Occupational Health of Health-Care Workers with Overnutrition: Scoping Review with Meta-Analysis
Abstract
:1. Introduction
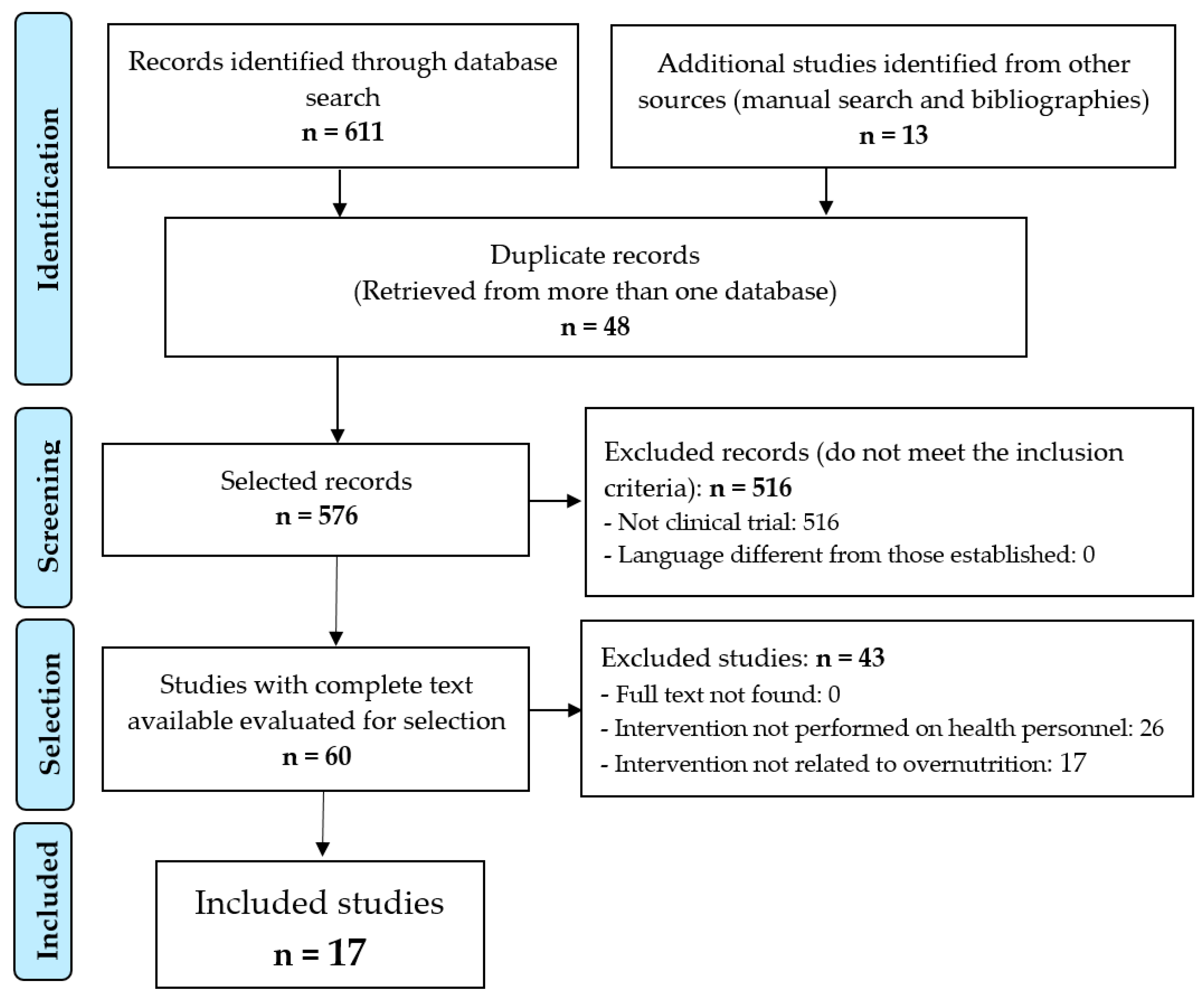
2. Materials and Methods
2.1. Design
2.2. Source of Data Collection
2.3. Information Processing
- Population: Health Personnel—Men and women working in the provision of health services, whether as individual practitioners or employees of health institutions and programs, whether professionally trained or not, and whether subject to public regulation or not.“Health Personnel”[Mesh] OR “Health Personnel”[Title/Abstract] OR “Health Care Provider*”[Title/Abstract] OR “Healthcare Provider*”[Title/Abstract] OR “Healthcare Worker*”[Title/Abstract] OR “Health Care Professional*”[Title/Abstract] OR “Nurse*”[Title/Abstract] OR “Pharmacist*”[Title/Abstract] OR “Physician*”[Title/Abstract] OR “Health Care Personnel”[Title/Abstract] OR “Health Care Practitioner*”[Title/Abstract] OR “Health Care Worker*”[Title/Abstract] OR “Health Profession Personnel”[Title/Abstract] OR “Healthcare Personnel”[Title/Abstract] OR “Healthcare Practitioner*”[Title/Abstract] OR “Healthcare Professional*”[Title/Abstract]
- Intervention: Overnutrition—An imbalanced nutritional status resulting from excessive intake of nutrients. Generally, overnutrition generates an energy imbalance between food consumption and energy expenditure, leading to disorders such as obesity.“Overnutrition”[Mesh] OR “Overnutrition”[Title/Abstract] OR “Hypernutrition”[Title/Abstract] OR “Overweight”[Title/Abstract] OR “Obesity”[Title/Abstract] OR “Hyperphagia”[Mesh] OR “Hyperphagia”[Title/Abstract] OR “Overeating”[Title/Abstract] OR “Polyphagia*”[Title/Abstract] OR “Dietary Excess”[Title/Abstract] OR “Excessive Feeding*”[Title/Abstract] OR “Hyper-Nutrition”[Title/Abstract] OR “Over-Nutrition”[Title/Abstract] OR “Overeating”[Title/Abstract] OR “Overfeeding”[Title/Abstract]
- Result: Occupational Health—The promotion and maintenance of physical and mental health in the work environment.“Occupational Health”[Mesh] OR “Occupational Health”[Title/Abstract] OR “Industrial Hygiene”[Title/Abstract] OR “Industrial Health”[Title/Abstract] OR “Occupational Safety”[Title/Abstract] OR “Employee Health”[Title/Abstract] OR “Occupational Exposure”[Mesh] OR “Occupational Exposure”[Title/Abstract] OR “Occupational Stress”[Mesh] OR “Occupational Stress”[Title/Abstract] OR “Occupational Disease”[Mesh] OR “Occupational Disease*”[Title/Abstract] OR “Occupational Hazard*”[Title/Abstract] OR “Occupational Medicine”[Mesh] OR “Occupational Medicine”[Title/Abstract] OR “Occupational Health Safety”[Title/Abstract] OR “Occupational Health Service*”[Title/Abstract] OR “Occupational Stressors”[Title/Abstract] OR “Occupational Factors”[Title/Abstract] OR “Workplace”[Mesh] OR “Workplace*”[Title/Abstract] OR “Workplace Health”[Title/Abstract] OR “Workplace Safety”[Title/Abstract] OR “Safety Climate”[Title/Abstract] OR “Total Worker Health”[Title/Abstract] OR “Working Environment”[Title/Abstract] OR “Job Satisfaction”[Mesh] OR “Job Satisfaction*”[Title/Abstract] OR “Job Stress”[Title/Abstract] OR “Job Security”[Title/Abstract] OR “Psychosocial Working Condition*”[Title/Abstract] OR “Employee Health”[Title/Abstract]
2.4. Final Selection of Articles
- Inclusion: being a clinical trial, being published in peer-reviewed journals, and written in English, Spanish, and Portuguese.
