Description of Baseline Nutrition and Physical Activity Knowledge and Behavior in Acute Stroke/TIA Patients Enrolled in the Health Education on Information Retention and Behavior Change in Stroke (HERBS) Pilot Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Evaluations
2.4. Data Analysis
3. Results
3.1. Nutrition Knowledge
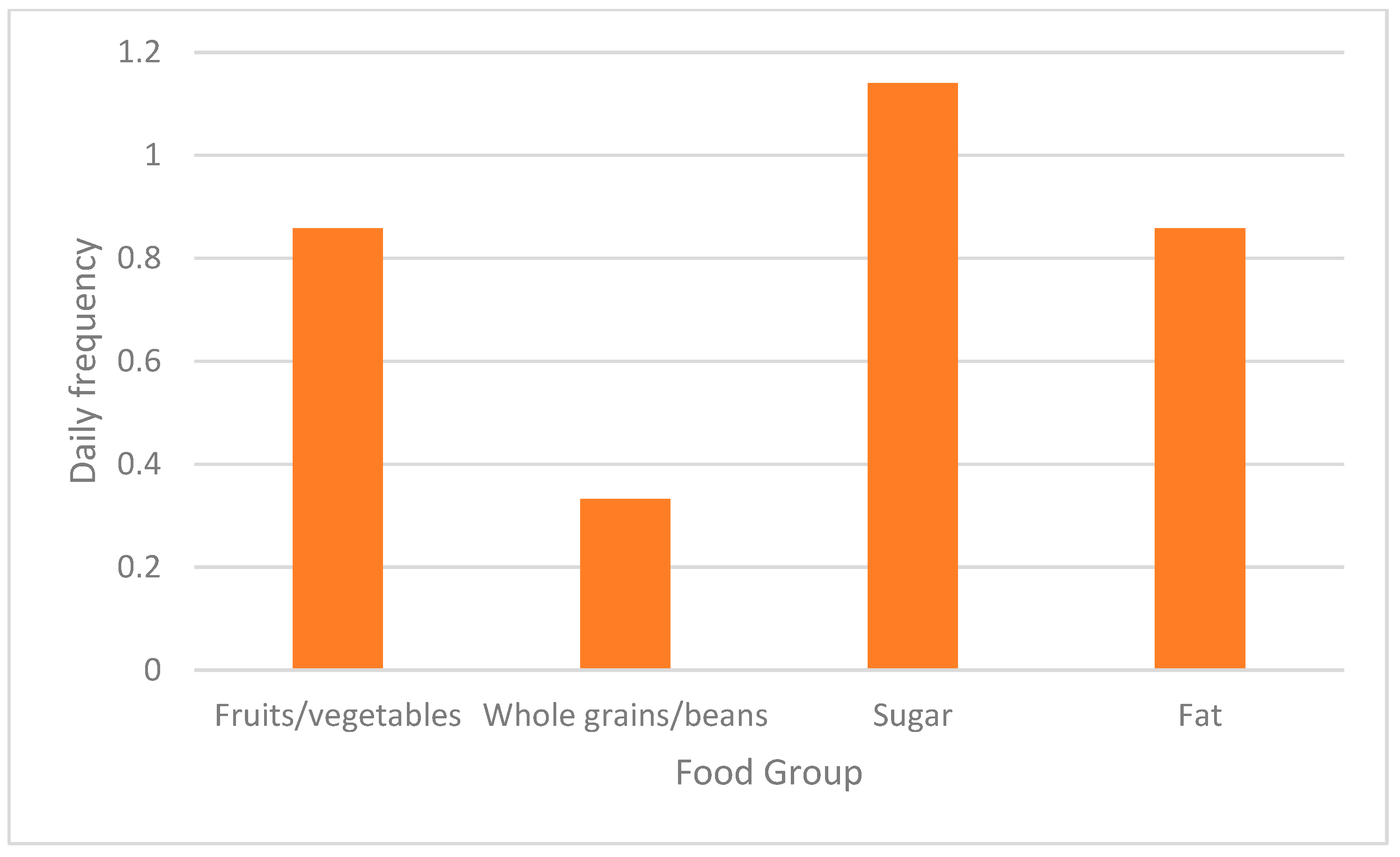
3.2. Nutrition Behavior
3.3. Physical Activity Knowledge
3.4. Physical Activity Behavior
3.5. Combined Knowledge
3.6. Combined Behavior
3.7. Self-Efficacy
3.8. Behavior Intent
3.9. Stage of Change
3.10. Barriers to Change
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pandian, J.D.; Gall, S.L.; Kate, M.P.; Silva, G.S.; Akinyemi, R.O.; Ovbiagele, B.I.; Lavados, P.M.; Gandhi, D.B.C.; Thrift, A.G. Prevention of stroke: A global perspective. Lancet 2018, 392, 1269–1278. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez, J.; Esenwa, C. Secondary stroke prevention: Challenges and solutions. Vasc. Health Risk Manag. 2015, 11, 437–450. [Google Scholar] [CrossRef] [PubMed]
- Towfighi, A.; Markovic, D.; Ovbiagele, B. Impact of a healthy lifestyle on all-cause and cardiovascular mortality after stroke in the USA. J. Neurol. Neurosurg. Psychiatry 2012, 83, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.P.; Ovbiagele, B.; Markovic, D.; Towfighi, A. “Life’s simple 7” and long-term mortality after stroke. J. Am. Heart Assoc. 2015, 4, e001470. [Google Scholar] [CrossRef]
