Extrauterine Growth Restriction and Optimal Growth of Very Preterm Neonates: State of the Art
Abstract
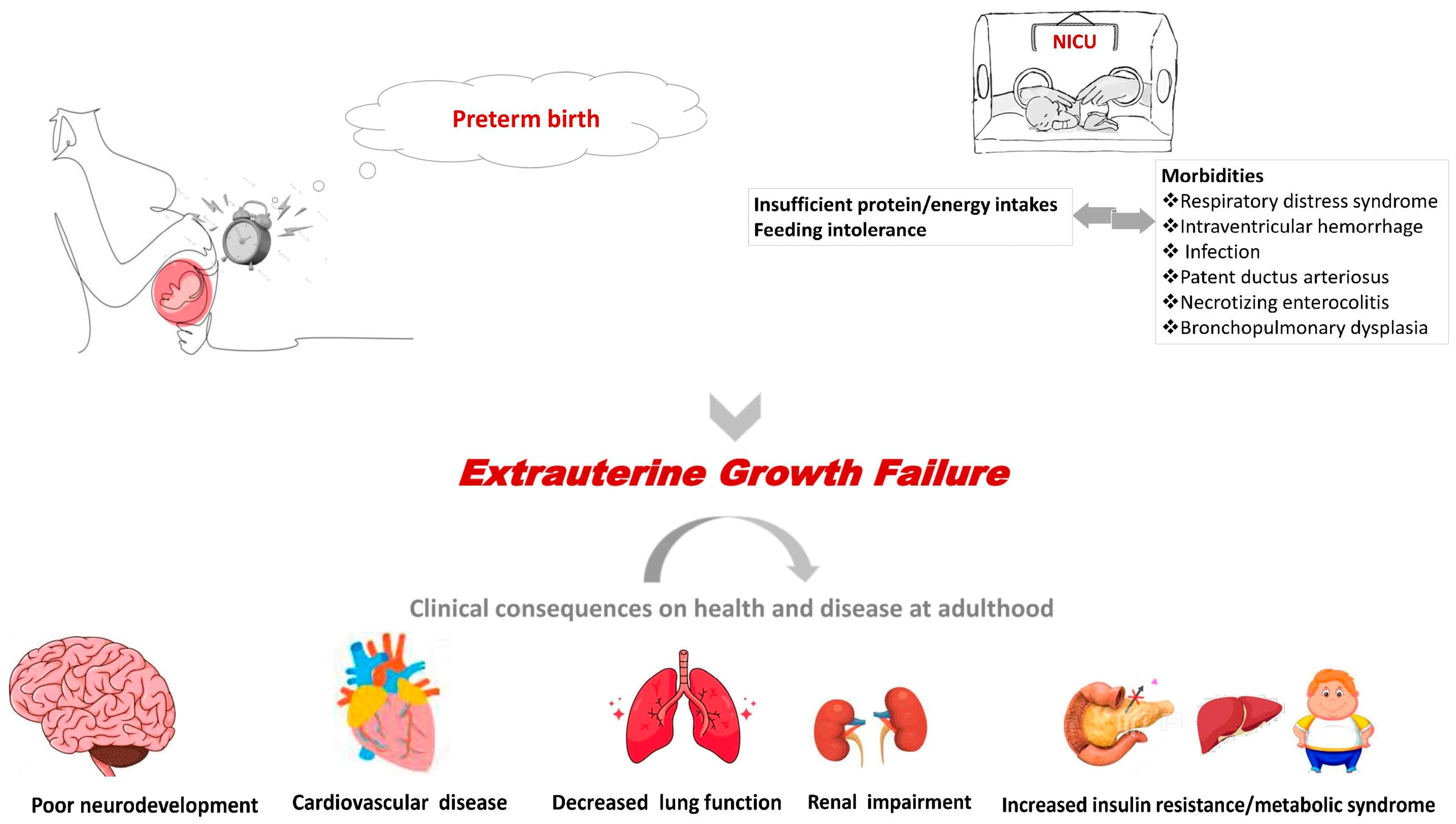
:1. Introduction
2. Feeding Policies Pre-2000 and Effect on VPN Growth and Prognosis
3. The Effect of Early “Aggressive” Feeding Strategies Post-2000
4. Factors Influencing Nutritional Supply and Growth of Preterm Infants
4.1. Breast Milk Fortification
4.2. VPN with Major Morbidities and Growth
5. Feeding Policies and Reducing the Percentage of VPN with EGR
6. And Now What: Current and Future Demands
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fenton, T.R.; Cormack, B.; Goldberg, D.; Nasser, R.; Alshaikh, B.; Eliasziw, M.; Hay, W.W.; Hoyos, A.; Anderson, D.; Bloomfield, F.; et al. “Extrauterine growth restriction” and “postnatal growth failure” are misnomers for preterm infants. J. Perinatol. Off. J. Calif. Perinat. Assoc. 2020, 40, 704–714. [Google Scholar] [CrossRef] [PubMed]
- Greenbury, S.F.; Angelini, E.D.; Ougham, K.; Battersby, C.; Gale, C.; Uthaya, S.; Modi, N. Birthweight and patterns of postnatal weight gain in very and extremely preterm babies in England and Wales, 2008–2019: A cohort study. Lancet Child Adolesc. Health 2021, 5, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Andrews, E.T.; Ashton, J.J.; Pearson, F.; Beattie, R.M.; Johnson, M.J. Early postnatal growth failure in preterm infants is not inevitable. Arch. Dis. Child. Fetal Neonatal 2019, 104, F235–F241. [Google Scholar] [CrossRef] [PubMed]
- McKinley, L.T.; Przystac, L.; Tucker, R.; Trail-Burns, E.; Vohr, B.R.; Laptook, A.R.; Bliss, J.M. Implementation of a Nutrition Care Bundle and Improved Weight Gain of Extremely Preterm Infants to 36 Weeks Postmenstrual Age. J. Pediatr. 2022, 241, 42–47.e2. [Google Scholar] [CrossRef]
- Wilson-Costello, D.; Friedman, H.; Minich, N.; Fanaroff, A.A.; Hack, M. Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics 2005, 115, 997–1003. [Google Scholar] [CrossRef]
- Lemons, J.A.; Bauer, C.R.; Oh, W.; Korones, S.B.; Papile, L.A.; Stoll, B.J.; Verter, J.; Temprosa, M.; Wright, L.L.; Ehrenkranz, R.A.; et al. Very low birth weight outcomes of the National Institute of Child health and human development neonatal research network, January 1995 through December 1996. NICHD Neonatal Research Network. Pediatrics 2001, 107, E1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barker, D.J.; Eriksson, J.G.; Forsén, T.; Osmond, C. Fetal origins of adult disease: Strength of effects and biological basis. Int. J. Epidemiol. 2002, 31, 1235–1239. [Google Scholar] [CrossRef] [Green Version]
- Sipola-Leppänen, M.; Vääräsmäki, M.; Tikanmäki, M.; Matinolli, H.M.; Miettola, S.; Hovi, P.; Wehkalampi, K.; Ruokonen, A.; Sundvall, J.; Pouta, A.; et al. Cardiometabolic risk factors in young adults who were born preterm. Am. J. Epidemiol. 2015, 181, 861–873. [Google Scholar] [CrossRef] [Green Version]
