Healthcare Burden Associated with Malnutrition Diagnoses in Hospitalized Children with Critical Illnesses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Population
2.2. Measures and Comparisons
2.3. Statistical Analyses
3. Results
3.1. Patient Demographics
3.2. Illness Severity
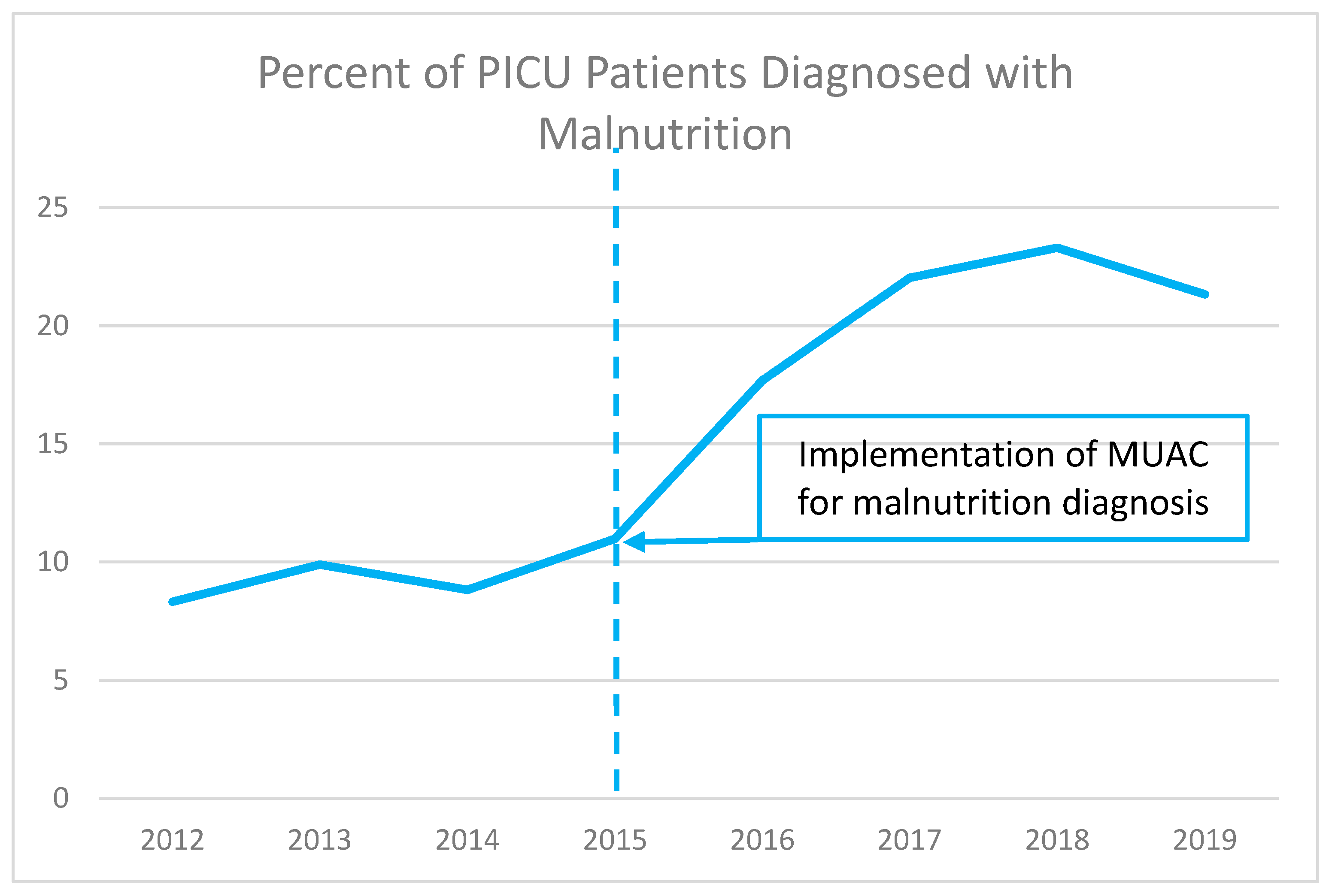
3.3. Identifying Malnutrition Risk by Use of Mid-Upper-Arm Circumference (MUAC) Measure
3.4. Impact of Malnutrition on Healthcare Use and Costs of Care
3.5. Regression Analysis of Factors Affecting Patient Length of Stay
4. Discussion
4.1. Overview of Findings
4.2. Pediatric Nutrition Screening and Assessment in Perspective
4.3. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Society of Critical Care Medicine. Critical Care Statistics. Society of Critical Care Medicine (SCCM). Available online: https://www.sccm.org/Communications/Critical-Care-Statistics (accessed on 8 August 2022).