- Exclusion: those articles for which the full text could not be found, there was no association between the intervention and the outcome under the study criterion of causality, and those that included a non-adult population (under 18 years of age).
2.5. Documentary Quality, Level of Evidence and Recommendation, and Study of Biases
2.6. Data Extraction
2.7. Data Analysis
2.8. Ethical Aspects
3. Results
3.1. Types of Interventions Observed
- A.
- Nutrition education and healthy lifestyles:
- Pre-order, with/without nutrition information
- Nutrition education sessions
- Exercise and nutrition resources
- Nutrition education sessions, color-coded food labeling
- Healthy snacks, nutrition seminars
- Information on nutrition and physical activity, strategies for lifestyle modification
- Weight loss session, online resources.
- B.
- Behavioral Intervention
- Comments on previous purchases in the coffee shop
- Peer comparisons
- Cognitive behavioral training
- Social marketing campaign
- Strategies to foster interpersonal support
- Behavioral lessons: structural guidance on a variety of weight loss topics: nutrition, exercise, or behavioral self-regulation strategies.
- C.
- Diet
- Low-carbohydrate nutrition and meal replacement therapy
- Diet
- Cold food, water bottle, snack
- Dietary recommendations
- Meal distribution
- Individual dietary plan
- Environmental strategies to promote a healthy diet.
- D.
- Physical exercise
- Telemetric devices to measure your weight and steps steadily
- Physical activity
- Pedometer, exercise session, yoga
- Strengthening exercises, aerobic exercise
- Environmental strategies to foster physical activity.
- E.
- Economic intervention
- Financial incentives for healthier purchases
- Direct cash input for weight loss
- Discounts on food at the workplace cafeteria
- Bestowing rewards for getting involved in different activities—co-food and exercise equipment of varying values
- Loss of money if the objectives have not been achieved, and a financial gain if the targets have been accomplished.
- F.
- Coaching
- Telemedical coaching
- Coaching sessions
- Mindful eating training
- Standardized counseling
3.2. Results Procured from the Interventions Performed
3.3. Results Obtained from the Developed Strategies
3.4. Results from the Meta-Analysis
4. Discussion
4.1. Critical Analysis
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Obesity: Preventing and Managing the Global Epidemic (WHO Technical Report Series 894); WHO: Geneva, Switzerland, 2000. [Google Scholar]
- Goettler, A.; Grosse, A.; Sonntag, D. Productivity Loss Due to Overweight and Obesity: A Systematic Review of Indirect Costs. BMJ Open 2017, 7, e014632. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferrie, J.E.; Head, J.; Shipley, M.J.; Vahtera, J.; Marmot, M.G.; Kivimäki, M. BMI, Obesity, and Sickness Absence in the Whitehall II Study. Obesity 2007, 15, 1554–1564. [Google Scholar] [CrossRef]
- Sharma, S.V.; Upadhyaya, M.; Karhade, M.; Baun, W.B.; Perkison, W.B.; Pompeii, L.A.; Brown, H.S.; Hoelscher, D.M. Are Hospital Workers Healthy? A Study of Cardiometabolic, Behavioral, and Psychosocial Factors Associated With Obesity Among Hospital Workers. J. Occup. Environ. Med. 2016, 58, 1231–1238. [Google Scholar] [CrossRef]
- Luckhaupt, S.E.; Cohen, M.A.; Li, J.; Calvert, G.M. Prevalence of Obesity among U.S. Workers and Associations with Occupational Factors. Am. J. Prev. Med. 2014, 46, 237–248. [Google Scholar] [CrossRef]
- Estabrook, B.; Zapka, J.; Lemon, S.C. Evaluating the Implementation of a Hospital Work-Site Obesity Prevention Intervention: Applying the RE-AIM Framework. Health Promot. Pract. 2012, 13, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Christensen, J.R.; Overgaard, K.; Hansen, K.; Søgaard, K.; Holtermann, A. Effects on Presenteeism and Absenteeism from a 1-Year Workplace Randomized Controlled Trial among Health Care Workers. J. Occup. Environ. Med. 2013, 55, 1186–1190. [Google Scholar] [CrossRef] [PubMed]
- Gea Cabrera, A.; Caballero, P.; Wanden-Berghe, C.; Sanz-Lorente, M.; López-Pintor, E. Effectiveness of Workplace-Based Diet and Lifestyle Interventions on Risk Factors in Workers with Metabolic Syndrome: A Systematic Review, Meta-Analysis and Meta-Regression. Nutrients 2021, 13, 4560. [Google Scholar] [CrossRef]
- Kelly, M.; Wills, J. Systematic Review: What Works to Address Obesity in Nurses? Occup. Med. Oxf. Engl. 2018, 68, 228–238. [Google Scholar] [CrossRef] [Green Version]
- Power, B.T.; Kiezebrink, K.; Allan, J.L.; Campbell, M.K. Effects of Workplace-Based Dietary and/or Physical Activity Interventions for Weight Management Targeting Healthcare Professionals: A Systematic Review of Randomised Controlled Trials. BMC Obes. 2014, 1, e23. [Google Scholar] [CrossRef] [Green Version]
- Upadhyaya, M.; Sharma, S.; Pompeii, L.A.; Sianez, M.; Morgan, R.O. Obesity Prevention Worksite Wellness Interventions for Health Care Workers: A Narrative Review. Workplace Health Saf. 2020, 68, 32–49. [Google Scholar] [CrossRef]
- Melián-Fleitas, L.; Franco-Pérez, Á.; Caballero, P.; Sanz-Lorente, M.; Wanden-Berghe, C.; Sanz-Valero, J. Influence of Nutrition, Food and Diet-Related Interventions in the Workplace: A Meta-Analysis with Meta-Regression. Nutrients 2021, 13, 3945. [Google Scholar] [CrossRef] [PubMed]
