PEMT rs7946 Polymorphism and Sex Modify the Effect of Adequate Dietary Choline Intake on the Risk of Hepatic Steatosis in Older Patients with Metabolic Disorders
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Blood Biochemistry Marker Measurements
2.3. Assessment of Dietary Intake of MDNs
2.4. Measurements of Body Composition, Body Fat Distribution, and Obesity
2.5. Determination of PEMT Genotypes
2.6. Statistical Analysis
3. Results
3.1. Participant Characteristics
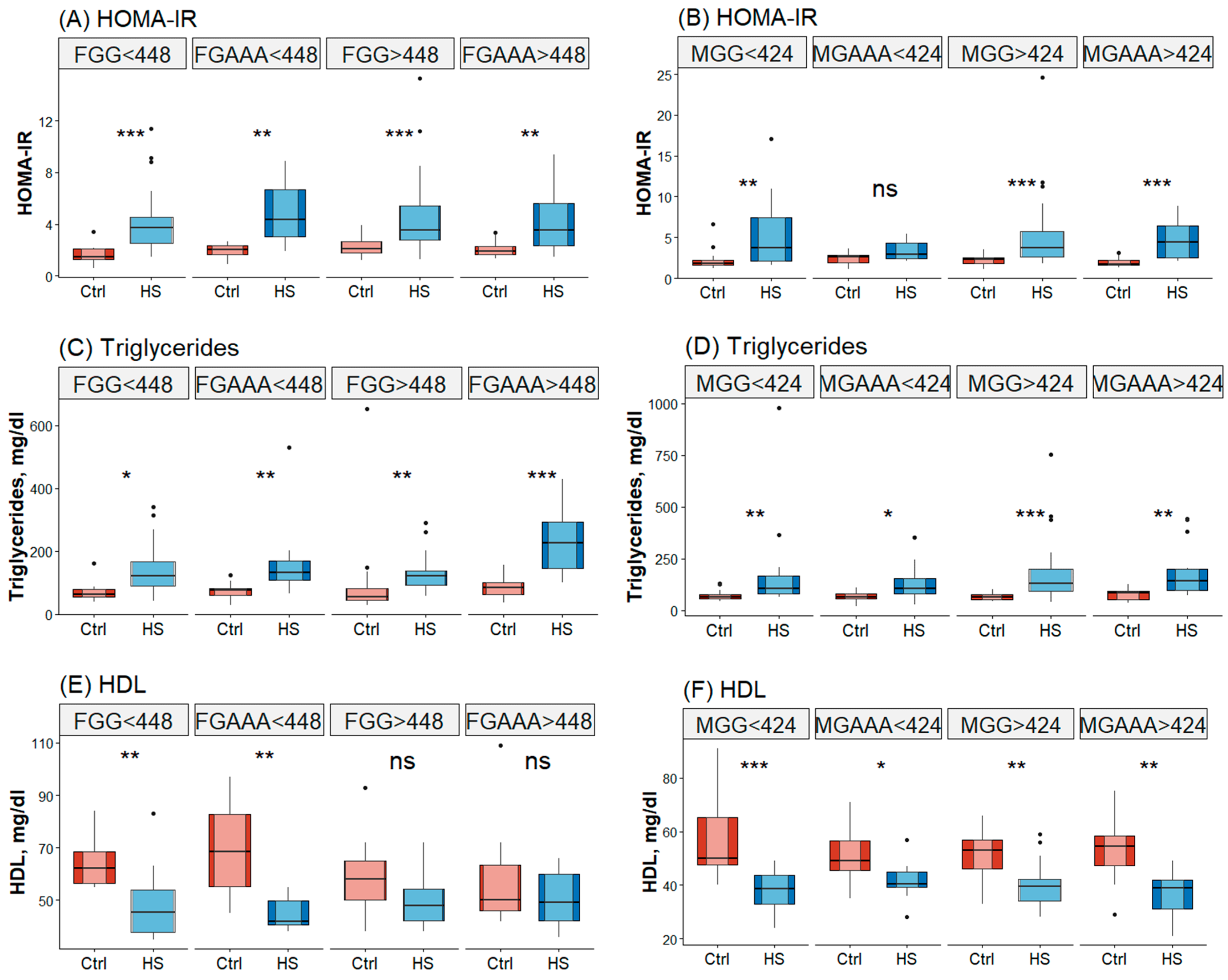
3.2. Association of Energy-Adjusted Choline Intake with the Metabolic Markers of HS Varies Depending on PEMT rs7946 Polymorphism and Sex
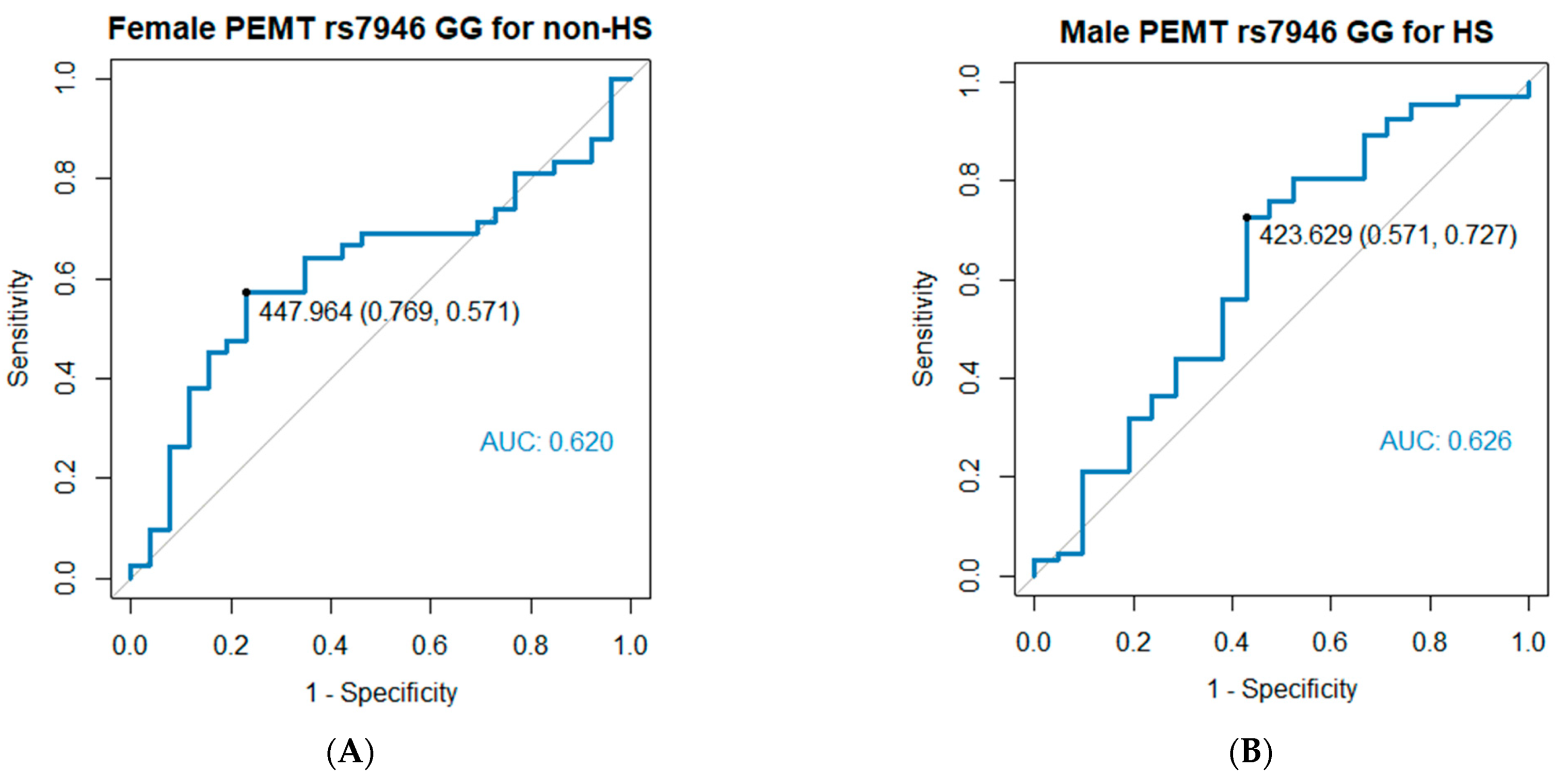
3.3. Cutoff Values of Daily Dietary Choline Intake Influence the Risk of HS According to ROC Analysis
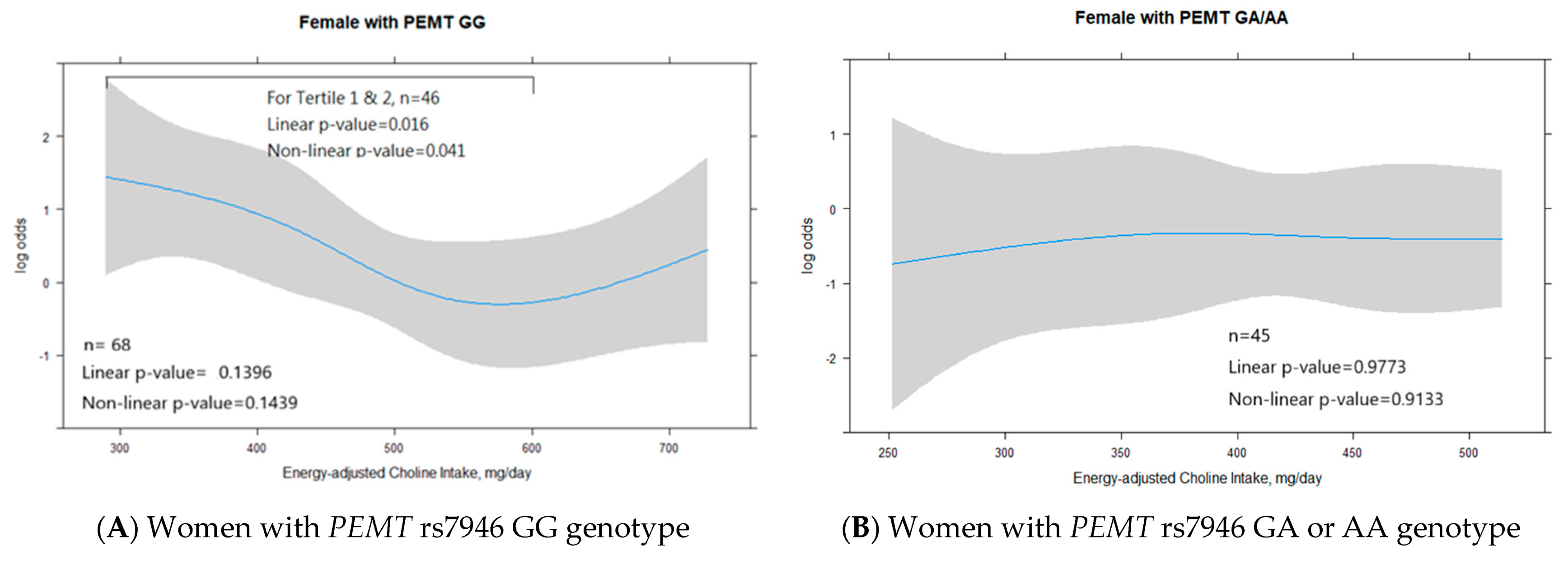
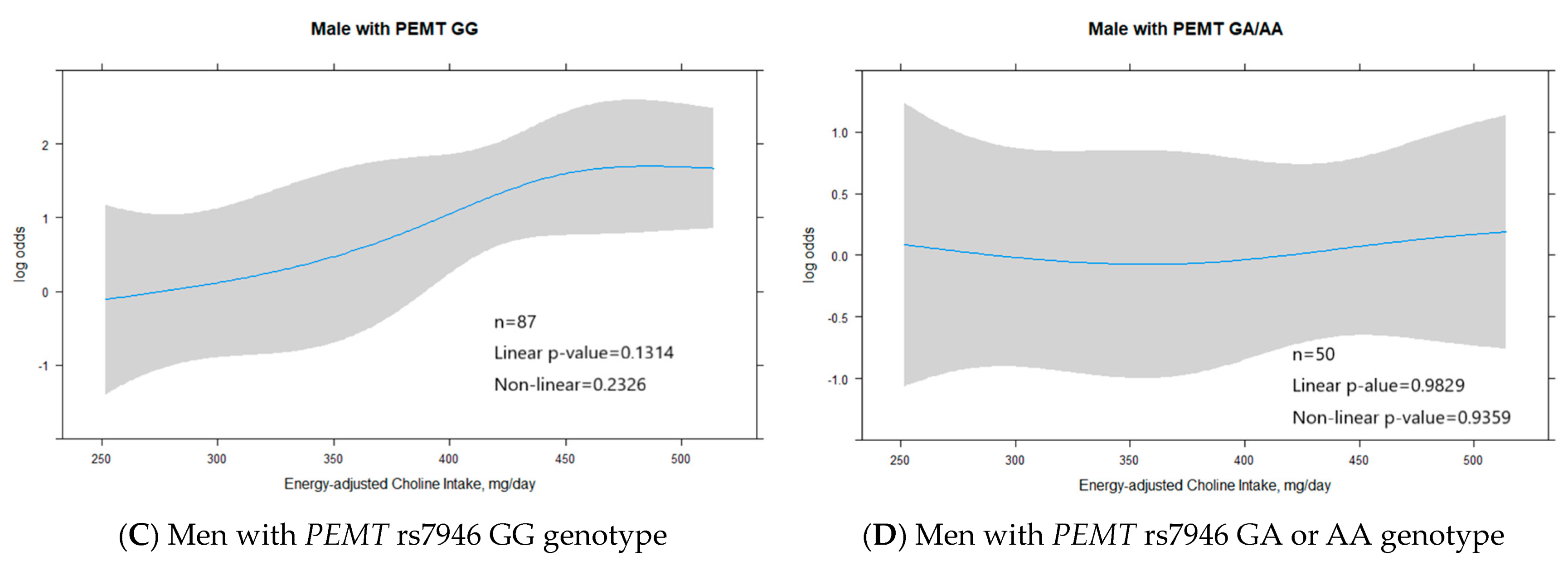
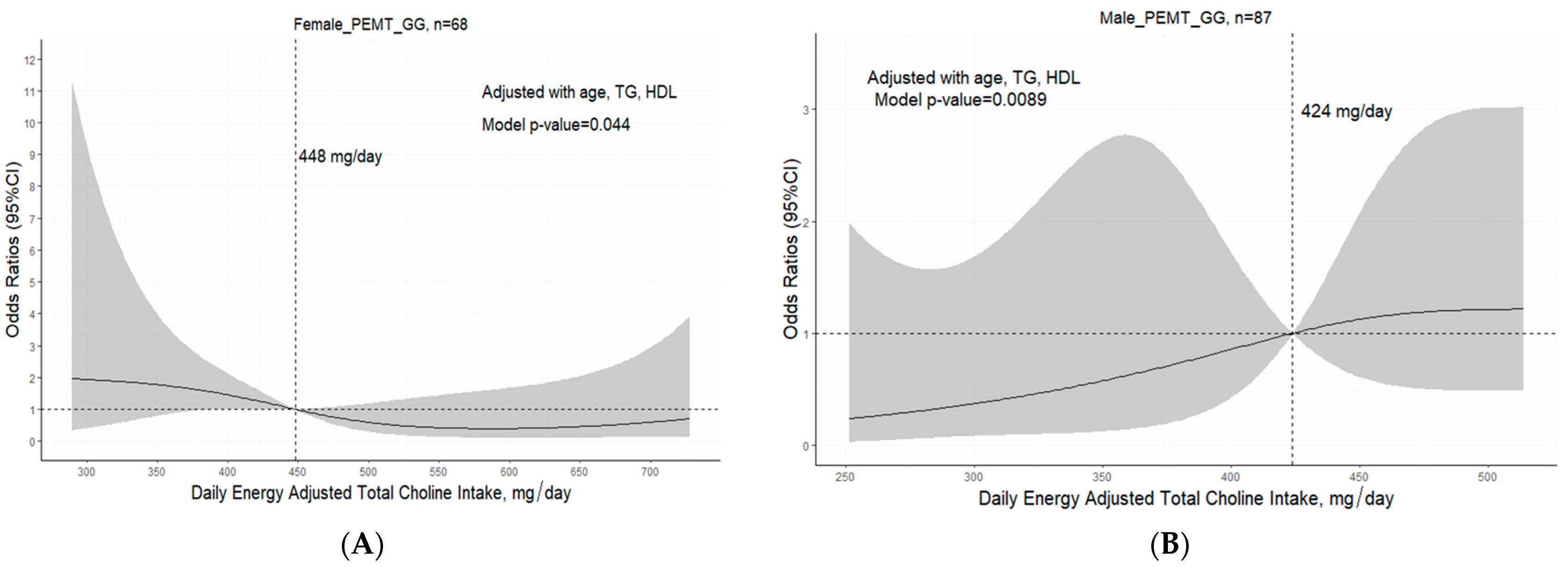
3.4. Interaction of PEMT rs7946 Polymorphism, Energy-Adjusted Daily Dietary Choline Intake, and Sex in Relation to HS Risk
3.5. PEMT rs7946 Polymorphism and Sex Regulate the Role of Adequate Choline Intake in Minimizing HS Risk
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Farrell, G.C. Non-alcoholic steatohepatitis: What is it, and why is it important in the Asia-Pacific region? J. Gastroenterol. Hepatol. 2003, 18, 124–138. [Google Scholar] [CrossRef] [PubMed]
- Chitturi, S.; Farrell, G.C.; George, J. Non-alcoholic steatohepatitis in the Asia-Pacific region: Future shock? J. Gastroenterol. Hepatol. 2004, 19, 368–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henry, L.; Paik, J.; Younossi, Z.M. Review article: The epidemiologic burden of non-alcoholic fatty liver disease across the world. Aliment. Pharmacol. Ther. 2022, 56, 942–956. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.A.; Patil, R.; Harrison, S.A. NAFLD-related hepatocellular carcinoma: The growing challenge. Hepatology 2023, 77, 323–338. [Google Scholar] [CrossRef] [PubMed]
- Riazi, K.; Azhari, H.; Charette, J.H.; Underwood, F.E.; King, J.A.; Afshar, E.E.; Swain, M.G.; Congly, S.E.; Kaplan, G.G.; Shaheen, A.-A. The prevalence and incidence of NAFLD worldwide: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2022, 7, 851–861. [Google Scholar] [CrossRef]
- Corbin, K.D.; Zeisel, S.H. Choline metabolism provides novel insights into nonalcoholic fatty liver disease and its progression. Curr. Opin. Gastroenterol. 2012, 28, 159–165. [Google Scholar] [CrossRef] [Green Version]
- Nakatsuka, T.; Tateishi, R.; Koike, K. Changing clinical management of NAFLD in Asia. Liver Int. 2022, 42, 1955–1968. [Google Scholar] [CrossRef]
- Buzzetti, E.; Pinzani, M.; Tsochatzis, E.A. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD). Metabolism 2016, 65, 1038–1048. [Google Scholar] [CrossRef]
- Chang, T.-Y.; Wu, C.-H.; Chang, C.-Y.; Lee, F.-J.; Wang, B.-W.; Doong, J.-Y.; Lin, Y.-S.; Kuo, C.-S.; Huang, R.-F.S. Optimal Dietary Intake Composition of Choline and Betaine Is Associated with Minimized Visceral Obesity-Related Hepatic Steatosis in a Case-Control Study. Nutrients 2022, 14, 261. [Google Scholar] [CrossRef]