- Sun, J.W.; Bourgeois, F.T.; Haneuse, S.; Hernández-Díaz, S.; E Landon, J.; Bateman, B.T.; Huybrechts, K.F. Development and Validation of a Pediatric Comorbidity Index. Am. J. Epidemiol. 2021, 190, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Killien, E.; Hartman, M.; Watson, R. Epidemiology of intensive care admissions in children in the United States, 2010 and 2015. Pediatr. Crit. Care Med. 2021, 22, 34. [Google Scholar] [CrossRef]
- DiPasquale, V.; Cucinotta, U.; Romano, C. Acute Malnutrition in Children: Pathophysiology, Clinical Effects and Treatment. Nutrients 2020, 12, 2413. [Google Scholar] [CrossRef] [PubMed]
- Romano, C.; Dipasquale, V.; Gottrand, F.; Sullivan, P.B. Gastrointestinal and nutritional issues in children with neurological dis-ability. Dev. Med. Child Neurol. 2018, 60, 892–896. [Google Scholar] [CrossRef] [Green Version]
- USDA Economic Research Service. Food Security Status of US Households in 2020. US Department of Agriculture. Published 2022. Updated 22 April 2022. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/key-statistics-graphics/#foodsecure (accessed on 8 August 2022).
- Walson, J.L.; Berkley, J.A. The impact of malnutrition on childhood infections. Curr. Opin. Infect. Dis. 2018, 31, 231–236. [Google Scholar] [CrossRef]
- WHO. Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: A Joint Statement by the World Health Organization and the United Nations Children’s Fund; World Health Organization: Geneva, Switzerland, 2009. Available online: https://www.ncbi.nlm.nih.gov/books/NBK200775/ (accessed on 8 August 2022).
- Becker, P.J.; Nieman Carney, L.; Corkins, M.R.; Monczka, J.; Smith, E.; Smith, S.E.; Spear, B.A.; White, J.V. Consensus Statement of the Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition: Indicators Recommended for the Identification and Documentation of Pediatric Malnutrition (Undernutrition). J. Acad. Nutr. Diet. 2014, 114, 1988–2000. [Google Scholar] [CrossRef] [PubMed]
- Moore, B.J.; White, S.; Washington, R.; Coenen, N.; Elixhauser, A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: The AHRQ Elixhauser Comorbidity Index. Med. Care 2017, 55, 698–705. [Google Scholar] [CrossRef]
- Hsu, B.S.; Brazelton, T.B., 3rd. A Comparison of Costs Between Medical and Surgical Patients in an Academic Pediatric Intensive Care Unit. WMJ 2015, 114, 236–239. [Google Scholar]
- U.S. Bureau of Labor Statistics. Consumer Price Index. Division of Consumer Prices and Price Indexes. Published 2023. Available online: https://www.bls.gov/cpi/ (accessed on 18 March 2023).
