High Prevalence of Energy and Nutrients Inadequacy among Brazilian Older Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
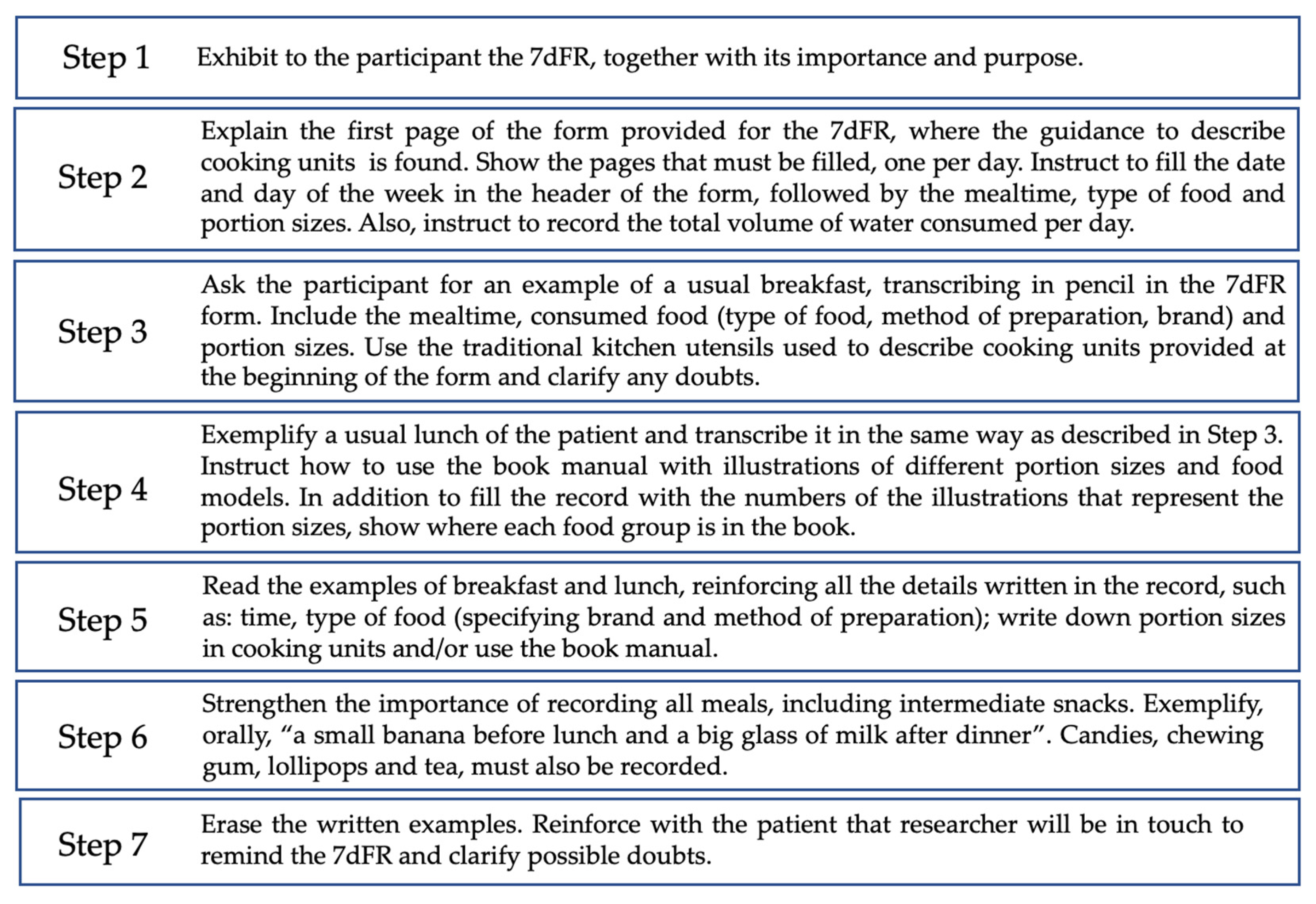
2.2. Dietary Assessment
- Culinary preparations, such as pies, cakes, and soups, were recorded in detail, with an indication of the ingredient used and the method of preparation.
- Processed and ultra-processed foods [23] were recorded, including the name and brand of the product.
- Information regarding the addition of salt, sugar, oil, and sauces was recorded, as well as information on the consumption of whole or peeled fruits and vegetables; and diet and/or light food or beverage products.
- Participants were asked to specify the type of juice (natural or bottled), type of milk (whole, reduced fat, low fat), type of bread and cereals (whole grain or refined grain), and type of meat (ex: chicken breast, beef chuck, pork rib).
- Participants received phone calls on alternating days to remind them of the 7dFR and to clarify any doubts.
Nutrients Intake and Prevalence of Inadequacy
2.3. Anthropometric Measurements
2.4. Diagnosis of Sarcopenia
Muscle Mass, Strength, and Performance
2.5. Statistical Analysis
3. Results
3.1. Participants’ Descriptive Data
3.2. Nutrients Intake and Prevalence of Inadequacy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Ageing. Available online: https://www.who.int/health-topics/ageing (accessed on 29 May 2023).