- Song, J.; da Costa, K.A.; Fischer, L.M.; Kohlmeier, M.; Kwock, L.; Wang, S.; Zeisel, S.H. Polymorphism of the PEMT gene and susceptibility to nonalcoholic fatty liver disease (NAFLD). FASEB J. 2005, 19, 1266–1271. [Google Scholar] [CrossRef] [Green Version]
- Zeisel, S.H.; Da Costa, K.-A.; Franklin, P.D.; Alexander, E.A.; Lamont, J.T.; Sheard, N.F.; Beiser, A. Choline, an essential nutrient for humans. FASEB J. 1991, 5, 2093–2098. [Google Scholar] [CrossRef]
- Li, Z.; Vance, D.E. Thematic review series: Glycerolipids. Phosphatidylcholine and choline homeostasis. J. Lipid Res. 2008, 49, 1187–1194. [Google Scholar] [CrossRef] [Green Version]
- Cole, L.K.; Vance, J.E.; Vance, D.E. Phosphatidylcholine biosynthesis and lipoprotein metabolism. Biochim. Biophys. Acta 2012, 1821, 754–761. [Google Scholar] [CrossRef]
- Yao, Z.M.; Vance, D.E. The active synthesis of phosphatidylcholine is required for very low density lipoprotein secretion from rat hepatocytes. J. Biol. Chem. 1988, 263, 2998–3004. [Google Scholar] [CrossRef]
- Anderson, O.S.; Sant, K.E.; Dolinoy, D.C. Nutrition and epigenetics: An interplay of dietary methyl donors, one-carbon metabolism and DNA methylation. J. Nutr. Biochem. 2012, 23, 853–859. [Google Scholar] [CrossRef] [Green Version]
- Zeisel, S.H.; Blusztajn, J.K. Choline and Human Nutrition. Annu. Rev. Nutr. 1994, 14, 269–296. [Google Scholar] [CrossRef]
- Lever, M.; Slow, S. The clinical significance of betaine, an osmolyte with a key role in methyl group metabolism. Clin. Biochem. 2010, 43, 732–744. [Google Scholar] [CrossRef]
- Wiedeman, A.M.; Barr, S.I.; Green, T.J.; Xu, Z.; Innis, S.M.; Kitts, D.D. Dietary Choline Intake: Current State of Knowledge Across the Life Cycle. Nutrients 2018, 10, 1513. [Google Scholar] [CrossRef] [Green Version]
- Machado, M.V.; Michelotti, G.A.; Xie, G.; Almeida Pereira, T.; Boursier, J.; Bohnic, B.; Guy, C.D.; Diehl, A.M. Mouse models of diet-induced nonalcoholic steatohepatitis reproduce the heterogeneity of the human disease. PLoS ONE 2015, 10, e0127991. [Google Scholar] [CrossRef] [Green Version]
- Zeisel, S.H. People with fatty liver are more likely to have the PEMT rs7946 SNP, yet populations with the mutant allele do not have fatty liver. FASEB J. 2006, 20, 2181–2182. [Google Scholar] [CrossRef]
- Fischer, L.M.; daCosta, K.A.; Kwock, L.; Stewart, P.W.; Lu, T.-S.; Stabler, S.P.; Allen, R.H.; Zeisel, S.H. Sex and menopausal status influence human dietary requirements for the nutrient choline. Am. J. Clin. Nutr. 2007, 85, 1275–1285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Da Costa, K.-A.; Corbin, K.D.; Niculescu, M.D.; Galanko, J.A.; Zeisel, S.H. Identification of new genetic polymorphisms that alter the dietary requirement for choline and vary in their distribution across ethnic and racial groups. FASEB J. 2014, 28, 2970–2978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Waite, K.A.; Cabilio, N.R.; Vance, D.E. Choline deficiency-induced liver damage is reversible in Pemt−/− mice. J. Nutr. 2002, 132, 68–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; Xin, Y.; Li, J.; Chen, H.; Li, H. Phosphatidylethanolamine N-methyltransferase: From Functions to Diseases. Aging Dis. 2023, 14, 879–891. