The Association of Surrogates of Insulin Resistance with Hyperuricemia among Middle-Aged and Older Individuals: A Population-Based Nationwide Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
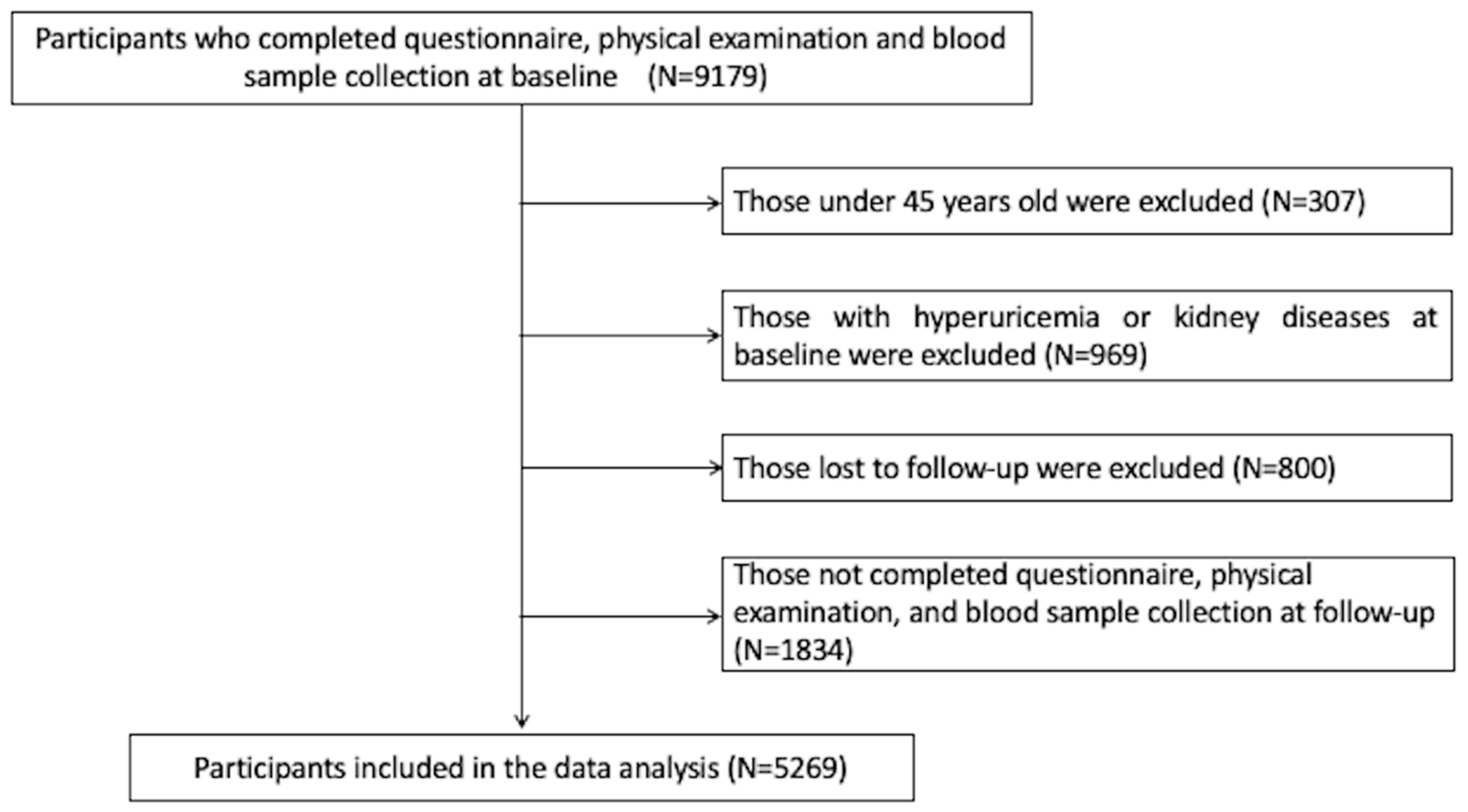
2.1. Study Design and Population
2.2. Data Collection and Measurement
2.3. Definitions of Covariates
2.4. Definitions of TyG Index, TG/HDL-C Ratio, METS-IR, TyG-BMI and Hyperuricemia
2.5. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Association between Baseline Insulin Resistance Surrogates and Hyperuricemia Risk
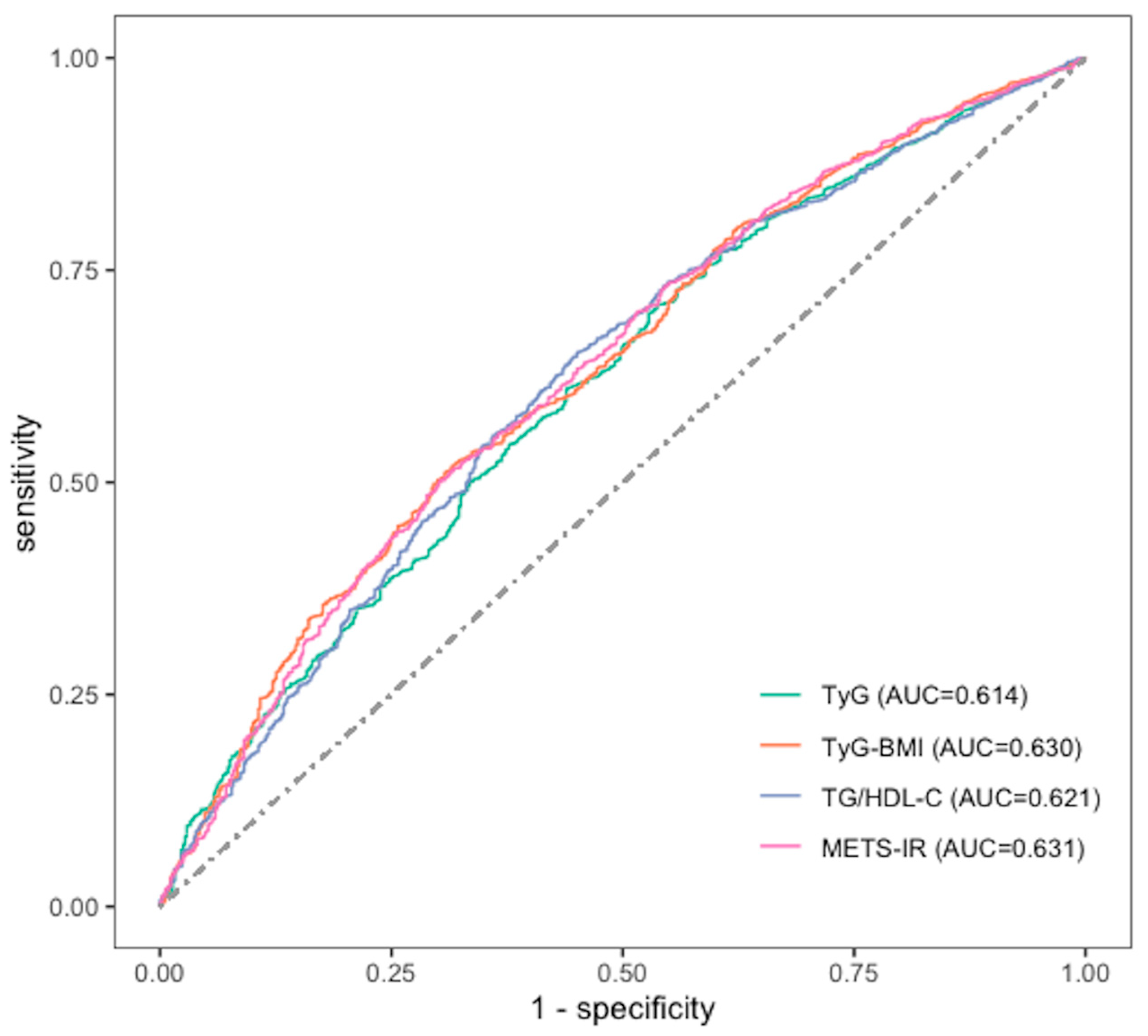
3.3. ROCs of TyG Index, TyG/HDL-C Ratio, METS-IR, TyG-BMI for Hyperuricemia
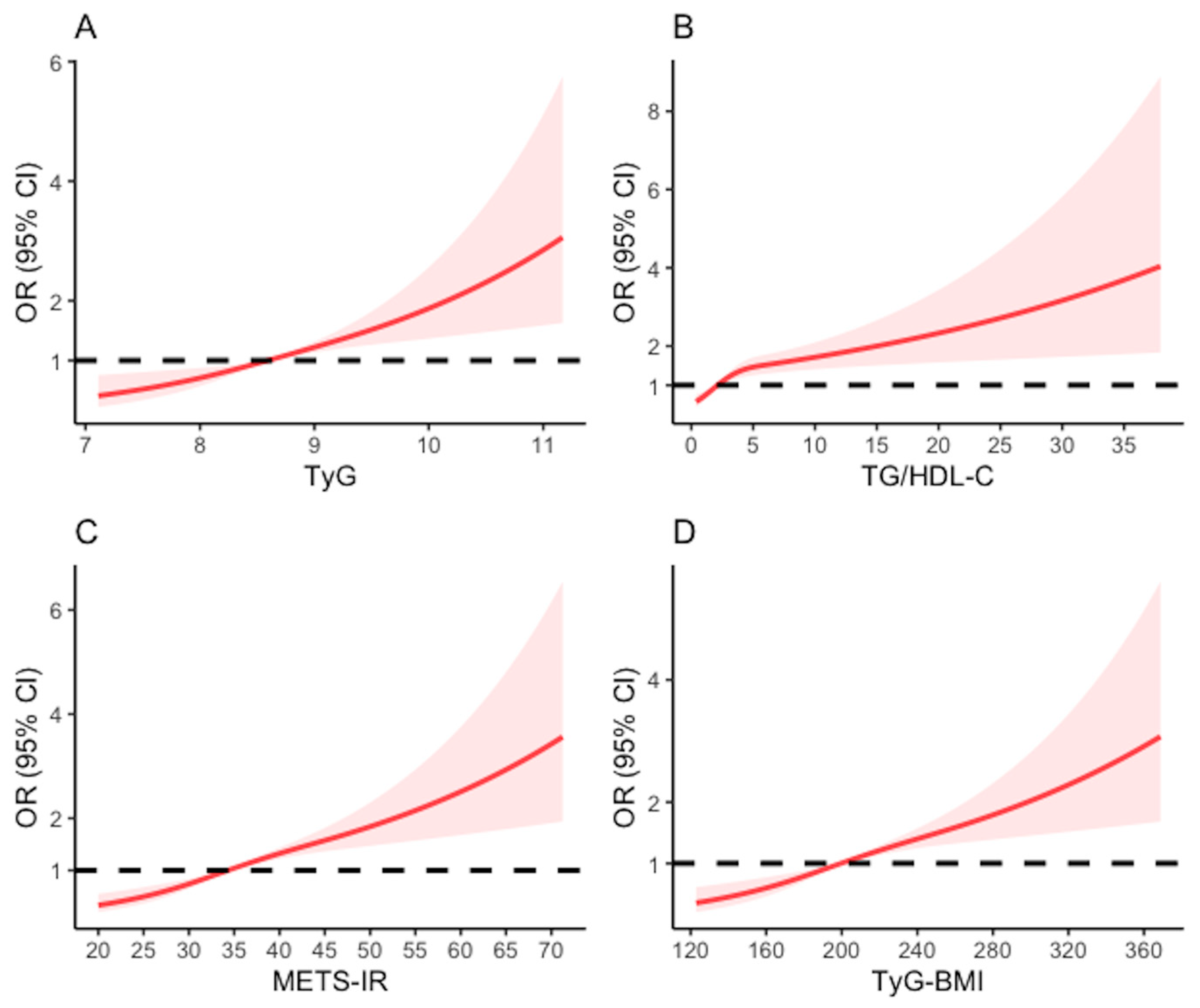
3.4. Restricted Cubic Spline Regression
3.5. Association between the Variation of TyG, TG/HDL-C, METS-IR, TyG-BMI and Hyperuricemia
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Waheed, Y.; Yang, F.; Sun, D. Role of asymptomatic hyperuricemia in the progression of chronic kidney disease and cardiovascular disease. Korean J. Intern. Med. 2021, 36, 1281–1293. [Google Scholar] [CrossRef] [PubMed]
- Mortada, I. Hyperuricemia, Type 2 Diabetes Mellitus, and Hypertension: An Emerging Association. Curr. Hypertens. Rep. 2017, 19, 69. [Google Scholar] [CrossRef] [PubMed]
- Sharaf El Din, U.A.A.; Salem, M.M.; Abdulazim, D.O. Uric acid in the pathogenesis of metabolic, renal, and cardiovascular diseases: A review. J. Adv. Res. 2017, 8, 537–548. [Google Scholar] [CrossRef]
- Xu, C. Hyperuricemia and nonalcoholic fatty liver disease: From bedside to bench and back. Hepatol. Int. 2016, 10, 286–293. [Google Scholar] [CrossRef]
- Chen-Xu, M.; Yokose, C.; Rai, S.K.; Pillinger, M.H.; Choi, H.K. Contemporary Prevalence of Gout and Hyperuricemia in the United States and Decadal Trends: The National Health and Nutrition Examination Survey, 2007–2016. Arthritis Rheumatol. 2019, 71, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Kang, J.; Kim, G.T. Prevalence of hyperuricemia and its associated factors in the general Korean population: An analysis of a population-based nationally representative sample. Clin. Rheumatol. 2018, 37, 2529–2538. [Google Scholar] [CrossRef] [PubMed]
- Piao, W.; Zhao, L.; Yang, Y.; Fang, H.; Ju, L.; Cai, S.; Yu, D. The Prevalence of Hyperuricemia and Its Correlates among Adults in China: Results from CNHS 2015–2017. Nutrients 2022, 14, 4095. [Google Scholar] [CrossRef]
- Li, L.; Zhang, Y.; Zeng, C. Update on the epidemiology, genetics, and therapeutic options of hyperuricemia. Am. J. Transl. Res. 2020, 12, 3167–3181. [Google Scholar]