- Schliemann, D.; Woodside, J.V. The Effectiveness of Dietary Workplace Interventions: A Systematic Review of Systematic Reviews. Public Health Nutr. 2019, 22, 942–955. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panchbhaya, A.; Baldwin, C.; Gibson, R. Improving the Dietary Intake of Healthcare Workers through Workplace Dietary Interventions: A Systematic Review and Meta-Analysis. Adv. Nutr. 2021, 13, 595–620. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Wanden-Berghe, C.; Sanz-Valero, J. Systematic Reviews in Nutrition: Standardized Methodology. Br. J. Nutr. 2012, 107, S3–S7. [Google Scholar] [CrossRef] [Green Version]
- Cobos-Carbó, A.; Augustovski, F. CONSORT 2010 Declaration: Updated guideline for reporting parallel group randomised trials. Med. Clin. 2011, 137, 213–215. [Google Scholar] [CrossRef] [Green Version]
- Harbour, R.; Miller, J. A New System for Grading Recommendations in Evidence Based Guidelines. BMJ 2001, 323, 334–336. [Google Scholar] [CrossRef] [Green Version]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Del Estado, B.O. Ley 14/2007, de 3 de Julio, de Investigación Biomédica. BOE Núm. 2007, 159, 28826–28848. [Google Scholar]
- Thorndike, A.N.; McCurley, J.L.; Gelsomin, E.D.; Anderson, E.; Chang, Y.; Porneala, B.; Johnson, C.; Rimm, E.B.; Levy, D.E. Automated Behavioral Workplace Intervention to Prevent Weight Gain and Improve Diet: The ChooseWell 365 Randomized Clinical Trial. JAMA Netw. Open 2021, 4, e2112528. [Google Scholar] [CrossRef]
- Röhling, M.; Martin, K.; Ellinger, S.; Schreiber, M.; Martin, S.; Kempf, K. Weight Reduction by the Low-Insulin-Method-A Randomized Controlled Trial. Nutrients 2020, 12, 3004. [Google Scholar] [CrossRef]
- Choy, K.H.K.; Chu, O.H.K.; Keung, W.Y.; Lim, B.; Tang, W.P.Y. A Nutritional Wellness Program For Overweight Health Care Providers In Hospital Setting: A Randomized Controlled Trial Pilot Study. Int. J. Med. Health Sci. 2017, 11, 223–226. [Google Scholar] [CrossRef]
- Faghri, P.D.; Simon, J.; Huedo-Medina, T.; Gorin, A. Perceived Self-Efficacy and Financial Incentives: Factors Affecting Health Behaviors and Weight Loss in a Workplace Weight Loss Intervention. J. Occup. Environ. Med. 2017, 59, 453–460. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leedo, E.; Beck, A.M.; Astrup, A.; Lassen, A.D. The Effectiveness of Healthy Meals at Work on Reaction Time, Mood and Dietary Intake: A Randomised Cross-over Study in Daytime and Shift Workers at an University Hospital. Br. J. Nutr. 2017, 118, 121–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Østbye, T.; Stroo, M.; Brouwer, R.J.N.; Peterson, B.L.; Eisenstein, E.L.; Fuemmeler, B.F.; Joyner, J.; Gulley, L.; Dement, J.M. Steps to Health Employee Weight Management Randomized Control Trial: Short-Term Follow-up Results. J. Occup. Environ. Med. 2015, 57, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Stites, S.D.; Singletary, S.B.; Menasha, A.; Cooblall, C.; Hantula, D.; Axelrod, S.; Figueredo, V.M.; Phipps, E.J. Pre-Ordering Lunch at Work. Results of the What to Eat for Lunch Study. Appetite 2015, 84, 88–97. [Google Scholar] [CrossRef]
- Christensen, J.R.; Overgaard, K.; Carneiro, I.G.; Holtermann, A.; Søgaard, K. Weight Loss among Female Health Care Workers--a 1-Year Workplace Based Randomized Controlled Trial in the FINALE-Health Study. BMC Public Health 2012, 12, 625. [Google Scholar] [CrossRef] [Green Version]
- Speroni, K.G.; Earley, C.; Seibert, D.; Kassem, M.; Shorter, G.; Ware, C.C.; Kosak, E.; Atherton, M. Effect of Nurses Living FitTM Exercise and Nutrition Intervention on Body Mass Index in Nurses. J. Nurs. Adm. 2012, 42, 231–238. [Google Scholar] [CrossRef]
- Thorndike, A.N.; Sonnenberg, L.; Healey, E.; Myint-U, K.; Kvedar, J.C.; Regan, S. Prevention of Weight Gain Following a Worksite Nutrition and Exercise Program: A Randomized Controlled Trial. Am. J. Prev. Med. 2012, 43, 27–33. [Google Scholar] [CrossRef] [Green Version]
- Christensen, J.R.; Faber, A.; Ekner, D.; Overgaard, K.; Holtermann, A.; Søgaard, K. Diet, Physical Exercise and Cognitive Behavioral Training as a Combined Workplace Based Intervention to Reduce Body Weight and Increase Physical Capacity in Health Care Workers—A Randomized Controlled Trial. BMC Public Health 2011, 11, 671. [Google Scholar] [CrossRef] [Green Version]
- Lemon, S.C.; Zapka, J.; Li, W.; Estabrook, B.; Rosal, M.; Magner, R.; Andersen, V.; Borg, A.; Hale, J. Step Ahead a Worksite Obesity Prevention Trial among Hospital Employees. Am. J. Prev. Med. 2010, 38, 27–38. [Google Scholar] [CrossRef]
- Lowe, M.R.; Tappe, K.A.; Butryn, M.L.; Annunziato, R.A.; Coletta, M.C.; Ochner, C.N.; Rolls, B.J. An Intervention Study Targeting Energy and Nutrient Intake in Worksite Cafeterias. Eat. Behav. 2010, 11, 144–151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Racette, S.B.; Deusinger, S.S.; Inman, C.L.; Burlis, T.L.; Highstein, G.R.; Buskirk, T.D.; Steger-May, K.; Peterson, L.R. Worksite Opportunities for Wellness (WOW): Effects on Cardiovascular Disease Risk Factors after 1 Year. Prev. Med. 2009, 49, 108–114. [Google Scholar] [CrossRef] [Green Version]
- Van Wier, M.F.; Ariëns, G.A.M.; Dekkers, J.C.; Hendriksen, I.J.M.; Smid, T.; van Mechelen, W. Phone and E-Mail Counselling Are Effective for Weight Management in an Overweight Working Population: A Randomized Controlled Trial. BMC Public Health 2009, 9, 6. [Google Scholar] [CrossRef]
- Tate, D.F.; Wing, R.R.; Winett, R.A. Using Internet Technology to Deliver a Behavioral Weight Loss Program. JAMA 2001, 285, 1172–1177. [Google Scholar] [CrossRef] [Green Version]
- Follick, M.J.; Fowler, J.L.; Brown, R.A. Attrition in Worksite Weight-Loss Interventions: The Effects of an Incentive Procedure. J. Consult. Clin. Psychol. 1984, 52, 139–140. [Google Scholar] [CrossRef]