- Saraiva, M.D.; Rangel, L.F.; Cunha, J.L.L.; Rotta, T.C.A.; Douradinho, C.; Khazaal, E.J.B.; Aliberti, M.J.R.; Avelino-Silva, T.J.; Apolinario, D.; Suemoto, C.K.; et al. Prospective GERiatric Observational (ProGERO) Study: Cohort Design and Preliminary Results. BMC Geriatr. 2020, 20, 427. [Google Scholar] [CrossRef] [PubMed]
- Instituto Brasileiro de Geografia e Estatística. Síntese de Indicadores Sociais. Uma Análise das Condições de Vida da População Brasileira. 2020. Available online: https://biblioteca.ibge.gov.br/visualizacao/livros/liv101760.pdf (accessed on 27 June 2023).
- Ciosak, S.I.; Braz, E.; Costa, M.F.B.N.A.; Nakano, N.G.R.; Rodrigues, J.; Alencar, R.A.; Rocha, A.C.A.L. da Senescência e senilidade: Novo paradigma na atenção básica de saúde. Rev. Esc. Enferm. USP 2011, 45, 1763–1768. [Google Scholar] [CrossRef] [Green Version]
- Ceccon, R.F.; Vieira, L.J.E.D.S.; Brasil, C.C.P.; Soares, K.G.; Portes, V.D.M.; Garcia Júnior, C.A.S.; Schneider, I.J.C.; Carioca, A.A.F. Envelhecimento e dependência no Brasil: Características sociodemográficas e assistenciais de idosos e cuidadores. Ciência Saúde Coletiva 2021, 26, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Furman, D.; Campisi, J.; Verdin, E.; Carrera-Bastos, P.; Targ, S.; Franceschi, C.; Ferrucci, L.; Gilroy, D.W.; Fasano, A.; Miller, G.W.; et al. Chronic Inflammation in the Etiology of Disease across the Life Span. Nat. Med. 2019, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Trombetti, A.; Reid, K.F.; Hars, M.; Herrmann, F.R.; Pasha, E.; Phillips, E.M.; Fielding, R.A. Age-Associated Declines in Muscle Mass, Strength, Power, and Physical Performance: Impact on Fear of Falling and Quality of Life. Osteoporos. Int. 2016, 27, 463–471. [Google Scholar] [CrossRef] [Green Version]
- Ponti, F.; Santoro, A.; Mercatelli, D.; Gasperini, C.; Conte, M.; Martucci, M.; Sangiorgi, L.; Franceschi, C.; Bazzocchi, A. Aging and Imaging Assessment of Body Composition: From Fat to Facts. Front. Endocrinol. 2020, 10, 861. [Google Scholar] [CrossRef] [Green Version]
- Abbatecola, A.M.; Russo, M.; Barbieri, M. Dietary Patterns and Cognition in Older Persons. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 10–13. [Google Scholar] [CrossRef]
- Pinto de Souza Fernandes, D.; Duarte, M.S.L.; Pessoa, M.C.; Franceschini, S.d.C.C.; Ribeiro, A.Q. Evaluation of Diet Quality of the Elderly and Associated Factors. Arch. Gerontol. Geriatr. 2017, 72, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Jyväkorpi, S.K.; Pitkälä, K.H.; Puranen, T.M.; Björkman, M.P.; Kautiainen, H.; Strandberg, T.E.; Soini, H.H.; Suominen, M.H. High Proportions of Older People with Normal Nutritional Status Have Poor Protein Intake and Low Diet Quality. Arch. Gerontol. Geriatr. 2016, 67, 40–45. [Google Scholar] [CrossRef] [Green Version]
- Keller, H.H.; Carrier, N.; Slaughter, S.E.; Lengyel, C.; Steele, C.M.; Duizer, L.; Morrison, J.; Brown, K.S.; Chaudhury, H.; Yoon, M.N.; et al. Prevalence and Determinants of Poor Food Intake of Residents Living in Long-Term Care. J. Am. Med. Dir. Assoc. 2017, 18, 941–947. [Google Scholar] [CrossRef] [Green Version]
- Koponen, S.; Nykänen, I.; Savela, R.-M.; Välimäki, T.; Suominen, A.L.; Schwab, U. Inadequate Intake of Energy and Nutrients Is Common in Older Family Caregivers. Nutrients 2021, 13, 2763. [Google Scholar] [CrossRef]
- O’Connell, M.L.; Coppinger, T.; Lacey, S.; Arsenic, T.; McCarthy, A.L. The Nutritional Status and Dietary Intake of Free-Living Seniors: A Cross-Sectional Study. Clin. Nutr. ESPEN 2021, 43, 478–486. [Google Scholar] [CrossRef]
- Liu, Z.; Zhao, L.; Man, Q.; Wang, J.; Zhao, W.; Zhang, J. Dietary Micronutrients Intake Status among Chinese Elderly People Living at Home: Data from CNNHS 2010–2012. Nutrients 2019, 11, 1787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Instituto Brasileiro de Geografia e Estatística; Diretoria de Pesquisas. Coordenação de Trabalho e Rendimento Pesquisa de Orçamentos Familiares 2008–2009: Análise Do Consumo Alimentar Pessoal No Brasil. Available online: https://biblioteca.ibge.gov.br/index.php/biblioteca-catalogo?view=detalhes&id=250063 (accessed on 29 May 2023).