- Franz, A.R.; Pohlandt, F.; Bode, H.; Mihatsch, W.A.; Sander, S.; Kron, M.; Steinmacher, J. Intrauterine, early neonatal, and postdischarge growth and neurodevelopmental outcome at 5.4 years in extremely preterm infants after intensive neonatal nutritional support. Pediatrics 2009, 123, e101–e109. [Google Scholar] [CrossRef] [Green Version]
- Vohr, B.R.; Wright, L.L.; Dusick, A.M.; Mele, L.; Verter, J.; Steichen, J.J.; Simon, N.P.; Wilson, D.C.; Broyles, S.; Bauer, C.R.; et al. Neurodevelopmental and functional outcomes of extremely low birth weight infants in the National Institute of Child Health and Human Development Neonatal Research Network, 1993–1994. Pediatrics 2000, 105, 1216–1226. [Google Scholar] [CrossRef] [Green Version]
- Zozaya, C.; Díaz, C.; Saenz de Pipaón, M. How Should We Define Postnatal Growth Restriction in Preterm Infants? Neonatology 2018, 114, 177–180. [Google Scholar] [CrossRef]
- Sammallahti, S.; Pyhälä, R.; Lahti, M.; Lahti, J.; Pesonen, A.K.; Heinonen, K.; Hovi, P.; Eriksson, J.G.; Strang-Karlsson, S.; Andersson, S.; et al. Infant growth after preterm birth and neurocognitive abilities in young adulthood. J. Pediatr. 2014, 165, 1109–1115.e3. [Google Scholar] [CrossRef] [PubMed]
- Crump, C.; Groves, A.; Sundquist, J.; Sundquist, K. Association of Preterm Birth with Long-term Risk of Heart Failure into Adulthood. JAMA Pediatr. 2021, 175, 689–697. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, E.E.; Thureen, P.J.; Carlson, S.J. Aggressive nutrition of the very low birthweight infant. Clin. Perinatol. 2002, 29, 225–244. [Google Scholar] [CrossRef] [PubMed]
- Horbar, J.D.; Ehrenkranz, R.A.; Badger, G.J.; Edwards, E.M.; Morrow, K.A.; Soll, R.F.; Buzas, J.S.; Bertino, E.; Gagliardi, L.; Bellù, R. Weight Growth Velocity and Postnatal Growth Failure in Infants 501 to 1500 Grams: 2000–2013. Pediatrics 2015, 136, e84–e92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El Rafei, R.; Jarreau, P.-H.; Norman, M.; Maier, R.F.; Barros, H.; Van Reempts, P.; Pedersen, P.; Cuttini, M.; Zeitlin, J. Variation in very preterm extrauterine growth in a European multicountry cohort. Arch. Dis. Child. Fetal Neonatal 2021, 106, 316. [Google Scholar] [CrossRef]
- Embleton, N.E.; Pang, N.; Cooke, R.J. Postnatal malnutrition and growth retardation: An inevitable consequence of current recommendations in preterm infants? Pediatrics 2001, 107, 270–273. [Google Scholar] [CrossRef]
- Martínez-Jiménez, M.D.; Gómez-García, F.J.; Gil-Campos, M.; Pérez-Navero, J.L. Comorbidities in childhood associated with extrauterine growth restriction in preterm infants: A scoping review. Eur. J. Pediatr. 2020, 179, 1255–1265. [Google Scholar] [CrossRef]
- Ehrenkranz, R.A.; Dusick, A.M.; Vohr, B.R.; Wright, L.L.; Wrage, L.A.; Poole, W.K. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics 2006, 117, 1253–1261. [Google Scholar] [CrossRef] [Green Version]