- Daskalou, E.; Galli-Tsinopoulou, A.; Karagiozoglou-Lampoudi, T.; Augoustides-Savvopoulou, P. Malnutrition in Hospitalized Pediatric Patients: Assessment, Prevalence, and Association to Adverse Outcomes. J. Am. Coll. Nutr. 2016, 35, 372–380. [Google Scholar] [CrossRef]
- Ehwerhemuepha, L.; Bendig, D.; Steele, C.; Rakovski, C.; Feaster, W. The Effect of Malnutrition on the Risk of Unplanned 7-Day Readmission in Pediatrics. Hosp. Pediatr. 2018, 8, 207–213. [Google Scholar] [CrossRef] [Green Version]
- Pelizzo, G.; Calcaterra, V.; Acierno, C.; Cena, H. Malnutrition and associated risk factors among disabled children. Special con-siderations in the pediatric surgical “fragile” patients. Front. Pediatr. 2019, 7, 86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yilmaz Ferhatoglu, S.; Yurdakok, O.; Yurtseven, N. Malnutrition on admission to the paediatric cardiac intensive care unit in-creases the risk of mortality and adverse outcomes following paediatric congenital heart surgery: A prospective cohort study. Aust. Crit. Care 2021, 35, 550–556. [Google Scholar] [CrossRef]
- Abdelhadi, R.A.; Bouma, S.; Bairdain, S.; Wolff, J.; Legro, A.; Plogsted, S.; Guenter, P.; Resnick, H.; Slaughter-Acey, J.C.; Corkins, M.R.; et al. Characteristics of hospitalized children with a diagnosis of malnutrition: United States, 2010. JPEN J. Parenter. Enter. Nutr. 2016, 40, 623–635. [Google Scholar] [CrossRef]
- Bagri, N.K.; Jose, B.; Shah, S.K.; Bhutia, T.D.; Kabra, S.K.; Lodha, R. Impact of Malnutrition on the Outcome of Critically Ill Children. Indian J. Pediatr. 2015, 82, 601–605. [Google Scholar] [CrossRef] [PubMed]
- Correia, M. Nutrition screening vs nutrition assessment: What′s the difference? Nutr. Clin. Pract. 2018, 33, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Murray, R.D.; Kerr, K.W.; Brunton, C.; Williams, J.A.; DeWitt, T.; Wulf, K.L. A First Step Towards Eliminating Malnutrition: A Proposal for Universal Nutrition Screening in Pediatric Practice. Nutr. Diet. Suppl. 2021, 13, 17–24. [Google Scholar] [CrossRef]
- Joosten, K.F.; Hulst, J.M. Prevalence of malnutrition in pediatric hospital patients. Curr. Opin. Pediatr. 2008, 20, 590–596. [Google Scholar] [CrossRef]
- Klanjsek, P.; Pajnkihar, M.; Marcun Varda, N.; Povalej Brzan, P. Screening and assessment tools for early detection of malnutri-tion in hospitalised children: A systematic review of validation studies. BMJ Open 2019, 9, e025444. [Google Scholar] [CrossRef] [Green Version]
- Hulst, J.M.; Huysentruyt, K.; Joosten, K.F. Pediatric screening tools for malnutrition: An update. Curr. Opin. Clin. Nutr. Metab. Care 2020, 23, 203–209. [Google Scholar] [CrossRef]
- Becker, P.J.; Bellini, S.G.; Vega, M.W.; Corkins, M.R.; Spear, B.A.; Spoede, E.; Hoy, M.K.; Piemonte, T.A.; Rozga, M. Validity and Reliability of Pediatric Nutrition Screening Tools for Hospital, Outpatient, and Community Settings: A 2018 Evidence Analysis Center Systematic Review. J. Acad. Nutr. Diet. 2020, 120, 288–318.e2. [Google Scholar] [CrossRef]
- Carter, L.; Shoyele, G.; Southon, S.; Farmer, A.; Persad, R.; Mazurak, V.C.; BrunetWood, M.K. Screening for pediatric malnutrition at hospital admission: Which screening tool is best? Nutr. Clin. Pract. 2020, 35, 951–958. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- White, M.; Lawson, K.; Ramsey, R.; Dennis, N.; Hutchinson, Z.; Soh, X.Y.; Matsuyama, M.; Doolan, A.; Todd, A.; Elliott, A.; et al. Simple Nutrition Screening Tool for Pediatric Inpatients. J. Parenter. Enter. Nutr. 2016, 40, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Lambebo, A.; Mezemir, Y.; Tamiru, D.; Belachew, T. Validating the diagnostic performance of MUAC in screening moderate acute malnutrition and developing an optimal cut-off for under five children of different regions in Ethiopia. PLoS ONE 2022, 17, e0273634. [Google Scholar] [CrossRef] [PubMed]