- Instituto Brasileiro de Geografia e Estatística; Diretoria de Pesquisas. Coordenação de Trabalho e Rendimento Pesquisa de Orçamentos Familiares: 2017–2018: Análise Do Consumo Alimentar Pessoal No Brasil/IBGE, Coordenação de Trabalho e Rendimento. Available online: https://biblioteca.ibge.gov.br/index.php/biblioteca-catalogo?view=detalhes&id=2101742 (accessed on 29 May 2023).
- Verly Junior, E.; Marchioni, D.M.; Araujo, M.C.; Carli, E.D.; Oliveira, D.C.R.S.D.; Yokoo, E.M.; Sichieri, R.; Pereira, R.A. Evolution of Energy and Nutrient Intake in Brazil between 2008–2009 and 2017–2018. Rev. Saude Publica 2021, 55, 5s. [Google Scholar] [CrossRef]
- Guligowska, A.; Pigłowska, M.; Fife, E.; Kostka, J.; Sołtysik, B.K.; Kroc, Ł.; Kostka, T. Inappropriate Nutrients Intake Is Associated with Lower Functional Status and Inferior Quality of Life in Older Adults with Depression. Clin. Interv. Aging 2016, 11, 1505–1517. [Google Scholar] [CrossRef] [Green Version]
- Volkert, D.; Schrader, E. Dietary assessment methods for older persons: What is the best approach? Curr. Opin. Clin. Nutr. Metab. Care 2013, 16, 534–540. [Google Scholar] [CrossRef]
- Fisberg, R.M.; Marchioni, D.M.L.; Colucci, A.C.A. Avaliação do consumo alimentar e da ingestão de nutrientes na prática clínica. Arq. Bras. Endocrinol. Metabol. 2009, 53, 617–624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro, J.P.; Chiarello, P. Consumo Alimentar: Visualizando Porções; Guanabara Koogan: Rio de Janeiro, Brazil, 2007. [Google Scholar]
- Monteiro, C.A.; Cannon, G.; Levy, R.B.; Moubarac, J.-C.; Louzada, M.L.; Rauber, F.; Khandpur, N.; Cediel, G.; Neri, D.; Martinez-Steele, E.; et al. Ultra-Processed Foods: What They Are and How to Identify Them. Public Health Nutr. 2019, 22, 936–941. [Google Scholar] [CrossRef] [PubMed]
- TACO. Tabela Brasileira de Composição de Alimentos, 4th ed.; NEPA UNICAMP: Campinas, Brazil, 2011. [Google Scholar]
- Philippi, S.T. Table of Food Composition: Nutritional Support for Decision, 2nd ed.; Coronário: São Paulo, Brazil, 2002. [Google Scholar]
- Pinheiro, A.B. Tabela Para Avaliação de Consumo Alimentar Em Medidas Caseiras, 5th ed.; Atheneu: Rio de Janeiro, Brazil, 2004. [Google Scholar]
- Institute of Medicine (U.S.); Food Forum. Nutrition Concerns for Aging Populations. In Providing Healthy and Safe Foods as We Age: Workshop Summary; National Academies Press: Cambridge, MA, USA, 2010. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements; National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.C.; et al. ESPEN Guideline on Clinical Nutrition and Hydration in Geriatrics. Clin. Nutr. 2019, 38, 10–47. [Google Scholar] [CrossRef] [Green Version]
- Lipschitz, D.A. Screening for nutritional status in the elderly. Prim. Care 1994, 21, 55–67. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, K.V.; Hsu, T.H.; Wu, W.T.; Huang, K.C.; Han, D.S. Is sarcopenia associated with depression? A systematic review and meta-analysis of observational studies. Age Ageing 2017, 46, 738–746. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeung, S.S.Y.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.M.; Maier, A.B. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500. [Google Scholar] [CrossRef] [Green Version]
- Beaudart, C.; Zaaria, M.; Pasleau, F.; Reginster, J.Y.; Bruyère, O. Health Outcomes of Sarcopenia: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0169548. [Google Scholar] [CrossRef] [Green Version]
- Wongpakaran, N.; Wongpakaran, T.; Sirirak, T.; Jenraumjit, R.; Jiraniramai, S.; Lerttrakarnnon, P. Predictors of polypharmacy among elderly Thais with depressive and anxiety disorders: Findings from the DAS study. BMC Geriatr. 2018, 18, 309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tefera, Y.G.; Alemayehu, M.; Mekonnen, G.B. Prevalence and determinants of polypharmacy in cardiovascular patients attending outpatient clinic in Ethiopia University Hospital. PLoS ONE 2020, 15, e0234000. [Google Scholar] [CrossRef]