- Neuhouser, M.L. The importance of healthy dietary patterns in chronic disease prevention. Nutr. Res. 2019, 70, 3–6. [Google Scholar] [CrossRef]
- Saint-Maurice, P.F.; Graubard, B.I.; Troiano, R.P.; Berrigan, D.; Galuska, D.A.; Fulton, J.E.; Matthews, C.E. Estimated Number of Deaths Prevented Through Increased Physical Activity Among US Adults. JAMA Intern. Med. 2022, 182, 349–352. [Google Scholar] [CrossRef]
- Van Horn, L.; Carson, J.A.S.; Appel, L.J.; Burke, L.E.; Economos, C.; Karmally, W.; Lancaster, K.; Lichtenstein, A.H.; Johnson, R.K.; Thomas, R.J.; et al. Recommended dietary pattern to achieve adherence to the American Heart Association/American College of Cardiology (AHA/ACC) guidelines: A scientific statement from the American Heart Association. Circulation 2016, 134, e505–e529. [Google Scholar] [CrossRef]
- da Costa, G.G.; Nepomuceno, G.d.C.; Pereira, A.d.S.; Simões, B.F.T. Worldwide dietary patterns and their association with socioeconomic data: An ecological exploratory study. Global Health 2022, 18, 6. [Google Scholar] [CrossRef]
- McDonnell, M.N.; Hillier, S.L.; Hooker, S.P.; Le, A.; Judd, S.E.; Howard, V.J. Physical activity frequency and risk of incident stroke in a national us study of blacks and whites. Stroke 2013, 44, 2519–2524. [Google Scholar] [CrossRef]
- Tran, P.; Tran, L.; Tran, L. A Cross-Sectional Analysis of Differences in Physical Activity Levels between Stroke Belt and Non-Stroke Belt US Adults. J. Stroke Cerebrovasc. Dis. 2019, 28, 104432. [Google Scholar] [CrossRef]
- WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 23 April 2021).