- Belfort, M.B.; Rifas-Shiman, S.L.; Sullivan, T.; Collins, C.T.; McPhee, A.J.; Ryan, P.; Kleinman, K.P.; Gillman, M.W.; Gibson, R.A.; Makrides, M. Infant growth before and after term: Effects on neurodevelopment in preterm infants. Pediatrics 2011, 128, e899–e906. [Google Scholar] [CrossRef]
- Ordóñez-Díaz, M.D.; Pérez-Navero, J.L.; Flores-Rojas, K.; Olza-Meneses, J.; Muñoz-Villanueva, M.C.; Aguilera-García, C.M.; Gil-Campos, M. Prematurity with Extrauterine Growth Restriction Increases the Risk of Higher Levels of Glucose, Low-Grade of Inflammation and Hypertension in Prepubertal Children. Front. Pediatr. 2020, 8, 180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schneider, J.; Fischer Fumeaux, C.J.; Duerden, E.G.; Guo, T.; Foong, J.; Graz, M.B.; Hagmann, P.; Chakravarty, M.M.; Hüppi, P.S.; Beauport, L.; et al. Nutrient Intake in the First Two Weeks of Life and Brain Growth in Preterm Neonates. Pediatrics 2018, 141, e20172169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Groene, S.G.; Stegmeijer, K.J.J.; Tan, R.; Steggerda, S.J.; Haak, M.C.; Slaghekke, F.; Roest, A.A.W.; Heijmans, B.T.; Lopriore, E.; van Klink, J.M.M. Long-term effects of selective fetal growth restriction (LEMON): A cohort study of neurodevelopmental outcome in growth discordant identical twins in the Netherlands. Lancet. Child Adolesc. Health 2022, 6, 624–632. [Google Scholar] [CrossRef]
- Sériès, T.; Guillot, M.; Angoa, G.; Pronovost, E.; Ndiaye, A.; Mohamed, I.; Simonyan, D.; Lavoie, P.M.; Synnes, A.; Marc, I. Does Growth Velocity Affect Associations Between Birth Weight and Neurodevelopment for Infants Born Very Preterm? J. Pediatr. 2023, 260, 113531. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.; Tang, Q.; Wang, Y.; Wu, J.; Ruan, H.; Lu, L.; Tao, Y.; Cai, W. Analysis of Nutrition Support in Very Low-Birth-Weight Infants with Extrauterine Growth Restriction. Nutr. Clin. Pract. Off. Publ. Am. Soc. Parenter. Enter. Nutr. 2019, 34, 436–443. [Google Scholar] [CrossRef] [Green Version]
- Brennan, A.M.; Fenton, S.; Murphy, B.P.; Kiely, M.E. Transition Phase Nutrition Recommendations: A Missing Link in the Nutrition Management of Preterm Infants. JPEN J. Parenter. Enter. Nutr. 2018, 42, 343–351. [Google Scholar] [CrossRef]
- Wang, N.; Zhang, J.; Wang, B.; Yu, Z.; Zhang, J.; Qu, L.; Tang, B. Relationship between nutrient intakes in the transition phase and postnatal growth of preterm infants: A systematic review. Ital. J. Pediatr. 2023, 49, 13. [Google Scholar] [CrossRef]
- Greenbury, S.F.; Ougham, K.; Wu, J.; Battersby, C.; Gale, C.; Modi, N.; Angelini, E.D. Identification of variation in nutritional practice in neonatal units in England and association with clinical outcomes using agnostic machine learning. Sci. Rep. 2021, 11, 7178. [Google Scholar] [CrossRef]
