrossRef]
- Spencer, R.; Bower, J.; Kirk, S.; Friesen, C.H. Peer Mentoring Is Associated with Positive Change in Physical Activity and Aerobic Fitness of Grades 4, 5, and 6 Students in the Heart Healthy Kids Program. Health Promot. Pract. 2014, 15, 803–811. [Google Scholar] [CrossRef]
- Smith, L.H. Piloting the use of teen mentors to promote a healthy diet and physical activity among children in Appalachia. J. Spéc. Pediatr. Nurs. 2011, 16, 16–26. [Google Scholar] [CrossRef]
- Smith, L.H.; Holloman, C. Comparing the Effects of Teen Mentors to Adult Teachers on Child Lifestyle Behaviors and Health Outcomes in Appalachia. J. Sch. Nurs. 2013, 29, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.H.; Petosa, R.L.; Laurent, D. Efficacy of “Mentoring to Be Active” on Weight Loss, Body Mass Index, and Body Fat among Obese and Extremely Obese Youth in Rural Appalachia. J. Rural. Health 2019, 36, 77–87. [Google Scholar] [CrossRef]
- Tymms, P.B.; Curtis, S.E.; Routen, A.; Thomson, K.H.; Bolden, D.; Bock, S.C.; Dunn, C.E.; Cooper, A.; Elliott, J.G.; Moore, H.; et al. Clustered randomised controlled trial of two education interventions designed to increase physical activity and well-being of secondary school students: The MOVE Project. BMJ Open 2016, 6, e009318. [Google Scholar] [CrossRef] [PubMed]
- Sebire, S.J.; Banfield, K.; Jago, R.; Edwards, M.J.; Campbell, R.; Kipping, R.; Blair, P.S.; Kadir, B.; Garfield, K.; Matthews, J.; et al. A process evaluation of the PLAN-A intervention (Peer-Led physical Activity iNtervention for Adolescent girls). BMC Public Health 2019, 19, 1203. [Google Scholar] [CrossRef] [PubMed]
- Sebire, S.J.; Jago, R.; Banfield, K.; Edwards, M.J.; Campbell, R.; Kipping, R.; Blair, P.S.; Kadir, B.; Garfield, K.; Matthews, J.; et al. Results of a feasibility cluster randomised controlled trial of a peer-led school-based intervention to increase the physical activity of adolescent girls (PLAN-A). Int. J. Behav. Nutr. Phys. Act. 2018, 15, 50. [Google Scholar] [CrossRef] [PubMed]
- Muzaffar, H.; Nikolaus, C.J.; Ogolsky, B.G.; Lane, A.; Liguori, C.; Nickols-Richardson, S.M. Promoting Cooking, Nutrition, and Physical Activity in Afterschool Settings. Am. J. Health Behav. 2019, 43, 1050–1063. [Google Scholar] [CrossRef]
- Perry, C.; Klepp, K.-I.; Halper, A.; Dudovitz, B.; Smyth, M.; Golden, D.; Griffin, G. Promoting healthy eating and physical activity patterns among adolescents: A pilot study of ‘Slice of Life’. Health Educ. Res. 1987, 2, 93–103. [Google Scholar] [CrossRef]
- Bogart, L.M.; Elliott, M.N.; Uyeda, K.; Hawes-Dawson, J.; Klein, D.J.; Schuster, M.A. Preliminary Healthy Eating Outcomes of SNaX, a Pilot Community-Based Intervention for Adolescents. J. Adolesc. Health 2011, 48, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Hamdan, S.; Story, M.; French, S.A.; Fulkerson, J.A.; Nelson, H. Perceptions of adolescents involved in promoting lower-fat foods in schools: Associations with level of involvement. J. Am. Diet. Assoc. 2005, 105, 247–251. [Google Scholar] [CrossRef]
- Lytle, L.A.; Murray, D.; Perry, C.L.; Story, M.; Birnbaum, A.S.; Kubik, M.Y.; Varnell, S. School-Based Approaches to Affect Adolescents’ Diets: Results from the TEENS Study. Health Educ. Behav. 2004, 31, 270–287. [Google Scholar] [CrossRef]
- Story, M.; Lytle, L.A.; Birnbaum, A.S.; Perry, C.L. Peer-led, school-based nutrition education for young adolescents: Feasibility and process evaluation of the TEENS study. J. Sch. Health 2002, 72, 121–127. [Google Scholar] [CrossRef]
- Carlin, A.; Murphy, M.H.; Nevill, A.; Gallagher, A.M. Effects of a peer-led Walking In ScHools intervention (the WISH study) on physical activity levels of adolescent girls: A cluster randomised pilot study. Trials 2018, 19, 31. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Danielli, S.; Coffey, T.; Ashrafian, H.; Darzi, A. Systematic Review into City Interventions to Address Obesity. EClinicalMedicine 2021, 32, 100710. [Google Scholar] [CrossRef] [PubMed]
- Elvsaas, I.K.Ø.; Giske, L.; Fure, B.; Juvet, L.K. Multicomponent Lifestyle Interventions for Treating Overweight and Obesity in Children and Adolescents: A Systematic Review and Meta-Analyses. J. Obes. 2017, 2017, 5021902. [Google Scholar] [CrossRef] [PubMed]
- Mikkelsen, B.E.; Novotny, R.; Gittelsohn, J. Multi-Level, Multi-Component Approaches to Community Based Interventions for Healthy Living—A Three Case Comparison. Int. J. Environ. Res. Public Health 2016, 13, 1023. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).