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, A.; Nash-Barboza, S.; Hinkis, S.; Caudill, M.A. Genetic Variants in Phosphatidylethanolamine N-methyltransferase and Methylenetetrahydrofolate Dehydrogenase Influence Biomarkers of Choline Metabolism When Folate Intake Is Restricted. J. Am. Diet. Assoc. 2009, 109, 313–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bale, G.; Vishnubhotla, R.V.; Mitnala, S.; Sharma, M.; Padaki, R.N.; Pawar, S.C.; Duvvur, R.N. Whole-Exome Sequencing Identifies a Variant in Phosphatidylethanolamine N-Methyltransferase Gene to be Associated With Lean-Nonalcoholic Fatty Liver Disease. J. Clin. Exp. Hepatol. 2019, 9, 561–568. [Google Scholar] [CrossRef]
- Dong, H.; Wang, J.; Li, C.; Hirose, A.; Nozaki, Y.; Takahashi, M.; Ono, M.; Akisawa, N.; Iwasaki, S.; Saibara, T.; et al. The phosphatidylethanolamine N-methyltransferase gene V175M single nucleotide polymorphism confers the susceptibility to NASH in Japanese population. J. Hepatol. 2007, 46, 915–920. [Google Scholar] [CrossRef]
- Resseguie, M.; Song, J.; Niculescu, M.D.; da Costa, K.-A.; Randall, T.A.; Zeisel, S.H. Phosphatidylethanolamine N-methyltransferase (PEMT) gene expression is induced by estrogen in human and mouse primary hepatocytes. FASEB J. 2007, 21, 2622–2632. [Google Scholar] [CrossRef] [Green Version]
- Walkey, C.J.; Yu, L.; Agellon, L.B.; Vance, D.E. Biochemical and evolutionary significance of phospholipid methylation. J. Biol. Chem. 1998, 273, 27043–27046. [Google Scholar] [CrossRef] [Green Version]
- Wan, S.; van der Veen, J.N.; Bakala N’Goma, J.-C.; Nelson, R.C.; Vance, D.E.; Jacobs, R.L. Hepatic PEMT activity mediates liver health, weight gain, and insulin resistance. FASEB J. 2019, 33, 10986–10995. [Google Scholar] [CrossRef] [Green Version]
- Jacobs, R.L.; Zhao, Y.; Koonen, D.P.Y.; Sletten, T.; Su, B.; Lingrell, S.; Cao, G.; Peake, D.A.; Kuo, M.-S.; Proctor, S.D.; et al. Impaired de novo choline synthesis explains why phosphatidylethanolamine N-methyltransferase-deficient mice are protected from diet-induced obesity. J. Biol. Chem. 2010, 285, 22403–22413. [Google Scholar] [CrossRef] [Green Version]
- Graif, M.; Yanuka, M.; Baraz, M.; Blank, A.; Moshkovitz, M.; Kessler, A.; Gilat, T.; Weiss, J.; Walach, E.; Amazeen, P.; et al. Quantitative estimation of attenuation in ultrasound video images: Correlation with histology in diffuse liver disease. Investig. Radiol. 2000, 35, 319–324. [Google Scholar] [CrossRef]
- Matthews, D.R.; Hosker, J.P.; Rudenski, A.S.; Naylor, B.A.; Treacher, D.F.; Turner, R.C. Homeostasis model assessment: Insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985, 28, 412–419. [Google Scholar] [CrossRef] [Green Version]
- Cheng, C.-P.; Chen, C.-H.; Kuo, C.-S.; Kuo, H.-T.; Huang, K.-T.; Shen, Y.-L.; Chang, C.-H.; Huang, R.F.S. Dietary choline and folate relationships with serum hepatic inflammatory injury markers in Taiwanese adults. Asia Pac. J. Clin. Nutr. 2017, 26, 642–649. [Google Scholar] [CrossRef]