- Bardin, T.; Richette, P. Impact of comorbidities on gout and hyperuricaemia: An update on prevalence and treatment options. BMC Med. 2017, 15, 123. [Google Scholar] [CrossRef]
- Dehlin, M.; Jacobsson, L.; Roddy, E. Global epidemiology of gout: Prevalence, incidence, treatment patterns and risk factors. Nat. Rev. Rheumatol. 2020, 16, 380–390. [Google Scholar] [CrossRef]
- Freeman, A.M.; Pennings, N. Insulin Resistance. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2023. [Google Scholar]
- Facchini, F.; Chen, Y.D.; Hollenbeck, C.B.; Reaven, G.M. Relationship between resistance to insulin-mediated glucose uptake, urinary uric acid clearance, and plasma uric acid concentration. JAMA 1991, 266, 3008–3011. [Google Scholar] [CrossRef]
- Toyoki, D.; Shibata, S.; Kuribayashi-Okuma, E.; Xu, N.; Ishizawa, K.; Hosoyamada, M.; Uchida, S. Insulin stimulates uric acid reabsorption via regulating urate transporter 1 and ATP-binding cassette subfamily G member 2. Am. J. Physiol. Renal Physiol. 2017, 313, F826–F834. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, W.; Xie, D.; Yamamoto, T.; Koyama, H.; Cheng, J. Mechanistic insights of soluble uric acid-induced insulin resistance: Insulin signaling and beyond. Rev. Endocr. Metab. Disord. 2023, 24, 327–343. [Google Scholar] [CrossRef] [PubMed]
- McCormick, N.; O’Connor, M.J.; Yokose, C.; Merriman, T.R.; Mount, D.B.; Leong, A.; Choi, H.K. Assessing the Causal Relationships Between Insulin Resistance and Hyperuricemia and Gout Using Bidirectional Mendelian Randomization. Arthritis Rheumatol. 2021, 73, 2096–2104. [Google Scholar] [CrossRef]
- Joshi, H.; Shah, K.; Patel, P.; Prajapati, J.; Parmar, M.; Doshi, D.; Chaurushia, S. Novel indexes for diagnosing metabolic syndrome in apparently healthy Gujarati Asian Indians: A cross-sectional study. QJM 2016, 109, 717–722. [Google Scholar] [CrossRef] [Green Version]
- Liu, T.; Zhang, Q.; Wang, Y.; Ma, X.; Zhang, Q.; Song, M.; Cao, L.; Shi, H. Association between the TyG index and TG/HDL-C ratio as insulin resistance markers and the risk of colorectal cancer. BMC Cancer 2022, 22, 1007. [Google Scholar] [CrossRef] [PubMed]
- Er, L.K.; Wu, S.; Chou, H.H.; Hsu, L.A.; Teng, M.S.; Sun, Y.C.; Ko, Y.L. Triglyceride Glucose-Body Mass Index Is a Simple and Clinically Useful Surrogate Marker for Insulin Resistance in Nondiabetic Individuals. PLoS ONE 2016, 11, e0149731. [Google Scholar] [CrossRef]