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Anderson, E.S.; Winett, R.A.; Wojcik, J.R. Self-regulation, self-efficacy, outcome expectations, and social support: Social cognitive theory and nutrition behavior. Ann. Behav. Med. 2007, 34, 304–312. [Google Scholar] [CrossRef] [PubMed]
- Joseph, R.P.; Ainsworth, B.E.; Mathis, L.; Hooker, S.P.; Keller, C. Utility of Social Cognitive Theory in Intervention Design for Promoting Physical Activity among African-American Women: A Qualitative Study. Am. J. Health Behav. 2017, 41, 518–533. [Google Scholar] [CrossRef] [PubMed]
- Greenlund, K.J.; Giles, W.H.; Keenan, N.L.; Croft, J.B.; Mensah, G.A. Physician Advice, Patient Actions, and Health-Related Quality of Life in Secondary Prevention of Stroke Through Diet and Exercise. Stroke 2002, 33, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Choi-Kwon, S.; Lee, S.; Park, H.; Kwon, S.; Ahn, J.; Kim, J. What stroke patients want to know and what medical professionals think they should know about stroke: Korean perspectives. Patient Educ. Couns. 2005, 56, 85–92. [Google Scholar] [CrossRef]
- Vetter, M.L.; Herring, S.J.; Sood, M.; Shah, N.R.; Kalet, A.L. What do resident physicians know about nutrition? An evaluation of attitudes, self-perceived proficiency and knowledge. J. Am. Coll. Nutr. 2008, 27, 287–298. [Google Scholar] [CrossRef]
- Benameur, K. Nutritional knowledge and counseling of stroke patients by neurology residents (P3.3-019). Neurology 2019, 92 (Suppl. S15). Available online: https://n.neurology.org/content/92/15_Supplement/P3.3-019 (accessed on 23 April 2021).
- Aspry, K.E.; Van Horn, L.; Carson JA, S.; Wylie-Rosett, J.; Kushner, R.F.; Lichtenstein, A.H.; Devries, S.; Freeman, A.M.; Crawford, A.; Kris-Etherton, P.; et al. Medical nutrition education, training, and competencies to advance guideline-based diet counseling by physicians: A science advisory from the American Heart Association. Circulation 2018, 137, e821–e841. [Google Scholar] [CrossRef]
- Adams, K.M.; Butsch, W.S.; Kohlmeier, M. The State of Nutrition Education at US Medical Schools. J. Biomed. Educ. 2015, 2015, 357627. [Google Scholar] [CrossRef]
- Dietary Screener Questionnaire in the NHANES 2009-10: Background [Internet]. EGRP/DCCPS/NCI/NIH. Available online: https://epi.grants.cancer.gov/nhanes/dietscreen/ (accessed on 1 March 2021).
- Converting Frequency Responses to Daily Frequency. [Internet]. EGRP/DCCPS/NCI/NIH. Available online: https://epi.grants.cancer.gov/nhanes/dietscreen/scoring/current/convert.html (accessed on 23 April 2021).
- Hekler, E.B.; Buman, M.P.; Haskell, W.L.; Conway, T.L.; Cain, K.L.; Sallis, J.F.; Saelens, B.E.; Frank, L.D.; Kerr, J.; King, A.C. Reliability and validity of CHAMPS self-reported sedentary-to-vigorous intensity physical activity in older adults. J. Phys. Act. Health 2012, 9, 225–236. [Google Scholar] [CrossRef]
- American Heart Association Recommendations for Physical Activity in Adults and Kids [Internet]. 2018. Available online: https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults (accessed on 23 April 2021).
- Fruits and Vegetables Serving Sizes Infographic [Internet]. 2017. Available online: https://www.heart.org/en/healthy-living/healthy-eating/add-color/fruits-and-vegetables-serving-sizes (accessed on 23 April 2021).
- Serving Size Visuals [Internet]. Available online: https://www.heart.org/idc/groups/heart-public/@wcm/@global/documents/downloadable/ucm_321862.pdf (accessed on 23 April 2021).
- Decker, J.W.; Dennis, K.E. The Eating Habits Confidence Survey: Reliability and validity in overweight and obese postmenopausal women. J. Nurs. Meas. 2013, 21, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Pinski, R.B.; Grossman, R.M.; Patterson, T.L.; Nader, P.R. The development of self-efficacy scales for health-related diet and exercise behaviors. Health Educ. Res. 1988, 3, 283–292. [Google Scholar] [CrossRef]
- Prochaska, J.O.; DiClemente, C.C. Stages and processes of self-change of smoking: Toward an integrative model of change. J. Consult. Clin. Psychol. 1983, 51, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Wessa, P. Cronbach alpha (v1.0.5) in Free Statistics Software (v1.2.1). Office for Research Development and Education. 2017. Available online: https://www.wessa.net/rwasp_cronbach.wasp/ (accessed on 15 May 2021).