- Ministry of Health and Welfare. Nutrition and Health Survey in Taiwan; Ministry of Health and Welfare: Taipei City, Taiwan, 2019.
- Chu, D.-M.; Wahlqvist, M.L.; Chang, H.-Y.; Yeh, N.-H.; Lee, M.-S. Choline and betaine food sources and intakes in Taiwanese. Asia Pac. J. Clin. Nutr. 2012, 21, 547–557. [Google Scholar]
- Patterson, K.Y.B.; Bhagwat, S.A.; Williams, J.R.; Howe, J.C.; Holden, J.M. USDA Database for the Choline Content of Common Foods: Release Two; U.S. Department of Agriculture: Beltsville, MD, USA, 2008.
- World Health Organization. Waist Circumference and Waist-Hip Ratio: Report of A WHO Expert Consultation; WHO: Geneva, Switzerland, 2008. [Google Scholar]
- Vance, D.E.; Ridgway, N.D. The methylation of phosphatidylethanolamine. Prog. Lipid Res. 1988, 27, 61–79. [Google Scholar] [CrossRef]
- Brown, C.C.; Kipnis, V.; Freedman, L.S.; Hartman, A.M.; Schatzkm, A.; Wacholder, S. Energy Adjustment Methods for Nutritional Epidemiology: The Effect of Categorization. Am. J. Epidemiol. 1994, 139, 323–338. [Google Scholar] [CrossRef] [Green Version]
- Gauthier, J.; Wu, Q.V.; Gooley, T.A. Cubic splines to model relationships between continuous variables and outcomes: A guide for clinicians. Bone Marrow Transplant. 2020, 55, 675–680. [Google Scholar] [CrossRef] [Green Version]
- Desquilbet, L.; Mariotti, F. Dose-response analyses using restricted cubic spline functions in public health research. Stat. Med. 2010, 29, 1037–1057. [Google Scholar] [CrossRef]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, 1220S–1228S. [Google Scholar] [CrossRef] [Green Version]
- Willett, W.; Stampfer, M.J. Total energy intake: Implications for epidemiologic analyses. Am. J. Epidemiol. 1986, 124, 17–27. [Google Scholar] [CrossRef] [PubMed]
- Piras, I.S.; Raju, A.; Don, J.; Schork, N.J.; Gerhard, G.S.; DiStefano, J.K. Hepatic PEMT Expression Decreases with Increasing NAFLD Severity. Int. J. Mol. Sci. 2022, 23, 9296. [Google Scholar] [CrossRef] [PubMed]
- Tan, H.-L.; Mohamed, R.; Mohamed, Z.; Zain, S.M. Phosphatidylethanolamine N-methyltransferase gene rs7946 polymorphism plays a role in risk of nonalcoholic fatty liver disease: Evidence from meta-analysis. Pharm. Genom. 2016, 26, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Romeo, S.; Cohen, J.C.; Hobbs, H.H. No association between polymorphism in PEMT (V175M) and hepatic triglyceride content in the Dallas Heart Study. FASEB J. 2006, 20, 2180. [Google Scholar] [CrossRef] [PubMed]
- Bauer, K.C.; Littlejohn, P.T.; Ayala, V.; Creus-Cuadros, A.; Finlay, B.B. Nonalcoholic Fatty Liver Disease and the Gut-Liver Axis: Exploring an Undernutrition Perspective. Gastroenterology 2022, 162, 1858–1875.e2. [Google Scholar] [CrossRef] [PubMed]
- Lyman, R.L.; Sheehan, G.; Tinoco, J. Diet and 14CH3-methionine incorporation into liver phosphatidylcholine fractions of male and female rats. Can. J. Biochem. 1971, 49, 71–79. [Google Scholar] [CrossRef]