- Bello-Chavolla, O.Y.; Almeda-Valdes, P.; Gomez-Velasco, D.; Viveros-Ruiz, T.; Cruz-Bautista, I.; Romo-Romo, A.; Sánchez-Lázaro, D.; Meza-Oviedo, D.; Vargas-Vázquez, A.; Campos, O.A.; et al. METS-IR, a novel score to evaluate insulin sensitivity, is predictive of visceral adiposity and incident type 2 diabetes. Eur. J. Endocrinol. 2018, 178, 533–544. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.Y.; Wu, Q.Y.; Chen, Z.H.; Yan, G.Y.; Lu, Y.; Dai, H.J.; Li, Y.; Yang, P.T.; Yuan, H. Elevated triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio increased risk of hyperuricemia: A 4-year cohort study in China. Endocrine 2020, 68, 71–80. [Google Scholar] [CrossRef]
- Shi, W.; Xing, L.; Jing, L.; Tian, Y.; Liu, S. Usefulness of Triglyceride-glucose Index for estimating Hyperuricemia risk: Insights from a general Population. Postgrad. Med. 2019, 131, 348–356. [Google Scholar] [CrossRef]
- Wang, H.; Zhang, J.; Pu, Y.; Qin, S.; Liu, H.; Tian, Y.; Tang, Z. Comparison of different insulin resistance surrogates to predict hyperuricemia among U.S. non-diabetic adults. Front. Endocrinol. 2022, 13, 1028167. [Google Scholar] [CrossRef]
- Liu, X.Z.; Xu, X.; Zhu, J.Q.; Zhao, D.B. Association between three non-insulin-based indexes of insulin resistance and hyperuricemia. Clin. Rheumatol. 2019, 38, 3227–3233. [Google Scholar] [CrossRef]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef] [Green Version]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, D.T.; LeFevre, M.L.; MacKenzie, T.D.; Ogedegbe, O.; et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2014, 37 (Suppl. 1), S81–S90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joint Committee for Guideline Revision. 2016 Chinese guidelines for the management of dyslipidemia in adults. J. Geriatr. Cardiol. 2018, 15, 1–29. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Kang, B.; Yang, Y.; Lee, E.Y.; Yang, H.K.; Kim, H.S.; Lim, S.Y.; Lee, J.H.; Lee, S.S.; Suh, B.K.; Yoon, K.H. Triglycerides/glucose index is a useful surrogate marker of insulin resistance among adolescents. Int. J. Obes. 2017, 41, 789–792. [Google Scholar] [CrossRef]
- Liu, X.Z.; Fan, J.; Pan, S.J. METS-IR, a novel simple insulin resistance indexes, is associated with hypertension in normal-weight Chinese adults. J. Hypertens. 2019, 21, 1075–1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Song, P.; Wang, H.; Xia, W.; Chang, X.; Wang, M.; An, L. Prevalence and correlates of hyperuricemia in the middle-aged and older adults in China. Sci. Rep. 2018, 8, 4314. [Google Scholar] [CrossRef] [Green Version]
- Menard, S. Six Approaches to Calculating Standardized Logistic Regression Coefficients. Am. Stat. 2004, 58, 218–223. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef] [PubMed]