- Adinkrah, E.; Bazargan, M.; Wisseh, C.; Assari, S. Adherence to Hypertension Medications and Lifestyle Recommendations among Underserved African American Middle-Aged and Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 6538. [Google Scholar] [CrossRef]
- Benton, D. Portion size: What we know and what we need to know. Crit. Rev. Food Sci. Nutr. 2015, 55, 988–1004. [Google Scholar] [CrossRef]
- Kruskall, L.J. Portion Distortion. ACSM’s Health Fit. J. 2006, 10, 8–14. [Google Scholar] [CrossRef]
- Towfighi, A.; Cheng, E.M.; Hill, V.A.; Barry, F.; Lee, M.; Valle, N.P.; Mittman, B.; Ayala-Rivera, M.; Moreno, L.; Espinosa, A.; et al. Results of a Pilot Trial of a Lifestyle Intervention for Stroke Survivors: Healthy Eating and Lifestyle after Stroke. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2020, 29, 105323. [Google Scholar] [CrossRef]
- Hill, V.A.; Vickrey, B.G.; Cheng, E.M.; Valle, N.P.; Ayala-Rivera, M.; Moreno, L.; Munoz, C.; Dombish, H.; Espinosa, A.; Wang, D.; et al. A Pilot Trial of a Lifestyle Intervention for Stroke Survivors: Design of Healthy Eating and Lifestyle after Stroke (HEALS). J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2017, 26, 2806–2813. [Google Scholar] [CrossRef]
- Heredia, N.I.; Fernandez, M.E.; Berg, A.E.v.D.; Durand, C.P.; Kohl, H.W.; Reininger, B.M.; Hwang, K.O.; McNeill, L.H. Coaction Between Physical Activity and Fruit and Vegetable Intake in Racially Diverse, Obese Adults. Am. J. Health Promot. 2020, 34, 238–246. [Google Scholar] [CrossRef]
- Smith, M.L.; Lee, S.; Towne, S.D.; Han, G.; Quinn, C.; Peña-Purcell, N.C.; Ory, M.G. Impact of a Behavioral Intervention on Diet, Eating Patterns, Self-Efficacy, and Social Support. J. Nutr. Educ. Behav. 2020, 52, 180–186. [Google Scholar] [CrossRef]
- Pawlak, R.; Colby, S. Benefits, barriers, self-efficacy and knowledge regarding healthy foods; perception of African Americans living in eastern North Carolina. Nutr. Res. Pract. 2009, 3, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Zazo, F.; Romero-Blanco, C.; Castro-Lemus, N.; Dorado-Suárez, A.; Aznar, S. Transtheoretical Model for Physical Activity in Older Adults: Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 9262. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Psouni, S.; Hassandra, M.; Theodarakis, Y. Exercise and Healthy Eating Intentions and Behaviors among Normal Weight and Overweight/Obese Adults. Psychology 2016, 7, 598–611. [Google Scholar] [CrossRef][Green Version]
- Muschalik, C.; Elfeddali, I.; Candel, M.J.J.M.; de Vries, H. A longitudinal study on how implicit attitudes and explicit cognitions synergistically influence physical activity intention and behavior. BMC Psychol. 2018, 6, 18. [Google Scholar] [CrossRef] [PubMed]
- Centis, E.; Trento, M.; Cas, A.D.; Pontiroli, A.E.; De Feo, P.; Bruno, A.; Sasdelli, A.S.; Arturi, F.; Strollo, F.; Kreutzenberg, S.V.D.; et al. Stage of change and motivation to healthy diet and habitual physical activity in type 2 diabetes. Acta Diabetol. 2014, 5, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Siero, F.W.; Broer, J.; Bemelmans, W.J.E.; Jong, B.M.M.-D. Impact of group nutrition education and surplus value of Prochaska-based stage-matched information on health-related cognitions and on Mediterranean nutrition behavior. Health Educ. Res. 2000, 5, 635–647. [Google Scholar] [CrossRef]
- Brug, J.; Oenema, A.; Campbell, M. Past, present, and future of computer-tailored nutrition education. Am. J. Clin. Nutr. 2003, 77 (Suppl. S4), 1028S–1034S. [Google Scholar] [CrossRef]
- Wallace, R.; Lo, J.; Devine, A. Tailored Nutrition Education in the Elderly Can Lead to Sustained Dietary Behaviour Change. J. Nutr. Health Aging 2016, 20, 8–15. [Google Scholar] [CrossRef]
- Zimmerman, G.L.; Olsen, C.G.; Bosworth, M.F. A ‘Stages of Change’ Approach to Helping Patients Change Behavior. Am. Fam. Physician 2000, 61, 1409–1416. [Google Scholar]
- Motivational Interviewing–Stages of Change. [Internet] Massachusetts Behavioral Health Partnership. Available online: https://www.masspartnership.com/pdf/MotivationalInterviewingStagesofChange.pdf (accessed on 23 April 2021).