- Mills, L.; Coulter, L.; Savage, E.; Modi, N. Macronutrient content of donor milk from a regional human milk bank: Variation with donor mother-infant characteristics. Br. J. Nutr. 2019, 122, 1155–1167. [Google Scholar] [CrossRef] [Green Version]
- Brown, J.V.; Embleton, N.D.; Harding, J.E.; McGuire, W. Multi-nutrient fortification of human milk for preterm infants. Cochrane Database Syst. Rev. 2016, 5, CD000343. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Liu, X.; Modi, N.; Uthaya, S. Impact of breast milk intake on body composition at term in very preterm babies: Secondary analysis of the Nutritional Evaluation and Optimisation in Neonates randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. 2019, 104, F306–F312. [Google Scholar] [CrossRef]
- Perrin, T.; Pradat, P.; Larcade, J.; Masclef-Imbert, M.; Pastor-Diez, B.; Picaud, J.C. Postnatal growth and body composition in extremely low birth weight infants fed with individually adjusted fortified human milk: A cohort study. Eur. J. Pediatr. 2023, 182, 1143–1154. [Google Scholar] [CrossRef]
- Embleton, N.D.; Sproat, T.; Uthaya, S.; Young, G.R.; Garg, S.; Vasu, V.; Masi, A.C.; Beck, L.; Modi, N.; Stewart, C.J.; et al. Effect of an Exclusive Human Milk Diet on the Gut Microbiome in Preterm Infants: A Randomized Clinical Trial. JAMA Netw. Open 2023, 6, e231165. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.V.; Lin, L.; Embleton, N.D.; Harding, J.E.; McGuire, W. Multi-nutrient fortification of human milk for preterm infants. Cochrane Database Syst. Rev. 2020, 6, CD000343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arslanoglu, S.; Boquien, C.Y.; King, C.; Lamireau, D.; Tonetto, P.; Barnett, D.; Bertino, E.; Gaya, A.; Gebauer, C.; Grovslien, A.; et al. Fortification of Human Milk for Preterm Infants: Update and Recommendations of the European Milk Bank Association (EMBA) Working Group on Human Milk Fortification. Front. Pediatr. 2019, 7, 76. [Google Scholar] [CrossRef] [PubMed]
- Milanesi, B.G.; Lima, P.A.; Villela, L.D.; Martins, A.S.; Gomes-Junior, S.C.S.; Moreira, M.E.L.; Méio, M. Assessment of early nutritional intake in preterm infants with bronchopulmonary dysplasia: A cohort study. Eur. J. Pediatr. 2021, 180, 1423–1430. [Google Scholar] [CrossRef]
- Ehrenkranz, R.A.; Das, A.; Wrage, L.A.; Poindexter, B.B.; Higgins, R.D.; Stoll, B.J.; Oh, W.; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Early Nutrition Mediates the Influence of Severity of Illness on Extremely LBW Infants. Pediatr. Res. 2011, 69, 522–529. [Google Scholar] [CrossRef] [Green Version]
- Panagiotounakou, P.; Sokou, R.; Gounari, E.; Konstantinidi, A.; Antonogeorgos, G.; Grivea, I.N.; Daniil, Z.; Gourgouliannis, K.I.; Gounaris, A. Very preterm neonates receiving “aggressive” nutrition and early nCPAP had similar long-term respiratory outcomes as term neonates. Pediatr. Res. 2019, 86, 742–748. [Google Scholar] [CrossRef]