- Gu, Q.; Hu, X.; Meng, J.; Ge, J.; Wang, S.J.; Liu, X.Z. Associations of Triglyceride-Glucose Index and Its Derivatives with Hyperuricemia Risk: A Cohort Study in Chinese General Population. Int. J. Endocrinol. 2020, 2020, 3214716. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.W.; Chang, C.C.; Chou, R.H.; Tsai, Y.L.; Liu, L.K.; Chen, L.K.; Huang, P.H.; Lin, S.J. Gender difference in the association between TyG index and subclinical atherosclerosis: Results from the I-Lan Longitudinal Aging Study. Cardiovasc. Diabetol. 2021, 20, 206. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, Y.; Hashimoto, Y.; Hamaguchi, M.; Fukuda, T.; Nakamura, N.; Ohbora, A.; Kato, T.; Kojima, T.; Fukui, M. Triglycerides to high-density lipoprotein cholesterol ratio is an independent predictor of incident fatty liver; a population-based cohort study. Liver Int. 2016, 36, 713–720. [Google Scholar] [CrossRef] [PubMed]
- De Paoli, M.; Zakharia, A.; Werstuck, G.H. The Role of Estrogen in Insulin Resistance: A Review of Clinical and Preclinical Data. Am. J. Pathol. 2021, 191, 1490–1498. [Google Scholar] [CrossRef]
- Kodama, K.; Tojjar, D.; Yamada, S.; Toda, K.; Patel, C.J.; Butte, A.J. Ethnic differences in the relationship between insulin sensitivity and insulin response: A systematic review and meta-analysis. Diabetes Care 2013, 36, 1789–1796. [Google Scholar] [CrossRef] [Green Version]
- Fuente-Martín, E.; Argente-Arizón, P.; Ros, P.; Argente, J.; Chowen, J.A. Sex differences in adipose tissue: It is not only a question of quantity and distribution. Adipocyte 2013, 2, 128–134. [Google Scholar] [CrossRef]
- Zhu, J.; Sun, L.; Yang, J.; Fan, J.; Tse, L.A.; Li, Y. Genetic Predisposition to Type 2 Diabetes and Insulin Levels Is Positively Associated With Serum Urate Levels. J. Clin. Endocrinol. Metab. 2021, 106, e2547–e2556. [Google Scholar] [CrossRef]
- Hu, X.; Rong, S.; Wang, Q.; Sun, T.; Bao, W.; Chen, L.; Liu, L. Association between plasma uric acid and insulin resistance in type 2 diabetes: A Mendelian randomization analysis. Diabetes Res. Clin. Pract. 2021, 171, 108542. [Google Scholar] [CrossRef]
- Yanai, H.; Adachi, H.; Hakoshima, M.; Katsuyama, H. Molecular Biological and Clinical Understanding of the Pathophysiology and Treatments of Hyperuricemia and Its Association with Metabolic Syndrome, Cardiovascular Diseases and Chronic Kidney Disease. Int. J. Mol. Sci. 2021, 22, 9221. [Google Scholar] [CrossRef] [PubMed]
- Bjornstad, P.; Eckel, R.H. Pathogenesis of Lipid Disorders in Insulin Resistance: A Brief Review. Curr. Diab Rep. 2018, 18, 127. [Google Scholar] [CrossRef] [PubMed]
| Variables | Overall | Hyperuricemia | p Value | |
|---|---|---|---|---|
| No | Yes | |||
| Overall, n (%) | 5269 (100.00) | 4752 (90.19) | 517 (9.81) | - |
| Age (years, mean ± SD) | 58.58 ± 8.61 | 58.41 ± 8.53 | 60.11 ± 9.15 | <0.001 |
| Gender, n (%) | ||||