- Shen, L.; Fan, J.-G.; Shao, Y.; Zeng, M.-D.; Wang, J.-R.; Luo, G.-H.; Li, J.-Q.; Chen, S.-Y. Prevalence of nonalcoholic fatty liver among administrative officers in Shanghai: An epidemiological survey. World J. Gastroenterol. 2003, 9, 1106–1110. [Google Scholar] [CrossRef]
- Zhu, X.; Song, J.; Mar, M.-H.; Edwards, L.J.; Zeisel, S.H. Phosphatidylethanolamine N-methyltransferase (PEMT) knockout mice have hepatic steatosis and abnormal hepatic choline metabolite concentrations despite ingesting a recommended dietary intake of choline. Biochem. J. 2003, 370, 987–993. [Google Scholar] [CrossRef]
- Tessitore, L.; Sesca, E.; Greco, M.; Pani, P.; Dianzani, M.U. Sexually differentiated response to choline in choline deficiency and ethionine intoxication. Int. J. Exp. Pathol. 1995, 76, 125–129. [Google Scholar]
- Ratsavong, K.; van Elsacker, T.; Doungvichit, D.; Siengsounthone, L.; Kounnavong, S.; Essink, D. Are dietary intake and nutritional status influenced by gender? The pattern of dietary intake in Lao PDR: A developing country. Nutr. J. 2020, 19, 31. [Google Scholar] [CrossRef] [Green Version]
- Zeisel, S.H. Choline: Critical role during fetal development and dietary requirements in adults. Annu. Rev. Nutr. 2006, 26, 229–250. [Google Scholar] [CrossRef] [Green Version]
- Vasconcellos, C.; Ferreira, O.; Lopes, M.F.; Ribeiro, A.F.; Vasques, J.; Guerreiro, C.S. Nutritional Genomics in Nonalcoholic Fatty Liver Disease. Biomedicines 2023, 11, 319. [Google Scholar] [CrossRef]
- Sulaiman, S.A.; Dorairaj, V.; Adrus, M.N.H. Genetic Polymorphisms and Diversity in Nonalcoholic Fatty Liver Disease (NAFLD): A Mini Review. Biomedicines 2023, 11, 106. [Google Scholar] [CrossRef]
- Guerrerio, A.L.; Colvin, R.M.; Schwartz, A.K.; Molleston, J.P.; Murray, K.F.; Diehl, A.; Mohan, P.; Schwimmer, J.B.; Lavine, J.E.; Torbenson, M.S.; et al. Choline intake in a large cohort of patients with nonalcoholic fatty liver disease. Am. J. Clin. Nutr. 2012, 95, 892–900. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, D.; Shu, X.-O.; Xiang, Y.-B.; Li, H.; Yang, G.; Gao, Y.-T.; Zheng, W.; Zhang, X. Higher Dietary Choline Intake Is Associated with Lower Risk of Nonalcoholic Fatty Liver in Normal-Weight Chinese Women. J. Nutr. 2014, 144, 2034–2040. [Google Scholar] [CrossRef] [Green Version]
- Dobrzyn, A.; Dobrzyn, P.; Miyazaki, M.; Sampath, H.; Chu, K.; Ntambi, J.M. Stearoyl-CoA Desaturase 1 Deficiency Increases CTP:Choline Cytidylyltransferase Translocation into the Membrane and Enhances Phosphatidylcholine Synthesis in Liver. J. Biol. Chem. 2005, 280, 23356–23362. [Google Scholar] [CrossRef] [Green Version]
- Theofilis, P.; Vordoni, A.; Kalaitzidis, R.G. Trimethylamine N-Oxide Levels in Non-Alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis. Metabolites 2022, 12, 1243. [Google Scholar] [CrossRef]
- Department of Health. Daily Reference Intakes, DRI. In DOH; ROC: Taipei City, Taiwan, 2011; Volume 2011. [Google Scholar]
- Food and Nutrition Board IOM. Dietary Reference Intakes: Thiamin, R., Niacin, Vitamin B6, Vitamin B12, Pantothenic Acid, Biotin, and Choline. In Food and Nutrition Board IOMNA; Food and Nutrition Board, Institute of Medicine National Academic, National Academy of Sciences: Washington, DC, USA, 1998. [Google Scholar]