- Matilla-Hernandez, L.C.; Nino-Bautista, L.; Prieto-Pinilla, E.E.; Galvis-Padilla, D.C.; Bueno-Perez, I. Validating mid-upper arm cir-cumference (MUAC measurement for detecting acute malnutrition in 6-59 month-old children in emergency and disaster situations. Rev. Salud Publica 2014, 16, 1950207. [Google Scholar]
- Haque, M.A.; Choudhury, N.; Ahmed, S.M.T.; Farzana, F.D.; Ali, M.; Naz, F.; Raihan, M.J.; Rahman, S.S.; Siddiqua, T.J.; Faruque, A.S.G.; et al. Does a child’s mid-upper arm circumference-for-age z-score represent another nutritional indicator of childhood malnutrition status? Matern. Child Nutr. 2022, 18, e13404. [Google Scholar] [CrossRef]
- Stephens, K.; Escobar, A.; Jennison, E.N.; Vaughn, L.; Sullivan, R.; Abdel-Rahman, S.; on behalf of the CMH Nutrition Services Z-Score Research Team. Evaluating Mid-Upper Arm Circumference Z-Score as a Determinant of Nutrition Status. Nutr. Clin. Pr. 2018, 33, 124–132. [Google Scholar] [CrossRef]
- Chou, J.H.; Roumiantsev, S.; Singh, R. PediTools Electronic Growth Chart Calculators: Applications in Clinical Care, Research, and Quality Improvement. J. Med. Internet Res. 2020, 22, e16204. [Google Scholar] [CrossRef]
- Vella, V.; Tomkins, A.; Ndiku, J.; Marshal, T.; Cortinovis, I. Anthropometry as a predictor for mortality among Ugandan children, allowing for socio-economic variables. Eur. J. Clin. Nutr. 1994, 48, 189–197. [Google Scholar]
- Rasmussen, J.; Andersen, A.; Fisker, A.B.; Ravn, H.; Sodemann, M.; Rodrigues, A.; Benn, C.S.; Aaby, P. Mid-upper-arm-circumference and mid-upper-arm circumference z-score: The best predictor of mortality? Eur. J. Clin. Nutr. 2012, 66, 998–1003. [Google Scholar] [CrossRef] [Green Version]
- Taneja, S.; Rongsen-Chandola, T.; Mohan, S.B.; Mazumder, S.; Bhandari, N.; Kaur, J.; Arya, N.; Chowdhury, R.; Martines, J.C.; Bahl, R.; et al. Mid upper arm circumference as a predictor of risk of mortality in children in a low resource setting in India. PLoS ONE 2018, 13, e0197832. [Google Scholar] [CrossRef]
- O’brien, K.S.; Amza, A.; Kadri, B.; Nassirou, B.; Cotter, S.Y.; Stoller, N.E.; West, S.K.; Bailey, R.L.; Porco, T.C.; Keenan, J.D.; et al. Comparison of anthropometric indicators to predict mortality in a population-based prospective study of children under 5 years in Niger. Public Health Nutr. 2020, 23, 538–543. [Google Scholar] [CrossRef] [PubMed]
- Lakdawalla, D.N.; Mascarenhas, M.; Jena, A.B.; Vanderpuye-Orgle, J.; Lavallee, C.; Linthicum, M.T.; Snider, J.T. Impact of Oral Nutrition Supplements on Hospital Outcomes in Pediatric Patients. J. Parenter. Enter. Nutr. 2014, 38 (Suppl. S2), 42S–49S. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.L.; Stein, A.D. The Impact of Nutritional Interventions beyond the First 2 Years of Life on Linear Growth: A Systematic Review and Meta-Analysis. Adv. Nutr. 2017, 8, 323–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, R.; Wolf, S.; Alkazemi, M.H.; Pomann, G.-M.; Purves, J.T.; Wiener, J.S.; Routh, J.C. The evaluation of three comorbidity indices in predicting postoperative complications and readmissions in pediatric urology. J. Pediatr. Urol. 2018, 14, 244.e1–244.e7. [Google Scholar] [CrossRef] [PubMed]
| Variable | |
|---|---|
| Age (years), Median (IQR) | 5 (1–12) |
| Male, % of total | 52% |