- Beaudart, C.; Locquet, M.; Touvier, M.; Reginster, J.-Y.; Bruyère, O. Association between dietary nutrient intake and sarcopenia in the SarcoPhAge study. Aging Clin. Exp. Res. 2019, 31, 815–824. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, M.; Becker, W.; Michaëlsson, K.; Cederholm, T.; Sjögren, P. Associations between dietary patterns at age 71 and the prevalence of sarcopenia 16 years later. Clin. Nutr. 2019, 39, 1077–1084. [Google Scholar] [CrossRef]
- Isanejad, M.; Mursu, J.; Sirola, J.; Kröger, H.; Rikkonen, T.; Tuppurainen, M.; Erkkilä, A.T. Dietary protein intake is associated with better physical function and muscle strength among elderly women. Br. J. Nutr. 2016, 115, 1281–1291. [Google Scholar] [CrossRef] [Green Version]
- Alexandre, T.S.; Duarte, Y.A.; Santos, J.L.; Wong, R.; Lebrão, M.L. Prevalence and associated factors of sarcopenia among elderly in Brazil: Findings from the SABE Study. J. Nutr. Health Aging 2014, 18, 284–290. [Google Scholar] [CrossRef]
- Gonçalves, T.J.M.; Horie, L.M.; Bailer, M.C.; Barbosa-Silva, T.G.; Barrére, A.P.N.; Barreto, P.A.; Campos, L.F.; de Campos, G.C.; Castro, M.G.; Celano, R.M.G.; et al. Diretriz Braspen De Terapia Nutricional No Envelhecimento. Braspen J. 2019, 34 (Suppl. S3), 2–58. [Google Scholar]
- Stover, P.J.; Garza, C.; Durga, J.; Field, M.S. Emerging Concepts in Nutrient Needs. J. Nutr. 2020, 150, 2593S–2601S. [Google Scholar] [CrossRef] [PubMed]
- Martini, L.A.; Verly, E.; Marchioni, D.M.L.; Fisberg, R.M. Prevalence and Correlates of Calcium and Vitamin D Status Adequacy in Adolescents, Adults, and Elderly from the Health Survey-São Paulo. Nutrition 2013, 29, 845–850. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, E.; Miller, M.; Yaxley, A.; Isenring, E. Malnutrition in the Elderly: A Narrative Review. Maturitas 2013, 76, 296–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coelho-Júnior, H.J.; Rodrigues, B.; Uchida, M.; Marzetti, E. Low Protein Intake Is Associated with Frailty in Older Adults: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2018, 10, 1334. [Google Scholar] [CrossRef] [Green Version]
- Suidasari, S.; Uragami, S.; Yanaka, N.; Kato, N. Dietary vitamin B6 modulates the gene expression of myokines, Nrf2-related factors, myogenin and HSP60 in the skeletal muscle of rats. Exp. Ther. Med. 2017, 14, 3239–3246. [Google Scholar] [CrossRef] [Green Version]
- Struijk, E.A.; Lana, A.; Guallar-Castillón, P.; Rodríguez-Artalejo, F.; Lopez-Garcia, E. Intake of B vitamins and impairment in physical function in older adults. Clin. Nutr. 2018, 37, 1271–1278. [Google Scholar] [CrossRef]
- Behrouzi, P.; Grootswagers, P.; Keizer, P.L.; Smeets, E.T.; Feskens, E.J.; de Groot, L.C.; Van Eeuwijk, F.A. Dietary Intakes of Vegetable Protein, Folate, and Vitamins B-6 and B-12 Are Partially Correlated with Physical Functioning of Dutch Older Adults Using Copula Graphical Models. J. Nutr. 2020, 150, 634–643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ter Borg, S.; de Groot, L.C.; Mijnarends, D.M.; de Vries, J.H.; Verlaan, S.; Meijboom, S.; Luiking, Y.C.; Schols, J.M. Differences in Nutrient Intake and Biochemical Nutrient Status Between Sarcopenic and Nonsarcopenic Older Adults-Results from the Maastricht Sarcopenia Study. J. Am. Med. Dir. Assoc. 2016, 17, 393–401. [Google Scholar] [CrossRef] [Green Version]
- Lengelé, L.; Moehlinger, P.; Bruyère, O.; Locquet, M.; Reginster, J.Y.; Beaudart, C. Association between Changes in Nutrient Intake and Changes in Muscle Strength and Physical Performance in the SarcoPhAge Cohort. Nutrients 2020, 12, 3485. [Google Scholar] [CrossRef]
- Rathnayake, N.; Alwis, G.; Lenora, J.; Lekamwasam, S. Factors associated with measures of sarcopenia in pre and postmenopausal women. BMC Womens Health 2021, 21, 5. [Google Scholar] [CrossRef]