| Male | 2386 (45.28) | 2119 (44.59) | 267 (51.64) | 0.003 |
| Female | 2883 (54.72) | 2633 (55.41) | 250 (48.36) | |
| Residence, n (%) | ||||
| Rural | 3540 (67.19) | 3210 (67.55) | 330 (63.83) | 0.097 |
| Urban | 1729 (32.81) | 1542 (32.45) | 187 (36.17) | |
| Education status, n (%) | ||||
| Illiterate | 1509 (28.64) | 1374 (28.91) | 135 (26.11) | 0.369 |
| Primary school and below | 2234 (42.40) | 2003 (42.15) | 231 (44.68) | |
| Middle school and above | 1526 (28.96) | 1375 (28.94) | 151 (29.21) | |
| Marital status, n (%) | ||||
| Single | 4704 (89.28) | 4250 (89.44) | 454 (87.81) | 0.291 |
| Married/cohabiting | 565 (10.72) | 502 (10.56) | 63 (12.19) | |
| Smoking history, n (%) | ||||
| Non-smoker | 3272 (62.10) | 2967 (62.44) | 305 (58.99) | 0.138 |
| Smoker | 1997 (37.90) | 1785 (37.56) | 212 (41.01) | |
| Drinking status, n (%) | ||||
| Non-drinker | 3277 (62.19) | 2993 (62.98) | 284 (54.93) | <0.001 |
| Drinker | 1992 (37.81) | 1759 (37.02) | 233 (45.07) | |
| Hypertension, n (%) | ||||
| No | 3212 (60.96) | 2988 (62.88) | 224 (43.33) | <0.001 |
| Yes | 2057 (39.04) | 1764 (37.12) | 293 (56.67) | |
| Diabetes mellitus, n (%) | ||||
| No | 4428 (84.04) | 4010 (84.39) | 418 (80.85) | 0.037 |
| Yes | 841 (15.96) | 742 (15.61) | 99 (19.15) | |
| Cardiovascular disease, n (%) | ||||
| No | 4587 (87.06) | 4162 (87.58) | 425 (82.21) | <0.001 |
| Yes | 682 (12.94) | 590 (12.42) | 92 (17.79) | |
| Dyslipidemia, n (%) | ||||
| No | 3024 (57.39) | 2801 (58.94) | 223 (43.13) | <0.001 |
| Yes | 2245 (42.61) | 1951 (41.06) | 294 (56.87) | |
| BMI, kg/m2, mean ± SD | 23.55 ± 3.70 | 23.41 ± 3.67 | 24.75 ± 3.75 | <0.001 |
| FPG, mg/dL, median (IQR) | 102.42 (94.5, 112.68) | 102.24 (94.32, 112.32) | 104.4 (95.76, 116.28) | 0.001 |
| HDL-C, mg/dL, median (IQR) | 49.48 (40.59, 59.92) | 49.87 (40.98, 60.31) | 45.62 (37.11, 54.51) | <0.001 |
| TG, mg/dL, median (IQR) | 105.32 (74.34, 152.22) | 102.66 (73.46, 147.79) | 130.98 (87.61, 194.7) | <0.001 |
| Total cholesterol, mg/dL, median (IQR) | 190.59 (167.01, 214.95) | 190.01 (166.62, 214.56) | 195.62 (173.97, 219.59) | <0.001 |
| HbA1c, %, median (IQR) | 5.1 (4.9, 5.4) | 5.1 (4.9, 5.4) | 5.2 (4.9, 5.5) | 0.002 |
| Creatinine, mg/dL, median (IQR) | 0.75 (0.64, 0.86) | 0.73 (0.63, 0.85) | 0.80 (0.71, 0.94) | <0.001 |
| C-reactive protein, mg/L, median (IQR) | 0.98 (0.54, 2.02) | 0.95 (0.52, 1.94) | 1.31 (0.71, 2.70) | <0.001 |
| eGFR, ml/min per 1.73 m2, median (IQR) | 95.87 (86.2, 102.78) | 96.39 (87.16, 103.19) | 90.41 (79.30, 98.62) | <0.001 |
| BUN, mg/dL, median (IQR) | 14.99 (12.49, 18.04) | 14.93 (12.44, 18.04) | 15.55 (13.08, 17.87) | 0.017 |
| SUA, mg/dL, median (IQR) | 4.17 (3.51, 4.94) | 4.08 (3.45, 4.79) | 5.22 (4.57, 5.93) | <0.001 |