- Wallace, T.C.; Blusztajn, J.K.; Caudill, M.A.; Klatt, K.C.; Natker, E.; Zeisel, S.H.; Zelman, K.M. Choline: The Underconsumed and Underappreciated Essential Nutrient. Nutr. Today 2018, 53, 240–253. [Google Scholar] [CrossRef]
- Dongiovanni, P.; Stender, S.; Pietrelli, A.; Mancina, R.M.; Cespiati, A.; Petta, S.; Pelusi, S.; Pingitore, P.; Badiali, S.; Maggioni, M.; et al. Causal relationship of hepatic fat with liver damage and insulin resistance in nonalcoholic fatty liver. J. Intern. Med. 2018, 283, 356–370. [Google Scholar] [CrossRef] [Green Version]
- Da Costa, K.-A.; Kozyreva, O.G.; Song, J.; Galanko, J.A.; Fischer, L.M.; Zeisel, S.H. Common genetic polymorphisms affect the human requirement for the nutrient choline. FASEB J. 2006, 20, 1336–1344. [Google Scholar] [CrossRef] [Green Version]
- Bianco, C.; Tavaglione, F.; Romeo, S.; Valenti, L. Genetic risk scores and personalization of care in fatty liver disease. Curr. Opin. Pharmacol. 2021, 61, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Hennein, R.; Liu, C.; Long, M.T.; Hoffmann, U.; Jacques, P.F.; Lichtenstein, A.H.; Hu, F.B.; Levy, D. Improved diet quality associates with reduction in liver fat, particularly in individuals with high genetic risk scores for nonalcoholic fatty liver disease. Gastroenterology 2018, 155, 107–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Ibrahim, A.A.; Jackson, R.T. Healthy eating index versus alternate healthy index in relation to diabetes status and health markers in US adults: NHANES 2007–2010. Nutr. J. 2019, 18, 26. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.H.; Chang, T.-Y.; Huang, R.-F.S. Relationship Between PEMT Gene rs7946 Polymorphism and Nutritional Choline Status in Association With Nonalcoholic Fatty Liver Risk. Curr. Dev. Nutr. 2022, 6, 1128. [Google Scholar] [CrossRef]
- Hernaez, R.; Lazo, M.; Bonekamp, S.; Kamel, I.; Brancati, F.L.; Guallar, E.; Clark, J.M. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: A meta-analysis. Hepatology 2011, 54, 1082–1090. [Google Scholar] [CrossRef] [Green Version]

| Characteristics | GG | GA | AA | GG vs. GA | GG vs. AA | GG vs. GA/AA | p for Trend |
|---|---|---|---|---|---|---|---|
| Women (n = 113) | 68 (60.2) | 31 (27.4) | 14 (12.4) | p-Value | p-Value | p-Value | |
| n (%) | 68 (60.2) | 31 (27.4) | 14 (12.4) | ||||
| Age, yrs | 64 (56–69) | 59 (56–67) | 60.5 (56.8–66.0) | 0.233 | 0.234 | 0.135 | 0.155 |
| BMI, kg/m2 | 24.9 (22.6–28.0) | 23.6 (22.2–26.5) | 22.4 (19.6–25.3) | 0.123 | 0.047 | 0.032 | 0.020 |
| Hepatic steatosis | 42 (61.8) | 14 (45.2) | 4 (28.6) | 0.122 | 0.023 | 0.023 | 0.013 |
| Obesity * | 54 (79.5) | 24 (77.4) | 8 (57.1) | 0.822 | 0.077 | 0.311 | 0.127 |
| Cholesterol (mg/dL) | 199 (172–224) | 196 (183–231) | 209 (173–244) | 0.544 | 0.618 | 0.478 | 0.467 |
| Triglycerides (md/dL) | 98.5 (62.3–138) | 112 (77–156) | 83 (57.5–125) | 0.264 | 0.562 | 0.554 | 0.784 |
| HDL (mg/dL) | 51 (42.3–62.0) | 48 (42–60) | 60.5 (50.5–78.3) | 0.841 | 0.016 | 0.321 | 0.138 |