- Alhussain, M.H.; Alkahtani, S.; Aljuhani, O.; Habib, S.S. Effects of Nutrient Intake on Diagnostic Measures of Sarcopenia among Arab Men: A Cross-Sectional Study. Nutrients 2020, 13, 114. [Google Scholar] [CrossRef]
- Bhattacharya, S.; Bhadra, R.; Schols, A.M.W.J.; van Helvoort, A.; Sambashivaiah, S. Nutrition in the prevention and management of sarcopenia—A special focus on Asian Indians. Osteoporos. Sarcopenia 2022, 8, 135–144. [Google Scholar] [CrossRef]
- Shoemaker, M.E.; Salmon, O.F.; Smith, C.M.; Duarte-Gardea, M.O.; Cramer, J.T. Influences of Vitamin D and Iron Status on Skeletal Muscle Health: A Narrative Review. Nutrients 2022, 14, 2717. [Google Scholar] [CrossRef]
- van Dronkelaar, C.; van Velzen, A.; Abdelrazek, M.; van der Steen, A.; Weijs, P.J.M.; Tieland, M. Minerals and Sarcopenia; The Role of Calcium, Iron, Magnesium, Phosphorus, Potassium, Selenium, Sodium, and Zinc on Muscle Mass, Muscle Strength, and Physical Performance in Older Adults: A Systematic Review. J. Am. Med. Dir. Assoc. 2018, 19, 6–11.e3. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.D.; Guo, J. Obesity Energetics: Body Weight Regulation and the Effects of Diet Composition. Gastroenterology 2017, 152, 1718–1727.e3. [Google Scholar] [CrossRef] [Green Version]
- Venter, C.; Meyer, R.W.; Greenhawt, M.; Pali-Schöll, I.; Nwaru, B.; Roduit, C.; Untersmayr, E.; Adel-Patient, K.; Agache, I.; Agostoni, C.; et al. Role of Dietary Fiber in Promoting Immune Health—An EAACI Position Paper. Allergy 2022, 77, 3185–3198. [Google Scholar] [CrossRef] [PubMed]
- McKeown, N.M.; Fahey, G.C.; Slavin, J.; van der Kamp, J.-W. Fibre Intake for Optimal Health: How Can Healthcare Professionals Support People to Reach Dietary Recommendations? BMJ 2022, 378, e054370. [Google Scholar] [CrossRef] [PubMed]
- Frampton, J.; Murphy, K.G.; Frost, G.; Chambers, E.S. Higher dietary fibre intake is associated with increased skeletal muscle mass and strength in adults aged 40 years and older. J. Cachexia Sarcopenia Muscle 2021, 12, 2134–2144. [Google Scholar] [CrossRef] [PubMed]
- Heuberger, R.A.; Caudell, K. Polypharmacy and nutritional status in older adults: A cross-sectional study. Drugs Aging 2011, 28, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef] [Green Version]
- Gana, W.; De Luca, A.; Debacq, C.; Poitau, F.; Poupin, P.; Aidoud, A.; Fougère, B. Analysis of the Impact of Selected Vitamins Deficiencies on the Risk of Disability in Older People. Nutrients 2021, 13, 3163. [Google Scholar] [CrossRef]
- Kupisz-Urbańska, M.; Płudowski, P.; Marcinowska-Suchowierska, E. Vitamin D Deficiency in Older Patients—Problems of Sarcopenia, Drug Interactions, Management in Deficiency. Nutrients 2021, 13, 1247. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, L.J.; Farruggia, M.; Veronese, N.; Barbagallo, M. Vitamin D Sources, Metabolism, and Deficiency: Available Compounds and Guidelines for Its Treatment. Metabolites 2021, 11, 255. [Google Scholar] [CrossRef] [PubMed]
- Jun, S.; Cowan, A.E.; Bhadra, A.; Dodd, K.W.; Dwyer, J.T.; Eicher-Miller, H.A.; Gahche, J.J.; Guenther, P.M.; Potischman, N.; Tooze, J.A.; et al. Older Adults with Obesity Have Higher Risks of Some Micronutrient Inadequacies and Lower Overall Dietary Quality Compared to Peers with a Healthy Weight, National Health and Nutrition Examination Surveys (NHANES), 2011–2014. Public Health Nutr. 2020, 23, 2268–2279. [Google Scholar] [CrossRef] [PubMed]
- Meydani, S.N.; Lewis, E.D.; Wu, D. Perspective: Should Vitamin E Recommendations for Older Adults Be Increased? Adv. Nutr. 2018, 9, 533–543. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Luo, J.; Xiao, Z.; Wu, W.; Liang, X.; Ding, S.; Zhao, Q.; Zhao, X.; Wang, Y.; Ding, D. Low Dietary Vitamin E Intake Is Associated with High Risk of Incident Dementia among Older Adults: The Shanghai Aging Study. Front. Nutr. 2022, 9, 1036795. [Google Scholar] [CrossRef]