- Knight, C.J.; Jackson, O.; Rahman, I.; Burnett, D.O.; Frugé, A.D.; Greene, M.W. The Mediterranean Diet in the Stroke Belt: A Cross-Sectional Study on Adherence and Perceived Knowledge, Barriers, and Benefits. Nutrients 2019, 11, 1847. [Google Scholar] [CrossRef] [PubMed]
- Mc Morrow, L.; Ludbrook, A.; Macdiarmid, J.; Olajide, D. Perceived barriers towards healthy eating and their association with fruit and vegetable consumption. J. Public Health 2017, 39, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Lim, R.B.T.; Wee, W.K.; For, W.C.; Ananthanarayanan, J.A.; Soh, Y.H.; Goh, L.M.L.; Tham, D.K.T.; Wong, M.L. Correlates, facilitators and barriers of physical activity among primary care patients with prediabetes in Singapore—A mixed methods approach. BMC Public Health 2020, 20, 1. [Google Scholar] [CrossRef]
- Herazo-Beltrán, Y.; Pinillos, Y.; Vidarte, J.; Crissien, E.; Suarez, D.; García, R. Predictors of perceived barriers to physical activity in the general adult population: A cross-sectional study. Braz. J. Phys. Ther. 2017, 21, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, S.L.; Donaghy, M.; Johnston, M.; Sniehotta, F.F.; Van Wijck, F.; Johnston, D.; Greig, C.; McMurdo, M.E.T.; Mead, G. A qualitative theory guided analysis of stroke survivors’ perceived barriers and facilitators to physical activity. Disabil. Rehabil. 2014, 36, 1857–1868. [Google Scholar] [CrossRef]
- Damush, T.M.; Plue, L.; Bakas, T.; Schmid, A.; Williams, L.S. Barriers and facilitators to exercise among stroke survivors. Rehabil. Nurs. Off. J. Assoc. Rehabil. Nurses 2017, 32, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Simpson, L.A.; Eng, J.J.; Tawashy, A.E. Exercise perceptions among people with stroke: Barriers and facilitators to participation. Int. J. Ther. Rehabil. 2011, 18, 520–530. [Google Scholar] [CrossRef]
- Débora Pacheco, B.; Guimaraes Caetano, L.C.; Amorim Samora, G.; Sant’Ana, R.; Fuscaldi Teixeira-Salmela, L.; Scianni, A.A. Perceived barriers to exercise reported by individuals with stroke, who are able to walk in the community. Disabil. Rehabil. 2021, 43, 331–337. [Google Scholar] [CrossRef]




| Race/Ethnicity, n (%) | |
| White | 3 (10.7) |
| Black | 14 (50.0) |
| Hispanic | 4 (14.3) |
| Other | 1 (3.6) |
| Unable to determine | 6 (21.4) |
| Age, mean (SD) (years) | 61.7 (11.8) |
| Sex, n (%) | |
| Male | 13(46.4) |
| Highest level of education completed, n (%) | |
| <12 years of education | 8 (28.6) |
| High school graduate or GED | 8 (28.6) |
| >12 years of education | 12 (42.9) |
| Marital Status, n (%) | |
| Married or domestic partnership | 16 (57.1) |
| Without a partner (divorced, widowed, single) | 12 (42.9) |
| Lives alone, n (%) | |
| Yes | 8 (28.6) |
| Annual Income, n (%) | |
| ≤49,999 | 15 (53.6) |
| >$49,999 | 10 (35.7) |
| Decline to answer NIHSS, median (IQR) | 3 (10.7) 4.0 (3.0, 7.0) |