- Groene, S.G.; Spekman, J.A.; Te Pas, A.B.; Heijmans, B.T.; Haak, M.C.; van Klink, J.M.M.; Roest, A.A.W.; Lopriore, E. Respiratory distress syndrome and bronchopulmonary dysplasia after fetal growth restriction: Lessons from a natural experiment in identical twins. EClinicalMedicine 2021, 32, 100725. [Google Scholar] [CrossRef]
- Gounaris, A.K.; Sokou, R.; Gounari, E.; Panagiotounakou, P.; Grivea, I.N. Post-natal growth of very preterm neonates. Lancet. Child Adolesc. Health 2022, 6, e9–e10. [Google Scholar] [CrossRef] [PubMed]
- Stevens, T.P.; Shields, E.; Campbell, D.; Combs, A.; Horgan, M.; La Gamma, E.F.; Xiong, K.; Kacica, M. Statewide Initiative to Reduce Postnatal Growth Restriction among Infants <31 Weeks of Gestation. J. Pediatr. 2018, 197, 82–89.e2. [Google Scholar] [CrossRef] [PubMed]
- Travers, C.P.; Wang, T.; Salas, A.A.; Schofield, E.; Dills, M.; Laney, D.; Yee, A.; Bhatia, A.; Winter, L.; Ambalavanan, N.; et al. Higher- or Usual-Volume Feedings in Infants Born Very Preterm: A Randomized Clinical Trial. J. Pediatr. 2020, 224, 66–71.e1. [Google Scholar] [CrossRef] [PubMed]
- Gounaris, A.; Sokou, R.; Theodoraki, M.; Gounari, E.; Panagiotounakou, P.; Antonogeorgos, G.; Ioakeimidis, G.; Parastatidou, S.; Konstantinidi, A.; Grivea, I.N. “Aggressive” Feeding of Very Preterm Neonates and Body Mass Index at School Age. Nutrients 2021, 13, 1901. [Google Scholar] [CrossRef] [PubMed]
- Klingenberg, C.; Muraas, F.K.; Isaksen, C.E.; Nilsen, T.; Torgersen, M.; Melum-Hansen, C. Growth and neurodevelopment in very preterm infants receiving a high enteral volume-feeding regimen–A population-based cohort study. J. Matern. Neonatal Med. 2019, 32, 1664–1672. [Google Scholar] [CrossRef]
- Kosmeri, C.; Giapros, V.; Gounaris, A.; Sokou, R.; Siomou, E.; Rallis, D.; Makis, A.; Baltogianni, M. Are the current feeding volumes adequate for the growth of very preterm neonates? Br. J. Nutr. 2023, 1–5. [Google Scholar] [CrossRef]
- Rossholt, M.E.; Bratlie, M.; Wendel, K.; Aas, M.F.; Gunnarsdottir, G.; Fugelseth, D.; Stiris, T.; Domellöf, M.; Størdal, K.; Moltu, S.J. A standardized feeding protocol ensured recommended nutrient intakes and prevented growth faltering in preterm infants <29 weeks gestation. Clin. Nutr. ESPEN 2023, 53, 251–259. [Google Scholar] [CrossRef]
- Moltu, S.J.; Bronsky, J.; Embleton, N.; Gerasimidis, K.; Indrio, F.; Köglmeier, J.; de Koning, B.; Lapillonne, A.; Norsa, L.; Verduci, E.; et al. Nutritional Management of the Critically Ill Neonate: A Position Paper of the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2021, 73, 274–289. [Google Scholar] [CrossRef]
- Embleton, N.D.; Moltu, S.J.; Lapillonne, A.; van den Akker, C.H.P.; Carnielli, V.; Fusch, C.; Gerasimidis, K.; van Goudoever, J.B.; Haiden, N.; Iacobelli, S.; et al. Enteral Nutrition in Preterm Infants (2022): A Position Paper from the ESPGHAN Committee on Nutrition and Invited Experts. J. Pediatr. Gastroenterol. Nutr. 2023, 76, 248–268. [Google Scholar] [CrossRef]