- La Fata, G.; Weber, P.; Mohajeri, M.H. Effects of Vitamin E on Cognitive Performance during Ageing and in Alzheimer’s Disease. Nutrients 2014, 6, 5453–5472. [Google Scholar] [CrossRef] [Green Version]
- Kjeldby, I.K.; Fosnes, G.S.; Ligaarden, S.C.; Farup, P.G. Vitamin B6 Deficiency and Diseases in Elderly People—A Study in Nursing Homes. BMC Geriatr. 2013, 13, 13. [Google Scholar] [CrossRef] [Green Version]
- Grootswagers, P.; Mensink, M.; Berendsen, A.A.M.; Deen, C.P.J.; Kema, I.P.; Bakker, S.J.L.; Santoro, A.; Franceschi, C.; Meunier, N.; Malpuech-Brugère, C.; et al. Vitamin B-6 Intake Is Related to Physical Performance in European Older Adults: Results of the New Dietary Strategies Addressing the Specific Needs of the Elderly Population for Healthy Aging in Europe (NU-AGE) Study. Am. J. Clin. Nutr. 2021, 113, 781–789. [Google Scholar] [CrossRef]
- Nalder, L.; Zheng, B.; Chiandet, G.; Middleton, L.T.; de Jager, C.A. Vitamin B12 and Folate Status in Cognitively Healthy Older Adults and Associations with Cognitive Performance. J. Nutr. Health Aging 2021, 25, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Azzini, E.; Raguzzini, A.; Polito, A. A Brief Review on Vitamin B12 Deficiency Looking at Some Case Study Reports in Adults. Int. J. Mol. Sci. 2021, 22, 9694. [Google Scholar] [CrossRef] [PubMed]
- Beto, J.A. The Role of Calcium in Human Aging. Clin. Nutr. Res. 2015, 4, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Veldurthy, V.; Wei, R.; Oz, L.; Dhawan, P.; Jeon, Y.H.; Christakos, S. Vitamin D, Calcium Homeostasis and Aging. Bone Res. 2016, 4, 16041. [Google Scholar] [CrossRef] [Green Version]
- Alehagen, U.; Opstad, T.B.; Alexander, J.; Larsson, A.; Aaseth, J. Impact of Selenium on Biomarkers and Clinical Aspects Related to Ageing. A Review. Biomolecules 2021, 11, 1478. [Google Scholar] [CrossRef]
- Arredondo, M.; González, M.; Latorre, M. Copper. In Trace Elements and Minerals in Health and Longevity; Malavolta, M., Mocchegiani, E., Eds.; Healthy Ageing and Longevity; Springer International Publishing: Cham, Switzerland, 2018; pp. 35–62. ISBN 978-3-030-03742-0. [Google Scholar]
- Nascimento, C.Q.d.; Barros-Neto, J.A.; Vieira, N.F.L.; Menezes-Filho, J.A.; Neves, S.J.F.; Lima, S.O. Selenium Concentrations in Elderly People with Alzheimer’s Disease: A Cross-Sectional Study with Control Group. Rev. Bras. Enferm. 2021, 74, e20200984. [Google Scholar] [CrossRef]
- Lin, Z.; Gao, H.; Wang, B.; Wang, Y. Dietary Copper Intake and Its Association with Telomere Length: A Population Based Study. Front. Endocrinol. 2018, 9, 404. [Google Scholar] [CrossRef] [Green Version]
- Barbagallo, M.; Veronese, N.; Dominguez, L.J. Magnesium in Aging, Health and Diseases. Nutrients 2021, 13, 463. [Google Scholar] [CrossRef]
- Bahmanpour, S. Guideline: Potassium Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Rodríguez-Rodríguez, E.; Ortega, R.M.; Andrés Carvajales, P.; González-Rodríguez, L.G. Relationship between 24 h Urinary Potassium and Diet Quality in the Adult Spanish Population. Public Health Nutr. 2015, 18, 850–859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Souza, L.B.de.; Martins, K.A.; Bomfim, R.A. Inadequate distribution of dietary protein and muscle mass in older adults. Geriatr. Gerontol. Aging 2022, 16, 1–8. [Google Scholar] [CrossRef]
- Silva, G.M.d.; Assumpção, D.d.; Barros, M.B.d.A.; Barros Filho, A.d.A.; Corona, L.P. Low intake of dietary fibers among the elderly: 2014/2015 ISACAMP population-based study. Cien. Saude Colet. 2021, 26, 3865–3874. [Google Scholar] [CrossRef] [PubMed]
- Mello, A.V.d.; Pereira, J.L.; Leme, A.C.B.; Goldbaum, M.; Cesar, C.L.G.; Fisberg, R.M. Social Determinants, Lifestyle and Diet Quality: A Population-Based Study from the 2015 Health Survey of São Paulo, Brazil. Public Health Nutr. 2020, 23, 1766–1777. [Google Scholar] [CrossRef]