- Hagger, M.S. What Makes a ‘Good’ Review Article? Some Reflections and Recommendations. Health Psychol. Rev. 2012, 6, 141–146. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). Global Strategy on Occupational Health for All: The Way to Health at Work; WHO: Geneva, Switzerland, 1995. [Google Scholar]
- Carriedo-Diez, B.; Tosoratto-Venturi, J.L.; Cantón-Manzano, C.; Wanden-Berghe, C.; Sanz-Valero, J. The Effects of the Exogenous Melatonin on Shift Work Sleep Disorder in Health Personnel: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 10199. [Google Scholar] [CrossRef]
- Begg, C.; Cho, M.; Eastwood, S.; Horton, R.; Moher, D.; Olkin, I.; Pitkin, R.; Rennie, D.; Schulz, K.F.; Simel, D.; et al. Improving the Quality of Reporting of Randomized Controlled Trials: The CONSORT Statement. JAMA 1996, 276, 637–639. [Google Scholar] [CrossRef]
- Turner, L.; Shamseer, L.; Altman, D.G.; Schulz, K.F.; Moher, D. Does Use of the CONSORT Statement Impact the Completeness of Reporting of Randomised Controlled Trials Published in Medical Journals? A Cochrane Review. Syst. Rev. 2012, 1, 60. [Google Scholar] [CrossRef] [Green Version]
- Manterola, C.; Asenjo-Lobos, C.; Otzen, T. Hierarchy of evidence: Levels of evidence and grades of recommendation from current use. Rev. Chil. Infectol. Organo. Of. Soc. Chil. Infectol. 2014, 31, 705–718. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teufer, B.; Ebenberger, A.; Affengruber, L.; Kien, C.; Klerings, I.; Szelag, M.; Grillich, L.; Griebler, U. Evidence-Based Occupational Health and Safety Interventions: A Comprehensive Overview of Reviews. BMJ Open 2019, 9, e032528. [Google Scholar] [CrossRef] [Green Version]
- Boniol, M.; McIsaac, M.; Xu, L.; Wuliji, T.; Diallo, K.; Campbell, J. Gender Equity in the Health Workforce: Analysis of 104 Countries; World Health Organization: Geneve, Switzerland, 2019. [Google Scholar]
- Barriocanal-Gómez, P.; Del Pozo-Díez, C.M.; Kudryavtseva, O.; Portillo Chicano, I.; Sanz-Valero, J. Effects derived from occupational exposure to hazardous substances in pregnant working women: Systematic review. Arch. Prev. Riesgos Laborales 2021, 24, 263–296. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Adult Obesity Facts: Obesity Is a Common, Serious, and Costly Disease; CDC: Atlanta, GA, USA, 2022. [Google Scholar]
- Hall, K.D.; Kahan, S. Maintenance of Lost Weight and Long-Term Management of Obesity. Med. Clin. N. Am. 2018, 102, 183–197. [Google Scholar] [CrossRef] [PubMed]
- Thorndike, A.N.; Gelsomin, E.D.; McCurley, J.L.; Levy, D.E. Calories Purchased by Hospital Employees After Implementation of a Cafeteria Traffic Light-Labeling and Choice Architecture Program. JAMA Netw. Open 2019, 2, e196789. [Google Scholar] [CrossRef] [Green Version]
- Braeckman, L.; De Bacquer, D.; Maes, L.; De Backer, G. Effects of a Low-Intensity Worksite-Based Nutrition Intervention. Occup. Med. Oxf. Engl. 1999, 49, 549–555. [Google Scholar] [CrossRef] [Green Version]
- Hartmann-Boyce, J.; Ordóñez-Mena, J.M.; Theodoulou, A.; Butler, A.R.; Freeman, S.C.; Sutton, A.J.; Jebb, S.A.; Aveyard, P. Impact of Program Characteristics on Weight Loss in Adult Behavioral Weight Management Interventions: Systematic Review and Component Network Meta-Analysis. Obesity 2022, 30, 1778–1786. [Google Scholar] [CrossRef]
- Hilbert, A.; Neuhaus, P.; Köhler, N.; Petroff, D.; Hay, P.; Hübner, C. Group Cognitive Remediation Therapy Prior to Behavioral Weight Loss Treatment for Adults with Severe Obesity: A Randomized Clinical Trial (CRT Study). J. Consult. Clin. Psychol. 2021, 89, 695–706. [Google Scholar] [CrossRef]
- Chew, H.S.J.; Chng, S.; Rajasegaran, N.N.; Choy, K.H.; Chong, Y.Y. Effectiveness of Acceptance and Commitment Therapy on Weight, Eating Behaviours and Psychological Outcomes: A Systematic Review and Meta-Analysis. Eat. Weight Disord. EWD 2023, 28, 6. [Google Scholar] [CrossRef]
- Barratt, A.; Reznik, R.; Irwig, L.; Cuff, A.; Simpson, J.M.; Oldenburg, B.; Horvath, J.; Sullivan, D. Work-Site Cholesterol Screening and Dietary Intervention: The Staff Healthy Heart Project: Steering Committee. Am. J. Public Health 1994, 84, 779–782. [Google Scholar] [CrossRef] [Green Version]
- Anderson, L.M.; Quinn, T.A.; Glanz, K.; Ramirez, G.; Kahwati, L.C.; Johnson, D.B.; Buchanan, L.R.; Archer, W.R.; Chattopadhyay, S.; Kalra, G.P.; et al. The Effectiveness of Worksite Nutrition and Physical Activity Interventions for Controlling Employee Overweight and Obesity: A Systematic Review. Am. J. Prev. Med. 2009, 37, 340–357. [Google Scholar] [CrossRef]
- Verweij, L.M.; Coffeng, J.; van Mechelen, W.; Proper, K.I. Meta-Analyses of Workplace Physical Activity and Dietary Behaviour Interventions on Weight Outcomes. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2011, 12, 406–429. [Google Scholar] [CrossRef]
- Kullgren, J.T.; Troxel, A.B.; Loewenstein, G.; Asch, D.A.; Norton, L.A.; Wesby, L.; Tao, Y.; Zhu, J.; Volpp, K.G. Individual- versus Group-Based Financial Incentives for Weight Loss: A Randomized, Controlled Trial. Ann. Intern. Med. 2013, 158, 505–514. [Google Scholar] [CrossRef] [Green Version]
- Vermeer, W.M.; Steenhuis, I.H.M.; Leeuwis, F.H.; Heymans, M.W.; Seidell, J.C. Small Portion Sizes in Worksite Cafeterias: Do They Help Consumers to Reduce Their Food Intake? Int. J. Obes. 2011, 35, 1200–1207. [Google Scholar] [CrossRef] [Green Version]
- Sieczkowska, S.M.; de Lima, A.P.; Swinton, P.A.; Dolan, E.; Roschel, H.; Gualano, B. Health Coaching Strategies for Weight Loss: A Systematic Review and Meta-Analysis. Adv. Nutr. 2021, 12, 1449–1460. [Google Scholar] [CrossRef]
- Sforzo, G.A.; Moore, M.; Moore, G.E.; Harenberg, S. Comment on “Health Coaching: 100 Strategies for Weight Loss: A Systematic Review and Meta-Analysis”. Adv. Nutr. 2021, 12, 1042–1043. [Google Scholar] [CrossRef]