| Labs on Admission | |
| Creatinine, median (IQR) (mg/dL) | 1.0 (0.9, 1.2) |
| Cholesterol, total, median (IQR) (mg/dL) | 170.0 (133.0, 197.0) |
| Cholesterol, LDL, mean (SD) (mg/dL) | 99.9 (41.9) |
| Cholesterol, HDL, mean (SD) (mg/dL) | 50.9 (13.2) |
| Triglycerides, median (IQR) (mg/dL) | 106.0 (67.0, 130.0) |
| Glucose, median (IQR) (mg/dL) | 105.5 (94.0, 179.0) |
| Glycated Hemoglobin, median (IQR) (%) | 5.9 (5.4, 7.5) |
| Weight, median (IQR) (kg) | 84.1 (77.3, 102.3) |
| BMI, median (IQR) (kg/m2) | 31.0 (25.1, 38.9) |
| Systolic BP on admission, mean (SD), mm Hg | 144.7 (23.8) |
| Diastolic BP on admission, mean (SD), mm Hg | 82.2 (18.0) |
| tPA administered, n (%) | |
| Yes | 7 (25.0) |
| Intra-arterial therapy, n (%) | |
| Yes | 4 (14.3) |
| Discharge Diagnosis, n (%) | |
| TIA | 2 (7.1) |
| Stroke | 26 (92.9) |
| Hospital Length of Stay (days), median (IQR) | 5.0 (2.0, 8.0) |
| Discharge Location, n (%) | |
| Home | 18 (64.3) |
| Other | 10 (35.7) |
| Stroke Etiology *, n (%) | |
| Small artery occlusion | 7 (25.0) |
| Large artery occlusion | 5 (17.9) |
| Cardioembolic | 5 (17.9) |
| Undetermined/cryptogenic | 11 (39.3) |
| Medications prior to admission, n (%) | |
| Antiplatelet | 13 (46.4) |
| Anticoagulant | 0 (0) |
| Beta blocker | 8 (28.6) |
| ACEi/ARB | 8 (28.6) |
| Other anti-hypertensive | 12 (42.9) |
| Diabetic agents | 6 (21.4) |
| Statin | 11 (39.3) |
| Reported medication compliance, n (%) | |
| No | 2 (7.1) |
| Yes | 5 (17.9) |
| Unable to determine ᵞ | 15 (53.6) |
| Not applicable | 6 (21.4) |
| Nutrition Knowledge rs (p Value) | Healthy Diet rs (p Value) | Healthy Diet, Fruit and Vegetable rs (p Value) | Healthy Diet, Whole Grains rs (p Value) | Unhealthy Diet rs (p Value) | Unhealthy Diet, Fat rs (p Value) | Unhealthy Diet, Added Sugars rs (p Value) | Physical Activity Knowledge rs (p Value) | Physical Activity Behavior rs (p Value) | |
|---|---|---|---|---|---|---|---|---|---|
| Nutrition knowledge | N.A. | 0.189 (0.335) | 0.255 (0.190) | −0.064 (0.746) | −0.120 (0.543) | −0.063 (0.749) | −0.141 (0.474) | 0.088 (0.663) | 0.080 (0.686) |
| Healthy diet | 0.189 (0.335) | N.A. | 0.909 (<0.001) | 0.620 (<0.001) | 0.274 (0.158) | 0.265 (0.172) | 0.127 (0.521) | −0.330 (0.092) | 0.256 (0.188) |
| Healthy diet, fruit and vegetables | 0.255 (0.190) | 0.909 (<0.001) | N.A. | 0.265 (0.173) | 0.362 (0.059) | 0.340 (0.076) | 0.216 (0.269) | −0.245 (0.218) | 0.239 (0.221) |
| Healthy diet, whole grains | −0.064 (0.746) | 0.620 (<0.001) | 0.265 (0.173) | N.A. | 0.017 (0.933) | −0.0001 (0.100) | −0.007 (0.972) | −0.327 (0.096) | 0.239 (0.221) |
| Unhealthy diet | −0.120 (0.543) | 0.274 (0.158) | 0.362 (0.059) | 0.017 (0.933) | N.A. | 0.758 (<0.001) | 0.851 (<0.001) | 0.133 (0.508) | −0.185 (0.346) |
| Unhealthy diet, fat | −0.0633 (0.749) | 0.265 (0.172) | 0.341 (0.076) | −0.0001 (0.100) | 0.758 (<0.001) | N.A. | 0.393 (0.039) | 0.231 (0.246) | −0.103 (0.604) |