- Cruz-Góngora, V.D.l.; Martínez-Tapia, B.; Cuevas-Nasu, L.; Flores-Aldana, M.; Shamah-Levy, T. Dietary Intake and Adequacy of Energy and Nutrients in Mexican Older Adults: Results from Two National Health and Nutrition Surveys. Salud Pública México 2017, 59, 285–298. [Google Scholar] [CrossRef] [PubMed]
- Roman Viñas, B.; Ribas Barba, L.; Ngo, J.; Gurinovic, M.; Novakovic, R.; Cavelaars, A.; de Groot, L.C.P.G.M.; van’t Veer, P.; Matthys, C.; Serra Majem, L. Projected Prevalence of Inadequate Nutrient Intakes in Europe. Ann. Nutr. Metab. 2011, 59, 84–95. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total (n = 295) |
|---|---|
| Age, years | 70.41 ± 7.48 |
| Gender, n (%) | |
| Female | 241 (81.69) |
| Male | 54 (18.31) |
| Nutritional classification 1 n (%) | |
| Underweight | 31 (10.51%) |
| Eutrophic | 123 (41.69%) |
| Overweight | 141 (47.80%) |
| Muscle outcomes 2 | |
| SMM, kg 3 | 16.43 ± 4.58 |
| ASMI, kg/m2 4 | 6.59 ± 1.60 |
| HGS, kgf 5 | 16.90 ± 7.00 |
| Walking speed, m/s | 1.16 ± 0.35 |
| EWGSOP2 6, n (%) | |
| Sarcopenic | 65 (22.03) |
| Non-sarcopenic | 230 (77.97) |
| Comorbidities, n (%) | |
| No comorbidities | 16 (5.42%) |
| 1 comorbidity | 50 (16.95%) |
| 2 comorbidities | 72 (24.41%) |
| 3 comorbidities | 56 (18.98%) |
| 4 comorbidities | 47 (15.93%) |
| ≥5 comorbidities | 54 (18.31%) |
| Medications 7, n (%) | |
| no medications | 29 (9.83%) |
| 1 medication | 45 (15.25%) |
| 2 medications | 38 (12.88%) |
| 3 medications | 30 (10.17%) |
| ≥4 medications | 153 (51.86%) |
| Nutrients | Mean ± SD 1 | Median (Q25–Q75) 2 | Prevalence of Inadequacy (%) |
|---|---|---|---|
| Energy (kcal) | 1401.31 ± 452.01 | 1359.15 (1089.07–1634.00) | 96.94 |
| Carbohydrates (g) | 181.30 ± 30.73 | 181.57 (162.09–199.21) | |
| Carbohydrates (%) | 56.71 ± 18.80 | 54.47 (43.15–67.37) | |
| Protein (g/kg) | 58.02 ± 12.60 | 58.81 (51.31–66.13) | 69.15 |
| Protein (%) | 18.40 ± 7.19 | 17.46 (13.45–22.47) | |
| Fat (g) | 41.32 ± 9.57 | 41.97 (36.07–46.97) | |
| Fat (%) | 29.37 ± 11.33 | 28.66 (21.85–35.61) | |
| Dietary fiber (g) | 12.54 ± 4.30 | 11.98 (9.59–14.78) | 97.33 |
| Vitamin A (ug) | 766.35 ± 862.76 | 535.28 (328.4–908.94) | 48.52 |
| Vitamin B1 (mg) | 1.12 ± 0.63 | 0.97 (0.81–1.22) | 11.53 |
| Vitamin B2 (mg) | 0.86 ± 0.39 | 0.80 (0.60–1.05) | 34.91 |
| Vitamin B3 (mg) | 13.53 ± 4.48 | 12.83 (10.67–16.35) | 34.31 |
| Vitamin B6 (mg) | 0.97 ± 0.38 | 0.90 (0.70–1.21) | 77.81 |
| Vitamin B12 (ug) | 3.00 ± 7.05 | 1.28 (0.69–2.34) | 70.41 |
| Vitamin D (ug) | 1.71 ± 7.13 | 0.45 (0.28–0.78) | 95.26 |
| Vitamin E (mg) | 8.22 ± 3.39 | 7.66 (6.02–9.89) | 83.43 |
| Copper (ug) | 4.63 ± 34.76 | 0.67 (0.56–0.82) | 100.00 |
| Phosphorus (mg) | 560.71 ± 149.45 | 542.93 (468.42–655.03) | 56.50 |
| Magnesium (mg) | 134.43 ± 35.44 | 133.66 (110.21–156.35) | 99.11 |
| Potassium (g) | 1466.10 ± 406.43 | 1432.96 (1182.75–1725.03) | 98.22 |
| Selenium (ug) | 46.68 ± 34.09 | 40.81 (30.37–51.96) | 58.28 |
| Zinc (mg) | 6.56 ± 3.74 | 5.97 (4.34–7.70) | 30.47 |
| Calcium (mg) | 460.18 ± 180.04 | 433.02 (317.30–567.37) | 98.81 |
| Iron (mg) | 11.36 ± 14.86 | 9.01 (7.57–10.76) | 23.07 |
| Nutrients | Category | Underweight | Eutrophic | Overweight | p-Value 1 |
|---|---|---|---|---|---|
| Energy (kcal) | Inadequacy | 27 (87.1%) | 122 (99.2%) | 141 (100.0%) | 0.000 |
| Adequacy | 4 (12.9%) | 2 (0.8%) | 0 (0.0%) | ||
| Protein (g/kg) | Inadequacy | 25 (80.6%) | 66 (53.7%) | 117 (83.0%) | 0.000 |
| Adequacy | 6 (19.4%) | 57 (46.3%) | 24 (17.0%) | ||
| Dietary fiber (g) | Inadequacy | 27 (87.1%) | 119 (96.7%) | 140 (99.3%) | 0.005 |
| Adequacy | 4 (12.9%) | 4 (3.3%) | 1 (0.7%) | ||
| Vitamin A (ug) | Inadequacy | 11 (35.5%) | 57 (46.3%) | 71 (50.4%) | 0.318 |
| Adequacy | 20 (64.5%) | 66 (53.7%) | 70 (49.6%) | ||
| Vitamin B1 (mg) | Inadequacy | 4 (12.9%) | 18 (14.6%) | 16 (11.3%) | 0.720 |
| Adequacy | 27 (87.1%) | 105 (85.4%) | 125 (88.7%) | ||
| Vitamin B2 (mg) | Inadequacy | 9 (29.0%) | 40 (32.5%) | 49 (34.8%) | 0.833 |