- Muto, T.; Yamauchi, K. Evaluation of a Multicomponent Workplace Health Promotion Program Conducted in Japan for Improving Employees’ Cardiovascular Disease Risk Factors. Prev. Med. 2001, 33, 571–577. [Google Scholar] [CrossRef]
- Quintiliani, L.; Sattelmair, J.; Sorensen, G. The Workplace as a Setting for Interventions to Improve Diet and Promote Physical Activity; World Health Organization: Washington, DC, USA, 2007. [Google Scholar]
- Rapisarda, V.; Cannizzaro, E.; Barchitta, M.; Vitale, E.; Cinà, D.; Minciullo, F.; Matera, S.; Bracci, M.; Agodi, A.; Ledda, C. A Combined Multidisciplinary Intervention for Health Promotion in the Workplace: A Pilot Study. J. Clin. Med. 2021, 10, e1512. [Google Scholar] [CrossRef]
- Chia, A.; Ong, J.; Bundele, A.; Lim, Y.W. Social Entrepreneurship in Obesity Prevention: A Scoping Review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2022, 23, e13378. [Google Scholar] [CrossRef]
- Kunyahamu, M.S.; Daud, A.; Jusoh, N. Obesity among Health-Care Workers: Which Occupations Are at Higher Risk of Being Obese? Int. J. Environ. Res. Public. Health 2021, 18, 4381. [Google Scholar] [CrossRef]
- Bernabeu-Martínez, M.A.; Ramos Merino, M.; Santos Gago, J.M.; Álvarez Sabucedo, L.M.; Wanden-Berghe, C.; Sanz-Valero, J. Guidelines for Safe Handling of Hazardous Drugs: A Systematic Review. PLoS ONE 2018, 13, e0197172. [Google Scholar] [CrossRef]
- Álvarez Velásquez, S.; Sanz Valero, J. Ventajas de La Quimioterapia Domiciliaria En Los Enfermos Adultos Con Neoplasias: Revisión Sistemática. Hosp. Domic. 2020, 4, 25–41. [Google Scholar] [CrossRef] [Green Version]
- Allan, J.; Querstret, D.; Banas, K.; de Bruin, M. Environmental Interventions for Altering Eating Behaviours of Employees in the Workplace: A Systematic Review. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2017, 18, 214–226. [Google Scholar] [CrossRef] [Green Version]



| Author/Year | Population Studied | Country | Pathology | Intervention Period | Type of Intervention | Observed Outcome |
|---|---|---|---|---|---|---|
| Thorndike et al. 2021 [23] | N = 602 IG: n = 299 M/W = 69/230 Age Mean = 43.5 ± 12 years BMI = 28.6 ± 6.6 CG: n = 303 M/W = 55/248 Age Mean = 43.8 ± 12.5 years BMI = 28.0 ± 6.5 | USA | Overweight and obesity | 2 years | IG: Participants received two emails per week with feedback on previous cafeteria purchases and personalized health and lifestyle tips and one letter per month with peer comparisons and financial incentives for healthier purchases. CG: Participants received one letter per month with general healthy lifestyle information. | There were no between-group differences in weight change. IG increased green-labeled purchases and decreased red-labeled and calories purchased compared with CG (p < 0.001). The findings suggest that an automated behavioral intervention using workplace cafeteria data improved employees’ food choices but did not prevent weight gain. |
| Röhling et al. 2020 [24] | N = 30 IG: n = 15 M/W = 3/12 Age Mean = 44 ± 9 years BMI = 35.1 ± 6.9 CG: n = 15 M/W = 2/13 Age Mean = 49 ± 7 years BMI = 32.8 ± 6.1 | Germany | Overweight and obesity | 12 weeks | IG: Received seminars, low-carbohydrate nutrition including formula diet, continuous glucose monitoring, telemetric monitoring, and telemedical coaching) with weekly contacts. CG: Continued their habitual lifestyle. All participants were equipped with telemetric devices (scales and pedometers). | IG significantly reduced weight (p < 0.001) and improved in BMI, WC, fat mass, and all variables of eating behavior (all p < 0.05) compared to the CG. |
| Choy et al. 2017 [25] | N = 42 IG: n = 20 M/W = Not provided Age Mean = Not provided BMI = 28.59 ± 2.78 CG: n = 22 M/W = Not provided Age Mean = Not provided BMI = 28.9 ± 3.67 | China | Overweight and obesity | 8 weeks | IG: Received tailored weight management intervention, including individual nutrition counseling, nutrition pamphlets, telephone counseling, and smartphone text messages for eight weeks. CG: Received individual nutrition counseling and nutrition pamphlets. Both groups received a face-to-face education session for 45 min. | In comparison with the control group, the mean net weight loss in the intervention group increased at the end of the study. In the follow-up visit at week 8, the mean change in weight from baseline was −0.3 kg (95% CI) in the CG and −0.98 kg (95% CI) in the IG. The net difference in mean BMI in the intervention groups was −0.4 (95% CI). |
| Faghri et al. 2017 [26] | N = 99 IG: n = 51 M/W = Not provided Age Mean = Not provided BMI = Not provided CG: n = 48 M/W = Not provided Age Mean = Not provided BMI = Not provided | USA | Overweight and obesity | 16 weeks | IG: Financial incentive-based intervention. All participants received a personalized weight loss consultation based on their reported physical activity habits and dietary preferences. Each participant received an action plan based on the National Diabetes Prevention Program (NDPP). CG: No incentive. | IG reduced more weight (p = 0.027) and BMI (p = 0.043) than CG at week 16. At week 28, IG lost more weight than CG (p = 0.053) and reduced their BMI more than CG (p = 0.308). Eating and exercise self-efficacy were significant mediators between health behaviors and weight loss (p < 0.05). Incentives significantly moderated the effects of self-efficacy (p = 0.00) on weight loss. Self-efficacy and financial incentives may affect weight loss and play a role in weight-loss interventions. |