| Unhealthy diet, added sugars | −0.141 (0.474) | 0.127 (0.521) | 0.216 (0.269) | −0.007 (0.972) | 0.851 (<0.001) | 0.393 (0.039) | N.A. | 0.101 (0.617) | −0.058 (0.770) |
| Physical activity knowledge | 0.088 (0.663) | −0.330 (0.092) | −0.245 (0.218) | −0.189 (0.336) | 0.133 (0.508) | 0.231 (0.246) | 0.101 (0.617) | N.A. | 0.091 (0.653) |
| Physical Activity behavior | 0.799 (0.686) | 0.256 (0.188) | 0.239 (0.221) | 0.170 (0.387) | −0.185 (0.346) | −0.105 (0.604) | −0.0579 (0.770) | 0.091 (0.653) | N.A. |
| Combined Knowledge rs (p Value) | Combined Behavior rs (p Value) | Self-Efficacy rs (p Value) | Behavioral Intent rs (p Value) | |
|---|---|---|---|---|
| Combined knowledge | N.A. | −0.010 (0.961) | 0.210 (0.283) | −0.012 (0.954) |
| Combined behavior | −0.010 (0.961) | N.A. | 0.385 (0.043) | 0.229 (0.242) |
| Self-efficacy | 0.210 (0.283) | 0.385 (0.043) | N.A. | 0.284 (0.143) |
| Behavioral intent | −0.012 (0.954) | 0.229 (0.242) | 0.284 (0.143) | N.A. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uhlig-Reche, H.; Ontiveros, D.; Syzdek, R.; Mathews, P.; Dalal, L.; Amaro, A.; Wunnava, N.; Housammy, Z.; Schmitt, B.; Sharrief, A.; et al. Description of Baseline Nutrition and Physical Activity Knowledge and Behavior in Acute Stroke/TIA Patients Enrolled in the Health Education on Information Retention and Behavior Change in Stroke (HERBS) Pilot Trial. Nutrients 2023, 15, 3761. https://doi.org/10.3390/nu15173761
Uhlig-Reche H, Ontiveros D, Syzdek R, Mathews P, Dalal L, Amaro A, Wunnava N, Housammy Z, Schmitt B, Sharrief A, et al. Description of Baseline Nutrition and Physical Activity Knowledge and Behavior in Acute Stroke/TIA Patients Enrolled in the Health Education on Information Retention and Behavior Change in Stroke (HERBS) Pilot Trial. Nutrients. 2023; 15(17):3761. https://doi.org/10.3390/nu15173761
Chicago/Turabian StyleUhlig-Reche, Hannah, Diana Ontiveros, Riley Syzdek, Patenne Mathews, Leanne Dalal, Andrea Amaro, Nidhi Wunnava, Zina Housammy, Barrie Schmitt, Anjail Sharrief, and et al. 2023. "Description of Baseline Nutrition and Physical Activity Knowledge and Behavior in Acute Stroke/TIA Patients Enrolled in the Health Education on Information Retention and Behavior Change in Stroke (HERBS) Pilot Trial" Nutrients 15, no. 17: 3761. https://doi.org/10.3390/nu15173761
APA StyleUhlig-Reche, H., Ontiveros, D., Syzdek, R., Mathews, P., Dalal, L., Amaro, A., Wunnava, N., Housammy, Z., Schmitt, B., Sharrief, A., & Gonzales, N. R. (2023). Description of Baseline Nutrition and Physical Activity Knowledge and Behavior in Acute Stroke/TIA Patients Enrolled in the Health Education on Information Retention and Behavior Change in Stroke (HERBS) Pilot Trial. Nutrients, 15(17), 3761. https://doi.org/10.3390/nu15173761