| Adequacy | 22 (71.0%) | 83 (67.5%) | 92 (65.2%) | ||
| Vitamin B3 (mg) | Inadequacy | 9 (29.0%) | 37 (30.1%) | 51 (36.2%) | 0.547 |
| Adequacy | 22 (71.0%) | 86 (69.9%) | 90 (63.8%) | ||
| Vitamin B6 (mg) | Inadequacy | 21 (67.7%) | 89 (72.4%) | 115 (81.6%) | 0.091 |
| Adequacy | 10 (32.3%) | 34 (27.6%) | 26 (18.4%) | ||
| Vitamin B12 (ug) | Inadequacy | 23 (74.2%) | 85 (69.1%) | 101 (71.6%) | 0.837 |
| Adequacy | 8 (25.8%) | 38 (30.9%) | 40 (28.4%) | ||
| Vitamin D (ug) | Inadequacy | 29 (93.5%) | 122 (99.2%) | 132 (93.6%) | 0.028 |
| Adequacy | 2 (6.5%) | 1 (0.8%) | 9 (6.4%) | ||
| Vitamin E (mg) | Inadequacy | 26 (83.9%) | 99 (80.5%) | 118 (83.7%) | 0.776 |
| Adequacy | 5 (16.1%) | 24 (19.5%) | 23 (16.3%) | ||
| Copper (ug) | Inadequacy | 31 (100.0%) | 123 (100.0%) | 141 (100.0%) | NA 2 |
| Adequacy | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| Phosphorus (mg) | Inadequacy | 17 (54.8%) | 65 (52.8%) | 81 (57.4%) | 0.754 |
| Adequacy | 14 (45.2%) | 58 (47.2%) | 60 (42.6%) | ||
| Magnesium (mg) | Inadequacy | 30 (96.8%) | 121 (98.4%) | 141 (100.0%) | 0.085 |
| Adequacy | 1 (3.2%) | 2 (1.6%) | 0 (0.0%) | ||
| Potassium (g) | Inadequacy | 31 (100.0%) | 121 (98.4%) | 137 (97.2%) | 0.841 |
| Adequacy | 0 (0.0%) | 2 (1.6%) | 4 (2.8%) | ||
| Selenium (ug) | Inadequacy | 20 (64.5%) | 61 (49.6%) | 88 (62.4%) | 0.078 |
| Adequacy | 11 (35.5%) | 62 (50.4%) | 53 (37.6%) | ||
| Zinc (mg) | Inadequacy | 8 (25.8%) | 32 (26.0%) | 50 (35.5%) | 0.221 |
| Adequacy | 23 (74.2%) | 91 (74.0%) | 91 (64.5%) | ||
| Calcium (mg) | Inadequacy | 31 (100.0%) | 121 (98.4%) | 139 (98.6%) | 1.000 |
| Adequacy | 0 (0.0%) | 2 (1.6%) | 2 (1.4%) | ||
| Iron (mg) | Inadequacy | 9 (29.0%) | 31 (25.2%) | 30 (21.3%) | 0.542 |
| Adequacy | 22 (71.0%) | 92 (74.8%) | 111 (78.7%) |
| Nutrients | SMM 1 | ASMI 2 | HGS 3 | Walking Speed |
|---|---|---|---|---|
| β [95% CI] | β [95% CI] | β [95% CI] | β [95% CI] | |
| R2 (0.25) | R2 (0.11) | R2 (0.24) | R2 (0.10) | |
| Vitamin B12 | −0.10 [−0.16; −0.03] ** | −0.03 [−0.06; −0.01] * | --- | --- |
| Selenium | −0.02 [−0.03; −0.01] ** | −0.01 [−0.01; −0.00] *** | --- | --- |
| Iron | --- | --- | 0.07 [0.02; 0.12] ** | 0.003 [0.001; 0.006] ** |
| Variable | Sarcopenia | BMI |
|---|---|---|
| OR [95% CI] | OR [95% CI] | |
| Vitamin B6 Inadequacy | 2.18 [1.03–4.64] * | --- |
| Energy inadequacy | --- | 14.38 [1.44–143.43] * |
| Fiber inadequacy | --- | 4.97 [1.01–24.35] * |
| Protein inadequacy | --- | 4.88 [2.06–11.58] ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magalhães, N.V.; Waitzberg, D.L.; Lopes, N.C.; Vicedomini, A.C.C.; Prudêncio, A.P.A.; Jacob-Filho, W.; Busse, A.L.; Ferdinando, D.; Alves, T.P.; Pereira, R.M.R.; et al. High Prevalence of Energy and Nutrients Inadequacy among Brazilian Older Adults. Nutrients 2023, 15, 3246. https://doi.org/10.3390/nu15143246
Magalhães NV, Waitzberg DL, Lopes NC, Vicedomini ACC, Prudêncio APA, Jacob-Filho W, Busse AL, Ferdinando D, Alves TP, Pereira RMR, et al. High Prevalence of Energy and Nutrients Inadequacy among Brazilian Older Adults. Nutrients. 2023; 15(14):3246. https://doi.org/10.3390/nu15143246
Chicago/Turabian StyleMagalhães, Natalia Vieira, Dan Linetzky Waitzberg, Natalia Correia Lopes, Ana Carolina Costa Vicedomini, Ana Paula Aguiar Prudêncio, Wilson Jacob-Filho, Alexandre Leopold Busse, Douglas Ferdinando, Tatiana Pereira Alves, Rosa Maria Rodrigues Pereira, and et al. 2023. "High Prevalence of Energy and Nutrients Inadequacy among Brazilian Older Adults" Nutrients 15, no. 14: 3246. https://doi.org/10.3390/nu15143246
APA StyleMagalhães, N. V., Waitzberg, D. L., Lopes, N. C., Vicedomini, A. C. C., Prudêncio, A. P. A., Jacob-Filho, W., Busse, A. L., Ferdinando, D., Alves, T. P., Pereira, R. M. R., Torrinhas, R. S., & Belarmino, G. (2023). High Prevalence of Energy and Nutrients Inadequacy among Brazilian Older Adults. Nutrients, 15(14), 3246. https://doi.org/10.3390/nu15143246