| White, % of total | 75.8% |
| Black, % of total | 17.1% |
| Asia/Pacific Islander, % of total | 6.4% |
| Other, % of total | 0.7% |
| Variable | With Malnutrition Diagnosis (n = 783) | No Malnutrition Diagnosis (n = 3323) | p-Value |
|---|---|---|---|
| Age, Median (IQR) | 3 (0–12) | 5 (1–12) | <0.01 |
| Male, n (%) | 435 (55.6%) | 1700 (51.2%) | 0.03 |
| White, n (%) | 581 (74.2%) | 2532 (76.2%) | 0.23 |
| Black, n (%) | 134 (17.1%) | 568 (17.1%) | |
| Asia/Pacific Islander, n (%) | 63 (8.1%) | 201 (6.1%) | |
| Other, n (%) | 5 (0.6%) | 22 (0.7%) |
| With Malnutrition Diagnosis (CDM) n = 783 | No Malnutrition Diagnosis n = 3323 | p-Value | |
|---|---|---|---|
| Secondary diagnoses, Mean (S.D.) | 13 (8–18) | 6 (3–11) | <0.01 |
| Elixhauser readmission risk index, Median (IQR) | 0 (0–4) | 0 (0–4) | <0.01 |
| Elixhauser mortality risk index, Median (IQR) | 0 (0–2) | 0 (0–2) | <0.01 |
| With Malnutrition Diagnosis (CDM) n = 783 | No Malnutrition Diagnosis n = 3323 | p-Value | |
|---|---|---|---|
| Length of stay (days), Median (IQR) | 13 (6–28) | 5 (3–10) | <0.01 |
| 30-day readmission (occurrence), Mean (S.D.) | 0.10 (0.29) | 0.07 (0.26) | 0.03 |
| Before Matching | After Matching | |||||
|---|---|---|---|---|---|---|
| Pre-2015 Patients (n = 304) | Post-2015 Patients (n = 3802) | p-Value | Pre-2015 Patients (n = 304) | Post-2015 Patients (n = 304) | p-Value | |
| Asia/Pacific Islander, % | 5.6% | 6.5% | 0.32 | 5.6% | 5.6% | 0.95 |
| Black, % | 13.8% | 17.4% | 13.8% | 13.8% | ||
| White, % | 80.6% | 75.4% | 80.6% | 80.6% | ||
| Other races, % | 0% | 0.7% | 0% | 0% | ||
| Male, % | 50.0% | 52.2% | 0.47 | 50.0% | 50.0% | 0.99 |
| Female, % | 50.0% | 47.8% | 50.0% | 50.0% | ||
| Age, Mean (S.D.) | 4.95 (4.29) | 6.89 (6.22) | <0.01 | 4.95 (4.29) | 5.03 (4.53) | 0.83 |
| Elixhauser Readmission Index, Mean (S.D.) | 1.50 (2.39) | 1.77 (3.12) | 0.06 | 1.50 (2.39) | 1.34 (2.29) | 0.38 |
| Elixhauser Mortality Index–Mean (S.D.) | 1.32 (3.67) | 1.84 (5.60) | 0.02 | 1.32 (3.67) | 1.00 (3.60) | 0.28 |
| Dependent Variable = ln(Length of Stay) | |
|---|---|
| Variable | Coefficient (Standard Error) |
| Diagnosed malnutrition | 1.01 ** (0.21) |
| Admitted 2015 or later | −0.35 ** (0.09) |
| Admitted 2015 or later + diagnosed malnutrition | 0.06 (0.27) |
| Female | 0.02 (0.09) |
| Age | −0.05 ** (0.01) |
| Asia/Pacific Islander | 0.23 (0.19) |
| Black | 0.01 (0.13) |
| Elixhauser Readmission | 0.03 (0.02) |
| Elixhauser Mortality | −0.01 (0.01) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khlevner, J.; Naranjo, K.; Hoyer, C.; Carullo, A.S.; Kerr, K.W.; Marriage, B. Healthcare Burden Associated with Malnutrition Diagnoses in Hospitalized Children with Critical Illnesses. Nutrients 2023, 15, 3011. https://doi.org/10.3390/nu15133011
Khlevner J, Naranjo K, Hoyer C, Carullo AS, Kerr KW, Marriage B. Healthcare Burden Associated with Malnutrition Diagnoses in Hospitalized Children with Critical Illnesses. Nutrients. 2023; 15(13):3011. https://doi.org/10.3390/nu15133011
Chicago/Turabian StyleKhlevner, Julie, Kelly Naranjo, Christine Hoyer, Angela S. Carullo, Kirk W. Kerr, and Barbara Marriage. 2023. "Healthcare Burden Associated with Malnutrition Diagnoses in Hospitalized Children with Critical Illnesses" Nutrients 15, no. 13: 3011. https://doi.org/10.3390/nu15133011
APA StyleKhlevner, J., Naranjo, K., Hoyer, C., Carullo, A. S., Kerr, K. W., & Marriage, B. (2023). Healthcare Burden Associated with Malnutrition Diagnoses in Hospitalized Children with Critical Illnesses. Nutrients, 15(13), 3011. https://doi.org/10.3390/nu15133011