| Leedo et al. 2017 [27] | N = 59 IG: n = 59 M/W = 7/52 Age Mean = 45.1 ± 9.3 years BMI = 24.1 ± 3.5 CG: n = 59 M/W = 7/52 Age Mean = 45.1 ± 9.3 years BMI ± SD = 24.1 ± 3.5 | Denmark | Overweight and obesity | 8 weeks | Intervention period (4 weeks): Received a keyhole-labeled meal, snack, and bottled water during each shift. Control period (4 weeks): Instructed to continue with their habitual dietary intake. | The intake of fat (p = 0.03) and polyunsaturated fatty acid (p = 0.003) was lower, and the intake of carbohydrate (p = 0.008), dietary fibre (p = 0.031), and water (p < 0.001) was greater in the intervention period than in the control period. |
| Østbye et al. 2015 [28] | N = 550 IG: (WM+ behavioral): n = 275 M/W = 45/230 Age: ≤50 years = 175 >50 years = 100 BMI = 37.37 ± 6.61 CG: (WM educational): n = 275 M/W = 48/227 Age: ≤50 years = 187 >50 years = 88 BMI = 37.02 ± 6.14 | USA | Obesity | 1 year | WM+: Intensive behavioral intervention: (1) monthly counseling sessions, (2) meetings with an exercise physiologist, (3) quarterly biometric feedback, (4) targeted health education materials, (5) information and active linking with various Duke programs and wellness resources, and (6) use of eHealth trackers for diet and weight. WM: Educational program targeting healthy lifestyle changes for weight loss (portion control, education, healthy diets, and physical activity). | There were no statistically meaningful differences between groups but there were modest reductions in BMI. |
| Stites et al. 2015 [29] | N = 26 IG: n = 10 M/W = 1/9 Age Mean = 48.6 ± 11.6 years BMI = 33.9 ± 5.0 CG: n = 16 M/W = 2/14 Age Mean = 42.6 ± 9.6 years BMI = 33.1 ± 11.2 | USA | Overweight and obesity | 12 weeks | IG: Baseline (4 weeks): participants selected their lunches as usual from the cafeteria. Full intervention (4 weeks): mindful eating training, pre-ordered lunches, price discounts. Partial intervention (4 weeks): pre-ordered lunches without price discounts. CG: Baseline (8 weeks), full intervention (4 weeks), and partial intervention (4 weeks). | The IG purchased lunches with an average of 144.6 fewer kilocalories (p = 0.01) and 8.9 fewer grams of fat (p = 0.005) compared to controls. Participants decreased their body weight from the beginning to the end of the study by an average of 0.40 kg. |
| Christensen et al. 2012 [30] | N = 98 IG: n = 54 M/W: 0/54 Age Mean = 45.7 ± 8.7 years BMI = 30.7 ± 5.4 CG: n = 44 M/W: 0/44 Age Mean = 46.0 ± 8.6 years BMI = 30.4 ± 4.9 | Denmark | Overweight and obesity | 1 year | IG: One-hour weekly workplace intervention consisting of diet, physical exercise, and cognitive behavioral training. CG: Monthly two-hour oral presentation during working hours about the Danish Dietary recommendations and other health-related topics. | The intervention generated substantial reductions in body weight (p < 0.001), BMI (p < 0.001), and body fat percentage (p < 0.001). The positive results support the workplace as an efficient arena for weight loss among overweight females. |
| Speroni et al. 2012 [31] | N = 217 IG: n = 108 M/W = 2/106 Age Mean (range) = 47.6 (22–67) years BMI = 30.5 ± 6.8 CG: n = 109 M/W = 7/102 Age Mean (range) = 45.2 (22–67) years BMI = 27.6 ± 5.3 | USA | Overweight and obesity | 24 weeks | IG: Included exercise (12 weekly sessions), yoga and nutrition (4 monthly sessions), and diary completion (exercise/yoga, food/water consumption, and sleep), addressing healthy lifestyle principles. CG: There were no other procedures for the contrast group. All participants completed an evaluation form about exercises and overall health. | IG experienced a greater mean reduction from baseline to week 12 in BMI than CG (IG = −0.494, CG = −0.180). This reduction in BMI among IG was significant based on a 1-tailed t test (p < 0.05). IG experienced a greater mean reduction in waist circumference (IG = −0.895, CG = -0.091) (p < 0.001) from baseline to week 12. |
| Thorndike et al. 2012 [32] | N = 330 IG: n = 174 M/W: 17/157 Age Mean = 44.2 ± 11.8 years BMI = 28.0 ± 5.8 CG: n = 156 M/W: 28/128 Age Mean = 41.6 ± 13.6 years BMI = 27.5 ± 5.9 | USA | Overweight and obesity | 10 weeks | Ten-week exercise and nutrition program (IG and CG) immediately followed by a 9-month maintenance intervention. IG: Internet support with a website for goal-setting and self-monitoring of weight and exercise plus minimal personal support (for 9 months). CG: Usual care (for 9 months). | The initial program resulted in moderate weight loss and improvements in diet and exercise behaviors at 1 year (p < 0.001) in both groups, but no difference in weight loss between groups. The Internet-based maintenance program immediately after did not improve these outcomes. |
| Christensen et al. 2011 [33] | N = 144 IG: n = 76 M/W: 1/75 Age Mean = 44.8 ± 9.5 years BMI = 28.4 ± 6.0 CG: n = 68 M/W: 4/64 Age Mean = 46.4 ± 9.5 years BMI = 27.8 ± 5.6 | Denmark | Overweight and obesity | 1 year | IG: An individual dietary plan with an energy deficit of 1200 kcal/day, strengthening exercises, and cognitive behavioral training during working hours for 1 h/week. Leisure time aerobic fitness was planned for 2 h/week. CG: Monthly oral presentations. | The significantly reduced body weight, body fat, waist circumference, and blood pressure as well as increased aerobic fitness in the intervention group (p ≤ 0.001) show the great potential of workplace health promotion among this high-risk workgroup. |