| TyG, median (IQR) | 8.59 (8.22, 9.03) | 8.57 (8.21, 9.00) | 8.82 (8.42, 9.30) | <0.001 |
| TG/HDL-C, median (IQR) | 2.11 (1.32, 3.53) | 2.05 (1.29, 3.39) | 2.94 (1.71, 4.68) | <0.001 |
| METS-IR, median (IQR) | 34.31 (29.84, 40.17) | 33.91 (29.59, 39.60) | 37.67 (32.73, 44.38) | <0.001 |
| TyG-BMI, median (IQR) | 199.52 (176.27, 229.01) | 197.71 (175.18, 225.77) | 213.68 (191.58, 250.4) | <0.001 |
| Variables | No. of Cases (%) | OR (95% CI) | β | βs | |||
|---|---|---|---|---|---|---|---|
| Crude Model | Model 1 | Model 2 | Model 3 | ||||
| TyG | |||||||
| Q1 | 73 (5.54) | 1.00 | 1.00 | 1.00 | 1.00 | - | - |
| Q2 | 113 (8.49) | 1.58 (1.17, 2.15) | 1.62 (1.20, 2.22) | 1.51 (1.11, 2.07) | 1.49 (1.09, 2.04) | 0.396 | 0.035 |
| Q3 | 132 (9.73) | 1.84 (1.37, 2.49) | 1.92 (1.43, 2.61) | 1.67 (1.23, 2.28) | 1.57 (1.15, 2.16) | 0.454 | 0.040 |
| Q4 | 206 (15.49) | 3.13 (2.38, 4.16) | 3.33 (2.52, 4.44) | 2.64 (1.92, 3.67) | 2.39 (1.72, 3.34) | 0.870 | 0.081 |
| p for trend | <0.001 | <0.001 | <0.001 | <0.001 | - | - | |
| TyG change, per SD increase | 528 (9.79) | 1.45 (1.33, 1.57) | 1.47 (1.36, 1.61) | 1.40 (1.25, 1.57) | 1.36 (1.22, 1.54) | 0.312 | 0.010 |
| TG/HDL-C | |||||||
| Q1 | 78 (5.91) | 1.00 | 1.00 | 1.00 | 1.00 | - | - |
| Q2 | 99 (7.45) | 1.28 (0.94, 1.75) | 1.32 (0.97, 1.80) | 1.27 (0.93, 1.73) | 1.24 (0.91, 1.71) | 0.218 | 0.019 |
| Q3 | 135 (10.03) | 1.77 (1.33, 2.38) | 1.87 (1.4, 2.51) | 1.65 (1.22, 2.24) | 1.57 (1.16, 2.14) | 0.451 | 0.039 |
| Q4 | 213 (15.88) | 3.00 (2.30, 3.96) | 3.25 (2.48, 4.31) | 2.58 (1.86, 3.59) | 2.42 (1.74, 3.38) | 0.884 | 0.082 |
| p for trend | <0.001 | <0.001 | <0.001 | <0.001 | - | - | |
| TG/HDL-C change, per SD increase | 528 (9.79) | 1.27 (1.19, 1.36) | 1.28 (1.20, 1.38) | 1.19 (1.10, 1.28) | 1.20 (1.11, 1.30) | 0.184 | 0.004 |
| METS-IR | |||||||
| Q1 | 69 (5.24) | 1.00 | 1.00 | 1.00 | 1.00 | - | - |
| Q2 | 102 (7.52) | 1.47 (1.07, 2.03) | 1.59 (1.15, 2.19) | 1.49 (1.08, 2.06) | 1.49 (1.08, 2.07) | 0.401 | 0.037 |
| Q3 | 143 (10.86) | 2.20 (1.64, 2.99) | 2.52 (1.87, 3.44) | 2.12 (1.55, 2.92) | 2.09 (1.52, 2.88) | 0.735 | 0.066 |
| Q4 | 210 (15.64) | 3.36 (2.54, 4.49) | 4.06 (3.04, 5.49) | 3.03 (2.18, 4.25) | 2.89 (2.07, 4.07) | 1.061 | 0.101 |
| p for trend | <0.001 | <0.001 | <0.001 | <0.001 | - | - | |
| METS-IR change, per SD increase | 528 (9.79) | 1.49 (1.38, 1.62) | 1.58 (1.45, 1.72) | 1.44 (1.30, 1.59) | 1.43 (1.29, 1.58) | 0.356 | 0.010 |
| TyG-BMI | |||||||
| Q1 | 63 (4.78) | 1.00 | 1.00 | 1.00 | 1.00 | - | - |
| Q2 | 101 (7.67) | 1.47 (1.07, 2.03) | 1.82 (1.32, 2.53) | 1.71 (1.23, 2.39) | 1.67 (1.20, 2.34) | 0.512 | 0.048 |