| AST (U/L) | 26 (21.0–32.8) | 24 (21–32) | 26 (19.0–37.0) | 0.528 | 0.81 | 0.545 | 0.593 |
| ALT (U/L) | 27 (19.0–42.8) | 21 (18–38) | 24 (17.3–40.5) | 0.210 | 0.426 | 0.176 | 0.204 |
| HOMA-IR | 2.78 (1.97–4.05) | 2.36 (1.77–3.53) | 2.13 (1.71–2.81) | 0.346 | 0.156 | 0.159 | 0.159 |
| Choline, μmol/L | 10.5 (9.03–12.8) | 10.7 (9.38–13.1) | 10.3 (9.33–11.9) | 0.870 | 0.699 | 0.955 | 0.883 |
| Plasma Hcy, μmol/L | 9.18 (7.66–11.3) | 9.45 (7.06–12.2) | 8.56 (6.24–12.6) | 0.877 | 0.382 | 0.591 | 0.532 |
| Energy, kcal | 1320 (1105–1864) | 1348 (1115–1623) | 1569 (1037–2140) | 0.411 | 0.605 | 0.694 | 0.905 |
| Folate, μg | 647 (465–935) | 761 (568–1110) | 492 (341–1070) | 0.880 | 0.355 | 0.376 | 0.69 |
| Betaine, mg | 215 (151–318) | 250 (191–395) | 227 (160–322) | 0.085 | 0.786 | 0.143 | 0.229 |
| Choline intake, mg | 468 (383–557) | 499 (394–638) | 414 (342–541) | 0.419 | 0.388 | 0.828 | 0.909 |
| Men (n = 137) | |||||||
| n | 87 (63.5) | 38 (27.7) | 12 (8.8) | ||||
| Age, yrs | 59 (49–65) | 62.5 (48.5–68.0) | 60.5 (54.0–68.0) | 0.317 | 0.306 | 0.207 | 0.186 |
| BMI, kg/m2 | 27.2 (23.8–30.8) | 25.8 (22.8–28.2) | 24.2 (22.6–26.8) | 0.102 | 0.020 | 0.020 | 0.011 |
| Hepatic steatosis | 66 (75.9) | 24 (63.2) | 2 (16.7) | 0.146 | <0.001 | 0.004 | <0.001 |
| Obesity | 63 (72.4) | 18 (47.4) | 6 (50.0) | 0.007 | 0.113 | 0.004 | <0.011 |
| Cholesterol (mg/dL) | 193 (165–210) | 181 (166–200) | 199 (157–226) | 0.153 | 0.772 | 0.284 | 0.381 |
| Triglycerides (md/dL) | 105 (71.0–165) | 91.5 (62.8–146) | 82.5 (62.8–120) | 0.288 | 0.214 | 0.100 | 0.127 |
| HDL (mg/dL) | 41.0 (35.0–48.0) | 45.0 (39.5–51.0) | 46.5 (37.8–62.3) | 0.217 | 0.109 | 0.088 | 0.065 |
| AST (U/L) | 26 (21–36) | 25 (18–36) | 25 (20.5–33.0) | 0.207 | 0.679 | 0.221 | 0.252 |
| ALT (U/L) | 32 (22–52) | 24.5 (19.0–57.3) | 22.5 (18.5–37.8) | 0.168 | 0.189 | 0.090 | 0.085 |
| HOMA-IR | 3.23 (2.14–5.42) | 2.74 (2.04–4.25) | 2.53 (2.13–2.77) | 0.158 | 0.118 | 0.067 | 0.054 |
| Choline, μmol/L | 13.1 (10.9–15.5) | 12.3 (10.4–14.9) | 10.9 (10.8–14.6) | 0.316 | 0.336 | 0.217 | 0.196 |
| Plasma Hcy, μmol/L | 12.7 (10.5–15.2) | 12.7 (10.6–15.2) | 12.7 (11.3–17.2) | 0.788 | 0.447 | 0.589 | 0.476 |
| Energy, kcal | 1819 (1337–2174) | 1750 (1411–2174) | 1637 (1365–2168) | 0.797 | 0.94 | 0.806 | 0.813 |
| Folate, μg | 577 (416–810) | 476 (362–746) | 460 (320–859) | 0.127 | 0.319 | 0.092 | 0.099 |
| Betaine, mg | 206 (144–307) | 181 (133–235) | 297 (119–349) | 0.106 | 0.855 | 0.204 | 0.288 |
| Total choline, mg | 475 (395–577) | 462 (342–519) | 382 (323–447) | 0.308 | 0.015 | 0.062 | 0.036 |
| Choline Intake | Tertile 1 | Tertile 2 | Tertile 3 | p-Value | p-Trend |
|---|---|---|---|---|---|
| Female, PEMT rs7946 GG (n = 68) | |||||
| Choline, mg/day | 213–420 | 420–533 | 533–914 | ||
| Number | 23 | 23 | 22 | ||
| NAFLD | 19 (82.6) | 10 (43.5) | 13 (59.1) | 0.023 | 0.101 |
| Obesity * | 21 (91.3) | 16 (69.6) | 17 (77.3) | 0.181 | 0.241 |
| Female, PEMT rs7946 GA/AA (n = 45) | |||||
| Choline, mg/day | 170–404 | 404–528 | 528–982 | ||