| Lemon et al. 2010 [34] | N = 806 IG: n = 386 M/W = 21.7%/78.3% Age: ≤50 years = 67.0 %>50 years = 33.0% BMI: <25 = 36.9% ≥25.0 = 63.1% CG: n = 303 M/W = 15.8%/84.2% Age: ≤50 years = 70.5% >50 years = 29.5% BMI: <25 = 31.6% ≥25.0 = 68.4% | USA | Overweight and obesity | 2 years | IG: The intervention was designed to promote organizational and social norms related to healthy eating and physical activity in the worksite. CG: The control condition received no intervention. | Employees in intervention sites reported significantly greater improvements in perceptions of organizational commitment to employee health at 12 and 24 months compared to control sites, but there was no impact of the intervention on change in BMI from baseline to 12 (beta = 0.272; 95% CI = −0.271, 0.782) or 24 months (beta = 0.276; 95% CI = −0.338, 0.890) in intention-to-treat analysis. |
| Lowe et al. 2010 [35] | N = 96 IG: n = 47 M/W: 7/40 Age Mean = Not provided BMI = Not provided CG: n = 49 M/W: 11/38 Age Mean = Not provided BMI = Not provided | USA | Overweight and obesity | 1 year | IG: Environmental change plus pricing incentives for purchasing low-energy-density foods. Education sessions about low-energy-density eating. CG: Environmental change (introduction of ten new low-energy-density foods and food labels). | There was no statistically significant change in weight during the cafeteria monitoring phase in either intervention condition, when controlling for baseline weight (p = 0.11). |
| Racette et al. 2009 [36] | N = 123 IG: n = 68 M/W: Not provided Age Mean = Not provided BMI = 34.5 ± 9.7 CG: n = 55 M/W: Not provided Age Mean = Not provided BMI = 31.1 ± 7.2 | USA | Overweight and obesity | 1 year | IG: Assessment and intervention (promotion of physical activity and favourable dietary patterns using pedometers, healthy snack cart, weight watchers’ meetings, exercise classes, seminars, and team competitions and rewards). CG: Assessment only. All participants received personal health reports. | Improvements (p ≤ 0.05) were observed in both groups for fitness, blood pressure, and total, HDL, and LDL cholesterol. Additional improvements occurred in the IG in BMI, fat mass, Framingham risk score, and prevalence of metabolic syndrome; only the changes in BMI and fat mass were different between groups. |
| van Wier et al. 2009 [37] | N = 1386 IG phone: n = 462 M/F = 321/141 Age Mean = 43 ± 8.8 years BMI = 29.5 ± 3.5 IG internet: n = 464 M/W = 302/162 Age Mean = 43 ± 8.4 years BMI = 29.6 ± 3.4 CG: n = 460 M/W = 306/154 Age Mean = 43 ± 8.7 years BMI = 29.6 ± 3.7 | Overweight | Netherlands | 6 months | IG phone: Received self-help materials, a lifestyle intervention program (10 modules about nutrition and physical activity), and phone counseling. IG internet: Received self-help materials and e-mail counseling. CG: Received only the self-help materials and no counseling. | The phone IG had a significant weight loss of 1.5 kg (95% CI −2.2; −0.8) in comparison with the CG. For the internet IG, this was 0.6 kg (95% CI −1.3; −0.01). The difference between the intervention groups was not statistically significant as their coefficients were mutually included in their 95% confidence intervals. |
| Tate et al. 2001 [38] | N = 91 IG: n = 46 M/W = 5/41 Age Mean = 41.1 ± 11.6 years BMI = 29.1 ± 3.0 CG: n = 45 M/W = 5/40 Age Mean = 40.6 ± 9.7 years BMI = 28.9 ± 3.1 | USA | Overweight and obesity | 6 months | IG: Same as controls plus internet behavior therapy. Additional twenty-four weekly behavioral lessons via email, self-monitoring diaries, and individualised therapist feedback. CG: Internet education. One face-to-face group weight loss session and access to a web site with links to weight loss resources. | IG lost more weight than the CG (p = 0.005). Changes in waist circumference were also greater in the IG than in the CG at both 3 months (p = 0.001) and 6 months (p = 0.005). |
| Follick et al. 1984 [39] | N = 48 IG: n = 24 M/W = Not provided Age Mean = Not provided BMI = Not provided CG: n = 24 M/W = Not provided Age Mean = Not provided BMI = Not provided | USA | Overweight | 18 weeks | IG: Weight loss program (14-session behavior modification program) plus incentive procedure. 5$ (×14) deposit was returned (one for each treatment session). CG: Weight loss program alone. | Both groups lost weight over the course of the intervention (p < 0.001) and there were no significant differences in weight loss between groups. The inclusion of an incentive procedure may improve the effectiveness of a behavioral weight loss intervention by decreasing attrition (p < 0.01). |
| Clinical Trial | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | 25 | Total | % |
| Thorndike et al. [21] | 1 | 1 | 0.5 | 1 | 1 | 0.5 | 0.5 | 1 | 0 | 0 | 0.5 | 1 | 1 | 1 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 17 | 70.8 |
| Röhling et al. [22] | 1 | 1 | 0 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 0.5 | 1 | 1 | 1 | 1 | 1 | 1 | NA | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 19 | 79.2 |
| Choy et al. [23] | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0.5 | 0 | 0 | 0 | 1 | 0.5 | 0 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 14.5 | 60.4 |
| Faghri et al. [24] | 0.5 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 8.5 | 35.4 |
| Leedo et al. [25] | 1 | 1 | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 21.5 | 89.6 |
| Østbye et al. [26] | 1 | 1 | 1 | 1 | 1 | 0.5 | 0 | 0.5 | 0 | 0 | 0 | 0.5 | 1 | 1 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 16 | 66.7 |
| Stites et al. [27] | 0.5 | 1 | 0.5 | 1 | 1 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 1 | 1 | 0.5 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 16 | 66.7 |