| Q3 | 144 (10.93) | 2.20 (1.64, 2.99) | 2.88 (2.12, 3.97) | 2.40 (1.74, 3.34) | 2.25 (1.63, 3.14) | 0.812 | 0.075 |
| Q4 | 209 (15.87) | 3.36 (2.54, 4.49) | 4.78 (3.54, 6.53) | 3.65 (2.62, 5.13) | 3.35 (2.40, 4.73) | 1.209 | 0.116 |
| p for trend | <0.001 | <0.001 | <0.001 | <0.001 | - | - | |
| TyG-BMI change, per SD increase | 528 (9.79) | 1.51 (1.39, 1.64) | 1.62 (1.48, 1.77) | 1.47 (1.33, 1.63) | 1.43 (1.29, 1.59) | 0.361 | 0.011 |
| TyG Model | TG/HDL-C Model | METS-IR Model | TyG-BMI Model | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | βs | p | β | βs | p | β | βs | p | β | βs | p | |
| Age | 0.012 | 0.000 | 0.067 | 0.012 | 0.000 | 0.047 | 0.016 | 0.000 | 0.011 | 0.018 | 0.000 | 0.005 |
| Sex | 0.101 | 0.009 | 0.526 | 0.134 | 0.012 | 0.402 | 0.139 | 0.012 | 0.387 | 0.098 | 0.009 | 0.540 |
| Resident | −0.015 | −0.001 | 0.885 | −0.029 | −0.002 | 0.775 | −0.073 | −0.004 | 0.479 | −0.072 | −0.004 | 0.486 |
| Education status | 0.033 | 0.001 | 0.660 | 0.035 | 0.001 | 0.638 | 0.016 | 0.001 | 0.834 | 0.015 | 0.001 | 0.838 |
| Married status | 0.017 | 0.001 | 0.915 | 0.026 | 0.002 | 0.866 | 0.068 | 0.006 | 0.660 | 0.070 | 0.006 | 0.652 |
| Smoking history | −0.189 | −0.014 | 0.152 | −0.194 | −0.014 | 0.142 | −0.117 | −0.009 | 0.376 | −0.091 | −0.007 | 0.495 |
| Drinking history | 0.304 | 0.020 | 0.009 | 0.330 | 0.021 | 0.005 | 0.332 | 0.021 | 0.004 | 0.306 | 0.020 | 0.009 |
| Hypertension | 0.593 | 0.032 | 0.000 | 0.590 | 0.032 | 0.000 | 0.509 | 0.028 | 0.000 | 0.488 | 0.027 | 0.000 |
| Diabetes | −0.320 | −0.026 | 0.030 | −0.209 | −0.017 | 0.146 | −0.252 | −0.020 | 0.082 | −0.276 | −0.022 | 0.056 |
| Cardiovascular disease | 0.133 | 0.010 | 0.303 | 0.133 | 0.009 | 0.305 | 0.102 | 0.007 | 0.430 | 0.111 | 0.008 | 0.394 |
| Dyslipidemia | 0.304 | 0.019 | 0.006 | 0.160 | 0.011 | 0.189 | 0.213 | 0.013 | 0.056 | 0.263 | 0.015 | 0.014 |
| Total cholesterol | 0.000 | 0.000 | 0.962 | 0.001 | 0.000 | 0.335 | 0.002 | 0.000 | 0.200 | 0.000 | 0.000 | 0.781 |
| Blood urea nitrogen | −0.010 | 0.000 | 0.417 | −0.008 | 0.000 | 0.494 | −0.011 | 0.000 | 0.360 | −0.011 | 0.000 | 0.359 |
| Creatinine | 2.284 | 0.399 | 0.000 | 2.286 | 0.399 | 0.000 | 2.327 | 0.409 | 0.000 | 2.297 | 0.405 | 0.000 |
| Glycated hemoglobin | 0.075 | 0.003 | 0.226 | 0.090 | 0.003 | 0.150 | 0.066 | 0.002 | 0.296 | 0.060 | 0.002 | 0.342 |
| C-reactive protein | 0.006 | 0.000 | 0.250 | 0.007 | 0.000 | 0.245 | 0.005 | 0.000 | 0.381 | 0.006 | 0.000 | 0.320 |
| Variation Types During Follow-Up | No. of Cases (%) | OR (95% CI) | |||
|---|---|---|---|---|---|
| Crude Model | Model 1 | Model 2 | Model 3 | ||
| TyG | |||||
| Low–Low | 93 (5.59) | 1.00 | 1.00 | 1.00 | 1.00 |