- Agostoni, C.; Buonocore, G.; Carnielli, V.P.; De Curtis, M.; Darmaun, D.; Decsi, T.; Domellöf, M.; Embleton, N.D.; Fusch, C.; Genzel-Boroviczeny, O.; et al. Enteral nutrient supply for preterm infants: Commentary from the European Society of Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 85–91. [Google Scholar] [CrossRef]
- Shah, P.S.; Wong, K.Y.; Merko, S.; Bishara, R.; Dunn, M.; Asztalos, E.; Darling, P.B. Postnatal growth failure in preterm infants: Ascertainment and relation to long-term outcome. J. Perinat. Med. 2006, 34, 484–489. [Google Scholar] [CrossRef]
- Rochow, N.; Raja, P.; Liu, K.; Fenton, T.; Landau-Crangle, E.; Göttler, S.; Jahn, A.; Lee, S.; Seigel, S.; Campbell, D.; et al. Physiological adjustment to postnatal growth trajectories in healthy preterm infants. Pediatr. Res. 2016, 79, 870–879. [Google Scholar] [CrossRef] [PubMed]
| Energy/Macronutrient | ESPGHAN 2022 Recommendations for Enteral Nutrient Intake; Embleton [48] | Energy/Nutrient Requirements in Critically Ill Neonates; Moltu [47] | |||
|---|---|---|---|---|---|
| Early Acute | Late Acute | Recovery | |||
| Energy (kcal/kg /day) | 115–140 (160) | Enteral | 40–55 | 70–95 | 110–160 |
| Parenteral | 40–55 | 60–80 | 90–120 | ||
| Fluid, mL/kg/d | 135–200 (>200) | _ | _ | _ | _ |
| Glucose (g/kg/d) | 11–15 | Enteral | 5–8 | 7–11 | 11–15 (18) |
| Parenteral | 5–8 (10) | 7–10 (12) | 11–14 (17) | ||
| Protein (g/kg/ day) * | 3.5–4.0 (4.5) | Enteral | 1.0–2.0 | 2.0–3.0 | 3.5–4.5 |
| Parenteral | 1.0–2.0 | 2.0–3.0 | 2.5–3.5 | ||
| Lipids (g/kg/ day) | 4.8–8.1 | Enteral | 2.0–3.0 | 3.0–6.0 | 5.0–8.0 |
| Parenteral | 1.0–2.0 | 2.0–3.0 | 3.0–4.0 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gounaris, A.K.; Sokou, R.; Gounari, E.A.; Panagiotounakou, P.; Grivea, I.N. Extrauterine Growth Restriction and Optimal Growth of Very Preterm Neonates: State of the Art. Nutrients 2023, 15, 3231. https://doi.org/10.3390/nu15143231
Gounaris AK, Sokou R, Gounari EA, Panagiotounakou P, Grivea IN. Extrauterine Growth Restriction and Optimal Growth of Very Preterm Neonates: State of the Art. Nutrients. 2023; 15(14):3231. https://doi.org/10.3390/nu15143231
Chicago/Turabian StyleGounaris, Antonios K., Rozeta Sokou, Eleni A. Gounari, Polytimi Panagiotounakou, and Ioanna N. Grivea. 2023. "Extrauterine Growth Restriction and Optimal Growth of Very Preterm Neonates: State of the Art" Nutrients 15, no. 14: 3231. https://doi.org/10.3390/nu15143231
APA StyleGounaris, A. K., Sokou, R., Gounari, E. A., Panagiotounakou, P., & Grivea, I. N. (2023). Extrauterine Growth Restriction and Optimal Growth of Very Preterm Neonates: State of the Art. Nutrients, 15(14), 3231. https://doi.org/10.3390/nu15143231