| Christensen et al. [28] | 1 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0 | 0.5 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 15 | 62.5 |
| Speroni et al. [29] | 0.5 | 1 | 0.5 | 1 | 1 | 1 | 1 | NA | NA | NA | NA | 0 | 0.5 | 0.5 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 12.5 | 52.1 |
| Thorndike et al. [30] | 1 | 1 | 0 | 1 | 0 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 15 | 62.5 |
| Christensen et al. [31] | 1 | 1 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 1 | 1 | 0.5 | 0.5 | 1 | 1 | 0 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 15 | 62.5 |
| Lemon et al. [32] | 1 | 1 | 1 | 1 | 1 | 1 | 0.5 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 18 | 75.0 |
| Lowe et al. [33] | 0.5 | 1 | 0.5 | 1 | 1 | 1 | 1 | 0.5 | 1 | 0 | 0 | 1 | 0.5 | 0.5 | 0 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 14.5 | 60.4 |
| Racette et al. [34] | 0.5 | 1 | 0.5 | 1 | 1 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 1 | 1 | 0.5 | 0 | 1 | 1 | NA | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 14 | 58.3 |
| van Wier et al. [35] | 1 | 1 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0.5 | 1 | 0 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 12 | 50.0 |
| Tate et al. [36] | 0.5 | 1 | 1 | 1 | 1 | 1 | 1 | 0.5 | 0 | 0 | 0 | 1 | 1 | 0.5 | 1 | 1 | 1 | NA | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 16 | 66.7 |
| Follick et al. [37] | 0.5 | 1 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 | NA | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 12.5 |
| Strategy (Number of Interventions) | Types of Intervention |
|---|---|
| 1 intervention | |
| 2 interventions | |
| 3 interventions | |
| 4 interventions |
|
| Body Weight Data [kg] | |||||||
|---|---|---|---|---|---|---|---|
| Trial | Year | N Initial | M-Weight Initial | SD Initial | N Final | M-Weight Final | SD Final |
| Thorndike et al. [21] | 2021 | 299 | 79.8 | 18.8 | 255 | 81.3 | 17.3 |
| Röhling et al. [22] | 2020 | 15 | 104.0 | 25 | 14 | 96.2 | 21.2 |
| Choy et al. [23] | 2017 | 20 | 71.9 | 11.6 | 20 | 70.9 | 11.9 |
| Faghri et al. [24] | 2017 | 51 | NR | NR | NR | NR | NR |
| Leedo et al. [25] | 2017 | 59 | 70.4 | 10.6 | 59 | 70.3 | 10.8 |
| Østbye et al. [26] | 2015 | 275 | NR | NR | 215 | NR | NR |
| Stites et al. [27] | 2015 | 10 | 91.5 | 16.1 | 10 | NR | NR |
| Christensen et al. [28] | 2012 | 54 | 84.2 | 15.9 | 54 | 78.4 | 15.8 |
| Speroni et al. [29] | 2012 | 108 | NR | NR | 70 | NR | NR |
| Thorndike et al. [30] | 2012 | 174 | 76.9 | 16.8 | 157 | 74.7 | 15.8 |
| Christensen et al. [31] | 2011 | 54 | 84.3 | 16 | 54 | 80.7 | 12.2 |
| Lemon et al. [32] | 2010 | 386 | NR | NR | 299 | NR | NR |
| Lowe et al. [33] | 2010 | 47 | 85.5 | 16.2 | 47 | 86.3 | 16.9 |
| Racette et al. [34] | 2009 | 68 | 92.4 | 24.9 | 68 | 91.6 | 25.5 |
| van Wier et al. [35] | 2009 | 462 | 93.4 | 14.1 | 459 | 90.7 | 13.7 |
| van Wier et al. [35] | 2009 | 464 | 92.8 | 14.3 | 458 | 91.0 | 14.2 |
| Tate et al. [36] | 2001 | 46 | 77.4 | 9.4 | 36 | 73.3 | 4.5 |
| Follick et al. [37] | 1984 | 24 | NR | NR | NR | NR | NR |
| Data on body mass index [kg/m2] | |||||||
| Trial | Year | N initial | M-IMC initial | SD initial | N final | M-IMC Final | SD final |
| Thorndike et al. [21] | 2021 | 299 | 28.6 | 6.6 | 255 | 29.1 | 2 |
| Röhling et al. [22] | 2020 | 15 | 35.1 | 6.9 | 14 | 32.6 | 1.1 |
| Choy et al. [23] | 2017 | 20 | 28.6 | 2.8 | 20 | 28.2 | 3.0 |
| Faghri et al. [24] | 2017 | 51 | NR | NR | NR | NR | NR |
| Leedo et al. [25] | 2017 | 59 | 24.1 | 3.5 | 59 | NR | NR |
| Østbye et al. [26] | 2015 | 215 | 36.9 | 5.86 | 215 | 36.6 | 2.2 |
| Stites et al. [27] | 2015 | 10 | 33.9 | 5 | 10 | NR | NR |
| Christensen et al. [28] | 2012 | 54 | 30.7 | 5.4 | 54 | 28.5 | 5.5 |
| Speroni et al. [29] | 2012 | 70 | 29.6 | 6.6 | 70 | 29.1 | 6.5 |
| Thorndike et al. [30] | 2012 | 157 | 28 | 5.8 | 157 | 27.2 | 5.4 |
| Christensen et al. [31] | 2011 | 54 | 30.5 | 5.4 | 54 | 29.2 | 4.0 |
| Lemon et al. [32] | 2010 | 386 | 28.4 | NR | 299 | 28.9 | NR |
| Lowe et al. [33] | 2010 | 47 | NR | NR | NR | NR | NR |
| Racette et al. [34] | 2009 | 68 | 34.5 | 9.7 | 68 | 34.1 | 9.8 |
| van Wier et al. [35] | 2009 | 462 | 29.5 | 3.5 | NR | NR | NR |
| van Wier et al. [35] | 2009 | 462 | 29.5 | 3.5 | NR | NR | NR |
| Tate et al. [36] | 2001 | 46 | 29.1 | 3 | 36 | NR | NR |
| Follick et al. [37] | 1984 | 24 | NR | NR | NR | NR | NR |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garibay-Lagos, C.S.; Martos-Boira, M.I.; Landeta-Iza, E.; Contreras-González, G.B.; Wanden-Berghe, C.; Sanz-Valero, J. Occupational Health of Health-Care Workers with Overnutrition: Scoping Review with Meta-Analysis. Nutrients 2023, 15, 3416. https://doi.org/10.3390/nu15153416
Garibay-Lagos CS, Martos-Boira MI, Landeta-Iza E, Contreras-González GB, Wanden-Berghe C, Sanz-Valero J. Occupational Health of Health-Care Workers with Overnutrition: Scoping Review with Meta-Analysis. Nutrients. 2023; 15(15):3416. https://doi.org/10.3390/nu15153416
Chicago/Turabian StyleGaribay-Lagos, Cynthia Sarah, Maria Isabel Martos-Boira, Elizabeth Landeta-Iza, Giselle Beatriz Contreras-González, Carmina Wanden-Berghe, and Javier Sanz-Valero. 2023. "Occupational Health of Health-Care Workers with Overnutrition: Scoping Review with Meta-Analysis" Nutrients 15, no. 15: 3416. https://doi.org/10.3390/nu15153416
APA StyleGaribay-Lagos, C. S., Martos-Boira, M. I., Landeta-Iza, E., Contreras-González, G. B., Wanden-Berghe, C., & Sanz-Valero, J. (2023). Occupational Health of Health-Care Workers with Overnutrition: Scoping Review with Meta-Analysis. Nutrients, 15(15), 3416. https://doi.org/10.3390/nu15153416