| Low–High | 79 (9.34) | 1.74 (1.27, 2.38) | 1.86 (1.36, 2.55) | 1.71 (1.24, 2.35) | 1.71 (1.24, 2.36) |
| High–Low | 52 (7.18) | 1.31 (0.91, 1.85) | 1.34 (0.94, 1.90) | 1.19 (0.82, 1.69) | 1.12 (0.78, 1.61) |
| High–High | 293 (14.40) | 2.84 (2.24, 3.64) | 3.11 (2.44, 4.01) | 2.46 (1.88, 3.24) | 2.28 (1.73, 3.02) |
| TG/HDL-C | |||||
| Low–Low | 114 (5.79) | 1.00 | 1.00 | 1.00 | 1.00 |
| Low–High | 76 (8.67) | 1.54 (1.14, 2.08) | 1.65 (1.21, 2.23) | 1.54 (1.13, 2.08) | 1.53 (1.12, 2.08) |
| High–Low | 55 (9.11) | 1.63 (1.16, 2.27) | 1.72 (1.22, 2.40) | 1.50 (1.05, 2.12) | 1.46 (1.02, 2.07) |
| High–High | 272 (14.96) | 2.86 (2.28, 3.61) | 3.13 (2.49, 3.97) | 2.49 (1.91, 3.24) | 2.34 (1.80, 3.06) |
| METS-IR | |||||
| Low–Low | 123 (5.78) | 1.00 | 1.00 | 1.00 | 1.00 |
| Low–High | 46 (8.70) | 1.55 (1.08, 2.19) | 1.71 (1.19, 2.42) | 1.60 (1.11, 2.27) | 1.62 (1.12, 2.30) |
| High–Low | 43 (11.44) | 2.11 (1.45, 3.01) | 2.33 (1.59, 3.35) | 1.95 (1.32, 2.83) | 1.96 (1.32, 2.87) |
| High–High | 305 (13.65) | 2.58 (2.08, 3.22) | 2.97 (2.37, 3.74) | 2.26 (1.76, 2.91) | 2.19 (1.70, 2.83) |
| TyG-BMI | |||||
| Low–Low | 124 (5.90) | 1.00 | 1.00 | 1.00 | 1.00 |
| Low–High | 49 (8.25) | 1.43 (1.01, 2.01) | 1.68 (1.18, 2.37) | 1.58 (1.10, 2.22) | 1.58 (1.11, 2.24) |
| High–Low | 35 (10.39) | 1.85 (1.23, 2.71) | 2.06 (1.37, 3.04) | 1.70 (1.12, 2.53) | 1.63 (1.07, 2.44) |
| High–High | 309 (13.80) | 2.55 (2.06, 3.18) | 3.08 (2.46, 3.89) | 2.35 (1.83, 3.02) | 2.20 (1.71, 2.83) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, Y.; Zhou, Z.; Zhang, Y.; Zhao, G.; Xu, B. The Association of Surrogates of Insulin Resistance with Hyperuricemia among Middle-Aged and Older Individuals: A Population-Based Nationwide Cohort Study. Nutrients 2023, 15, 3139. https://doi.org/10.3390/nu15143139
Han Y, Zhou Z, Zhang Y, Zhao G, Xu B. The Association of Surrogates of Insulin Resistance with Hyperuricemia among Middle-Aged and Older Individuals: A Population-Based Nationwide Cohort Study. Nutrients. 2023; 15(14):3139. https://doi.org/10.3390/nu15143139
Chicago/Turabian StyleHan, Yutong, Zonglei Zhou, Yuge Zhang, Genming Zhao, and Biao Xu. 2023. "The Association of Surrogates of Insulin Resistance with Hyperuricemia among Middle-Aged and Older Individuals: A Population-Based Nationwide Cohort Study" Nutrients 15, no. 14: 3139. https://doi.org/10.3390/nu15143139
APA StyleHan, Y., Zhou, Z., Zhang, Y., Zhao, G., & Xu, B. (2023). The Association of Surrogates of Insulin Resistance with Hyperuricemia among Middle-Aged and Older Individuals: A Population-Based Nationwide Cohort Study. Nutrients, 15(14), 3139. https://doi.org/10.3390/nu15143139