| Number | 15 | 15 | 15 | ||
| NAFLD | 6 (40.0) | 7 (46.7) | 5 (33.3) | 0.757 | 0.712 |
| Obesity * | 10 (66.7) | 12 (80.0) | 10 (66.7) | 0.649 | 1 |
| Male, PEMT rs7946 GG (n = 87) | |||||
| Choline, mg/day | 219–418 | 418–506 | 506–865 | ||
| Number | 29 | 29 | 29 | ||
| NAFLD | 18 (62.1) | 24 (82.8) | 24 (82.8) | 0.104 | 0.067 |
| Obesity * | 11 (37.9) | 5 (17.2) | 5 (17.2) | ||
| Male, PEMT rs7946 GA/AA (n = 68) | |||||
| Choline, mg/day | 134–369 | 369–473 | 473–867 | ||
| Number | 17 | 16 | 17 | ||
| NAFLD | 10 (58.8) | 7 (43.8) | 9 (52.9) | 0.684 | 0.734 |
| Obesity * | 8 (47.1) | 9 (56.2) | 7 (41.2) | 0.684 | 0.734 |
| PEMT rs7946 | PEMT GG | PEMT GA/AA | PEMT GG | PEMT GA/AA | |
|---|---|---|---|---|---|
| Female | |||||
| Intake, mg/day | Choline < 448 | Choline < 448 | Choline > 448 | Choline > 448 | |
| HS (n) | 24 | 8 | 18 | 10 | |
| Control (n) | 7 | 12 | 19 | 15 | |
| Odds Ratio (95% CI) Ref | p-int | ||||
| Model 0 | 1 | 0.194 (0.057–0.664) | 0.276 (0.096–0.798) | 0.194 (0.061–0.621) | 0.115 |
| Model I | 1 | 0.125 (0.027–0.584) | 0.177 (0.048–0.658) | 0.113 (0.026–0.494) | 0.233 |
| Model II | 1 | 0.154 (0.032–0.755) | 0.193 (0.050–0.739) | 0.124 (0.027–0.558) | 0.263 |
| Model III | 1 | 0.191 (0.038–0.970) | 0.210 (0.054–0.819) | 0.136 (0.029–0.627) | 0.343 |
| Male | |||||
| Intake, mg/day | Choline < 424 | Choline < 424 | Choline > 424 | Choline > 424 | |
| HS (n) | 18 | 12 | 48 | 14 | |
| Control (n) | 12 | 12 | 9 | 12 | |
| Odds Ratio (95% CI) Ref | p-int | ||||
| Model 0 | 1 | 0.667 (0.226–1.970) | 3.556 (1.282–9.860) | 0.778 (0.269–2.250) | 0.124 |
| Model I | 1 | 1.246 (0.343–4.534) | 3.778 (1.190–11.994) | 0.799 (0.225–2.837) | 0.230 |
| Model II | 1 | 0.959 (0.229–4.017) | 3.094 (0.833–11.490) | 0.534 (0.127–2.252) | 0.161 |
| Model III | 1 | 0.719 (0.163–3.166) | 2.017 (0.508–8.006) | 0.456 (0.103–2.029) | 0.309 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, C.-H.; Chang, T.-Y.; Chen, Y.-C.; Huang, R.-F.S. PEMT rs7946 Polymorphism and Sex Modify the Effect of Adequate Dietary Choline Intake on the Risk of Hepatic Steatosis in Older Patients with Metabolic Disorders. Nutrients 2023, 15, 3211. https://doi.org/10.3390/nu15143211
Wu C-H, Chang T-Y, Chen Y-C, Huang R-FS. PEMT rs7946 Polymorphism and Sex Modify the Effect of Adequate Dietary Choline Intake on the Risk of Hepatic Steatosis in Older Patients with Metabolic Disorders. Nutrients. 2023; 15(14):3211. https://doi.org/10.3390/nu15143211
Chicago/Turabian StyleWu, Chien-Hsien, Ting-Yu Chang, Yen-Chu Chen, and Rwei-Fen S. Huang. 2023. "PEMT rs7946 Polymorphism and Sex Modify the Effect of Adequate Dietary Choline Intake on the Risk of Hepatic Steatosis in Older Patients with Metabolic Disorders" Nutrients 15, no. 14: 3211. https://doi.org/10.3390/nu15143211
APA StyleWu, C.-H., Chang, T.-Y., Chen, Y.-C., & Huang, R.-F. S. (2023). PEMT rs7946 Polymorphism and Sex Modify the Effect of Adequate Dietary Choline Intake on the Risk of Hepatic Steatosis in Older Patients with Metabolic Disorders. Nutrients, 15(14), 3211. https://doi.org/10.3390/nu15143211





